Professional Documents
Culture Documents
Occult Pneumothorax in Patients Presenting With Blunt Chest Trauma: An Observational Analysis
Uploaded by
Anangova PradiptaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Occult Pneumothorax in Patients Presenting With Blunt Chest Trauma: An Observational Analysis
Uploaded by
Anangova PradiptaCopyright:
Available Formats
RESEARCH ARTICLE
Occult Pneumothorax in Patients Presenting with
Blunt Chest Trauma: An Observational Analysis
Ismail Mahmood1, Basil Younis1, Khalid Ahmed1, Fuad Mustafa1,
Ayman El-Menyar2,3, Mohammad Alabdallat1, Ashok Parchani1, Ruben Peralta1,
Syed Nabir4, Nadeem Ahmed4, Hassan Al-Thani1
ABSTRACT
Address for Correspondence: Background: We aimed to assess the management
Ayman El-Menyar and outcome of occult pneumothorax and to
1
Department of Surgery, Trauma Surgery Section, determine the factors associated with failure of
Hamad Medical Corporation, Doha, Qatar observational management in patients with blunt
2
Clinical Research, Trauma & Vascular Surgery Section, chest trauma (BCT).
Hamad Medical Corporation, Doha, Qatar Methods: Patients with BCT were retrospectively
3
Clinical Medicine, Weill Cornell Medical College, Doha, identified from the trauma database over 4 years.
Qatar
4 Data were analyzed and compared on the basis
Department of Radiology, Hamad General Hospital,
Doha, Qatar
of initial management (conservative vs. tube
Email: aymanco65@yahoo.com thoracostomy).
Results: Across the study period, 1928 patients were
http://dx.doi.org/10.5339/qmj.2020.10 admitted with BCT, of which 150 (7.8%) patients
Submitted: 15 September 2019 were found to have occult pneumothorax. The mean
Accepted: 21 November 2019 patient age was 32.8 ^ 13.7 years, and the majority
ª 2020 Mahmood, Younis, Ahmed, Mustafa, El-Menyar, were male (86.7%). Positive-pressure ventilation
Alabdallat, Parchani, Peralta, Nabir, Ahmed, Al- Thani, licensee (PPV) was required in 32 patients, and bilateral occult
HBKU Press. This is an open access article distributed under
the terms of the Creative Commons Attribution license CC BY
pneumothorax was seen in 25 patients. In 85.3%
4.0, which permits unrestricted use, distribution and (n ¼ 128) of cases, occult pneumothorax was
reproduction in any medium, provided the original work is managed conservatively, whereas 14.7% (n ¼ 22)
properly cited. underwent tube thoracostomy. Five patients had
failed observational treatment requiring delayed tube
thoracostomy. Pneumonia was reported in 12.8% of
Cite this article as: Mahmood I, Younis B, cases. Compared with those who were treated
Ahmed K, Mustafa F, El-Menyar A, Alabdallat M, conservatively, patients who underwent tube
Parchani A, Peralta R, Nabir S, Ahmed N,
Al-Thani H. Occult Pneumothorax in Patients thoracostomy had thicker pneumothoraxes and a
Presenting with Blunt Chest Trauma: An higher rate of lung contusion, rib fracture, pneumonia,
Observational Analysis, Qatar Medical Journal prolonged ventilatory days, and prolonged hospital
2020:10 http://dx.doi.org/10.5339/
qmj.2020.10 length of stay. Overall mortality was 4.0%. The
deceased had more polytrauma and were treated
conservatively without a chest tube. Patients who
failed conservative management had a higher
frequency of lung contusion, greater pneumothorax
thickness, higher Injury Severity Scores (ISS), and
required more PPV.
QATAR MEDICAL JOURNAL 1
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
Conclusions: Occult pneumothorax is not uncommon To date, we do not have an institutional guideline for
in BCT and can be successfully managed the indications to opt for the initial insertion of
conservatively with a close clinical follow-up. chest tube in occult pneumothorax patients.
Intervention should be limited to patients who have Therefore, the important issue is to distinguish the
an increase in size of the pneumothorax on follow-up pneumothoraxes that can be treated conservatively
or become symptomatic under observation. Patients from those which require chest drainage. According to
who fail conservative management may have a the Eastern Association for the Surgery of
greater pneumothorax thickness and higher ISS. Trauma practice management guidelines, occult
However, large prospective studies are warranted pneumothorax can be observed in a stable patient
to support these findings and to establish the regardless of PPV.10 In contrast, Advanced Trauma
institutional guidelines for the management of occult Life Support guidelines recommend that traumatic
pneumothorax. pneumothorax is best treated with a chest tube,
especially in those requiring general anesthesia or
Keywords: chest trauma, occult pneumothorax, PPV.11 However, there is increasing evidence in the
chest CT scan, ventilation adult12,13 and pediatric literature suggesting that
occult pneumothoraxes may be safely observed even
INTRODUCTION while under PPV14,15; however, occult pneumothorax
progression and respiratory distress are independently
In BCT, the presence of air in the pleural space is
associated with the need for tube thoracostomy
referred to as pneumothorax, which has been
insertion.12
reported in up to 55% of cases.1 However, the
primary diagnostic modality for screening In this study we sought to analyze the clinical
pneumothorax in the emergency setting is chest presentations, management, and outcomes of trauma
radiography; it has lower sensitivity, which increases patients who presented with occult pneumothorax
the chances of misdiagnosis (30%–40%).2 – 4 The and to determine which clinical factors were
most accurate diagnostic tool to detect blood or air in associated with failure of initial conservative
the pleura in the initial trauma setting is the thoracic management in our Level I trauma center.
computed tomography (CT) scan, which has .95%
sensitivity and is the gold standard tool for detecting METHODS
thoracic lesions.5 In addition, the CT scan is
the modality of choice for diagnosing occult
Study participants and setting
pneumothorax in trauma patients that remain This is a retrospective chart review of all admitted
undetected by normal supine chest X-rays.6 It may be BCT patients who were diagnosed with
challenging to observe occult pneumothorax in pneumothorax on chest CT scan that was not evident
severely injured patients. In such patients, the clinical on initial supine chest X-ray. We reviewed the trauma
concern is the risk of progression to life-threatening registry database at Hamad General Hospital, the
tension pneumothorax, particularly if the patient is only Level I trauma center in the state of Qatar, from
undergoing positive-pressure ventilation (PPV).7 November 2010 to November 2014.
