Professional Documents
Culture Documents
Clinical Toxicology Lab Activity8
Uploaded by
Josefina Carmen RoaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Toxicology Lab Activity8
Uploaded by
Josefina Carmen RoaCopyright:
Available Formats
Roa, Josefina Carmen P.
June 4,
2021
Activity No. 8
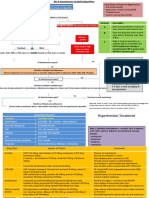
Management of Poisoning
(Cardiovascular System Involvement)
Explain how the following occur during poisoning and give emergency measures in correcting:
Occurrence Emergency Measures
a. Circulatory failure or Cardiotropic drugs may 1. Check if the patient is
shock compromise cardiac output conscious.
leading to circulatory shock at 2. Open the airway and make
toxic doses sure the tongue is not
blocking the throat.
3. Check if the patient is
breathing.
4. Clean out the mouth and
clear the throat.
5. Give mouth-to-mouth
respiration.
6. Check if the heart is
beating.
7. If the heart is beating, but
the patient is still not
breathing, carry on with
mouth-to-mouth respiration.
8. If the heart is not beating,
give heart massage.
9. If the patient is breathing
but is unconscious, turn him
or her onto one side, into the
recovery position.
10. Give first aid for fits if
necessary.
11. Call local emergency
service.
Specific treatment varies
depending on the nature and
the dose of the drugs
ingested as well as causal
mechanism including
vasopegia, hypovolaemia,
cardiogenic effects and
sepsis.
b. Congestive heart failure Poisons can reduce cardiac Beta-blockers, ACE
contractility, resulting in a inhibitors, glycosides, and
decrease in the cardiac ejection diuretics are the key
fraction and cardiac output, medications used for
hypotension, and development of managing congestive heart
congestive heart failure failure through regulating
renal function and the
sympathetic nervous
system.
c. Cardiac arrest Cardiac arrest can be caused by A rescuer who finds
anything that causes death. One
common cause, especially in someone unconscious
adults, is an abnormal heart should first determine if the
rhythm (arrhythmia). Another person is unresponsive by
possible cause is stopping
breathing, such as when a shaking the person and
person drowns or has severe loudly asking, "Are you OK?"
pneumonia. If there is no response, the
rescuer should turn the
person's body face up and
look to determine whether
breathing has also stopped.
If the person does not
respond to stimulation and is
not breathing or is breathing
abnormally (for example,
gasping), emergency
resuscitation measures are
begun and emergency
medical assistance should
be sought, for example, by
calling 911 or the local
emergency service.
2 (two) CPR methods:
Standard (done by
rescuers trained in
standard CPR)
Compression only
(done by rescuers
untrained in—or
reluctant to do—
artificial respiration)
References:
Kaji, AH, et al. 2020. MSD Manual Consumer Version. Injuries and Poisoning. First Aid.
Retrieved from https://www.msdmanuals.com/home/injuries-and-poisoning/first-
aid/cardiac-arrest
Klaassen, CD. 2013. Casarett & Doull’s Toxicology: The Basic Science of Poison. 8 th Edition.
Toxicant-Neurotransmitter Receptor Interactions. P77
Li, C, Miller, WT, Jiang, J. 2001. Pulmonary edema due to ingestion of organophosphate
insecticide. Am J Roentgenol. 1989;152(2):265–266. P.2. Retrieved from
https://www.ajronline.org/doi/pdfplus/10.2214/ajr.152.2.265
Physiopedia contributors. 2021. Pharmacological Managem ent of Congestive Heart Failur e.
Physiopedia. 275568. Retrieved from https://www.physio-
pedia.com/index.php?title=Pharmacological_Management_of_Congestive_Heart_Fa
ilure&oldid=275568
Taboulet P, Bismuth C. 1994. Collapsus par intoxication. Utilisation des agents cardiotropes
[Shock caused by poisoning. Use of cardiotropic agents]. Presse Med. 1994 Sep
17;23(27):1263-8. French. PMID: 7971861. Retrieved from
https://pubmed.ncbi.nlm.nih.gov/7971861/
Whitworth, G. 2019. Healthline: What is Pulmonary Edema? Retreived from
https://www.healthline.com/health/pulmonary-edema#treatment
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Pharmacology Notes NursingDocument25 pagesPharmacology Notes NursingKyle Marks100% (5)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Heart Blocks: "The Heart Block Poem"Document18 pagesHeart Blocks: "The Heart Block Poem"Bijay Kumar Mahato100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Adrenergic AntagonistsDocument6 pagesAdrenergic Antagonistsfiena92100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Understanding HemodynamicsDocument21 pagesUnderstanding HemodynamicsGiovanni Mictil86% (7)
