Professional Documents
Culture Documents
Asthma: DR Yusuf Adi Gunawan SPPD
Uploaded by
Ian GalihOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Asthma: DR Yusuf Adi Gunawan SPPD
Uploaded by
Ian GalihCopyright:
Available Formats
Asthma
dr Yusuf Adi Gunawan SpPD
Differential Diagnosis
• Allergic and Environmental Asthma
• Aspergillosis
• Bronchiectasis
• Bronchiolitis
• Chronic Obstructive Pulmonary Disease (COPD)
• Chronic Sinusitis
• Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss Syndrome)
• Cystic Fibrosis
• Foreign Body Aspiration
• Gastroesophageal Reflux Disease
• Heart Failure
• Pulmonary Embolism (PE)
• Pulmonary Eosinophilia
• Sarcoidosis
• Upper Respiratory Tract Infection
• Vocal Cord Dysfunction
Diagnostic
Criteria
Treatment
• Airway
– Oxygen, excessive sputum
• Breathing
– tachypneu
• Circulation
– Shock, altered conciousness
• Remove any possible allergenic agent form
patient’s body
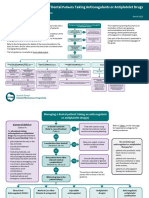
GINA 2020, Box 3-4A
© Global Initiative for Asthma, www.ginasthma.org
GINA 2020, Box 3-4B
© Global Initiative for Asthma, www.ginasthma.org
Adverse effects with montelukast
• FDA boxed warning in March 2020 about risk
of serious neuropsychiatric events, including
suicidality, with montelukast
– Includes suicidality in adults and adolescents
– Nightmares and behavioral problems in children
• Before prescribing montelukast, health
professionals should consider its benefits and
risks, and patients should be counselled about
the risk of neuropsychiatric events
Patients with features of asthma and COPD
• Also called ‘asthma-COPD overlap’ or ‘asthma+COPD’
– NOT a single disease, but a descriptive label for patients commonly seen in clinical
practice
• Asthma and COPD are heterogeneous and overlapping conditions
– The definitions of asthma and COPD are not mutually exclusive
– Each includes several phenotypes that are likely to have different underlying
mechanisms
– There is increasing interest in the potential for precision treatment
• However, the labels ‘asthma’ and ‘COPD’ are still clinically important, as evidence
supports safety-based differences in treatment recommendations
– Asthma: never treat with bronchodilators alone (risk of death, hospitalization, severe
exacerbations)
– COPD: start treatment with LABA and/or LAMA without ICS
– Patients with diagnoses of both asthma and COPD are more likely to die or be
hospitalized if treated with LABA vs ICS-LABA (Gershon et al, JAMA 2014; Kendzerska et al, Annals ATS 2019)
– High dose ICS may be needed for severe asthma, but should not be used in COPD (risk of
pneumonia)
• Chapter 5 has been rewritten for clinical utility, focusing on clinical recognition and
safe initial treatment
Patients with features of asthma and
COPD
GINA 2020, Box 5-2
Update 2020
A reminder – the key change in GINA 2019
© Global Initiative for Asthma, www.ginasthma.org
Background to changes in 2019 - the risks of SABA-only treatment
• Regular or frequent use of SABA is associated with adverse effects
– b-receptor downregulation, decreased bronchoprotection, rebound
hyperresponsiveness, decreased bronchodilator response (Hancox, Respir Med 2000)
– Increased allergic response, and increased eosinophilic airway
inflammation
(Aldridge, AJRCCM 2000)
• Higher use of SABA is associated with adverse clinical outcomes
– Dispensing of ≥3 canisters per year (average 1.7 puffs/day) is associated
with higher risk of emergency department presentations (Stanford, AAAI 2012)
– Dispensing of ≥12 canisters per year is associated with higher risk of
death (Suissa, AJRCCM 1994)
COVID-19 and asthma (as at April 3, 2020)
• Advise patients with asthma to continue taking their prescribed asthma medications,
particularly inhaled corticosteroids (ICS), and oral corticosteroids (OCS) if prescribed
– Asthma medications should be continued as usual. Stopping ICS often leads to potentially
dangerous worsening of asthma
– For patients with severe asthma: continue biologic therapy, and do not suddenly stop OCS if
prescribed
• Make sure that all patients have a written asthma action plan with instructions about:
– Increasing controller and reliever medication when asthma worsens
– Taking a short course of OCS for severe asthma exacerbations
– When to seek medical help
– See the GINA 2020 report for more information about treatment options for asthma action
plans.
