Professional Documents
Culture Documents
Management Strategies of Patients With Neuromyelitis Optica Spectrum Disorder During The COVID-19 Pandemic Era
Management Strategies of Patients With Neuromyelitis Optica Spectrum Disorder During The COVID-19 Pandemic Era
Uploaded by
Adriana BahnaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management Strategies of Patients With Neuromyelitis Optica Spectrum Disorder During The COVID-19 Pandemic Era
Management Strategies of Patients With Neuromyelitis Optica Spectrum Disorder During The COVID-19 Pandemic Era
Uploaded by
Adriana BahnaCopyright:
Available Formats
Therapeutics and Clinical Risk Management Dovepress
open access to scientific and medical research
Open Access Full Text Article
REVIEW
Management Strategies of Patients with
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
Neuromyelitis Optica Spectrum Disorder
During the COVID-19 Pandemic Era
This article was published in the following Dove Press journal:
Therapeutics and Clinical Risk Management
Sherif M Hamdy Abstract: The ongoing coronavirus (COVID-19) pandemic is a global health emergency of
Maged Abdel-Naseer international concern and has affected management plans of many autoimmune disorders.
Hatem S Shehata Immunosuppressive and immunomodulatory therapies are pivotal in the management of
Nevin M Shalaby neuromyelitis optica spectrum disorder (NMOSD), potentially placing patients at an
For personal use only.
increased risk of contracting infections such as COVID-19. The optimal management
Amr Hassan
strategy of NMOSD during the COVID-19 era remains unclear. Here, however, we examined
Alaa Elmazny
the evidence of NMOSD disease-modifying therapies (DMTs) use during the present period
Ehab Shaker
and highlighted different scenarios including treatment of relapses as well as initiation and
Mona AF Nada maintenance of DMTs in order to optimize care of NMOSD patients in the COVID-19 era.
Sandra M Ahmed Keywords: neuromyelitis optica spectrum disorder, COVID-19, pandemic
Mohamed I Hegazy
Husam S Mourad
Ahmed Abdelalim
Introduction
Rehab Magdy
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), identified as the
Alshimaa S Othman
cause of coronavirus disease 2019 (COVID-19), is the third known virus of the
Doaa A Mekkawy
coronaviridae family to cause outbreaks of severe acute respiratory syndrome.1
Nirmeen A Kishk
Since the recognition of the disease as a pandemic, concerns have arisen over
Neurology Department, Faculty of patients suffering immune-mediated illnesses requiring management with immuno
Medicine, Cairo University, Cairo, Egypt
modulatory (IM) or immunosuppressant (IS) therapies, given their higher risk for
suffering more severe forms of COVID-19.2
This review discusses the challenges in treating neuromyelitis optica spectrum
disorder (NMOSD) in the COVID-19 era and proposes algorithms for tailoring
potential management of acute relapses as well as the use of disease-modifying
therapies (DMTs) during this critical period.
Pathophysiology of Neuromyelitis Optica Spectrum
Disorder (NMOSD)
The NMOSD represents a group of immunologically mediated, inflammatory
central nervous system (CNS) disorders, involving the production of auto-reactive
antibodies (Abs) against various neuroglial structures. Autoantibodies against water
channel aquaporin-4 (Anti AQP-4 IgG1) are the most common Abs,3 although other
Correspondence: Alaa Elmazny known overlapping Abs include those against myelin oligodendrocyte glycoprotein
66-Manial-Street, Cairo, Egypt
Tel +966536012237
IgG (anti-MOG)4 and glial fibrillary acidic protein (GFAP).5 Cell-mediated immu
Email alaa_elmazny@kasralainy.edu.eg nity (CMI) contributes to the pathophysiology, where polarization of T-lymphocytes
submit your manuscript | www.dovepress.com Therapeutics and Clinical Risk Management 2020:16 759–767 759
DovePress © 2020 Hamdy et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.
http://doi.org/10.2147/TCRM.S261753
php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the
work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For
permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Powered by TCPDF (www.tcpdf.org)
Hamdy et al Dovepress
towards helper Th-17 and Th-2 subtypes results in cyto to patients suffering NMOSD. Questions that are yet to be
kine network alteration6,7 and promotes pro-inflammatory addressed include: (1) whether exposure to certain DMT
cascades and milieu conducive for B-lymphocytes. regimens poses a higher risk of severe COVID-19 infec
A major pathophysiologic role is played by Interleukin tion that may require discontinuation, transient interrup
(IL) 6, a cytokine specifically involved in relapse severity, tion or substitution of therapies, encouraging adoption of
CNS injury and degree of disability.8 Disability in appropriate risk-stratification strategies in the context of
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
NMOSD is highly related to relapses; reduction of relapse individual patient profiles as well as of drug properties; (2)
frequency and adequate relapse management are thus of whether infection with COVID-19, even if asymptomatic,
paramount importance.9 can precipitate acute relapses in otherwise stable patients,
as can any other infection although shared immuno-
pathological pathways between the two disorders would
Pathophysiology of COVID-19
necessitate further risk stratification.
Innate immunity is initially activated following SARS-
Limiting unnecessary procedures in medical centers to
CoV-2 infection, with increased expression of inflamma
preserve resources and reduce person-to-person contact
tory markers (eg CRP, procalcitonin, ferritin) and type-1
warrant consideration (eg delaying follow-up MRI scans
interferons (IFN) in an attempt to limit viral replication
and reducing the frequency of routine laboratory monitor
and spread. Ensuing activation of phagocytosis targets
ing in stable patients). Further measures, such as suspend
infected cells.2
ing non-essential in-person consultations and clinic visits
Eventually, adaptive immunity is activated, and a major
For personal use only.
or substituting it with remote interventions should also be
role is played by CMI via activation of virus-specific
encouraged (eg checking laboratory or MRI results
T-cytotoxic cells (Tc-CD8). Antibody-mediated immunity
through telecommunications).13
and the complement cascade (particularly involving C3, C5)
Tailored recommendations for neurologists managing
additionally aid antibody-dependent cellular cytotoxicity.10
NMOSD patients are currently needed, especially in the
Under optimal conditions, the immune response is well
case of patients acquiring COVID-19.