Moreover, emergency physicians often encounter As per the standard of care, we also retrieved data on
difficulty in choosing the appropriate treatment the in-hospital clinical follow-up, to review the erect
strategy for occult pneumothorax. The selection of P-A view chest X-rays (or, if this was not possible,
chest tube insertion over conservative management supine films) to assess the progression of pneumo-
remains controversial due to the association of more thorax during the hospital course.
complications from tube thoracostomy than from the Our inclusion criteria included all blunt thoracic trauma
pneumothorax itself.8 An earlier management patients with occult pneumothorax which was
strategy supported the placement of a chest tube diagnosed and measured by CT scan to quantify the
for all clinically or radiographically diagnosed highest perpendicular distance in millimeters from the
pneumothoraxes after trauma.9 However, this chest wall of the largest air pocket as described by
practice has been changed due to the reported risk of De Moya et al.16 The exclusion criteria were all
major complications (22%) secondary to intercostal patients who had concurrent occult hemothorax on
tube placement.9 chest CT scan and those who were aged ,14 years.
2 QATAR MEDICAL JOURNAL
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
Data collection Statistical analysis
Patient demographics (age and sex), mechanism of Data were presented as mean ^ standard deviation,
injury, presence of lung contusions, rib fracture, chest medians (range), and proportions, as appropriate.
CT scan findings (pneumothorax thickness, bilateral We categorized and compared the management of
pneumothorax), intubation, ventilation mode, chest pneumothorax in two groups as conservative versus
Abbreviated Injury Scale (AIS), Injury Severity Score chest tube insertion. Differences in categorical and
(ISS), management for pneumothorax, failure of continuous variables were analyzed using the x2 test
conservative management, length of hospital and and Student’s t-test, as appropriate. Yates' corrected
intensive care unit stay, ventilatory days, and chi-square was used for categorical variables, if the
mortality were examined. Outcomes such as chest expected cell frequencies were below 5. A significant
tube complications (pneumonia, empyema, and difference was considered when the two-tailed p
tension pneumothorax) were also recorded. Clinical value was ,0.05. Statistical Package for the Social
follow-up was carried out to determine when the Sciences version 18 (SPSS, Inc., Chicago, IL USA) was
chest tube was placed as part of management and for used for the data analysis.
other indications in each case with an occult
pneumothorax. RESULTS
A CT scan was performed using 120 ml of Omnipaque Across the study period, 1928 patients were
injected at 3 ml/s and with a Siemens Medical admitted with BCT; of them, 150 (7.8%) patients
Systems 64-slice scanner. Images were rebuilt with were found to have occult pneumothorax. The mean
slice thicknesses of 1.2, 2.5, or 5 mm, reviewed, and patient age was 32.8 ^ 13.7 years, and the majority
analyzed by a trauma consultant radiologist. of them were male (86.7%). The most frequent
In our trauma center, there are on an average, 2500 mechanism of injury was motor vehicle crash (50%)
trauma activations per year, of which approximately followed by pedestrian struck by a car (18.7%), and
1600–1800 patients require hospital admission. fall from a height (11.3%) (Table 1).
Roughly 80% of patients with significant injuries Lung contusion (72%) characterized the most
underwent a pan CT scan (Head, Neck, Chest & frequent chest injury, and 78 (52%) patients had rib
Abdomen), and the rest underwent region specific CT fractures with a median of 3.5 ribs (range 1–12).
scan based on the anatomical region, mechanism of On CT scan evaluation, the median pneumothorax
injury, and at the discretion of the treating physician. thickness was 8.5 (range: 2–173) mm. Half of
Occult pneumothorax referred to the findings of a patients had occult pneumothorax thickness in the
normal initial chest radiograph of the trauma patient, range of 1–9.9 mm (50.3%) followed by 10–19.9
which was later detected as a pneumothorax on a mm (22.8%). Only 16.8% of patients had occult
subsequent thoracic CT scan. pneumothorax thickness of $30 mm (Figure 1).
Pneumonia: Centers for Disease Control and Pre- Bilateral occult pneumothorax was seen in 25
vention in Atlanta, GA, USA (CDC) criteria (purulent (16.7%) patients.
sputum, leukocytosis, positive culture of endotracheal Endotracheal intubation and PPV were needed in
secretion, infiltrate on chest radiograph, and fever) 32 (22%) patients secondary to severe head injury
were used to make a diagnosis of pneumonia.17 (Glasgow Coma Scale (GCS) , 8). Seven patients on
Hamad General Hospital provides trauma services to PPV received a prophylactic chest tube as per the
the whole population of Qatar, and it successfully discretion of the treating physician and one patient
achieved Trauma Distinction Accreditation offered by developed respiratory distress with radiographic
Accreditation Canada International. The Qatar evidence of pneumothorax progression.
National Trauma Registry is a database that partici- Figure 2 shows examples of pneumothorax in two
pates in both the National Trauma Data Bank and the cases.
Trauma Quality Improvement Program of the Amer- Eight (5.3%) patients required general anesthesia
ican College of Surgeons-Committee on Trauma for surgical intervention involving maxillofacial,
(ACS-COT). The Medical Research Center (IRB# neurosurgical, or orthopedic procedures.
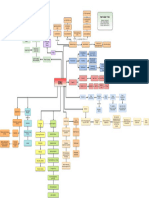
14513/14) at Hamad Medical Corporation, Doha, Figure 3 shows a flow chart for management of
Qatar, has approved the study. patients with occult pneumothorax. Conservative
QATAR MEDICAL JOURNAL 3
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
Table 1. Demographics, clinical presentation, and outcome of patients with occult pneumothorax based
on management approach.
