Professional Documents
Culture Documents
JCDR 9 ZC39
Uploaded by
Raluca ChisciucOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JCDR 9 ZC39
Uploaded by
Raluca ChisciucCopyright:
Available Formats
DOI: 10.7860/JCDR/2015/14580.
6488
Original Article
Effect of Cigarette Smoke on Surface
Dentistry Section
Roughness of Different Denture
Base Materials
Hamada Zaki Mahross1, Mahmoud Darwish Mohamed2, Ahmed Mohammed Hassan3, Kusai Baroudi4
ABSTRACT the smoke test groups used for exposure to cigarette smoking.
Background: Surface roughness is an important property of The smoke test groups specimens were exposed to smoking
denture bases since denture bases are in contact with oral in a custom made smoking chamber by using 20 cigarettes for
tissues and a rough surface may affect tissues health due to each specimen. The surface roughness was measured by using
microorganism accumulation. Therefore, the effect of cigarette Pocket SurfPS1 profilometer and the measurements considered
smoke on the surface roughness of two commercially available as the difference between the initial and final roughness
denture base materials was evaluated to emphasize which type measured before and after smoking.
has superior properties for clinical use. Results: The t-test for paired observation of test specimens
Materials and Methods: A total numbers of 40 specimens after exposure to smoking was indicated significant change in
were constructed from two commercially available denture surface roughness for Group II (p< 0.05) but has no significance
base materials; heat-cured PMMA and visible light cured UDMA with Group IV. Otherwise, there were no significant differences
resins (20 for each). The specimens for each type were randomly with control groups (Group I and III).
divided into: Group I: Heat cured resin control group; Group Conclusion: The surface roughness of the dentures constructed
II: Heat cured acrylic resin specimens exposed to cigarette from heat cured acrylic resin had been increased after exposure
smoking; Group III: Light cured resin control group; Group IV: to cigarette smoke but had no impact on the dentures
Light cured resin specimens exposed to cigarette smoking. constructed from visible light cured resin.
The control groups used for immersion in distilled water and
Keywords: Cigarette smoke, Denture base, Eclipse resin, Profilometer, Surface roughness
Introduction compounds which resulting in a biodegradation phenomenon that
Since Walter Wright first introduced it in 1937, the heat cured polymethyl altering the physical and mechanical properties of the material,
methacrylate (PMMA) polymers have referred to as conventional denture one of these is a cigarette smoking. According to the World Health
base materials and considered the most popular material for non- Organization, cigarette smoking is a public health problem reported in
metallic denture constructions. Its extensive use was due to low water almost 1.3 billion people around the world [8,10].
sorption, solubility and cost, as well as, ease of construction of denture The toxic substances of cigarettes may be in the tobacco plant or
bases by simple processing techniques with acceptable physical and produced during its burning. In case of denture wearer’s smoker
mechanical properties. Despite these favourable properties, a growing patients, the denture base materials were exposed to thousands of
number of patients are presenting with hypersensitivity reactions to
cigarettes toxic substances such as carbon monoxide, formaldehyde,
PMMA which induced by the residual methyl methacrylate monomer
radioactive polonium, ammonia, nickel, arsenic, tar and heavy metals
[1-3]. Recently, a presumably hypoallergenic resin such as visible light
such as lead and cadmium [11]. Previously, many investigators reported
activated Urethanedimethacrylate (UDMA) polymers have developed
that, cigarette smoke can change the colour, alter the microhardness
as a denture bases to surpass contact allergies, laboratory vapours
and increase the surface roughness of dental composites, highly cross
and the traditional lengthy lost wax technique which used with the
conventional PMMA materials. This system consists of special resin and linked resin teeth and other different types of denture teeth [8,12,13].
curing unit that emits high intensity light in the shorter blue wavelength Although, not many studies in literature have standardized the manner
as activated by light in the wavelength range of 460–470 nm [4-6]. of subjecting restorative materials to cigarette smoke. Such studies
Clinically, with any case the denture base material has smooth and evaluated the effect of cigarette smoke without standardizing the type
highly polished surface for patient’s comfort and for more denture of equipment used, number of cigarettes, smoke flow and time of the
longevity, good aesthetic, oral hygiene and low plaque retention [7]. material exposure to the agent [14,15]. Furthermore, literature lacks
Therefore, the surface roughness is an important property of the information regarding the effect of this common harmful oral habit on
denture bases since it is in contact with the buccal tissues and a rough different types of denture base materials.
surface may affect tissue health due to microorganism accumulation. Against this backdrop of information scarcity, this invitro study was
These microorganisms are protected from shear forces and oral undertaken to analyse the impact of cigarette smoke on surface
hygiene measures which may lead to an increase in the prevalence of roughness of heat polymerized PMMA and visible light polymerized
denture stomatitis, rate of staining, halitosis and discomfort. Therefore, UDMA. The null hypothesis undertaken was that, cigarette smoking
the surface roughness is of a great clinical relevance for dentures could increase the surface roughness of both types of denture base
success [8,9].
materials. The resulting foundation insuring that, the surface change of
In the oral cavity, the denture base materials were exposed to complex heat cured PMMA materials has occurred but no change with visible
environment that compress harmful endogenous and exogenous light cured UDMA.
