Professional Documents
Culture Documents
Cardiovascular Effects of COX-2 Inhibitors
Uploaded by
Fernandiita de LopezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular Effects of COX-2 Inhibitors
Uploaded by
Fernandiita de LopezCopyright:
Available Formats
The Cardiovascular Pharmacology of
COX-2 Inhibition
Susanne Fries and Tilo Grosser
Selective inhibitors of cyclooxygenase (COX)-2, the oppose mediators, which stimulate platelets, elevate
coxibs, were developed to inhibit inflammatory blood pressure, and accelerate atherogenesis,
prostaglandins derived from COX-2, while sparing including TxA2. Indeed, structurally distinct inhibitors
gastroprotective prostaglandins primarily formed by of COX-2 have increased the likelihood of hyperten-
COX-1. However, COX-2-derived prostaglandins sion, myocardial infarction and stroke in controlled
mediate not only pain and inflammation but also affect clinical trials. The detection of these events in patients
vascular function, the regulation of hemostasis/ is related to the duration of exposure and to their
thrombosis, and blood pressure control. All coxibs baseline risk of cardiovascular disease. Thus, coxibs
depress COX-2-dependent prostacyclin (PGI2) biosyn- should be withheld from patients with preexisting
thesis without effective suppression of platelet COX-1- cardiovascular risk factors, and exposed patients at
derived thromboxane (Tx) A2, unlike aspirin or tradi- low cardiovascular baseline risk should be monitored
tional nonsteroidal anti-inflammatory drugs, which for changes in their risk factor profile, such as in-
inhibit both COX-1 and COX-2. The actions of PGI2 creases in arterial blood pressure.
Traditional nonsteroidal anti-inflammatory drugs (tNSAIDs) The discovery of the second, rapidly inducible COX
and selective inhibitors of COX-2, the coxibs, are a chemi- isoform in the early 1990s afforded an opportunity to sup-
cally heterogeneous group of compounds, characterized press PG formation in a more targeted fashion by designing
by varying degrees of anti-inflammatory, analgesic and inhibitors with higher affinity for COX-2 than for COX-1,
antipyretic activity. Their unifying therapeutic effect is the the coxibs. The underlying hypothesis—sometimes referred
inhibition of prostaglandin (PG) biosynthesis. PGs are lipid to as the ‘COX-2 hypothesis’—was that inflammatory pros-
mediators formed from arachidonic acid by the PG G/H taglandins are primarily derived from COX-2, while pros-
synthases 1 and 2, commonly termed cyclooxygenases taglandins formed by COX-1 have generally homeostatic
(COX). Recruitment of leukocytes and induction of COX-2 roles, including the protection of the gastrointestinal mu-
expression by inflammatory stimuli account for the high cosa. Thus, selective inhibitors of COX-2 were expected to
levels of PGs found in inflammatory lesions. PGE2, which be as efficacious as non-selective tNSAIDs and cause less
sensitizes nociceptors, prostacyclin (PGI2) and perhaps serious gastrointestinal side effects, which are attributed to
thromboxane (Tx) A2 mediate pain and inflammation.1 Both inhibition of COX-1. Although biological reality turned
PGI2 and PGE2 contribute to the vasodilation at sites of out to be more complex—COX-2 has also important physi-
injury. In addition to such peripheral mechanisms, COX-1 ological functions in the absence of inflammation2 and
and COX-2 products modulate nociception centrally. COX-1 plays also a role in nociception3—all coxibs were
tNSAIDs such as ibuprofen, naproxen or indomethacin in- indeed shown to cause less gastroduodenal ulcerations than
hibit both COX isoforms reversibly. Aspirin is distinct, as it comparator tNSAIDs, as visualized by endoscopy. 2
blocks the COXs irreversibly, which explains the cardio- Celecoxib (Celebrex, Pfizer) and rofecoxib (Vioxx, Merck)
protective effect of low-dose aspirin; it inactivates platelet were approved by the FDA in 1999, valdecoxib (Bextra,
COX-1 irreversibly and new platelets have to be formed to Pfizer) in 2001. Other compounds (etoricoxib/Arcoxia,
restore function. Merck; lumiracoxib/Prexige, Novartis; parecoxib/Dynastat,
Pfizer) are pending approval. Boosted by the attraction of
the ‘COX-2 hypothesis’—and by aggressive marketing cam-
paigns—the coxibs achieved sales of about $9 billion by
Correspondence: Tilo Grosser, MD, Institute for Translational the time of the withdrawal of rofecoxib in September 2004.
Medicine and Therapeutics, University of Pennsylvania School
Interestingly, the majority of patients prescribed with a coxib
of Medicine, 809 Biomedical Research Building, 421 Curie
Blvd., Philadelphia, PA 19104-6084; Phone (215) 573 7600, Fax were not at particularly high risk for serious tNSAID re-
(215) 573 9004, tilo@spirit.gcrc.upenn.edu lated gastrointestinal complications and the incidence of
uncomplicated gastric upset on a coxib turned out to be no
Acknowledgements: Supported by grants from the American different from that of tNSAIDs. Only three randomized, con-
Heart Association (S.F.: Pennsylvania-Delaware Affiliate trolled outcome trials have studied whether the coxibs ac-
Postdoctoral Fellowship; T.G.: Scientist Development Grant tually reduce the incidence of serious gastrointestinal com-
0430148N). plications in larger populations. The Vioxx Gastrointesti-
Hematology 2005 445
nal Outcomes Research (VIGOR) Study and the Therapeu- platelets, elevate blood pressure, and accelerate atherogen-
tic Arthritis Research and Gastrointestinal Event Trial esis, including TxA2.10-12 Thus, drug selectivity for inhibi-
(TARGET) have shown that rofecoxib and lumiracoxib, tion of COX-2 may increase the likelihood of hyperten-
cause less serious gastrointestinal adverse events than non- sion, myocardial infarction and stroke.1 Three structurally
isoform selective tNSAIDs.4,5 The trial studying the oldest distinct compounds, rofecoxib, valdecoxib, and celecoxib,
marketed COX-2 inhibitor, the Celecoxib Long-term Ar- have increased the incidence of these cardiovascular com-
thritis Safety Study (CLASS) study,6 failed to support the plications significantly in controlled trials,4,13-15 suggest-
hypothesis, as its gastrointestinal endpoint did not differ- ing that the entire class of COX-2 inhibitors confers a car-
entiate this coxib from the comparator tNSAIDs.6 Never- diovascular hazard. Rofecoxib and valdecoxib have been
theless, celecoxib became the best selling coxib and, in- withdrawn from the market. This paper reviews the phar-
deed, remains the only such drug on the market. macology of COX inhibition, discusses mechanisms by
While no randomized controlled outcome trial of a which coxibs may promote thrombosis, atherosclerosis and
coxib has sought to demonstrate superiority of pain relief hypertension, summarizes results of clinical trials that de-
over comparator tNSAIDs, some patients report a unique tected a cardiovascular risk and provides perspective on
quality of pain relief by COX-2 inhibitors, which they had how this may inform clinical decisions regarding coxib
not experienced on tNSAIDs. It has been long recognized, and tNSAID use.
