Professional Documents
Culture Documents
Bartels AJGP2014
Uploaded by
Jiachun LiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bartels AJGP2014
Uploaded by
Jiachun LiCopyright:
Available Formats
Long-Term Outcomes of a Randomized Trial
of Integrated Skills Training and Preventive
Healthcare for Older Adults with Serious
Mental Illness
Stephen J. Bartels, M.D., M.S., Sarah I. Pratt, Ph.D., Kim T. Mueser, Ph.D.,
Brent P. Forester, M.D., Rosemarie Wolfe, M.S., Corinne Cather, Ph.D., Haiyi Xie, Ph.D.,
Gregory J. McHugo, Ph.D., Bruce Bird, Ph.D., Kelly A. Aschbrenner, Ph.D.,
John A. Naslund, M.P.H., James Feldman, M.D.
Objective: This report describes 1-, 2-, and 3-year outcomes of a combined psychosocial
skills training and preventive healthcare intervention (Helping Older People Experience
Success [HOPES]) for older persons with serious mental illness. Methods: A randomized
controlled trial compared HOPES with treatment as usual (TAU) for 183 older adults
(age ! 50 years [mean age: 60.2]) with serious mental illness (28% schizophrenia, 28%
schizoaffective disorder, 20% bipolar disorder, 24% major depression) from two
community mental health centers in Boston, Massachusetts, and one in Nashua, New
Hampshire. HOPES comprised 12 months of weekly skills training classes, twice-
monthly community practice trips, and monthly nurse preventive healthcare visits,
followed by a 1-year maintenance phase of monthly sessions. Blinded evaluations of
functioning, symptoms, and service use were conducted at baseline and at a 1-year (end
of the intensive phase), 2-year (end of the maintenance phase), and 3-year (12 months
after the intervention) follow-up. Results: HOPES compared with TAU was associated
with improved community living skills and functioning, greater self-efficacy, lower
overall psychiatric and negative symptoms, greater acquisition of preventive healthcare
(more frequent eye exams, visual acuity, hearing tests, mammograms, and Pap smears),
and nearly twice the rate of completed advance directives. No differences were found for
medical severity, number of medical conditions, subjective health status, or acute service
use at the 3-year follow-up. Conclusion: Skills training and nurse facilitated preventive
healthcare for older adults with serious mental illness was associated with sustained
long-term improvement in functioning, symptoms, self-efficacy, preventive healthcare
screening, and advance care planning. (Am J Geriatr Psychiatry 2014; 22:1251e1261)
Received September 25, 2012; revised March 28, 2013; accepted April 24, 2013. From the Department of Psychiatry (SJB, SIP, KTM, KAA) and
Department of Community and Family Medicine (SJB), Geisel School of Medicine at Dartmouth, Hanover, NH; The Dartmouth Institute for
Health Policy and Clinical Practice (SJB, SIP, JAN), Dartmouth College, Hanover, NH; Dartmouth Psychiatric Research Center (KTM, RW,
HX, GJM), Lebanon, NH; Center for Psychiatric Rehabilitation (KTM), Boston University, Boston, MA; Department of Psychiatry (BPF),
Harvard University, Cambridge, MA; Geriatric Psychiatry Research Program (BPF), McLean Hospital, Belmont, MA; Schizophrenia Program
(CC), Massachusetts General Hospital, Boston, MA; Vinfen (BB), Cambridge, MA; and Massachusetts Mental Health Center (JF), Boston, MA.
Send correspondence and reprint requests to Stephen J. Bartels, M.D., M.S., Centers for Health and Aging, 46 Centerra Parkway, Ste. 200,
Lebanon, NH 03766. e-mail: sbartels@dartmouth.edu
! 2014 American Association for Geriatric Psychiatry
http://dx.doi.org/10.1016/j.jagp.2013.04.013
Am J Geriatr Psychiatry 22:11, November 2014 1251
Long-Term Outcomes of the HOPES Intervention
Key Words: Older adults, serious mental illness, psychosocial skills training, healthcare
management, preventive healthcare, integrated care
in the community with nurse coordination of preven-
INTRODUCTION tive healthcare as an integrated component. In a series
of studies, we reported that HOPES is associated with
The aging of the baby boomer population will
improved psychosocial outcomes after 1 year of
dramatically impact the number of middle aged and
weekly skills training and a second year of monthly
older adults with serious mental illness (SMI) over
maintenance sessions18 and with improved executive
the coming decades, foreshadowing an unprece-
functioning at 1, 2, and 3 years of follow-up.19
dented challenge to a public mental health system
The purpose of this final report of primary study
unprepared to address the special needs of this
outcomes is to address the following two remaining
emerging demographic. Adults with SMI constituted
study questions: (1) Does HOPES result in long-term
over 4% of those age 55 and older or 3.4 million
improved psychosocial functioning that persists at
adults in 20101,2 and are projected to nearly double
the 3-year follow-up after withdrawing maintenance
by 2050.3 In contrast to an array of evidence-based
sessions and nurse health management? (2) Is HOPES
interventions and implementation guides targeting
associated with improved preventive healthcare and
younger adults,4,5 few models of care are specifically
reduced acute service use?
designed for older adults with SMI. Among available
To address these questions, we evaluated 3-year
interventions, those that have emerged as effective
psychosocial, preventive healthcare, and service use
include combined cognitive behavioral therapy and
outcomes of a randomized controlled trial comparing
social skills training (CBSST),6e8 group-based
HOPES with treatment as usual (TAU) at a 1-year
psychosocial support,9 and functional adaptation
(end of the intensive phase of skills training), 2-year
skills training (FAST).10,11 Interventions such as these
(end of the maintenance phase), and 3-year (12
are necessary to address the complex psychosocial
months after intervention withdrawal) follow-up. We
and healthcare needs of this rapidly growing
hypothesized that HOPES compared with TAU at the
subgroup with the highest per person Medicare and
3-year follow-up is associated with greater long-term
Medicaid costs,12 rates of institutionalization over
improvement in independent living skills, social
three times those of other Medicaid beneficiaries,13
skills, self-efficacy, and psychiatric symptom severity
and greater use of emergency care than older adults
and with a greater quality of preventive healthcare
without SMI.14
and lower acute service use.
Several factors—lack of independent living skills,
poor social skills, and medical comorbidity—are
strongly associated with high-cost service use and
differentiate older adults with SMI living in nursing METHODS
homes from those in the community.12 In addition,
A randomized controlled trial compared
persons with SMI, when compared with those
outcomes for HOPES and TAU at 1, 2, and 3 years.
without, are known to be at risk for receiving
Written informed consent was obtained through
preventive healthcare services at a lower rate.15 To
procedures approved by the Committee for the
address these needs, we developed and pilot-tested
Protection of Human Subjects at Dartmouth College
an intervention combining community living and
and by the institutional review boards specific to
social skills training with integrated preventive
each site.
healthcare.16,17 The HOPES (Helping Older People
Experience Success) program is designed to improve
Study Participants
independent functioning and community tenure by
teaching social skills, community living skills, and Community-dwelling adults with SMI age 50 or
healthy living skills to older persons with SMI living older (N ¼ 183) were recruited from two community
1252 Am J Geriatr Psychiatry 22:11, November 2014
Bartels et al.