Journal of Clinical and Diagnostic Research. 2015 Sep, Vol-9(9): ZC39-ZC42 39
Hamada Zaki Mahross et al., Effect of Cigarette Smoke on Surface Roughness of Different Denture Base Materials www.jcdr.net
MATERIALs AND METHODs The surface roughness (Ra) values were measured by using a pocket
A total numbers of 40 specimens were constructed from chemically profilometer ((Mar Surf PS1, Mahr, Germaine, version prog v1.01-
different two commercially available denture base materials with a 08). The pocket profilometer can measure small surface variations by
minimum thickness of 2mm to resemble the thickness of the denture moving a diamond stylus across the specimen surface [Table/Fig-1].
base clinically. The first group (Heat cured resin); 20 specimens of heat The tracing length of the instrument stylus was (5.6 mm) and a cut off
cured PMMA (Ecocryl, Hot protechno, Girona, Spain, BT 12-26964) (0.8 mm) at speed of (0.5 mm/s) [Table/Fig-2]. The stylus moved across
were prepared (10x10x2 mm) by investing the wax pattern (10x10x2 the specimen surface and three scanning lines were recorded with a
mm) in gypsum stone (LabStone, Dentsply) with a conventional flasking distance of 1 mm between each scanning line. The mean value for the
procedure in metallic denture flask. After dewaxing, the PMMA material three readings of the surface roughness was considered the measured
was mixed with its liquid, packed and processed in a thermostatically surface roughness value (Ra) for each specimen.
controlled water bath in accordance with manufacturer’s instructions. After the initial surface roughness was measured, the specimens of
The water was heated up to 80oC and maintained for 2 hours and both acrylic resins were randomly divided into four subgroups (n= 10)
then allowed to boil for further 30 minutes. After curing, the flasks were according to the treatment option. Group I: Heat cured resin control
cooled at room temperature before opening. group. Group II: Heat cured acrylic resin specimens exposed to cigarette
Another group (Light cured resin); 20 specimens of visible light cured smoking. Group III: Light cured resin control group. Group IV: Light
UDMA (Eclipse, Dentsply, New York, USA) were prepared (10x10x2 cured resin specimens exposed to cigarette smoking. For both resins
mm) in well-designed Perspex mold. By finger pressure the light type, the control groups (groups I and III) were used for immersion in
cured resins material was pressed into the mold cavity after applying distilled water at 37oC for another 48 hours and the smoke test groups
petroleum jelly and polymerization performed in light cured unit (Eclipse (group II and IV) were used for exposure to cigarette smoking.
Processing Unit, Dentsply Trubyte) at 400 to 500 nm for 10 minby The smoke test group specimens were subjected to smoking in a
exposing the sample to visible light [16]. custom made smoking chamber that simulated the process of smoking
After complete polymerization of both resins types, the specimens invivo. The study was conducted in Alfarabi collage at research unit
were retrieved from the flask for heat cured resin and from the mold for one week interval with ethical approval number 249/2015, the
for light cured resin then finished by finishing discs and stones using consent was obtained. The study was employed the smoking machine
a hand piece at low speed. Furthermore, one surface of each acrylic developed by the principles of Wasilewski S et al., in order to reproduce
specimen was finished using 280, 360 and 400 grit abrasive papers (in vitro) the smokers mouth cavity conditions but with some modification
(Middle East Factory- KSA) then polished on a wet rag wheel with slurry [13]. The modifications were done by using smaller size glass jar with
pumice. All the test specimens were stored in distilled water at 37oC silicon template fitting in its bottom to suite and fit only one specimen at
for 48 hours for residual monomer release. After incubation period, the a time and prevent the smoke from being dissipated into larger spaces
specimens were dried with air and the initial surface roughness (IRa) without changing the specimen position, also the device can receive
was measured for the polished surface of all specimens. only one cigarette at a time for trying to simulate the clinical condition.
In accordance of these principles, the chamber assembly was formed
from a glass jar of 20 ml volume tightly closed with a lid. The lid of the jar
had two opening passing two silicon tubes, one tube for snugly fit the
cigarette and the other tube fastened to a vacuum pump that causes a
negative pressure to aspirate the smoke released by cigarette.
The pre-prepared Silicon (Speedex Putty, Coltene/whaledent AG-
Switzerland) template was constructed to support one specimen at the
time in the center of the bottom of the glass jar. For the test procedure
performance, the specimen was placed in the jar fitted in its site of
template as the polished surface come in direct exposure to cigarette
smoke then, the lid was locked and the cigarette was snugly fitted in its
tube until 10mm distance from specimen surface. Then the machine
[Table/Fig-1]: Surface roughness test [Table/Fig-2]: Schematic representation of
pocket profilometer with diamond stylus for measuring surface roughness
[Table/Fig-3]: Smoking machine assembly fastened in vacuum pump machine [Table/Fig-4]: Schematic representation of smoking machine
40 Journal of Clinical and Diagnostic Research. 2015 Sep, Vol-9(9): ZC39-ZC42
www.jcdr.net Hamada Zaki Mahross et al., Effect of Cigarette Smoke on Surface Roughness of Different Denture Base Materials
was assembled in vacuum pump machine with another tube after Many techniques of polishing can be performed to reduce surface
adjusting the negative pressure (20 mm Hg; 1 mm Hg = 133 Pa) for roughness of heat and light cure denture base materials through
cigarettes (Marlboro, Phillip Morris, Germany) smoking [Table/Fig-3]. mechanical or chemical methods. Mechanical polishing is the
For each specimen exposure, 20 cigarettes were used and each conventional method performed by using abrasives, that causes
cigarette burned in a standard time of 10 minutes. The aspiration time/ controlled wear of the surface material, to reduce surface roughness.
pressure was controlled and programmed with a switch pressure and Alternatively, chemical polishing is performed by placing the finished
timer of the vacuum machine [Table/Fig-4]. After that, the specimen acrylic resin denture in a chemical polisher containing heated monomer
was removed, washed with distilled water and dried with air then, the at 75oC for 10 s [18-20].
