Professional Documents
Culture Documents
Pityriasis Rubra Pilaris in A 3-Year-Old Male
Uploaded by
Nicolás ArcosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pityriasis Rubra Pilaris in A 3-Year-Old Male
Uploaded by
Nicolás ArcosCopyright:
Available Formats
MILITARY MEDICINE, 181, 3:e298, 2016
Pityriasis Rubra Pilaris in a 3-Year-Old Male
CPT Stephen K. Stacey, MC USA*; Steven J. Novek, MD†; LTC Craig L. Maddox, MC USA‡
ABSTRACT A 3-year-old male presented with progressive pruritic red–orange plaques across most of his body with
erythema, desquamation, and fissuring of the hands and feet. He was diagnosed with classic juvenile (type III) pityriasis
rubra pilaris (PRP) and treated with oral isotretinoin for 6 months. His skin findings resolved quickly during the treatment
period, with residual postinflammatory hypopigmentation resolving within a year. PRP is rare in pediatric patients and
standard recommended treatment algorithms for this population are not currently available. Diagnostic and treatment
guidelines for PRP are based almost exclusively on case reports or case series, most of which focus on adult patients.
The presentation, evaluation, and management of PRP are discussed.
INTRODUCTION face. He was also given hydroxyzine and various emollients
for control of symptoms.
CASE The duration of isotretinoin therapy was 6 months. The
A 3-year-old male was brought to a military treatment facility papules and plaques resolved within a few weeks. The patient
by his mother to see his primary care pediatrician. The began to develop easy sloughing of the skin with minor
patient’s mother was concerned about a new rash he was trauma, but overall his symptoms were well controlled. He
forming. He presented with a 4-day history of erythematous suffered no adverse reactions to isotretinoin other than xerosis
lichenified plaques on the palms and soles in addition to cutis. Complete blood count (CBC), liver function tests, and
intensely pruritic well-demarcated red–orange plaques with lipid profile were within normal limits at onset of treatment
islands of sparing and overlying scale spread across his as well as during reassessment 3 months later. At the end of
elbows and knees (Figs. 1 and 2). He was also noted to have the treatment period, all signs and symptoms had resolved
mild desquamation of the upper lip, nose, and ears along with and the only remnants of his condition were areas of post-
pinpoint erythematous papules across his trunk. His past med- inflammatory hypopigmentation that slowly resolved over
ical history was notable only for mild xerosis cutis, while the next year (Figs. 5 and 6). The patient has had no recur-
family history and review of systems were noncontributory. rence of PRP after 3 years of follow-up.
An active duty dermatologist at the same military treatment
facility was consulted, who arrived to primary care to assist DISCUSSION
with management. A punch biopsy was performed of the PRP is a clinically heterogeneous skin disease that is rela-
right elbow and the patient was prescribed desonide and tively uncommon. Diagnostic and treatment guidelines for
ammonium lactate as well as hydroxyzine for pruritus. PRP are based almost exclusively off of case reports or case
Despite initial therapy, over the following several days the series, most of which focus on adult patients. Our patient
plaques spread throughout his face, scalp, torso, and limbs. was diagnosed with classic juvenile PRP (type III). The dis-
His hands and feet developed a yellow–red waxy appearance ease in our patient followed a fairly typical course with reso-
with desquamation, fissuring, and mild edema (Figs. 3 and 4). lution following isotretinoin therapy.
The pathology report from the punch biopsy revealed mild PRP is divided into six types, with type I (classic adult)
acanthosis and parakeratosis. Direct immunofluorescence being the most well-described. It first became recognized as
staining for immunoglobulin M, immunoglobulin G, immu- a distinct illness in the mid-1800s. Before that, diseases with
noglobulin A, complement C3, and Fibrin was performed with characteristics similar to PRP had been described as variants
negative results, suggesting against erythema multiforme, or of psoriasis.