Total Conservative Tube thoracostomy
(n 5 150) (n 5 128) (n 5 22) P
Age (mean ^ SD) 32.8 ^ 13.7 31.2 ^ 13 36.7 ^ 16.6 0.08
Males 130 (86.7%) 109 (85.2%) 21 (95.5%) 0.18
Mechanism of injury
Motor vehicle crash 75 (50.0%) 68 (53.1%) 7 (31.8%) 0.03 for all
Pedestrian 28 (18.7%) 25 (19.5%) 3 (13.6%)
Fall from height 17 (11.3%) 11 (8.6%) 6 (27.3%)
Others 30 (20.0%) 24 (18.8%) 6 (27.3%)
Pneumothorax thickness (mm) 8.5 (2 –173) 8 (2–173) 13 (2–50) 0.36
Bilateral pneumothorax 25 (16.7%) 20 (15.6%) 5 (22.7%) 0.60
Lung contusion 108 (72.0%) 89 (69.5%) 19 (86.4%) 0.10
Rib fracture 78 (52.0%) 64 (50.0%) 14 (63.6%) 0.23
Number of fractured ribs 3.5 (1 –12) 3 (1–12) 5.5 (1–9) 0.09
Injury severity score 16.4 ^ 9.4 16.3 ^ 9.7 17 ^ 7.6 0.74
Chest AIS median (range) 3 (2 –5) 3 (2–5) 3 (2–4) 0.01
mean ^ SD 2.52 ^ 0.55 2.82 ^ 0.50
Surgical intervention 8 (5.3%) 7 (5.5%) 1 (4.5%) 0.73
Mechanical ventilation 32 (21.3%) 25 (19.5%) 7 (31.8%) 0.19
Ventilatory days 10 (1 –25) 10 (1–25) 12 (1–18) 0.68
ICU length of stay 8.5 (1 –82) 7 (1–82) 9 (2–32) 0.40
Hospital length of stay 7 (1 –139) 7 (1–139) 8.5 (2–117) 0.05
Pneumonia 19 (12.8%) 15 (11.9%) 4 (18.2%) 0.41
Mortality 6 (4.0%) 6 (4.7%) 0 (0.0%) 0.65
AIS: Abbreviated injury score; ICU: Intensive care unit.
management of occult pneumothorax was effectively treated conservatively, patients who underwent
attained in 128 (85.3%) cases initially, and the tube thoracostomy had higher mean chest AIS
remaining 22 (14.7%) cases underwent tube (2.8 ^ 0.5 vs. 2.5 ^ 0.5; p ¼ 0.01) and were more
thoracostomy. Of the 22 patients who required chest likely to have prolonged length of hospital stay
tube insertion, 17 patients were managed with [8.5 days (2–117) vs. 7 (1–139); p ¼ 0.05].
immediate tube thoracostomy, whereas five On the other hand, conservatively treated patients
patients failed conservative management and were more likely to be involved in motor
required delayed chest tube insertion (2 patients vehicle crashes and pedestrian injuries (p ¼ 0.03
had a progression of the occult pneumothorax on for all).
follow-up chest radiographs, two developed The overall mortality was 4.0%, and all deaths
pleural effusion, and one had increased occurred during the index admission in patients who
respiratory distress with oxygen desaturation sustained polytrauma (ISS $ 29) and head injury
while on PPV). and were treated without a chest tube. Table 2
The mean ISS was 16.4 ^ 9.4 and the median chest shows the characteristics of patients who required
AIS was 3 (range 2–5). The median duration of PPV delayed tube thoracostomy. Although it was
was 10 (range: 1–25) days, and hospital length of statistically not significant, patients who failed
stay was 7 (range: 1–139) days. Pneumonia was the conservative management were more likely to
commonest in-hospital complication, observed in have frequent lung contusion, had greater
12.8% of cases. pneumothorax thickness, required PPV, and were
Table 1 reveals a comparison between tube severely injured with greater ISS as compared
thoracostomy and conservatively treated patients with those who were successfully treated
groups. As compared with those who were conservatively.
4 QATAR MEDICAL JOURNAL
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
Figure 1. Computed tomography scan findings of occult pneumothorax thickness in millimeters.
DISCUSSION pneumothorax. The present study, utilizing nationally
representative data, assessed the clinical presen-
Occult pneumothorax is a relatively infrequent
tation, management, and outcomes of thorax trauma
manifestation of blunt chest injuries that varies in
patients found to have occult pneumothorax on CT
frequency from 1.8% to 6%.6 In our center, around
scan. There are several key findings of this study. First,
7.8% of BCT patients were found to have occult
Figure 2. Case 1 (a) Chest radiograph and (b) corresponding computed tomography scan of a patient with a 31.5 mm
pneumothorax on the left side not identified on chest X-ray. Case 2: (c) Chest radiograph with evidence of pneumothorax
progression and (d) chest radiograph on admission.
QATAR MEDICAL JOURNAL 5
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
Figure 3. Management of patients with occult pneumothorax in the current study.
the majority (85%) of patients who were diagnosed Occult pneumothoraxes are relatively recent radio-
with occult pneumothorax could be successfully logical phenomena that appeared with the upsurge of
treated conservatively. Second, the leading mechan- thoracic CT scans as the initial screening modalities for
ism of injury was MVC and pedestrian trauma. Third, investigation of BCT.6,20 Several researchers suggest
the failure rate of conservative management was low that close observation for occult pneumothorax is
and was more likely to be associated with lung safer and feasible if there is no respiratory distress or
contusion, greater pneumothorax thickness, the need progression in the size of pneumothorax on the
for PPV, and greater injury severity. radiographic follow-up.21 – 23 This is in agreement
Historically, tube thoracostomy was the preferred with our findings of a 96% success rate of expectant
treatment approach for pneumothorax, hemothorax, management in occult pneumothorax patients.
empyema, and hemopneumothorax, and at the time Approximately 15% of patients in this series required
of the Vietnam War, it was considered as the standard chest tube placement. Of them, 17 patients were
of care.18 However, placement of a thoracostomy managed with immediate tube thoracostomy based
tube is not without risk, and in some cases there may on the attending physician’s discretion, and five
be a chance of incomplete drainage. The major patients who failed observation underwent delayed
complication rate for tube thoracostomy is nearly tube thoracostomy. Our incidence is slightly lower
22%, including pneumothorax after tube removal, than that reported by the American Association for
infections (empyema or wound infection), and the surgery of trauma (AAST) multicenter study and
insertional (intercostal artery or intraparenchymal may be due to the absence of concurrent occult
lung injuries) technical error.19 hemothorax, which was not regarded as an exclusion
6 QATAR MEDICAL JOURNAL
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
Table 2. Demographics, clinical presentation and outcome of patients with failed conservative
management.
