Professional Documents
Culture Documents
CHAPTER 2 Hematopoiesis
Uploaded by
AMELIA DALE MARQUEZCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CHAPTER 2 Hematopoiesis
Uploaded by
AMELIA DALE MARQUEZCopyright:
Available Formats
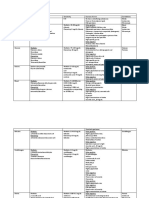
CHAPTER 2: HEMATOPOIESIS
HEMATOPOIESIS 2. HEPATIC PHASE
• A continuous, regulated process of blood cell production that • Begins at 5th to 7th gestational weeks and is characterized
includes: by recognizable granulocyte, erythroblasts and monocyte
o Cell renewal • Liver
o Proliferation o major site/chief site of hematopoiesis and retaining
o Differentiation activity until 1-2 weeks after birth
o Maturation • The spleen, kidney, thymus and lymph nodes contribute to
WHERE DID HEMATOPOIESIS CAME FROM? the hematopoietic process
• “HAIMA” – blood • Synthesis of hemoglobin F or Fetal hemoglobin but
• “POIESIS” – making or creating detectable level of adult hemoglobin may also be present but
• 2 types of approaching hematopoiesis F is more dominant
o Ontogeny – the embryonic point of view • Primitive hematopoiesis
o Phylogeny – evolution point of view of hematopoiesis o generates mainly erythrocyte and as gestation
ERYTHROPOIESIS increase this is when definitive hematopoiesis
• The term used for the proliferation and differentiation of generates and I is the start other blood cells arise.
RBC
LEUKOPOIESIS
• The term used for proliferation and differentiation of WBC
THROMBOPOIESIS
• The term used for proliferation and differentiation of
platelets
3. MEDULLARY PHASE/MYELOID PHASE
• At the 5th month of development, hematopoiesis begins in
the Bone Marrow (Chief Site)
• M:E ratio reaches adult levels of 3:1 at 21 weeks of gestation
• The relative numbers of myeloid cells also include
granulocytic and monocytic cells to nucleated erythroid
precursors in bone marrow
• Production of adult hemoglobin: HbA1 and HbA2
Summary:
at birth, the cavities of all bones are filled with blood forming
elements, the bone marrow is extremely cellular with much
active RBC and little inactive fatty bone marrow as we age. The
PHASES OF HEMATOPOIESIS: bone and cavities grow, the extra space become filled by fat. Bone
INTRAUTERINE PHASE marrow cellularity decreases and fat replacement increases, this
• Formation of blood inside the uterus (Embryonic phase) happens when we age. At 4 years of age hematopoiesis
• A.K.A. Extramedullary Hematopoiesis diminishes within the shafts of our long bones and at the age of
25, hematopoiesis is confined in our long bones and pelvic area
1. MESOBLASTIC OR MEGALOBLASTIC PHASE
• Hematopoiesis considered to begin around 19th day of the
embryonic development
• Begins during the embryonic development in blood islands
of the yolk sac at around 19th day of gestation
• Characterized by the development of primitive erythroblast
that produce hemoglobin like
o Portland
o Gower-1
o Gower-2
o These are needed for delivery of oxygen to rapidly
developing embryonic tissues
• This phase only produces RBC and the hemoglobin in this
RBC are called embryonic hemoglobin
• This phase of hematopoiesis occurs intravascularly
CHARLES REY GATCHALIAN[AUTHOR NAME] 1
CHAPTER 2: HEMATOPOIESIS
PHASES OF HEMATOPOIESIS: WHITE PULP
EXTRAUTERINE PHASE • consists of scattered follicles with germinal centers
MYELOID/ MEDULLARY PHASE containing lymphocytes, macrophages, and dendritic cells.
