Professional Documents
Culture Documents
2 PB
2 PB
Uploaded by
Pororo KewrenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 PB
2 PB
Uploaded by
Pororo KewrenCopyright:
Available Formats
Scrofuloderma: A Diagnosis to Bear in Mind in the Western
World
CASO CLÍNICO
Escrofuloderma: Um Diagnóstico a Ponderar no Mundo
Ocidental
Mariana BATISTA1, Barbara FERREIRA1, Gonçalo CRUZ2, Américo FIGUEIREDO1
Acta Med Port 2019 Apr;32(4):313-316 ▪ https://doi.org/10.20344/amp.10329
ABSTRACT
The incidence of tuberculosis has been increasing worldwide. Contrarily, a recent decrease in Portugal has been reported. Cutaneous
tuberculosis comprises a low percentage of all cases. We report a 70-year-old female with a 2-month-history of painful, nodular,
suppurative lesions in the groin area, bilaterally. Previous history was remarkable for Human Immunodeficiency Virus infection and
stage-IIIB cervical cancer. A skin biopsy, stained with periodic acid–Schiff and Fite’s stain, polymerase chain reaction on purulent
discharge and mycobacterial culture of the skin were performed, leading to the diagnosis of scrofuloderma. Tuberculostatic therapy
was initiated and complete response was observed. This case depicts an uncommon variant of tuberculosis, highlighting the need for
awareness of the cutaneous variants of tuberculosis that, although rare, can still present in the clinic today.
Keywords: Tuberculosis, Cutaneous
RESUMO
A incidência de tuberculose tem vindo a aumentar globalmente. Em Portugal, porém, esta incidência diminuiu na última década. A
tuberculose cutânea representa uma pequena percentagem de todos os casos. Apresenta-se o caso de uma mulher de 70 anos com
nódulos supurativos da região inguinal bilateralmente, dolorosos, evoluindo há 2 meses. Como antecedentes relevantes, apresentava
infeção por vírus da imunodeficiência humana e carcinoma do colo do útero, estadio IIIB. Foram realizadas biópsia cutânea (coloração
pelo ácido periódico de Shiff e coloração de Fite), pesquisa de micobactérias por polymerase chain reaction e estudo microbiológico
por cultura, tendo sido estabelecido o diagnóstico de escrofuloderma. Iniciou terapêutiva tuberculostática com resposta favorável. Este
artigo realça a importância do reconhecimento das formas cutâneas de tuberculose e a necessidade de manter um elevado índice de
suspeição, sobretudo em pacientes imunodeprimidos.
Palavras-chave: Tuberculose Cutânea
INTRODUCTION
Over the last few years the incidence of tuberculosis cant clinical findings. The patient was afebrile and denied
has increased worldwide especially due to the increasing night sweats or other systemic symptoms, and had not
incidence of human immunodeficiency virus (HIV),1 which traveled abroad.
is ultimately responsible for most deaths among these pa- Previous history was remarkable for HIV seropositivity
tients.2,3 In Portugal, tuberculosis is still an important health diagnosed 8 years before, under antiretroviral therapy with
care issue, although its incidence has been dropping – with a current CD4 count of 242/mm3, negative viral load, and
an estimate of 16.5 new cases for 100 000 inhabitants, with stage-IIIB cervical cancer treated with a chemo-radiothera-
the majority of cases reported in the districts of Lisbon and py scheme that had finished 2 years before.
Porto.4 Given the clinical picture described, the main diagnos-
Cutaneous involvement, although classical, remains an tic considerations included cutaneous metastases, myco-
uncommon presentation of tuberculosis, comprising only bacterial and deep fungal infections. However, sexually
1.0% - 1.5% of all extra-pulmonary manifestations.5-7 Cu- transmitted diseases were also excluded, namely venereal
taneous tuberculosis can be acquired exogenously (direct lymphogranuloma, syphilis, gonorrhea, herpes virus and
inoculation) or endogenously (contiguous infection or he- cytomegalovirus infections.