but never systematically studied, that the clinical response
to a particular tNSAID—or its toxicity—may vary substan- Pharmacology of COX Inhibition
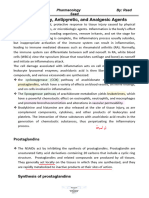
tially from patient to patient. Interestingly, the pharmaco- Arachidonic acid, released from cell membranes by the ac-
logical response within the group of selective COX-2 in- tivity of phospholipases, is the main COX substrate. Both,
hibitors is similarly variable,7 and detailed analyses of fac- COX-1 and COX-2 synthesize PGH2, a labile intermediate
tors that condition such diverse responses may lead to a that is further metabolized by downstream isomerases to
more individualized therapy with both, tNSAIDs and form the prostaglandins, PGE2, PGF2α, PGD2, PGI2 and TxA2
coxibs.7 (Figure 1), which activate specific transmembrane recep-
Concurrent with the clinical development of the tors coupled to G proteins. COX-1 is expressed constitu-
coxibs, it was recognized that—in contrast to the initial tively in most tissues. It is the only form of the enzyme in
hypothesis—COX-2-derived prostaglandins mediate not mature platelets and is expressed in vascular endothelium,
only pain and inflammation, but also affect vascular func- gastrointestinal epithelium, spinal cord, brain and kidney,
tion, thrombosis and blood pressure.8,9 Thus, COX-2 in- amongst other tissues. COX-2 is highly inducible by
hibitors depress the vascular biosynthesis of PGI2, leaving cytokines, tumor promoters and mitogens. In addition to
platelet COX-1-derived TxA2 unaffected—in contrast to its role in prostaglandin formation in inflammation it has
tNSAIDs or aspirin, which inhibit both COX-1 and COX- been implicated in carcinogenesis. The strict distinction
2.8,9 The actions of PGI2 oppose all mediators that stimulate between ‘inducible’ and ‘constitutive’ forms of the enzyme,
however, is an oversimplification;2 COX-2 is
constitutively expressed in several tissues,
such as spinal cord, brain, kidney and COX-1
can be upregulated to a certain degree in in-
flammation. COX-2 is also induced in vascu-
lar endothelium under physiological condi-
tions of flow16 and both isoforms both are de-
velopmentally regulated.17
While COX-1 and COX-2 are structurally
similar, the substrate-binding channel of COX-
2 contains a side pocket, which is absent in
COX-1. This allowed for the design of inhibi-
tors with side chains that fit within the COX-2
channel, but are too large to block COX-1 with
equally high affinity. Thus, the ratio of the
affinities to COX-1 and COX-2 determines
how ‘selective’ a compound is and represents
a continuous, rather than a discrete, variable.
The second generation coxibs, etoricoxib and
Figure 1. The cyclooxygenase (COX)-1 and -2 pathway. Prostaglandins lumiracoxib, were developed to be more se-
(PG) are formed by specific isomerases from the COX product PGH2. They act
through G protein transmembrane receptors. lective for COX-2 than rofecoxib and
Abbreviations: IP, prostacyclin receptor; TP, thromboxane receptor; DP, PGD2 valdecoxib, which are roughly similar in their
receptor, EP, PGE2 receptor, FP, PGF2α receptor. degree of selectivity but more selective than
446 American Society of Hematology
celecoxib (Figure 2).2 In human studies, the degree of COX- observations that both rofecoxib and celecoxib reduced
2 selectivity is commonly determined by whole blood as- PGI2 formation in healthy individuals by about 70% with-
says that measure the ratio of COX-1 and COX-2 inhibition out concurrent inhibition of platelet function.8,9 Biosyn-
ex vivo.18 As ‘selectivity’ is conditioned by differences in thesis of prostacyclin, a potent inhibitor of platelet aggre-
the affinity to the COX isoforms, the concentration of the gation, is increased in syndromes of platelet activation,
compound has an effect on ‘selectivity.’ Thus, high drug such as severe atherosclerosis and unstable angina prob-
concentrations will also inhibit COX-1 to a certain degree ably as a homeostatic response to accelerated platelet-vas-
and very high, supratherapeutic concentrations may not be cular interactions.10 Thus, deletion of the PGI2 receptor (IP)
COX-2 selective at all. Thus ‘selectivity’ achieved in hu- in mice augmented the cardiovascular effects of TxA2 in
mans is not a purely structural property of a compounds vivo.10 The mice responded with an exaggerated formation
but may also be influenced by pharmacokinetic (e.g., of TxA2 to vascular injury followed by more pronounced
plasma concentration) and pharmacodynamic factors (e.g., neointimal proliferation (Figure 3). Both responses were
genetic variations of the target enzymes).7 tNSAIDs can reverted by simultaneous deletion of the TxA2 receptor
also be ranked on the selectivity scale using the same crite- (TP).10 Thus, depression of COX-2 dependent PGI2 biosyn-
ria. Naproxen or ibuprofen are slightly more potent inhibi- thesis, without concomitant inhibition of platelet function
tors of COX-1 than of COX-2, while the degrees of selectiv- provides a mechanism for a prothrombotic effect of COX-2
ity of diclofenac, nimesulide and meloxicam are—perhaps inhibitors. However, the impact of PGI2 depression on throm-
surprisingly—comparable to that of celecoxib.2 One would botic events would be expected to pertain only when the
expect that these characteristics relate to the safety profile baseline risk of thrombosis is augmented, as mice deficient
of both tNSAIDs and coxibs. For example, the similarity of in the prostacyclin receptor do not develop thrombosis
diclofenac and celecoxib may be one reason why the CLASS spontaneously.