other autoimmune disorders. He was diagnosed with pityriasis The incidence and prevalence of PRP are not precisely
rubra pilaris (PRP) and started on oral isotretinoin 15 mg daily known, though the disease has been estimated to be present
(approximately 1 mg/kg). He continued to be treated with in approximately 1/5,000 patients presenting with a skin dis-
twice daily topical steroids including triamcinolone 0.1% order.1 It has a bimodal age distribution, being most common
ointment for the trunk and extremities, clobetasol 0.05% in the first and fifth decades of life. Men and women appear
foam for the scalp, and desonide 0.05% ointment for the to be equally affected by PRP and it occurs in all races. It
may occur in the setting of viral illnesses, superficial injury
or burn, malignancy, or seronegative arthritis.2,3 A severe
*1-503 IN(ABN), 173D IBCT(A), CMR 427 Box 2962, APO AE 09630. form of PRP may arise in patients with human immunodefi-
†U.S. Army Health Center-Vicenza, CMR 427, APO AE 09630.
‡Department of Clinical Specialties and Dermatology Services, U.S. Army
ciency virus (HIV).2
Health Center-Vicenza, CMR 427, APO AE 09630. PRP shows significant clinical diversity, with six subtypes
doi: 10.7205/MILMED-D-15-00316 defined by age of onset, distribution and appearance of
e298 MILITARY MEDICINE, Vol. 181, March 2016
Downloaded from https://academic.oup.com/milmed/article-abstract/181/3/e298/4159239
by guest
on 20 June 2018
Case Report
FIGURE 1. The patient at presentation.
FIGURE 3. The patient 10 days after presentation.
(islands of sparing). Common associated findings include fol-
licular keratoses, erythroderma, and palmoplantar keratoderma,
which may result in painful fissures on the hands or feet.2,3
Patients infrequently complain of pruritus. Maximum spread
is typically within 2 to 3 months. Mucosal involvement is
rare.4 Other forms of PRP are outlined in Table I.2,3
Diagnosis of PRP is based on clinical recognition con-
firmed by typical histopathological findings. A detailed history
should be obtained to help rule out other causes of the patient’s
symptoms. The differential diagnosis includes psoriasis, kera-
tosis pilaris, atopic dermatitis, ichthyoses, lichen spinulosus,
and other conditions, which can cause erythroderma such as
drug eruptions.2,5
The evaluation of suspected PRP should begin with skin
FIGURE 2. The patient at presentation. biopsy. Findings on biopsy may include follicular plugging,
increased granular cell layer, acantholysis, orthokeratosis,
and parakeratosis.4,6 Basic laboratory tests may be obtained to
lesions, and presence of HIV. The classic presentation of PRP evaluate possible coexisting conditions such as malignancy as
(types I and III) is diffuse red–orange scaling papules and well as to establish a baseline for monitoring during therapy.
plaques that spread in a cephalocaudal progression. The lesions Such laboratory tests include CBC with differential and com-
coalesce extensively with focal areas of normal-appearing skin plete metabolic profile, with fasting lipids added if isotretinoin
MILITARY MEDICINE, Vol. 181, March 2016 e299
Downloaded from https://academic.oup.com/milmed/article-abstract/181/3/e298/4159239
by guest
on 20 June 2018
Case Report
TABLE I. Classification of PRP
Type % of cases Clinical Characteristics Prognosis
Type I: Classic Adult 50 Diffuse red–orange scaling plaques with Typically resolves within 3 years
cephalocaudal spread and islands of sparing,
palmoplantar keratoderma, follicular
keratoses, erythroderma
Type II: Atypical Adult 5 Ichthyosiform lesions, palmoplantar Chronic
hyperkeratosis, alopecia
Type III: Classic Juvenile 10 Similar to classic adult, usual onset within first Typically resolves within 1–2 years
2 years of life
Type IV: Circumscribed Juvenile 25 Focal hyperkeratotic follicular papules on knees May resolve within a year or