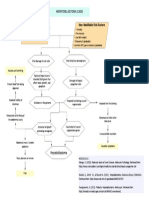
FIGURE 1. Consort diagram.
mental health agencies in Boston, Massachusetts, and conjunction with documented persistent impairment
one in Nashua, New Hampshire, and were random- in multiple areas of functioning. Exclusion criteria
ized to HOPES (N ¼ 90) or TAU (N ¼ 93). Eligibility were residence in a nursing home or other institu-
criteria included ability and willingness to provide tional setting, primary diagnosis of dementia or
informed consent and an Axis I disorder diagnosis of significant cognitive impairment as indicated by
schizophrenia, schizoaffective disorder, bipolar a Mini Mental Status Exam score less than 20,21
disorder, or major depression based on the Struc- physical illness expected to cause death within
tured Clinical Interview for Diagnostic and Statistical 1 year, or current substance dependence. Figure 1
Manual of Mental Disorders, Fourth Edition20 in summarizes the flow of participants in the study.
Am J Geriatr Psychiatry 22:11, November 2014 1253
Long-Term Outcomes of the HOPES Intervention
Interventions or outreach by non-nurse clinicians; individual
therapy; and access to rehabilitation services, such as
HOPES. HOPES targets psychosocial functioning
groups and psychoeducation.
and preventive healthcare.17 The psychosocial
component consists of weekly skills training classes
Measures
delivered over 1 year, followed by a 1-year mainte-
nance phase with monthly booster sessions. The Community living skills were assessed from three
HOPES social rehabilitation curriculum, based on perspectives: participant self-report, case manager
social skills training,22 is manualized and organized ratings of observed functioning in the community, and
into seven modules: Communicating Effectively, performance-based assessments of simulated tasks. The
Making and Keeping Friends, Making the Most of Independent Living Skills Survey23 is a participant
Leisure Time, Healthy Living, Using Medications self-report measure of functioning assessing 10 areas of
Effectively, Living Independently in the Community, community living activities. The Multnomah Commu-
and Making the Most of a Health Care Visit. A nity Ability Scale24 is a 17-item measure of observed
complete list of topics covered is found in our report of community functioning completed by interviewing
interim outcomes.17 Sessions were video recorded and each individual’s case manager. The University of
evaluated for fidelity by two authors (SIP and KTM). California San Diego (UCSD) Performance-based Skills
HOPES training sessions consisted of 8e10 partici- Assessment evaluates basic living skills using simulated
pants and were delivered in mental health centers and tasks and role play in five areas: communication, trip
senior centers in the community. To minimize trans- planning, transportation, finances, and shopping.25 The
portation challenges, participants attended two Social Behavior Schedule26 is a 23-item measure of
sessions on the same day consisting of a 90-minute social functioning in individuals with SMI. The Revised
morning session focused on a specific skill and a 60- Self-Efficacy Scale consists of 57 statements rating
minute afternoon session to consolidate the selected perceived self-efficacy in social functioning and in
skill using role-play exercises, with a lunch break in managing symptoms.27
between to encourage socialization. In addition, The Brief Psychiatric Rating Scale28 and the Scale for
twice-monthly community trips were organized so the Assessment of Negative Symptoms29 were used to
participants could practice skills related to the current assess psychiatric symptom severity and negative
module topics in the community (e.g., bus station to symptoms over the prior 2 weeks. Depressive
practice using public transportation), and participants symptom severity was assessed with the Center for
were encouraged to practice new skills with a family Epidemiologic Studies Depression Scale.30 Health
member or friend. Attendance across sites was status was assessed with the 36-item Short Form
approximately 75% in year 1 and 70% in year 2. Health Survey (SF-36)31 and an interview-based
The preventive healthcare component consists of version of the Charlson Comorbidity Index.32 Self-
monthly meetings with a nurse embedded in the report and medical record reviews were used to
mental health setting who evaluates participants’ determine acute service use (e.g., hospitalizations,
healthcare needs focusing on facilitating preventive emergency room visits) and to quantify the proportion
screening, advance care planning, and coordination of preventive healthcare indicators from recommended
of primary healthcare visits. Goals were collabora- screening examinations by the U.S. Preventive Services
tively set by the nurse and each participant based on Task Force.33 A detailed description of procedures and
a list of recommended preventive health screenings.17 measures are provided in a previous report.18
Skills training leaders and nurses met weekly to
coordinate the psychosocial and preventive health-
Study Procedures
care components. Participants attended an average of
66% of the nurse visits across sites. After obtaining informed consent, participants
TAU. Participants in both groups continued to completed baseline assessments and were random-
receive the same services they had been receiving ized to HOPES or TAU. Assessors were blind to
before the study. Routine mental health services at all treatment group, and participants were reminded not
sites included pharmacotherapy, case management, to reveal information about their treatment to the
1254 Am J Geriatr Psychiatry 22:11, November 2014
Bartels et al.
interviewer. Randomization was conducted at the and the correlation between baseline and 3-year
individual level and stratified by diagnosis (schizo- outcomes. The following thresholds, defined by
phrenia spectrum or mood disorder) and gender. A Cohen,37 were used to determine whether an effect
block randomization approach was used to ensure size was small (0.20), moderate (0.50) or large (0.80).
that no more than four participants could be Positive effect sizes denote increases in HOPES rela-
randomized to the same treatment group in a row. tive to TAU, and negative effect sizes denote
Participants were paid for completing assessments decreases in HOPES relative to TAU.38
but not for participating in HOPES. Chi-square analyses and number needed to treat
(NNT)39 were used to evaluate the categorical
outcomes of receipt of preventive healthcare. As
Statistical Analyses
determined in a prior study,40 NNT for one person to
Sample size was determined by computing statis- obtain preventive health screening, cancer screening,
tical power to detect effect sizes based on our pilot or completion of advance directives was calculated as
study of the HOPES program.16 Two tailed t tests and the inverse of the absolute risk reduction for not
c2 analyses were used to compare HOPES and TAU receiving either of these types of preventive healthcare.
on demographic characteristics, psychiatric history,
and outcome measures at baseline. Treatment effects
were evaluated by conducting intent-to-treat anal-
yses on the full sample of randomized study partic- RESULTS
ipants, regardless of their exposure to treatment.
HOPES Versus TAU at Baseline and 3-Year
A mixed-effects linear model was used for analysis,
Follow-Up
which does not drop subjects with missing data
because the statistical inference model assumes data Participants assigned to HOPES did not differ
missing at random. A doubly multivariate repeated significantly from those assigned to TAU on any
measures analysis of variance, simultaneously demographic, diagnostic, or baseline measures, with
analyzing all three dependent measures of commu- the exception of a greater rate of asthma in HOPES
nity functioning, guarded against potential inflation compared with TAU group (N ¼ 18 versus N ¼ 7;
of alpha with multiple dependent variables. There- p ¼ 0.017) (Table 1). We compared baseline demo-
after, an analysis of covariance approach controlling graphics, functioning, and symptoms of participants
for gender and diagnosis was used to test for treat- who completed the 3-year assessment (N ¼ 129) with
ment effects on each of the dependent variables those lost at the 3-year follow-up (N ¼ 54). Partici-
separately. Because there were no significant differ- pants lost to follow-up were slightly older (mean age:
ences between HOPES and TAU at baseline, rather 62.7 $ 9.3 versus 59.1 $ 7.1; t test ¼ 2.58; df ¼ 181;
than fitting parametric curves with random effects, p ¼ 0.01) and had greater self-efficacy (mean Revised
we included the baseline as a covariate and fit base- Self Efficacy Scale score: 72.5 $ 17.9 versus 65.6 $
line adjusted mean response profile models,34 also 19.0; t test ¼ %2.36; df ¼ 181; p ¼ 0.02).