• After the first 3 weeks of postpartum, the bone marrow MARGINAL ZONE
becomes the only normal site of blood cell production and
• forms a reticular mesh work containing different blood
remains so throughout life
vessels, macrophages, and specialized T – cells
• Locations of red marrow
RED PULP
o Children: skull, clavicle, ribs, vertebra, pelvis and
long bones • comprised of dendritic processes that create a filter.
o 18 years and older: skull, clavicle, ribs vertebra,
pelvis and the proximal ends of long bones
o The rate of bone marrow growth exceeds need for
blood cells resulting to the replacement of active
marrow space by areas of fatty reserves that happens
as we age
EXTRAMEDULLARY HEMATOPOIESIS
LIVER AND SPLEEN
• Occurs normally
• Certain disease states when the BM is unable to produce
sufficient numbers of hematopoietic cells
ADULT HEMATOPOIETIC TISSUE
• Located in flat bones or in the ends of long bones
1. BONE MARROW
• Two types
A. RED MARROW
• Hematopoietically active PITTING
• Predominant type during infancy and childhood
• splenic macrophages remove inclusions or damaged surface
• Composed of extramedullary cords that contain all
membrane from RBC’s. It doesn’t not kill RBC’s.
developing cells (stem and progenitor cells, adventitial cells,
and macrophages)
CULLING
• The hematopoietic cells tend to develop in specific niches
within chords: • degradation of the cells subsequently. Phagocytized with
o Normoblasts develop in small cluster adjacent to the subsequent degradation of cells and organelles.
outer surfaces of the vascular sinuses
o Megakaryocyte are located close to the vascular walls
of the sinuses
o Immature myeloid (granulocyte) cells through the
metamyelocytes stage are located deep within the
chords
B. YELLOW MARROW
• Hematopoietically inactive, comprised of ADIPOCYTES
• Between ages 5-7, adipocytes become more abundant
• Retrogression: the process of replacing the red marrow by
yellow marrow
• It is capable of reverting back to active marrow in cases of
increased demands
2. LIVER
• Significant role in hematopoiesis in the 2nd trimester
• Major site during the hepatic stage
4. LYMPH NODE
• Capable of extramedullary hematopoiesis.
• Formation of new lymphocytes from germinal centers
• Counterpart of hepatic phase in adults in cases of bone
• Processing of specific immunoglobulins.
marrow shut down.
• It filters particulate matter, debris and bacteria that enter
3. SPLEEN
out lymph node.
• Removes the senescent RBC’s
• Sequesters approximately 30% of platelets.
5. THYMUS
• Densely populated with progenitor lymphoid cells that
migrated from the bone marrow and will soon give rise to T-
cells.
CHARLES REY GATCHALIAN 2
CHAPTER 2: HEMATOPOIESIS
ORIGIN OF BLOOD CELLS TRIALISTIC THEORY
• In the embryo and even in the adults, in one single fixed • this was proposed by Schilling, he believed that monocytes
multipotent stem cell, this gives rise to different tissue and develop from reticuloendothelial cells lining the sinusoids of
blood cells. All blood cells arise from hematopoietic cells. the liver and splee.
3. COMPLETE THEORY
• There is a separate stem cell for each cell series
• Proposed by Sabin et. al
• This theory states that there is a stem cell for each of several
cell series:
o Myeoloblasts would give rise to granulocytes
o Lymphoblasts to lymphocytes
o Monoblasts to monocytes
ORIGIN AND DEVELOPMENT OF BLOOD CELLS
HEMOHISTIOBLAST
• Fixed multipotent stem cell – give rise to tissue and to
blood cells
HEMOCYTOBLAST
• Pluripotent cell – give rise to unipotent committed stem cell
and hematopoietic cell lines
THE STEM CELLS:
1. HEMOHISTIOBLAST GENERATIVE STEM CELL
• Large (25 – 35) oval cell having a relatively large oval • the matrix of all stem cells
nucleus with regular fine vesicular reticulated chromatin O. • Responsible for the production of second stem cells
• 1/3 of its volume is occupied by a lilac – gray cytoplasm SOMATIC STEM CELL
containing minute non-specific polychromatic granules. • these undergoes transformation from which specific cell
• It has dual abilities types are produced
o can replicate itself, and to differentiate to pluripotent • All blood cells are derived from a common ancestral
cells and give rise to unipotent stem cells provides hematopoietic cell in the bone marrow which is called the;
specific hematopoietic cell lines in various PLURIPOTENT STEM CELL (PPSC): CFU-LM/CFU-S
stimulating hormones. • Present in small numbers in the BM
2. MYELOBLAST • Not morphologically identifiable
• white blood cell (eosinophil, neutrophil, and basophil) • Has the ability to reproduce and differentiate (can
3. MONOBLAST repopulate the BM after injury)
• Monocyte
4. STEM CELL KINETICS CFU-LM/CFU-S/PPSC:
• A stem cell processes 2 basic characteristics: • Progenitors:
o It is a self-maintaining- gives rise to daughter cells o Common LYMPHOID STEM CELL
that have the same capabilities as the parent cell. o Common MYELOID STEM CELL
o It has the ability to give rise to further differentiated
cells.