and elbows, palmoplantar hyperkeratosis become chronic
Type V: Atypical Juvenile 5 Ichthyosiform dermatitis, follicular and Chronic
palmoplantar hyperkeratosis
Type VI: HIVAssociated Increasing Similar to type I, also with nodulocystic acne Chronic, poor prognosis
and lichen spinulosus
therapy will be used.7 Considering the association between primarily from case reports and case series, few of which deal
type-VI PRP and HIV, it is prudent to obtain an HIV test, directly with treatment of children. Systemic retinoids are
especially if the patient reports risk factors for HIV, the considered first-line therapy for PRP and treatment for adults
patient also presents with new-onset nodulocystic acne, or if may begin with 1 mg/kg daily isotretinoin or 0.5 mg/kg
the disease is refractory to standard therapy. There are no spe- daily acitretin.3,7,8 Treatment of children is less commonly
cific laboratory abnormalities or serologic markers for PRP. described with no single agent showing consistent benefit,
There are no treatments that are universally effective for though treatment with isotretinoin at 1 mg/kg was highly
PRP and evidence for the use of accepted therapies stems effective in our patient. It should be noted that acitretin is
teratogenic for up to 3 years after discontinuation of therapy,
and is therefore not recommended for women of childbear-
ing age. Effects of treatment are usually realized within 90 to
180 days.2
Methotrexate is considered a second-line agent, and has
been reported to be effective when used in combination with
oral retinoids for difficult cases.3,7 Other therapies which have
been employed with varying success include tumor necrosis
factor-alpha inhibitors, cyclosporine, and azathioprine. HIV-
associated PRP is generally refractory to standard therapy.
In these patients, initiation of antiretroviral therapy may
resolve symptoms.9
FIGURE 4. The patient 10 days after presentation. FIGURE 5. The patient after completion of isotretinoin therapy.
e300 MILITARY MEDICINE, Vol. 181, March 2016
Downloaded from https://academic.oup.com/milmed/article-abstract/181/3/e298/4159239
by guest
on 20 June 2018
Case Report
HIGHLIGHTS
— PRP is a rare skin disorder typically characterized by
diffuse orange–red scaling plaques with palmoplantar
keratoderma and follicular keratosis.
— Diagnosis is based off of clinical recognition and con-
firmed by biopsy. Obtaining a CBC, comprehensive
metabolic panel, and HIV test is also recommended.
— Systemic retinoids are the mainstay of therapy. Symp-
tomatic relief including emollients and possibly topical
steroids should also be provided.
REFERENCES
1. Griffiths WA: Pityriasis rubra pilaris. Clin Exp Dermatol 1980; 5(1):
105–12.
2. Habif TP: Pityriasis rubra pilaris. In: Clinical Dermatology: A Color
Guide to Diagnosis and Therapy, Ed 5, pp 309–11. Edinburgh, Scotland,
Mosby, 2010.
3. Klein A, Landthaler M, Karrer S: Pityriasis rubra pilaris: a review of
diagnosis and treatment. Am J Clin Dermatol 2010; 11(3): 157–70.
4. Martinez Calixto LE, Suresh L, Matsumura E, Aguirre A, Radfar L:
Oral pityriasis rubra pilaris. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod 2006; 101(5): 604–7.
5. Gajinov ZT, Matić MB, Duran VD, Vucković N, Prcić ST, Vujanović
LM: Drug-related pityriasis rubra pilaris with acantholysis. Vojnosanit
Pregl 2013; 70(9): 871–3.
6. Magro CM, Crowson AN: The clinical and histomorphological features
of pityriasis rubra pilaris. A comparative analysis with psoriasis. J Cutan
Pathol 1997; 24(7): 416–24.
7. Lebwohl MG, Heymann WR, Berth-Jones J, Coulson I: Pityriasis rubra
FIGURE 6. The patient after completion of isotretinoin therapy.
pilaris. In: Treatment of Skin Disease: Comprehensive Therapeutic
Strategies, pp 573–5. Edited by MG Lebwohl, J Berth-Jones, WR
Heymann, I Coulson. Edinburgh, Scotland, Saunders, 2010.