referred to as covariance pattern models,35 selecting Fewer than 2% of observations were missing at
appropriate covariance structures as well as missing baseline for the Center for Epidemiologic Studies
data with maximum likelihood estimation.36 Depression Scale, Charlson Comorbidity Index, and
Site was included in initial analyses but was Brief Psychiatric Rating Scale. At the 3-year follow-
dropped from the final models because it did not up, an average of 34% of observations were missing
alter the main effects. Because the baseline was (range: 31%e39%), except for the Multnomah Scale,
statistically adjusted, treatment effects were evalu- which had 50% missing observations. This rate of
ated with group main effects (i.e., differences in missing observations was expected because 30%
group mean response profiles). Two-tailed statistical (N ¼ 54) of participants were lost at the 3-year
tests were conducted, and differences were consid- follow-up and the Multnomah Scale requires
ered statistically significant based on p #0.05. Effect locating and interviewing clinical providers who
sizes were computed using Cohen’s d and an anal- have detailed knowledge of participants’ functioning
ysis of covariance approach to adjust for covariates in the community.
Am J Geriatr Psychiatry 22:11, November 2014 1255
Long-Term Outcomes of the HOPES Intervention
approach (F(2,151) ¼ 5.10, p ¼ 0.007). Next, we
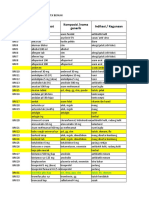
TABLE 1. Sample Characteristics by Group at Baseline
conducted independent tests on each of the three
Total Sample TAU HOPES dependent variables showing significant differences
(N [ 183) (N [ 93) (N [ 90)
favoring HOPES over TAU for participant self-report,
Characteristic N % N % N %
observed functioning in the community, and perfor-
Age, y (mean $ SD) 60.2 $ 7.9 60.1 $ 7.1 60.3 $ 8.0 mance on standardized simulated tasks. HOPES
Days in hospital 20.7 $ 39.6 21.1 $ 45.1 20.2 $ 31.1
(mean $ SD) contributed to greater overall self-efficacy compared
Gender with TAU. In testing for interactions by diagnostic
Female 106 58 53 57 53 59
group, we found that improved self-efficacy was
Male 77 42 40 43 37 41
Ethnicity greatest among participants with mood disorders.
White 157 86 78 84 79 88 No other interactions between group and diagnosis
Non-white 26 14 15 16 11 12
Latino
were observed for any other outcome variables. For
No 171 93 88 95 83 92 psychiatric symptoms, we compared both groups on
Yes 12 7 5 5 7 8 the primary outcome of overall psychiatric symptom
Marital status
Never married 118 65 59 63 59 66 severity (i.e., Brief Psychiatric Rating Scale total) and
Married 65 35 34 37 31 34 found lower overall symptom severity for HOPES.
Education We then separately evaluated primary symptom
High school 134 73 64 69 70 78
graduate outcomes between groups, finding lower negative
Less than high 49 27 29 31 20 22 symptom severity and a trend for lower depression
school
Residential
among HOPES participants. At the 3-year follow-up,
Living 94 51 49 53 45 50 no significant differences were found between groups
independently for behavior or mental/physical functioning
Supervised/ 89 49 44 47 45 50
supported outcomes as measured by the SF-36 or with respect
housing to medical severity or total number of medical
Medical diagnosis conditions.
Hypertension 80 44 47 51 33 37
Diabetes 50 27 23 25 27 30
COPD 42 23 23 25 19 21
Hypothyroidism 32 18 18 19 14 16 Preventive Healthcare Screening and Advanced
Asthmaa 25 14 7 8 18 20 Directives
Cardiac disease 23 13 14 15 9 10
Psychiatric diagnosis Table 4 compares HOPES with TAU with respect
Schizoaffective 52 28 28 30 24 27
Schizophrenia 51 28 26 28 25 28
to preventive healthcare across three categories of
Depression 44 24 20 22 24 27 indicators: (1) routine preventive care (blood pres-
Bipolar 36 20 19 20 17 19 sure, eye examination, visual acuity test, hearing test,
Notes: SD: standard deviation; COPD: chronic obstructive serum cholesterol, flu shot), (2) cancer screening
pulmonary disease.
a
(colon cancer, mammogram, Pap smear), and (3)
Fisher’s two-sided exact test ¼ 6.03; p ¼ 0.017; no other
comparisons were significant at p #0.05.
advance directives. A higher percentage of HOPES
participants received eye exams, visual acuity, and
hearing tests compared with TAU, with the greatest
between-group difference found for receipt of
Functioning, Symptom, and Health Status
mammograms and Pap smears (NNT ¼ 5.5 and 3.5,
Outcomes
respectively). Finally, a nearly twofold difference was
Tables 2 and 3 show results of the intent-to-treat found between HOPES and TAU for completing
analyses of outcomes for community functioning, advance directives (NNT ¼ 3.6). Excluding the rela-
psychiatric symptoms, and health status at the 1-, 2- tionship between female gender and mammograms
and 3-year follow-up. HOPES compared with TAU or Pap smears, there were no other gender differences
was associated with greater improvement in the with respect to receipt of the different preventive
weighted combination of the three approaches to healthcare screens or completion of advanced direc-
measuring community living skills using the multi- tives. We also explored possible interactions between
variate repeated measures analysis of variance years of education, cognitive status, and receipt of
1256 Am J Geriatr Psychiatry 22:11, November 2014
Bartels et al.
preventive healthcare screens or advanced directives,
0.033
0.024
0.014
0.190
0.010
p
and no significant relationship emerged.
Group Main Effect
1, 161
1, 150
1, 163
1, 162
1, 156
df
Acute Health Service Use
Greater decreases were observed from baseline to
4.64
5.23
6.13
1.73
6.85
F
the 3-year follow-up for HOPES compared with TAU
with respect to the proportion of participants who
0.25
0.26
0.27
%0.08
0.33
had at least one psychiatric hospitalization, medical
ES
hospitalization, or emergency room visit, although
these differences were not statistically significant. The
0.11
0.14
0.44
0.48
15.15
19.48
10.06
10.39
15.89
21.08
SD
proportion of participants experiencing at least one
3 Year
acute psychiatric hospitalization decreased 7% for
Mean
0.68
0.62
3.83
3.72
77.77
70.30
48.56
50.29
72.20
69.45
HOPES compared with 3% for TAU (HOPES: 22%
[N ¼ 17] at baseline and 15% [N ¼ 11] at the 3-year
follow-up; TAU: 26% [N ¼ 22] at baseline and 23%
0.11
0.12
0.51
0.53
14.35
21.06
8.41
9.58
16.37
18.49
SD
[N ¼ 16] at the 3-year follow-up). The proportion of
2 Year
participants experiencing at least one acute medical
Mean
0.68
0.65
3.78
3.61
77.32
69.44
46.74
49.14
71.46
71.33
hospitalization decreased by 3% for HOPES
compared with an increase of 3% for TAU (HOPES:
0.09
17.70
0.11
0.45
0.50
13.47
19.88
8.54
9.23
17.74
30% [N ¼ 24] at baseline and 27% [N ¼ 20] at the
SD
TABLE 2. Community Functioning Outcomes at 3-Year Follow-Up in HOPES Compared with TAU
3-year follow-up; TAU: 27% [N ¼ 23] at baseline and
1 Year
30% [N ¼ 21] at the 3-year follow-up). Finally, there
Mean
0.68
71.35
0.66
3.76
3.58
76.04
68.97
49.30
50.75
68.76
was a 14% decrease in the proportion of participants
experiencing at least one emergency room visit for
0.10
19.16
0.11
0.51
0.51
15.93
19.04
8.94
7.97
18.61
HOPES compared with a 5% decrease for TAU
SD
Baseline
(HOPES: 55% [N ¼ 43] at baseline and 41% [N ¼ 31]
at the 3-year follow-up; TAU: 49% [N ¼ 42] at base-
Mean
0.66
66.24
0.65
3.66
3.69
72.85
68.54
51.42
51.17
68.99
line and 44% [N ¼ 31] at the 3-year follow-up).