Variables Value
Age (mean ^ SD) yrs 25.0 ^ 9.3
Males 4 (80.0%)
Lung contusion 5 (100%)
Rib fracture 3 (60.0%)
Number of fractured ribs 2 (1–7)
Pneumothorax thickness (mm) median, range 15 (3–46)
Bilateral pneumothorax 1 (20.0%)
Intubation 2 (40.0%)
Mechanical ventilation 2 (40.0%)
Chest abbreviated injury score 2 (2–3)
Injury severity score 21.8 ^ 2.9
Surgical intervention 0 (0.0%)
Pneumonia 1 (20.0%)
Ventilatory days 11 (5–17)
ICU length of stay 11.5 (5–21)
Hospital length of stay 16 (9–21)
Mortality 0 (0.0%)
ICU: Intensive care unit.
criterion in that study.24 Moreover, none of our critically ill patients is based on decreased airway
patients developed complications related to delayed pressures and tidal volumes. The management
tube thoracostomy. Given the 10-fold increase that guidelines for mechanical ventilation focused on
has occurred in the use of chest CT for trauma controlling mean and peak airway pressures and very
evaluation, Plurad et al.25 studied 1,873 chest CT low pressures.30 The lower tidal volumes (5 –7 mL/
results after negative chest X-rays. They concluded kg) and average peak inspiratory pressure (18.7) were
that the number of patients who needed treatment used in the current study. In our cohort, 32 patients
was small in spite of the increase in occult findings. required PPV, 26 (78.8%) were treated conserva-
Enderson et al.26 evaluated the efficacy of tube tively, and seven (21.2%) patients required tube
thoracostomy in trauma patients with occult thoracostomy; of them, two failed expectant
pneumothorax in a randomized prospective study. management and later on underwent tube
The authors reported that the size of initial occult thoracostomy.
pneumothorax could not predict the formation or Similar to our findings, Barrios et al.31 reported an
progression of a tension pneumothorax. Patient with 80% success rate for observational management in
occult pneumothorax that requires mechanical patients with occult pneumothorax (80%) who
ventilation should undergo chest tube insertion.26 required mechanical ventilation with PPV. An earlier
Other investigators also recommended chest tube study showed successful conservative management
insertion in occult pneumothorax patients subjected in 53% of occult pneumothorax patients requiring
to PPV due to the associated risk of developing PPV.26
tension pneumothorax.7,27,28 It has been suggested that a conservative
The current strategies for mechanical ventilation have management approach can be considered in
been improved because of evidence-based medicine. patients with mild injuries who are hemodynamically
Pinhu et al.29 recommended adjustment of few stable. Therefore, tube thoracostomy in chest
parameters including an increase in tidal volumes from trauma patients is not an essential part of the
8 to 10 mL/kg, peak inspiratory pressure limits of management strategy.32 Moreover, a prior study
40 –50 cm H2O, and limited positive end-expiratory showed that observation is at least as safe and
pressure. Standard practice for the management of effective as tube thoracostomy in patients with
QATAR MEDICAL JOURNAL 7
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
occult pneumothorax.33 A recent study by Zhang determining the need for tube thoracostomy. Patients
et al.34 also supported conservative management in who fail conservative management may have a
occult pneumothorax due to the lower rate of greater pneumothorax thickness and higher ISS.
complications compared with chest tube insertion; However, large prospective studies are warranted to
these observations corroborate well with our support these results and to establish institutional
findings.35 – 37 guidelines for the management of occult
pneumothorax.
Limitations
The major limitation of the study is the single center ACKNOWLEDGEMENT
and small sample size of patients who underwent tube
thoracostomy. As this is a retrospective study, We thank the registry database team in the Trauma
management decisions, with the placement of Surgery Section, Hamad General Hospital, Qatar.
prophylactic tube thoracostomy on admission, Ethics Approval
especially for patients who required PPV, were not
The study obtained ethical approval from Research
dictated by the study protocol but represented a lack
Ethics Committee, at Medical Research Center,
of consensus in the current practice. The lack of
Hamad Medical Corporation, Doha, Qatar
understanding of why 17 patients underwent
(IRB#14513/14). A waiver of consent was granted as
immediate chest tube placement could be in part
no direct contact with patients and data were
explained by the physician’s discretion in the lack of
anonymous.
consensus and institutional protocols. In addition,
multivariate analysis to identify the clinical predictors Data Availability
of failure of conservative management was imprac- Data will be available upon request after approval and
tical due to the small numbers of outcomes (five signing agreement with the Medical Research Center
patients who underwent delayed tube thoracostomy (research@hmc.org.qa)
after failed observation). The incidence of occult
pneumothorax in our database may have been Funding
underestimated as we did not have an institutional This research did not receive any specific grant from
protocol to follow during that era. any funding agency in the public, commercial or not-
for-profit sector.
CONCLUSIONS
Patients with occult pneumothorax can be success- Competing Interests
fully managed conservatively with clinical follow-up The authors have no conflict of interest, no financial
as the treatment of choice. Intervention should be issues to disclose and no funding was received for this
limited to those patients who have a pneumothorax of study.
increasing size on follow-up radiographs or become This study was presented in part at the 18th European
symptomatic under observation. The initial size of the Congress for Trauma and Emergency Surgery (ECTES
occult pneumothorax did not seem to be significant in 2017), May 7-9, 2017, in Bucharest, Romania.
REFERENCES
1. Ball CG, Kirkpatrick AW, Laupland KB, Fox DI, Nicolaou critically ill adult. Am J Roentgenol. 1985;144:
S, Anderson IB, et al. Incidence, risk factors, and 901 – 905.
outcomes for occult pneumothoraces in victims of
4. Kurdziel JC, Dondelinger RF, Hemmer M. Radiological
major trauma. J Trauma. 2005;59(4):917-24;
discussion: 924 – 925. management of blunt polytrauma with CT and
angiography: an integrated approach. Ann Radiol.