matogenous dissemination) and can present a wide variety A skin biopsy showed a dermal tuberculoid granuloma-
of clinical features.8 tous infiltrate with caseous necrosis, containing numerous
multinucleated giant cells of the Langhans type accompa-
CASE REPORT nied by a rim of lymphocytes, plasma cells and occasional
A 70-year-old caucasian female was seen with a eosinophils (Fig. 2). Periodic acid–Schiff (PAS) and Fite’s
2-month-history of multiple, painful, erythematous, nodular, staining were negative. Polymerase chain reaction (PCR)
ulcerated and suppurative lesions in the groin area, bilater- performed on the exsudate revealed the presence of My-
ally (Fig. 1). cobacterium tuberculosis complex and routine bacterial
Physical examination revealed palpable inguinal lym- culture was positive for Mycobacterium tuberculosis (MTB)
phadenopathy on the right side, without any other signifi- (confirmed only 4 weeks later). IGRA (interferon gamma
1. Dermatology Department. Hospitais da Universidade de Coimbra. Centro Hospitalar e Universitário de Coimbra. Coimbra. Portugal.
2. Infectious Diseases Department. Hospitais da Universidade de Coimbra. Centro Hospitalar e Universitário de Coimbra. Coimbra. Portugal.
Autor correspondente: Mariana Batista. sousabatistamariana@gmail.com
Recebido: 01 de fevereiro de 2018 - Aceite: 19 de junho de 2018 | Copyright © Ordem dos Médicos 2019
Revista Científica da Ordem dos Médicos 313 www.actamedicaportuguesa.com
Batista M, et al. Scrofuloderma: a case report, Acta Med Port 2019 Apr;32(4):313-316
CASO CLÍNICO
Figure 1 – Erythematous nodular lesions in the groin area with ulceration and suppurative content
release assay) test was also positive. A computed tomog- charge. This clinical manifestation is classically described
raphy scan showed contiguity between inguinal nodes and in young patients,10 and is more often seen in the axillae,
the overlying skin surface (Fig. 3). Chest x-ray did not re- neck, groin and chest.11,12 It’s mainly associated with a state
veal any abnormality. of lower immunity, with accompanying lower number of lym-
The patient began treatment with a combination of phocytes present in the granulomas and higher bacillary
pyrazinamide, isoniazid, ethambutol and rifampicin and her counts.
condition improved considerably in just two weeks of treat- It’s interesting to note that other variants of cutaneous
ment. After 3 months of treatment only scarring was present tuberculosis – such as lupus vulgaris and tuberculosis ver-
(Fig. 4). rucosa cutis, are associated with higher and intermediate
immunocompetence states, respectively.13
DISCUSSION Given the many clinical features of cutaneous tubercu-
Scrofuloderma is a variant of cutaneous tuberculosis losis and the fact that lesions resemble many other derma-
resulting from endogenous spread of the infection from a tological conditions, diagnosis can be difficult and requires
contiguous underlying focus, usually a lymph node or bone, correlation between clinical findings and diagnostic tests. In
with breakdown of the skin.9 The lesion starts as a subcuta- face of the delay in obtaining microbiological confirmation
neous, mobile nodule, which attaches to the overlying skin – 4 weeks, PCR can be of value. It has high sensitivity and
afterwards leading to abscess formation and purulent dis- specificity, with results in less than 24 - 48 hours. However,
A B
Figure 2 – (A) Diffuse epidermal hyperplasia with dermal granulomatous infiltrate of tuberculoid type. (B) Central necrosis with numerous
multinucleated giant cells of the Langhans type. Haematoxylin and eosin, original magnification (A) x 40, (B) x 200.
Revista Científica da Ordem dos Médicos 314 www.actamedicaportuguesa.com
Batista M, et al. Scrofuloderma: a case report, Acta Med Port 2019 Apr;32(4):313-316
CASO CLÍNICO
Figure 3 – Chest-abdomen-pelvis CT showing a contiguity between the nodular lesions and the skin (yellow arrows)
a positive result may not always correspond to an active in- weeks later. Sensitivity testing showed susceptibility to first-
fection and a negative result does not exclude it. Therefore, line tuberculostatics. The recommended treatment for cuta-
despite its utility, clinical correlation in mandatory14,15 In the neous tuberculosis is the same as for systemic disease (two
setting of compatible clinical and histological features, even months of isoniazid, rifampin, ethambutol and pyrazinamide
without a microbiological confirmation, tuberculostatic treat- plus four months of isoniazid and rifampin). This scheme
ment should be started and, in these cases, the response to was carried out in our patient with good response.