final surface roughness (FRa) was measured by using the profilometer The clinical threshold value of surface roughness (Ra) for plaque retention
as before exposure to smoking, as well as, for the control group’s on intraoral materials was 0.2 μm as advocated by Bollen C et al., [21].
specimens that incubated in distilled water. Changes in the surface In accordance, below a value there was no further reduction in plaque
roughness were calculated by the difference between the initial (IRa) accumulation was expected but above it, a proportional increase in
and final (FRa) measurements found before and after smoking test plaque accumulation occurs [20]. Therefore, smooth polished surface
of the samples, respectively. The data was collected and statistically of a denture base material is highly recommended.
analysed according to the paired sample t-test. The findings of this study were revealed that, the exposure of the PMMA
specimens to cigarette smoke increased the surface roughness values,
STATISTICAL ANALYSIS this may be attributed to the deposition of cigarette substances on the
The mean value and standard deviation of initial and final surface surface of the acrylic resin specimens. As when burning the cigarette,
roughness (Ra) for studied groups were calculated using descriptive the resultant smoke contains multiple components, such as carbon
data analysis. The data collected from the different groups were analysed monoxide, carbon dioxide, nicotine, ammonia, nickel, arsenic, tar and
by using the paired sample t-test at a predetermined significance level heavy metals such as lead and cadmium [10,22]. Another possible
of p< 0.05. All statistical comparisons were made with reference to the explanation may be due to the increase of temperature within the
control groups and not to each other. smoking chamber, i.e. the thermal effects of the smoking, as reported
in previous study [23].
RESULTS For further interpretations, the increased roughness of PMMA
The mean values and standard deviations of the initial (IRa) and final specimens may be attributed to the adherence of the cigarette
(FRa) surface roughness measurements of the tested groups were substances that cannot be totally removed when washed under
showed in [Table/Fig-5]. distilled water. Therefore, it is recommended to use denture-cleaning
Type of Sub- IRa value FRa value ΔRa Values p-value
agents for effective removal of these deposits, especially in elderly
resin groups (μm) (μm) (μm) people with reduced manual dexterity. This is in agreement with Ayaz
Heat cured Group I 0.137 (0.024) 0.138 (0.025) 0.001 (0.047) 0.968** E et al., who found an increase in surface roughness of all the tested
PMMA denture teeth materials after exposure to cigarette smoke and overall
resin Group II 0.135 (0.026) 0.168 (0.021) 0.033 (0.041) 0.032*
decrease in surface roughness value after subsequent immersion in
Light cured Group III 0.114 (0.034) 0.115 (0.035) 0.001 (0.033) 0.912** denture cleaning agent [10].
UDMA resin
Group IV 0.115 (0.035) 0.135 (0.021) 0.020 (0.032) 0.08** As regarding the effects of cigarette in this study, smoke on visible
[Table/Fig-5]: The Mean values and standard deviations of the initial (IRa) and final light cured UDMA specimens demonstrated a less increase in surface
(FRa) surface roughness measurements of the tested groups roughness that was statistically non-significant. This may be due to the
*Denotes significant difference (p< 0.05) smoother surface of these specimens that did not allow adherence of
**Denotes no significant difference (p>0.05)
cigarette smoke substance to it and the subsequent easy wash ability
by distilled water.
The paired sample t-test was showed that, there were a significant
differences in surface roughness between Group I and II, (0.968 and Furthermore, in comparison between the initial Ra of UDMA specimens
0.032) respectively, (p<0.05). Otherwise, there were no significant (0.115) with PMMA specimens (0.135) the results found that, the UDMA
differences in surface roughness between Group III and IV, (0.912 and specimens have a smoother surface than the PMMA specimens. This
0.08) respectively, (p>0.05). may explain the fewer adherences of smoke substances to the UDMA
specimens than the PMMA specimens as well as the difference in the
According to the statistical analysis, there were significant changes
chemical composition between both resins types as the presence of
in surface roughness of the heat cured PMMA specimens that have
silica filler within the light polymerized UDMA render its surface and
exposed to smoking test but no impact significance with visible light
makes it more resistant to the thermal effect of smoke. This finding
cured UDMA specimens. Otherwise, there were no significant changes
was in agreement to the previous studies which reported that, cigarette
in surface roughness with group I and group III specimens that were
smoke does not cause change in roughness of dental composites that
inserted in distilled water (control groups).
contain UDMA and silica fillers in its composition, but brushing after
The same statistical test for Group II and Group IV comparison revealed smoking may give rise to the surface alteration [13,24,25].
that, cigarette smoking increased the surface roughness of heat
According to Mathias P et al., the tar of cigarette contains aromatic
cured type resin more than light cured type resin but had no impact
hydrocarbons that have a surface dissolving action on the polymeric
significance for them.
materials, the polymeric material are insoluble in oral fluids, but they are
soluble to some extent in aromatic hydrocarbons [14]. From another
DISCUSSION point of view, there is a possibility of the cigarette smoke getting mixed
The effect of cigarette smoking on the surface roughness of two saliva which may have produced an acidic pH solution, damaging the
chemically different denture base resins was evaluated with this study surface integrity of the materials [8].
and the hypothesis that, cigarette smoke will increase the surface
Some studies had been reported that, cigarette smoke does not cause
roughness of both types of denture resins could be partially supported.
change in surface roughness, but brushing after smoking may have led
It has known that, the surface roughness of the denture base materials
to this alteration. So, it is extremely important to perform the surface
is one of the physical properties that may be changed because of
finishing/polishing adequately to avoid residual surface roughness
surface degradation and considered as one of the determinant factors
[12,23-26]. In the study of Alandia-Roman et al., there was an increase
in the clinical longevity of the dental prosthesis [13,17].