2. Chiles C, Ravin CE. Radiographic recognition of 1987;30:121 – 124.
pneumothorax in the intensive care unit. Crit Care
5. Chen L, Zhang Z. Bedside ultrasonography for
Med. 1986;14:677 –680.
diagnosis of pneumothorax. Quant Imaging Med Surg.
3. Tocino IM, Miller MH, Fairfax WR. Distribution of 2015;5(4):618– 623.
pneumothorax in the supine and semirecumbent
8 QATAR MEDICAL JOURNAL
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
6. Ball CG, Kirkpatrick AW, Feliciano DV. The occult 19. Deneuville M. Morbidity of percutaneous tube
pneumothorax: what have we learned? Can J Surg. thoracostomy in trauma patients. Eur J Cardiothorac
2009;52(5):E173 – E179. Surg. 2002;22:673 – 678.
7. Ball CG, Hameed SM, Evans D, Kortbeek JB, 20. Guerrero-López F, Vazquez-Mata G, Alcazar-Romero
Kirkpatrick AW. Canadian Trauma Trials Collaborative. PP, Fernández-Mondéjar E, Aguayo-Hoyos E, Linde-
Occult pneumothorax in the mechanically Valverde CM. Evaluation of the utility of computed
ventilated trauma patient. Can J Surg. 2003;46(5): tomography in the initial assessment of the critical
373 – 379. care patient with chest trauma. Crit Care Med.
2000;28:1370–1375.
8. Omar HR, Abdelmalak H, Mangar D, Rashad R, Helal E,
Camporesi EM. Occult pneumothorax, revisited. 21. Brasel KJ, Stafford RE, Weigelt JA, Tenquist JE,
J Trauma Manag Outcomes. 2010 Oct;4:12. Borgstrom DC. Treatment of occult pneumothoraces
from blunt trauma. J Trauma. 1999;46:987 – 991.
9. Ball CG, Lord J, Laupland KB, Gmora S, Mulloy RH, Ng
AK, et al. Chest tube complications: how well are we 22. Hill SL, Edmisten T, Holtzman G, Wright A. The occult
training our residents? Can J Surg. 2007;50(6): pneumothorax: an increasing entity in trauma. Am
450 – 458. Surg. 1999;65:254 – 258.
10. Mowery NT, Gunter OL, Collier BR, Diaz JJ, Jr, Haut E, 23. Collins JC, Levine G, Waxman K. Occult traumatic
Hildreth A, et al. Practice management guidelines for pneumothorax: immediate tube thoracostomy versus
management of hemothorax and occult pneu- expectant management. Am Surg. 1992;58:
mothorax. J Trauma. 2011;70(2):510 –518. 743 –746.
11. American College of Surgeons Committee. Advanced 24. Moore FO, Goslar PW, Coimbra R, Velmahos G,
trauma life support program for doctors. 9th ed. Brown CV, Coopwood TB Jr, et al. Blunt traumatic
Chicago: American College of Surgeons; 2013. occult pneumothorax: is observation safe?-results
of a prospective, AAST multicenter study.
12. Michaeli P, Munnangi S, Digiacomo JC, Gonzalez E,
J Trauma. 2011;70(5):1019–1023, discussion
Catherine AMK. Factors associated with chest tube
1023-5.
placement in blunt trauma patients with an occult
pneumothorax. Crit Care Res Pract. 2019;2019. 25. Plurad D, Green D, Demetriades D, Rhee P. The
increasing use of chest computed tomography for
13. Hefny AF, Kunhivalappil FT, Matev N, Avila NA, Bashir
trauma: is it being over utilized? J Trauma.
MO, Abu-Zidan FM. Management of computed
2007;62:631 – 635.
tomography-detected pneumothorax in patients with
blunt trauma: experience from a community-based 26. Enderson BL, Abdalla R, Frame SB, Casey MT,
hospital. Singapore Med J. 2018;59(3):150 –154. Gould H, Maull KI. Tube thoracostomy for occult
pneumothorax: a prospective randomized study of
14. Fulton C, Bratu I. Occult pneumothoraces in ventilated
its use. J Trauma. 1993;35(5):726 –729, discussion
pediatric trauma patients: a review. Can J Surg.
729-30.
2015;58(3):177 –180.
27. Bridges KG, Welch G, Silver M, Schinco MA, Esposito B.
15. Kirkpatrick AW, Rizoli S, Ouellet JF, Roberts DJ, Sirois
CT detection of occult pneumothorax in multiple
M, Ball CG, et al. Canadian Trauma Trials Collaborative
trauma patients. J Emerg Med. 1993;11(2):
and the Research Committee of the Trauma Associ-
179 –186.
ation of Canada. Occult pneumothoraces in critical
care: a prospective multicenter randomized controlled 28. Omert L, Yeaney WW, Protech J. Efficacy of thoracic
trial of pleural drainage for mechanically ventilated computerized tomography in blunt chest trauma.
trauma patients with occult pneumothoraces. Am Surg. 2001;67:660 – 667.
J Trauma Acute Care Surg. 2013;74(3):747 –54,
29. Pinhu L, Whitehead T, Evans T, Griffiths M. Ventilator-
discussion 754-5.
associated lung injury. Lancet. 2003;361(9354):
16. De Moya MA, Seaver C, Spaniolas K, Inaba K, Nguyen 332 –340.
M, Veltman Y, et al. Occult pneumothorax in trauma
30. Pham T, Brochard LJ, Slutsky AS. Mechanical
patients: development of an objective scoring system.
Ventilation: State of the Art. Mayo Clin Proc.
J Trauma. 2007;63:13 – 17.
2017;92(9):1382 – 1400.
17. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM.
31. Barrios C, Tran T, Malinoski D, Lekawa M, Dolich M,
CDC definitions for nosocomial infections. Am J Infect
Lush S, et al. Successful management of occult
Control. 1988;16:128 –140.
pneumothorax without tube thorocostomy despite
18. Monaghan SF, Swan KG. Tube thoracostomy: the positive pressure ventilation. Am Surg. 2008;74(10):
struggle to the standard of care. Ann Thorac Surg. 958 –961.
