Professional Documents
Culture Documents
Antibiotic Guidelines For Pediatrics
Uploaded by
Varshini Tamil SelvanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibiotic Guidelines For Pediatrics
Uploaded by
Varshini Tamil SelvanCopyright:
Available Formats
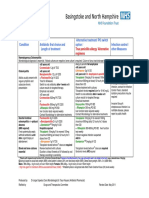
PEDIATRIC ANTIBIOTIC
GUIDELINES
2019
CONTENTS
INSTRUCTIONS……………………………………………………………………………………………………………. 2
RESPIRATORY INFECTIONS……………………………………………………………………………………………. 3
EAR, NOSE AND THROAT INFECTIONS………………………………………………………………………………..5
OPHTHALMIC INFECTIONS……………………………………………………………………………………………….8
CENTRAL NERVOUS SYSTEM INFECTIONS…………………………………………………………………………. 10
GASTROINTESTINAL INFECTIONS…………………………………………………………………………………….. 12
SKIN AND SOFT TISSUE INFECTIONS………………………………………………………………………………….15
BONE AND JOINT INFECTIONS…………………………………………………………………………………………..20
OTHER INFECTIONS…............................................................………………......….…….….......…………............ 21
PROPHYLAXIS IN SELECTED CLINICAL SETTINGS ……………………………………….……….……….……..23
ABBREVIATIONS LEGEND CHART ………………………………………………………………….……………..…...30
REFERENCES………………………………………………………………………………………….…………..………..30
APPENDIX (CDC MALARIA TREATMENT TABLE) ………………………………………….…………………………31
Dr. Zainab A. Malik MD, MSc, FAAP. 2019
Pediatric Antibiotic Guidelines
2019
INSTRUCTIONS
1. These guidelines are based on the most recent evidence available at of the time of issue.
2. These guidelines are meant for empiric treatment - antibiotics should be modified once culture
& sensitivity data become available.
3. Check the drug interactions & antibiotic precautions/monitoring specific to your patient.
4. These guidelines are meant to serve as a guide & are not all-encompassing for various
infections.
5. Doses given here are for children < 45kg; for heavier children refer to adult dosing or maximum
daily dosing.
6. Monitor renal function for nephrotoxic antimicrobials; close monitoring required when there are
two nephrotoxic agents on board (i.e. vancomycin and gentamicin).
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 2 of 33
Pediatric Antibiotic Guidelines
2019
RESPIRATORY INFECTIONS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Mild Pneumonia Amoxicillin Clindamycin Duration: 7 days
(Outpatient) 90 mg/kg/day PO 30 mg/kg/day PO
divided Q8 - Q12hr (max divided Q8 hrs (max 1.8 Target pathogen: Streptococcus
4 g/day) g/day) pneumoniae
OR OR Clindamycin active against 72% of
S. pneumoniae (Mediclinic Dubai
Amoxicillin- Erythromycin data)
Clavulanate 40-50 mg/kg/day in 4
90 mg/kg/day of the divided doses (max 2 Oral cephalosporins inferior to
amoxicillin component in g/day as base, 3.2 g/day high-dose amoxicillin for S.
2 or 3 divided doses as ethylsuccinate) pneumoniae,
(max 4 g/day of
amoxicillin component) OR *High rates of macrolide resistance
among S.pneumoniae isolates in
Azithromycin UAE (azithromycin 48%;
10 mg/kg on Day 1, then erythromycin 53%; clarithromycin
5 mg/kg/day for 4 more 44%), therefore these agents are
days (max 500 mg on not recommended as first line.
Day 1 and 250 mg
thereafter)
Moderate Pneumonia Ampicillin (IV) Clindamycin (IV) Duration: 7 days total (including IV
>6mo of age (Inpatient) 150-200 mg/kg/day 40 mg/kg/day divided Q8 & PO therapy), or at least 48 hours
divided Q6hrs (max hrs (max 2.7 g/day) from resolution of fever and
12g/day) tachypnea (whichever is longer).
OR Target pathogen: S. pneumoniae
Ceftriaxone (IV)
50-100 mg/kg/day Q12-
Q24 hrs (max 4g/day)
OR
Cefotaxime (IV)
150mg/kg/day divided
Q8 hrs (max 8g/day)
Severe Complicated Vancomycin (IV) Vancomycin (IV) Duration: 7 days from afebrile.
Pneumonia (ICU) 40-60mg/kg/day divided (15 mg/kg/dose Q6 (max
Q6-Q 8hrs (max 4g/day) 4g/day) Target pathogens: S.
pneumoniae, S. pyogenes, S.
AND AND aureus
Ceftriaxone (IV) Levofloxacin (IV) Vancomycin for suspected MRSA
100 mg/kg/day divided ≥ 6mo and < 5 yrs: 20 in severe or life-threatening
Q12 hrs (max: 4g/day) mg/kg/day divided Q12 conditions
hrs ≥ 5yr: 10 mg/kg/day,
OR Q24 hrs (max: 500 mg) *May add coverage for atypical
pathogens (as given below) if
Cefotaxime (IV) clinically indicated.
150mg/kg/day divided
Q6hrs (max 8g/day) *Add empiric antiviral treatment for
influenza depending on the season
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 3 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Atypical Pneumonia Azithromycin (IV/PO) Target pathogens: Mycoplasma
(all locations and 10 mg/kg on day 1, pneumoniae, Legionella
severities) single dose (max: 500 pneumophila, Chlamydia.
Non-lobar, patchy, or mg/day); followed by 5
interstitial pattern on mg/kg/day once daily *Note that serological & DNA tests
CXR; insidious onset; Q24 thereafter do NOT differentiate between
low-grade of fever, (max: 250 mg/day) asymptomatic carriage or
malaise, headache, symptomatic infection with
cough; minimal Mycoplasma pneumoniae
auscultatory findings
relative to CXR. Alternatives: Clarithromycin (15
mg/kg/day div Q12) or oral
Often caused by Erythromycin (40 mg/kg/day div
respiratory viruses, but Q12). For children >7 years old,
may be caused by Doxycycline (2–4 mg/kg/day div
atypical bacterial Q12).
pathogens including For adolescents with skeletal
Mycoplasma maturity, Levofloxacin (500 mg
pneumoniae and once daily) or Moxifloxacin (400
Legionella mg once daily).
pneumophila.
Azithromycin does not treat S.
Most atypical pneumoniae or S. aureus.
pneumonia is mild and Levofloxacin has activity against
self-limited. However, S. pneumonia (98%
for disease requiring susceptibility) as well as atypical
hospitalization, bacteria, so no additional agents
consider diagnostic are needed when levofloxacin is
testing and treatment. otherwise indicated.
Whooping Cough Azithromycin (PO) Target pathogens: Bordetella
<6mo: 10mg/kg Q24hr pertussis, Bordetella parapertussis
≥6mo: 10mg/kg once on
day 1; then 5mg/kg Q24 *Duration of treatment: 5 days
for 4 days (max 500mg
on day 1, then max *Azithromycin is 1st line for infants
250mg for subsequent <1month of age.
doses)
*Close contacts that are
unimmunized or underimmunized
should have their pertussis
vaccination initiated or continued
according to age-appropriate
recommendations.
*Post-exposure prophylaxis is
recommended for all household
contacts and other close contacts
including children in childcare,
regardless of immunization status.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 4 of 33
Pediatric Antibiotic Guidelines
2019
EAR, NOSE AND THROAT INFECTIONS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Acute otitis media Amoxicillin (PO) Azithromycin (PO) Target pathogens: S pneumoniae,
(AOM) 80-90mg/kg/day div Q12 10 mg/kg on day 1, non-typeable Haemophilus
(max 1000mg/dose) single dose (max: 500 influenzae, and Moraxella
mg/day); followed by 5 catarrhalis.
OR mg/kg/day once daily
Q24 thereafter * High dose amoxicillin is the
Amoxicilin-Clavulanate (max: 250 mg/day) preferred 1st line agent for AOM
(Augmentin ES-600) due to its safety & high efficacy. It is
90mg/kg/day div Q12 OR active against 94% of S.
(dose based on pneumoniae isolates (Mediclinic
amoxicillin component) Clarithromycin (PO) Dubai data).
15 mg/kg/day div Q12)
Failure of initial *Non-first line antibiotics vary in
antibiotic treatment For children with mild, their efficacy against AOM
after 48-72hrs: non-anaphylactic pathogens.
reaction to penicillin
Ceftriaxone (IM/IV) (maculopapular rash), *For children who have received
50mg/kg Q24 for 1-3 the following may be amoxicillin in the preceding 30
days (max 1g/dose) used: days, those with conjunctivitis or
concern about infection with H.
Cefdinir (PO) influenzae or M. catarrhalis,
14mg/kg/day div Q12-24 treatment should be initiated with
(max 600mg/day) amoxicillin-clavulanate.
Cefuroxime (PO) *Duration of therapy:
30mg/kg/day div Q12 10 days: children <2yr & those with
(max 1000mg/day) severe symptoms;
7 days: children 2-5yr with
moderate symptoms;
5-7 days: children >6yr with mild to
moderate symptoms.