Group
HOPES
HOPES
HOPES
HOPES
HOPES
TAU
TAU
TAU
TAU
TAU
DISCUSSION
Case manager/clinician
Participant interview/
Participant interview
Participant interview
Performance-based
Participation in HOPES was associated with
observation
observation
Data Source
improved community living skills at the 3-year
follow-up from three perspectives: participant self-
Notes: SD: standard deviation; ES: effect size.
report, case manager observation of functioning in
the community, and performance on simulated tasks
of independent living skills. HOPES contributed to
greater self-efficacy and to decreased overall severity
Self-reported: Independent Living
Self-efficacy: Revised Self-Efficacy
Performance Skills Assessment
Social behaviors: Social Behavior
Community Ability Scale total
of psychiatric and negative symptoms. These results
Simulated performance: UCSD
Social behaviors and self-efficacy
Observed functioning in the
demonstrate the persistence of improved outcomes at
community: Multnomah
Skills Survey (ILSS total)
1-year post-intervention. Integrated preventive
Community living skills
Scale (R-SES total)
Survey (SBS total)
healthcare was also associated with greater receipt of
preventive health screening and greater completion
(UPSA total)
of advanced directives.
These results contribute to a limited empirical
Measures
research literature, including the FAST and CBSST
programs. These interventions focus on middle-aged
Am J Geriatr Psychiatry 22:11, November 2014 1257
Long-Term Outcomes of the HOPES Intervention
and older adults with schizophrenia and do not
0.936
HOPES 46.90 11.56 45.54 11.97 47.94 12.22 46.09 13.25 0.07 0.12 1, 159 0.732
0.048
0.053
0.073
HOPES 3.03 2.49 2.77 2.48 2.72 2.52 2.73 2.43 %0.22 0.26 1, 156 0.614
HOPES 5.48 3.99 8.55 5.44 8.78 4.68 10.43 8.42 %0.14 0.10 1, 94 0.749
P
include an integrated component of preventive
Group Main Effect
healthcare management. FAST is a 6-month interven-
11.86 0.05 0.01 1, 159
13.75 %0.17 3.97 1, 157
0.64 %0.27 3.70 1, 155
11.64 %0.22 3.26 1, 158
df
tion to improve skills for independent living,
communication, and psychiatric illness manage-
F
ment.10 In a randomized trial (N ¼ 240), FAST was
associated with greater improvement compared with
ES
usual care in negative symptoms and in performance
14.98
0.65
14.27
14.88
TAU 47.04 11.79 46.83 11.02 47.26 11.76 48.50 11.73
2.30 2.13 2.54 2.36 2.41 2.34 2.22 2.04
5.84 3.77 8.07 6.00 10.14 7.68 13.17 9.81
of community living skills.11 CBSST is a 3-month
SD
3 Year
intervention combining cognitive behavioral therapy
Mean
41.99
19.52
50.53
49.92
2.21
2.50
19.43
41.99
(e.g., cognitive restructuring) with social skills
training.11 A randomized trial (N ¼ 76) found that
10.61
10.68
13.84
13.75
13.27
0.55
0.65
13.18
SD
CBSST contributed to greater improvement in
2 Year
6-month outcomes for insight and on the leisure and
Mean
40.65
12.38
50.43
51.09
2.26
2.52
19.59
42.93
transportation subscales of the Independent Living
Skills Survey,23 but, in contrast to HOPES, no differ-
11.42
11.86
12.34
13.66
0.49
0.57
11.42
13.11
SD
TABLE 3. Psychiatric Symptoms and Health Status Outcomes at 3-Year Follow-Up in HOPES Compared with TAU
1 Year
ences were found between groups in the total scores
for living skills.8 Our 3-year findings from the current
Mean
41.77
20.01
52.82
54.34
2.29
2.51
20.63
41.27
study suggest that skills training can result in sus-
tained improvements in psychosocial functioning and
11.38
12.99
13.86
12.75
0.54
0.54
12.82
13.81
SD
Baseline
symptom severity for a heterogeneous group of older
Group Mean
38.99
23.85
55.54
54.23
2.42
2.50
20.83
41.25
adults with SMI.
In addition to achieving improved functioning and
HOPES
HOPES
HOPES
HOPES
decreased psychiatric symptoms, HOPES partici-
TAU
TAU
TAU
TAU
TAU
TAU
pants compared with TAU experienced greater
preventive healthcare screening. It is noteworthy that
Participant interview/medical records
Participant interview/observation
Participant interview/observation
the greatest improvement was found for mammo-
grams, Pap smears, and advance care planning.
Participant interview
Participant interview
Participant interview
Medical records
However, we did not observe greater improvement
Data Source
in subjective health status (as measured by the SF-36)
or lower ratings of medical severity. Of interest, the
number of identified medical diseases approximately
doubled (rather than decreased) for both HOPES and
TAU over the 3-year period of study, most likely
reflecting the impact of increased attention to
comorbid medical disorders resulting from repeated
Negative symptoms: Scale for the Assessment of
Physical functioning: SF-36 Physical Component
Notes: SD: standard deviation; ES: effect size.
Psychiatric symptoms: Brief Psychiatric Rating
participant interviews, clinician ratings, and requests
Depression: Center for Epidemiologic Studies
Mental functioning: SF-36 Mental Component
for primary care medical records. Finally, decreases
Medical severity: Charlson Severity Index
in the proportion of participants who were hospital-
Negative Symptoms (SANS total)
ized or who had an emergency room visit were
Depression Scale (CES-D total)
greater for HOPES compared with TAU, although
the sample size may not have been adequate to
Total number of diseases
demonstrate statistically significant differences.
Scale (BPRS total)
Score (MCS total)
Several limitations warrant consideration when
Psychiatric symptoms
Score (PCS total)
interpreting the results. First, our study sample was
predominantly white (86%; N ¼ 157), suggesting the
Health status
need to evaluate HOPES in diverse populations and to
Measures
explore the need for cultural adaptations.41 A version
of HOPES tailored for African Americans, developed
1258 Am J Geriatr Psychiatry 22:11, November 2014
Bartels et al.