▪ Under normal conditions, the
number of stem cell in each person
remains more or less constant.
• When stem cells are stimulated, they could divide
asymmetrically
THEORIES ON THE ORIGIN OF BLOOD CELLS
1. MONOPHYLETIC/ UNITARIAN THEORY
• States that blood cells come from one stem cell which is
totipotent, giving rise to any series of cell types
NEOUNITARIAN THEORY
• maintains that the lymphocyte of normal blood does not HEMATOPOIETIC CHART DISCUSSION
usually transform to some other cell type, but that it has • Hematopoiesis – refers to commitment and differentiation
such marked developmental potentialities of forces of a stem cell due to different types of cells found in
2. POLYPHYLETIC THEORY the blood.
• States that there are two to three cell origins • Occur mainly in the bone marrow particularly in adult.
• There is a separate and distinct stem cell compartment • Can also occur in liver, bone marrow and spleen.
• This has been divided into 2 groups:
DUALISTIC THEORY HEMATOPOIETIC STEM CELL
• differentiate into common lymphoid progenitor cell or
• this proposes that there are 2 or perhaps 3 cells of origin
common myeloid progenitor cell.
• Lymphoblasts which give origin to the lymphocytes
• The common lymphoid progenitor cell
• Myeloblasts which give rise to the granulocytes, monocytes,
o further differentiates into different lymphoblasts
and megakaryocyte cell series
with different genetic profiles which allow them to
• Pronormoblast which develop into the red cell series
form and mature to different types of lymphocytes.
CHARLES REY GATCHALIAN 3
CHAPTER 2: HEMATOPOIESIS
• The different lymphoblasts with different genetic profiles
will become either naive B cells, pre-T cells and NK cells
• Common lymphoid progenitor cells can differentiate into
certain types of dendritic cells
• The dendritic cells when it is formed will move into tissues
and will become lymphoid dendritic cell (DC)
• Dendritic cells
o peripheral antigen presenting cells that are very
important in the connection between the innate
immune system and adaptive immune system.
COMMON MYELOID PROGENITOR CELL
• Can become myeloblast and eventually become
granulocytes.
• These granulocytes can be band neutrophils, band basophils
and band eosinophils; these granulocytes are band cells
because they are immature but once they enter the
circulation they mature and become neutrophil, basophils
and eosinophils.
NEUTROPHILS
• important in acute response in inflammation and infection
BASOPHILS
• important in allergies and parasitic infections
EOSINOPHILS
• important in allergies and sensitivity
Liver and Spleen- has no minimal role in hematopoiesis, but
• The common myeloid progenitor cells can differentiate and
they have a role particularly in period of infection or during
become pro monocytes and mast cell precursors
pathological changes.
• The promonocytes become mature and becomes monocytes Liver, Spleen and Lymph Node- Extramedullary
which are essentially circulating macrophages Hematopoiesis
• Monocyte/promonocyte can also become dendritic cell; if
they become dendritic cell in the tissue they are referred to GROWTH FACTORS/ CYTOKINES
as myeloid dendritic cells • Essential part of inflammatory process
MACROPHAGE AND DENDRITIC CELLS
• Produce by several kinds of immune cells including the
• important antigen presenting cells innate macrophages, dendritic cells, natural killer cells and
MAST CELLS adaptive T and B lymphocytes
• important cells in allergy, inflammatory response and COLONY STIMULATING FACTORS (CSF)
hypersensitivity • GM-CSF (gran, mono, ery, mega, and eos)
• The mast cell precursor can become mature mast cell once • G-CSF
they enter circulation and move into tissues • M-CSF/CSF (mono-macrophages)
INTERLEUKINS
• Common myeloid progenitor cell can differentiate and • Also produced by a variety of WBC
become megakaryocytes with stimulation of thrombopoietin ERYTHROPOIETIN (EPO)
o a hormone produced by the liver and the kidneys • Production of RBC
• Common myeloid progenitor cells can also become • Responsible in carrying oxygen from the lungs to body
erythroblasts through stimulation of erythropoietin – a THROMBOPOIETIN (TRO)
hormone released by the kidneys • Stimulates the formation of megakaryocyte
MEGAKARYOCYTES
• normally present in the bone marrow not in the circulating CYTOKINE CELL MODIFIER
blood, but these gives rise to the platelets found in the blood; IL-2 T-cells, B-cells, NK cells
megakaryocyte rupture releasing platelets into circulation IL-3 Multilineage stimulating factor
and platelets are very important in clotting. IL-4 T-cells, B-cells, mast cells
• Erythroblasts are still nucleated RBC, once they enter IL-5 Activates eosinophil progenitor