regulated and results in effective viral clearance and a good
clinical outcome.2 However, in other conditions, viral viru
lence mechanisms result in dysregulation of the immune
Relapse Management
In patients with NMOSD, studies have shown that perma
response and unrestrained viral replication, increased viral
nent damage from relapses leads to cumulative disability;
load, delayed IFN production, accumulation of neutrophils
therefore, the consensus among NMOSD experts is that
and monocytes, and reduction in B and T cells. A storm of
every relapse requires treatment and that rescue medica
pro-inflammatory cytokines follows, characterized by pool
tions should be initiated as early as possible. Preventive
ing of IL-2, −6, −8, −10, and −21, and tumour necrosis factor
treatments should be continued during relapse manage
(TNF)-ß.11 This creates a vicious circle of overactive innate
ment as they play a role in recovery and ameliorating
and dampened adaptive immune responses that are usually
relapse severity.5,14,15
associated with clinical deterioration, acute lung injury, acute
Treatment decisions regarding NMOSD relapses should
respiratory distress syndrome, thrombophilia and multiple
be individualized according to COVID-19 suspicion, relapse
systems organ failure.4
manifestations, need for hospitalization and previous patient
Older age, male gender, smoking, the presence of
responses. Escalation of relapse treatment improves out
comorbidities (particularly diabetes, cardiac and respira
come, and the sequence of therapies is crucial until
tory diseases) and immunosuppression were all found to
a satisfactory response is achieved. Administration of intra
be factors predisposing to dysregulation of the immune
venous methylprednisolone, 1 g daily for 5–7 consecutive
response and thus a worse clinical course among COVID-
days, is typically considered to be the initial treatment of
19 positive patients.2,4,12
choice and patients are encouraged to receive infusions at
home whenever possible.16–19 However, in severe relapses
Dilemmas in NMOSD Management (expanded disability status scale (EDSS) scores ≥2 points),
During COVID-19 this first-line treatment is not sufficient and additional strate
The ongoing COVID-19 pandemic has created unparal gies are required to minimize any residual impairments.20–22
leled challenges for neurologists to deliver the best care In view of the pathophysiology of NMOSD where a strong
760 submit your manuscript | www.dovepress.com Therapeutics and Clinical Risk Management 2020:16
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hamdy et al
humoral response underlies the disease process, plasma throughout the COVID-19 pandemic, owing to its
exchange (PLEX) seems to be the most appropriate therapy immune-boosting and antiviral properties.35–37
in severe relapses and it is accepted as the second-line ther
apy for severe steroid-refractory NMOSD attacks with more
Initiation and Maintenance of DMTs
favorable outcome.23,24 The American Society for Apheresis
Various immunosuppressive agents including azathioprine
(ASFA) considers NMOSD to be a category II indication for
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
(AZA), mycophenolate mofetil (MMF), and cyclopho
PLEX.
sphamide (CTX), as well as monoclonal antibodies includ
With the evidence of complex interactions between the
ing rituximab (RTX), eculizumab, and tocilizumab have
cytokine storm, inflammation, endothelial dysfunction, and
been reported effective in reducing the annualized relapse
thrombophilia resulting from COVID-19 infection25,26
rate and stabilizing EDSS scores of NMOSD patients.38–42
PLEX offers effective removal of inflammatory cytokines
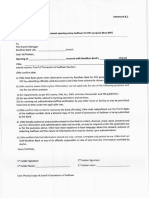
The suggested treatment algorithm for the initiation and
from the blood, stabilization of endothelial membranes,
maintenance of DMTs is outlined in Figure 2.
and reversal of hypercoagulability.25–27
However, PLEX is an invasive procedure with a longer
hospital stay as well as a higher risk of infections and Azathioprine
hemodynamic instability when compared to intravenous This purine antimetabolite is structurally similar to endogen
immunoglobulin (IVIG), especially for patients on ous purine bases and interferes with DNA synthesis. This
immunosuppressants.28 Hence, IVIG administration could results in T cell apoptosis and subsequent
For personal use only.
be a relatively safer option with favorable results in immunosuppression.43 As an immunosuppressive medica
relapse treatment in patients with neurological manifesta tion, this drug increases the risk of bacterial, viral and fungal
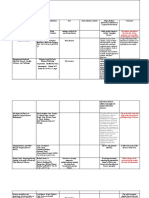
tions not warranting hospital admission29–31 (Figure 1). infection especially when combined with corticosteroids.43
Furthermore, high IVIG doses administered to patients Lymphopenia (especially grade 3 and 4; <500 cells/mL) was
with severe COVID-19 were found to successfully halt the found to increase the risk of opportunistic infection, so fre
progression of the illness and improve clinical outcomes.33,34 quent WBC monitoring as well as dose reduction or even
Monthly IVIG administration is also considered to be medication cessation should be considered.44,45
an effective treatment option in preventing NMOSD In the management of NMOSD, AZA is considered to
relapses in patients with anti-MOG disease, especially be a first-line therapy, and no evidence to date has
Figure 1 Management of a relapse in NMOSD patients during COVID-19 pandemic.32
*After improvement continue on oral steroids for 3-6 months and consider initiation of disease-modifying therapies in newly diagnosed patients.
Abbreviations: CBC, complete blood count; COVID-19, coronavirus disease 2019; CRP, C reactive protein; CT, computed tomography; IVIG, intravenous immunoglo
bulins; IVMP, intravenous methylprednisolone; NMOSD, neuromyelitis optica spectrum disorder; PLEX, plasma exchange.
submit your manuscript | www.dovepress.com
Therapeutics and Clinical Risk Management 2020:16 761
DovePress
Powered by TCPDF (www.tcpdf.org)
Hamdy et al Dovepress
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
Figure 2 Algorithm for initiation and maintenance of DMTs in NMOSD patients during the COVID-19 pandemic.
Abbreviations: ABs, antibodies; COVID-19, coronavirus disease 2019; CTX, cyclophosphamide; DMT, disease modifying therapy; IVIG, intravenous immunoglobulins; MMF,
mycophenolate mofetil; MTX, methotrexate; NMOSD, neuromyelitis optica spectrum disorder.
For personal use only.
suggested that interrupting AZA treatment decreases risks remains effective at controlling disease activity beyond 6
posed by COVID-19.46 months.50
Recommendations Recommendations
AZA can be continued as a maintenance therapy in
Initiation of RTX in NMOSD patients throughout the
NMOSD patients throughout the COVID-19 pandemic
COVID-19 pandemic is not preferable. Stable patients
with regular blood count monitoring. Dosages can be
already undergoing RTX treatment are advised to have their
adjusted based on individual patient profile, disease sever
next infusion postponed for 3 months especially if CD19+
ity and lymphocytic counts.45 However, it is likely safer
and CD27+ memory B cell counts are severely decreased.
not to start AZA in newly diagnosed patients.
In situations where CD19+ and CD27+ memory B cell
levels have stabilized or when 9 months have passed since
Rituximab the prior infusion, the next medication dose cannot be
This monoclonal antibody against CD20-expressing
postponed and it is recommended to either shift from
B lymphocytes has not been found to increase the risk of
RTX to one of the other approved safer monoclonal anti
viral infection; there is likewise no evidence to date that
bodies, or to continue the patient on the same drug after
RTX increases the risk of developing COVID-19.47 Anti-
explaining potential risks and benefits.
CD20 therapies leave the CD8-positive T cell compart
ment of the immune system relatively intact, which is
important to eradicate the virus. However, it is not prefer Mycophenolate Mofetil
able to initiate B cell-depleting agents during a pandemic A prodrug of mycophenolic acid, MMF causes depletion
because they may preclude the formation of long-lasting of guanosine and deoxyguanosine in both T and
immunity against reinfection as well as response to vac B lymphocyte lines via inhibition of inosine-5′-
cines when they become available.48 monophosphate dehydrogenase (type II), an enzyme that
The timing of RTX doses can be determined by mon facilitates the production of an intermediate metabolite of
itoring CD19+ CD27+ memory B cells and does not neces guanosine.52 Net effects include the inhibition of de novo
sarily follow the 6-month interval dosing. Disease control purine synthesis and the suppression of DNA synthesis
in NMOSD patients can be achieved with RTX for an with subsequent interference in both T and B lymphocyte
average of 6–9 months,49–51 and it is now obvious from proliferation, decrease in cytotoxic T cell activity and
the Swedish experience in multiple sclerosis that rituximab diminished antibody formation.53–55 Promising results
762 submit your manuscript | www.dovepress.com Therapeutics and Clinical Risk Management 2020:16
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hamdy et al
have been reported in the setting of many immune- monitoring of patients treated with MTX are recommended;
mediated neurological illnesses including NMOSD.56,57 reduction of doses to less than 10 mg/week should be con
Compared to AZA, MMF was more effective at sidered for patients already undergoing MTX therapy based
achieving remission in some patients with NMOSD and on individual profiles and disease severity. If patients develop
did so with fewer adverse events.58 MIP, are infected with COVID-19 or if lymphocytic count
This drug interferes with IL-17 production by Th17 falls below 1100/mL, MTX should be stopped.
