Professional Documents
Culture Documents
Parkinson
Uploaded by
AlmaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Parkinson
Uploaded by
AlmaCopyright:
Available Formats
Biomedical Research 2017; 28 (1): ISSN 0970-938X
www.biomedres.info
The effects of a pulmonary rehabilitation program on exercise tolerance,
quality of life, sleep quality and emotional status in the patients with
Parkinson's disease.
Belma Güngen1*, Yusuf Aydemir2, Yeşim Aras1, Adil Güngen2, Dilcan Kotan1, Serdar Bal3
1Department of Neurology, Sakarya University, Research and Training Hospital, Sakarya, Turkey
2Department of Pulmonology, Sakarya University, Research and Training Hospital, Sakarya, Turkey
3Department of Physical Medicine and Rehabilitation, Sakarya University, Research and Training Hospital, Sakarya,
Turkey
Abstract
Introduction: We aimed in the present study to investigate the effects of pulmonary rehabilitation on the
respiratory parameters and effort capacity, quality of life (QoL), anxiety, depression, and sleepiness in
the patients with Parkinson's disease (PD).
Methods: The study included 34 mobilized patients with PD. Patients underwent a 12-week pulmonary
physiotherapy (PPT). Pulmonary function tests (PFT), six-minute walk test (6mWT), Hoehn and Yahr
Scale (HYS), Unified Parkinson's Disease Rating Scale (UPDRS), QoL, Parkinson's Disease
Questionnaire (PDQ), Beck Anxiety Inventory (BAI), Beck Depression Inventory (BDI), and Epworth
Sleepiness Scale (ESS) scores were evaluated before and after PPT.
Results: PPT improved parameters of PFT significantly, and caused an increase of about 35 m in the
6mWT (p<0.001). HYS (p=0.002), UPDRS, QoL, PDQ, BAI, BDI and ESS scores were found to improve
significantly after the PPT (p<0.001 for all).
Conclusion: Results of our study indicated that PPT is effective significantly and positively especially on
the non-motor complications, by increasing effort capacity and walking distance in the patients with PD.
Keywords: Parkinson's disease, Pulmonary rehabilitation, Anxiety, Depression, Sleepiness, Quality of life.
Accepted on June 27, 2016
Introduction peripheral and central mechanisms. Motor manifestations such
as rigidity, tremor and weakness affect the upper airway and
Parkinson’s disease (PD) is a chronic and progressive the respiratory pump muscles. Non-motor brain stem
neurodegenerative condition, affecting approximately 10 involvement has effect at the level of respiratory control [5]. In
million people worldwide [1]. People with PD have more addition to these ventilatory abnormalities, evidences of a high
motor and autonomic, cognitive, behavioural and sensorial incidence of obstructive and restrictive pulmonary dysfunction
complications. The motor complications include tremor, were found [6,7]. Exercise therapy poses the potential to
rigidity, bradykinesia, decreased pulmonary capacity and improve many clinical domains of PD [8]. Indeed studies on
deterioration of muscle strength, balance and walking PD have shown improvements of muscle strength, cardio
performance, while the non-motor complications include respiratory fitness, balance, walking performance, and QoL,
autonomic dysfunction, fatigue, apathy, sensory complaints, following exercise therapy [2]. In the previous studies, it has
sleep disturbances, depression, cognitive dysfunction and been reported that pulmonary rehabilitation improves the PFT
ultimately decreased quality of life (QoL) [2,3]. Because of parameters, and increases the scores of six-minute walk test
these physical insufficiencies, patients with PD maintain (6mWT) [9,10]; however, as far as we know, a study is not
sedentary lives, with less motor activity [4]. This life style available indicating the effects of pulmonary rehabilitation on
causes social isolation, and increased dependency to others, the emotional status and sleep quality.
leading to a vicious cycle that worsens the emotional disorder
and life quality. In our study, we aimed to investigate effects of the increased
effort capacity and mobilization by pulmonary physiotherapy
Another important reason of inactivity in PD patients is the (PPT), on the general and Parkinson-specific life qualities,
respiratory complication that leads to decreased effort capacity. emotional status, and sleep quality.
Respiratory involvement with PD could occur through both
Biomed Res- India 2017 Volume 28 Issue 1 1
Güngen/Aydemir/Aras/Güngen/Kotan/Bal
Materials and Methods Patients were administered 12-week exercise program by an
experienced pulmonary physiotherapist. During the exercise
From April 2014 to April 2015, 123 consecutive PD program, pursed lips pulmonary, and diaphragmatic pulmonary
outpatients were recruited at regular check-ups at the exercises were applied, after training. PFT, 6mWT, QoL,
Department of Neurology Clinic, Sakarya University Medical UPDRS, HYS, PDQ-39, SF-36, BAI, BDI, and ESS were
Faculty (Turkey). The diagnosis was made according to the evaluated before and after the exercises. Six of the patients
United Kingdom Parkinson's Disease Society Brain Bank were excluded from the study because of the alteration in
criteria. Participants were evaluated for disease severity using treatment dose during the follow-up period, three cases were
the Unified Parkinson’s Disease Rating Scale (UPDRS) [11] in excluded due to the inability in applying physiotherapy
the “on-state” and Hoehn and Yahr Scale (HYS) [12]. All program, and two cases were excluded because of not
patients were clinically stable (without fluctuations or attending to controls. The study was completed with the
dyskinesia). Accompanying malignancy, congestive heart participating 34 patients. Ethical approval for the study was
failure, insulin-dependent diabetes mellitus, inflammation, granted by the Sakarya University Ethics Committee. All
infection, neurological dysfunction, severe depression, patients were informed about the aim of the study, and written
dementia and other conditions that could influence the mobility consent was obtained.