circulation and mature, they become erythrocytes which are IL-6 Stem cells, B-cells
anucleated
IL-7 Pre-B cells, T-cells, early granulocytes
NOTE: IL-9 Stimulates neutrophil production
• In healthy adults, hematopoiesis occurs in the bone marrow IL-11 Megakaryocytes
particularly in the pelvis, vertebrae and sternum, however GM-CSF Granulocytes, macrophages, fibroblasts,
hematopoiesis can occur in other organs which is call endothelial cells
extramedullary hematopoiesis
• Before earth, hematopoiesis occurs predominantly in the KIT LIGAND (KL)
liver and spleen but then it drops off by birth, which is • “Stem cell factor” or “steel factor”
because, slowly the bone marrow will take over the role by o Stimulates myeloid, erythroid and lymphoid
adulthood the bone marrow has the main role in progenitors
hematopoiesis particularly the vertebrae bone marrow and FIT-3 LIGAND (FL)
pelvis and sternum. • Primitive progenitor cells
CHARLES REY GATCHALIAN 4
CHAPTER 2: HEMATOPOIESIS
ANTIGENIC MARKERS • There are 4 different types of granules:
• Cell surface proteins that are used in the recognition or o Neutrophilic
differentiation of cells and molecules o Basophilic
• Cluster of differentiation o Eosinophilic
o proteins that are found in the surface of the cells and o Azurophilic granules
each cell molecule is assigned with different numbers. • As cells become older, specific granules become less
• This numbers are used for the identification of phenotypes. prominent and smaller.
CYTOKINE CELL MODIFIER CYTOPLASMIC AND NUCLEAR VARIATIONS
CD34 Stem cell marker (lymphoid and myeloid SYNCHRONOUS
precursor) • cytoplasm and nucleus of the blast cell they form at the same
CD33 Pan myeloid cells rate (same time in developing)
CD13 Pan myeloid cells • Contaminant, coordinate and parallel development of
nucleus and cytoplasm
CD11c, CD14 Monocytes
• Normal physiologic maturation
CD17 Erythroid ASYNCHRONOUS
CD2, CD3 Lymphoid, Pan T-cells • the cytoplasm or nucleus mature first before others
CD4 Help/Inducer T-cells • Abnormal development of blood cells where the rate of
CD8 Suppressor/ Cytotoxic T-cells maturation of nucleus and cytoplasm differs
CD10, CD19, CD20 Lymphoid, Pan B-cells o When this development is seen it means the age of
CD16, CD56 NK cells the cell is best classified based on the nuclear stage of
maturation except nuclear abnormalities or
hereditary of origin
- Pathologic
RELEASE OF BLOOD CELLS FROM THE BONE MARROW TO
THE CIRCULATION
To summarize
• Release of RBC’s is promoted by the EPO (erythropoietin)
1. Loss of cytoplasmic basophilia
• WBC’s leave the BM through chemotaxis
2. Modification and differentiation of cytoplasmic granules
• Platelets are released to the circulation through platelet
shedding and formation of a specific cytoplasmic constituent
3. Reduction in nuclear size, condensation of chromatin,
CHANGES DURING NORMAL BLOOD CELL MATURATION and reduction in the number of nucleoli
• Cell size: decrease 4. Alteration of nuclear shape
• Nuclear/ Cytoplasmic (N/c) ration: decrease 5. Reduction in total cell size
NUCLEUS:
o Size: decreases RELEASE OF BLOOD CELLS INTO THE PERIPHERAL BLOOD
o Nuclear chromatin: becomes coarser and more 1. FACTORS AFFECTING RED CELL RELEASE:
clumped • Spleen – in cases of clinical splenism
o Number of nucleoli: decrease • Level of maturation reached by the RBC series and the
o Staining: from reddish to bluish – purple pressure exerted by the intramarrow growth cells of the RBC
CYTOPLASM series
• Cell deformity
o Basophilia: gradually decreases
2. FACTORS AFFECTING THE RELEASE OF THE WBC
o Amount/ Size: increases
• The number of circulating white cells
o In some cells, some cytoplasmic constituents are
produced. • Glycoprotein-Colony-Stimulating activity
• And exemption to this rule is the megakaryocytes which do • Liberation and distribution of WBC into the peripheral blood
not decrease during cell maturation. (maybe due to the stimulation of diencephalon or various
CRITERIA FOR ASSESSING CELL MATURATION endocrine glands and the splenic inhibitory influence
associated by hypersplenism)
• Cell size
• Cortisone (special cause and causes increase in circulating
• Nuclear maturation
neutrophils and decrease in lymphocytes, eosinophil, and
• Cytoplasmic Maturation/changes
basophils
3. FACTORS AFFECTING THE RELEASE OF PLATELETS
CELL MATURATION
• Megakaryocyte throws out pseudopodia that pass through
• Blast cells contain no granules
the wall of marrow sinusoids and become nipped off to form
• Blast cells contains a large nucleus and a small amount of
platelets in the circulation
cytoplasm. Usually, the nucleus makes up about ¾ to 7/8 of
• Contractile system of the platelet (the release reaction of
the cell area.