Symptomatic relief should be offered with topical emol- 8. Dicken CH: Isotretinoin treatment of pityriasis rubra pilaris. J Am Acad
lients.7 If pruritus is present, the patient may be offered oral Dermatol 1987; 16(2 Pt 1): 297–301.
antihistamines. Medium to high-potency topical steroids may 9. González-López A, Velasco E, Pozo T, Del Villar A: HIV-associated
pityriasis rubra pilaris responsive to triple antiretroviral therapy. Br J
be used, though they are unlikely to alter the overall course Dermatol 1999; 140(5): 931–4.
of disease unless the patient has limited skin involvement 10. Allison DS, El-Azhary RA, Calobrisi SD, Dicken CH: Pityriasis rubra
(such as in type IV).10 pilaris in children. J Am Acad Dermatol 2002; 47(3): 386–9.
MILITARY MEDICINE, Vol. 181, March 2016 e301
Downloaded from https://academic.oup.com/milmed/article-abstract/181/3/e298/4159239
by guest
on 20 June 2018
You might also like
- Mehu131 - U1 - T7 - Serbian Journal of Dermatology and Venereology) Pityriasis Rubra Pilaris - A Report of Two Cases and Literature ReviewDocument14 pagesMehu131 - U1 - T7 - Serbian Journal of Dermatology and Venereology) Pityriasis Rubra Pilaris - A Report of Two Cases and Literature ReviewJohanny ortizNo ratings yet
- Childhood PsioriasisDocument6 pagesChildhood PsioriasisYuliana DaisongNo ratings yet
- PITYRIASIS ROSEA eisman2015-DIPLOMADO DERMATOLOGIA CLINICA 2023Document6 pagesPITYRIASIS ROSEA eisman2015-DIPLOMADO DERMATOLOGIA CLINICA 2023taniasolisNo ratings yet
- Clinical Cases in PsoriasisFrom EverandClinical Cases in PsoriasisJashin J. WuNo ratings yet
- Biomedicines: Relapsing Polychondritis: An Updated ReviewDocument14 pagesBiomedicines: Relapsing Polychondritis: An Updated ReviewThane ManoonNo ratings yet
- Dermatomyositis and Undifferentiated Nasopharyngeal Carcinoma. A Rare Presentation of A Rare MalignancyDocument4 pagesDermatomyositis and Undifferentiated Nasopharyngeal Carcinoma. A Rare Presentation of A Rare MalignancyasclepiuspdfsNo ratings yet
- 3712-Article Text-32012-1-10-20230110Document4 pages3712-Article Text-32012-1-10-20230110sesiaNo ratings yet
- 17.pityriasis RoseaDocument5 pages17.pityriasis RoseahaidarTRVNo ratings yet
- Phenytoininduced DRESSDocument4 pagesPhenytoininduced DRESSCamille MalilayNo ratings yet
- Pomfoliks JurnalDocument4 pagesPomfoliks JurnalTri RatnawatiNo ratings yet
- 18.palmar NwabudikeLCDocument4 pages18.palmar NwabudikeLCblacklist16No ratings yet
- Pityriasis Rubra Pilaris Case Series Explores Psychological ImpactDocument6 pagesPityriasis Rubra Pilaris Case Series Explores Psychological ImpactUmmi RinandariNo ratings yet
- Penatalaksanaan Fisioterapi Pada LymphedemaDocument19 pagesPenatalaksanaan Fisioterapi Pada Lymphedemamaevy dwiNo ratings yet
- Scurvy Masquerading as Rheumatic ConditionsDocument6 pagesScurvy Masquerading as Rheumatic ConditionsZach Segmuel MiñanoNo ratings yet
- Rajat Sanker Roy Biswas, Md. Habib Khan: AbstractDocument3 pagesRajat Sanker Roy Biswas, Md. Habib Khan: Abstractstudentstoma61No ratings yet
- Psoriasis Guide for Primary CareDocument22 pagesPsoriasis Guide for Primary CareRama_Aditya_KNo ratings yet