- Pharmacology - Lecture Notes, Study Material and Important Questions, AnswersDocument236 pagesPharmacology - Lecture Notes, Study Material and Important Questions, AnswersM.V. TVNo ratings yet
- 1 Drugs For HypertensionDocument62 pages1 Drugs For HypertensionSaniNo ratings yet
- Hypertension Urgency and EmergencyDocument8 pagesHypertension Urgency and EmergencySanditia GumilangNo ratings yet
- ACLS Review TestDocument5 pagesACLS Review Testtostc60% (5)
- Dds Lab MidtermsDocument4 pagesDds Lab MidtermsJosefina Carmen RoaNo ratings yet
- Dds Lab MidtermsDocument4 pagesDds Lab MidtermsJosefina Carmen RoaNo ratings yet
- Vasodilators 1233318450814478 3Document29 pagesVasodilators 1233318450814478 3Nehal AmjadNo ratings yet
- English Translation:: Falling in Love by 2NE1Document3 pagesEnglish Translation:: Falling in Love by 2NE1Josefina Carmen RoaNo ratings yet
- Dreaming Alone ChordsDocument2 pagesDreaming Alone ChordsJosefina Carmen RoaNo ratings yet
- Ice Cream CakeDocument3 pagesIce Cream CakeJosefina Carmen RoaNo ratings yet
- Heels Over HeadDocument2 pagesHeels Over HeadJosefina Carmen RoaNo ratings yet
- Tongue TiedDocument3 pagesTongue TiedJosefina Carmen RoaNo ratings yet
- Nobody's HomeDocument1 pageNobody's HomeJosefina Carmen RoaNo ratings yet
- C.H.A.O.S.M.Y.T.H. Yokubou Ni Michi Ta SeinendanDocument3 pagesC.H.A.O.S.M.Y.T.H. Yokubou Ni Michi Ta SeinendanJosefina Carmen RoaNo ratings yet
- Clinical Patient CaseDocument1 pageClinical Patient CaseJosefina Carmen RoaNo ratings yet
- Wa0027Document20 pagesWa0027Ahmed ElshiekhNo ratings yet
- Decompensated Congestive Cardiac Failure Secondary To No1Document4 pagesDecompensated Congestive Cardiac Failure Secondary To No1Qi YingNo ratings yet
- The Cardiovascular Effects of CocaineDocument13 pagesThe Cardiovascular Effects of CocaineRoberto López Mata100% (1)
- The Ultimate Krok2 Companion Comprehensive Explanations and InsiDocument263 pagesThe Ultimate Krok2 Companion Comprehensive Explanations and InsiRamy Aso ZainalNo ratings yet
- Myocardial Infarction Medication: Aspirin (Ascriptin, Bayer Aspirin, Aspirtab, Ecotrin, Durlaza)Document11 pagesMyocardial Infarction Medication: Aspirin (Ascriptin, Bayer Aspirin, Aspirtab, Ecotrin, Durlaza)Ashutosh SinghNo ratings yet
- HCM 2020 GuidelinesDocument81 pagesHCM 2020 Guidelinesdipak patadeNo ratings yet
- CLORPROMAZINDocument15 pagesCLORPROMAZINphantomboyzNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument6 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- Hypertension Nursing Care Plan..nkDocument16 pagesHypertension Nursing Care Plan..nkchishimba louisNo ratings yet
- Diabetes and Cardiovascular DiseaseDocument119 pagesDiabetes and Cardiovascular DiseaseAlina PopaNo ratings yet
- Which of The Following H1 Antihistamines Is Non SedatingDocument7 pagesWhich of The Following H1 Antihistamines Is Non SedatingJafer DetamoNo ratings yet
- Sympathetic Agonist and Antagonist 23Document12 pagesSympathetic Agonist and Antagonist 23PNo ratings yet
- 2014-JNC-8-Hypertension WRDocument2 pages2014-JNC-8-Hypertension WRismailuntung0% (1)
- LO Dan WO Cardio Week 4 (Jumat)Document38 pagesLO Dan WO Cardio Week 4 (Jumat)Alan Dwi SetiawanNo ratings yet
- Myocardial Infarction 2017Document12 pagesMyocardial Infarction 2017Mateo Daniel Gutierrez CastañedaNo ratings yet
- Copy 1 of Treatment Profile For Intern Docto 2Document57 pagesCopy 1 of Treatment Profile For Intern Docto 2AminulNo ratings yet
- Mi (Case # 1) : 1. How Would You Classify Mr. Smith's Chest Pain?Document11 pagesMi (Case # 1) : 1. How Would You Classify Mr. Smith's Chest Pain?Faizan MazharNo ratings yet
- Beta-Blocker Use in Pregnancy and Risk of SpecificDocument13 pagesBeta-Blocker Use in Pregnancy and Risk of SpecificpyprattNo ratings yet
- Emergency Drug Review: UHHS BMH Paramedic Training ProgramDocument116 pagesEmergency Drug Review: UHHS BMH Paramedic Training ProgramShailja HanumantaNo ratings yet
- Cardiology High Blood Pressure - University of Nigeria Nsukka 73rd-Inaugural-Lecture - OnwubereDocument29 pagesCardiology High Blood Pressure - University of Nigeria Nsukka 73rd-Inaugural-Lecture - OnwubereAnonymous 9QxPDpNo ratings yet
- Beta-Blockers For Hypertension (Review) : Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Mbewu A, Opie LHDocument3 pagesBeta-Blockers For Hypertension (Review) : Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Mbewu A, Opie LHAntônio GoulartNo ratings yet