platelet is dependent upon that contractile system)
• As the cells become older, the cytoplasm becomes less
• Tissue destruction, possibly splenic hormones or splenic
basophilic, the deeper blue the cytoplasm the younger the
sequestration, adrenal cortical and medullary substances
cell.
and possibly circulating antibodies
• As cells become older, the chromatin of the nucleus becomes
heavier, and the darker the nucleus stains, the heavier the
chromatin is.
8 GENERAL STATEMENTS TO BE MADE IN CELL
MATURATION
• As the cells become older, they become smaller
• Nucleoli are present in young cells and tend to disappear in
mature cells
CHARLES REY GATCHALIAN 5
CHAPTER 2: HEMATOPOIESIS
REVIEW QUESTIONS 11. When a patient has severe anemia and the bone marrow
1. The process of formation and development of blood cells is unable to effectively produce red blood cells to meet the
is termed: increased demand, one of the body’s responses is:
a. Hematopoiesis a. Extramedullary hematopoiesis in the liver and spleen
b. Hematemesis b. Decreased production of erythropoietin by the kidney
c. Hematocytometry c. Increased apoptosis of erythrocyte progenitor cells
d. Hematorrhea d. Increase the proportion of yellow marrow in the long
2. During the second trimester of fetal development, the bones
primary site of blood cell production is the:
a. Bone marrow 12. Hematopoietic stem cells produce all lineages of blood
b. Spleen cells in sufficient quantities over the lifetime of an individual
c. Lymph nodes because they:
d. Liver a. Are unipotent
b. Have the ability of self-renewal by asymmetric division
3. Which one of the following organs is responsible for the c. Are present in large numbers in the bone marrow niches
maturation of T lymphocytes and regulation of their d. Have a low mitotic potential in response to growth
expression of CD4 and CD8? factors
a. Spleen
b. Liver
c. Thymus
d. Bone marrow
4. The best source of active bone marrow from a 20-year-old
would be:
a. Iliac crest
b. Femur
c. Distal radius
d. Tibia
5. Physiologic programmed cell death is termed:
a. Angiogenesis
b. Apoptosis
c. Aneurysm
d. Apohematics
6. Which organ is the site of sequestration of platelets?
a. Liver
b. Thymus
c. Spleen
d. Bone marrow
7. Which one of the following morphologic changes occurs
during normal blood cell maturation:
a. Increase in cell diameter
b. Development of cytoplasm basophilia
c. Condensation of nuclear chromatin
d. Appearance of nucleoli
8. Which one of the following cells is a product of the CLP?
a. Megakaryocyte
b. T lymphocyte
c. Erythrocyte
d. Granulocyte
9. What growth factor is produced in the kidneys and is used
to treat anemia associated with kidney disease?
a. EPO
b. TPO
c. G-CSF
d. KIT ligand
10. Which one of the following cytokines is required very
early in the differentiation of a hematopoietic stem cell?