in roughness of all the evaluated materials and it was observed that
Journal of Clinical and Diagnostic Research. 2015 Sep, Vol-9(9): ZC39-ZC42 41
Hamada Zaki Mahross et al., Effect of Cigarette Smoke on Surface Roughness of Different Denture Base Materials www.jcdr.net
the type of finishing had an influence on the change in roughness of [5] Diaz-Arnold AM, Vargas MA, Shaull KL, Laffoon JE, Qian F. Flexural and fatigue
strengths of denture base resin. J Prosthet Dent. 2008;100:47-51.
composites, with significant difference between the finishing procedures
[6] Cilingir A, Bilhan H, Geckili O, Sulun T, Bozdag E, Sunbuloglu E. Invitro comparison
[12]. These results were in disagreement with the result of the present of two different materials for the repair of urethan dimethacrylate denture bases.
study, wherein smoking altered the surface roughness of both tested The Journal of Advanced Prosthodontics. 2013;5:396-401.
resin types. [7] Pereira-Cenci T, Del Bel Cury AA, Crielaard W, Ten Cate JM. Development
of Candida-associated denture stomatitis: new insights. J Appl Oral Sci.
Regarding the smoking device used in the present study, its design 2008;16:86-94.
principles were similar to that used in previous studies but with some [8] Patil SS, Dhakshaini MR, Gujjari AK. Effect of Cigarette Smoke on Acrylic Resin
Teeth. Journal of Clinical and Diagnostic Research. 2013;7:2056-59.
modifications [10,13]. The surface roughness changes were evaluated
[9] Casemiro LA, Gomes Martins CH, Pires-de-Souza Fde C, Panzeri H. Antimicrobial
for each acrylic resin specimen, after exposure to 20 cigarettes and and mechanical properties of acrylic resins with incorporated silver-zinc zeolite-
each cigarette burned in a standard time of 10 minutes as in the Part I. Gerodontology. 2008;25:187-94.
previous study regimens [12]. [10] Ayaz EA, Altintas SH, Turgut S. Effects of cigarette smoke and denture cleaners
on the surface roughness and colour stability of different denture teeth. J Prosthet
Both Profilometry and SEM analysis can be used to assess qualitatively Dent. 2014;112:241-48.
the surface characteristics of different denture material. Profilometry is [11] Bertoldo CE, Miranda D, Souza-Júnior EJ, Aguiar FHB, Lima DANL, Ferreira RL,
et al. Surface hardness and colour change of dental enamel exposed to cigarette
most useful in the evaluation of the Ra properties of dental materials
smoke. International Journal of Dental Clinics. 2011;3:1-4.
because it produces numerical data but with SEM provide visual [12] Alandia-Roman CC, Cruvinel DR, Sousa AB, Pires-de-Souza FC, Panzeri H.
comparisons [10]. Effect of cigarette smoke on colour stability and surface roughness of dental
composites. J Dent. 2013;41:73-79.
The changes in the surface roughness of the acrylic resin specimens [13] WasilewskiM de S, Takahashi MK, Kirsten GA, de Souza EM. Effect of cigarette
was measured by using profilometer as in previous investigations smoke and whiskey on the colour stability of dental composites. Am J Dent.
[12,27]. The main advantages of this method, is that, it is easy to 2010;23:4-8.
[14] Mathias P, Silva LD, SaraivaL de O, Costa L, Sampaio MD, de Araujo RP, et al.
conduct, accurate and the mean surface roughness of the acrylic
Effect of surface sealant and repolishing procedures on the colour of composite
specimens can be easily calculated in accordance to the manufacture’s resin exposed to cigarette smoke. Gen Dent. 2010;58:331–35.
recommendation. [15] Mathias P, Rossi TA, Cavalcanti AN, Lima MJ, Fontes CM, Nogueira-FilhoGda
R. Cigarette smoke combined with staining beverages decreases luminosity and
increases pigmentation in composite resin restorations. Compend Contin Educ
LIMITATIONS OF THE STUDY Dent. 2011;32:66–70.
This study being invitro might not have formulated an oral condition [16] Al-Kheraif AA. The effect of mechanical and chemical polishing techniques on
as would an cigarette smoke in oral cavity, in an invivo study (such as the surface roughness of heat-polymerized and visible light-polymerized acrylic
denture base resins. Saudi Dent J. 2014;26:56-62.
the presence of saliva that have washing and buffering effect into the
[17] Constantinescu IR, Ursache M, Mardarez D. Effect of pH on the surface
smoke substances that might reduce the thermal effect of smoke on roughness of heat cured denture base acrylic resins. Rev Med ChirSoc Med Nat
the denture base materials). Therefore, in the future, additional clinical Iasi. 2007;111:477-81.
studies are necessary to clarify the long-term effect of cigarette smoke [18] Abuzar MA, Bellur S, Duong N, Kim BB, Lu P, Palfreyman N, et al. Evaluating
surface roughness of a polyamidedenture base material in comparison with poly
on the surface properties of denture base materials. (methyl methacrylate). J Oral Sci. 2010;52:577–81.
[19] Braun KO, Mello JAN, Rached RN, Del Bel Cury AA. Surface texture and some
CONCLUSION properties of acrylic resins submitted to chemical polishing. J Oral Rehabil.
2003;30:91–98.