status were excluded from the study. Pulmonary system was
evaluated in detail in all patients, by a specialist in chest Statistical analysis
diseases. All pulmonary function tests (PFT) were carried out
by the same technician in accordance with the directives of the Statistical analyses were carried out using the SPSS/PC
American Thoracic Society. software (version 21.0). Descriptive statistics were presented
as mean values with a standard deviation for numeric variables.
Patients with asthma-COPD and obstructive pulmonary disease The paired-samples t-test for comparison of parametric data
were not included in the study. Cases, who have previously among groups. The limit for statistical significance was
participated in an exercise program, and those receiving drugs accepted as p<0.05.
for anxiety, depression and sleep disturbances, were also
excluded. The remaining 45 patients with mental and cognitive
status suitable for physiotherapy (mini mental state
Results
examination ≥ 24), have undergone 6mWT according to the Of the original sample of 129 PD patients, 45 patients met the
standard protocol [13]. The level of quality of life was assessed inclusion criteria. An additional 11 patients were excluded
by means of the quality of life scale in Parkinson’s Disease because of missing data. This resulted in a total sample size of
Questionnaire (PDQ-39) [14]; it is a 39-item self-report 34 patients. The demographics and clinical features of patients
questionnaire which measures eight dimensions of health, are listed in Table 1.
namely mobility, activities of daily living, emotional well-
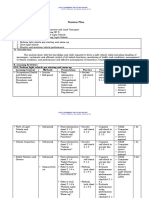
being, stigma, social support, cognition, communication, and Table1. Demographic and clinical characteristics of the subjects.
bodily discomfort. Higher score of PDQ-39 indicates poorer
QoL in PD patients. This scale evaluates the effect of Mean ± SD Min-max
Parkinson’s disease on the quality of life, within the last one Male/Female 21/13
month.
Age 68.21 ± 12.20 48-86
For evaluation of quality of life (QoL), Short Form-36 (SF-36)
Disease duration (yr) 5.8 ± 4.4 20-Mar
was used. The SF-36 Health Survey questionnaire was used to
measure health-related QoL [15]. It is composed of 36 items, Age of onset (yr) 62.94 ± 12.8 34-84
addressing eight dimensions of QoL: physical functioning,
UPDRS 31.7 ± 10.03 Oct-46
physical role limitations, bodily pain, general health, vitality,
social functioning, emotional role limitations and mental HYS 1.6 ± 0.4 (median: 2) 1-2.5
health. These scores range from 0 to 100, with higher scores UPDRS: Unified Parkinson’s Disease Rating Scale; HYS: Hoehn and Yahr
representing better health quality. For evaluation of emotional Stage.
status, Beck Anxiety Inventory (BAI) and Beck Depression
Inventory (BDI) were used [16,17]. The BAI and BDI are Spirometric parameters of the patients improved significantly
widely used, 21-item standardized self-administered following the PPT. The mean value of FEV1 increased from
questionnaires that measure various symptoms of anxiety- 77.6, to 86.3. Similarly, FVC also increased from 78.85 to
depression and describe the somatic and cognitive-affective 86.97. The walking distance increased significantly in the
symptoms on a four-point scale that ranges from 0 to 3. A 6mWT performed after physiotherapy, from the mean value of
higher score indicates a more severe depression. The sleep 233 m, to 269 m as shown in Figure 1.
quality was assessed by the Epworth Sleepiness Scale (ESS)
[18]. Epworth 0-10 was categorized as mild, and over 10 was
categorized as severe.
2 Biomed Res- India 2017 Volume 28 Issue 1
The effects of a pulmonary rehabilitation program on exercise tolerance, quality of life, sleep quality and emotional
status in the patients with Parkinson's disease
progressive disease may lead to anxiety and depression, and
debilitating and unpredictable motor symptoms may also
contribute to this [24]. However mood disorders in PD cannot
be solely explained by the psychological response to the
diagnosis of PD, since anxiety and depression are reported
more frequently in PD compared to patients with other
similarly chronic and debilitating diseases [23]. The
dopaminergic neurotransmitter alterations can be directly
related to anxiety symptoms in PD [23]. Furthermore studies
suggest possible associations with both serotonergic and
noradrenergic systems and white-matter abnormalities. On the
upshot it is largely attributed to a combination of
neurobiological and psychological causes [23]. Whatever the
cause may be, PPT was determined to affect anxiety and
depression significantly in our study, and rates of anxiety and
Figure 1. The effect of PPT on pulmonary functions, walk distance
depression decreased to 44.1% and 32.3%, respectively
and quality of life.