Clinicians should NOT prescribe
daily prophylactic antibiotics to
reduce the frequency of episodes of
AOM in children with recurrent
AOM.
Clinicians may offer tympanostomy
tubes/grommets for recurrent AOM
(3 episodes in 6 months or 4
episodes in 1 year, with 1 episode
in the preceding 6 months).
Otitis externa Cipro HC (otic drops) Target pathogens: Pseudomonas
(“swimmer’s ear”) 3 drops BID x7 days to aeruginosa, S. aureus
affected ear
* Cipro HC (ciprofloxacin 0.2% and
hydrocortisone 1%) presferred
because of fewer side effects than
Cortisporin (neomycin 0.35%,
polymyxin B 10,000 units/mL, and
hydrocortisone 0.5%)
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 5 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line TherapyType 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Cervical lymphadenitis Amoxicillin- Clindamycin (PO) Target pathogens depend on
Clavulanate (PO) 30mg/kg/day div Q6-Q8 acuity & location of adenitis:
25-45mg/kg/day div Q12 (max 1.8g/day)
(max 1.75g/day. Dose *Acute bilateral: Rhinovirus,
based on amoxicillin Epstein-Barr virus (EBV),
component) Cytomegalovirus (CMV), Herpes
simplex virus (HSV), Adenovirus,
OR Enterovirus,
Mycoplasma pneumonia, Group A
Clindamycin (PO) Streptococcus, Influenza
30mg/kg/day div Q6-Q8 *Acute unilateral:
(max 1.8g/day) S.aureus, Group A Streptococcus,
Anaerobes
OR *Chronic unilateral:
Mycobaterium tuberculosis
Cephalexin (PO) Non-tuberculous mycobacteria
25-50 mg/kg/day div Q6- (NTM) Bartonella henselae (Cat-
Q12 (max 4 g/day) dose scratch disease)
depends on severity of *Chronic bilateral: Epstein-Barr
adenitis. virus Cytomegalovirus
OR *Amoxicllin-Clavulanate &
Clindamycin provide anaerobic
Cefadroxil (PO) coverage & may be preferred to
30 mg/kg/day div Q12- other listed options if there is
Q24 (max 2 g/day) concern for anaerobic infection i.e.,
poor oral hygiene or dental caries.
Streptococcal Amoxicillin (PO) Clindamycin (PO) Target pathogen: Streptococcus
pharyngitis 50mg/kg Q24 for 10 7mg/kg/dose Q8 for 10 pyogenes (GAS)
OR days (max 1000mg). days (max 300mg/dose)
Scarlet fever Alternate 25mg/kg/dose *Resistance of GAS to
Q12 (max 500mg Q12) OR Azithromycin & Clarithromycin is
well-documented and varies
OR Azithromycin (PO) geographically. Hence these are
12mg/kg Q24 (max not considered first-line agents.
Penicillin V (PO) 500mg) for 5 days
Children 250mg Q12; *Cephalexin & Cefadroxil (1st
Adolescents 250mg Q8 OR generation cephalosporins) can
for 10 days also be used as alternatives;
Clarithromycin (PO) however, avoid in patients with type
OR 15mg/kg/day div Q12 1 hypersensitivity to penicillin.
(max 250mg/dose) for
Benzathine penicillin G 10 days.
(single dose IM)
<27kg: 600,000 units
≥27kg: 1.2 million units
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 6 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Acute bacterial Amoxicilin-Clavulanate Cefixime (PO) Target pathogens: S pneumoniae,
sinusitis (Augmentin ES-600) 8mg/kg/day div Q12-24 nont-ypeable Haemophilus
90mg/kg/day div Q12 influenzae, and Moraxella
(dose based on AND catarrhalis.
amoxicillin component)
Clindamycin (PO) * Consider CT or MRI with contrast
Failure of initial 30-40mg/kg/day div Q8 of the paranasal sinuses whenever
antibiotic treatment orbital or CNS complications of
after 48-72hrs: OR acute bacterial sinusitis are
suspected.
Ceftriaxone (IM/IV) Levofloxacin (PO)
50mg/kg Q24 x1-3 days 10-20mg/kg/day div Q12 * Macrolides, trimethoprim-
(max 2g/day). Followed (max 500mg/ day) sulfamethoxazole, oral 2nd and 3rd
by appropriate outpatient generation cephalosporins are not
therapy. recommended for empiric therapy
due to high rates of resistance
among S. pneumoniae and H.
influenzae.isolates.
*No evidence to support
decongestants, antihistamines or
nasal irrigation in children
(Cochrane review).
*Duration of therapy: 7 days after
resolution of symptoms, minimum
of 10 days.
Acute mastoiditis No prior history of Aztreonam (IV) Target pathogens: Streptococcus
AOM or recent 30 mg/kg/dose Q6 (max pneumoniae, Streptococcus
antibiotic use: 2g/dose) pyogenes, and Staphylococcus
Vancomycin (IV) aureus (including MRSA).
15mg/kg/dose Q6 (max AND
1g/dose) * Pseudomonas aeruginosa is a
Vancomycin (IV) consideration for children with a
Recurrent AOM (within 15mg/kg/dose Q6 (max history of recurrent acute otitis
6 months) or recent 1g/dose) media
antibiotics:
*Diagnostic clinical features:
Vancomycin (IV) 1. Postauricular erythema,
AND tenderness, swelling, fluctuance
Ceftazidime (IV) or mass;
50mg/kg/dose Q8 2. Protrusion of the auricle;
(max 2g/dose) 3. Otalgia;
OR 4. Fever.
Cefepime (IV) *Consider early referral to ENT due
50mg/kg/dose Q8 to risk of intracranial or extracranial
(max 2g/dose) complications & incomplete
OR response to antimicrobial therapy
PipercillinTazobactam alone without drainage.
(IV) *Switch to oral antibiotics after
300 mg/kg/day div Q6- sustained clinical improvement &
8hr (max 16g/day of based on culture/sensitivity results.
piperacillin component) TOTAL duration of antibiotic
therapy is 4 weeks.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 7 of 33
Pediatric Antibiotic Guidelines
2019
OPHTHALMIC INFECTIONS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Infectious Erythromycin Target pathogens: Viruses, esp.
Conjunctivitis ophthalmic ointment Adenovirus, are the most common
QID 5-7days cause of conjunctivitis. Bacterial
pathogens include: S. aureus, S.
OR pneumoniae, H. influenzae, &
Moraxella catarrhalis.
Quinolone ophthalmic
drops (ciprofloxacin, *Contralateral eye involvement is
moxifloxacin, ofloxacin) common, esp. in younger children.
1-2 drops QID 5-7days
*Contact lens wearers with
conjunctivitis are at risk of
Pseudomonas keratitis. Advise to
discontinue contact lens use
immediately & refer to
ophthalmologist.
*Red flag signs requiring immediate
referral to an ophthalmologist:
1. Reduction of visual acuity
2. Ciliary flush
3. Photophobia
4. Severe foreign body sensation
5. Corneal opacity
6. Fixed pupil
7. Severe headache & nausea
Periorbital (preseptal) Clindamycin (PO) Target pathogens: S.
cellulitis: OUTPATIENT 30-40 mg/kg/day div Q6 pneumoniae,
TREATMENT or Q8 (max 1.8 g/day) S. aureus, MRSA, non-typeable H.
.influenzae, other streptococci
AND
*MRSA prevalence ~37%
Amoxicillin- (Mediclinic Dubai Data). Consider
Clavulanate (PO) empiric coverage against MRSA
45 mg/kg/day div Q12 when treating preseptal cellulitis.
(use 90mg/kg/day div
Q12 dosing for severe *Clindamycin is active against 80%
infections) of MRSA isolates (Mediclinic Data,
Dubai) hence provides good
OR empiric coverage for MRSA.
However, it does not cover non-
Cefdinir (PO) typeable H.influenzae, and should
7 mg/kg/dose Q12 (max be used in combination with either
600 mg/day) of the two agents.
*Total duration of therapy 10 days
or resolution of symptoms.
*If no clinical improvement within
24-48hrs of starting outpatient
therapy, admit & treat as for orbital
cellulitis.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 8 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Orbital cellulitis Vancomycin (IV) Vancomycin (IV) Target pathogens: S.
15 mg/kg/dose Q6 or Q8 15 mg/kg/dose Q6 or Q8 pneumoniae, H.influenzae,
(max 4g/day) (max 4g/day) M.catarrhalis, S.aureus, MRSA,
anaerobes, Group A streptococci
AND AND (consider Mucorales or Aspergillus
in immunocompromised patients)
Cetriaxone (IV) Ciprofloxacin (PO/IV)
50mg/kg/dose Q24 20-30mg/kg/day div Q12 *Total duration of therapy 2-3
Give 50mg/kg Q12 if (max 800mg/day IV or weeks (up to 4 weeks for severe
intracranial extension 1.5g/day PO) infection).
suspected.