treatment can support the diagnosis. This case is remarkable for several features: an uncom-
In our patient, on clinical grounds alone, there was a mon presentation of tuberculosis – scrofuloderma - in a
possibility of cutaneous metastases from cervical cancer, higher age group than average, maybe due to HIV-immu-
given her medical history. However, the presence of typi- nosuppression, with negative histochemical stain for myco-
cal tuberculoid granulomas in the skin combined with posi- bacteria in the cutaneous biopsy (unusual, although previ-
tive PCR for MBT, pointed to scrofuloderma, even in the ously described), with a positive PCR for MBT and positive
absence of positive FITE and PAS stainings on histopa- mycobacterial tissue culture.
thology. This was ultimately confirmed by isolation of MBT Tuberculosis is still an important health issue and cli-
on routine bacterial culture (Löwestein-Jensen medium) 4 nicians should be aware of atypical clinical presentations,
especially in the context of immunosuppression. Timely in-
vestigation is key and can prevent further complications.
OBSERVATIONS
This case was presented as a clinical case report in the
Congress: Reunião da Primavera - Sociedade Portuguesa
de Dermatologia e Venereologia, Lisbon, 2-3 June 2017.
PROTECTION OF HUMANS AND ANIMALS
The authors declare that the procedures were followed
according to the regulations established by the Clinical Re-
search and Ethics Committee and to the Helsinki Declara-
tion of the World Medical Association.
Figure 4 – Clinical appearance after three months of treatment
Revista Científica da Ordem dos Médicos 315 www.actamedicaportuguesa.com
Clérigo V, et al. Granulomatous pneumonitis due to intravesical BCG, Acta Med Port 2019 Apr;32(4):316-320
DATA CONFIDENTIALITY CONFLICTS OF INTEREST
The authors declare having followed the protocols in All authors report no conflict of interest.
use at their working center regarding patients’ data publica-
CASO CLÍNICO
tion. FUNDING SOURCES
This research received no specific grant from any fund-
PATIENT CONSENT ing agency in the public, commercial, or not-for-profit sec-
Obtained. tors.
REFERENCES
1. Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, 7. van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and
et al. The growing burden of tuberculosis: global trends and interactions current treatment regimens. Tuberculosis. 2015;95:629-38.
with the HIV epidemic. Arch Intern Med. 2003;163:1009-21. 8. Beyt BE Jr, Ortbals DW, Santa Cruz DJ, Kobayashi GS, Eisen AZ,
2. Koenig SP, Riviere C, Leger P, Joseph P, Severe P, Parker K, et al. Medoff G. Cutaneous mycobacteriosis: analysis of 34 cases with a new
High mortality among patients with AIDS who received a diagnosis of classification of the disease. Medicine. 1981;60:95-109.
tuberculosis in the first 3 months of antiretroviral therapy. Clin Infect Dis. 9. Hill MK, Sanders CV. Cutaneous tuberculosis. Microbiol Spectr. 2017;5.
2009;48:829-31. 10. Ilgazli A, Boyaci H, Basyigit I, Yildiz F. Extrapulmonary tuberculosis:
3. Etard JF, Ndiaye I, Thierry-Mieg M, Guèye N, Guèye P, Lanièce I, et clinical and epidemiologic spectrum of 636 cases. Med Res Arch.
al. Mortality and causes of death in adults receiving highly active 2004;35:435-41.
antiretroviral therapy in Senegal: a 7- year cohort study. AIDS. 11. Concha RM, Fich SF, Rabagliati BR, Pinto SC, Rubio LR, Navea DÓ, et
2006;20:1181-9. al. Cutaneous tuberculosis: two cases and review. Rev Chilena Infectol.