TABLE 4. Preventive Healthcare, Screening, and Advance Directives at 3-Year Follow-Up in HOPES Compared with TAUa
HOPES TAU
(N [ 90) (N [ 93)
Preventive Healthcare and Advance Directives N % N % NNT Effect Size c2 Testb p
Routine preventive care
Blood pressure 87 100 89 99 90.9 0.00 1.00 0.508
Eye exam 84 97 79 88 11.2 0.36 4.96 0.048
Visual acuity test 74 85 65 72 7.8 0.32 4.39 0.045
Hearing test 52 60 40 44 6.5 0.32 4.18 0.051
Cholesterol 84 97 84 93 30.3 0.13 0.97 0.497
Flu shot 75 86 68 76 9.4 0.26 3.28 0.087
Cancer screening
Colon cancer screen 71 82 76 84 %35.7c %0.07 0.25 0.690
Mammogram (women) 45 85 34 67 5.5 0.43 4.81 0.039
Pap smear (women) 41 77 25 49 3.5 0.59 9.16 0.004
Care planning
Advance directives 51 61 28 33 3.6 0.59 13.20 <0.001
a
Percent receiving preventive healthcare screening at least once over the 3-year study period and presence of documented advance
directives.
b
Fisher’s two-sided Exact Test.
c
Because a slightly greater proportion of TAU participants received colon cancer screening compared with HOPES participants, the NNT is
a negative value, more appropriately interpreted as number needed to harm.
after this trial, is now available. Second, because standards on clinical significance have not been
HOPES consists of both skills training and preventive established. However, the UCSD Performance-based
healthcare, we are unable to attribute the study Skills Assessment has an established cutoff for clini-
outcomes to either component. Third, the nurse cally significant improvement in functioning: a score
component emphasized preventive healthcare and of at least 75 is predictive of residential indepen-
healthcare coordination. We found improved quality dence.42 At the 3-year follow-up, two-thirds of
of preventive healthcare (a proximal outcome) but did HOPES participants achieved at least 75 on the UCSD
not demonstrate significant improvement in health Performance-based Skills Assessment (67%; N ¼ 37)
status (a distal outcome) as measured by the SF-36. compared with slightly more than half of those
More targeted disease management (as opposed to receiving TAU (54%; N ¼ 30) (NNT ¼ 7.3).
general care coordination) and a longer follow-up These findings advance the evidence base on
period may be needed to demonstrate improved effective interventions for older adults with SMI in
health outcomes. several ways. Our study demonstrates the feasibility
In addition, because HOPES consists of seven and effectiveness of integrating group-based skills
discrete modules delivered over 1 year followed by training and preventive healthcare targeting older
a second year of monthly booster sessions, our study adults with SMI. An important strength was that
was not designed to assess the comparative or HOPES demonstrated improved independent living
incremental contributions of the individual modules skills and community functioning from multiple
to improved outcomes. A more targeted and indi- perspectives including self-report, case manager
vidually tailored approach may be more effective and observation, and role-play assessments of skills. We
efficient. We are currently engaged in pilot studies also found that integrated preventive healthcare
exploring the feasibility and potential effectiveness of coordination by an embedded nurse can significantly
matching participant need and preference for improve adherence to preventive screening, especially
selected components of HOPES. Finally, although we for procedures such as mammograms and Pap
found statistically significant improvements on smears, in addition to substantially improving
several measures of functioning and symptoms over advance care planning. Finally, HOPES participants
3 years, the clinical significance of these improve- maintained gains in improved functioning and
ments is uncertain. For most of the measures, symptoms at the 3-year follow-up. To our knowledge,
Am J Geriatr Psychiatry 22:11, November 2014 1259
Long-Term Outcomes of the HOPES Intervention
this improvement in functioning provides the longest between science and services provided in the
and largest demonstration of the effectiveness of community. To respond to the rapidly growing
psychosocial skills training for persons with SMI, population of older adults with SMI, a future
regardless of age group. research agenda should include identifying success-
There are several potential implications of these ful strategies for implementing and sustaining effec-
findings. First, as underscored by the 2012 Institute of tive integrated rehabilitation and healthcare services
Medicine Report on the mental health workforce for in the community.
older adults,5 the burgeoning population of older
adults with SMI will require more providers trained The authors thank the following individuals for their
to supply evidence-based practices for this high-risk assistance in conducting this project: Kay Allen, Therese
group.43 HOPES adds to the small number of Andrews, Rachel Berman, Sarah Bishop-Horton, Alice
psychosocial interventions validated for use among Cassidy, Sara Castillo, Martha Curtis, Vanessa D’Anna,
older adults with SMI8,11 and confirms that the Meghan Driscoll, Carol Farmer, Susan Fitzpatrick, Anne
effectiveness of psychosocial rehabilitation is not Fletcher, Carol Furlong, Severina Haddad, Carol Johnson,
limited to younger adults. These interventions may Sarah Kelly, Lisa Kennedy, Meghan Santos, Cynthia
also provide a strategy for responding to the U.S. Meddich, Katie Merrill, Krystal Murray, Brenda Nick-
Supreme Court Olmstead Decision mandating that erson, Thomas Patterson, Reni Poulakos, Christina Riggs,
states provide services supporting the preference of Brenda Wilbert, Joanne Wojcik, and Valerie Zelonis.
adults with disabilities to reside in noninstitutional The study was supported by a grant from the National
settings.2 Finally, there remains a dramatic gap Institute of Mental Health (R01 MH62324).
References
1. Bartels SJ, Miles KM, Dums AR, et al: Factors associated with 10. Patterson TL, McKibbin C, Taylor M, et al: Functional Adaptation
community mental health service use by older adults with severe Skills Training (FAST): a pilot psychosocial intervention study in
mental illness. J Mental Health Aging 2003; 9:123e135 middle-aged and older patients with chronic psychotic disorders.