trial failed to detected difference in the gastrointestinal Depression of COX-2-derived PGI2 formation may also
endpoint between the groups.6 Very little information ex- impact atherosclerotic plaque development, as deletion of
ists about the cardiovascular safety of tNSAIDs 19 and pro- the IP accelerates the initiation and early development of
spective, placebo-controlled outcome studies have not atherosclerosis in mice (Figure 3).12,25 In this context, PGI2
been performed. acts to limit the interactions of platelets and leukocytes
with the vasculature and the attendant oxidant stress.12,25
Impact of COX Inhibition on Thrombogenesis, Deletion of the IP increases the biosynthesis of TxA2 in
Atherogenesis and Blood Pressure Regulation
Products of the COX pathway have established relevance
in clinical syndromes of vascular occlusion. Thus, aspirin
reduces the secondary incidence of myocardial infarction,
stroke and important vascular events by roughly 25%.20
Suppression of the major product of platelet COX-1, TxA2,
which is a potent platelet activator, vasoconstrictor, and
mitogen,21 is the basis of cardioprotection by aspirin. TXA2
biosynthesis is increased in conditions of acute or chronic
platelet activation, such as coronary thrombosis and dia-
betes, and augmented TxA2 biosynthesis has been linked
to the risk of future events.22 Low-dose aspirin suppresses
platelet TxA2 formation by acetylation of a serine residue
within the substrate binding channel of COX-1 obstructing
access of arachidonic acid to the active site. This modifica-
tion results in the irreversible inhibition of platelet func- Figure 2. The degrees of cyclooxygenase (COX)-selectivity
tion, due to the limited capacity of the anucleate platelets of various traditional non-steroidal anti-infammatory
to form new proteins. tNSAIDs other than aspirin attain drugs (tNSAIDs) and coxibs (open circles). The
concentrations required to inhibit COX-1 and COX-2 by 50%
maximal inhibition of platelet COX-1 only transiently dur- (IC50) have been measured using whole blood assays of COX-1
ing the dosing interval, due to their reversible interaction and COX-2 activity in vitro.18 The line indicates equivalent COX-1
with the enzyme. Thus, tNSAIDs are not cardioprotective. and COX-2 inhibition. Drugs plotted below the line are more
COX-2 is not expressed in mature platelets, although small potent inhibitors of COX-2 than drugs plotted above the line. The
distance to the line is a measure of selectivity. Lumiracoxib is
quantities of COX-2 protein are detectable in immature the compound with the highest degree of selectivity for COX-2
platelet forms.23,24 Thus, the coxibs depress platelet TxA2 as its distance to the line is the largest. Celecoxib and diclofenac
formation only marginally at high concentrations and have have similar degrees of COX-2 selectivity, as their distances to
no effect on platelet function.8,9 the line are similar; however, diclofenac is active at lower
concentrations and, thus, located more to the left. (Updated
The possibility that selective inhibitors of COX-2 may from FitzGerald GA, Patrono C. The coxibs, selective inhibitors
increase cardiovascular risk was raised in 1999 based on of cyclooxygenase-2. N Engl J Med. 2001;345:433-442.)
Hematology 2005 447
that an increasing degree of selectivity for
COX-2 may proportionately accelerate pro-
gression of atherogenesis.
The elevation of blood pressure by the
COX-inhibitors is a more indirect mechanism
by which they may accelerate atherogenesis
and increase cardiovascular risk. It is well rec-
ognized that tNSAIDs and coxibs can induce
sodium retention, edema and hypertension.29,30
Figure 3. The impact of deletion of the prostacyclin receptor on the However, it remains unclear whether the coxibs
thrombotic (left panel) and proliferative (right panel) response to differ from tNSAIDs in their effects on blood
catheter-induced carotid vascular injury in mice. The endothelium of the pressure regulation. Very little data exist on
common carotid artery was denuded in this model using a fine wire. This
activates platelets, as reflected by an enhanced biosynthesis of thromboxane the relative roles of COX isoforms in the hu-
(Tx) A2 (left panel), and causes neointimal formation, which can be quantified man kidney. Some information, however, can
on histological crossections two weeks after the procedure (right panel). The be derived from experiments in mice. Interest-
procedure-related platelet activation and thromboxane biosynthesis, as ingly, these show—just like in the case of
reflected by urinary excretion of its metabolite 2,3 dinor TxB2, was augmented
in mice deficient for the prostacyclin receptor (IP). Deletion of the atherogenesis—that COX-1 and COX-2 may
thromboxane receptor (TP) reduced the procedure-related increment in have opposing functions in the kidney.11 In
thromboxane biosynthesis. Simultaneous deletion of both receptors (IPTP) mice, COX-1 products, likely TxA2 and per-
compensated for the effects of the individual receptors. haps PGF2α, contribute to blood pressure ho-
Redrawn with permission from Cheng Y, Austin SC, Rocca B, et al. Role of
prostacyclin in the cardiovascular response to thromboxane A2. Science. meostasis by the renin angiontensin system
2002; 296(5567):539-541. and increase blood pressure.31 Conversely, the
vasodilator COX-2 products, PGI2 and PGE2,
increase renal medullary blood flow, which
hypercholesterolemic mice, as an index of increased plate- drives pressure natriuresis and diuresis.29 COX-2 inhibition,
let activation in vivo.25 Platelet activation contributes to just like nonselective COX-inhibition, reduces acutely
atherogenesis and suppression of TxA2 activity retards medullary blood flow, sodium excretion and urine vol-
atherogenesis (Figure 4).12,26,27 These observations suggest ume.11 However, this results only in a hypertensive response
that COX-1-derived TxA2 and COX-2-derived PGI2 may have when the autoregulatory mechanisms are already otherwise
opposing activities in atherogenesis,12,28 although this has stressed.11,32 In humans, hypertensive responses to COX in-
not yet been addressed directly in humans. This implies hibition tend to occur when predisposing conditions exist,
such as excessive salt intake, preexisting hypertension,
heart disease and diabetes, or depletion of the effective
circulating volume. This is consistent with clinical obser-
vations in young and healthy individuals, in which both
nonselective COX inhibition and selective COX-2 inhibi-
tion have no effects on arterial pressure despite transient
changes in sodium handling and glomerular filtration rate
on initiation of dosing.33 The latter may be caused by the
inhibition of dilator prostanoids that contribute to the pa-
tency of afferent arterioles and by a reduction of COX-2
dependent, cortical PGE2 formation, a component of the
tubuloglomerular feedback mechanism.31,34 Thus, given the
role of COX-1 in elevating blood pressure, one would ex-
pect that the degree of selectivity of COX-2 inhibition could
affect blood pressure control in susceptible individuals.