4. Direção Geral da Saúde. Programa Nacional para a Infeção VIH, SIDA 2011;28:262-8.
e Tuberculose 2017. [consulted 2017 Dec 16]. Available from: http:// 12. Kim GW, Park HJ, Kim HS, Kim SH, Ko HC, Kim BS, et al. Delayed
www.dgs.pt/portal-da- estatistica-da- saude/diretorio-de- informacao/ diagnosis of scrofuloderma misdiagnosed as a bacterial abscess. Ann
diretorio-de- informacao/por-serie- 845551- pdf.aspx?v=11736b14- Dermatol. 2012;24:70-3.
73e6- 4b34-a8e8- d22502108547. 13. Ramos-e- Silva M, Castro MC. Mycobacterial infections. In: Bolognia JL,
5. Zhang J, Fan YK, Wang P, Chen QQ, Wang G, Xu AE, et al. Cutaneous Schaffer JV, Cerroni L. Dermatology. Elsevier; 2018. p. 1296-318.
tuberculosis in China: a multicenter retrospective study of cases 14. Hsiao PF, Tzen CY, Chen HC, Su HY. Polymerase chain reaction
diagnosed between 1957 and 2013. J Eur Acad Dermatol Venereol. J based detection of Mycobacterium tuberculosis in tissues showing
Eur Acad Dermatol Venereol. 2018;32:632-8. granulomatous inflammation without demonstrable acid-fast bacilli. Int.
6. Kivanc-Altunay I, Baysal Z, Ekmekçi TR, Koslu A. Incidence of J. Dermatol. 2003;42:281-6.
cutaneous tuberculosis in patients with organ tuberculosis. Int J 15. Bento J, Silva AS, Rodrigues F, Duarte R. Diagnostic tools in
Dermatol. 2003;42:197-200. tuberculosis. Acta Med Port. 2011;24:145-54.
A Rare Case of Granulomatous Pneumonitis Due to
Intravesical BCG for Bladder Cancer
Um Caso Raro de Pneumonite Granulomatosa
Secundária a Instilação Intravesical de BCG no Contexto
de Neoplasia da Bexiga
Vera CLÉRIGO1, Ana CASTRO2, Teresa MOURATO2, Conceição GOMES2
Acta Med Port 2019 Apr;32(4):316-320 ▪ https://doi.org/10.20344/amp.10250
ABSTRACT
Granulomatous pneumonitis is a rare complication of bacillus Calmette-Guerin immunotherapy following intravesical administration of
bacillus Calmette-Guerin. The authors present an unusual case of a 67-year-old man who developed mild and non-specific symptoms,
following intravesical bacillus Calmette-Guerin instillations. Examinations revealed features of miliary tuberculosis and granuloma sug-
gestive of mycobacterial infection. Anti-tuberculosis treatment resulted in a remarkable improvement in his symptoms and gradually
upgrading of radiological appearance. The symptoms were less severe than some others described but this case provides evidence
that, even in some cases, specific treatment may be necessary. We highlight the importance of recognizing miliary Mycobacterium bo-
vis as a probable complication of bacillus Calmette-Guerin immunotherapy. The clinical disease course can be mild, despite extensive
bilateral miliary nodules on primary presentation.
Keywords: BCG Vaccine; Granuloma/chemically induced; Pneumonia/chemically induced; Urinary Bladder Neoplasms/drug therapy
RESUMO
A pneumonite granulomatosa é uma complicação rara da imunoterapia com bacillus Calmette-Guerin após administração intravesical
de bacillus Calmette-Guerin. Os autores apresentam um caso incomum de um homem de 67 anos de idade que desenvolveu
sintomas ligeiros e inespecíficos, após instilações de bacillus Calmette-Guerin intravesical. Os exames revelaram características da