(max 4g/day). *Obtain blood cultures before
starting antibiotic therapy (can be
OR positive in up to 33% of children
with orbital cellulitis).
Cefotaxime(IV)
150-200mg/kg/day div *Most patients on IV therapy who
Q8 (max 12g/day) are able to take PO meds should
be switched to PO therapy after
sustained clinical improvement.
*If a methicillin-susceptible strain of
S. aureus (MSSA) is recovered
from cultures of blood, sinuses,
orbital or subperiosteal aspirates,
treatment should be changed from
vancomycin to fluloxacillin because
this is more rapidly bactericidal for
MSSA than vancomycin.
*In patients with suspected
intracranial extension, or those with
orbital cellulitis secondary to
chronic sinusitis or dental abscess,
metronidazole (30 mg/kg/day div
Q6 PO/IV) should be added for
anaerobic coverage.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 9 of 33
Pediatric Antibiotic Guidelines
2019
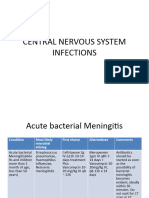
CENTRAL NERVOUS SYSTEM INFECTIONS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
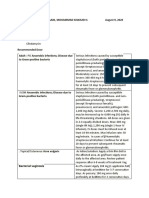
Bacterial meningitis Vancomycin (IV) Target pathogens: E. coli, Listeria
(infants >1mo and 60 mg/kg/day div Q6 monocytogenes, Group B
children) (max 4 g/day) streptococcus (<3mo);
Streptococcus pneumoniae,
AND Neisseria meningitides (all ages)
Ceftriaxone (IV) *Consider Haemophilius influenzae
100 mg/kg/day div Q12 B (HiB) in an unvaccinated or
(max 4 g/day) incompletely vaccinated child.
OR *Obtain blood cultures on
admission & a formal hearing
Cefotaxime (IV) assessment prior to discharge.
300 mg/kg/day div Q6 or
Q8 (max 12 g/day) *Dexamethasone treatment
decreases the risk of hearing loss
in children with HiB meningitis only;
no impact on hearing loss from
other aetiologies of bacterial
meningitis. However, it does NOT
decrease the risk of neurological
sequelae or mortality from bacterial
meningitis & is not routinely
recommended in children.
*If there is an increased risk of
meningitis with HiB (i.e.
unvaccinated child),
dexamethasone should be given
BEFORE or WITH the first dose of
antibiotics. If >1hr has elapsed
since the antibiotic dose,
dexamethasone is unlikely to have
any significant benefit.
*Do not delay empiric antibiotic
therapy in a child with suspected
meningitis.
*Add aminoglycosides to the
empiric regimen if gram negative
rods are seen on CSF gram stain or
suspected clinically i.e. penetrating
head trauma.
*Therapy can be modified once
final CSF culture/sensitivity results
are available.
*Chemoprophylaxis for selected
contacts of patients with meningitis
due to H. influenzae or N.
meningitides.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 10 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Bacterial meningitis, *Duration of treatment (full antibiotic
continued. course should be given IV):
Group B Strep: 14 days
L. monocytogenes: 14-
21days
Gram-negative rod: 21days
N. meningitidis: 5-7 days
S. pneumoniae: 10-14 days
H. influenzae: 7-10 days
*Children with H. influenzae or
N. meningitides meningitis treated
with antibiotics other than
cefotaxime or ceftriaxone do not
clear the organism from their
nasopharynx. They require
antimicrobial therapy to eradicate
nasopharyngeal carriage before
hospital discharge to prevent
transmission of the organism to
contacts.
HSV encephalitis Acyclovir (IV) Target pathogens: Herpes simplex
virus (HSV) 1 and 2.
>28 days to <3 months
20 mg/kg/dose Q8 *Duration of treatment: 21 days
≥3 months to <12 years *Glucocorticoids are NOT indicated
10-15 mg/kg/dose Q8 in the treatment of HSV
encephalitis.
≥12 years
10 mg/kg/dose Q8 *Repeat CSF towards the end of
treatment is advised. If HSV PCR
remains positive, give additional
days of acyclovir IV until CSF HSV
*Infants with HSV PCR clears up.
encephalitis should
receive daily acyclovir *MRI is the neuroimaging modality
prophylaxis (300mg/m² of choice because it is more
PO Q8 for 6mo) after sensitive and specific for
completing 21 days of IV encephalitis than CT.
acyclovir to prevent
recurrences & improve *Temporal lobe localization on MRI
developmental is highly specific for HSV (not
outcomes. sensitive).
*At least 66% of children &
adolescents who survive HSV
encephalitis have some form of
neurologic debility (i.e. seizure
disorder, global developmental
delay, residual hemiplegia).
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 11 of 33
Pediatric Antibiotic Guidelines
2019
GASTROINTESTINAL INFECTIONS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Clostridium difficile Initial episode, non- *Due to the high prevalence of
severe: asymptomatic carriage of toxigenic
Making a diagnosis of Metronidazole (PO) C. difficile in infants, testing for CDI
Clostridium difficile 7.5mg/kg/dose Q6 or Q8 should never be routinely
infection (CDI) requires for 10 days. recommended for neonates or
the presence of both: (max 500mg/dose) infants ≤12 months of age with
Diarrhoea AND diarrhoea.
C.dificile toxin. OR
*Clostridium difficile testing should
(NOTE: Stool PCR Vancomycin (PO) not be routinely performed in
positive for C. difficile 10mg/kg/dose Q6 for 10 children with diarrhoea who are 1–2
without presence of days years of age unless other infectious
antigen is not diagnostic (max 125mg/dose) or non-infectious causes have been
of CDI) excluded.
Initial episode,
severe/fulminant: *Do not perform repeat testing
Vancomycin (PO/PR) (within 7 days) during the same
10mg/kg/dose Q6 for 10 episode of diarrhoea & do not test
days (max 125mg/dose) stool from asymptomatic patients,
except for epidemiological studies.
WITH
*There are insufficient data to
Metronidazole (IV) recommend screening for
10mg/kg/dose Q8 for 10 asymptomatic carriage or placing
days asymptomatic carriers on contact
(max 500mg/dose) precautions.
*Continue contact precautions for at
least 48 hours after diarrhea has
resolved.
*Hand hygiene with soap & water
has greater efficacy for spore
removal than hand washing with an
alcohol-based hand rub.
Giardiasis First-line agent: Target pathogen: Giardia
Tinidazole (PO) duodenalis (also known as
Age ≥3 years: 50 mg/kg G.lamblia or
orally, single dose G. intestinalis)
(maximum dose 2g/day)
*Transmission through food, water
OR or faeco-oral route.
Second-line agent:
Metronidazole (PO) *Patients whose symptoms
15 mg/kg/day div Q8, 5- resolved for weeks or months prior
7 days (max 250 to recurrence may be retreated with
mg/dose) the same antimicrobial agent.
*Stool tests to rule out co-infection
with other intestinal parasites.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 12 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Amoebiasis: First line: Target pathogen: Entamoeba
Acutely symptomatic histiolytica (trophozoites)
Metronidazole (PO)
35-50mg/kg/day divided *Stool microscopy will not
Q8 for 10 days. differentiate between E. histiolytica
from non- pathogenic E. dispar.
Alternative: Request stool E. histiolytica antigen
test.
Tinidazole (PO)
50mg/kg PO Q12 for 3 *If severe intestinal disease,
days (max 2g/dose). consider extra-intestinal infection
Only for children >3yr. (liver abscess).
Either regimen should be *Metronidazole is well-absorbed
followed by an from the GI tract; IV therapy offers
intraluminal cysticide no significant advantage as long as
(see below) the patient can take oral
medication.
*Shorter duration or lower doses of
metronidazole are not
recommended for treating
amoebiasis.
* After completing the course of
treatment for acute amoebiasis,
patients should be treated with an
intraluminal cysticide to prevent
relapse, even if no cysts are seen
on stool microscopy.
Amoebiasis: First line: Target pathogen: Entamoeba
Asymptomatic cyst histiolytica (cysts)
excreter Paromomycin (PO)
25-35mg/kg/day divided *All asymptomatic cysts excreters
Q8 for 10 days. should be treated to prevent the
risk of invasive infection or
OR transmission to household contacts.
Iodoquinol (PO)
30-40mg/kg/day div Q8
for 20 days (max
1950mg/day)
Alternative:
Diloxanide furoate (PO)
20mg/kg/day div Q8 for
10 days (max 1.5g/day)
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 13 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Hookworm Albendazole (PO) Target pathogens: Necator
12-23mo: 200mg single americanus, Ancylostoma
dose duodenale
>2yr: 400mg single dose
* Dermal penetration of the skin
OR frequently produces a focal pruritic
maculopapular eruption at the site
Mebendazole (PO) of larval penetration.
>2yr: 100mg BID x3
days (Repeat course *Albendazole therapy is superior to
after 3 weeks). & more effective than Mebendazole
therapy for hookworm infection.