2008;86(6):2019 – 2022.
QATAR MEDICAL JOURNAL 9
VOL. 2020 / ART. 10
Occult pneumothorax in trauma Mahmood et al.
32. Pramod T, Shashirekha CA, Chandan KR, Harsha R. patients with significant blunt chest trauma:
Role of conservative management of traumatic incidence and management. Injury. 2010;41:
chest injuries: a retrospective study & review 492 –494.
of literature. Int J Sci Stud. 2015;3(8):
36. Wilson H, Ellsmere J, Tallon J, Kirkpatrick A. Occult
147 –150.
pneumothorax in the blunt trauma patient: tube
33. Yadav K, Jalili M, Zehtabchi S. Management of thoracostomy or observation? Injury. 2009;40(9):
traumatic occult pneumothorax. Resuscitation. 928 –931.
2010;81(9):1063 – 1068.
37. Mahmood I, Tawfeek Z, El-Menyar A, Zarour A, Afifi I,
34. Zhang M, Teo LT, Goh MH, Leow J, Go KT. Occult Kumar S, et al. Outcome of concurrent occult
pneumothorax in blunt trauma: is there a need for tube hemothorax and pneumothorax in trauma patients
thoracostomy? Eur J Trauma Emerg Surg. 2016; who required assisted ventilation. Emerg Med Int.
42(6):785 – 790. 2015;2015.
35. Lee KL, Graham CA, Yeung JHH, Ahuja AT,
Rainer TH. Occult pneumothorax in Chinese
10 QATAR MEDICAL JOURNAL
VOL. 2020 / ART. 10
You might also like
- Anatomy and Physiology of LarynxDocument37 pagesAnatomy and Physiology of Larynxsuci100% (1)
- Surface Anatomy: de La Salle-Lipa College of LawDocument79 pagesSurface Anatomy: de La Salle-Lipa College of LawFatzie MendozaNo ratings yet
- SURGERY 2020-2008 Chapter Wise Question Papers WBUHS © Medical JunctionDocument18 pagesSURGERY 2020-2008 Chapter Wise Question Papers WBUHS © Medical JunctionRanjan SorenNo ratings yet
- Thoracic Trauma ManagementDocument122 pagesThoracic Trauma ManagementMarina Maleș100% (1)
- Tues 10-20 Peripheral Nerve Disorders - A Practical OverviewDocument36 pagesTues 10-20 Peripheral Nerve Disorders - A Practical OverviewGery FirmansyahNo ratings yet
- Normal and Pathological Bronchial Semiology: A Visual ApproachFrom EverandNormal and Pathological Bronchial Semiology: A Visual ApproachPierre Philippe BaldeyrouNo ratings yet
- Edwardus T. Adar 1308012050: Consultant Dr. Stef D. Soka, SP.BDocument21 pagesEdwardus T. Adar 1308012050: Consultant Dr. Stef D. Soka, SP.BAlbert RanggaNo ratings yet
- Occult PneumotoraxDocument30 pagesOccult PneumotoraxAdif FlysNo ratings yet
- Early and Persistent Hemothorax and PneumothoraxDocument7 pagesEarly and Persistent Hemothorax and Pneumothoraxtri_budi_20No ratings yet
- A Case of Pneumoperitoneum in A Patient With Blunt Injury ThoraxDocument4 pagesA Case of Pneumoperitoneum in A Patient With Blunt Injury ThoraxRajeev ThilakNo ratings yet
- Myz 058Document7 pagesMyz 058tituandreescu6810No ratings yet
- Research Paper On PneumothoraxDocument7 pagesResearch Paper On Pneumothoraxgz8xbnex100% (1)
- Occult Pneumothorax, Revisited: Review Open AccessDocument6 pagesOccult Pneumothorax, Revisited: Review Open AccessRendy NunuhituNo ratings yet
- Bmri2016 3741426Document7 pagesBmri2016 3741426MandaNo ratings yet
- Vats Yustinus Rurie WirawanDocument6 pagesVats Yustinus Rurie Wirawanrurie wirawanNo ratings yet
- Ajtccm 27 1 054Document5 pagesAjtccm 27 1 054Saniska NCTNo ratings yet
- Olesen2018 PDFDocument9 pagesOlesen2018 PDFS3V4_9154No ratings yet
- Mahmood2011 PDFDocument4 pagesMahmood2011 PDFVõ Ngọc ThiệnNo ratings yet
- Occult Hemopneumothorax Following Chest Trauma Does Not Need A Chest TubeDocument5 pagesOccult Hemopneumothorax Following Chest Trauma Does Not Need A Chest TubeNoven MezaNo ratings yet
- Treatment Options of Spontaneous Pneumothorax: Abdullah Al-QudahDocument10 pagesTreatment Options of Spontaneous Pneumothorax: Abdullah Al-QudahIneMeilaniNo ratings yet
- Usg PneumotoraksDocument7 pagesUsg Pneumotoraksdicky wahyudiNo ratings yet
- Clinical Approach For The Pneumomediastinum After Blunt Chest TraumaDocument7 pagesClinical Approach For The Pneumomediastinum After Blunt Chest TraumaIdham Adyasa Manggala PutraNo ratings yet
- Current Treatment of Mesothelioma TCNA 2016Document17 pagesCurrent Treatment of Mesothelioma TCNA 2016Javier VegaNo ratings yet
- Prehospital Ultrasound Imaging Improves Management of Abdominal TraumaDocument5 pagesPrehospital Ultrasound Imaging Improves Management of Abdominal TraumaAhmad Hasbi Al-MuzakyNo ratings yet
- Thoracoscopy in The Management of Pediatric Empyemas: Original ArticleDocument6 pagesThoracoscopy in The Management of Pediatric Empyemas: Original ArticleBALTAZAR OTTONELLONo ratings yet
- Posttrx Empyema PDFDocument6 pagesPosttrx Empyema PDFAndyGcNo ratings yet
- TRAUMA Pulmones, Traquea y EsofagoDocument14 pagesTRAUMA Pulmones, Traquea y EsofagosantigarayNo ratings yet
- Thoracoscopic Drainage of EmpyemaDocument5 pagesThoracoscopic Drainage of EmpyemaDr Nilesh NagdeveNo ratings yet
- ACI Evidence Review Diagnosis Treatment Traumatic PneumothoraxDocument41 pagesACI Evidence Review Diagnosis Treatment Traumatic Pneumothoraxhenryyech2No ratings yet