1. Pulmonology – Thorax Department, Centro Hospitalar Lisboa Norte, Lisboa, Portugal.
2. Pulmonary Diagnosis Center Dr. Ribeiro Sanches, Lisboa, Portugal.
Autor correspondente: Vera Clérigo. vclerigo21@gmail.com
Recebido: 15 de janeiro de 2018 - Aceite: 17 de agosto de 2018 | Copyright © Ordem dos Médicos 2019
Revista Científica da Ordem dos Médicos 316 www.actamedicaportuguesa.com
You might also like
- TB Cutis 3Document9 pagesTB Cutis 3Vika CikitaNo ratings yet
- Ports and Marines FacilitiesDocument36 pagesPorts and Marines Facilities허윤호No ratings yet
- 13 Tuberculosis Cutánea Como Absceso Tuberculoso MetastásicoDocument3 pages13 Tuberculosis Cutánea Como Absceso Tuberculoso Metastásicojhon_4548No ratings yet
- Escholarship UC Item 55d3f43cDocument5 pagesEscholarship UC Item 55d3f43cDhessy SusantoNo ratings yet
- Case Report: Leprosy and Tuberculosis Co-Infection: Clinical and Immunological Report of Two Cases and Review of The LiteratureDocument5 pagesCase Report: Leprosy and Tuberculosis Co-Infection: Clinical and Immunological Report of Two Cases and Review of The LiteraturekristinaNo ratings yet
- Jcad 2 10 19 PDFDocument9 pagesJcad 2 10 19 PDFAkbal Nur KarimNo ratings yet
- Diagnosis BandingDocument7 pagesDiagnosis BandingSyafar SmNo ratings yet
- Tuberculosis of The Cavum Case ReportDocument3 pagesTuberculosis of The Cavum Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- CUTANEOUS Tuberculosis - AjmDocument3 pagesCUTANEOUS Tuberculosis - Ajmfredrick damianNo ratings yet
- A Case of Skin and Soft Tissue Infection Caused by Mycobacterium AbscessusDocument4 pagesA Case of Skin and Soft Tissue Infection Caused by Mycobacterium AbscessusAnonymous so6ZnlKywNo ratings yet
- Case Report Paracoccidioidomycosis in A Liver Transplant RecipientDocument6 pagesCase Report Paracoccidioidomycosis in A Liver Transplant RecipientCarlos AlbertoNo ratings yet
- Ajmcr 10 1 1Document4 pagesAjmcr 10 1 1jghcl.221No ratings yet
- Presternal Scrofuloderma in A HIV Infected Patient Case Report and Discussion of The Literature DataDocument5 pagesPresternal Scrofuloderma in A HIV Infected Patient Case Report and Discussion of The Literature DataAthenaeum Scientific PublishersNo ratings yet
- Malignant Syphilis As The Presenting Complaint of Advanced HIVDocument4 pagesMalignant Syphilis As The Presenting Complaint of Advanced HIVManuel López FuentesNo ratings yet
- Actaapa 2021 23Document3 pagesActaapa 2021 23Saifani AzzamNo ratings yet
- Pi Is 0278239103007407Document5 pagesPi Is 0278239103007407tengoplatita2008No ratings yet
- ScrofulodermDocument4 pagesScrofulodermIzmi AzizahNo ratings yet
- Medicine: An Unusual Extranodal Natural Killer/t-Cell Lymphoma Presenting As Chronic LaryngitisDocument4 pagesMedicine: An Unusual Extranodal Natural Killer/t-Cell Lymphoma Presenting As Chronic Laryngitisnurul atika havizNo ratings yet
- Parakeratosis Variegata: A Possible Role of Environmental Hazards?Document4 pagesParakeratosis Variegata: A Possible Role of Environmental Hazards?Ega AihenaNo ratings yet
- Clinical Patterns of Cutaneous Nontuberculous Mycobacterial InfectionsDocument8 pagesClinical Patterns of Cutaneous Nontuberculous Mycobacterial Infectionsluck2livNo ratings yet
- GM 09055Document6 pagesGM 09055inggitsiregarNo ratings yet
- Scrofuloderma: A Common Type of Cutaneous Tuberculosis. A Case ReportDocument5 pagesScrofuloderma: A Common Type of Cutaneous Tuberculosis. A Case ReportIndah IndrianiNo ratings yet