The denture bases constructed from heat-cured acrylic resin material
[20] Rahal JS, Mesquita MF, Henriques GE, Nobilo MA. Surface roughness of
have a marked increase of surface roughness after exposure to acrylic resins submitted to mechanical and chemical polishing. J Oral Rehabil.
cigarette smoke, but the denture bases constructed from visible light 2004;31:1075–79.
cured resin material have superior surface characteristics. The use of [21] Bollen CML, Lambrechts P, Quirynen M. Comparison of surface roughness
of oral hard materials to the threshold surface roughness for bacterial plaque
more accurate finishing and polishing surface procedures can reduce retention: a review of the literature. Dent Mater. 1997;13:258-69.
the adherence of harmful substances on denture base, in conjugation [22] Kuhar M, Funduk N. Effect of polishing techniques on the surface roughness of
with subsequent good oral hygiene. Findings of this invitro study may acrylic denture base resins. J Prosthet Dent. 2005;93:76-85.
[23] Mathias P, Costa L, Saraiva TA, Cavalcanti AN, da Rocha Nogueira-Filho
guide the dental practitioners in proper selection of denture base
G. Morphologic texture characterization allied to cigarette smoke increase
materials and correct surface finishing procedures for smoker patients pigmentation in composite resin restorations. J Esthet Restor Dent.
to ensure long duration of services. 2010;22:252‑61.
[24] Penteado RA, Tonholo J, Júnior JG, Silva MF, QueirozCda S, Cavalli V, et al.
Evaluation of surface roughness of microhybrid and nanofilled composites
References after pH-cycling and simulated tooth brushing. J Contemp Dent Pract.
[1] Mumcu E, Cilingir A, Gencel B, Sülün T. Flexural properties of a light-cure and a 2010;11:17‑24.
self-cure denture. The Journal of Advanced Prosthodontics. 2011;3:136-39. [25] Garcia FC, Wang L, D’Alpino PH, Souza JB, Arau´ jo PA, Mondelli RF. Evaluation
[2] Abuzar MA, Bellur S, Duong N, Kim BB, Lu P, Palfreyman N, et al. Evaluating of the roughness and mass loss of the flowable composites after simulated tooth
surface roughness of a polyamide denture base material in comparison with poly brushing abrasion. Braz Oral Res. 2004;18:156-61.
(methyl methacrylate). J Oral Sci. 2010;52:577-81. [26] Santos M, Soo S, Petridis H. The effect of Parylene coating on the surface
[3] Parvizi A, Lindquist T, Schneider R, Williamson D, Boyer D, Dawson DV. roughness of PMMA after brushing. J Dent. 2013;41:802-08.
Comparison of the dimensional accuracy of injection-molded denture base [27] Machado AL, Giampaolo ET, Pavarina AC, Jorge JH, Vergani CE. Surface
materials to that of conventional pressure-pack acrylic resin. J Prosthodont. roughness of denture base and reline materials after disinfection by immersion in
2004;13:83-89. chlorhexidine or microwave irradiation. Gerodontology. 2012;29:375-82.
[4] Pfeiffer P, Rosenbauer EU. Residual methyl methacrylate monomer, water
sorption, and water solubility of hypoallergenic denture base materials. J Prosthet
Dent. 2004;92:72-78.
PARTICULARS OF CONTRIBUTORS:
1. Assistant Professor, Department of Prosthodontics, Alfarabi Collages, Riyadh, Saudi Arabia.
2. Assistant Professor, Department of Prosthodontics, Alfarabi Collages, Riyadh, Saudi Arabia.
3. Assistant Professor, Department of Restorative Dental Sciences, Alfarabi Collages, Riyadh, Saudi Arabia.
4. Assistant Professor, Department of Preventive Dental Sciences, Alfarabi Collages, Riyadh, Saudi Arabia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Kusai Baroudi,
King Abdullah Road East, Eshbilia, Alfarabi Collages. Date of Submission: Apr 21, 2015
E-mail: d_kusai@yahoo.co.uk Date of Peer Review: Jun 30, 2015
Date of Acceptance: Jul 22, 2015
Financial OR OTHER COMPETING INTERESTS: None. Date of Publishing: Sep 01, 2015
42 Journal of Clinical and Diagnostic Research. 2015 Sep, Vol-9(9): ZC39-ZC42
You might also like
- Tribology: Friction and Wear of Engineering MaterialsFrom EverandTribology: Friction and Wear of Engineering MaterialsRating: 5 out of 5 stars5/5 (1)
- GENCHEM1-12-Q1-WEEK1-MELC3-MOD-Salitamos, Kaye - Sherwin Jay PalaspasDocument19 pagesGENCHEM1-12-Q1-WEEK1-MELC3-MOD-Salitamos, Kaye - Sherwin Jay PalaspasYer Bal67% (3)
- Jips 19 42Document7 pagesJips 19 42Raluca ChisciucNo ratings yet
- Tipos de Pos Cura e ImporntanciaDocument7 pagesTipos de Pos Cura e ImporntanciaDanilo BianchiNo ratings yet
- Effects of Cigarette Smoking On Color Stability of Dental Resin CompositesDocument8 pagesEffects of Cigarette Smoking On Color Stability of Dental Resin CompositesSkAliHassanNo ratings yet
- Life Cycle Considerations For EngineeredDocument4 pagesLife Cycle Considerations For Engineeredfirooziahmad1986No ratings yet