- JTD 10 06 3216Document9 pagesJTD 10 06 3216madeNo ratings yet
- Clearing The Air - A Conservative Option For Spontaneous PneumothoraxDocument2 pagesClearing The Air - A Conservative Option For Spontaneous PneumothoraxDivara SyautaNo ratings yet
- Doenças PleuraisDocument9 pagesDoenças Pleuraiselizete rodriguesNo ratings yet
- Timing of Tracheostomy For Prolonged Respiratory Wean in Critically Ill Coronavirus Disease 2019 Patients A Machine Learning ApproachDocument9 pagesTiming of Tracheostomy For Prolonged Respiratory Wean in Critically Ill Coronavirus Disease 2019 Patients A Machine Learning ApproachDewa OkaNo ratings yet
- Abordaje Nodulo PulmonarDocument11 pagesAbordaje Nodulo PulmonarDore NanNo ratings yet
- PnemotoraksDocument4 pagesPnemotoraksGung Citra PratikaNo ratings yet
- Comparative Treatments of EmpyemaDocument4 pagesComparative Treatments of EmpyemaIJAR JOURNALNo ratings yet
- Egyptian Journal of Ear, Nose, Throat and Allied SciencesDocument5 pagesEgyptian Journal of Ear, Nose, Throat and Allied SciencesLuis De jesus SolanoNo ratings yet
- Chest: Postgraduate Education CornerDocument8 pagesChest: Postgraduate Education CornerCristian LermaNo ratings yet
- Tierney2019 PDFDocument7 pagesTierney2019 PDFKarlita BrocaNo ratings yet
- Five Years Experience of Tracheostomy at A Tertiary Level Hospital (Dhaka Medical College Hospital) in Bangladesh Review of 257 CasesDocument8 pagesFive Years Experience of Tracheostomy at A Tertiary Level Hospital (Dhaka Medical College Hospital) in Bangladesh Review of 257 CasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1 s2.0 S000709122200366X MainDocument12 pages1 s2.0 S000709122200366X MainTlally Itzel Zamora CastroNo ratings yet
- Pnemothorax PDFDocument10 pagesPnemothorax PDFHelpful HandNo ratings yet
- Sonographic Diagnosis of Pneumothorax: Journal of Emergencies Trauma and Shock January 2012Document7 pagesSonographic Diagnosis of Pneumothorax: Journal of Emergencies Trauma and Shock January 2012Сергей КапустинNo ratings yet
- Management of Primary Spontaneous Pneumothorax in Chinese ChildrenDocument7 pagesManagement of Primary Spontaneous Pneumothorax in Chinese ChildrenArsy Mira PertiwiNo ratings yet
- Pediatric Pulmonology - 2023 - Zarfati - Conservative and Operative Management of Spontaneous Pneumothorax in Children andDocument7 pagesPediatric Pulmonology - 2023 - Zarfati - Conservative and Operative Management of Spontaneous Pneumothorax in Children andRezidenti GrigoreNo ratings yet
- 76 FullDocument12 pages76 FullRodrigo Navia ValenzuelaNo ratings yet
- Main PDFDocument6 pagesMain PDFEdison HernandezNo ratings yet
- Pulmonary Contusion in Mechanically Ventilated Subjects After Severe TraumaDocument5 pagesPulmonary Contusion in Mechanically Ventilated Subjects After Severe TraumaFauzan KurniawanNo ratings yet
- Asthma: Further ReadingDocument13 pagesAsthma: Further ReadingcarlosNo ratings yet
- Gaudet 2016Document11 pagesGaudet 2016Giancarlo Maruri MunarettoNo ratings yet
- Efficacy of Portable Ultrasound To Detect Pneumothorax Post Lung ResectionDocument5 pagesEfficacy of Portable Ultrasound To Detect Pneumothorax Post Lung ResectionPaul HartingNo ratings yet
- P Nemo ThorakDocument5 pagesP Nemo ThoraklukmanNo ratings yet
- Jurnal 5Document7 pagesJurnal 5nskhldNo ratings yet
- Microcoil-Guided Video-Assisted ThoracoscopicDocument6 pagesMicrocoil-Guided Video-Assisted Thoracoscopicomamah.almousaNo ratings yet
- Current Practices in Endotracheal Tube Size Selection For AdultsDocument5 pagesCurrent Practices in Endotracheal Tube Size Selection For AdultsBriando Stevano LinelejanNo ratings yet
- Early Management of Retained Hemothorax in Blunt HeadDocument15 pagesEarly Management of Retained Hemothorax in Blunt HeadArHamNo ratings yet
- HRT 08900369Document2 pagesHRT 08900369Gonzalo Cedrés Di MarcoNo ratings yet
- Thoracictrauma: Which Chest Tube When and Where?Document11 pagesThoracictrauma: Which Chest Tube When and Where?Nilson Bruges MarinNo ratings yet
- The Value of HRCT Chest in Diagnosis of COVID 19 and Its Correlation With RT-PCRDocument5 pagesThe Value of HRCT Chest in Diagnosis of COVID 19 and Its Correlation With RT-PCREditor IJETBSNo ratings yet
- Pneumotoraks Management GuidelinesDocument44 pagesPneumotoraks Management GuidelinesWewik PenaNo ratings yet
- Pneumotoraks Management GuidelinesDocument44 pagesPneumotoraks Management GuidelinesYohana KoliNo ratings yet
- Blunt Abdominal Trauma Treatment & Management - Approach Considerations, Prehospital Care, Emergency Department CareDocument8 pagesBlunt Abdominal Trauma Treatment & Management - Approach Considerations, Prehospital Care, Emergency Department CareyunikayunNo ratings yet
- GJHS 6 221Document5 pagesGJHS 6 221Teuku FaisalNo ratings yet
- Jurnal PneumoniaDocument14 pagesJurnal PneumoniaArmy OktaviantoNo ratings yet