Roundworm Mebendazole (PO) Target pathogen: Ascaris
>2yr: 100mg single dose lumbricoides
OR *Intestinal obstruction, biliary
obstruction or eosinophilic
Albendazole (PO) pulmonary infiltrates due to
12-23mo:200mg single migration of larvae or adult worms.
dose
>2yr: 400mg single dose *Oral or nasogastric regurgitation of
large adult worms in young
children.
*Repeat dosing is not necessary for
roundworm infections.
Pinworm Mebendazole (PO) Target pathogen: Enterobious
>2yr: 100mg single vermacularis
dose. May repeat dose
after 2-3 weeks; OR *Self-oral re-infection is common in
children, from eggs trapped under
Albendazole (PO) fingernails during anal itching.
12-23mo: 200mg PO x1
>2yr: 400mg PO x1 *If >1 infected in the household,
(Repeat dose after 2 wk) treat all household members.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 14 of 33
Pediatric Antibiotic Guidelines
2019
SKIN AND SOFT TISSUE INFECTIONS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Tinea capitis (hair) First-line: Target pathogens: Trichophyton,
Microsporum, and Epidermophyton
Griseofulvin- not (dermatophyte fungi)
available in the UAE
*Acquired through direct contact
Alternative: with an infected individual or
through infected formites.
Terbinafine (PO)
10 to 20 kg: 62.5 mg *Household members of an
Q24 for 4-6 weeks individual diagnosed with tinea
capitis should be physically
20 to 40 kg: 125 mg examined for signs of tinea capitis
Q24 for 4-6 weeks and should be treated
simultaneously if tinea capitis is
>40 kg: 250 mg Q24 for detected.
4-6 weeks
*Asymptomatic carriers of
dermatophytes may serve as
reservoirs for recurrent infection.
Hence it is recommended that all
household members of a patient
with tinea capitis use an antifungal
shampoo for two to four weeks.
*Cats or dogs (especially kittens
and puppies) may be reservoirs for
infection and may be symptomatic
or asymptomatic. If there is an
outbreak or recurrence of tinea in a
family, the pet should be evaluated
by a veterinarian.
*Topical therapy ALONE has no
role in the treatment of tinea capitis.
*There is limited data for terbinafine
in children <4yr of age.
*Baseline LFTs before starting
treatment with terbinafine; repeat
LFT and FBC for treatment beyond
6 weeks.
*Fluconazole & itraconazole may
be used as second-line agents but
have lower efficacy.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 15 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Toxic Shock Syndrome MRSA Clindamycin (IV) Target pathogens:
Staphylococcus aureus (MSSA &
Clindamycin (IV) AND MRSA) most common.
25-40 mg/kg/day div Q8 Streptococcus pyogenes (less
Vancomycin (IV) common).
AND
*Since this is a toxin-mediated
Vancomycin (IV) infection, a protein-synthesis
40 mg/kg/day div Q6 inhibitor (clindamycin or linezolid)
should always be a part of the
MSSA or GAS treatment regimen
Clindamycin (IV) *In patients with S.aureus TSS,
25-40 mg/kg/day div Q8 nasal culture to evaluate carrier
state. If positive, requires nasal
AND mupirocin BID x5 days
Flucloxacillin (IV) *Treatment duration typically 1-2
25-50 mg/kg/day div Q6- weeks
Q8
*No established role of IVIG, but
may be considered in severe
infection with hypotension
refractory to fluids & vasopressors.
However, there are no controlled
trials.
Scabies Permethrin 5% cream Target pathogens: Sarcoptes
Massage thoroughly into scabiei (mite)
the skin from the neck to
the soles of the feet, *Transmission occurs through
including scalp in infants, direct & prolonged skin-to-skin
& wash off after 8-14 contact with an infected individual.
hours. Repeat treatment
after 1-2 weeks.
*Indirect transmission through
Ivermectin (PO) formites or animals does not occur.
<15kg: not
recommended.
>15kg: 200 mcg/kg PO *Infants and children may have
x1 dose. Repeat dose involvement of their scalp, hands &
after 1-2 wks. feet in addition to the typical sites of
infection.
*Bacterial superinfection especially
with Streptococcus pyogenes
(GAS) is common & should be
promptly treated.
*Children may return to daycare or
school as soon as the first
treatment is completed.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 16 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Scalded Skin Flucloxacillin (IV) Target
Syndrome 25-50 mg/kg/day div Q6- pathogens: Staphylococcus
(Ritter Disease) Q8 aureus (MSSA & MRSA)
OR *Blisters are sterile
Cefazolin (IV) *Obtain cultures from blood, nares,
50 mg/kg/day div Q8 peri-anal area & umbilicus in
(max 6g/day) neonates.
AND *Gentle pressure applied to the skin
results in separation of the upper
Vancomycin (IV) epidermis (Nikolsky’s sign)
40 mg/kg/day div Q6
*Since cleavage is intra epidermal,
scarring does not occur
Bite wounds Amoxicillin- Ciprofloxacin (PO) Target pathogens:
Clavulanate (PO) 20-30mg/kg/day div Q12 Staphylococcus aureus,
(max 750mg/dose) Streptococcus pyogenes (all bites).
45 mg/kg/day div Q12 Anaerobes, Eikenella corrodens
(use 90mg/kg/day div AND (human bites). Pasteurella
Q12 dosing for severe multicoda, Capnocytophaga sp.
infections) Metronidazole (PO) (dog & cat bites)
30mg/kg/day div Q6-Q8
(max 4g/day) *Bartonella henselae (cat-scratch
disease) risk following cat bites.
*Consider tetanus & rabies
prophylaxis (see prophylaxis
section)
*Human bites: There is risk of
hepatitis B transmission. Check
Hepatitis B vaccination status of
victim. Hepatitis C & HIV
transmission risk very low.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 17 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Head lice First-line: Target pathogen: Pediculus capitis
Permethrin 1% *Direct contact with the head of the
cream/lotion infected person is the primary mode
Apply to dry hair & wash of transmission. Lice do not jump,
off after 10 minutes. fly or use pets as vectors.
Repeat another
application after 9 days. *Household members should be
Can be used in children examined and treated if infested;
2 months. bedmates should be treated
prophylactically.
OR
*Children should NOT be excluded
Malathion 0.5% from school if presence of lice/nits
Apply to dry hair & wash is noted, since these are typically
off after 8-12hrs. present for weeks before detection.
Reapplication not
needed unless live lice *Permethrin 5% has no added
are seen. Not indicated efficacy over permethrin 1%
in children 2 years.
Alternative: *Cetaphil cleanser is an effective
alternative treatment for head lice
Ivermectin (PO) with a cure rate of up to 97%
200mcg/kg single dose (Nuvo® Method):
indicated in children
>15kg Apply throughout to dry hair.
After all the hair is wet, wait 2
minutes for Cetaphil to soak in.
Comb out as much excess
cleanser as possible.
Blowdry the child’s hair
thoroughly.
Dried Cetaphil will smother the
lice. Leave it in for at least 8
hrs.
In the morning, wash off with
shampoo.
Repeat this process after 1 and
2 weeks.
Kerion Treatment same as Target pathogens: Trichophyton,
tinea capitis Microsporum, and Epidermophyton
(dermatophyte fungi)
AND
*Kerion is an auto-eczematization
Systemic reaction (“id” reaction) secondary to
glucocorticoids (eg, a scalp deramatophye infection.
prednisolone 0.5 to 1 The pathogenesis involves an
mg/kg PO x 1 week) for immunologic reaction to fungal
patients with severe antigens similar to a
inflammation. delayed-type hypersensitivity
response.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 18 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Skin and soft tissue OUTPATIENT: OUTPATIENT: Target pathogens: Streptococcus
infections (SSTIs) pyogenes, and Staphylococcus
Flucloxacillin (PO) Clindamycin (PO) aureus (including MRSA).
Children <2 years: 30-40 mg/kg/day Q6 or
62.5-125mg Q 6 Q8 (max 1.8 g/day) *If MRSA is suspected, add
Children 2 -10 years: --------------- clindamycin to outpatient regimen,
125- 250mg Q6 or vancomycin to inpatient regimen.
Children >10 years: INPATIENT:
250-500mg Q6 *Duration of therapy 5-7 days for
Clindamycin (IV) uncomplicated SSTI.
OR 40 mg/kg/day, divided
Q8 (max 2.7 g/day) *In fluctuant SSTI with abscess size
Cephalexin (PO) >4cm, drainage is the mainstay of
25-50mg/kg/day div Q12 AND therapy & results in more rapid
symptom resolution than antibiotics
------------- Vancomycin (IV) alone.