- Comparison of Conventional Varnishes With Nanolacke UV Varnish With Respect To Hardness and Adhesion DurabilityDocument10 pagesComparison of Conventional Varnishes With Nanolacke UV Varnish With Respect To Hardness and Adhesion DurabilityJohn Bartolo CubaNo ratings yet
- Thermal Degradation and Fire Resistance of Unsaturated Polyester, Modified Acrylic Resins and Their Composites With Natural FibresDocument7 pagesThermal Degradation and Fire Resistance of Unsaturated Polyester, Modified Acrylic Resins and Their Composites With Natural Fibressarul_murugan2483No ratings yet
- Gad, Abualsaud - 2019 - Behavior of PMMA Denture Base Materials Containing Titanium Dioxide Nanoparticles A Literature ReviewDocument14 pagesGad, Abualsaud - 2019 - Behavior of PMMA Denture Base Materials Containing Titanium Dioxide Nanoparticles A Literature ReviewMorteza AtaeiNo ratings yet
- Adv 21842Document13 pagesAdv 21842Alexandru LetNo ratings yet
- Dental Research JournalDocument5 pagesDental Research Journaldrvivek reddyNo ratings yet
- Characterization of Waste Plastic Bag As A Novel Binder System and Homogeneity Test For Stainless Steel 316L Metal Injection MoldingDocument7 pagesCharacterization of Waste Plastic Bag As A Novel Binder System and Homogeneity Test For Stainless Steel 316L Metal Injection MoldingFera FaelaNo ratings yet
- Evaluation of Different Light-Curing Lamps HalogenDocument7 pagesEvaluation of Different Light-Curing Lamps HalogenKenny Rafael Iglesias AlvarezNo ratings yet
- Hahnel 2007Document9 pagesHahnel 2007Özlem Alan ÇölgeçenNo ratings yet
- An Application of Nanotechnology in Advanced Dental MaterialsDocument9 pagesAn Application of Nanotechnology in Advanced Dental MaterialsSevgi SözügeçerNo ratings yet
- A Pilot Study On Microwave Heating For Production and Recycling of RoadDocument9 pagesA Pilot Study On Microwave Heating For Production and Recycling of RoadAhmadreza AminianNo ratings yet
- Effect of Microwave Disinfection On Dimensional Stability of Polymethyl Methacrylate and Polyamide Denture Base MaterialDocument5 pagesEffect of Microwave Disinfection On Dimensional Stability of Polymethyl Methacrylate and Polyamide Denture Base MaterialInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Current Status On Lithium Disilicate and ZirconiaDocument14 pagesCurrent Status On Lithium Disilicate and ZirconiaTanya HernandezNo ratings yet
- LD 1Document15 pagesLD 1kapilesh singhNo ratings yet
- Ahmad Za Uzi 2019Document7 pagesAhmad Za Uzi 2019phillynovitaNo ratings yet
- Supervision of Ethylene Propylene Diene M-Class (EPDM) Rubber Vulcanization and Recovery Processes Using Attenuated Total Reflection Fourier Transform Infrared (ATR FT-IR) Spectroscopy and Multivariate AnalysisDocument12 pagesSupervision of Ethylene Propylene Diene M-Class (EPDM) Rubber Vulcanization and Recovery Processes Using Attenuated Total Reflection Fourier Transform Infrared (ATR FT-IR) Spectroscopy and Multivariate AnalysisFairmont Ind Quality DivisionNo ratings yet
- Paper294215 PDFDocument17 pagesPaper294215 PDFkirandevi1981No ratings yet
- UntitledDocument38 pagesUntitledGOPI CHANDUNo ratings yet
- 51 Improvement in Ammonia Gas Sensing Properties of La Doped MoO3 Thin Films Fabricated by Nebulizer Spray Pyrolysis Method - ScienceDirectDocument10 pages51 Improvement in Ammonia Gas Sensing Properties of La Doped MoO3 Thin Films Fabricated by Nebulizer Spray Pyrolysis Method - ScienceDirectAruthra (It’s Aru’s time)No ratings yet
- Aniagor2020 - Relational Description of An Adsorption System Based On IsothermDocument26 pagesAniagor2020 - Relational Description of An Adsorption System Based On Isothermco.aniagorNo ratings yet
- Research Article: Tio and Zno Nanoparticles in Photocatalytic and Hygienic CoatingsDocument7 pagesResearch Article: Tio and Zno Nanoparticles in Photocatalytic and Hygienic CoatingsHermes David Guerrero NietoNo ratings yet
- Silicon Nitride Ceramic For All-Ceramic Dental RestorationsDocument7 pagesSilicon Nitride Ceramic For All-Ceramic Dental RestorationsAmelia Disa Penti AryaniNo ratings yet
- NexcoDocument14 pagesNexcoDella MeirandaNo ratings yet
- 0021998316669578Document14 pages0021998316669578Riston SinagaNo ratings yet
- Tanin in Silica Emulsion PolymersDocument12 pagesTanin in Silica Emulsion PolymersDani M RamdhaniNo ratings yet
- Laboratory Testing of Brake Pads Made of Organic MDocument8 pagesLaboratory Testing of Brake Pads Made of Organic M刘牛No ratings yet
- Ujjwal Bansal - 211119012Document47 pagesUjjwal Bansal - 211119012ujjwal bansalNo ratings yet
- Tribology International: Rongping Yun, Peter Filip, Yafei LuDocument10 pagesTribology International: Rongping Yun, Peter Filip, Yafei LuRajiv Gandhi Rajiv GandhiNo ratings yet