2. Bartels SJ: Commentary: the forgotten older adult with serious Am J Geriatr Psychiatry 2003; 11:17e23
mental illness: the final challenge in achieving the promise of 11. Patterson TL, Mausbach BT, McKibbin C, et al: Functional
Olmstead? J Aging Soc Policy 2011; 23:244e257 Adaptation Skills Training (FAST): a randomized trial of
3. U.S. Census Bureau: National Population Projections Released a psychosocial intervention for middle-aged and older patients
2008: Table 12: Projections of the Population by Age and Sex for with chronic psychotic disorders. Schizophr Res 2006; 86:
the United States: 2010 to 2050. Washington, DC, U.S. Census 291e299
Bureau, 2008 12. Bartels SJ, Clark RE, Peacock WJ, et al: Medicare and Medicaid
4. Substance Abuse and Mental Health Services Administration: costs for schizophrenia patients by age cohort compared with
MedTEAM: How to Use the Evidence-Based Practices KITs. costs for depression, dementia, and medically ill patients. Am J
Rockville, MD, Center for Mental Health Services, Substance Geriatr Psychiatry 2003; 11:648e657
Abuse and Mental Health Services Administration, U.S. Depart- 13. Bartels SJ, Miles KM, Dums AR, et al: Are nursing homes appro-
ment of Health and Human Services, 2010 priate for older adults with severe mental illness? Conflicting
5. Institute of Medicine: The Mental Health and Substance Use consumer and clinician views and implications for the Olmstead
Workforce for Older Adults: In Whose Hands?. Washington, DC, decision. J Am Geriatr Soc 2003; 51:1571e1579
The National Academies Press, 2012 14. Hendri HC, Lindgren D, Hay DP, et al: Comorbidity profile and
6. Granholm E, Holden J, Link PC, et al: Randomized controlled trial healthcare utilization in elderly patients with serious mental
of cognitive behavioral social skills training for older consumers illnesses. Am J Geriatr Psychiatry 2013; 21:1267e1276
with schizophrenia: defeatist performance attitudes and func- 15. Druss BG, Rosenheck RA, Desai MM, et al: Quality of preventive
tional outcome. Am J Geriatr Psychiatry 2013; 21:251e262 medical care for patients with mental disorders. Med Care 2002;
7. Granholm E, McQuaid JR, McClure FS, et al: Randomized 40:129e136
controlled trial of cognitive behavioral social skills training for 16. Bartels SJ, Forester B, Mueser KT, et al: Enhanced skills training
older people with schizophrenia: 12-month follow-up. J Clin and health care management for older persons with severe
Psychiatry 2007; 68:730e737 mental illness. Commun Mental Health J 2004; 40:75e90
8. Granholm E, McQuaid JR, McClure FS, et al: A randomized, 17. Pratt SI, Bartels SJ, Mueser KT, et al: Helping Older People
controlled trial of cognitive behavioral social skills training for Experience Success: an integrated model of psychosocial
middle-aged and older outpatients with chronic schizophrenia. rehabilitation and health care management for older adults
Am J Psychiatry 2005; 162:520e529 with serious mental illness. Am J Psychiatr Rehabil 2008; 11:
9. Berry K, Purandare N, Drake R, et al: A mixed-methods evaluation 41e60
of a pilot psychosocial intervention group for older people with 18. Mueser KT, Pratt SI, Bartels SJ, et al: Randomized trial of
schizophrenia. Behav Cogn Psychother 2014; 42:199e210 social rehabilitation and integrated health care for older
1260 Am J Geriatr Psychiatry 22:11, November 2014
Bartels et al.
people with severe mental illness. J Consult Clin Psychol instrument for depression among community-residing older
2010; 78:561e573 adults. Psychol Aging 1997; 12:277e287
19. Pratt SI, Mueser KT, Bartels SJ, et al: The impact of skills training 31. Ware JE Jr, Snow KK, Kosinski M, et al: SF-36 Health Survey
on cognitive functioning in older people with serious mental Manual and Interpretation Guide. Boston, MA, The Health Insti-
illness. Am J Geriatr Psychiatry 2013; 21:242e250 tute, New England Medical Center, 1997
20. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Inter- 32. Charlson M, Pompei P, Ales K, et al: A new method of classifying
view for DMS-IV Axis-I Disorders—Patient Edition (SCID-I/P, prognostic comorbidity in longitudinal studies: development and
Version 2.0). New York, Biometrics Research Department, 1996 validation. J Chronic Dis 1987; 40:373e383
21. Folstein MF, Folstein SE, McHugh PR: Mini-mental state: a prac- 33. U.S. Preventive Services Task Force: Recommendations for
tical method for grading the cognitive state of patients for the Adults. Rockville, MD, USPSTF Program Office, 2013
clinician. J Psychiatr Res 1975; 12:189e198 34. Fitzmaurice G, Laird N, Ware J: Applied Longitudinal Analysis.
22. Bellack AS: Skills training for people with severe mental illness. New York, John Wiley & Sons, 2004
Psychiatr Rehabil J 2004; 27:375e391 35. Hedeker D, Gibbons RD: Longitudinal Data Analysis. New York,
23. Wallace CJ, Liberman RP, Tauber R, et al: The Independent Living Wiley, 2006
Skills Survey: a comprehensive measure of the community func- 36. Jennrich R, Schluchter M: Unbalanced repeated-measures models
tioning of severely and persistently mentally ill individuals. with structured covariance matrices. Biometrics 1986; 42:
Schizophr Bull 2000; 26:631e658 805e820
24. Barker S, Barron N, McFarland BH, et al: A community ability 37. Cohen J: Statistical Power Analysis for the Behavioral Sciences,
scale for chronically mentally ill consumers: part I. reliability and 2nd edition. Hillsdale, NJ, Lawrence Erlbaum Associates, 1988
validity. Commun Mental Health J 1994; 30:363e379 38. Kazis LE, Anderson JJ, Meenan RF: Effect sizes for interpreting
25. Patterson TL, Goldman S, McKibbin CL, et al: USCD Performance- changes in health status. Med Care 1989; 27:S178eS189
based Skills Assessment: development of a new measure of 39. Laupacis A, Sackett DL, Roberts RS: An assessment of clinically
everyday functioning for severely mentally ill adults. Schizophr useful measures of the consequences of treatment. N Engl J Med
Bull 2001; 27:235e245 1988; 318:1728e1733
26. Wykes T, Sturt E: The measurement of social behaviour in 40. Crowther RE, Marshall M, Bond GR, et al: Helping people with
psychiatric patients: an assessment of the reliability and validity severe mental illness to obtain work: systematic review. BMJ
of the SBS Schedule. Br J Psychiatry 1986; 148:1e11 2001; 322:204e208
27. McDermott BE: Development of an instrument for assessing self- 41. Patterson TL, Bucardo J, McKibbin CL, et al: Development
efficacy in schizophrenic spectrum disorders. J Clin Psychol and pilot testing of a new psychosocial intervention for older
1995; 51:320e331 Latinos with chronic psychosis. Schizophr Bull 2005; 31:
28. Andersen J, Larsen JK, Korner A, et al: The brief psychiatric rating 922e930
scale: schizophrenia, reliability and validity studies. Nord J 42. Mausbach BT, Bowie CR, Harvey PD, et al: Usefulness of the
Psychiatry 1986; 40:135e138 UCSD Performance-Based Skills Assessment (UPSA) for predicting
29. Andreasen NC: Modified Scale for the Assessment of Negative residential independence in patients with chronic schizophrenia.