Indeed, a recent meta-analysis of approximately 45,000
Figure 4. Quantification of atherosclerotic lesions area patients in 19 clinical trials suggests that selective inhibi-
in aortas of wildtype (+/+), TP deficient (TP-/-) and IP tion of COX-2 elevates blood pressure more than non-se-
deficient (IP -/-) mice on an apoE deficient background at
20 weeks of age. TP deficiency retarded and IP deficiency
lective inhibition.30
accelerated atherogenesis, suggesting that these mediators
have opposing roles in atherosclerotic lesion development. Data Detection of a Cardiovascular Risk of the Coxibs
are means ± SEM (n = 5 each). Epidemiological approaches and clinical trials have rela-
(Redrawn with permission from Kobayashi T, Tahara Y,
Matsumoto M, et al. Roles of thromboxane A2 and prostacyclin
tively poor precision for the detection of uncommon but
in the development of atherosclerosis in apoE-deficient mice. J serious adverse effects, such as clinical events that are preva-
Clin Invest. 2004;114(6):784-94.) lent in the relevant populations. The first clinical evidence
448 American Society of Hematology
of a cardiovascular hazard of the coxibs arose when a 5- stopped at 36 months of treatment when a twofold increase
fold higher incidence of myocardial infarction was observed in the cardiovascular event rate (rofecoxib: 1.5% vs pla-
in the rofecoxib group as compared to the naproxen com- cebo: 0.78%) was noticed. This suggests that a small mi-
parator group of the VIGOR study, the prospective trial nority of the patients, apparently of initial low risk of car-
designed to assess rofecoxib’s gastrointestinal safety.4 Ap- diovascular disease, might have proceeded to increase that
proximately 8000 rheumatoid arthritis patients were treated risk to a point that culminated in clinical events. A similar
either with rofecoxib or naproxen with a median follow-up pattern, again, implying a time-dependent change of car-
of 9 months. The gastrointestinal event rate was reduced diovascular risk, was observed in a long-term cancer pre-
from 4.5 to 2.1 per 100 patient-years by rofecoxib. The vention trials of celecoxib in patients of initially low ap-
study population would probably be considered medium parent cardiovascular risk. The Adenoma Prevention with
cardiovascular risk at baseline—with chronic rheumatoid Celecoxib (APC) study detected a dose-dependent increase
inflammation as an independent risk factor. Two explana- in the cardiovascular event rate (placebo, 1%; celecoxib
tions for the adverse cardiovascular outcome were discussed 200 mg/bid, 2.3%; celecoxib 400 mg/bid, 3.4%) in a study
at the time—aside from the possibility that this was due to population of 2035 patients after 36 months of exposure.14
chance:2 (i) a reduction of the cardiovascular event rate in An unpublished, smaller trial (“preSAP Trial”) that included
the control group by a cardioprotective effect of naproxen; approximately 1500 adenoma patients receiving a single
and/or (ii) a cardiovascular hazard of rofecoxib. Naproxen, daily dose of 400 mg celecoxib has shown a non-signifi-
unlike other tNSAIDs, has a long elimination half-life and cant increase in cardiovascular events (placebo: 0.91% vs
causes an extended inhibition of platelet function and celecoxib: 1.23%; FDA Advisory Committee Meeting,
might provide some degree of cardioprotection.2 However, Gaithersburg, Maryland, February 16–18, 2005). This may
the substantial interindividual variability of its activity relate to the difference in dosing (once daily vs twice daily
suggests that much fewer patients would benefit from in the APC study) and to the lower power of the preSAP
naproxen than from aspirin.35 This is consistent with obser- trial.
vational studies that detected a small cardioprotective ben- The cardiovascular signal was detected very early in
efit from naproxen—approximately half that of aspirin.36 two postoperative pain management trials of high risk pa-
While the absolute number of cardiovascular events in tients, referred to as ‘CABG-1’ and ‘CABG-2.’15, 38 Patients
VIGOR was too small to estimate accurately the size of the undergoing coronary bypass surgery were initially treated
effect, the potential cardioprotective effect of naproxen intravenously with the prodrug of valdecoxib, parecoxib,
alone is unlikely to account for the 5-fold difference be- or placebo and then switched to oral valdecoxib or pla-
tween the groups. It seems more plausible that this coin- cebo. The majority of cardiovascular events occurred
cided with a cardiovascular hazard of rofecoxib. In contrast within days of treatment initiation in these populations,
to rofecoxib, no excess cardiovascular risk was initially who were subject to intense hemostatic activation after
associated with celecoxib therapy in its gastrointestinal bypass surgery. The outcomes of the CABG studies are com-
safety study, the CLASS trial.6 However, in this study the patible with a prothrombotic effect of the coxibs in situa-
use of low-dose aspirin was allowed and one of the tNSAID tions of elevated thrombotic risk. In summary, the com-
comparators was diclofenac, which is similar to celecoxib bined clinical experience of trials that detected cardiovas-
in its degree of COX-2 selectivity. Additionally, the patient cular complications attributable to the coxibs suggests that
population in the CLASS trial was probably at lower the emergence of events relates to baseline cardiovascular
baseline risk for cardiovascular events as compared to the risk and to the duration of drug exposure, which accords
VIGOR trial. The third large gastrointestinal safety study, remarkably with the biological observations discussed
the TARGET trial, assessed also the cardiovascular safety above.
profile of lumiracoxib in comparison to ibuprofen and
naproxen in approximately 18,000 osteoarthritis patients, Conclusions and Future Directions
of which a quarter took also low-dose aspirin. An impor- The distinct roles of the COX isoforms in platelet function,
tant finding of this study was that the favorable gastrointes- atherogenesis and blood pressure control provide a uni-
tinal safety profile of the COX-2 inhibitor was offset by tary, plausible mechanism—depression of vascular PGI2
concurrent low-dose aspirin therapy and the advantage over biosynthesis—by which selective inhibition of COX-2 may
a tNSAID was lost.5 Lumiracoxib was not associated with a increase the likelihood of myocardial infarction and stroke
statistically significant increase in cardiovascular risk in in at-risk patients and in patients who are exposed for ex-
this population of apparently low baseline risk exposed for tended periods of time. Mouse biology, human pharmacol-
only 12 months.37 ogy, and clinical evidence suggest that the cardiovascular
The trial that led to the withdrawal of rofecoxib—the hazard pertains to all coxibs. However, it seems likely that
Adenomatous Polyp Prevention on Vioxx (APPROVe) study, differences in the degree of selectivity attained by various
a placebo controlled cancer prevention trial of approxi- drugs may translate into quantitative differences in clini-
mately 2600 patients—detected the cardiovascular risk cal outcomes. Both the US Food and Drug Administration
only after a much longer time of drug exposure.13 It was (FDA) and the European Agency for the Evaluation of
Hematology 2005 449
Medicinal Products (EMEA) concluded that rofecoxib, in their response to the coxibs7 and the existence of
valdecoxib and celecoxib conveyed a small (1%–2%), but clinical conditions that can modulate the response may
absolute risk of cardiovascular adverse events. Rofecoxib be exploited to identify the small number of patients
and valdecoxib have been withdrawn from the market in at emerging cardiovascular risk. Regular monitoring
the US and Europe. The FDA applied a “black box” warn- of risk factors during the treatment, including frequent
ing to celecoxib, which remains on the market, and the blood pressure measurement, is a first step.
EMEA imposed restrictions on celecoxib (and on etori-
coxib, which is on the market in some European countries), References
and it is possible that new coxibs will be introduced to the 1. FitzGerald GA. COX-2 and beyond: approaches to prostag-
market probably with similar restrictions. landin inhibition in human disease. Nat Rev Drug Discov.
2003;2:879-890.
What role, then, can the coxibs play in the treatment of 2. FitzGerald GA, Patrono C. The coxibs, selective inhibitors of
chronic inflammatory conditions in the future? cyclooxygenase-2. N Engl J Med. 2001;345:433-442.
i. They should be reserved for patients who are most 3. Ballou LR, Botting RM, Goorha S, Zhang J, Vane JR.
likely to benefit from them, for example those who Nociception in cyclooxygenase isozyme-deficient mice.