following PPT (p<0.001). We could not reach a study in the
The overall life quality and the anxiety-depression scores of literature evaluating the effect of PPT on psychological status.
patients improved significantly following PPT. Results are However in the previous studies, activities like exercising and
illustrated in Table 2. dancing were shown to decrease anxiety and depression
[25-27]. This fact can be explained by positive effect of the
Table 2. The effect of PPT on clinical characteristics, emotional status increased capability of activity, on the mood.
and sleep quality of subjects.
Insomnia and excessive daytime sleepiness (EDS) is an
Before PPT After PPT Difference p value
increasingly recognized problem in PD, and it causes clinically
significant problems and impairs the quality of life of patients
UPDRS 31.7 ± 10.03 25.6 ± 9.6 -6.35 <0.0001 [28,29]. EDS affects up to 50% of Parkinson’s disease patients
HYS 1.6 ± 0.4 1.6 ± 0.4 0 0.002 and is 15-fold more frequent in PD patients than in the age-
matched healthy subjects [30]. Epworth Sleepiness Scale has
PDQ-39 59.3 ± 39.5 52.4 ± 37.3 -6.912 <0.0001
been reported to be reasonably well to evaluate excessive
BAI 20.09 ± 12.2 16.91 ± 11.0 -3.176 <0.0001 daytime sleepiness in PD [31]. In our study, ESS score was
found to be 8.82 prior to PPT, and 41.1% of the patients were
BDI 18.74 ± 12.45 16.21 ± 12.33 -2.529 <0.0001
found to exist with EDS. Following PPT, the mean ESS score
ESS 8.82 ± 4.54 7.26 ± 4.22 -1.559 <0.0001 decreased to 7.26, and rate of EDS decreased to 20.5%; the
differences were found to be significant (p<0.0001). In a recent
BAI: Beck Anxiety Inventory; BDI: Beck Depression Inventory; ESS: Epworth
Sleepiness Scale; Data are shown as mean ± SD. general population-based study, exercise was shown to exert
positive effect on EDS [32]. However a study evaluating the
effect of PPT is not available yet. Besides physical activity,
Discussion PPT may help to decrease sleep disturbances also by
Likely, our study is the first to prospectively demonstrate decreasing anxiety, and by its positive effects on the respiratory
improved QoL, anxiety, depression, sleepiness, 6mWT, parameters. Quality of life has become an increasingly
spirometry and UPDRS in individuals with PD after important parameter in the evaluation of the efficacy of
participation in a Pulmonary rehabilitation program. Our interventions in patients suffering from Parkinson's disease.
results have confirmed the views that respiratory parameters of Multiple studies, using a variety of approaches and methods,
the patients would improve, their effort capacities would have shown a reduction of QoL in PD patients [33]. In our
increase resulting in decreases of dependency and social study, overall life quality and also Parkinson-specific life
isolation, which might improve quality of life in these cases, quality improved significantly after the PPT (p>0.001 and
and additionally anxiety-depression and sleepiness might p<0.0001, respectively).
decrease, following a PPT program. Anxiety and depression Systematic reviews have indicated non-motor symptoms
exists more frequently in the patients with PD, compared to the [including depression and anxiety] as major factors in
general population [19], and this affects life quality of the determining health-related quality of life, progression of
patients negatively [20]. In large serial studies, rates of anxiety disability, and home nursing in PD patients [34]. A significant
and depression have been reported to be 45%-51% and relationship between postural instability, gait dysfunction
35%-45%, respectively [19,21,22]. We determined signs of dominant symptoms and anxiety is also observed [24].
anxiety and depression in 64.7%, and 41.1% of the patients in Furthermore exercise was indicated to increase PDQ in the
our study, respectively. randomized studies [35], and thus increased walking distance
The mechanisms of mood disorders in the patients with PD and decreased anxiety may improve quality of life. UPDRS
have not been clarified yet [23]. Possessing a chronic and score decreased significantly following PPT in our study; this
Biomed Res- India 2017 Volume 28 Issue 1 3
Güngen/Aydemir/Aras/Güngen/Kotan/Bal
decrease may be explained by the decreases in anxiety and 2. Uhrbrand A, Stenager E, Pedersen MS, Dalgas U.
depression in these patients. Negative effect of anxiety on the Parkinsons disease and intensive exercise therapy-a
motor symptoms is well-known [24]. In the metaanalyses, systematic review and meta-analysis of randomized
exercise has been determined to decrease depression in the controlled trials. J Neurol Sci 2015; 353: 9-19.
patients with neurological disorders [36]. Moreover Klusevky 3. Zhang N, Liu W, Ye M, Cohen AD, Zhang Y. The
et al. have shown that treatment of depression in PD patients heterogeneity of non-motor symptoms of Parkinsons
by sertraline exerts positive effects on motor functions, and disease. Neurol Sci 2015; 36: 577-584.
improves UPDRS score compared to basal level [37]. Recent 4. Nimwegen M, Speelman AD, Hofman EJ. Physical
studies also demonstrated that exercise decreases UPDRS inactivity in Parkinsons disease. J Neurol 2011; 258:
scores [35]. 2214-2221.
