Professional Documents
Culture Documents
Fournier's Gangrene Guidelines
Uploaded by
David Morales ZepedaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fournier's Gangrene Guidelines
Uploaded by
David Morales ZepedaCopyright:
Available Formats
VUMC Multidisciplinary Surgical Critical Care Service
Fournier’s Gangrene Guidelines
Definition: A variant of necrotizing soft tissue infection that involves the scrotum and penis or vulva.
Isolation Requirement
• Contact isolation AND droplet precautions is required for 24 hours after the first dose of broad
spectrum antibiotics. After 24 hours of contact and droplet precautions, both can be discontinued as
long as the patient does not grow a pathogen that requires isolation per VUMC guidelines.
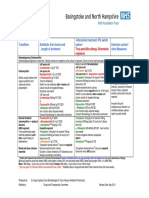
Antimicrobial Therapy
Preferred Regimen: Severe Penicillin Allergy:
Vancomycin Vancomycin
(+) (+)
Empiric Therapy OR
Clindamycin Clindamycin
(+) (+)
Piperacillin/Tazobactam* Meropenem or Cefepime
Narrow Therapy
Streptococcus Polymicrobial without
Clostridium
Pyogenes Staph Aureus Pseudomonas or
species
(Group A Strep) Staph Aureus
Definitive Therapy
Penicillin G** Ampicillin/Sulbactam
MSSA: Cefazolin
(unless severe Or
MRSA: Vancomycin
allery) Ceftriaxone (+)
metronidazole
*Consider Cefepime as an alternative option
**Continue Clindamycin if exhibiting signs of toxic shock
Labs/Cultures
• Peripheral blood cultures x 2 on presentation
• Operative tissue cultures
• Daily CBC and CRP
• Hemoglobin A1c
Infectious Disease Consult
The infectious disease service should be consulted for any of the following criteria
• Bacteremia
• Multidrug resistant pathogens
• Debridement with osteoarticular involvement (bone or exposed bone)
• Consult required per VUMC policy (e.g. Staph Aureus bacteremia)
Antibiotic Duration
Systemic antibiotics in soft tissue infections should be continued until the following criteria are met:
1. Source control has been obtained
2. Patient is hemodynamically stable
3. Fever has been absent for 48 hours
4. White blood cell count has improved
5. CRP down trending
Glucose Management
Blood Glucose Target
• 110-150 mg/dL
Insulin Therapy
• Initiate insulin therapy if blood glucose is >150mg/dL or the patient has diabetes
• Consider initiating an insulin infusion for ≥ 2 blood glucoses > 200 mg/dl (requires admission to an ICU)
Endocrinology Consult
• Consider consulting endocrinology/glucose management service for the following
o Hemoglobin A1c > 6.5 to assist with inpatient control and outpatient follow-up
o Transitioning off the insulin infusion
Dosing Guidance
Creatinine Clearance (ml/min)
Drug >80 50-80 30-50 10-30 <10 or HD
Ampicillin/Sulbactam 3000mg q6h 3000mg q6-8h 3000mg q12h 3000mg q24h
Cefazolin 2000mg Q8h 1000mg Q12h 1000mg Q24h
Cefepime 2000mg Q8h 2000mg Q12h 2000mg Q24h 1000mg Q24h
Ceftriaxone 2000mg Q24h
Clindamycin 900mg Q8h
Meropenem 1000mg Q8h 1000mg Q12h 1000mg Q24h
Metronidazole 500mg Q8h
Penicillin G 4 million units Q4h 2-4 million units Q6h 2 million units
Q6h
Piperacillin/Tazobactam 3.375mg Q8h 3.375mg Q12h
References
1. Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue
infections: 2014 update by the infectious diseases society of America. Clin Infect Dis 2014; 26:147.