INPATIENT: 15 mg/kg/dose Q6
(max 4g/day) *Flucloxacillin is active against
Flucloxacillin (IV) 100% of S.aureus isolates
25-50 mg/kg/day div Q6- (Mediclinic Dubai data data)
Q8
AND
Vancomycin (IV)
15 mg/kg/dose Q6
(max 4g/day)
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 19 of 33
Pediatric Antibiotic Guidelines
2019
BONE AND JOINT INFECTIONS
Infection First Line Therapy β-lactam Allergy Comments
Type 1 hypersensitivity:
Urticaria or anaphylaxis
Septic arthritis Vancomycin (IV) Target pathogens: S.aureus
40-60 mg/kg/day div Q8 (MRSA & MSSA)- all ages, Group
(max dose 4g/day) B Streptococcus & gram-negative
rods (infants <3mo), Group A
AND Streptococcus, S.pneumoniae,
H.influenza (type B & non-
Flucloxacillin (IV) typeable), Kingella kingae
25-50 mg/kg/day div Q6-
Q8 *Surgical drainage is essential!!
OR *Duration of therapy:
S. aureus: 3 weeks (minimum)
Cefazolin (IV) S. pneumoniae,GBS,GAS: 2-3 wks
100 mg/kg/day div Q8 K.kingae,N.meningitidis,H.influenza
(max 6g/day) e & gram-negative: 2-3 weeks
Culture-negative arthritis: 2 weeks
*MRSA prevalence ~37%
(Mediclinic Dubai Data), hence
vancomycin should be a part of the
empiric regimen.
*Flucloxacillin is superior to
vancomycin for MSSA infection.
Osteomyelitis Vancomycin (IV) Target pathogens: S.aureus
40-60 mg/kg/day div Q8 (MRSA & MSSA)- predominant
(max dose 4g/day) pathogen
AND *Obtain blood cultures
Flucloxacillin (IV) *Duration of therapy: 4 weeks or
25-50 mg/kg/day div Q6- until normalization of inflammatory
Q8 markers (whichever is longer)
OR *MRSA prevalence ~37%
(Mediclinic Dubai Data), hence
Cefazolin (IV) vancomycin should be a part of the
100 mg/kg/day div Q8 empiric regimen.
(max 6g/day)
*Flucloxacillin is superior to
vancomycin for MSSA infection.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 20 of 33
Pediatric Antibiotic Guidelines
2019
OTHER INFECTIONS
Infection First Line Therapy β-lactam Allergy Comments
Type 1 hypersensitivity:
Urticaria or anaphylaxis
Malaria treatment *See below CDC Malaria N/A Target pathogens: P. falciparum,
Treatment Table* P. vivax, P. ovale, P. malariae, and
P. knowlesi.
*Young children, especially those
<5 years of age, are particularly
prone to rapid deterioration and
experience higher rates of severe
and cerebral malaria than adults.
*A single negative film or antigen
does not exclude malaria - thick
and thin films should be repeated
with fever spikes until positive test
or 3 negative films.
*If a person develops malaria
despite taking prophylaxis, that
medicine should not form a part of
the treatment regimen- use another
regimen instead.
*All cases of P. vivax, P. ovale or
unknown species should have liver
hypnozoite eradication treatment.
All patients should undergo G6PD
deficiency screening prior to the
administration of primaquine.
Influenza Oseltamivir (Tamiflu) Target pathogens: Influenza A
and B
2wk-11mo: 3mg/kg PO
BID x5 days * Oral oseltamivir is approved by
the FDA for treatment of acute
1-12yr, <15kg: 30mg uncomplicated influenza within 2
PO BID x5 days days of illness onset in persons 14
days and older, and for
1-12yr, 15-23kg: 45mg chemoprophylaxis in persons 1
PO BID x5 days year and older.
1-12yr, 23.1-40kg: *Although not part of the FDA-
60mg PO BID x5 days approved indications, use of oral
oseltamivir for treatment of
1-12yr, >40kg: 75mg influenza in infants less than 14
PO BID x5 days days old, and for chemoprophylaxis
in infants 3 months to 1 year of age,
13yr & older: 75mg PO is recommended by the CDC and
BID x5 days the American Academy of
Paediatrics.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 21 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Typhoid Ceftriaxone (IV) Ciprofloxacin (PO/IV) Target pathogen: Salmonella typhi
100mg/kg Q24 20-30mg/kg/day div Q12
(max 4g/day) (max 800mg/day IV or *Obtain baseline blood & stool
1.5g/day PO) cultures
OR *Total duration of therapy 10-14
days
Azithromycin (PO/IV)
10mg/kg Q24 x3-7d *Antibiotics can be switched to oral
once patient has defervesced &
blood cultures have cleared. Choice
of PO antibiotic based on
culture/sensitivity data.
*Note: high rates of ampicillin,
TMP-SMX & fluoroquinolone
resistance in S.typhi isolates
globally.
*Obtain stool cultures x3 AFTER
72hrs of completing total antibiotic
course to determine if patient is a
chronic carrier. Exclude from
swimming pools until all stool
cultures are negative off antibiotics.
Urinary Tract Infection Cefuroxime (PO) Target pathogens: E. coli
20-30mg/kg/day div Q12
(max 1g/day) *Duration of treatment: 7 days
OR *Probability of culture-positive UTI
is 90% if urine is positive for BOTH
Amoxicillin- leukocyte esterase & nitrites; and
Clavulanate (PO) only 8% if both are negative.
25-45mg/kg/day div Q12
(max 1.75g/day) *Cefuroxime is active against 89%,
Amoxicillin-clavulanate is active
OR against 82% & nitrofurantoin is
active against 95% of E. coli
Nitrofurantoin (PO) isolates (Mediclinic Dubai data)
5-7mg/kg/day div Q6
*Nitrofurantoin has limited renal
penetration. Avoid in pyelonephritis.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 22 of 33
Pediatric Antibiotic Guidelines
2019
PROPHYLAXIS IN SELECTED CLINICAL SETTINGS
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Malaria All Plasmodium species N/A Atovaquone-Proguanil
in chloroquine-resistant *Start 1-2 days before exposure &
areas (drugs of choice): continue for 7 days after leaving
malaria- endemic area.
Atovaquone-
Proguanil (PO) *Cannot be used during pregnancy,
5-8kg: ½ peds tab/d 9- breastfeeding or children <5kg.
10kg: ¾ peds tab/d 11-
20kg: 1 peds tab/d 21- Doxycycline
30kg: 2 peds tab/d *Start 1-2 days before exposure &
31-40kg: 3 peds tab/d continue for 4 weeks after leaving
>40kg: 1 adult tab/d malaria-endemic area.
*Not recommended for children
OR <8yrs or pregnant women.
*Increases sun sensitivity (use
Doxycycline (PO) sunscreens).
2mg/kg/d (max 100mg/d)
Mefloquine
OR *Once weekly dosing. Start 2
weeks before exposure & continue
Mefloquine (PO) for 4 weeks after leaving malaria-
≤9kg: 5mg/kg once/ endemic area.
week *Not recommended for patients with
9-19kg: ¼ tab once/ cardiac conduction defects, seizure
week disorder or neuropsychiatric
>19-30kg: ½ tab illnesses.
once/week
>31-45kg: ¾ tab Chloroquine
once/week *Cannot be used in areas with
>45kg: 1 tab once/ week chloroquine or mefloquine
resistance.
All Plasmodium species *Once weekly dosing. Start 2
in chloroquine-sensitive weeks before exposure & continue
areas (drug of choice): for 4 weeks after leaving malaria-
endemic area.
Chloroquine *May exacerbate psoriasis.
phosphate (PO)
0.5mg/kg base once/wk.
(max 300mg base)
Surgical Site Infection *See SSI prevention Target pathogens: Streptococci.
(SSI) prevention policy S. aureus and gram-negative rods.
*Narrow-spectrum antibiotics i.e.,
Cefazolin, offer better coverage &
reduced risk of antibacterial
resistance than broad-spectrum
alternatives.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 23 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Influenza Tamiflu (Oseltamivir) Target pathogens: Influenza A
3-11mo: and B
3mg/kg PO QD x10 days * Oral oseltamivir is approved by
(full term infants only; the FDA for chemoprophylaxis in
per CDC, give persons 1 year and older.
throughout exposure
period & x10 days after *Although not part of the FDA-
last known exposure to approved indications, use of oral
confirmed case) oseltamivir for chemoprophylaxis in
infants 3 months to 1 year of age, is
1-12yr, <15kg: 30mg recommended by the CDC and the
PO QD x10 days American Academy of Paediatrics.
1-12yr, 15-23kg: 45mg *If a child is younger than 3 months
PO QD x10 days old, use of oseltamivir for
chemoprophylaxis is not
1-12yr, 23.1-40kg: recommended unless the situation
60mg PO QD x10 days is judged critical due to limited data
in this age group.
1-12yr, >40kg: 75mg
PO QD x 10 days *Per CDC, give x10 days after
household exposure; for x7 days
13yr & older: 75mg PO after non-household exposure and
QD x 10 days x14 days for institutional settings.
Cochlear Implant *Children should receive the full
course of HiB & PCV13 vaccination
*Children >2yr of age who have
completed the full course of PCV13
vaccination should receive a single
dose of PPSV23 vaccine.
*Second dose of PPSV23 is NOT
recommended unless the child has
an underlying immunological issue.
*Cochlear implant candidates or
recipients 6-18 years of age who
have received a full series of PCV7
followed by PPSV23 should be
given a single dose of PCV13.