a. IL-2 REFERENCES
b. IL-8 Notes from synchronous session by Ms. Cielito Trinidad, RMT
c. EPO
d. FLT3 ligand University of Baguio PowerPoint presentation and module
CHARLES REY GATCHALIAN 6
CHAPTER 2: HEMATOPOIESIS
CHARLES REY GATCHALIAN 7
You might also like
- Hematopoiesis Reading NotesDocument7 pagesHematopoiesis Reading NotesMemeowwNo ratings yet
- Hematopoiesis ExplainedDocument10 pagesHematopoiesis ExplainedJezzah Mae CañeteNo ratings yet
- HemopoesisDocument31 pagesHemopoesisChandra Shinoda100% (2)
- (Hema) 1.1 Intro To Hema (Perez) - PANDADocument6 pages(Hema) 1.1 Intro To Hema (Perez) - PANDATony DawaNo ratings yet
- Complete Blood Count Pt. 1 (Module-Based)Document5 pagesComplete Blood Count Pt. 1 (Module-Based)Iya BangalanNo ratings yet
- 2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyDocument3 pages2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyAisle Malibiran PalerNo ratings yet
- Chapter 13 Rodaks HematologyDocument10 pagesChapter 13 Rodaks HematologyRALPH JAN T. RIONo ratings yet
- Poikilocytosis Review TableDocument5 pagesPoikilocytosis Review Tablekat100% (1)
- Hematology NotesDocument17 pagesHematology NotesEly Sibayan100% (2)
- Hematology Review NotesDocument29 pagesHematology Review NotesCattrainuh100% (2)
- Histology & Cell BiologyDocument33 pagesHistology & Cell BiologyMohSen100% (1)
- PoikilocytosisDocument3 pagesPoikilocytosisJasonNo ratings yet
- HEMATOPOIESISDocument50 pagesHEMATOPOIESISGalih Maygananda Putra87% (23)
- A Manual of Laboratory Techniques in Clinical Hematology 1Document15 pagesA Manual of Laboratory Techniques in Clinical Hematology 1Jaycel Mae Ba-ay (Gaikokujinn)No ratings yet
- Hematology 2 LaboratoryDocument11 pagesHematology 2 LaboratoryChristine BadilloNo ratings yet
- Non Malignant Hereditary Disorders of LeukocytesDocument6 pagesNon Malignant Hereditary Disorders of LeukocytesGilo IlaganNo ratings yet
- P. vivax vs P. ovale vs P. malariae vs P. falciparumDocument2 pagesP. vivax vs P. ovale vs P. malariae vs P. falciparumCJMALNo ratings yet
- Hematology Review NotesDocument28 pagesHematology Review NotesMeLaiyee89% (9)
- CSF and Other Body FluidsDocument9 pagesCSF and Other Body FluidsJobelle0% (1)
- Comprehensive LectureDocument87 pagesComprehensive LectureDeniel Busi100% (1)
- Histopathology Lab Management ProceduresDocument29 pagesHistopathology Lab Management ProceduresShara AboNo ratings yet
- (CLINPATH) 2.02 Transfusion II - Dr.-VillamayorDocument7 pages(CLINPATH) 2.02 Transfusion II - Dr.-VillamayorpasambalyrradjohndarNo ratings yet
- Hematology Lecture Notes for Medical StudentsDocument88 pagesHematology Lecture Notes for Medical StudentsharpreetNo ratings yet
- AUB - Urine Screening For Metabolic DisordersDocument3 pagesAUB - Urine Screening For Metabolic DisordersJeanne Rodiño100% (1)
- Histologic TechniquesDocument12 pagesHistologic TechniquesCatherine Merilleno100% (1)
- HEMA 1 QUIZ multiple choice and matching practiceDocument2 pagesHEMA 1 QUIZ multiple choice and matching practiceChristian John Mabalot CarilloNo ratings yet
- Disorders of Iron Kinetics and Heme Metabolism ConceptsDocument12 pagesDisorders of Iron Kinetics and Heme Metabolism ConceptsJoanne JardinNo ratings yet
- Rumple LeedeDocument3 pagesRumple LeedeIrene Dewi Isjwara40% (5)
- HEMOGLOBINOPATHY GUIDEDocument3 pagesHEMOGLOBINOPATHY GUIDEChatie PipitNo ratings yet
- Introduction To UrinalysisDocument28 pagesIntroduction To UrinalysisNicnoc RiveraNo ratings yet