2. Stevens DL, Bryant AE. Necrotizing Soft-Tissue Infections. NEJM. 2017; 377:2253.
3. Jacobi J, Bircher N, Krinsley J, et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in
critically ill patients. Critical Care Medicine 2012; 40:3251–3276
4. Lauerman MH, Kolesnik O, Sethuraman K, et al. Less is more? Antibiotic duration and outcomes in Fournier’s gangrene.
Trauma and Acute Care Surgery. 2017; 83: 443-448
5. Beauchamp LC, Mostafavifar LG, Evanc DC, et al. Sweet and Sour: Impact of Early Glycemic Control on Outcomes in
Necrotizing Soft- Tissue Infections. Surgical Infections. 2019; 20: 305-310
Authors:
Austin Ing, PharmD
Kelli Rumbaugh, PharmD
Niels Johsnen, MD MPH
Patty Wright, MD
Liza Weavind, MD
You might also like
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- Antibiotic Surgical Prophylaxis Protocol SMH October 2018 UpdateDocument7 pagesAntibiotic Surgical Prophylaxis Protocol SMH October 2018 Updatessrnew2023No ratings yet
- Antimicrobial Therapy in Veterinary MedicineFrom EverandAntimicrobial Therapy in Veterinary MedicineSteeve GiguèreRating: 4 out of 5 stars4/5 (1)
- CNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Document1 pageCNS: Ent:: Review Antibiotic Therapy Daily - Can You: Stop? Switch? Simplify? or State Duration?Fitri RachmadaniNo ratings yet
- Antibiotic hospital manDocument1 pageAntibiotic hospital manarshiya.manasekiNo ratings yet
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- Protcolo NacDocument2 pagesProtcolo NacJdmp Lopez MorenoNo ratings yet
- Sepsis and Catheter Infections: Early Conversion From IV To Oral AntibioticsDocument4 pagesSepsis and Catheter Infections: Early Conversion From IV To Oral AntibioticsChaim HerreraNo ratings yet
- Central Nervous System InfectionsDocument9 pagesCentral Nervous System InfectionsSaddamNo ratings yet
- IDSA - ATS 2016 Guideline for HAP and VAPDocument1 pageIDSA - ATS 2016 Guideline for HAP and VAPMariana MarpaungNo ratings yet
- Paclitaxel With Dose Dense EC Adjuvant or Neo-Adjuvant Protocol V1.0Document7 pagesPaclitaxel With Dose Dense EC Adjuvant or Neo-Adjuvant Protocol V1.0smokkerNo ratings yet
- Empiric Antibiotic ListDocument2 pagesEmpiric Antibiotic ListpasswordNo ratings yet
- NAG Upper Respiratory Tract InfectionsDocument20 pagesNAG Upper Respiratory Tract InfectionsJun JimenezNo ratings yet
- Adult Sepsis Order SetDocument3 pagesAdult Sepsis Order SetYoussef MokdadNo ratings yet
- Sepsis Antibiotics 2019 PDFDocument3 pagesSepsis Antibiotics 2019 PDFKobra CaktusNo ratings yet
- Treatment of MalariaDocument49 pagesTreatment of MalariaShanza AmaanNo ratings yet
- TREATING OBSTETRIC/GYNECOLOGIC INFECTIONSDocument3 pagesTREATING OBSTETRIC/GYNECOLOGIC INFECTIONSHarshit RastogiNo ratings yet
- Paclitaxel With EC Adjuvant or Neoadjuvant Protocol V1.1Document7 pagesPaclitaxel With EC Adjuvant or Neoadjuvant Protocol V1.1smokkerNo ratings yet
- Paclitaxel Trastuzumab Breast Cancer ProtocolDocument9 pagesPaclitaxel Trastuzumab Breast Cancer ProtocolsmokkerNo ratings yet
- 2012 Aug IMG Poster 165760a SepsisDocument1 page2012 Aug IMG Poster 165760a SepsisTeng Huei LeeNo ratings yet
- SQC ABx Guidelines 2-21-2011 PDFDocument2 pagesSQC ABx Guidelines 2-21-2011 PDFMinh SteveNo ratings yet
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocument1 pageGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxNo ratings yet
- Internal-Abdominal-infection-Treatment-ProtocolDocument9 pagesInternal-Abdominal-infection-Treatment-Protocolhatem newishyNo ratings yet
- Severe Sepsis and Septic Shock Antibiotic Guide: Community AcquiredDocument6 pagesSevere Sepsis and Septic Shock Antibiotic Guide: Community AcquiredAnonymous G6zDTD2yNo ratings yet
- Pneumonia Treatment Algorithm With Addendum For Aspiration 2015-2016.01.19Document2 pagesPneumonia Treatment Algorithm With Addendum For Aspiration 2015-2016.01.19Irsalina TriastutikNo ratings yet
- BTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Document2 pagesBTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Corry ApriliaNo ratings yet