- Landouzy Septicemia (Sepsis Tuberculosa Acutissima) Due To Mycobacterium Microti in An Immunocompetent ManDocument4 pagesLandouzy Septicemia (Sepsis Tuberculosa Acutissima) Due To Mycobacterium Microti in An Immunocompetent Manreadyboy89No ratings yet
- Coexistence of Cutaneous Tuberculosis (Scrofuloderma) and Hanseniasis-A Rare PresentationDocument2 pagesCoexistence of Cutaneous Tuberculosis (Scrofuloderma) and Hanseniasis-A Rare PresentationGesza Utama PutraNo ratings yet
- Cold AbscessDocument5 pagesCold AbscesssaikrishnamedicoNo ratings yet
- Rakesh Kumar Mahajan, Et AlDocument4 pagesRakesh Kumar Mahajan, Et AlMark JohnsonNo ratings yet
- Histoplasmosis Review INF DIS CLIN NA 2021Document21 pagesHistoplasmosis Review INF DIS CLIN NA 2021Tatiana DiazNo ratings yet
- Cutaneous Tuberculosis - StatPearls - NCBI BookshelfDocument5 pagesCutaneous Tuberculosis - StatPearls - NCBI BookshelfLinuel Quetua TrinidadNo ratings yet
- Answers To Continuing Medical Education QuestionsDocument2 pagesAnswers To Continuing Medical Education QuestionsKhalid AbdullahNo ratings yet
- 2016 Piis1201971216310761Document4 pages2016 Piis1201971216310761Soraya Eugenia Morales LópezNo ratings yet
- Infectious Diseases: A Case of Tuberculosis Verrucosa Cutis in Brazil Undiagnosed For 15 YearsDocument3 pagesInfectious Diseases: A Case of Tuberculosis Verrucosa Cutis in Brazil Undiagnosed For 15 YearsAnthony SetiawanNo ratings yet
- Cutaneous Tuberculosis: Epidemiologic, Etiopathogenic and Clinical Aspects - Part IDocument10 pagesCutaneous Tuberculosis: Epidemiologic, Etiopathogenic and Clinical Aspects - Part IDellNo ratings yet
- Human OrfDocument3 pagesHuman OrfDeba P SarmaNo ratings yet
- Lectura 4 Seminario Micosis ProfundaDocument3 pagesLectura 4 Seminario Micosis ProfundaAlessandra Saravia PachecoNo ratings yet
- Journal Reading - Muhamad Al Hafiz - 1920221169Document12 pagesJournal Reading - Muhamad Al Hafiz - 1920221169David Al Haviz100% (1)
- Pi Is 0190962214011566Document2 pagesPi Is 0190962214011566LewishoppusNo ratings yet
- Changing Pattern of Cutaneous Tuberculosis: A Prospective StudyDocument7 pagesChanging Pattern of Cutaneous Tuberculosis: A Prospective StudyErtyWitalayaL.ToruanNo ratings yet
- LungIndia323241-4636559 125245Document5 pagesLungIndia323241-4636559 125245Nishant AggarwalNo ratings yet
- Inflammatory Conditions Mimicking Tumours in Calabar: A 30 Year Study (1978-2007)Document7 pagesInflammatory Conditions Mimicking Tumours in Calabar: A 30 Year Study (1978-2007)International Organization of Scientific Research (IOSR)No ratings yet
- Therapeutic Hotline: Tinea Profunda of The Genital Area. Successful Treatment of A Rare Skin DiseaseDocument3 pagesTherapeutic Hotline: Tinea Profunda of The Genital Area. Successful Treatment of A Rare Skin Diseasesoekarnohatta94No ratings yet
- Disseminated Tuberculous Myositis in A Child With Acut 2009 Pediatrics NeoDocument4 pagesDisseminated Tuberculous Myositis in A Child With Acut 2009 Pediatrics NeoFrankenstein MelancholyNo ratings yet
- Lucivero Et Al 2011 Lupus Mastitis in Systemic Lupus Erythematosus A Rare Condition Requiring A Minimally InvasiveDocument5 pagesLucivero Et Al 2011 Lupus Mastitis in Systemic Lupus Erythematosus A Rare Condition Requiring A Minimally Invasiveruthdaniel6041No ratings yet