Respiratory function parameters were shown to be impaired in 5. Seccombe LM, Giddings HL, Rogers PG. Abnormal
PD, compared to normal population [7,38]. However number ventilatory control in Parkinsons disease-further evidence
of studies investigating the effects of pulmonary rehabilitation for non-motor dysfunction. Respir Physiol Neurobiol 2011;
programs is considerably limited. Koseoglu et al. have reported 179: 300-344.
that some of the PFT parameters improve with PPT [9]. 6. Sabate M, Gonzalez I, Ruperez F, Rodríguez M.
Significantly different FEV1 and FVC values determined in Obstructive and restrictive pulmonary dysfunctions in
our study may contribute to the literature in this regard. In PD Parkinsons disease. J Neurol Sci 1996; 138: 114-119.
patients, the reduction in walking capacity is an important 7. Sathyaprabha TN, Kapavarapu PK, Pall PK, Thennarasu K,
factor that negatively affects the perception of QoL [39]. In the Raju TR. Pulmonary functions in Parkinsons disease.
study of Cagusi et al., in addition to improvements in the Indian J Chest Dis Allied Sci 2005; 47: 251-257.
scores of PDRS-III, BDI and PDQ, a significant increase in 8. Pelosin E, Faelli E, Lofrano F, Avanzino L, Marinelli L,
walking distance was observed with the tailored exercise Bove M, Ruggeri P, Abbruzzese G. Effects of treadmill
program [40]. In our study, walking distance increased about training on walking economy in Parkinsons disease: a pilot
35 m with PPT, and this difference was significant. This study. Neurol Sci 2009; 30: 499-504.
increase may be the main cause of all improvements in the 9. Koseoglu F, Inan L, Ozel S. The effects of a pulmonary
patients. There are several limitations to this study. The lack of rehabilitation program on pulmonary function tests and
a non-physiotherapy control group does not allow direct exercise tolerance in patients with Parkinsons disease.
comparison of PPT versus no PPT. Furthermore, we did not Funct Neurol 1997; 12: 319-325.
have a follow-up period to determine whether the effects of
10. Frazzitta G, Maestri R, Bertotti G. Intensive rehabilitation
PPT lasted over time.
treatment in early Parkinsons disease: a randomized pilot
Evidences from published trials and guidelines have suggested study with a 2-year follow-up. Neurorehabil Neural Repair
potential benefits of physiotherapy for patients with 2015; 29: 123-131.
Parkinson’s disease [41,42]. Referral rates for physiotherapy in 11. Fahn S, Elton RL. Recent Developments in Parkinsons
Parkinson’s disease are low [41], and the main objective of Disease. Macmil Health Info 1987; 2: 153-163.
rehabilitation in PD is usually to recover motor function; 12. Hoehn MM, Yahr MD. Parkinsonism: onset, progression,
however our study has demonstrated that PPT application in and mortality. Neurol 1967; 17: 427-442.
PD is also effective in decreasing the non-motor symptoms 13. American Thoracic Society Statement Guidelines for the
(including anxiety, depression, and sleepiness), and in six-minute walk test. Am J Respir Crit Care Med 2002;
increasing the quality of life. As a conclusion, addition of 166: 111-117.
pulmonary exercises to the physical therapy program of the
14. Martinez-Martin P, Jeukens-Visser M, Lyons KE. Health-
patients with Parkinson’s disease, suggests potential benefits.
related quality-of-life scales in Parkinsons disease: critique
and recommendations. Mov Disord 2011; 26: 2371-2380.
Author Roles 15. Gazibara T, Pekmezovic T, Kisic Tepavcevic D. Health-
Design: BDG, YA; data acquisition: BDG, YGA, ACG; DD, related quality of life in patients with Parkinsons disease:
SB; statistical analysis: YA; first draft of the manuscript: YA. Implications for falling. Parkinsonism Relat Disord 2015;
All authors reviewed and commented on the final manuscript. 21: 573-576.
16. Beck AT, Epstein N, Brown G, Steer RA. An inventory for
Conflicts of Interest measuring clinical anxiety: psychometric properties. J
Consult Clin Psychol 1988; 56: 893-897.
The authors declare that they have no conflicts of interest in
17. Beck AT, Steer RA. Internal consistencies of the original
relation to this article.
and revised Beck Depression Inventory. J Clin Psychol
1984; 40: 1365-1367.
References 18. Johns MW. A new method for measuring daytime
1. Foundation PsD Understanding Parkinsons 2014. sleepiness: the Epworth Sleepiness Scale. Sleep 1991; 14:
540-545.