- Obstetrics / Gynaecological Infections: Indications First Line AlternateDocument2 pagesObstetrics / Gynaecological Infections: Indications First Line AlternateAli ShanNo ratings yet
- Medicine RotatationbookletDocument20 pagesMedicine RotatationbookletJanelle JosephsNo ratings yet
- SHC Antimicrobial Prophylaxis RecommendationsDocument3 pagesSHC Antimicrobial Prophylaxis RecommendationsCatherine MorrisNo ratings yet
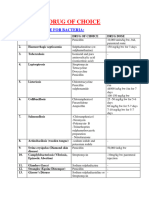
- Share Drugs of Choice To DiseasesDocument4 pagesShare Drugs of Choice To DiseasesDrkhanmianiNo ratings yet
- Febrile NeutropeniaDocument3 pagesFebrile Neutropeniatheseus5No ratings yet
- Fluconazole: ErthromycinDocument7 pagesFluconazole: ErthromycinAseel AlsheeshNo ratings yet
- Antibiotic Guidelines For PediatricsDocument33 pagesAntibiotic Guidelines For PediatricsVarshini Tamil SelvanNo ratings yet
- Antimicrobials - SPDocument27 pagesAntimicrobials - SPAmisha VastaniNo ratings yet
- Vancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., PharmDocument78 pagesVancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., Pharmkharbosham100% (1)
- Pocket Guide June2013 PDFDocument2 pagesPocket Guide June2013 PDFSergeyGruntov100% (1)
- NICU ABX ChartDocument11 pagesNICU ABX ChartdrchiNo ratings yet
- Cisplatin-Pemetrexed (NSCLC)Document5 pagesCisplatin-Pemetrexed (NSCLC)Sindu SankarNo ratings yet
- CAP Guidance 2020 Revision Final UpdatedDocument11 pagesCAP Guidance 2020 Revision Final UpdatedNeerajaNo ratings yet
- GDL 01240Document7 pagesGDL 01240Christian KosiNo ratings yet
- Antimicrobial Dosage Adjustments in Renal Impairment For FormularyDocument20 pagesAntimicrobial Dosage Adjustments in Renal Impairment For Formularyangkatanjuli2019No ratings yet
- Guidelines For Inpatient Management of PneumoniaDocument2 pagesGuidelines For Inpatient Management of PneumoniaHamza El-ȜfifiNo ratings yet
- NAG Central Nervous System Infections As of Nov 2017Document9 pagesNAG Central Nervous System Infections As of Nov 2017Rhod Bernaldez EstaNo ratings yet
- Management of CAP in Adults - Ontario GovernmentDocument2 pagesManagement of CAP in Adults - Ontario GovernmentSukhvir AujlaNo ratings yet
- AHS антибиотики рекомендацDocument42 pagesAHS антибиотики рекомендацMaksym DemianchukNo ratings yet
- Wound Infections: Common PathogensDocument1 pageWound Infections: Common PathogensAnonymous KGxzow5zxhNo ratings yet
- Paediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeDocument9 pagesPaediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeZamzam DomaNo ratings yet
- Antibiotic/Antiviral Policy - Paediatric PCF (EWMSCDocument9 pagesAntibiotic/Antiviral Policy - Paediatric PCF (EWMSCLizbet parrondoNo ratings yet
- Empiric Treatment Guidelines Common InfectionsDocument9 pagesEmpiric Treatment Guidelines Common InfectionsShiza Batool100% (1)
- Rapid Blood Pathogen Identification Panel: Staphylococcus Genus Analyte Will Be DetectedDocument8 pagesRapid Blood Pathogen Identification Panel: Staphylococcus Genus Analyte Will Be DetectedAlessia JankowskiNo ratings yet
- HSB Pneumonia Antibiotic AlgorithmDocument4 pagesHSB Pneumonia Antibiotic AlgorithmDr.Senthil KumarNo ratings yet
- Antibiotic PolicyDocument10 pagesAntibiotic Policykrutarth shahNo ratings yet
- Antibiotic ProphylaxisDocument2 pagesAntibiotic Prophylaxisabdelhamed aliNo ratings yet
- Day 1 Typhoid Fever_ItableDocument42 pagesDay 1 Typhoid Fever_ItableRye CalderonNo ratings yet
- Bone and Joint Infection Treatment GuidelinesDocument3 pagesBone and Joint Infection Treatment GuidelinesDanissa Fidia PuteriNo ratings yet
- SSTI and Skin Infection Treatment GuideDocument22 pagesSSTI and Skin Infection Treatment GuideAlexis TranNo ratings yet
- Ritemed Clindamycin HCL: Therapeutic CategoryDocument4 pagesRitemed Clindamycin HCL: Therapeutic CategoryJ Ohn P AulNo ratings yet
- Paclitaxel Carboplatin Protocol Gynae CancerDocument8 pagesPaclitaxel Carboplatin Protocol Gynae CancerHeryanti PusparisaNo ratings yet