Proc Natl Acad Sci U S A. 2000;97:10272-10276.
develop gastrointestinal complications on tNSAIDs in 4. Bombardier C, Laine L, Reicin A, et al. Comparison of upper
combination with a gastroprotective medication, such gastrointestinal toxicity of rofecoxib and naproxen in patients
as a proton pump inhibitor. The dilemma is that the with rheumatoid arthritis. VIGOR Study Group. N Engl J Med.
only drug presently on the US market, celecoxib, has 2000;343:1520-1528.
5. Schnitzer TJ, Burmester GR, Mysler E, et al. Comparison of
not convincingly demonstrated a gastrointestinal ben- lumiracoxib with naproxen and ibuprofen in the Therapeutic
efit in its outcome trial even if this may relate in part to Arthritis Research and Gastrointestinal Event Trial (TAR-
a suboptimal study design.6 GET), reduction in ulcer complications: randomised
ii. Coxibs should be avoided when patients have preex- controlled trial. Lancet. 2004;364:665-674.
6. Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal
isting risk factors for cardiovascular events. toxicity with celecoxib vs nonsteroidal anti-inflammatory
iii. The cardiovascular roles of the COX products affected drugs for osteoarthritis and rheumatoid arthritis: the CLASS
by the coxibs are not meant to be viewed as an imbal- study: a randomized controlled trial. Celecoxib Long-term
ance of PGI2 and TxA2, which might imply that sup- Arthritis Safety Study. JAMA. 2000;284:1247-1255.
7. Fries S, Grosser T, Price TS, et al. Marked interindividual
pression of TxA2 by low-dose aspirin would be com- variability in the response to selective inhibitors of
pletely protective against a cardiovascular hazard. PGI2 cyclooxygenase-2. Gastroenterology. 2005;in press.
acts as a constraint on the biological activity of all 8. McAdam BF, Catella-Lawson F, Mardini IA, Kapoor S,
agonists, which stimulate platelets, elevate blood pres- Lawson JA, FitzGerald GA. Systemic biosynthesis of
prostacyclin by cyclooxygenase (COX)-2: the human
sure, and accelerate atherogenesis, of which TxA2 is pharmacology of a selective inhibitor of COX-2. Proc Natl
only one mediator. Thus, low dose aspirin would be Acad Sci U S A. 1999;96:272-277.
expected to attenuate, rather than abolish the cardio- 9. Catella-Lawson F, McAdam B, Morrison BW, et al. Effects of
vascular hazard deriving from selective inhibition of specific inhibition of cyclooxygenase-2 on sodium balance,
hemodynamics, and vasoactive eicosanoids. J Pharmacol
COX-2. Exp Ther. 1999;289:735-741.
iv. We know very little about the cardiovascular safety 10. Cheng Y, Austin SC, Rocca B, et al. Role of prostacyclin in
profile of individual tNSAIDs. The FDA applied a the cardiovascular response to thromboxane A2. Science.
“black box” warning of potential cardiovascular risks 2002;296:539-541.
11. Qi Z, Hao CM, Langenbach RI, et al. Opposite effects of
also to all tNSAIDs, while the EMEA concluded that cyclooxygenase-1 and -2 activity on the pressor response
there was no evidence to prompt a change in their ad- to angiotensin II. J Clin Invest. 2002;110:61-69.
vice about tNSAIDs. Clearly, prospective studies are 12. Kobayashi T, Tahara Y, Matsumoto M, et al. Roles of
warranted to determine if patients are at elevated car- thromboxane A2 and prostacyclin in the development of
atherosclerosis in apoE-deficient mice. J Clin Invest.
diovascular risk with long-term use of specific 2004;114:784-794.
tNSAIDs. Pharmacologic studies have already found 13. Bresalier RS, Sandler RS, Quan H, et al. Cardiovascular
that ibuprofen and naproxen can undermine the anti- events associated with rofecoxib in a colorectal adenoma
platelet effectiveness of low-dose aspirin, but not chemoprevention trial. N Engl J Med. 2005;352:1092-1102.
14. Solomon SD, McMurray JJ, Pfeffer MA, et al. Cardiovascular
diclofenac.39,40 This indicates that tNSAIDs are not a risk associated with celecoxib in a clinical trial for colorectal
homogenous group of compounds and it is likely that adenoma prevention. N Engl J Med. 2005;352:1071-1080.
differences in their cardiovascular safety profiles will 15. Nussmeier NA, Whelton AA, Brown MT, et al. Complications
be revealed, just like the differences in their gastrointes- of the COX-2 inhibitors parecoxib and valdecoxib after
cardiac surgery. N Engl J Med. 2005;352:1081-1091.
tinal safety profiles. 16. Topper JN, Cai J, Falb D, Gimbrone MA, Jr. Identification of
v. Finally, as we move towards an individualization of vascular endothelial genes differentially responsive to fluid
therapy, we should identify paradigms within which mechanical stimuli: cyclooxygenase-2, manganese
these useful drugs can be administered safely for ex- superoxide dismutase, and endothelial cell nitric oxide
synthase are selectively up-regulated by steady laminar
tended periods in individuals at low cardiovascular shear stress. Proc Natl Acad Sci U S A. 1996;93:10417-
risk. The detectable variability between individuals 10422.
450 American Society of Hematology
17. Grosser T, Yusuff S, Cheskis E, Pack MA, FitzGerald GA. 29. Francois H, Coffman TM. Prostanoids and blood pressure:
Developmental expression of functional cyclooxygenases in which way is up? J Clin Invest. 2004;114:757-759.
zebrafish. Proc Natl Acad Sci U S A. 2002;99:8418-8423. 30. Aw TJ, Haas SJ, Liew D, Krum H. Meta-analysis of
18. Patrignani P, Panara MR, Greco A, et al. Biochemical and cyclooxygenase-2 inhibitors and their effects on blood
pharmacological characterization of the cyclooxygenase pressure. Arch Intern Med. 2005;165:490-496.
activity of human blood prostaglandin endoperoxide 31. Athirakul K, Kim HS, Audoly LP, Smithies O, Coffman TM.
synthases. J Pharmacol Exp Ther. 1994;271:1705-1712. Deficiency of COX-1 causes natriuresis and enhanced
19. Jick SS. The risk of gastrointestinal bleed, myocardial sensitivity to ACE inhibition. Kidney Int. 2001;60:2324-2329.
infarction, and newly diagnosed hypertension in users of 32. Zewde T, Mattson DL. Inhibition of cyclooxygenase-2 in the
meloxicam, diclofenac, naproxen, and piroxicam. Pharmaco- rat renal medulla leads to sodium-sensitive hypertension.
therapy. 2000;20:741-744. Hypertension. 2004;44:424-428.