- New Resin Cements Agents in Conservative Dentistry: Indications and Possible Risks. Rev LiteratureDocument7 pagesNew Resin Cements Agents in Conservative Dentistry: Indications and Possible Risks. Rev LiteraturemaiNo ratings yet
- EPL 0006286 ArticleDocument11 pagesEPL 0006286 Articlekevin tayoNo ratings yet
- J Esthet Restor Dent - 2023 - Çakmak - Effect of Coffee Thermocycling On The Surface Roughness and Stainability of DentureDocument7 pagesJ Esthet Restor Dent - 2023 - Çakmak - Effect of Coffee Thermocycling On The Surface Roughness and Stainability of DentureHugo MoralesNo ratings yet
- 987 Ijar-6524Document11 pages987 Ijar-6524Hoda SolimanNo ratings yet
- Manso 2018Document6 pagesManso 2018matiaspenrozvaldiviaNo ratings yet
- Adsorption of Methylene Blue Dye From in 47b23880Document8 pagesAdsorption of Methylene Blue Dye From in 47b23880Gusmi SusiartiNo ratings yet
- 1.microporous and Mesoporous Materials 131 (2010) 170-176-2-2Document1 page1.microporous and Mesoporous Materials 131 (2010) 170-176-2-2Ramkumar SekarNo ratings yet
- Effect of Ethanol Treatment On Mechanical Properties of Heat-Polymerized Polymethyl Methacrylate Denture Base PolymerDocument8 pagesEffect of Ethanol Treatment On Mechanical Properties of Heat-Polymerized Polymethyl Methacrylate Denture Base PolymerGladis ARNo ratings yet
- TMP F222Document7 pagesTMP F222FrontiersNo ratings yet
- Effect of Nanoparticle Addition On Polymethylmethacrylate ResinsDocument7 pagesEffect of Nanoparticle Addition On Polymethylmethacrylate ResinsR RahmadaniNo ratings yet
- Comparative Study of Resin Composite Class I RestoDocument9 pagesComparative Study of Resin Composite Class I RestoSholehudin Al AyubiNo ratings yet
- Bonding Performance of Self-Adhesive Flowable Composites To Enamel, Dentin and A Nano-Hybrid CompositeDocument10 pagesBonding Performance of Self-Adhesive Flowable Composites To Enamel, Dentin and A Nano-Hybrid CompositeSoraya BouchammaNo ratings yet
- Ali I .Al-Mosawi, Salim J.Abbas, Salim H.flayah: Influence of Retardant Agent On Flame Through Composite SurfaceDocument4 pagesAli I .Al-Mosawi, Salim J.Abbas, Salim H.flayah: Influence of Retardant Agent On Flame Through Composite Surfacesar0000No ratings yet
- Komposisi z350Document9 pagesKomposisi z350muchlis fauziNo ratings yet
- Water-Based Indium Tin Oxide Nanoparticle InkDocument17 pagesWater-Based Indium Tin Oxide Nanoparticle Inkslem.kasemmNo ratings yet
- Jumlah DAN Lama Paparan Debu Akrilik Pada Pembuatan Peranti Ortodonti LepasanDocument9 pagesJumlah DAN Lama Paparan Debu Akrilik Pada Pembuatan Peranti Ortodonti LepasanNurlina NurdinNo ratings yet
- Pilot Study BenedettoDocument9 pagesPilot Study Benedettoaparnanoojilla1729No ratings yet
- Emw 2007 FP 02093Document390 pagesEmw 2007 FP 02093boj87No ratings yet
- 62 Naskah 296 1 10 20200630Document8 pages62 Naskah 296 1 10 20200630Lani AccNo ratings yet
- Kekasaran Permukaan Resin Komposit Nanofilled Dan Nanohybrid Setelah Paparan Asap Rokok KretekDocument6 pagesKekasaran Permukaan Resin Komposit Nanofilled Dan Nanohybrid Setelah Paparan Asap Rokok KretekRuth Rosanya SiraitNo ratings yet
- Improving Polymethyl Methacrylate Resin Using A Novel Titanium Dioxide CoatingDocument7 pagesImproving Polymethyl Methacrylate Resin Using A Novel Titanium Dioxide Coatingsilencer recnelisNo ratings yet
- Three-Dimensional Defect Evaluation of Air Polishing On Extracted Human RootsDocument8 pagesThree-Dimensional Defect Evaluation of Air Polishing On Extracted Human RootsHaoWangNo ratings yet
- Preparation and Studies of Nitrile Rubber Nanocomposites With MMT NanoparticlesDocument13 pagesPreparation and Studies of Nitrile Rubber Nanocomposites With MMT NanoparticlesAnish KumarNo ratings yet
- Advanced Powder TechnologyDocument11 pagesAdvanced Powder TechnologyDeepakrao Bornare PatilNo ratings yet
- Influence of Curing Time, Overlay Material and Thickness On Three Light-Curing Composites Used For Luting Indirect Composite RestorationsDocument8 pagesInfluence of Curing Time, Overlay Material and Thickness On Three Light-Curing Composites Used For Luting Indirect Composite RestorationsAbhishek Isaac MathewNo ratings yet
- Carbon Nanotube Reinforced Composites: CNT Polymer Science and TechnologyFrom EverandCarbon Nanotube Reinforced Composites: CNT Polymer Science and TechnologyNo ratings yet
- Pollution Control and Resource Recovery: Municipal Solid Wastes Incineration: Bottom Ash and Fly AshFrom EverandPollution Control and Resource Recovery: Municipal Solid Wastes Incineration: Bottom Ash and Fly AshNo ratings yet
- Clay-Containing Polymer Nanocomposites: From Fundamentals to Real ApplicationsFrom EverandClay-Containing Polymer Nanocomposites: From Fundamentals to Real ApplicationsNo ratings yet