4 Biomed Res- India 2017 Volume 28 Issue 1
The effects of a pulmonary rehabilitation program on exercise tolerance, quality of life, sleep quality and emotional
status in the patients with Parkinson's disease
19. Rutten S, Ghielen I, Vriend C. Anxiety in Parkinsons 33. Gustafsson H, Nordstrom P, Strahle S, Nordstrom A.
disease: Symptom dimensions and overlap with depression Parkinsons disease: a population-based investigation of life
and autonomic failure. Parkinsonism Relat Disord 2015; satisfaction and employment. J Rehabil Med 2015; 47:
21: 189-193. 45-51.
20. Rodriguez-Violante M, Cervantes-Arriaga A, Corona T. 34. Burn DJ, Landau S, Hindle JV. Parkinsons disease motor
Clinical determinants of health-related quality of life in subtypes and mood. Mov Disord 2012; 27: 379-386.
Mexican patients with Parkinsons disease. Arch Med Res 35. King LA, Wilhelm J, Chen Y. Effects of Group, Individual,
2013; 44: 110-114. and Home Exercise in Persons With Parkinson Disease: A
21. Negre-Pages L, Grandjean H, Lapeyre-Mestre M. Anxious Randomized Clinical Trial. J Neurol Phys Ther 2015; 39:
and Depressive Symptoms in Parkinsons Disease: The 204-212.
French Cross-Sectionnal DoPAMiP Study. Mov Disord 36. Adamson BC, Ensari I, Motl RW. Effect of exercise on
2010; 25: 157-166 depressive symptoms in adults with neurologic disorders: a
22. Reijnders JS, Ehrt U, Weber WE. A systematic review of systematic review and meta-analysis. Arch Phys Med
prevalence studies of depression in Parkinsons disease. Rehabil 2015; 96: 1329-1338.
Mov Disord 2008; 23: 183-189 37. Kulisevsky J, Pagonabarraga J, Pascual-Sedano B. Motor
23. Dissanayaka NN, White E, OSullivan JD. The clinical changes during sertraline treatment in depressed patients
spectrum of anxiety in Parkinsons disease. Mov Disord with Parkinsons disease. Eur J Neurol 2008; 15: 953-959.
2014; 29: 967-975 38. Wang Y, Shao WB, Gao L. Abnormal pulmonary function
24. Burn DJ, Landau S, Hindle JV. Parkinsons disease motor and respiratory muscle strength findings in Chinese patients
subtypes and mood. Mov Disord 2012; 27: 379-386. with Parkinsons disease and multiple system atrophy--
25. Blonder LX, Slevin JT. Emotional dysfunction in comparison with normal elderly. PLoS One 2014; 9:
Parkinsons disease. Behav Neurol 2011; 24: 201-217. 116123.
26. Adamson BC, Ensari I, Motl RW. Effect of exercise on 39. Scalzo PL, Flores CR, Marques JR. Impact of changes in
depressive symptoms in adults with neurologic disorders: a balance and walking capacity on the quality of life in
systematic review and meta-analysis. Arch Phys Med patients with Parkinsons disease. Arq Neuropsiquiatr 2012;
Rehabil 2015; 96: 1329-1338. 70: 119-124.
27. Hackney ME, Earhart GM. Effects of dance on movement 40. Cugusi L, Solla P, Zedda F. Effects of an adapted physical
control in Parkinsons disease: a comparison of Argentine activity program on motor and non-motor functions and
tango and American ballroom. J Rehabil Med 2009; 41: quality of life in patients with Parkinsons disease. Neur
475-481. Rehabilit 2014; 35: 789-94.
28. Ylikoski A, Martikainen K, Sieminski M, Partinen M. 41. Tomlinson CL, Patel S, Meek C. Physiotherapy
Parkinsons disease and insomnia. Neurol Sci 2015; 36: intervention in Parkinsons disease: systematic review and
2003-2010. meta-analysis. BMJ 2012; 6: 5004.
29. Pellecchia MT, Antonini A, Bonuccelli U. Observational 42. Vitale C, Agosti V, Avella D. Effect of Global Postural
study of sleep-related disorders in Italian patients with Rehabilitation program on spatiotemporal gait parameters
Parkinsons disease: usefulness of the Italian version of of parkinsonian patients: a three-dimensional motion
Parkinsons disease sleep scale. Neurol Sci 2012; 33: analysis study. Neurol Sci 2012; 33: 1337-1343.
689-694.
*Correspondence to
30. Knie B, Mitra MT, Logishetty K, Chaudhuri KR. Excessive
daytime sleepiness in patients with Parkinsons disease.
Belma Gungen
CNS Drugs 2011; 25: 203-212.
31. Santamaria J. How to evaluate excessive daytime Department of Neurology
sleepiness in Parkinsons disease. Neurol 2004; 63: 21-23. Sakarya University
32. Andrianasolo RM, Menai M, Galan P. Leisure-Time
Physical Activity and Sedentary Behavior and Their Cross- Research and Training Hospital
Sectional Associations with Excessive Daytime Sleepiness Turkey
in the French SUVIMAX-2 Study. Int J Behav Med 2015;
7.