*Annual influenza vaccination for
the child & all household contacts.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 24 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Rheumatic fever First-line: Azithromycin (PO) Target pathogen: Streptococcus
27kg: 5mg/kg QD pyogenes (GAS)
Penicillin G (IM) (max 250mg)
every 28 days >27kg: 250mg QD *IM penicillin is the preferred
27kg: 600,000 units regimen for secondary prevention.
>27kg: 1.2million units Oral medications are considered
second line.
Alternative:
*Shorter interval 21 days is
Penicillin V (PO) preferred for patients with
250mg BID (all weights) breakthrough RF despite 28 day
dosing.
*Erythromycin is an acceptable
alternative to azithromycin,
however, there are more GI side-
effects.
Needle stick injury *See Needle Stick Injury Target pathogens: Hepatitis B,
Policy Hepatitis C, HIV
Bacterial meningitis Neisseria meningitidis: Target pathogens: Streptococcus
pneumoniae, Neisseria
Ceftriaxone (IM) meningitides (all ages),
<15yr: 125mg x1 dose H.influenzae type B
>15yr: 250mg x1 dose
*Antimicrobial chemoprophylaxis
H.influenzae type B: should be initiated as soon as index
case is diagnosed to provide
Rifampin (PO) maximum benefit.
20mg/kg Q24 x4 days
(max 600mg/dose) *Prophylaxis is not indicated for
non-B H.influenzae infection.
*No role of prophylaxis for
S.pneumoniae meningitis
Whooping cough Azithromycin (PO) Target pathogen: Bordetella
Infants 0-6mo: 10mg/kg pertussis
QD
Infants ≥6mo & children: *Offer prophylaxis to close contacts
10mg/kg QD on Day1; of index patient with diagnosed
5mg/kg QD on Days2-5. whooping cough.
OR *Duration: Azithromycin 5 days;
Clarithromycin 7 days.
Clarithromycin (PO)
15mg/kg/day div Q12 *Clarithromycin is not
recommended in infants <1mo.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 25 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Asplenia Target pathogens: Streptococcus
pneumoniae (predominant) but also
Haemophilus influenzae &
Neisseria meningitidis.
*Population at risk of fulminant
sepsis: those with congenital or
functional asplenia
*Children should receive the full
course of HiB & PCV13 vaccination
* Children >2yr of age who have
completed the full course of PCV13
vaccination should receive a dose
PPSV23 vaccine at least 8 weeks
after the last PCV13 dose.
*PPSV23 should be repeated every
5 years.
*Annual influenza vaccination for
asplenic children & household
contacts (to reduce the risk of
secondary bacterial infections)
*Quadrivalent meningococcal
conjugate vaccine (Aramen or
Menactra) is recommended at the
age-appropriate schedule.
*Caution: do not administer PCV13
& Menactra at the same time.
Menactra interferes with antibody
production after PCV13 vaccination
& these should be separated by 4
weeks. No precautions needed for
Aramen vaccine.
*Daily antibiotic prophylaxis with
amoxicillin 10mg/kg PO BID
*Duration of antibiotic prophylaxis:
-Up to 5yrs of age in sickle cell dz;
or
-At least 1 year after splenectomy;
or
-Up to 18yrs of age (minimum) in
children with
hpogammaglobulinemia, HIV
infection, solid organ transplant
recipients, advanced liver disease
& survivors of pneumococcal
sepsis.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 26 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
RSV Palivizumab Target pathogen: Respiratory
(Synagis®) syncytial virus
15mg/kg IM monthly
during RSV season RSV prophylaxis is indicated:
(max 5 doses) *Infants born before 29 wks, 0 days’
gestation, who are <12months old
during RSV season.
*Term infants with CLD of
prematurity, defined as birth at <32
weeks, 0 days’ gestation with
oxygen requirement for >21% for at
least 28 days after birth, who are
<12mo old during RSV season.
* Infants with hemodynamically
significant heart disease during the
first year of life.
*Children with pulmonary
abnormality or neuromuscular
disease that impairs the ability to
clear secretions from the upper
airways may be considered for
prophylaxis in the first year of life.
*Children <24 months who will be
profoundly immunocompromised
during the RSV season may be
considered for prophylaxis.
RSV prophylaxis is NOT
indicated:
*Otherwise healthy infants born at
or after 29 weeks, 0 days’
gestation.
*Prophylaxis is not recommended
in the second year of life except for
children who required at least 28
days of supplemental oxygen after
birth and who continue to require
medical intervention (supplemental
oxygen, chronic corticosteroid, or
diuretic therapy).
*Insufficient data are available to
recommend prophylaxis for children
with cystic fibrosis or Down
syndrome.
*Monthly prophylaxis should be
discontinued in any child who
experiences a breakthrough RSV
hospitalization.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 27 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Neonates born to HepB *Hepatitis B vaccine AND hepatitis
sAg positive mothers B immunoglobulin (HBIG) to be
given within 12hrs (CDC) or 24hrs
(WHO) after birth.
*Both need to be given in separate
anatomical sites
*For infants <2000gm at birth, give
dose of HepB vaccine as above.
However, this dose will not be
counted towards the infant’s HepB
vaccination series. Hence repeat
another dose of HepB vaccine after
1 month or when the infant’s weight
is >2000gm (whichever is later).
*Check infant’s HepB surface
Antigen and surface antibody at 9-
12 months to document adequate
immunity & carrier status.
*No indication to delay BCG
vaccine (NHS guidelines)
Rabies No previous rabies *As much of the full dose of rabies
vaccination: immunoglobulin should be
infiltrated around the wounds. Any
Rabies remaining should be given IM.
immunoglobulin
20u/kg- see note *In a patient with history of rabies
vaccination, RIG is not indicated.
AND
Rabies vaccine (IM)
1 dose each on Days 0,
3, 7 & 14
Previously vaccinated:
Rabies vaccine (IM)
1 dose each on Days 0
&3
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 28 of 33
Pediatric Antibiotic Guidelines
2019
β-lactam Allergy
Infection First Line Therapy Type 1 hypersensitivity: Comments
Urticaria or anaphylaxis
Tetanus Target pathogen: Clostridium
tetani
*Clean or minor wounds. Human
tetanus immunoglobulin (HTIG) is
not indicated:
Receipt of <3 doses (or unknown)
of tetanus-containing vaccine. Give
vaccine.
Receipt of ≥3 doses of tetanus-
containing vaccine, no need for
booster unless last dose was
>10yrs ago.
*All other wounds i.e.,
contaminated with dirt, feces, soil,
or saliva; puncture wounds;
avulsions; wounds resulting from
missiles, crushing, burns, or
frostbite:
Receipt of <3 doses (or unknown)
of tetanus-containing vaccine. Give
vaccine & HTIG
Receipt of ≥3 doses of tetanus-
containing vaccine, booster
indicated if last dose was ≥5yrs
ago. HTIG not indicated.
*250 units of HTIG intramuscularly
at a different site than tetanus
toxoid.
*Intravenous immune globulin
(IVIG) should be administered if
human tetanus immune globulin is
not available.
Endocarditis Amoxicillin (PO) Clindamycin (PO) *Antibiotics should be given 30-
prophylaxis 50mg/kg 20mg/kg 60min prior to dental or respiratory
(max 2g) (max 600mg) procedures requiring endocarditis
prophylaxis per AHA Guidelines.
OR OR
*If a patient is receiving penicillin
Cephalexin (PO) Azithromycin or prophylaxis for rheumatic heart
50mg/kg Clarithromycin (PO) disease, they should be offered IE
(max 2g) 15mg/kg prophylaxis with a different class of
(max 500mg) antibiotic i.e, clindamycin.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 29 of 33
Pediatric Antibiotic Guidelines
2019
ABBREVIATION LEGEND CHART
Abbrev. Expansion Abbrev. Expansion Abbrev. Expansion
IV Intravenous mg Milligram kg Kilogram
PO Per Oral hrs Hours max Maximum
g Gram Q6H 6th Hourly Q8H or TID 8th Hourly
Q12H or Q24H/
12th Hourly Once Daily yr(s) Year(s)
BID OD
AOM Acute Otitis Media mo Months div Divided
REFERENCES
1. Mediclinic City Hospital, Dubai. Microbiology Laboratory Susceptibility Data 2018.
2. Jamsheer et al. Results from the Survey of Antibiotic Resistance (SOAR) 2011– 13 in the Gulf States. J
Antimicrob Chemother 2016; 71 (Suppl 1): i45-i61.
3. Adapted from Children’s Hospital of Philadelphia (CHOP): Pathway for the Evaluation and Treatment of a child
with Community-Acquired Pneumonia.
4. Bradley et al. The Management of CAP in Infants and Children Older than 3 months of age: Clinical Practice
Guidelines by the Pediatric Infectious Disease Society and the Infectious Disease Society of America. Clin Inf Dis.
Aug 2011.
5. Williams et al. Narrow Vs Broad-spectrum Antimicrobial Therapy for Children Hospitalized with Pneumonia.
Pediatrics. Nov 2013.