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
cells. A potent pro-inflammatory cytokine that plays
a crucial rule in COVID-19 infection, chronic use of Cyclophosphamide
MMF could have a protective role against serious clinical An alkylating antineoplastic agent, CTX exerts its effects
complications of the disease.59,60 via the active metabolite phosphoramide, resulting in cross-
linkages within and between adjacent DNA strands, ulti
Recommendations mately leading to induction of apoptosis.65 This medication
It is likely safer not to start MMF in newly diagnosed also selectively suppresses T cells and increases the secre
NMOSD patients throughout the pandemic. For patients tion of Th2 cytokines (eg IL-4, IL-10) and decreases the
who are already being treated with MMF, treatment can be secretion of INF-gamma and IL-12 both in the CSF and
maintained with regular blood count monitoring. peripherally.66 Common adverse events include hemorrha
gic cystitis, gonadal toxicity and myelosuppression67.
Methotrexate Myelosuppression increases the risk of infection, which
For personal use only.
A folate antagonist that has multiple dose-related mechanisms may trigger sepsis, particularly at high treatment doses68.
of action, MTX inhibits dihydrofolate reductase and thus DNA Furthermore, immunosuppression induced by CTX in
synthesis in high-dose regimens and aminoimidazole-4-car a murine model infected with influenza A revealed viral
boxamide ribonucleotide in low-dose regimens, ultimately persistence with prolonged shedding.69 The European
interfering with T-cell function, augmenting the release of Medicines Agency approves CTX as a second-line main
intra- and extracellular adenosine that suppresses inflamma tenance therapy for NMOSD patients, especially for those
tion, suppressing the release of pro-inflammatory cytokines (eg with comorbid systemic lupus erythematosus or systemic
TNF-α, IL-6, IL-8, IL-12) and enhancing the production of sclerosis.
anti-inflammatory mediators (eg IL-10 and IL-1).61
In the treatment of NMOSD, MTX is considered to be Recommendations
a second-line option when first-line medications fail or are It is not preferable to initiate CTX in NMOSD patients
inappropriate.62 throughout the COVID-19 pandemic. As CTX is a second-
In addition, MTX therapy is associated with increased line agent, the choice of another alternative as mainte
risk of infection and myelosuppression63 while in up to 14% nance therapy is preferable.
of patients treated with low-dose MTX, a troublesome
adverse event mimicking symptoms of COVID-19, termed Eculizumab
MTX-induced pneumonitis (MIP), has been reported. It typi Eculizumab is a humanized monoclonal antibody
cally presents with dyspnea, dry cough and fever, as well as approved for the treatment of NMOSD in patients who
ground glass opacities on chest CT imaging. Cessation of are AQP4-IgG-seropositive. It binds with high affinity to
MTX and glucocorticoids typically results in a favorable C5, thereby blocking the activation of the terminal com
outcome, although, in some cases, it may be fatal.64 plement pathway.70
An interim Australia/New Zealand recommendation The complements C3a and C5a in particular have very
for patients with severe inflammatory skin disorders was potent pro-inflammatory properties as they trigger neutro
to reduce MTX dosing to less than 10 mg/week to protect phil recruitment and activation, thus playing a vital role in
against COVID-19 infection.45 the immune response to COVID-19 infection. Interestingly,
anti-C5aR antibody was reported to alleviate lung and tissue
Recommendations damage in Middle East respiratory syndrome-related coro
As a second-line agent, it is preferable not to initiate MTX in navirus (MERS-CoV)-infected mice.71
NMOSD patients throughout the COVID-19 pandemic. Despite the fact that experience with the novel mono
Frequent clinical evaluations and complete blood count clonal antibodies in NMOSD treatment is very limited,
submit your manuscript | www.dovepress.com
Therapeutics and Clinical Risk Management 2020:16 763
DovePress
Powered by TCPDF (www.tcpdf.org)
Hamdy et al Dovepress
eculizumab, as a modulator of distal complement, was Satralizumab
found to hold promise in the treatment of patients infected Satralizumab is another humanized monoclonal antibody
with COVID-19.72 that binds the IL-6 receptor but exhibits a more favorable
Commonest reported adverse effects of eculizumab are pharmacokinetic profile than tocilizumab due to
headache (27.0%), upper respiratory tract infection a prolonged elimination half-life.80
(25.5%), nasopharyngitis (22.6%) and bacterial pneumonia As an IL-6 inhibitor, satralizumab is likely beneficial in
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
(2.9%).73 Such adverse respiratory effects may either fal the setting of COVID-19 infection; however, this drug has
sely suggest COVID-19 infection, or mask it. not been investigated in COVID-19 patients.
Recommendations Recommendations
Initiation and maintenance therapy with eculizumab in Initiation and maintenance therapy with satralizumab in
NMOSD patients throughout the COVID-19 pandemic is NMOSD patients throughout the COVID-19 pandemic is
likely safe, even in patients with suspected or confirmed likely safe even in patients with suspected or confirmed
COVID-19. However, careful monitoring for possible upper COVID-19 infection.
respiratory infections as well as bacterial pneumonia is
warranted. Conclusions
There is little evidence to formulate specific recommenda
For personal use only.
tions for patients with NMOSD receiving immunomodula
Tocilizumab
tory treatment with regards to COVID-19. However, in
Tocilizumab is a humanized monoclonal antibody that
everyday clinical practice throughout the pandemic, health
binds to IL-6 receptors and thus blocks their binding IL-
care providers face several obstacles regarding acute and
6, a pro-inflammatory cytokine with a major role in
preventive management of NMOSD patients. Here, we listed
NMOSD pathogenesis.38 Tocilizumab is highly effective
recommendations based on the mechanism of action of each
for aggressive cases of NMOSD refractory to RTX ther
drug and its preferential effects on the immune system, taking
apy. Notably, tocilizumab has an additional role in the
into consideration currently available data, ongoing studies
effective management of chronic neuropathic pain and
and expert opinion. However, treatment decisions regarding
fatigue in NMOSD patients.74 NMOSD patients should be individualized according to dis
In patients with COVID-19 infection, IL-6 levels are ease duration, course and severity, as well as COVID-19 risk.
significantly elevated and associated with adverse outcomes.
Thus, tocilizumab was found to effectively dampen the
inflammatory response and improve patient outcomes.75–77
Disclosure
The authors report no conflicts of interest in this work.
Tocilizumab is generally a safe drug with injection site
reactions the commonest adverse effect (10%). However,
neutropenia, thrombocytopenia and elevated liver enzymes
References
may rarely occur.78 1. Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients
with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733.
Importantly, impaired IL-6 signaling results in normal doi:10.1056/NEJMoa2001017
ization of CRP levels and body temperature even in the 2. Yi Y, Lagniton PNP, Ye S, Li E, Xu R-H. COVID-19: what has been
learned and to be learned about the novel coronavirus disease.
presence of systemic infection.79 Suspicion of COVID-19 Int J Biol Sci. 2020;16(10):1753. doi:10.7150/ijbs.45134
infection in patients receiving IL-6 inhibitors should be 3. Wingerchuk DM, Banwell B, Bennett JL, et al. International consensus
diagnostic criteria for neuromyelitis optica spectrum disorders.
high in the setting of relevant symptomology.