- Brezinski - Cutaneous Plasmacytosis With Perineural InvolvementDocument5 pagesBrezinski - Cutaneous Plasmacytosis With Perineural InvolvementEva YustianaNo ratings yet
- Pytriasis RosseaDocument4 pagesPytriasis Rosseayubi arsanaNo ratings yet
- Skin and Soft Tissue InfectionsDocument15 pagesSkin and Soft Tissue InfectionsAmirah Warsid JauriNo ratings yet
- Pityriasis Rubra Pilaris A Report of Two Cases andDocument14 pagesPityriasis Rubra Pilaris A Report of Two Cases andFernando Oeghoede YewunNo ratings yet
- Case Report of DermatomyositisDocument3 pagesCase Report of DermatomyositisMarvin de ManuelNo ratings yet
- 1793-Article Text-19545-2-10-20190508 PDFDocument5 pages1793-Article Text-19545-2-10-20190508 PDFRezkyRamadhaniSyarifNo ratings yet
- Recurrent Pityriasis Rosea A Case ReportDocument4 pagesRecurrent Pityriasis Rosea A Case ReportdanialghafariNo ratings yet
- Prevalence of Tinea Corporis and Tinea Cruris in Outpatient Department of Dermatology Unit of A Tertiary Care HospitalDocument3 pagesPrevalence of Tinea Corporis and Tinea Cruris in Outpatient Department of Dermatology Unit of A Tertiary Care HospitalRetno WahyudiNo ratings yet
- CMJ 130 2011Document2 pagesCMJ 130 2011studentstoma61No ratings yet
- Dermatophyte Case ReportDocument8 pagesDermatophyte Case ReportnikfarisNo ratings yet
- Therapy Selection For Tinea Corporis and Cruris With CommorbidityDocument9 pagesTherapy Selection For Tinea Corporis and Cruris With CommorbidityShimie Shimie KokobopNo ratings yet
- Psoriasis A Biological and Behavioral Management ApproachDocument5 pagesPsoriasis A Biological and Behavioral Management ApproachAthenaeum Scientific PublishersNo ratings yet
- Bur FieldDocument6 pagesBur FieldNexi anessaNo ratings yet
- Cde 0006 0119Document5 pagesCde 0006 0119Mati AjaNo ratings yet
- Recurrent Pericarditis in Children and AdolescentsDocument12 pagesRecurrent Pericarditis in Children and AdolescentsRafael TerceiroNo ratings yet
- Immune Thrombocytopenic Purpura (ITP) :: A New Look at An Old DisorderDocument6 pagesImmune Thrombocytopenic Purpura (ITP) :: A New Look at An Old DisorderAsri Alifa SholehahNo ratings yet
- A Case of Multiple Myeloma Misdiagnosed As Seronegative ARDocument6 pagesA Case of Multiple Myeloma Misdiagnosed As Seronegative ARRaíla SoaresNo ratings yet
- Pathogenesis Psoriasis Update 2017Document2 pagesPathogenesis Psoriasis Update 2017eby_3tamaNo ratings yet
- Arpa - 2018 0219 RaDocument6 pagesArpa - 2018 0219 Rahuseikha velayazulfahdNo ratings yet
- Maladie de Mondor 2019Document3 pagesMaladie de Mondor 2019Naouel BenatNo ratings yet
- Psoriasis Therapy by Chinese Medicine and Modern AgentsDocument10 pagesPsoriasis Therapy by Chinese Medicine and Modern AgentsRute MacedoNo ratings yet
- Case Reports in Clinical Practice: A 53-Year-Old Woman With Persistent Erythroderma and DyspneaDocument3 pagesCase Reports in Clinical Practice: A 53-Year-Old Woman With Persistent Erythroderma and Dyspneashinta saingNo ratings yet
- Unusual Cause of Fever in A 35-Year-Old Man: ECP YuenDocument4 pagesUnusual Cause of Fever in A 35-Year-Old Man: ECP YuenhlNo ratings yet