Biomed Res- India 2017 Volume 28 Issue 1 5
You might also like
- Exercise Physiology for the Pediatric and Congenital CardiologistFrom EverandExercise Physiology for the Pediatric and Congenital CardiologistNo ratings yet
- JPP2006Document10 pagesJPP2006Gaoudam NatarajanNo ratings yet
- Pilates 1Document12 pagesPilates 1aniakurowska2000No ratings yet
- Articulo Asma 2020Document6 pagesArticulo Asma 2020steven garciaNo ratings yet
- Leal 2019Document6 pagesLeal 2019Erik ArturNo ratings yet
- EXCELENTEDocument7 pagesEXCELENTEJorge GámezNo ratings yet
- Equilibrio y Movilidad en Pacientes Con Enfermedad de Parkinson Recién Diagnosticada Seguimiento de Cinco Años de Una Cohorte en El Norte de SueciaDocument10 pagesEquilibrio y Movilidad en Pacientes Con Enfermedad de Parkinson Recién Diagnosticada Seguimiento de Cinco Años de Una Cohorte en El Norte de SueciacamilaNo ratings yet
- Effects of Physical Exercise On Quality of Life, Exercise Capacity and Pulmonary Function in Children With AsthmaDocument6 pagesEffects of Physical Exercise On Quality of Life, Exercise Capacity and Pulmonary Function in Children With AsthmaFebry FirmansyahNo ratings yet
- Effect of Health Baduanjin Qigong For Mild To Moderate Parkinson's DiseaseDocument9 pagesEffect of Health Baduanjin Qigong For Mild To Moderate Parkinson's DiseaseHevin GokulNo ratings yet
- The Effect of Progressive Relaxation Exercises On Pain, Fatigue, and Quality of Life in Dialysis PatientsDocument8 pagesThe Effect of Progressive Relaxation Exercises On Pain, Fatigue, and Quality of Life in Dialysis PatientsNova DenisaNo ratings yet
- Importante Protocolo de Ejercicios en PiscinaDocument14 pagesImportante Protocolo de Ejercicios en PiscinaEduardo Santana SuárezNo ratings yet
- Parkinson Subtypes Progress Differently PDFDocument8 pagesParkinson Subtypes Progress Differently PDFParisNo ratings yet
- Dance For PDDocument6 pagesDance For PDfozia hayyatNo ratings yet
- Jurnal PendukungDocument5 pagesJurnal PendukungrekaNo ratings yet
- Jurnal PendukungDocument5 pagesJurnal PendukungrekaNo ratings yet
- Rosenbaum 2014 - Atividade Fisica em Saude MentalDocument11 pagesRosenbaum 2014 - Atividade Fisica em Saude MentalTav NetoNo ratings yet
- Journal of ScienceDocument4 pagesJournal of ScienceEndang SetiawatiNo ratings yet
- The Therapeutic Effects of Exercise Training On Elderly Patients With DementiaDocument23 pagesThe Therapeutic Effects of Exercise Training On Elderly Patients With DementiamarshaNo ratings yet
- Brief Illness Perception QuestionnaireDocument7 pagesBrief Illness Perception QuestionnairemarthamilenNo ratings yet
- Ai Chi Parkinson's DiseaseDocument8 pagesAi Chi Parkinson's Disease黃姵儒No ratings yet
- Frazzitta Et AlDocument8 pagesFrazzitta Et Alalex ormazabalNo ratings yet
- Effect of Sensory Cueing On Gait and Balance During Both "On" and "Off" Drug Phase of Parkinson'S DiseaseDocument9 pagesEffect of Sensory Cueing On Gait and Balance During Both "On" and "Off" Drug Phase of Parkinson'S DiseaseDr. Krishna N. SharmaNo ratings yet
- Comparison of Health-Related Quality of Life Measures in Chronic Obstructive Pulmonary DiseaseDocument6 pagesComparison of Health-Related Quality of Life Measures in Chronic Obstructive Pulmonary Diseasealfer_73No ratings yet
- 6 Cheng2017Document7 pages6 Cheng2017Sergio Machado NeurocientistaNo ratings yet
- Article HUNT Model For VO2peakDocument20 pagesArticle HUNT Model For VO2peakAntonio JairoNo ratings yet
- The Library: Archives of Physical Medicine and Rehabilitation. Changes Resulting From TheDocument20 pagesThe Library: Archives of Physical Medicine and Rehabilitation. Changes Resulting From TheRaoof ARIFNo ratings yet
- Heijden2013 Article EffectsOfExerciseTrainingOnQuaDocument16 pagesHeijden2013 Article EffectsOfExerciseTrainingOnQuaALberta YosheNo ratings yet
- Rehabilitasi CopdDocument8 pagesRehabilitasi CopdHenny RahmawatiNo ratings yet
- Predictors of Psych Intervention To Promote Health Behaviour Adherence in HF 2021Document14 pagesPredictors of Psych Intervention To Promote Health Behaviour Adherence in HF 2021Bob JoeNo ratings yet