Neurology. 2015;85(2):177–189. doi:10.1212/WNL.0000000000001729
4. Chen G, Wu D, Guo W, et al. Clinical and immunological features of
severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130
Recommendations (5):5. doi:10.1172/JCI137244
Initiation and maintenance therapy with tocilizumab in 5. Kimbrough DJ, Fujihara K, Jacob A, et al. Treatment of neuromyelitis
optica: review and recommendations. Mult Scler Relat Disord. 2012;1
NMOSD patients throughout the COVID-19 pandemic (4):180–187. doi:10.1016/j.msard.2012.06.002
is likely safe, even in patients with suspected or con 6. Varrin-Doyer M, Spencer CM, Schulze-Topphoff U, et al. Aquaporin
4-specific T cells in neuromyelitis optica exhibit a Th17 bias and
firmed COVID-19 as tocilizumab is possibly dually recognize Clostridium ABC transporter. Ann Neurol. 2012;72
effective. (1):53–64. doi:10.1002/ana.23651
764 submit your manuscript | www.dovepress.com Therapeutics and Clinical Risk Management 2020:16
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hamdy et al
7. Uzawa A, Masahiro M, Kuwabara S. Cytokines and chemokines in 26. Gyawali B, Ramakrishna K, Dhamoon AS. Sepsis: the evolution in
neuromyelitis optica: pathogenetic and therapeutic implications. definition, pathophysiology, and management. SAGE Open Med.
Brain Pathol. 2014;24(1):67–73. doi:10.1111/bpa.12097 2019;7:2050312119835043. doi:10.1177/2050312119835043
8. Uzawa A, Mori M, Kuwabara S. Role of interleukin-6 in the patho 27. Nguyen TC, Carcillo JA. Bench-to-bedside review: thrombocytope
genesis of neuromyelitis optica. Clin Exp Neuroimmunol. 2013;4 nia-associated multiple organ failure–a newly appreciated syndrome
(2):167–172. doi:10.1111/cen3.12024 in the critically ill. Critical Care. 2006;10(6):235. doi:10.1186/
9. Huda S, Whittam D, Bhojak M, Chamberlain J, Noonan C, Jacob A. cc5064
Neuromyelitis optica spectrum disorders. Clin Med. 2019;19 28. Jacob S, Muppidi S, Guidon A, et al. Guidance for the management
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
(2):169–176. doi:10.7861/clinmedicine.19-2-169 of myasthenia gravis (MG) and Lambert-Eaton myasthenic syndrome
10. Channappanavar R, Perlman S. Pathogenic human coronavirus infec (LEMS) during the COVID-19 pandemic. J Neurol Sci. 2020;412.
tions: causes and consequences of cytokine storm and 29. Magraner MJ, Coret F, Casanova B. The effect of intravenous immu
immunopathology. Seminars in Immunopathology. 2017;39 noglobulin on neuromyelitis optica. Neurología. 2013;28(2):65–72.
(5):529–539. doi:10.1007/s00281-017-0629-x doi:10.1016/j.nrleng.2012.03.014
11. Cao W, Li T. COVID-19: towards understanding of pathogenesis. 30. Bakker J, Metz L. Devic’s neuromyelitis optica treated with intrave
Cell Res. 2020;30(5):367–369. doi:10.1038/s41422-020-0327-4 nous gamma globulin (IVIG). Canadian J Neurol Sci. 2004;31
12. Sormani MP. An Italian programme for COVID-19 infection in (2):265–267. doi:10.1017/S0317167100053932
multiple sclerosis. Lancet Neurol. 2020;19(6):481–482. doi:10.1016/ 31. Okada K, Tsuji S, Tanaka K. Intermittent intravenous immunoglobu
S1474-4422(20)30147-2 lin successfully prevents relapses of neuromyelitis optica. Int Med.
13. Brownlee W, Bourdette D, Broadley S, Killestein J, Ciccarelli O. 2007;46(19):1671–1672. doi:10.2169/internalmedicine.46.0217
Treating multiple sclerosis and neuromyelitis optica spectrum disor 32. Wang Y, Jiang W, He Q, et al. A retrospective cohort study of
der during the COVID-19 pandemic. Neurology. 2020;94 methylprednisolone therapy in severe patients with COVID-19
(22):949–952. doi:10.1212/WNL.0000000000009507 pneumonia. Signal Transduct Targeted Ther. 2020;5(1):57. doi:10.10
14. Elsone L, Kitley J, Luppe S, et al. Long-term efficacy, tolerability 38/s41392-020-0158-2
and retention rate of azathioprine in 103 aquaporin-4 33. Cao W, Liu X, Bai T, et al. High-dose intravenous immunoglobulin
antibody-positive neuromyelitis optica spectrum disorder patients: as a therapeutic option for deteriorating patients with Coronavirus
For personal use only.
a multicentre retrospective observational study from the UK. Disease 2019. Paper presented at: Open forum infectious diseases
Multiple Sclerosis J. 2014;20(11):1533–1540. doi:10.1177/1352 2020.
458514525870 34. Xie Y, Cao S, Dong H, et al. Effect of regular intravenous immuno
15. Mealy MA, Wingerchuk DM, Palace J, Greenberg BM, Levy M. globulin therapy on prognosis of severe pneumonia in patients with
Comparison of relapse and treatment failure rates among patients COVID-19. J Infect. 2020;S0163–S4453(0120):30172–30179.
with neuromyelitis optica: multicenter study of treatment efficacy. 35. Altunrende B, Akdal G, Bajin MS, et al. Intravenous immunoglobu
JAMA Neurol. 2014;71(3):324–330. doi:10.1001/jamaneurol.2013. lin treatment for recurrent optic neuritis. Arch Neuropsych. 2019;56
5699 (1):3.
16. Wingerchuk DM, Lennon VA, Lucchinetti CF, Pittock SJ, 36. Borisow N, Mori M, Kuwabara S, Scheel M, Paul F. Diagnosis and
Weinshenker BG. The spectrum of neuromyelitis optica. Lancet treatment of NMO spectrum disorder and MOG-encephalomyelitis.