20. Collaborative meta-analysis of randomised trials of 33. Dilger K, Herrlinger C, Peters J, Seyberth HW, Schweer H,
antiplatelet therapy for prevention of death, myocardial Klotz U. Effects of celecoxib and diclofenac on blood
infarction, and stroke in high risk patients. Br Med J. pressure, renal function, and vasoactive prostanoids in
2002;324:71-86. young and elderly subjects. J Clin Pharmacol. 2002;42:985-
21. Grosser T, Zucker TP, Weber AA, et al. Thromboxane A2 994.
induces cell signaling but requires platelet-derived growth 34. Cheng HF, Wang JL, Zhang MZ, Wang SW, McKanna JA,
factor to act as a mitogen. Eur J Pharmacol. 1997;319:327- Harris RC. Genetic deletion of COX-2 prevents increased
332. renin expression in response to ACE inhibition. Am J Physiol
22. Eikelboom JW, Hirsh J, Weitz JI, Johnston M, Yi Q, Yusuf S. Renal Physiol. 2001;280:F449-456.
Aspirin-resistant thromboxane biosynthesis and the risk of 35. Capone ML, Tacconelli S, Sciulli MG, et al. Clinical pharma-
myocardial infarction, stroke, or cardiovascular death in cology of platelet, monocyte, and vascular cyclooxygenase
patients at high risk for cardiovascular events. Circulation. inhibition by naproxen and low-dose aspirin in healthy
2002;105:1650-1655. subjects. Circulation. 2004;109:1468-1471.
23. Rocca B, Secchiero P, Ciabattoni G, et al. Cyclooxygenase- 36. Juni P, Nartey L, Reichenbach S, Sterchi R, Dieppe PA,
2 expression is induced during human megakaryopoiesis Egger M. Risk of cardiovascular events and rofecoxib:
and characterizes newly formed platelets. Proc Natl Acad cumulative meta-analysis. Lancet. 2004;364:2021-2029.
Sci U S A. 2002;99:7634-7639. 37. Farkouh ME, Kirshner H, Harrington RA, et al. Comparison
24. Zimmermann N, Wenk A, Kim U, et al. Functional and of lumiracoxib with naproxen and ibuprofen in the Therapeu-
biochemical evaluation of platelet aspirin resistance after tic Arthritis Research and Gastrointestinal Event Trial
coronary artery bypass surgery. Circulation. 2003;108:542- (TARGET), cardiovascular outcomes: randomised con-
547. trolled trial. Lancet. 2004;364:675-684.
25. Egan KM, Lawson JA, Fries S, et al. COX-2 derived 38. Ott E, Nussmeier NA, Duke PC, et al. Efficacy and safety of
prostacyclin confers atheroprotection on female mice. the cyclooxygenase 2 inhibitors parecoxib and valdecoxib in
Science. 2004;360:1954-1957. patients undergoing coronary artery bypass surgery. J
26. Burleigh ME, Babaev VR, Oates JA, et al. Cyclooxygenase- Thorac Cardiovasc Surg. 2003;125:1481-1492.
2 promotes early atherosclerotic lesion formation in LDL 39. Catella-Lawson F, Reilly MP, Kapoor SC, et al.
receptor-deficient mice. Circulation. 2002;105:1816-1823. Cyclooxygenase inhibitors and the antiplatelet effects of
27. Egan KM, Wang M, Lucitt MB, et al. Cyclooxygenases, aspirin. N Engl J Med. 2001;345:1809-1817.
thromboxane, and atherosclerosis: plaque destabilization by 40. Capone ML, Sciulli MG, Tacconelli S, et al. Pharmacody-
cyclooxygenase-2 inhibition combined with thromboxane namic interaction of naproxen with low-dose aspirin in
receptor antagonism. Circulation. 2005;111:334-342. healthy subjects. J Am Coll Cardiol. 2005;45:1295-1301.
28. Cayatte AJ, Du Y, Oliver-Krasinski J, Lavielle G, Verbeuren
TJ, Cohen RA. The thromboxane receptor antagonist
S18886 but not aspirin inhibits atherogenesis in apo E-
deficient mice: evidence that eicosanoids other than
thromboxane contribute to atherosclerosis. Arterioscler
Thromb Vasc Biol. 2000;20:1724-1728.
Hematology 2005 451
You might also like
- Obstetric Highlights Elmar P. Sakala PDFDocument47 pagesObstetric Highlights Elmar P. Sakala PDFwalt65No ratings yet
- IGCSE Excretion in Humans (Edited)Document59 pagesIGCSE Excretion in Humans (Edited)elizabethNo ratings yet
- Ncm117-Lecture NotesDocument18 pagesNcm117-Lecture NotesTherese Margaret100% (1)
- Approach To Patient With Endocrine DisordersDocument2 pagesApproach To Patient With Endocrine DisordersSeff CausapinNo ratings yet
- Community health nursing exam questionsDocument10 pagesCommunity health nursing exam questionsCiena MaeNo ratings yet
- Annotated Bibliography of Obstetrics & Gynaecology ResourcesDocument4 pagesAnnotated Bibliography of Obstetrics & Gynaecology ResourcesKaku ManishaNo ratings yet
- COX-2 Inhibitors and Cardiovascular RiskDocument3 pagesCOX-2 Inhibitors and Cardiovascular RiskelhierofanteNo ratings yet
- HNPDocument10 pagesHNPPattia1980No ratings yet
- Coxibs and Heart Disease: What We Have Learned and What Else We Need To KnowDocument14 pagesCoxibs and Heart Disease: What We Have Learned and What Else We Need To KnowYariCárdenasNo ratings yet
- Mechanisms Underlying The Cardiovascular Effects of COX-InhibitionDocument14 pagesMechanisms Underlying The Cardiovascular Effects of COX-InhibitionRangwani NesbitNo ratings yet
- Update On The Clinical Pharmacology of Etoricoxib A Potent Cyclooxygenase2 InhibitorDocument21 pagesUpdate On The Clinical Pharmacology of Etoricoxib A Potent Cyclooxygenase2 InhibitorAnh Quoc LeNo ratings yet
- Cox 2 InhibitorsDocument9 pagesCox 2 InhibitorsirlandagarandaNo ratings yet
- Walker 2017Document18 pagesWalker 2017ericdgNo ratings yet
- Cyclooxygenase-2 in Cardiovascular Biology: BackgroundDocument6 pagesCyclooxygenase-2 in Cardiovascular Biology: BackgroundDiego PicchioNo ratings yet
- EditorialDocument2 pagesEditorialWulandari EmyNo ratings yet