- Quality of Life and Psychological Well-Being in Patients With Various Pacing ModesDocument7 pagesQuality of Life and Psychological Well-Being in Patients With Various Pacing ModesFahmi Azhari BasyaNo ratings yet
- Otago Home-Based Strength and Balance Retraining Improves Executive Functioning in Older Fallers - A Randomized Controlled Trial.Document10 pagesOtago Home-Based Strength and Balance Retraining Improves Executive Functioning in Older Fallers - A Randomized Controlled Trial.Ed RibeiroNo ratings yet
- The Effect of Pulmonary Rehabilitation On Physical Performance and Health Related Quality of Life in Patients With Chronic Lung DiseaseDocument1 pageThe Effect of Pulmonary Rehabilitation On Physical Performance and Health Related Quality of Life in Patients With Chronic Lung Diseasedr. Amori Amar LakcandraNo ratings yet
- Bartlett 2020Document9 pagesBartlett 2020Erick SolisNo ratings yet
- Progressive Resistance ExercisesDocument9 pagesProgressive Resistance ExercisesNaomi AperutaNo ratings yet
- Seyedichegeni 2018Document7 pagesSeyedichegeni 2018Hafidz Ma'rufNo ratings yet
- Chapter 2 Literature ReviewDocument10 pagesChapter 2 Literature ReviewIqra AsimNo ratings yet
- Physical Activity Coaching Via Telehealth For.3Document11 pagesPhysical Activity Coaching Via Telehealth For.3Montserrat Suárez SánchezNo ratings yet
- LSVT BigDocument13 pagesLSVT BigAgatha SharmaNo ratings yet
- 1 KowalczykDocument6 pages1 KowalczykLuis Diego Verastegui LeguaNo ratings yet
- Gordon Et Al., (2019) Efecct of Pulmonary Rehabilitation On Symptoms of Anxiety and Depression in Chronic Obstructive Pulmonary DiseaseDocument12 pagesGordon Et Al., (2019) Efecct of Pulmonary Rehabilitation On Symptoms of Anxiety and Depression in Chronic Obstructive Pulmonary DiseaseAna Flávia SordiNo ratings yet
- Goodwin Et Al-2008-Movement DisordersDocument10 pagesGoodwin Et Al-2008-Movement DisordersyuliatinnisaNo ratings yet
- Exercise and Sleep-Disordered Breathing: An Association Independent of Body HabitusDocument5 pagesExercise and Sleep-Disordered Breathing: An Association Independent of Body HabitusponnuswamyvNo ratings yet
- 2022 Article 14213Document16 pages2022 Article 14213Gabriel DelfinoNo ratings yet
- The Use of A Drum Circle To Improve The Symptoms and Signs of Parkinson's DiseaseDocument7 pagesThe Use of A Drum Circle To Improve The Symptoms and Signs of Parkinson's DiseaseMatt LaffanNo ratings yet
- Cardioresp and Young Adults With DiabetesDocument8 pagesCardioresp and Young Adults With DiabetesNicole GreeneNo ratings yet
- 10 1 1 880 5438 PDFDocument8 pages10 1 1 880 5438 PDFĚlîâȟ Gṫȓ GûângûlNo ratings yet
- PD and Exercise Review AcceptedDocument23 pagesPD and Exercise Review AcceptedPooja HandujaNo ratings yet
- Garssen, 2004 - Physical Training and Fatigue, Fitness, and Quality of Life in Guillain-Barre Syndrome and CIDPDocument3 pagesGarssen, 2004 - Physical Training and Fatigue, Fitness, and Quality of Life in Guillain-Barre Syndrome and CIDPkarinaNo ratings yet
- Vastly Different Exercise Programs Similarly Improve Parkinsonian SymptomsDocument8 pagesVastly Different Exercise Programs Similarly Improve Parkinsonian SymptomsSuislian MarjorieNo ratings yet
- Working On Asymmetry in Parkinsons DiseaseDocument7 pagesWorking On Asymmetry in Parkinsons DiseaseSuislian MarjorieNo ratings yet
- Indian Heart Journal: Original ArticleDocument5 pagesIndian Heart Journal: Original ArticleRendi KurniawanNo ratings yet
- Artikel 1Document11 pagesArtikel 1wardatul UllyaNo ratings yet
- Ecam2015 792895Document8 pagesEcam2015 792895Meri Fitria HandayaniNo ratings yet
- Determinants and Outcomes of Physical Activity in Patients With COPD A Systematic ReviewDocument10 pagesDeterminants and Outcomes of Physical Activity in Patients With COPD A Systematic ReviewHansCristopherSaegerPizarroNo ratings yet
- 10.1093 PTJ Pzac153Document13 pages10.1093 PTJ Pzac153evelyn.minichNo ratings yet