Neurol. 2007;6(9):805–815. doi:10.1016/S1474-4422(07)70216-8 Front Neurol. 2018;9:888. doi:10.3389/fneur.2018.00888
17. Sherman E, Han MH. Acute and chronic management of neuromye 37. Huang W, Wang L, Zhang B, Zhou L, Zhang T, Quan C. Effectiveness
litis optica spectrum disorder. Curr Treat Options Neurol. 2015;17 and tolerability of immunosuppressants and monoclonal antibodies in
(11):48. doi:10.1007/s11940-015-0378-x preventive treatment of neuromyelitis optica spectrum disorders:
18. Kowarik MC, Soltys J, Bennett JL. The treatment of neuromyelitis A systematic review and network meta-analysis. Mult Scler Relat
optica. J Neuro Ophthalmol. 2014;34(1):70. doi:10.1097/WNO. Disord. 2019;35:246–252. doi:10.1016/j.msard.2019.08.009
0000000000000102 38. Araki M, Matsuoka T, Miyamoto K, et al. Efficacy of the anti–IL-6
19. Freedman MS, Selchen D, Arnold DL, et al. Treatment optimization receptor antibody tocilizumab in neuromyelitis optica: a pilot study.
in MS: canadian MS Working Group updated recommendations. Neurology. 2014;82(15):1302–1306. doi:10.1212/WNL.0000000000
Canadian J Neurol Sci. 2013;40(3):307–323. doi:10.1017/S0317 000317
167100014244 39. Huang Q, Wang J, Zhou Y, et al. Low-dose mycophenolate mofetil
20. Bonnan M, Valentino R, Olindo S, Mehdaoui H, Smadja D, Cabre P. for treatment of neuromyelitis optica spectrum disorders:
Plasma exchange in severe spinal attacks associated with neuromye a prospective multicenter study in South China. Front Immunol.
litis optica spectrum disorder. Multiple Sclerosis J. 2009;15 2018;9:2066. doi:10.3389/fimmu.2018.02066
(4):487–492. doi:10.1177/1352458508100837 40. Kim S-H, Huh S-Y, Lee SJ, Joung A, Kim HJ. A 5-year follow-up of
21. Bonnan M, Cabre P. Plasma exchange in severe attacks of neuro rituximab treatment in patients with neuromyelitis optica spectrum
myelitis optica. Mult Scler Int. 2012;2012. disorder. JAMA Neurol. 2013;70(9):1110–1117. doi:10.1001/
22. Keegan M, Pineda AA, McClelland RL, Darby CH, Rodriguez M, jamaneurol.2013.3071
Weinshenker BG. Plasma exchange for severe attacks of CNS 41. Li X, Mei S, Gong X, et al. Relationship between Azathioprine
demyelination: predictors of response. Neurology. 2002;58 metabolites and therapeutic efficacy in Chinese patients with neuro
(1):143–146. doi:10.1212/WNL.58.1.143 myelitis optica spectrum disorders. BMC Neurol. 2017;17(1):130.
23. Baharnoori M, Hohol M, Pavenski K, O’Connor P. Therapeutic doi:10.1186/s12883-017-0903-5
Effect of Plasma Exchange (PLEX) in Neuromyelitis Optica 42. Xu Y, Wang Q, Ren H-T, et al. Comparison of efficacy and toler
(NMO): immediate and Long Term Response (S63. 005). AAN ability of azathioprine, mycophenolate mofetil, and cyclophospha
Enterprises. 2014. mide among patients with neuromyelitis optica spectrum disorder:
24. Kleiter I, Gahlen A, Borisow N, et al. Neuromyelitis optica: evalua a prospective cohort study. J Neurol Sci. 2016;370:224–228.
tion of 871 attacks and 1153 treatment courses. Ann Neurol. 2016;79 doi:10.1016/j.jns.2016.09.035
(2):206–216. doi:10.1002/ana.24554 43. Tiede I, Fritz G, Strand S, et al. CD28-dependent Rac1 activation is
25. Chang JC. Sepsis and septic shock: endothelial molecular pathogen the molecular target of azathioprine in primary human CD4+ T
esis associated with vascular microthrombotic disease. Thromb J. lymphocytes. J Clin Invest. 2003;111(8):1133–1145. doi:10.1172/
2019;17(1):10. doi:10.1186/s12959-019-0198-4 JCI16432
submit your manuscript | www.dovepress.com
Therapeutics and Clinical Risk Management 2020:16 765
DovePress
Powered by TCPDF (www.tcpdf.org)
Hamdy et al Dovepress
44. Konidari A, El Matary W. Use of thiopurines in inflammatory bowel 62. Kitley J, Elsone L, George J, et al. Methotrexate is an alternative to
disease: safety issues. World J Gastrointest Pharmacol Ther. 2014;5 azathioprine in neuromyelitis optica spectrum disorders with
(2):63. doi:10.4292/wjgpt.v5.i2.63 aquaporin-4 antibodies. J Neurol Neurosurg Psychiatry. 2013;84
45. Rademaker M, Baker C, Foley P, Sullivan J, Wang C. Advice regard (8):918–921. doi:10.1136/jnnp-2012-304774
ing COVID-19 and use of immunomodulators, in patients with severe 63. Ibrahim A, Ahmed M, Conway R, Carey JJ. Risk of Infection with
dermatological diseases. Australasian J Dermatol. 2020;61 Methotrexate Therapy in Inflammatory Diseases: A Systematic
(2):158–159. doi:10.1111/ajd.13295 Review and Meta-Analysis. J Clin Med. 2019;8(1):15. doi:10.3390/
46. Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis jcm8010015
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
Campaign: guidelines on the management of critically ill adults 64. Zisman D, McCune W, Tino G. Drug-induced pneumonitis: the role
with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. of methotrexate. Sarcoidosis Vasculitis Diffuse Lung Dis. 2001;18
2020;1–34. (3):243–252.
47. Gao F, Chai B, Gu C, et al. Effectiveness of rituximab in neuromye 65. Colvin O. An overview of cyclophosphamide development and clin
litis optica: a meta-analysis. BMC Neurol. 2019;19(1):36. ical applications. Curr Pharm Des. 1999;5:555–560.
doi:10.1186/s12883-019-1261-2 66. Ahlmann M, Hempel G. The effect of cyclophosphamide on the
48. Amor S, Baker D, Khoury SJ, Schmierer K, Giovanonni G. SARS-CoV immune system: implications for clinical cancer therapy. Cancer
-2 and Multiple Sclerosis: not All Immune Depleting DMTs are Equal or Chemother Pharmacol. 2016;78(4):661–671. doi:10.1007/s00280-
Bad. Ann Neurol. 2020;87(6):794–797. doi:10.1002/ana.25770 016-3152-1
49. Kimby E. Tolerability and safety of rituximab (MabThera®). Cancer 67. Poonsombudlert K, Kewcharoen J, Prueksapraopong C,
Treat Rev. 2005;31(6):456–473. doi:10.1016/j.ctrv.2005.05.007 Limpruttidham N. Post transplant cyclophosphamide based
50. Juto A, Fink K, Al Nimer F, Piehl F. Interrupting rituximab treatment haplo-identical transplant versus umbilical cord blood transplant; a
in relapsing-remitting multiple sclerosis; no evidence of rebound meta-analysis. Jpn J Clin Oncol. 2019;49(10):924–931. doi:10.1093/
disease activity. Mult Scler Relat Disord. 2020;37:101468. jjco/hyz099
doi:10.1016/j.msard.2019.101468 68. Atilla E, Ates C, Uslu A, et al. Prospective Analysis of Hemorrhagic
51. Lebrun C, Cohen M, Rosenthal-Allieri MA, et al. Only follow-up of Cystitis and BK Viremia in Allogeneic Hematopoietic Stem Cell
memory B cells helps monitor rituximab administration to patients Transplantation. Turkish j Haematol. 2019. doi:10.4274/tjh.