- Thorac Clinics Prophylaxis of ComplicationsDocument15 pagesThorac Clinics Prophylaxis of Complicationsvinicius.alvarez3No ratings yet
- Spontaneous Pneumothorax: New Horizons: Avinash AujayebDocument4 pagesSpontaneous Pneumothorax: New Horizons: Avinash AujayebAnangova PradiptaNo ratings yet
- Diagnosis and Treatment of Thoracic In-Juries and Traumatic HemopneumothoraxDocument4 pagesDiagnosis and Treatment of Thoracic In-Juries and Traumatic HemopneumothoraxAnangova PradiptaNo ratings yet
- Hitscrubs: InvoiceDocument1 pageHitscrubs: InvoiceAnangova PradiptaNo ratings yet
- Open and Closed Treatment of Chest Injuries: Mortality, Hospitalization, Trauma Indices and Physiological DataDocument2 pagesOpen and Closed Treatment of Chest Injuries: Mortality, Hospitalization, Trauma Indices and Physiological DataAnangova PradiptaNo ratings yet
- Diagnosis and Treatment of Thoracic In-Juries and Traumatic HemopneumothoraxDocument4 pagesDiagnosis and Treatment of Thoracic In-Juries and Traumatic HemopneumothoraxAnangova PradiptaNo ratings yet
- Survive After Cardiac Arrest During Emergency Thoracotomy Due To Penetrating Thoracic Trauma in Resource Limited SettingsDocument8 pagesSurvive After Cardiac Arrest During Emergency Thoracotomy Due To Penetrating Thoracic Trauma in Resource Limited SettingsAnangova PradiptaNo ratings yet
- Bauman2021 Article RandomizedClinicalTrialOf14-FrDocument7 pagesBauman2021 Article RandomizedClinicalTrialOf14-FrAnangova PradiptaNo ratings yet
- Survive After Cardiac Arrest During Emergency Thoracotomy Due To Penetrating Thoracic Trauma in Resource Limited SettingsDocument8 pagesSurvive After Cardiac Arrest During Emergency Thoracotomy Due To Penetrating Thoracic Trauma in Resource Limited SettingsAnangova PradiptaNo ratings yet
- Thoracic Trauma - Principals of Surgical Management: Jerzy Lasek, Eugeniusz JadczukDocument9 pagesThoracic Trauma - Principals of Surgical Management: Jerzy Lasek, Eugeniusz JadczukAnangova PradiptaNo ratings yet
- Travel Characteristics of Older and Disaled People in The Colombo DistrictDocument4 pagesTravel Characteristics of Older and Disaled People in The Colombo DistrictShan BasnayakeNo ratings yet
- SURGERY 07 BurnsDocument1 pageSURGERY 07 BurnsMikhail LamayoNo ratings yet
- Surgery (Ortho) NotesDocument155 pagesSurgery (Ortho) NotesprestigeuniversaltradingNo ratings yet
- Unit 7 - Answer KeyDocument2 pagesUnit 7 - Answer KeyRico Rusli100% (1)
- Journal of Sports SciencesDocument7 pagesJournal of Sports SciencesASD2019No ratings yet
- Referat Limba Engleză-Zidaroiu Ionuț-EduardDocument6 pagesReferat Limba Engleză-Zidaroiu Ionuț-EduardEduard IonutNo ratings yet
- Introduction To LocomotorDocument148 pagesIntroduction To LocomotorsherinprinceNo ratings yet
- Bench Posture US WebDocument1 pageBench Posture US WebFelipe JuniorNo ratings yet
- Black and Decker Mouse Sander ms600bDocument32 pagesBlack and Decker Mouse Sander ms600bd sNo ratings yet
- Application of Roller-Elastic BandageDocument6 pagesApplication of Roller-Elastic Bandagekuro hanabusaNo ratings yet
- Biomechanics of Ankle and Foot - 20 Questions-2Document3 pagesBiomechanics of Ankle and Foot - 20 Questions-2rehab aymanNo ratings yet
- ASIADocument2 pagesASIALuis Galván BastidasNo ratings yet
- Incomplete Spinal Cord Injury Nursing CareDocument6 pagesIncomplete Spinal Cord Injury Nursing CareTherese MargaretNo ratings yet
- Axila: Mesole Samuel Bolaji (B.SC M.SC PHD (In-View) ) Course: Anatomy Course Code: Han 3010Document15 pagesAxila: Mesole Samuel Bolaji (B.SC M.SC PHD (In-View) ) Course: Anatomy Course Code: Han 3010Tinotenda KarumeNo ratings yet
- Accessory NavicularDocument24 pagesAccessory NavicularsprapurNo ratings yet
- Hip Injuries in Athletes: Understanding the AnatomyDocument24 pagesHip Injuries in Athletes: Understanding the AnatomysaadNo ratings yet
- Manual Material Handling Shoveling DiggingDocument2 pagesManual Material Handling Shoveling Diggingluis VelozNo ratings yet
- Le Orthopedic Conditions: Ankle - Ankle SprainDocument9 pagesLe Orthopedic Conditions: Ankle - Ankle SprainJyrra NeriNo ratings yet
- Physical Education: Festival DancesDocument41 pagesPhysical Education: Festival DancesPinoy Ziraniko VlogzNo ratings yet
- Taller Bone TissueDocument2 pagesTaller Bone TissueANDREA CATALINA CORTES HERNANDEZNo ratings yet
- Accessory, Hypoglossal NervesDocument21 pagesAccessory, Hypoglossal NervesArbin PanjaNo ratings yet
- Management RTSDocument6 pagesManagement RTSilham Maulana ArifNo ratings yet
- Manual - HM1801-HM1812 DEMOLEDOR ELECTRICO-minDocument20 pagesManual - HM1801-HM1812 DEMOLEDOR ELECTRICO-minYeraldin SalinasNo ratings yet
- Abordaje Deltopectoral Vs TransdeltoideoDocument34 pagesAbordaje Deltopectoral Vs TransdeltoideoNinhoTonyOfficialNo ratings yet
- First Middle East Experience WDocument8 pagesFirst Middle East Experience WAsmat BurhanNo ratings yet