- 1678 7757 Jaos 29 E20200448Document10 pages1678 7757 Jaos 29 E20200448Raluca ChisciucNo ratings yet
- Pone 0145837Document16 pagesPone 0145837Raluca ChisciucNo ratings yet
- New Nordic and Scandinavian Retro Reassessment ofDocument12 pagesNew Nordic and Scandinavian Retro Reassessment ofRaluca Chisciuc100% (1)
- 1 s2.0 S0300571216302202 MainDocument6 pages1 s2.0 S0300571216302202 MainRaluca ChisciucNo ratings yet
- Imaginile Fac Cladiri - Patru Articole PDFDocument116 pagesImaginile Fac Cladiri - Patru Articole PDFRaluca ChisciucNo ratings yet
- !!!!!!architectural PhotographyDocument15 pages!!!!!!architectural PhotographyRaluca ChisciucNo ratings yet
- A&GDocument216 pagesA&GRaluca ChisciucNo ratings yet
- Imaginile Fac Cladiri - Patru Articole PDFDocument116 pagesImaginile Fac Cladiri - Patru Articole PDFRaluca ChisciucNo ratings yet
- Flexible Denture Base Material A Viable AlternativDocument5 pagesFlexible Denture Base Material A Viable AlternativRaluca ChisciucNo ratings yet
- New Concepts For Increasing The Buildings Energy Efficiency: Anca DUTA, Ion Visa, Macedon MOLDOVAN, Mihai COMSITDocument8 pagesNew Concepts For Increasing The Buildings Energy Efficiency: Anca DUTA, Ion Visa, Macedon MOLDOVAN, Mihai COMSITRaluca ChisciucNo ratings yet
- Use of EnglishDocument16 pagesUse of Englishrox17No ratings yet
- Opinion EssayDocument1 pageOpinion EssayiloveanjuNo ratings yet
- The Colonnade, April 11, 2014Document17 pagesThe Colonnade, April 11, 2014Bobcat NewsNo ratings yet
- 9th Form An OverviewDocument62 pages9th Form An OverviewElâa Ben Hadj DahmenNo ratings yet
- Manual of Regulating Smoking in Public PlacesDocument30 pagesManual of Regulating Smoking in Public PlacesNikita JayswalNo ratings yet
- Latihan Soal PAT Bahasa Inggris Kelas XI Tahun 2022Document10 pagesLatihan Soal PAT Bahasa Inggris Kelas XI Tahun 2022Rhaisya AaliyahNo ratings yet
- Gso Iso 8243 1995 eDocument19 pagesGso Iso 8243 1995 eMuhammad Masood AbbasNo ratings yet
- Session 16 1 3Document16 pagesSession 16 1 3Nikita DaceraNo ratings yet
- Pakistan 2014: Global Adult Tobacco Survey Fact SheetDocument2 pagesPakistan 2014: Global Adult Tobacco Survey Fact Sheetziauddin2No ratings yet
- UntitledDocument3 pagesUntitledapi-235146564No ratings yet
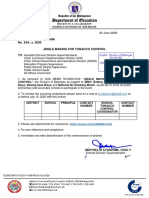
- Division Memorandum - s2020 - 241Document16 pagesDivision Memorandum - s2020 - 241ARLENE MARASIGANNo ratings yet
- Unit Test Health 8 Q4Document2 pagesUnit Test Health 8 Q4MADELINE R. SEDIEGONo ratings yet
- NCD High-Risk Assessment (Community Case Finding Form) NCD High-Risk Assessment (Community Case Finding Form)Document1 pageNCD High-Risk Assessment (Community Case Finding Form) NCD High-Risk Assessment (Community Case Finding Form)Gen GenNo ratings yet
- Gold Leaf New Modern Pack PresentationDocument21 pagesGold Leaf New Modern Pack PresentationMuhammad AbidNo ratings yet
- New Microsoft Word DocumentDocument67 pagesNew Microsoft Word DocumentRahmat Zainun Abdullah100% (1)
- Danger of Smoking in The MorningDocument6 pagesDanger of Smoking in The MorningindriNo ratings yet
- Question Bank (English - 1st Year)Document13 pagesQuestion Bank (English - 1st Year)Anonymous nPU0jkHmNo ratings yet
- Itc CSRDocument15 pagesItc CSRjayavigneshNo ratings yet
- Minnesota Fact SheetDocument2 pagesMinnesota Fact Sheetnchc-scribdNo ratings yet
- Smoking IntroductionDocument3 pagesSmoking IntroductionKimberly Montalvo100% (1)
- ITC LTD. Toward A Triple Bottom Line PerformanceDocument10 pagesITC LTD. Toward A Triple Bottom Line PerformanceAbhilasha BagariyaNo ratings yet
- Electronic Cigarettes and Youth: E-Cigarette Use Among YouthDocument7 pagesElectronic Cigarettes and Youth: E-Cigarette Use Among Youthmaria5basNo ratings yet
- Dynamic Business Law 3rd Edition Kubasek Solutions ManualDocument25 pagesDynamic Business Law 3rd Edition Kubasek Solutions ManualMrsJenniferCarsonjrcy100% (60)
- Wigan Council Electronic Cigarettes PolicyDocument6 pagesWigan Council Electronic Cigarettes PolicyDick Puddlecote100% (1)
- Siti Sarah Alawiyah-FKIK PDFDocument145 pagesSiti Sarah Alawiyah-FKIK PDFDhini MandasariNo ratings yet
- Group ProjectDocument48 pagesGroup Projecthazyhazy9977No ratings yet
- Philippine Virginia Tobacco Administration Vs CIR (1975)Document8 pagesPhilippine Virginia Tobacco Administration Vs CIR (1975)Pamela TambaloNo ratings yet
- Soal2 News ItemDocument7 pagesSoal2 News ItemRiriArikaPutriNo ratings yet
- Levels of Smoking and Dental Implants Failure: A Systematic Review and Meta-AnalysisDocument11 pagesLevels of Smoking and Dental Implants Failure: A Systematic Review and Meta-AnalysisJuan Pablo Aguilera MardonesNo ratings yet