For personal use only.
with neuromyelitis optica spectrum disorders. Neurol Ther. 2018;7 galenos.2019.2019.0296
(2):373–383. doi:10.1007/s40120-018-0101-4 69. Silva T. Immunossupression murine model to study antiviral resis
52. Lamba V, Sangkuhl K, Sanghavi K, Fish A, Altman RB, Klein TE. tance emergence during Influenza A infection. 2019.
PharmGKB summary: mycophenolic acid pathway. Pharmacogenet 70. Frampton JE. Eculizumab: A Review in Neuromyelitis Optica
Genomics. 2014;24(1):73. doi:10.1097/FPC.0000000000000010 Spectrum Disorder. Drugs. 2020;80(7):719–727. doi:10.1007/
53. Ritter M, Pirofski L-A. Mycophenolate mofetil: effects on cellular s40265-020-01297-w
immune subsets, infectious complications, and antimicrobial activity. 71. Jiang Y, Zhao G, Song N, et al. Blockade of the C5a–C5aR axis
Transplant Infect Dis. 2009;11(4):290–297. doi:10.1111/j.1399- alleviates lung damage in hDPP4-transgenic mice infected with
3062.2009.00407.x MERS-CoV. Em Microb Infect. 2018;7(1):1–12.
54. Eugui E, Mirkovich A, Allison A. Lymphocyte-selective antiproli 72. Diurno F, Numis FG, Porta G, et al. Eculizumab treatment in patients
ferative and immunosuppressive effects of mycophenolic acid in with COVID-19: preliminary results from real life ASL Napoli 2
mice. Scand J Immunol. 1991;33(2):175–183. doi:10.1111/j.1365- Nord experience. Eur Rev Med Pharmacol Sci. 2020;24
3083.1991.tb03747.x (7):4040–4047.
55. Song ATW, Abdala E, Bonazzi PR, Bacchella T, Machado MCC. 73. Wingerchuk D, Pittock S, Berthele A, et al. Long-term safety and
Does mycophenolate mofetil increase the risk of cytomegalovirus effectiveness of eculizumab in neuromyelitis optica spectrum
infection in solid organ transplant recipients?: A mini-review. Br disorder. Paper presented at: MULTIPLE SCLEROSIS JOURNAL
J Infect Dis. 2006;10(2):132–138. 2019.
56. Karnell JL, Karnell FG, Stephens GL, et al. Mycophenolic acid 74. Araki M. Blockade of IL-6 signaling in neuromyelitis optica.
differentially impacts B cell function depending on the stage of Neurochem Int. 2019;130:104315. doi:10.1016/j.neuint.2018.10.012
differentiation. J Immunol. 2011;187(7):3603–3612. doi:10.4049/ 75. Zhang C, Wu Z, Li J-W, Zhao H, Wang G-Q. The cytokine release
jimmunol.1003319 syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor
57. Nosadini M, Gadian J, Lim M, Sartori S, Thomas T, Dale RC. (IL-6R) antagonist Tocilizumab may be the key to reduce the
Mycophenolate mofetil in paediatric autoimmune or immune- mortality. Int J Antimicrob Agents. 2020;55(5):105954. doi:10.1016/
mediated diseases of the central nervous system: clinical experience j.ijantimicag.2020.105954
and recommendations. Dev Med Child Neurol. 2019;61(4):458–468. 76. Francesco P, Perrone M.Tocilizumab in COVID-19 Pneumonia
doi:10.1111/dmcn.14020 (TOCIVID-19) (TOCIVID-19). 2020https://clinicaltrials.gov/ct2/
58. Jacob A, Matiello M, Weinshenker BG, et al. Treatment of neuro show/NCT04317092. Accessed August 6, 2020.
myelitis optica with mycophenolate mofetil: retrospective analysis of 77. Xu X, Han M, Li T, et al. Effective treatment of severe COVID-19
24 patients. Arch Neurol. 2009;66(9):1128–1133. doi:10.1001/ patients with tocilizumab. Proc Natl Acad Sci U S A. 2020;117
archneurol.2009.175 (20):10970–10975. doi:10.1073/pnas.2005615117
59. Abadja F, Atemkeng S, Alamartine E, Berthoux F, Mariat C. Impact 78. Lallana JM, Clares RH, Guarnizo EC, et al. Efficacy and Safety of
of mycophenolic acid and tacrolimus on Th17-related immune Tocilizumab as Second Line Therapy in Neuromyelitis Optica
response. Transplantation. 2011;92(4):396–403. doi:10.1097/ Unresponsive to Rituximab (P5. 262). AAN Enterprises. 2015.
TP.0b013e3182247b5f 79. Ayzenberg I, Faissner S, Tomaske L, Richter D, Behrendt V, Gold R.
60. Antonio R, Silvia M. Immunosuppression drug-related and clinical General principles and escalation options of immunotherapy in
manifestation of Coronavirus disease 2019: a therapeutical hypoth autoantibody-associated disorders of the CNS. Neurol Res Pract.
esis. Am J Transplant. 2020;1. 2019;1(1):32. doi:10.1186/s42466-019-0037-x
61. Malaviya AN, Sharma A, Agarwal D, Kapoor S, Garg S, Sawhney S. 80. Yamamura T, Kleiter I, Fujihara K, et al. Trial of satralizumab in
Low-dose and high-dose methotrexate are two different drugs in neuromyelitis optica Spectrum disorder. N Eng J Med. 2019;381
practical terms. Int J Rheum Dis. 2010;13(4):288–293. doi:10.1111/ (22):2114–2124. doi:10.1056/NEJMoa1901747
j.1756-185X.2010.01564.x
766 submit your manuscript | www.dovepress.com Therapeutics and Clinical Risk Management 2020:16
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hamdy et al
Therapeutics and Clinical Risk Management downloaded from https://www.dovepress.com/ by 83.142.55.49 on 06-Sep-2020
For personal use only.
Therapeutics and Clinical Risk Management Dovepress
Publish your work in this journal
Therapeutics and Clinical Risk Management is an international, peer- EMBase, Scopus and the Elsevier Bibliographic databases. The
reviewed journal of clinical therapeutics and risk management, focusing manuscript management system is completely online and includes
on concise rapid reporting of clinical studies in all therapeutic areas, a very quick and fair peer-review system, which is all easy to use.
outcomes, safety, and programs for the effective, safe, and sustained Visit http://www.dovepress.com/testimonials.php to read real quotes
use of medicines. This journal is indexed on PubMed Central, CAS, from published authors.