- Jurnal 2Document3 pagesJurnal 2Renita Mandalinta SitepuNo ratings yet
- Case Report Paracoccidioidomycosis in A Liver Transplant RecipientDocument3 pagesCase Report Paracoccidioidomycosis in A Liver Transplant RecipientCarlos AlbertoNo ratings yet
- An Unusual Case of Transient Neonatal Pustular Melanosis: A Diagnostic PuzzleDocument4 pagesAn Unusual Case of Transient Neonatal Pustular Melanosis: A Diagnostic PuzzlecebadawitNo ratings yet
- Efficacy of Fine Needle Aspiration Cytology, Ziehl-Neelsen Stain and Culture (Bactec) in Diagnosis of Tuberculosis LymphadenitisDocument4 pagesEfficacy of Fine Needle Aspiration Cytology, Ziehl-Neelsen Stain and Culture (Bactec) in Diagnosis of Tuberculosis LymphadenitisTëk AñdotNo ratings yet
- Respiratory Medicine Case ReportsDocument3 pagesRespiratory Medicine Case ReportsPororo KewrenNo ratings yet
- Endemic Mycosis: Review Questions: Self-Assessment in Infectious DiseasesDocument2 pagesEndemic Mycosis: Review Questions: Self-Assessment in Infectious DiseasesNicolas CortezNo ratings yet
- Otolaryngology Case Reports: Dominique Bohorquez, Jason G. Newman, John Stern, Karthik Rajasekaran TDocument3 pagesOtolaryngology Case Reports: Dominique Bohorquez, Jason G. Newman, John Stern, Karthik Rajasekaran TarifcetungtakNo ratings yet
- Tuberculosis Verrucosa Cutis: Case Report of A Diagnostic ChallengeDocument4 pagesTuberculosis Verrucosa Cutis: Case Report of A Diagnostic Challengeyerich septaNo ratings yet
- Scrofuloderma: Images in DermatologyDocument1 pageScrofuloderma: Images in DermatologyAkira MasumiNo ratings yet
- Cryptococcal Cellulitis in A Patient With Myelodysplastic SyndromeDocument2 pagesCryptococcal Cellulitis in A Patient With Myelodysplastic SyndromeSan Maria SitompulNo ratings yet
- RJZ 269Document3 pagesRJZ 269Saffa AzharaaniNo ratings yet
- Fine-Needle Aspiration Cytology in The Diagnosis of Tuberculous LesionsDocument9 pagesFine-Needle Aspiration Cytology in The Diagnosis of Tuberculous Lesionsmohamaed abbasNo ratings yet
- Case Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureDocument6 pagesCase Report: Subcorneal Pustular Dermatosis in Childhood: A Case Report and Review of The LiteratureIrsalinaHusnaAzwirNo ratings yet
- The History Holds The Key in This Gardener With A Skin InfectionDocument4 pagesThe History Holds The Key in This Gardener With A Skin InfectionPercy Ureta SierraNo ratings yet
- Venkatraman K PDFDocument3 pagesVenkatraman K PDFRana Zara AthayaNo ratings yet
- Artigo 5 Relato de CasoDocument6 pagesArtigo 5 Relato de Casobreno menezesNo ratings yet
- Jurnal KedokteranDocument4 pagesJurnal Kedokteranbunga farnadaNo ratings yet
- Two Cases of Pulmonary Tuberculosis Caused by Mycobacterium Tuberculosis SubspDocument7 pagesTwo Cases of Pulmonary Tuberculosis Caused by Mycobacterium Tuberculosis Subspmitz_ni_pits10No ratings yet
- Cutaneous Lymphomas: Unusual Cases 3From EverandCutaneous Lymphomas: Unusual Cases 3Oleg E. AkilovNo ratings yet
- Update SkrofulodermaDocument8 pagesUpdate SkrofulodermaPororo KewrenNo ratings yet
- Respiratory Medicine Case ReportsDocument3 pagesRespiratory Medicine Case ReportsPororo KewrenNo ratings yet
- Nihms 445487Document13 pagesNihms 445487Pororo KewrenNo ratings yet
- TB in ChildrenDocument7 pagesTB in ChildrenPororo KewrenNo ratings yet