- Eritem PolimorfDocument3 pagesEritem PolimorfMădălina ŞerbanNo ratings yet
- Juvenile localized scleroderma case reportDocument3 pagesJuvenile localized scleroderma case reportMarisol Susan Poma CastilloNo ratings yet
- Clinical Cases in PruritusFrom EverandClinical Cases in PruritusShannon C. TrotterNo ratings yet
- Artigo Carcinoma NUTDocument6 pagesArtigo Carcinoma NUTlorranatayna202201No ratings yet
- American Trypanosomiasis: Causative Agent: TrypanosomaDocument32 pagesAmerican Trypanosomiasis: Causative Agent: TrypanosomaMasali MacdonaNo ratings yet
- Defenisi PDFDocument2 pagesDefenisi PDFNyoman SuryaNo ratings yet
- Medicina 57 01004Document12 pagesMedicina 57 01004Ilham MahardikaNo ratings yet
- Biological Basis of Keloid Formation and TreatmentTITLEDocument11 pagesBiological Basis of Keloid Formation and TreatmentTITLEAndriantkNo ratings yet
- Seminar: Epidemiology and Disease BurdenDocument15 pagesSeminar: Epidemiology and Disease BurdenLuis Miguel Murcia CastilloNo ratings yet
- Jamadermatology Wang 2019 Lo 1900191 PDFDocument3 pagesJamadermatology Wang 2019 Lo 1900191 PDFvijaya abburamNo ratings yet
- A Double-Blind Randomized Controlled Trial Comparing The Efficacy of 0.0003% Calcitriol With 1% Pimecrolimus Versus Placebo in The Management of Pityriasis AlbaDocument6 pagesA Double-Blind Randomized Controlled Trial Comparing The Efficacy of 0.0003% Calcitriol With 1% Pimecrolimus Versus Placebo in The Management of Pityriasis AlbayosaNo ratings yet
- Inflammatory Dermatopathology: A Pathologist's Survival GuideFrom EverandInflammatory Dermatopathology: A Pathologist's Survival GuideNo ratings yet
- Chronic Recurrent Multifocal Osteomyelitis in Association With Pyoderma GangraenosumDocument7 pagesChronic Recurrent Multifocal Osteomyelitis in Association With Pyoderma GangraenosumDha Dina SevofrationNo ratings yet
- Patogenie LILI CompletDocument8 pagesPatogenie LILI CompletDianaNo ratings yet
- 9930 PDFDocument9 pages9930 PDFAnonymous 2BC7omLaWCNo ratings yet
- H-Ferritin and CD68Document9 pagesH-Ferritin and CD68Aleksandar KitanovskiNo ratings yet
- Benedictmitnick2019 PDFDocument9 pagesBenedictmitnick2019 PDFArthur TeixeiraNo ratings yet
- 329-Article Text-1006-2-10-20200429Document5 pages329-Article Text-1006-2-10-20200429Drina PaglinawanNo ratings yet
- Recent insights into immunopathogenesis of psoriasis open doors for targeted therapiesDocument13 pagesRecent insights into immunopathogenesis of psoriasis open doors for targeted therapiesraudhatul muttaqinNo ratings yet
- Beauty Therapy Final FullDocument298 pagesBeauty Therapy Final FullMONTOYA BASTIDAS IVAN DARIO100% (1)
- Name: Josiah Guenn P. Villaraza Group: B Clinical Instructor: Ma'am Irene Cheeries Apal-Enriquez, RN Date: November 7, 2021Document3 pagesName: Josiah Guenn P. Villaraza Group: B Clinical Instructor: Ma'am Irene Cheeries Apal-Enriquez, RN Date: November 7, 2021Princess EduaveNo ratings yet
- Tinjauan Pustaka: Respon Imunologi Pada Dermatitis Kontak IritanDocument7 pagesTinjauan Pustaka: Respon Imunologi Pada Dermatitis Kontak IritanSatriadwykiyprasetya ThiodwkiyNo ratings yet