Submit your manuscript here: https://www.dovepress.com/therapeutics-and-clinical-risk-management-journal
submit your manuscript | www.dovepress.com
Therapeutics and Clinical Risk Management 2020:16 767
DovePress
Powered by TCPDF (www.tcpdf.org)
You might also like
- Procure To PayDocument2 pagesProcure To PaySanjeewa PrasadNo ratings yet
- BPW Axle Spare PartsDocument24 pagesBPW Axle Spare PartsSanhory Abd AlgaderNo ratings yet
- Clinical Efficiency of Nigella Sativa Linn in Novel Covid 19 A ReviewDocument6 pagesClinical Efficiency of Nigella Sativa Linn in Novel Covid 19 A ReviewDr Ayesha FatemahNo ratings yet
- Nontuberculous Mycobacteria Lung Disease (NTM-LD) Current Recommendations On Diagnosis, Treatment, and Patient ManagementDocument11 pagesNontuberculous Mycobacteria Lung Disease (NTM-LD) Current Recommendations On Diagnosis, Treatment, and Patient Managementalfred1294No ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- New Cfo ListDocument9 pagesNew Cfo Listmahesh malveNo ratings yet
- SMEDA Fast Food RestaurantDocument30 pagesSMEDA Fast Food Restaurantengagedsword100% (9)
- Shi NAC Review 2020-1Document9 pagesShi NAC Review 2020-1M PNo ratings yet
- Effects of Vitamin D On COVID-19 Infection and Prognosis: A Systematic ReviewDocument9 pagesEffects of Vitamin D On COVID-19 Infection and Prognosis: A Systematic ReviewA A Christina AquerilaNo ratings yet
- Bioengineering 09 00072Document16 pagesBioengineering 09 00072Anania ClementNo ratings yet
- Drug Treatment of Neuromyelitis Optica Spectrum Disorders: Out With The Old, in With The New?Document15 pagesDrug Treatment of Neuromyelitis Optica Spectrum Disorders: Out With The Old, in With The New?audreyNo ratings yet
- 2019-Emerging Treatment Options For The Management of Pemphigus VulgarisDocument22 pages2019-Emerging Treatment Options For The Management of Pemphigus VulgarisSherlyNo ratings yet
- Role of Targeted Therapies in RheumaticDocument13 pagesRole of Targeted Therapies in RheumaticJesús Tomás Sánchez CostaNo ratings yet
- TRT2017 4920209Document12 pagesTRT2017 4920209ADVOCATE ASHUTOSH SHARMANo ratings yet
- BNM CovidDocument8 pagesBNM CovidAlonso Marcelo Herrera VarasNo ratings yet
- Mask or No MaskDocument17 pagesMask or No MaskPascha ParamurthiNo ratings yet
- Thyroid Eye Disease How A Novel Therapy May Change The TreaDocument14 pagesThyroid Eye Disease How A Novel Therapy May Change The Treatrent boneNo ratings yet
- Artículo - Resumen de Las Principales Vacunas Anti-SARS-CoV-2Document18 pagesArtículo - Resumen de Las Principales Vacunas Anti-SARS-CoV-2Jeancarlo Alarcon CustodioNo ratings yet
- Current Perspectives On The Systemic Management of Atopic DermatitisDocument13 pagesCurrent Perspectives On The Systemic Management of Atopic DermatitisMiftach KhoirunnisaNo ratings yet
- Viruses: Amantadine Inhibits Sars-Cov-2 in VitroDocument10 pagesViruses: Amantadine Inhibits Sars-Cov-2 in VitroTiberiu ScanteieNo ratings yet
- Update On Safety Profiles of Vitamins B1, B6, and B12: A Narrative ReviewDocument14 pagesUpdate On Safety Profiles of Vitamins B1, B6, and B12: A Narrative ReviewOktavinda Ayu Kusumawardani farmasiNo ratings yet
- Main 9Document11 pagesMain 9Eltohn JohnNo ratings yet
- JurnalDocument4 pagesJurnalAnonymous pfHZusnNo ratings yet
- Pandemic Prevention: Lessons From COVID-19: Mario CocciaDocument12 pagesPandemic Prevention: Lessons From COVID-19: Mario CocciaChieyanshaNo ratings yet
- Jurnal 4Document5 pagesJurnal 4Andi WarlyNo ratings yet
- Prevalence and Determinants of Multidrug-Resistant Tuberculosis in Makkah, Saudi ArabiaDocument8 pagesPrevalence and Determinants of Multidrug-Resistant Tuberculosis in Makkah, Saudi Arabia0fadiiii19900No ratings yet
- Assessment and Management of Diabetic Patients DurDocument16 pagesAssessment and Management of Diabetic Patients DurDivya RasoiNo ratings yet
- Novel Therapeutic Approaches To Invasive CandidiasisDocument12 pagesNovel Therapeutic Approaches To Invasive Candidiasisstephanie bojorquezNo ratings yet
- Consideration of Severe Coronavirus Disease 2019.12Document5 pagesConsideration of Severe Coronavirus Disease 2019.12yovanNo ratings yet
- Soluciones de VIDocument2 pagesSoluciones de VILailaNo ratings yet
- Akk Jurnal Internasional 1Document7 pagesAkk Jurnal Internasional 1Onnii SltrNo ratings yet
- TABULATION of ILRDocument5 pagesTABULATION of ILRChit RamirezNo ratings yet
- JIR 307333 Fat Soluble Vitamins and The Current Global Pandemic of CoviDocument20 pagesJIR 307333 Fat Soluble Vitamins and The Current Global Pandemic of CoviSeptian TheaNo ratings yet
- Treatment of Hospital-Acquired and Ventilator-Associated Pneumonia in Adults - UpToDateDocument58 pagesTreatment of Hospital-Acquired and Ventilator-Associated Pneumonia in Adults - UpToDateduong tien truongNo ratings yet
- Clinmed 2020-0351 FullDocument4 pagesClinmed 2020-0351 FullIsro AlhaqiNo ratings yet
- Ef Ficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-AnalysisDocument11 pagesEf Ficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-AnalysisCRS1973No ratings yet
- Antibiotics 10 01278Document11 pagesAntibiotics 10 01278BaronKornNo ratings yet
- Potencial Uso de Ivermectina en Tratamiento y Profilaxis de Covid19Document18 pagesPotencial Uso de Ivermectina en Tratamiento y Profilaxis de Covid19Andrimar Del Carmen Torres MuñozNo ratings yet
- Aman 2Document13 pagesAman 2Amardeep YadavNo ratings yet
- Minimal Residual Disease in Multiple Myeloma - An Important Tool in Clinical TrialsDocument2 pagesMinimal Residual Disease in Multiple Myeloma - An Important Tool in Clinical TrialsSeungman ParkNo ratings yet
- European J of Heart Fail 2022 Dom Nguez Rodr GuezDocument10 pagesEuropean J of Heart Fail 2022 Dom Nguez Rodr GuezErnesto TrindadeNo ratings yet
- COVID-19 Treatment Guidelines: Do They Really Reflect Best Medical Practices To Manage The Pandemic?Document26 pagesCOVID-19 Treatment Guidelines: Do They Really Reflect Best Medical Practices To Manage The Pandemic?Mostafa SalahNo ratings yet
- Komorbid Autoimun DR Dwi BudiDocument36 pagesKomorbid Autoimun DR Dwi BudiLiliyanhNo ratings yet
- Authors' Reply To The Comment “ Treatment CoDocument2 pagesAuthors' Reply To The Comment “ Treatment Conadya aliviaNo ratings yet
- Lecture MDR TBDocument3 pagesLecture MDR TBRoy Anthony CenizaNo ratings yet
- Mesotrerapia Protocolo Seguro y Manejo de ComplicacionesDocument5 pagesMesotrerapia Protocolo Seguro y Manejo de ComplicacionesOrlando GaduNo ratings yet
- Onabotulinumtoxina For Chronic Migraine: A Critical AppraisalDocument11 pagesOnabotulinumtoxina For Chronic Migraine: A Critical AppraisalAlexandra ConstantinescuNo ratings yet