- Evolution of Nonsteroidal Anti-Inflammatory Drugs (Nsaids) : Cyclooxygenase (Cox) Inhibition and BeyondDocument30 pagesEvolution of Nonsteroidal Anti-Inflammatory Drugs (Nsaids) : Cyclooxygenase (Cox) Inhibition and BeyondnesakusumaNo ratings yet
- The Fall of Selective COX-2 InhibitorsDocument2 pagesThe Fall of Selective COX-2 Inhibitorssujay3001No ratings yet
- COX-2 Selectivity Alone Does Not de Ne The Cardiovascularrisks Associated With Non-Steroidal Anti-In Ammatory DrugsDocument4 pagesCOX-2 Selectivity Alone Does Not de Ne The Cardiovascularrisks Associated With Non-Steroidal Anti-In Ammatory DrugsruleshellzNo ratings yet
- Coxibs - 2001 PDFDocument10 pagesCoxibs - 2001 PDFJavier Apolinario VargasNo ratings yet
- CELECOXIBDocument5 pagesCELECOXIBdwikNo ratings yet
- Sem+5 Yu+Et+Al.+ +2012+ +Vascular+COX 2+Modulates+Blood+Pressure+and+Thrombosis+in+MiceDocument8 pagesSem+5 Yu+Et+Al.+ +2012+ +Vascular+COX 2+Modulates+Blood+Pressure+and+Thrombosis+in+MiceJaviera Lecaros VásquezNo ratings yet
- Selective COX-2 Inhibitors: A Review of Their Structure-Activity RelationshipsDocument30 pagesSelective COX-2 Inhibitors: A Review of Their Structure-Activity RelationshipsMona SalihNo ratings yet
- Selective COX-2 Inhibitors and Risk of Cardiovascular EventsDocument6 pagesSelective COX-2 Inhibitors and Risk of Cardiovascular EventsAditya Rahman RYNo ratings yet
- Cyclooxygenase-2 Inhibitors and Atherosclerosis : Editorial CommentDocument3 pagesCyclooxygenase-2 Inhibitors and Atherosclerosis : Editorial CommentNyoman Marsel Rama GranditaNo ratings yet
- Update on COX-2-selective NSAIDs for treating pain and inflammation in horsesDocument4 pagesUpdate on COX-2-selective NSAIDs for treating pain and inflammation in horsesSusanaNo ratings yet
- Cox and CancerDocument8 pagesCox and CancerIvana YunitaNo ratings yet
- Risk PDFDocument50 pagesRisk PDFErick Antonio Castillo GurdianNo ratings yet
- Cyclooxygenase-2 Inhibitors - StrokeDocument17 pagesCyclooxygenase-2 Inhibitors - StrokeSaidah AzlanNo ratings yet
- Cox in Health & Disease.pDocument11 pagesCox in Health & Disease.pSuji SusanthNo ratings yet
- Drug-Induced Renal FailureDocument14 pagesDrug-Induced Renal FailureFiorella Mamani AceroNo ratings yet
- Per A Zella 2003Document14 pagesPer A Zella 2003Fathanah Yanti MphNo ratings yet
- Cardiovascular Risk of Nonsteroidal Anti-Inflammatory Drugs: An Under-Recognized Public Health IssueDocument12 pagesCardiovascular Risk of Nonsteroidal Anti-Inflammatory Drugs: An Under-Recognized Public Health IssueAri Dwi PrasetyoNo ratings yet
- Celecoxib Pharmacogenomics: CYP2C9 Role in MetabolismDocument5 pagesCelecoxib Pharmacogenomics: CYP2C9 Role in MetabolismdwikNo ratings yet
- Cox 2 DocumentDocument29 pagesCox 2 DocumentLanggeng Perdhana Jangan MenyerahNo ratings yet
- KetorolacDocument8 pagesKetorolacwalit1101 mukrininNo ratings yet
- Review Article: Alleviating Promotion of Inflammation and Cancer Induced by Nonsteroidal Anti-Inflammatory DrugsDocument18 pagesReview Article: Alleviating Promotion of Inflammation and Cancer Induced by Nonsteroidal Anti-Inflammatory DrugsNadiaa MJNo ratings yet
- Perspective: Structural and Functional Basis of Cyclooxygenase InhibitionDocument17 pagesPerspective: Structural and Functional Basis of Cyclooxygenase InhibitionAlexandre Valério MussioNo ratings yet
- Indomethacin in 700100 PDFDocument28 pagesIndomethacin in 700100 PDFAdrien JacintoNo ratings yet
- Renal Effects of Selective Cyclo-Oxygenase-2 (COX-2) InhibitorsDocument3 pagesRenal Effects of Selective Cyclo-Oxygenase-2 (COX-2) InhibitorsMohammedMukdadNo ratings yet
- Evolution of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Cyclooxygenase (COX) Inhibition and BeyondDocument31 pagesEvolution of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Cyclooxygenase (COX) Inhibition and BeyondAlexandru SavaNo ratings yet
- Inibizione Della Ciclossigenasi e Rischio Cardiovascolare: Farmaci Antinfiammatori Non Steroidei Tradizionali e Selettivi Per La Ciclossigenasi-2Document18 pagesInibizione Della Ciclossigenasi e Rischio Cardiovascolare: Farmaci Antinfiammatori Non Steroidei Tradizionali e Selettivi Per La Ciclossigenasi-2CeceNo ratings yet
- Selective Cox-2 Inhibitor: Visha.M.GDocument6 pagesSelective Cox-2 Inhibitor: Visha.M.GinventionjournalsNo ratings yet
- Intermittent Hypoxia-Activated Cyclooxygenase Pathway: Role in AtherosclerosisDocument10 pagesIntermittent Hypoxia-Activated Cyclooxygenase Pathway: Role in AtherosclerosisaditNo ratings yet
- Targeting NOX, INOS and COX-2 in in Ammatory Cells: Chemoprevention Using Food PhytochemicalsDocument7 pagesTargeting NOX, INOS and COX-2 in in Ammatory Cells: Chemoprevention Using Food PhytochemicalsLe Cong HuanNo ratings yet
- Renal Medullary Interstitial COX-2 Is Essential in Preventing Saltsensitve Hypertension and Maintaining Renal Inner MedullaDocument17 pagesRenal Medullary Interstitial COX-2 Is Essential in Preventing Saltsensitve Hypertension and Maintaining Renal Inner MedullaMumtaz Maulana HidayatNo ratings yet
- 2012 Carnevale D. PI3K in Hypertension A Novel Therapeutic Target Controlling Vascular Myogenic Tone and Target Organ DamageDocument6 pages2012 Carnevale D. PI3K in Hypertension A Novel Therapeutic Target Controlling Vascular Myogenic Tone and Target Organ DamageAndi Suchy Qumala SarieNo ratings yet
- Pharmacology - Anti-Inflammatory Drugs - Corticosteroid, NSAID, Leukotriene (Eicosanoids)Document9 pagesPharmacology - Anti-Inflammatory Drugs - Corticosteroid, NSAID, Leukotriene (Eicosanoids)Itharshan IndreswaranNo ratings yet