Symptoms. Bethesda, MD, U.S. Department of Health and Human J Psychiatr Res 2008; 42:320e327
Services, 1984 43. Bartels SJ, Naslund JA: The underside of the silver tsunami—
30. Lewinsohn PM, Seeley JR, Roberts RE, et al: Center for Epidemi- older adults and mental health care. N Engl J Med 2013; 368:
ologic Studies Depression Scale (CES-D) as a screening 493e496
Am J Geriatr Psychiatry 22:11, November 2014 1261
You might also like
- Head To Toe Assessment Checklist Older Adults-1Document1 pageHead To Toe Assessment Checklist Older Adults-1spatrick32100% (4)
- ACLS Megacode Testing ScenariosDocument12 pagesACLS Megacode Testing Scenariosealm10100% (2)
- Pulp Exposure in Permanent Teeth CG-A012-04 UpdatedDocument7 pagesPulp Exposure in Permanent Teeth CG-A012-04 UpdatedmahmoudNo ratings yet
- Grandón Et Al - 2021 - Effectiveness of An Intervention To Reduce StigmaDocument9 pagesGrandón Et Al - 2021 - Effectiveness of An Intervention To Reduce StigmaAlejandra DìazNo ratings yet
- Older Adults and Integrated Health Settings: Opportunities and Challenges For Mental Health CounselorsDocument15 pagesOlder Adults and Integrated Health Settings: Opportunities and Challenges For Mental Health CounselorsGabriela SanchezNo ratings yet
- 4 Vancouver English B30Document14 pages4 Vancouver English B30aditiarrtuguNo ratings yet
- Hospitalization EditedDocument6 pagesHospitalization EditedmercyNo ratings yet
- Psychological and Social Interventions For Mental Health Issues and Disorders in Southeast Asia: A Systematic ReviewDocument13 pagesPsychological and Social Interventions For Mental Health Issues and Disorders in Southeast Asia: A Systematic ReviewMico Joshua OlorisNo ratings yet
- Marinucci Et Al. - 2023 - A Scoping Review and Analysis of Mental Health LitDocument16 pagesMarinucci Et Al. - 2023 - A Scoping Review and Analysis of Mental Health Litreeba khanNo ratings yet
- Igx004 2993Document1 pageIgx004 2993Arifah Budiarti NurfitriNo ratings yet
- FWD - Mixed Anxiety and Depression Among The Adult Population of The UK.Document8 pagesFWD - Mixed Anxiety and Depression Among The Adult Population of The UK.Sonal PandeyNo ratings yet
- Population-Health Approach: Mental Health and Addictions SectorDocument5 pagesPopulation-Health Approach: Mental Health and Addictions SectorNilanjana ChakrabortyNo ratings yet
- A Systematic Review and Meta-Analysis of Dyadic Psychological InterventionsDocument22 pagesA Systematic Review and Meta-Analysis of Dyadic Psychological InterventionsCristina MPNo ratings yet
- Fernandez 2022 Smartphone Famliy ConnectionsDocument7 pagesFernandez 2022 Smartphone Famliy ConnectionsBrayan PomaNo ratings yet
- Mental Health and Coping Strategies of Private Secondary School Teachers in The New Normal: Basis For A Psycho-Social Wellbeing Developmental ProgramDocument18 pagesMental Health and Coping Strategies of Private Secondary School Teachers in The New Normal: Basis For A Psycho-Social Wellbeing Developmental ProgramPsychology and Education: A Multidisciplinary JournalNo ratings yet
- JengMun - 2023 - Development of Brief Cognitive Behavioral Therapy Workshop Protocol MalaysiaDocument11 pagesJengMun - 2023 - Development of Brief Cognitive Behavioral Therapy Workshop Protocol Malaysiags67461No ratings yet
- Digital Mental Health Clinic in Secondary SchoolsDocument11 pagesDigital Mental Health Clinic in Secondary Schoolssoyjeric3266No ratings yet
- Betts2018 Article APsychoeducationalGroupInterveDocument7 pagesBetts2018 Article APsychoeducationalGroupInterveCralosNo ratings yet
- Hearing LossDocument10 pagesHearing LossAndreaNo ratings yet
- Ann 18 04 07Document8 pagesAnn 18 04 07EuNo ratings yet
- Mental Health Literacy, Level of Stressful Experiences and Coping Strategies of Elementary School TeachersDocument15 pagesMental Health Literacy, Level of Stressful Experiences and Coping Strategies of Elementary School TeachersPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Literature ReviewDocument8 pagesLiterature Reviewapi-584310341No ratings yet
- Understanding The Relationships Between Mental Disorders, Self-Reported Health Outcomes and Positive Mental Health: Findings From A National SurveyDocument10 pagesUnderstanding The Relationships Between Mental Disorders, Self-Reported Health Outcomes and Positive Mental Health: Findings From A National SurveyHung TranNo ratings yet
- Fisher 2017Document6 pagesFisher 2017Bogdan NeamtuNo ratings yet
- Child Adolesc Psychiatr Clin N Am 2020 29 1 211-23Document13 pagesChild Adolesc Psychiatr Clin N Am 2020 29 1 211-23Fernando SousaNo ratings yet
- Collaboration Among The Education, Mental Health, and Public Health Systems To Promote Youth Mental HealthDocument4 pagesCollaboration Among The Education, Mental Health, and Public Health Systems To Promote Youth Mental HealthKouseiNo ratings yet
- A Psychoeducational Group Intervention For FamilyDocument8 pagesA Psychoeducational Group Intervention For FamilyIoannis MalogiannisNo ratings yet
- Lay CounselorDocument12 pagesLay Counselornurul cahya widyaningrumNo ratings yet
- Mental Health Literacy Programs For School Teachers: A Systematic Review and Narrative SynthesisDocument12 pagesMental Health Literacy Programs For School Teachers: A Systematic Review and Narrative Synthesisnefe_emeNo ratings yet
- Primary Health Care Nurses Attitude Towards People With Severe Mental Disorders in Addis Ababa, Ethiopia: A Cross Sectional StudyDocument8 pagesPrimary Health Care Nurses Attitude Towards People With Severe Mental Disorders in Addis Ababa, Ethiopia: A Cross Sectional StudyleticiaNo ratings yet
- Mindfulness Based Interventions For People With Dementia and Their Caregivers Keeping A Dyadic BalanceDocument4 pagesMindfulness Based Interventions For People With Dementia and Their Caregivers Keeping A Dyadic BalanceMile RojasNo ratings yet
- Minding The Treatment Gap: Results of The Singapore Mental Health StudyDocument10 pagesMinding The Treatment Gap: Results of The Singapore Mental Health StudyNicholasNo ratings yet
- Research Paper ReviewDocument14 pagesResearch Paper ReviewGnaneswar PiduguNo ratings yet
- Jacm 03.2011Document6 pagesJacm 03.2011Meek ElNo ratings yet
- Examination of Telemental Health Practices in Caregivers of Children and Adolescents With Mental Illnesses A Systematic ReviewDocument14 pagesExamination of Telemental Health Practices in Caregivers of Children and Adolescents With Mental Illnesses A Systematic ReviewMushlih RidhoNo ratings yet
- TESTDocument11 pagesTESTANKITA YADAVNo ratings yet
- Peerj 4598Document27 pagesPeerj 4598David QatamadzeNo ratings yet
- Effects of The Tailored Activity ProgramDocument14 pagesEffects of The Tailored Activity ProgramBarbara Aguilar MaulenNo ratings yet
- 1Document13 pages1Erika HandayaniNo ratings yet
- Behaviour Research and TherapyDocument11 pagesBehaviour Research and TherapyCata PazNo ratings yet
- Addressing Mental Health in Aged Care ResidentsDocument9 pagesAddressing Mental Health in Aged Care ResidentsCarlos Hernan Castañeda Ruiz100% (1)