- Wintrobe Test PDFDocument9 pagesWintrobe Test PDFMaria Chacón CarbajalNo ratings yet
- CSF Analysis GuideDocument248 pagesCSF Analysis GuideGennelyn Ross Delos Reyes0% (1)
- Hematopoiesis: by Hiranya DekaDocument15 pagesHematopoiesis: by Hiranya DekaHiranya Deka100% (2)
- Bleeding: 1. Vessel Wall 2. Platelets 3. Coagulation Protein 4. Anticoagulant Protein 5. Fibrinolytic SystemDocument5 pagesBleeding: 1. Vessel Wall 2. Platelets 3. Coagulation Protein 4. Anticoagulant Protein 5. Fibrinolytic Systemsarguss14100% (3)
- Hematology 2 TEST QUESTIONSDocument4 pagesHematology 2 TEST QUESTIONSa a r o n b a u t i s t aNo ratings yet
- WBC AbnormalitiesDocument37 pagesWBC AbnormalitiesMajj MajjNo ratings yet
- Role of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CDocument10 pagesRole of Blood Vessels in Hemostasis: Villa, M.D. MLS 4CMarianne Dennesse100% (1)
- Mls 419: Aubf Lab Semen Analysis 5% Spermatozoa 60-70% Seminal Fluid 20-30% Prostate FluidDocument24 pagesMls 419: Aubf Lab Semen Analysis 5% Spermatozoa 60-70% Seminal Fluid 20-30% Prostate FluidLyra Dennise LlidoNo ratings yet
- MTLB Week 1 and 2Document86 pagesMTLB Week 1 and 2Josh Buenafe Macapallag100% (1)
- AUBF SemenDocument7 pagesAUBF SemenRichelyn Grace B. VenusNo ratings yet
- Hematology 1Document5 pagesHematology 1jaish8904100% (1)
- Hematology Peripheral Blood SmearDocument7 pagesHematology Peripheral Blood SmearJosephine Armanne AluyenNo ratings yet
- Blood Cell AnomaliesDocument4 pagesBlood Cell AnomaliesCiullaeNo ratings yet
- Hematology ReviewerDocument4 pagesHematology ReviewerAbigail Puno100% (1)
- Hematology ReviewerDocument10 pagesHematology ReviewerAldren BeliberNo ratings yet
- RBC InclusionsDocument6 pagesRBC Inclusionsjingx5100% (1)
- Routine Laboratory Evaluation of CoagulationDocument32 pagesRoutine Laboratory Evaluation of CoagulationArshie08No ratings yet
- Mixing StudiesDocument14 pagesMixing StudiesHery PriyantoNo ratings yet
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- HistopathDocument23 pagesHistopathElla SalesNo ratings yet
- 11 - Hemostasis & Blood CoagulationDocument66 pages11 - Hemostasis & Blood CoagulationISRAELNo ratings yet
- General Approach in Investigation of Haemostasis: Lecture 2: Bleeding TimeDocument28 pagesGeneral Approach in Investigation of Haemostasis: Lecture 2: Bleeding TimeClorence John Yumul FerrerNo ratings yet
- Hematology Lecture Notes PDFDocument102 pagesHematology Lecture Notes PDFMarisa IzzaNo ratings yet
- Platelet Count ManualDocument2 pagesPlatelet Count ManualAli Ahmad Khameini100% (1)
- Hematology 1 L2 Hematopoiesis LectureDocument4 pagesHematology 1 L2 Hematopoiesis LectureChelze Faith DizonNo ratings yet
- Module 2 CANVAS NOTES HematopoiesisDocument6 pagesModule 2 CANVAS NOTES HematopoiesisMohammad MasacalNo ratings yet
- Hematology Module 2 and 3Document11 pagesHematology Module 2 and 3SEAN MELNOR LOSBAÑESNo ratings yet
- Hematopoiesis GuideDocument8 pagesHematopoiesis GuideASHLEY ALEXIS GUEVARRANo ratings yet
- 2 - Introduction To Hematopoiesis and RBC ProductionDocument71 pages2 - Introduction To Hematopoiesis and RBC ProductionClaire GonoNo ratings yet
- Graphic Organizer Assignment Checklist RubricDocument3 pagesGraphic Organizer Assignment Checklist Rubricapi-335603391No ratings yet
- Lecture 1 - Animal Cell Types and TissuesDocument67 pagesLecture 1 - Animal Cell Types and TissuesEthel Gerardo PabloNo ratings yet