- LT467 - Biomimetic LRF Complex - Rev.02-IDocument7 pagesLT467 - Biomimetic LRF Complex - Rev.02-Idaniel7327748No ratings yet
- FACIAL BAR SOAP NewDocument7 pagesFACIAL BAR SOAP NewZainab AjaniNo ratings yet
- Mycv Lec MycosesDocument2 pagesMycv Lec MycosesChris Angelo De GuzmanNo ratings yet
- Formulation and Development of Transdermal Patch of Tizanidine HydrochlorideDocument7 pagesFormulation and Development of Transdermal Patch of Tizanidine HydrochloridediskaNo ratings yet
- Elc590 PitchingDocument2 pagesElc590 PitchingNURUL ANIS SURAYA MOHD SUKRINo ratings yet
- Aging Changes of The Midfacial Fat Compartments A.45Document11 pagesAging Changes of The Midfacial Fat Compartments A.45Juliana BrunettoNo ratings yet
- Perineal and Genital Care ChecklistDocument2 pagesPerineal and Genital Care ChecklistLoren MisticaNo ratings yet
- Evaluation of The Topical Antiperspirant Effects oDocument4 pagesEvaluation of The Topical Antiperspirant Effects oLeane Enero DarayNo ratings yet
- Herbal CosmeticsDocument13 pagesHerbal CosmeticsKhushbuChemical RautNo ratings yet
- PagesDocument68 pagesPagesAhmet SaygılıNo ratings yet
- Female GuideDocument5 pagesFemale GuideproductiveraunakNo ratings yet
- Zinc-Glycine Complex PresentationDocument34 pagesZinc-Glycine Complex PresentationJames WuNo ratings yet
- Rationale HwSterileGDocument3 pagesRationale HwSterileGStefany JoyNo ratings yet
- PC Product Catalogue - AP (2014) PDFDocument33 pagesPC Product Catalogue - AP (2014) PDFeggy mushadiNo ratings yet
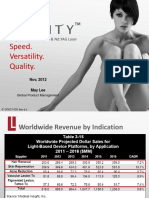
- Speed. Versatility. Quality.: Long Pulsed Alexandrite & Nd:YAG LaserDocument51 pagesSpeed. Versatility. Quality.: Long Pulsed Alexandrite & Nd:YAG LaserasdNo ratings yet
- Oecd 402Document7 pagesOecd 402Sandro SotomayorNo ratings yet
- 3-In-1 40K Ultrasonic Cavitaton Machine User ManualDocument26 pages3-In-1 40K Ultrasonic Cavitaton Machine User ManualJosé Emmanuel Chacón ChavarríaNo ratings yet
- Cenovnik - HemelDocument4 pagesCenovnik - HemelclassicreviewNo ratings yet
- Unit 3, Novel Drug Delivery Systems, B Pharmacy 7th Sem, Carewell PharmaDocument33 pagesUnit 3, Novel Drug Delivery Systems, B Pharmacy 7th Sem, Carewell Pharmaayush pathak100% (1)
- Treating The Lips and Its Anatomical Correlate in Respect To Vascular CompromiseDocument11 pagesTreating The Lips and Its Anatomical Correlate in Respect To Vascular CompromiseDoctores Duarte BarrosNo ratings yet
- Cosmetic Treatment J.clindermatol.2013.06.008Document5 pagesCosmetic Treatment J.clindermatol.2013.06.008Vita BūdvytėNo ratings yet
- Internal Medicine Standard FrameworkDocument16 pagesInternal Medicine Standard FrameworkMohammed S. Al GhamdiNo ratings yet
- Health Condition1Document22 pagesHealth Condition1Barrack koderaNo ratings yet
- Bedroom BathroomDocument8 pagesBedroom BathroomLimar Geoff G. RosalesNo ratings yet
- To Research Spa BusinessDocument7 pagesTo Research Spa BusinessMaria CarmelaNo ratings yet
- Analyzing Hand ConditionsDocument7 pagesAnalyzing Hand ConditionsLoraineTenorioNo ratings yet
- TLE (1) - CosmetologyDocument7 pagesTLE (1) - CosmetologyJoel Malsi Junior100% (2)