- Antibiotic Guidelines for Skin and Soft Tissue InfectionsDocument11 pagesAntibiotic Guidelines for Skin and Soft Tissue InfectionslaptopgreyNo ratings yet
- NAG Skin and Soft Tissue Infections AdultsDocument21 pagesNAG Skin and Soft Tissue Infections AdultsJun JimenezNo ratings yet
- Post Graduate Academic Report Vion FinalDocument18 pagesPost Graduate Academic Report Vion FinalVishali RayapudiNo ratings yet
- nuRSING rEVIEWER PART 2Document9 pagesnuRSING rEVIEWER PART 2Johny VillanuevaNo ratings yet
- Surat Buat VisaDocument12 pagesSurat Buat VisaNurul FitrianaNo ratings yet
- In The High Court of Judicature at MadrasDocument17 pagesIn The High Court of Judicature at MadrasChinna Balanna NalamalaNo ratings yet
- Multiple Choice Question (MCQ) Exam: 15 Sample QuestionsDocument4 pagesMultiple Choice Question (MCQ) Exam: 15 Sample QuestionssheryNo ratings yet
- New PRC FormDocument6 pagesNew PRC Formduke1206No ratings yet
- MIT Technology Review 2020 11Document92 pagesMIT Technology Review 2020 11pppaolo100% (1)
- Code of Medical Ethics Chapter 8Document12 pagesCode of Medical Ethics Chapter 8api-324680787No ratings yet
- Improving Attitudes and Perceptions About End-of-Life Nursing On A Hospital-Based Palliative Care UnitDocument8 pagesImproving Attitudes and Perceptions About End-of-Life Nursing On A Hospital-Based Palliative Care UnitSERGIO ANDRES CESPEDES GUERRERONo ratings yet
- Sandra A. Mouloudj Recognized As A Professional of The Year by Strathmore's Who's Who Worldwide PublicationDocument2 pagesSandra A. Mouloudj Recognized As A Professional of The Year by Strathmore's Who's Who Worldwide PublicationPR.comNo ratings yet
- DOH Updates For PHA - May 6 Baguio PDFDocument49 pagesDOH Updates For PHA - May 6 Baguio PDFKaren BalanayNo ratings yet
- Living Donor Transplantation BrochureDocument13 pagesLiving Donor Transplantation BrochureShani KushwahaNo ratings yet
- Correspondence: The Fishmouth Phenomenon in Retinal DetachmentDocument1 pageCorrespondence: The Fishmouth Phenomenon in Retinal DetachmentSushi HtetNo ratings yet
- Children's Hospital Pain Clinic BrochureDocument2 pagesChildren's Hospital Pain Clinic BrochureM CurtissNo ratings yet
- The Gazette April 2013Document12 pagesThe Gazette April 2013St George's Healthcare NHS TrustNo ratings yet
- Draft Guidelines On Post Registration Variations To Registered Pharmaceutical and Biological Drug Products.Document35 pagesDraft Guidelines On Post Registration Variations To Registered Pharmaceutical and Biological Drug Products.vafaashkNo ratings yet
- Young Latina MS PatientDocument14 pagesYoung Latina MS PatientSnezana MihajlovicNo ratings yet
- Cannulation and Venepuncture WorkbookDocument58 pagesCannulation and Venepuncture WorkbookNorbertus Maceka83% (6)
- Ethics in Health CareDocument23 pagesEthics in Health CareShimmering MoonNo ratings yet
- LFD FormatDocument2 pagesLFD FormatKristine Angie RamosNo ratings yet
- Neurología NatalizumabDocument41 pagesNeurología Natalizumablorcy9No ratings yet
- Interview Questions-Ronak ShahDocument3 pagesInterview Questions-Ronak Shahapi-277297976No ratings yet
- Resume - Viroja Sweta For PortfolioDocument1 pageResume - Viroja Sweta For Portfolioapi-608195339No ratings yet
- Lesson 1.1: Historical Perspectives of Nursing InformaticsDocument33 pagesLesson 1.1: Historical Perspectives of Nursing InformaticsJustine Jean GuillermoNo ratings yet
- Long Resume and ApplicationDocument5 pagesLong Resume and ApplicationCarlo Domingo LadieroNo ratings yet
- 1 CBT Sample Questionnaires-1Document101 pages1 CBT Sample Questionnaires-1Mhee FaustinaNo ratings yet
- Essay On Academic BurnoutDocument1 pageEssay On Academic BurnoutrighteousindignationNo ratings yet
- Phs 801 Introduction To Public Health and Primary Health CareDocument107 pagesPhs 801 Introduction To Public Health and Primary Health CareEnobong UsoroNo ratings yet
- Post and Cores CaseDocument7 pagesPost and Cores Caseanuj sharmaNo ratings yet
- Clarion Technologies: at A GlanceDocument7 pagesClarion Technologies: at A GlanceChetan PrasadNo ratings yet