- Study of Osteoarthritis Treatment With Anti-InflammatoryDocument11 pagesStudy of Osteoarthritis Treatment With Anti-InflammatoryDezha DetiroNo ratings yet
- PainoxiaDocument66 pagesPainoxiaOmar WahbiNo ratings yet
- In Silico Study of Selected Lignins As COX-2 InhibitorsDocument22 pagesIn Silico Study of Selected Lignins As COX-2 InhibitorsRahmat Eko SanjayaNo ratings yet
- Lec 17Document15 pagesLec 17Abdullahayad farouqNo ratings yet
- Defining The Problem of Treating The Patient With Hypertension and Arthritis PainDocument7 pagesDefining The Problem of Treating The Patient With Hypertension and Arthritis PainromzikerenzNo ratings yet
- Batlouni Introduação PDFDocument8 pagesBatlouni Introduação PDFEryclisNunesNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs in Animals - Pharmacology - MSD Veterinary ManualDocument12 pagesNonsteroidal Anti-Inflammatory Drugs in Animals - Pharmacology - MSD Veterinary ManualFairuz Nanda MarhabanazNo ratings yet
- COX-1, COX-2, and COX-3 and The Future Treatment of Chronic Inflammatory DiseaseDocument3 pagesCOX-1, COX-2, and COX-3 and The Future Treatment of Chronic Inflammatory DiseaseFabiula AbreuNo ratings yet
- Aspirin Insensitive Eicosanoid Biosynthesis in Cardiovascular DiseaseDocument6 pagesAspirin Insensitive Eicosanoid Biosynthesis in Cardiovascular DiseaseBryam Smith MolinaNo ratings yet
- Myocardial Glutathione Synthase and TRXIDocument12 pagesMyocardial Glutathione Synthase and TRXImercuryboss90No ratings yet
- Aines HorseDocument15 pagesAines HorseOscar Ivan AngaritaNo ratings yet
- And Prevention of Thrombosis, 9th Ed: Antiplatelet Drugs: Antithrombotic TherapyDocument33 pagesAnd Prevention of Thrombosis, 9th Ed: Antiplatelet Drugs: Antithrombotic TherapyNube AzulNo ratings yet
- Using N, N, N',N'-tetramethyl-p-phenylenediamine (TMPD) To Assay Cyclooxygenase Activity in VitroDocument13 pagesUsing N, N, N',N'-tetramethyl-p-phenylenediamine (TMPD) To Assay Cyclooxygenase Activity in VitroTatianaAlejandraCárdenasSolanoNo ratings yet
- 01 HYP 0000115921 55353 E0-2Document5 pages01 HYP 0000115921 55353 E0-2marie gold sorilaNo ratings yet
- Review Article: Review of The Cardiovascular Safety of Coxibs Compared To NsaidsDocument6 pagesReview Article: Review of The Cardiovascular Safety of Coxibs Compared To NsaidsPutu Gede GandharaNo ratings yet
- Cycloxygenase Enzymes COX I& IIDocument29 pagesCycloxygenase Enzymes COX I& IISufyan AshrafNo ratings yet
- Cyclooxygenase-2 Biology: Joan ClàriaDocument15 pagesCyclooxygenase-2 Biology: Joan ClàriajustrudinNo ratings yet
- Pharmacological Analysis of Cyclooxygenase-1 in InflammationDocument7 pagesPharmacological Analysis of Cyclooxygenase-1 in InflammationUrias P. VazNo ratings yet
- Comparative Pathophysiology and Toxicology of CyclooxygenasesFrom EverandComparative Pathophysiology and Toxicology of CyclooxygenasesNo ratings yet
- Acute pancreatitis symptoms, causes and diagnosisDocument12 pagesAcute pancreatitis symptoms, causes and diagnosisAmol DhopteNo ratings yet
- Health Psychology Migraine ProjectDocument46 pagesHealth Psychology Migraine Projectwajiha yaminNo ratings yet
- Artificial HeartDocument17 pagesArtificial HeartRAKESHKANNAN100% (1)
- Respiratory Physiology in Pregnancy ReviewDocument13 pagesRespiratory Physiology in Pregnancy ReviewAlejandra RequesensNo ratings yet
- HAI Surveillance ChallengesDocument78 pagesHAI Surveillance ChallengesMichael EdmondNo ratings yet
- Caduet (Dr. Ismahun Maret 2009)Document41 pagesCaduet (Dr. Ismahun Maret 2009)Yulia SumarnaNo ratings yet
- Clinical Practice Handbook For Quality Abortion CareDocument66 pagesClinical Practice Handbook For Quality Abortion CareRaj ShahNo ratings yet
- Bovi-Shield Gold FP 5 VL5Document2 pagesBovi-Shield Gold FP 5 VL5טורו קוראזוןNo ratings yet
- Concept of Pregnancy Final NCM 107 07172019Document6 pagesConcept of Pregnancy Final NCM 107 07172019Jarod Hembrador100% (1)
- Unit - One: Renowned Biologists in EthiopiaDocument1 pageUnit - One: Renowned Biologists in EthiopiaMmeklit Mmeklit0% (1)
- Center For BrainHealthDocument5 pagesCenter For BrainHealthJames KuhnNo ratings yet
- DISORDERDocument3 pagesDISORDERMia Grace GarciaNo ratings yet
- Complex Regional Pain Syndrome (CRPS) Type I: Historical Perspective and Critical IssuesDocument7 pagesComplex Regional Pain Syndrome (CRPS) Type I: Historical Perspective and Critical IssuesSheilaNo ratings yet
- Cad NCPDocument1 pageCad NCPKrizzia Mae F. MayoresNo ratings yet
- Renal PhysiologyDocument5 pagesRenal PhysiologyJayricDepalobosNo ratings yet
- DAFTAR PUSTAKA ProposalDocument2 pagesDAFTAR PUSTAKA ProposalPipik TaufikNo ratings yet
- Shigella SPP, Vibrio SPPDocument6 pagesShigella SPP, Vibrio SPPtomal7811islamNo ratings yet
- Health Insurance Guidelines 2020-21Document25 pagesHealth Insurance Guidelines 2020-21NIRAJ BAHEKARNo ratings yet
- Monkeypox Contact Tracing Classification and Vaccination MatrixDocument2 pagesMonkeypox Contact Tracing Classification and Vaccination MatrixCemNo ratings yet
- Nama ObatDocument13 pagesNama Obatsahmin sahminNo ratings yet
- American Journal of Emergency MedicineDocument7 pagesAmerican Journal of Emergency MedicineVirgi AgustiaNo ratings yet
- 1st GNM VivaDocument144 pages1st GNM VivaPatel MitanshiNo ratings yet
- Admit List PG 2nd Counselling 2013Document113 pagesAdmit List PG 2nd Counselling 2013gautambobNo ratings yet
- The Pocket DoctorDocument132 pagesThe Pocket DoctorArthur Hebert100% (1)