- Prevention and Treatment of Postoperative Nausea and Vomiting (PONV) : A Review of Current Recommendations and Emerging TherapiesDocument13 pagesPrevention and Treatment of Postoperative Nausea and Vomiting (PONV) : A Review of Current Recommendations and Emerging TherapiesMARCOS HUACONo ratings yet
- Molnupiravir para COVID-19Document12 pagesMolnupiravir para COVID-19joelNo ratings yet
- NeumoníaDocument19 pagesNeumoníadery sernaNo ratings yet
- Ferraresi Isidoro COVID19 Vaccinomics Adversomics Biomedicines 26Document11 pagesFerraresi Isidoro COVID19 Vaccinomics Adversomics Biomedicines 26ioannesturrisoricisNo ratings yet
- 10 2147@cpaa S269156 PDFDocument7 pages10 2147@cpaa S269156 PDFMarco Antonio Tarazona MoyaNo ratings yet
- Cells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Document29 pagesCells: Thymoquinone: A Tie-Breaker in Sars-Cov2-Infected Cancer Patients?Yoni LinggaNo ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicineRudy SanabriaNo ratings yet
- Possible Treatment and Strategies For COVID-19: Review and AssessmentDocument16 pagesPossible Treatment and Strategies For COVID-19: Review and AssessmentAni RahayuNo ratings yet
- Psychological Distress Amongst Health Workers and The General Public During The COVID-19 Pandemic in Saudi Arabia (Kuesioner CPDI)Document10 pagesPsychological Distress Amongst Health Workers and The General Public During The COVID-19 Pandemic in Saudi Arabia (Kuesioner CPDI)Febri YolandaNo ratings yet
- Severe Covid-19 Pneumonia - Pathogenesis and Clinical ManagementDocument19 pagesSevere Covid-19 Pneumonia - Pathogenesis and Clinical ManagementRodrigoNo ratings yet
- The Management of Glioblastomas During The Sars-Cov-19 Pandemic: A Narrative OverviewDocument4 pagesThe Management of Glioblastomas During The Sars-Cov-19 Pandemic: A Narrative OverviewAdil LagmarNo ratings yet
- Severe Covid 19 Pneumonia Pathogenesis and ManagementDocument19 pagesSevere Covid 19 Pneumonia Pathogenesis and ManagementRey CaesarNo ratings yet
- Glycopeptides As Potential Interventions For Covid-19Document8 pagesGlycopeptides As Potential Interventions For Covid-19adane yehualawNo ratings yet
- Editorials: Covid-19: Should The Public Wear Face Masks?Document2 pagesEditorials: Covid-19: Should The Public Wear Face Masks?steven saputraNo ratings yet
- The Global Prevalence of Anxiety DepressDocument19 pagesThe Global Prevalence of Anxiety DepresswalkensiocsNo ratings yet
- Perspectives On Monoclonal Antibody Therapy As Potential Therapeutic Intervention For Coronavirus Disease-19 (COVID-19)Document9 pagesPerspectives On Monoclonal Antibody Therapy As Potential Therapeutic Intervention For Coronavirus Disease-19 (COVID-19)Juan Gonzalez RoblesNo ratings yet
- 1 s2.0 S1319016420302681 MainDocument20 pages1 s2.0 S1319016420302681 Mainazanne okta verzonaNo ratings yet
- COVID-19 and Multiple Sclerosis: Predisposition and Precautions in TreatmentDocument6 pagesCOVID-19 and Multiple Sclerosis: Predisposition and Precautions in TreatmentAdriana BahnaNo ratings yet
- An Intergenerational Approach To Break The Cycle of MalnutritionDocument9 pagesAn Intergenerational Approach To Break The Cycle of MalnutritionAdriana BahnaNo ratings yet
- Experience in Multiple Sclerosis Patients With COVID-19 and Disease-Modifying Therapies: A Review of 873 Published CasesDocument12 pagesExperience in Multiple Sclerosis Patients With COVID-19 and Disease-Modifying Therapies: A Review of 873 Published CasesAdriana BahnaNo ratings yet
- Are Patients With Multiple Sclerosis (MS) at Higher Risk of COVID-19 Infection?Document2 pagesAre Patients With Multiple Sclerosis (MS) at Higher Risk of COVID-19 Infection?Adriana BahnaNo ratings yet
- Feeding of LBWDocument45 pagesFeeding of LBWAdriana BahnaNo ratings yet
- Pediatric NeurologyDocument13 pagesPediatric NeurologyAdriana BahnaNo ratings yet
- CXC Jan 2000 p2Document7 pagesCXC Jan 2000 p2omar_oj_40% (1)
- 2023 - Tute 7 - Risk, Return, CAPMDocument4 pages2023 - Tute 7 - Risk, Return, CAPMThảo TrươngNo ratings yet
- SPE-70129-PA OnepetroDocument7 pagesSPE-70129-PA OnepetroAlex ZamanNo ratings yet
- Examination Papers On Introductory GeotechnicsDocument53 pagesExamination Papers On Introductory GeotechnicsTakchandra JaikeshanNo ratings yet
- iBOXIFY Packaging ProfileDocument16 pagesiBOXIFY Packaging ProfileGanesh BadheNo ratings yet
- Chempak BrochureDocument2 pagesChempak BrochurehcabanillaspNo ratings yet
- Inner Cover For Langstroth Hive: Ed RiceDocument4 pagesInner Cover For Langstroth Hive: Ed RiceFernandes HélioNo ratings yet
- Ultrasound - Versana Active BrochureDocument5 pagesUltrasound - Versana Active BrochureAriNo ratings yet
- Marbett English08 PDFDocument344 pagesMarbett English08 PDFNguyenHuanNo ratings yet
- Sist Din 19643 1 2003Document11 pagesSist Din 19643 1 2003hidroprojektemiNo ratings yet
- Fargo DTC550 Service Manual PDFDocument614 pagesFargo DTC550 Service Manual PDFnelutuanv-1No ratings yet
- Professional SummaryDocument3 pagesProfessional SummaryAbrar UL Haq SyedNo ratings yet
- Kredx Documentation List UpdatedDocument4 pagesKredx Documentation List UpdatedSwapnil CallaNo ratings yet
- Annexure B.2Document1 pageAnnexure B.2Mayapur Communication100% (1)
- Drug Alert List of Oct - 2022Document11 pagesDrug Alert List of Oct - 2022Gopal RaoNo ratings yet
- Proc ListDocument9 pagesProc ListIvan CastillaNo ratings yet
- Chpt.1 Overview Process'' PDFDocument62 pagesChpt.1 Overview Process'' PDFLija BinuNo ratings yet
- Strategic Management AssignmentDocument3 pagesStrategic Management Assignmenthzgl250% (1)
- BUS357 Starting and Managing A Business 30 Oct 2023 1698374280573Document12 pagesBUS357 Starting and Managing A Business 30 Oct 2023 1698374280573AtaNu MonDalNo ratings yet
- Project ExperiencesDocument14 pagesProject Experiencessmart_onyx17No ratings yet
- WW C70 Product-Page English 12-2015 1Document5 pagesWW C70 Product-Page English 12-2015 1rafaelcoserNo ratings yet
- OpenstackDocument68 pagesOpenstackick semarangNo ratings yet
- Group 1: Abordo, Jezzle Anne Boreros, Christall Jane Gumobao, Winzelle Morales, Jane Erica Sibala, Rayshell KateDocument14 pagesGroup 1: Abordo, Jezzle Anne Boreros, Christall Jane Gumobao, Winzelle Morales, Jane Erica Sibala, Rayshell KateRudy LugasNo ratings yet
- Pid 2 BombaDocument1 pagePid 2 BombaIvan JulonNo ratings yet
- Crisostomo v. Court of Appeals, 409 SCRA 528 (2003)Document8 pagesCrisostomo v. Court of Appeals, 409 SCRA 528 (2003)Tris LeeNo ratings yet
- NB: Use Only Blue Ink Pen For Preparing Assignment and Case AnalysisDocument9 pagesNB: Use Only Blue Ink Pen For Preparing Assignment and Case AnalysiszodNo ratings yet