- Biopharma Expression Systems 080926Document340 pagesBiopharma Expression Systems 080926Sungsik ParkNo ratings yet
- Fish immune system and vaccines-Springer (2022)-1Document293 pagesFish immune system and vaccines-Springer (2022)-1Rodolfo Velazco100% (1)
- Protein-Protein Interaction Analysis of Alzheimer's Disease and NAFLD Based On Systems Biology Methods Unhide Common Ancestor PathwaysDocument7 pagesProtein-Protein Interaction Analysis of Alzheimer's Disease and NAFLD Based On Systems Biology Methods Unhide Common Ancestor PathwaysRicardo CastilloNo ratings yet
- The Cell As The Basic Unit of Life: Multiple-Choice QuestionsDocument72 pagesThe Cell As The Basic Unit of Life: Multiple-Choice QuestionsRyan100% (1)
- Phagocytosis Assay Kit (Igg Fitc) : Item No. 500290Document9 pagesPhagocytosis Assay Kit (Igg Fitc) : Item No. 500290drfiatNo ratings yet
- Histology of Nervous TissueDocument40 pagesHistology of Nervous TissueSHARON MARIA SUNNYNo ratings yet
- Fatty Acid Synthesis and RegulationDocument13 pagesFatty Acid Synthesis and RegulationrJNo ratings yet
- Biochemistry Course Outline FinalDocument3 pagesBiochemistry Course Outline FinalMiriam JonesNo ratings yet
- NK Cells MemoryDocument8 pagesNK Cells MemoryDanielaNo ratings yet
- Biology Multiple Choice ReviewDocument3 pagesBiology Multiple Choice ReviewGlen MillarNo ratings yet
- Capturing Light Energy in PhotosynthesisDocument3 pagesCapturing Light Energy in PhotosynthesisJulia ZouNo ratings yet
- Jadual Spesifikasi Ujian Bio t4Document2 pagesJadual Spesifikasi Ujian Bio t4Elyna Tony MuntingNo ratings yet
- AquactivLS BrochureDocument2 pagesAquactivLS Brochurepjanovic.rajkaNo ratings yet
- Urticaria and AngioedemaDocument40 pagesUrticaria and AngioedemaDea LeeteukNo ratings yet
- Transes Anaphy BloodDocument5 pagesTranses Anaphy BloodPia LouiseNo ratings yet
- CAPE Biology Past Papers 2006Document10 pagesCAPE Biology Past Papers 2006Leighton ThompsonNo ratings yet
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFDocument9 pagesChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFChethranNo ratings yet
- AS LEVEL BIOLOGY Paper 1 EnzymesDocument54 pagesAS LEVEL BIOLOGY Paper 1 EnzymesADEEL AHMADNo ratings yet
- Intro To Biohacking: or "How I Learned To Stop Worrying and Love The Zombie Apocalypse"Document31 pagesIntro To Biohacking: or "How I Learned To Stop Worrying and Love The Zombie Apocalypse"rasromeoNo ratings yet
- 2 CHO Structures SlidesDocument36 pages2 CHO Structures SlidesRicky GargNo ratings yet
- Transfer of Genetic InformationDocument13 pagesTransfer of Genetic InformationjaneNo ratings yet
- Question Paper 2nd YearDocument2 pagesQuestion Paper 2nd YearRay MrinalNo ratings yet
- An Introduction To Molecular Biology: Savannah Mwesigwa Adapted From Aala A. AbulfarajDocument25 pagesAn Introduction To Molecular Biology: Savannah Mwesigwa Adapted From Aala A. AbulfarajMwanja MosesNo ratings yet
- MICRODocument9 pagesMICROCyrelle Heart YoshikawaNo ratings yet
- General Biology 1Document16 pagesGeneral Biology 1marushu valoNo ratings yet
- Stella MIN - 3.2 BioNinja WorksheetDocument2 pagesStella MIN - 3.2 BioNinja WorksheetStella Min Eun SuNo ratings yet
- Review: Translational Regulation of Gene Expression During Conditions of Cell StressDocument10 pagesReview: Translational Regulation of Gene Expression During Conditions of Cell StressBayan GhanimNo ratings yet
- Prausnitz Derm Book Chapter 2012Document10 pagesPrausnitz Derm Book Chapter 2012Valentina AdindaNo ratings yet