- Blok Metode Belajar Evidence Based Medicine: Disusun Oleh: Nama: Hanny Silviana NPM: 1102016080Document7 pagesBlok Metode Belajar Evidence Based Medicine: Disusun Oleh: Nama: Hanny Silviana NPM: 1102016080Pororo KewrenNo ratings yet
- Report On Special Assignment "Implementation of 8-Bit ALU On SPARTAN-3"Document18 pagesReport On Special Assignment "Implementation of 8-Bit ALU On SPARTAN-3"Dhruv Joshi100% (6)
- Carvin Schematic - s204000CDocument2 pagesCarvin Schematic - s204000CdodNo ratings yet
- Non ProfitDocument7 pagesNon ProfitBabatunde DokunNo ratings yet
- M-Series Replacement Poster M-300 en SPDocument2 pagesM-Series Replacement Poster M-300 en SPCarlos Bravo MaciasNo ratings yet
- Spatial: Buffer ToolDocument5 pagesSpatial: Buffer ToolSubhrangsu AdhikariNo ratings yet
- 5 Great Anthropologists of India and Their Contributions in The Field of AnthropologyDocument5 pages5 Great Anthropologists of India and Their Contributions in The Field of AnthropologyVersha BansalNo ratings yet
- Ignition System: Tech A Tech BDocument8 pagesIgnition System: Tech A Tech BHiếuNo ratings yet
- Principles of Neutralization TitrationDocument32 pagesPrinciples of Neutralization TitrationAldwin CantosNo ratings yet
- Introduction To Healthcare System of IndiaDocument22 pagesIntroduction To Healthcare System of Indiakratika GaurNo ratings yet
- Defining Social Sciences As The Study of SocietyDocument8 pagesDefining Social Sciences As The Study of SocietyMari Zechnas OsnolaNo ratings yet
- IGuard LM Manual ENGDocument92 pagesIGuard LM Manual ENGAntónio LeitãoNo ratings yet
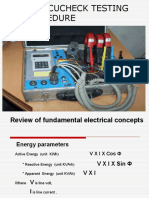
- LT Accucheck Testing ProcedureDocument15 pagesLT Accucheck Testing ProcedureGautam ChattopadhyayNo ratings yet
- 2010 Fodera Price ListDocument3 pages2010 Fodera Price ListPhil BassNo ratings yet
- Root Resorption Diagnosis, Classification and Treatment Choices Based On Stimulation FactorsDocument8 pagesRoot Resorption Diagnosis, Classification and Treatment Choices Based On Stimulation FactorsAhmad AssariNo ratings yet
- DUB01CB Eng PDFDocument4 pagesDUB01CB Eng PDFAnonymous hj273CMNo ratings yet
- Science and Technology Humanities and Social SciencesDocument2 pagesScience and Technology Humanities and Social SciencesThanawan ChakkhuchanNo ratings yet
- Times NIE Web Ed June18 2021Document4 pagesTimes NIE Web Ed June18 2021sdNo ratings yet
- Communication Skills in EnglishDocument13 pagesCommunication Skills in Englishpavan panwalaNo ratings yet
- Tattle TaleDocument3 pagesTattle TaleFilipino ZinergyNo ratings yet
- Kreativnost I Emocije - Frias I Dr.Document15 pagesKreativnost I Emocije - Frias I Dr.Dragana Veljković StankovićNo ratings yet
- Lemon Meringue Custard With Violet SpongeDocument24 pagesLemon Meringue Custard With Violet SpongeLaenNo ratings yet
- Full FormDocument1 pageFull Formmohit bohraNo ratings yet
- Sanskrit Siddhantas & VedasDocument6 pagesSanskrit Siddhantas & VedasnairsdocsNo ratings yet
- Case Study - Wal-Mart Failure in GermanyDocument5 pagesCase Study - Wal-Mart Failure in GermanyYasser SadekNo ratings yet
- SKMT Tot For Ydos-2023-ProgramDocument1 pageSKMT Tot For Ydos-2023-ProgramCrafty PsycheNo ratings yet
- Practice Test: Very SimilarDocument7 pagesPractice Test: Very SimilarAfzal ShaikhNo ratings yet
- ResearchDocument5 pagesResearchNyhtes EsohpNo ratings yet
- English Newspaper ThingyDocument13 pagesEnglish Newspaper Thingytimothy.imannuelNo ratings yet
- WeldingDocument23 pagesWeldingSuneel Kumar MeenaNo ratings yet