6. The Management of Community-Acquired Pneumonia in Infants and Children Older Than 3 Months of Age:
Clinical Practice Guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of
America. Clin Inf Dis 2011.
7. Spuesens et al. Carriage of Mycoplasma pneumoniae in the Upper Respiratory Tract of Symptomatic and
Asymptomatic Children: An Observational Study. PLOS Medicine. May 2013.
8. American Academy of Pediatrics. Clinical Practice Guideline for the Diagnosis and Management of Acute Otitis
Media. Pediatrics. Mar 2013.
9. American Academy of Pediatrics. Clinical Practice Guideline for the Diagnosis and Management of Acute Bacterial
Sinusitis in Children Aged 1 to 18 Years. Pediatrics. Jul 2013.
10. IDSA Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults. Clin Inf Dis 2012.
11. Clinical Practice Guideline for the Diagnosis & Management of Group A Streptococcal Pharyngitis: 2012 Update
by the Infectious Diseases Society of America (IDSA). Clin Inf Dis 2012.
12. NICE Guideline: Meningitis (bacterial) and meningococcal septicaemia in under 16s: recognition, diagnosis and
management. Feb 2015.
13. Urinary Tract Infection in Children. National Institute for Health and Clinical Excellence (NICE). Aug 2007.
14. American Academy of Pediatrics. Technical Report: Urinary Tract Infections in Febrile Infants and Young Children.
Pediatrics. April 1999- Endorsed by the Royal College of Pediatrics and Child Health (RCPCH).
15. Revised AAP Guideline on UTI in Febrile Infants and Young Children. Am Fam Physician. Nov 2012.
16. Reaffirmation of AAP Clinical Practice Guideline: The Diagnosis and Management of the Initial Urinary Tract
Infection in Febrile Infants and Young Children 2-24 Months of Age. Pediatrics. Dec 2016.
17. Adapted from Children’s Hospital of Philadelphia (CHOP): Pathway for the Evaluation and Treatment of Children
with Febrile UTI.
18. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious
Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Inf Dis
2017.
19. Sanford Guide to Antimicrobial Therapy©, 2019.
20. American Academy of Pediatrics RED BOOK: Report of the Committee on Infectious Diseases, 2018.
21. Centers for Disease Control (CDC).
22. UpToDate.
23. Epocrates Dx® and Epocrates ID®.
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 30 of 33
Pediatric Antibiotic Guidelines
2019
A
APPENDIX: CDC MALARIA TREATMENT TABLE
Dr. Zainab A. Malik MD, MSc, FAAP. 2019 Page 1 of 33
Dr. Zainab A. Malik MD, MSc, FAAP. 2019
Dr. Zainab A. Malik MD, MSc, FAAP. 2019
You might also like
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- Central Nervous System InfectionsDocument9 pagesCentral Nervous System InfectionsSaddamNo ratings yet
- Lampiran OM & FaringitisDocument6 pagesLampiran OM & FaringitisAdhinyDistiHelmiNo ratings yet
- Streptococcus Pneumoniae Haemophilus Influenzae: Click HereDocument3 pagesStreptococcus Pneumoniae Haemophilus Influenzae: Click HereSiti Hidayatul FitriNo ratings yet
- Antibiotic ConversionDocument9 pagesAntibiotic ConversionfabianNo ratings yet
- National Drug Policy on Malaria TreatmentDocument22 pagesNational Drug Policy on Malaria Treatmentdocsaurabh777No ratings yet
- Obat UKMPPDDocument54 pagesObat UKMPPDMuh.ikhsan zainalNo ratings yet
- Bone and Joint Infection Treatment GuidelinesDocument3 pagesBone and Joint Infection Treatment GuidelinesDanissa Fidia PuteriNo ratings yet
- Recommended Antibiotics for Acute Otitis Media TreatmentDocument1 pageRecommended Antibiotics for Acute Otitis Media Treatmentpriskilas911No ratings yet
- Guide of MedicationDocument4 pagesGuide of MedicationتَبٰارْكـNo ratings yet
- Sepsis and Catheter Infections: Early Conversion From IV To Oral AntibioticsDocument4 pagesSepsis and Catheter Infections: Early Conversion From IV To Oral AntibioticsChaim HerreraNo ratings yet
- Clindamycin Dose, Uses, Side EffectsDocument4 pagesClindamycin Dose, Uses, Side EffectsKenMNo ratings yet
- Antibiotics PDFDocument4 pagesAntibiotics PDFNilamdeen Mohamed ZamilNo ratings yet
- AST and Dosing Info Card - FINALDocument2 pagesAST and Dosing Info Card - FINALGAYATHIRINo ratings yet
- Drugs Acting On Immune SystemDocument6 pagesDrugs Acting On Immune SystemSORENI SORENINo ratings yet
- Treatment Protocol Against Covid 19 From WWW - Ippocrateorg.orgDocument4 pagesTreatment Protocol Against Covid 19 From WWW - Ippocrateorg.orgJohnuri MoraNo ratings yet
- YOUNG MIN LEE CASE STUDY Update 2Document7 pagesYOUNG MIN LEE CASE STUDY Update 2E.R.ONo ratings yet
- Pediatric Antibiotic DosingDocument7 pagesPediatric Antibiotic DosingAnonymous mm1yTelKNo ratings yet
- Antibiotic PolicyDocument16 pagesAntibiotic PolicykariNo ratings yet
- Brucella Presentation To UploadDocument31 pagesBrucella Presentation To UploadDrishti PoudelNo ratings yet
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaNo ratings yet
- Aminoglycosides: Under Supervision ofDocument5 pagesAminoglycosides: Under Supervision ofKhaled NagyNo ratings yet
- Medication Fact Sheets: 3rd Edition ContributorsDocument50 pagesMedication Fact Sheets: 3rd Edition ContributorsIndumathi ThangathirupathiNo ratings yet
- Lecture Treatment Malaria IKU - 2017Document23 pagesLecture Treatment Malaria IKU - 2017syuhaida deqsuNo ratings yet
- TropmedDocument92 pagesTropmedYusni Anita NainggolanNo ratings yet
- UK guideline on diagnosis and management of acute meningitisDocument2 pagesUK guideline on diagnosis and management of acute meningitisZara SaeedNo ratings yet
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- Paediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeDocument9 pagesPaediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeZamzam DomaNo ratings yet
- Antimicrobial PDFDocument7 pagesAntimicrobial PDFvhonNo ratings yet
- Empiric Treatment Guidelines Common InfectionsDocument9 pagesEmpiric Treatment Guidelines Common InfectionsShiza Batool100% (1)
- NICU ABX ChartDocument11 pagesNICU ABX ChartdrchiNo ratings yet
- MALARIA TREATMENT REGIMENSDocument2 pagesMALARIA TREATMENT REGIMENSMuhammad NuansaNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- Paediatric Dosage of Some Drugs-1Document45 pagesPaediatric Dosage of Some Drugs-1JaneNo ratings yet
- Obat Dosis Obat: Pneumonia, Community-AcquiredDocument2 pagesObat Dosis Obat: Pneumonia, Community-Acquiredannisa shalihahNo ratings yet
- Respiratory Tract Infections - Med DidacticsDocument59 pagesRespiratory Tract Infections - Med Didacticsapi-649060644No ratings yet
- Picu NotesDocument65 pagesPicu NotesAhmed Mohammed100% (2)
- Aminoglycoside Dosing Guide 2019-05-20 PDFDocument10 pagesAminoglycoside Dosing Guide 2019-05-20 PDFAbu Hammoud AlyazeediNo ratings yet
- Antimycobacterial Drug StudyDocument5 pagesAntimycobacterial Drug StudyKathNo ratings yet
- Amoxicillin 250 MG Capsules-Summary of Product CharacteristicsDocument65 pagesAmoxicillin 250 MG Capsules-Summary of Product CharacteristicsBrown and Burk UK Ltd100% (1)
- Analgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVDocument9 pagesAnalgesik/Pire Tik Dosis Sediaan Obat DOA OOA Drug Interaction Paracetamol IVNicole NgoNo ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- Immunorel Indication and DosageDocument1 pageImmunorel Indication and DosageKaela JaenNo ratings yet
- Endometrialcarcinoma r0416 7941Document2 pagesEndometrialcarcinoma r0416 7941crisibarra911No ratings yet
- Drug Study AZITHROMYCINDocument2 pagesDrug Study AZITHROMYCINDannah BulliandayNo ratings yet
- Table - Antimicrobial Drugs Used in Reptiles - MSD Veterinary ManualDocument5 pagesTable - Antimicrobial Drugs Used in Reptiles - MSD Veterinary ManualFaker FockerNo ratings yet