- Psychosocial Interventions For People With Dementia: An Overview and Commentary On Recent DevelopmentsDocument28 pagesPsychosocial Interventions For People With Dementia: An Overview and Commentary On Recent DevelopmentsMahendra SusenoNo ratings yet
- JurnalkepjiwaaDocument21 pagesJurnalkepjiwaaDewi AgustianiNo ratings yet
- 10 11648 J Ejb 20190702 13 PDFDocument6 pages10 11648 J Ejb 20190702 13 PDFfitriNo ratings yet
- Asia-Pacific Psychiatry - 2020 - Ismail - The Prevalence of Psychological Distress and Its Association With CopingDocument8 pagesAsia-Pacific Psychiatry - 2020 - Ismail - The Prevalence of Psychological Distress and Its Association With CopingbellaajsarraNo ratings yet
- Tugas 1Document10 pagesTugas 1Siti QomariaNo ratings yet
- 2023 Article 426Document23 pages2023 Article 426Kiran AbbasNo ratings yet
- Ijerph 18 00314Document15 pagesIjerph 18 00314Afifah Az-ZahraNo ratings yet
- The Effectiveness of CMHN (Community Mental Health Nursing) To Improve Mental Health in The Community - A Systematic ReviewDocument4 pagesThe Effectiveness of CMHN (Community Mental Health Nursing) To Improve Mental Health in The Community - A Systematic Reviewfanizha apriliantiNo ratings yet
- Art in InquiryDocument13 pagesArt in InquiryEmmanuel Emma NdikuryayoNo ratings yet
- Mobile Health (Mhealth) Versus Clinic-Based Group Intervention For People With Serious Mental Illness: A Randomized Controlled TrialDocument8 pagesMobile Health (Mhealth) Versus Clinic-Based Group Intervention For People With Serious Mental Illness: A Randomized Controlled TrialOlivia NasarreNo ratings yet
- Factors Associated With The Burden of Family Caregivers of Patients With Mental Disorders: A Cross-Sectional StudyDocument10 pagesFactors Associated With The Burden of Family Caregivers of Patients With Mental Disorders: A Cross-Sectional StudyKrishna RaoNo ratings yet
- Clinical Efficacy of A Combined AcceptanDocument16 pagesClinical Efficacy of A Combined AcceptanEmanuel EspinosaNo ratings yet
- Harris Et Al., 2013 (BA - Depression - Physical Illness)Document6 pagesHarris Et Al., 2013 (BA - Depression - Physical Illness)Alba EneaNo ratings yet
- Reyes-Ortega 2019 ACT or DBT or Both - With Borderline Personality DisorderDocument16 pagesReyes-Ortega 2019 ACT or DBT or Both - With Borderline Personality DisorderMario Lopez PadillaNo ratings yet
- Early Intervention Psych - 2019 - Courtney - A Way Through The Woods Development of An Integrated Care Pathway For 1Document9 pagesEarly Intervention Psych - 2019 - Courtney - A Way Through The Woods Development of An Integrated Care Pathway For 1U of T MedicineNo ratings yet
- Effectiveness of The Therapeutic Intervention Program On The Socio-Emotional Development of Persons With Substance Use DisorderDocument8 pagesEffectiveness of The Therapeutic Intervention Program On The Socio-Emotional Development of Persons With Substance Use DisorderPsychology and Education: A Multidisciplinary JournalNo ratings yet
- Ref 2 India Mental HealthDocument7 pagesRef 2 India Mental Healthdnyanesh1inNo ratings yet
- Bài 3Document2 pagesBài 3Quỳnh Như Nguyễn TrịnhNo ratings yet
- Acceptance and Valued Living As Critical Appraisal and Coping Strengths For Caregivers Dealing With Terminal Illness and BereavementDocument10 pagesAcceptance and Valued Living As Critical Appraisal and Coping Strengths For Caregivers Dealing With Terminal Illness and BereavementPaula Catalina Mendoza PrietoNo ratings yet
- Effectiveness of The Online "DDocument14 pagesEffectiveness of The Online "DdewisimooNo ratings yet
- Population-Based Approaches To Mental Health: History, Strategies, and EvidenceDocument28 pagesPopulation-Based Approaches To Mental Health: History, Strategies, and EvidenceMatías Muñoz L.No ratings yet
- Adult Survivors of Childhood Sexual Abuse The Effects On Mental Health And The Role Of Cognitive Behavior TherapyFrom EverandAdult Survivors of Childhood Sexual Abuse The Effects On Mental Health And The Role Of Cognitive Behavior TherapyNo ratings yet
- BAT and KCL Study ProposalDocument4 pagesBAT and KCL Study ProposalAnuNo ratings yet
- Pocket-Book MCH Emergencies - English PDFDocument286 pagesPocket-Book MCH Emergencies - English PDFAbigail Kusi-Amponsah100% (1)
- DR Antonious CV N & AEDocument27 pagesDR Antonious CV N & AEdoctorantoniNo ratings yet
- 4th Year Write Up 2 - Int. MedDocument11 pages4th Year Write Up 2 - Int. MedLoges TobyNo ratings yet
- EXAMEN - 3EPPLI 30i+RFMHS 6 PDFDocument13 pagesEXAMEN - 3EPPLI 30i+RFMHS 6 PDFS Lucy PraGaNo ratings yet
- Hand Hygiene in Dental Health-Care SettingsDocument55 pagesHand Hygiene in Dental Health-Care SettingsManu DewanNo ratings yet
- Male InfertilityDocument38 pagesMale InfertilityPrincessMagnoliaFranciscoLlantoNo ratings yet
- PNSS Drug StudyDocument2 pagesPNSS Drug Studyrain peregrinoNo ratings yet
- Hepatic Dysfunction in Dengue Fever - A ProspectiveDocument20 pagesHepatic Dysfunction in Dengue Fever - A ProspectiveSanjay RaoNo ratings yet
- Rectovaginal FistulaDocument8 pagesRectovaginal FistulaRomi Mauliza FauziNo ratings yet
- BVCCT-501 Cardiac Catheterization Laboratory BasicsDocument52 pagesBVCCT-501 Cardiac Catheterization Laboratory BasicsManisha khan100% (1)
- Obs Exam QuestionsDocument265 pagesObs Exam Questionsreza_adrian_2100% (2)
- KodingDocument12 pagesKodingAva Vav100% (1)
- DRUG STUDY Setera Case 8Document10 pagesDRUG STUDY Setera Case 8Ceria Dorena Fe SeteraNo ratings yet
- Role of Atypical Pathogens in The Etiology of Community-Acquired PneumoniaDocument10 pagesRole of Atypical Pathogens in The Etiology of Community-Acquired PneumoniaJaya Semara PutraNo ratings yet
- Gait AnalysisDocument2 pagesGait AnalysisIvin KuriakoseNo ratings yet
- Beta Lactam AntibioticsDocument52 pagesBeta Lactam AntibioticsKaymie ReenNo ratings yet
- Specialize Immunity at Epithelial Barriers and in Immune Privilege TissuesDocument27 pagesSpecialize Immunity at Epithelial Barriers and in Immune Privilege TissuesUmar UsmanNo ratings yet
- 901-Article Text-1856-1-10-20221129Document6 pages901-Article Text-1856-1-10-20221129Made NujitaNo ratings yet
- Solution Manual For Understanding The Essentials of Critical Care Nursing 2nd Edition by PerrinDocument15 pagesSolution Manual For Understanding The Essentials of Critical Care Nursing 2nd Edition by PerrinMarieHughesebgjp100% (75)
- Nama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, DemamDocument52 pagesNama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, Demamrio1995No ratings yet
- Non-Modifiable Risk Factors: Hepatoblastoma CaseDocument1 pageNon-Modifiable Risk Factors: Hepatoblastoma CaseALYSSA AGATHA FELIZARDONo ratings yet
- Pharmaceutical Assasination (Partial)Document14 pagesPharmaceutical Assasination (Partial)jamie_clark_2100% (2)
- Pain Management in ChildrenDocument19 pagesPain Management in ChildrenNeo SamontinaNo ratings yet
- Ventouse - FinalDocument10 pagesVentouse - FinalJasmine KaurNo ratings yet
- Hyperemesis GravidarumDocument7 pagesHyperemesis GravidarumPrawira Weka AkbariNo ratings yet
- DrugsDocument2 pagesDrugsJeff MarekNo ratings yet