- Body Mass IndexDocument6 pagesBody Mass Indexayu yuliantiNo ratings yet
- JCM 11 00683Document14 pagesJCM 11 00683Metin HakkanNo ratings yet
- Validation of A Health-Related Quality of LifeDocument8 pagesValidation of A Health-Related Quality of LifeMarcellaNo ratings yet
- A 12-Month, Moderate-Intensity Exercise Training Program Improves Fitness and Quality of Life in Adults With Asthma: A Controlled TrialDocument3 pagesA 12-Month, Moderate-Intensity Exercise Training Program Improves Fitness and Quality of Life in Adults With Asthma: A Controlled TrialAmir SaifudinNo ratings yet
- KahramanDocument6 pagesKahramanNicolásAlcaláNo ratings yet
- PHASE 2 NCP (Injury, Risk For Bleeding)Document3 pagesPHASE 2 NCP (Injury, Risk For Bleeding)NE TdrNo ratings yet
- Environmental Health and Sustainable Development in Ogoni DR UzorkaDocument30 pagesEnvironmental Health and Sustainable Development in Ogoni DR UzorkaBettyNo ratings yet
- L.P. of Transcultural NursingDocument14 pagesL.P. of Transcultural Nursingvikas takNo ratings yet
- EULAR Points To Consider For The Management of Difficult To Treat Rheumatoid ArthritisDocument14 pagesEULAR Points To Consider For The Management of Difficult To Treat Rheumatoid ArthritisseleneNo ratings yet
- Iv PrimingDocument16 pagesIv PrimingZahra jane A.No ratings yet
- Pre-Birth Waiting Rooms - Proposal TemplateDocument8 pagesPre-Birth Waiting Rooms - Proposal TemplateKisslay AnandNo ratings yet
- PreviewpdfDocument88 pagesPreviewpdfHeidy Montes Galarza100% (1)
- Module - 5 - PPPQMS - Lifecycle Management 2018Document11 pagesModule - 5 - PPPQMS - Lifecycle Management 2018Indra Maghfurin100% (1)
- Askhole #2 - Sheet1Document15 pagesAskhole #2 - Sheet1gottfriedackermannNo ratings yet
- Short Increment Sensitivity Index Test (SISI)Document2 pagesShort Increment Sensitivity Index Test (SISI)Anish RajNo ratings yet
- MST Observation FeedbackDocument7 pagesMST Observation Feedbackapi-380948601No ratings yet
- Social Psychology Myers 10th Edition Test BankDocument42 pagesSocial Psychology Myers 10th Edition Test BankHeidi Keller100% (31)
- How To Get The Perfect Tattoo PDFDocument11 pagesHow To Get The Perfect Tattoo PDFSebastian GuevaraNo ratings yet
- Session Plan: Learning OutcomeDocument6 pagesSession Plan: Learning OutcomeByron AbelitaNo ratings yet
- Challenges Faced by Roma Women in EuropeDocument29 pagesChallenges Faced by Roma Women in EuropeaurimiaNo ratings yet
- Emdad's Answers For SST in PTEDocument9 pagesEmdad's Answers For SST in PTEGlishna Peushan Widanapathirana100% (1)
- 9RESPIRATORY THERAPY EQUIPMENT PPTDocument6 pages9RESPIRATORY THERAPY EQUIPMENT PPTJack OneNo ratings yet
- Meta 2Document14 pagesMeta 2S2-IKM ULMNo ratings yet
- BillSilversEthicalWill Digital LetterheadDocument3 pagesBillSilversEthicalWill Digital LetterheadCPR DigitalNo ratings yet
- New (Oumh1303) Breakfast Is The Most Important Meal of The DayDocument6 pagesNew (Oumh1303) Breakfast Is The Most Important Meal of The DayjeckNo ratings yet
- ApplicationForm - Intake 2024 MidwiferyDocument14 pagesApplicationForm - Intake 2024 Midwiferyanthonylota84No ratings yet
- Theories of Personality: Rollo Reese MayDocument4 pagesTheories of Personality: Rollo Reese MayShammah PradesNo ratings yet
- Social Media and Its Negative EffectsDocument25 pagesSocial Media and Its Negative EffectsRhowen Jay RamaNo ratings yet
- Introduction To SportsDocument16 pagesIntroduction To SportsAlabaster 3927No ratings yet
- Lecture 2-Environmental Health HazardsDocument13 pagesLecture 2-Environmental Health HazardsAzizulHuqueNo ratings yet
- Garces PsychDocument2 pagesGarces PsychSherlyn Miranda GarcesNo ratings yet
- The 6 Nutrients WorksheetsDocument4 pagesThe 6 Nutrients WorksheetschillNo ratings yet
- Ingles 2018Document12 pagesIngles 2018Carmen GarciaNo ratings yet
- Fetal DevelopmentDocument15 pagesFetal DevelopmentOmar HammadNo ratings yet
- CDC Misinformation EmailsDocument76 pagesCDC Misinformation EmailsZerohedge Janitor100% (2)