- NAG Urinary Tract InfectionsDocument14 pagesNAG Urinary Tract InfectionsJun JimenezNo ratings yet
- Drug Dosages in PediatricsDocument4 pagesDrug Dosages in Pediatricsmarry.as2012No ratings yet
- Theraputic Agent in NeonateDocument7 pagesTheraputic Agent in Neonateد. محمد فريد الغنامNo ratings yet
- Management of CAP in Adults - Ontario GovernmentDocument2 pagesManagement of CAP in Adults - Ontario GovernmentSukhvir AujlaNo ratings yet
- Pneumonia: Fever Cough Breathlessnes S DR J Pap/ich/ GMC Kottayam/19723Document4 pagesPneumonia: Fever Cough Breathlessnes S DR J Pap/ich/ GMC Kottayam/19723Firdouse ShajiNo ratings yet
- NAG Central Nervous System Infections As of Nov 2017Document9 pagesNAG Central Nervous System Infections As of Nov 2017Rhod Bernaldez EstaNo ratings yet
- AB Doses Common DiseasesDocument15 pagesAB Doses Common DiseasesTariqNo ratings yet
- Paediatric Dosage of Some DrugsDocument46 pagesPaediatric Dosage of Some DrugsS S LNo ratings yet
- Antituberculosis Drug OverviewDocument7 pagesAntituberculosis Drug OverviewMarc AntonioNo ratings yet
- AntibiocardDocument25 pagesAntibiocardchildicuNo ratings yet
- Empiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Document7 pagesEmpiric Antibiotic Guidelines For Paediatric Intensive Care Unit (PICU)Benny Chris TantoNo ratings yet
- Pharma - CCRDocument24 pagesPharma - CCRPrathik YanalaNo ratings yet
- Leukemia Treatment Regimens 7937Document3 pagesLeukemia Treatment Regimens 7937Irfan FathurrahmanNo ratings yet
- PPK SepsisDocument4 pagesPPK SepsisTria SanmaNo ratings yet
- Reading Reference 4-Hypertensive EmergenciesDocument6 pagesReading Reference 4-Hypertensive EmergenciesVarshini Tamil SelvanNo ratings yet
- Reading Reference 5-Approach To BurnsDocument4 pagesReading Reference 5-Approach To BurnsVarshini Tamil SelvanNo ratings yet
- Reading Reference 3-Approach To Chest PainDocument14 pagesReading Reference 3-Approach To Chest PainVarshini Tamil SelvanNo ratings yet
- Carcinoma Q & ADocument22 pagesCarcinoma Q & AVarshini Tamil SelvanNo ratings yet
- Reading Reference 6-Approach To Multiple TraumaDocument9 pagesReading Reference 6-Approach To Multiple TraumaVarshini Tamil SelvanNo ratings yet
- Acute + Chronic + HealingDocument6 pagesAcute + Chronic + HealingVarshini Tamil SelvanNo ratings yet
- Antibiotic Guidelines For AdultsDocument9 pagesAntibiotic Guidelines For AdultsVarshini Tamil SelvanNo ratings yet
- Reading Reference 1-Approach To Critically Ill Undifferntiated PatientDocument17 pagesReading Reference 1-Approach To Critically Ill Undifferntiated PatientVarshini Tamil SelvanNo ratings yet
- Patho Weekly QsDocument55 pagesPatho Weekly QsVarshini Tamil SelvanNo ratings yet
- Pathology of Diseases of Infancy and ChildhoodDocument7 pagesPathology of Diseases of Infancy and ChildhoodVarshini Tamil SelvanNo ratings yet
- Robbins Basic Pathology 9th Edition QBankDocument4 pagesRobbins Basic Pathology 9th Edition QBankVarshini Tamil SelvanNo ratings yet
- First Aid Q&A PDFDocument764 pagesFirst Aid Q&A PDFStephanie Williams100% (9)
- History TakingConcise History TakingDocument2 pagesHistory TakingConcise History TakingVarshini Tamil SelvanNo ratings yet
- Path OmaDocument232 pagesPath OmaVarshini Tamil SelvanNo ratings yet
- Steps - Psychological First Aid CourseraDocument3 pagesSteps - Psychological First Aid CourseraVarshini Tamil SelvanNo ratings yet
- Lauren Sompayrac - How Pathogenic Viruses Think - Making Sense of Virology-Jones & Bartlett Learning (2012)Document182 pagesLauren Sompayrac - How Pathogenic Viruses Think - Making Sense of Virology-Jones & Bartlett Learning (2012)Varshini Tamil Selvan100% (1)
- Graphic Guide Diseases PDFDocument382 pagesGraphic Guide Diseases PDFRafael100% (3)
- Medical Microbiology Made MemorableDocument113 pagesMedical Microbiology Made MemorableParna Praveen90% (10)
- Blood and Guts - A Short History of MedicineDocument161 pagesBlood and Guts - A Short History of MedicineVarshini Tamil SelvanNo ratings yet
- Abdomen Anatomy - Peritoneum and Peritoneal CavityDocument4 pagesAbdomen Anatomy - Peritoneum and Peritoneal CavityVarshini Tamil SelvanNo ratings yet
- Reversible Dementia and DeliriumDocument65 pagesReversible Dementia and Deliriummpm8471No ratings yet
- COVID-19 Knowledge and Stigma StudyDocument15 pagesCOVID-19 Knowledge and Stigma Studypia espanillo100% (1)
- Case Questions: I. Understanding The Disease and PathophysiologyDocument8 pagesCase Questions: I. Understanding The Disease and Pathophysiologyapi-532124328No ratings yet
- The Flushing PatientDocument35 pagesThe Flushing Patientliu_owen17No ratings yet
- OtoscopeDocument3 pagesOtoscopeVpjunaib JunaibNo ratings yet
- Chapter 1: Healthy Lifestyles: Multiple ChoiceDocument8 pagesChapter 1: Healthy Lifestyles: Multiple Choiceaznknight323No ratings yet
- GitDocument19 pagesGitHasan AsdiNo ratings yet
- 07 PtosisDocument25 pages07 Ptosisbc22yNo ratings yet
- Lista LiliengreenDocument55 pagesLista LiliengreenMauroNo ratings yet
- Abdominal ExaminationDocument14 pagesAbdominal ExaminationValeria Guerra CastilloNo ratings yet
- APA DSM 5 Gender DysphoriaDocument2 pagesAPA DSM 5 Gender DysphoriaDebra GibsonNo ratings yet
- JaundiceDocument29 pagesJaundiceMurali TiarasanNo ratings yet
- The Caregiving Experiences of Fathers and Mothers of Children With Rare Diseases in Italy: Challenges and Social Support PerceptionsDocument14 pagesThe Caregiving Experiences of Fathers and Mothers of Children With Rare Diseases in Italy: Challenges and Social Support PerceptionsLupita LeyvaNo ratings yet
- DKA To CRFDocument4 pagesDKA To CRFMark Anthony YabresNo ratings yet
- Incomplete Spinal Cord InjuryDocument4 pagesIncomplete Spinal Cord InjurypuchioNo ratings yet
- Exclusive Breastfeeding Knowledge, Attitudes and PracticesDocument47 pagesExclusive Breastfeeding Knowledge, Attitudes and PracticesAbiodun GideonNo ratings yet
- NAC OSCE - A Comprehensive Review (October 30, 2011) - (146646416X) - (CreateSpace Independent Publishing Platform)Document170 pagesNAC OSCE - A Comprehensive Review (October 30, 2011) - (146646416X) - (CreateSpace Independent Publishing Platform)Vikrant100% (1)
- Snake Control 101: The Basics of Keeping Snakes AwayDocument8 pagesSnake Control 101: The Basics of Keeping Snakes AwaynayakyaNo ratings yet
- Mudra - Supra PowersDocument3 pagesMudra - Supra PowersmakkuhotmailNo ratings yet
- Hearing ImpairmentDocument7 pagesHearing ImpairmentIrene MendozaNo ratings yet
- Poliomyelitis Causes, Symptoms, Treatment and PreventionDocument10 pagesPoliomyelitis Causes, Symptoms, Treatment and PreventionQzmp1No ratings yet
- Assessing Infection Control Program RisksDocument7 pagesAssessing Infection Control Program Riskssostro0% (1)
- Type2dm PDFDocument3 pagesType2dm PDFapi-303065684No ratings yet
- Biomecanica Da ObesidadeDocument9 pagesBiomecanica Da ObesidadehgtrainerNo ratings yet
- A Homoeopathic Drug Proving of Trachyspermum Ammi: DR Ajith Kumar D SDocument47 pagesA Homoeopathic Drug Proving of Trachyspermum Ammi: DR Ajith Kumar D Sdipnar6379No ratings yet
- Laporan Pendahuluan Demensia - Id.enDocument11 pagesLaporan Pendahuluan Demensia - Id.enRaudatul jannahNo ratings yet
- 3 Preanestesic EvaluaciónDocument15 pages3 Preanestesic EvaluaciónManu BGNo ratings yet
- Physiologic Changes PregnancyDocument53 pagesPhysiologic Changes PregnancyDeedong Zydee100% (1)
- Improve Your Breathing With The Alexander TechniqueDocument3 pagesImprove Your Breathing With The Alexander TechniqueLeland Vall86% (14)
- Articles CSPCDocument61 pagesArticles CSPCStephanieNo ratings yet