• Avoid nebulizers where possible
– Nebulizers increase the risk of disseminating virus to other patients AND to health care
professionals
– Pressurized metered dose inhaler via a spacer is the preferred treatment during severe
exacerbations, with a mouthpiece or tightly fitting face mask if required
You might also like
- Bronchial AsthmaDocument59 pagesBronchial Asthmashefalika mandremNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Zuhaib SynopsisDocument24 pagesZuhaib Synopsisthehealer7No ratings yet
- Managing Breathlessness in the CommunityFrom EverandManaging Breathlessness in the CommunityRating: 3.5 out of 5 stars3.5/5 (2)
- Whats New in GINA 2021 - Final - V2Document52 pagesWhats New in GINA 2021 - Final - V2Wialda Dwi rodyahNo ratings yet
- Severe Asthma in Primary Care: Identification and ManagementDocument8 pagesSevere Asthma in Primary Care: Identification and ManagementIzza UrfanNo ratings yet
- Global Initiative For Asthma (GINA) What's New in GINA 2020?Document35 pagesGlobal Initiative For Asthma (GINA) What's New in GINA 2020?Daniela PopNo ratings yet
- 6 - Asthma GuidelinesDocument21 pages6 - Asthma Guidelineshassan mohamedNo ratings yet
- Jurnal Fadhila AsthmaDocument32 pagesJurnal Fadhila AsthmaJannah Miftahul JannahNo ratings yet
- Journal Reading: Asma: Raden Muhamad HidayatDocument28 pagesJournal Reading: Asma: Raden Muhamad HidayatRaden Muhammad HidayatNo ratings yet
- Asthma and COPD 2019 by Tuty Sriwahyuni, M.FarmKlin, AptDocument22 pagesAsthma and COPD 2019 by Tuty Sriwahyuni, M.FarmKlin, AptPuskesmas I SokarajaNo ratings yet
- Kegawatdaruratan Asma Dan PPOKDocument27 pagesKegawatdaruratan Asma Dan PPOKPark JiminNo ratings yet
- Global Initiative For Asthma (GINA) What's New in GINA 2020?Document35 pagesGlobal Initiative For Asthma (GINA) What's New in GINA 2020?Lizangela Utrera100% (1)
- Guideline On Management of Asthma in Adult and ChildrenDocument24 pagesGuideline On Management of Asthma in Adult and ChildrenJerry TanNo ratings yet
- BTS Advice For Healthcare Professionals Treating Patients With AsthmaDocument3 pagesBTS Advice For Healthcare Professionals Treating Patients With AsthmaIzamar RomeroNo ratings yet
- Whats New in GINA 2020Document35 pagesWhats New in GINA 2020Deshielanny AlagumolyNo ratings yet
- GINA Guidelines 2019 SummaryDocument36 pagesGINA Guidelines 2019 Summaryfelly iswaNo ratings yet
- BPOC in Medicina PrimaraDocument3 pagesBPOC in Medicina PrimaraAlina GheNo ratings yet
- Bronchial Asthma: Marshell Tendean, MD Departemen of Internal Medicine UKRIDA - JakartaDocument39 pagesBronchial Asthma: Marshell Tendean, MD Departemen of Internal Medicine UKRIDA - JakartaMel DaNo ratings yet
- Acute CoughDocument5 pagesAcute CoughSundar RamanathanNo ratings yet
- Tataksana Asma 3Document8 pagesTataksana Asma 3yunitriNo ratings yet
- Global Initiative For Asthma (2021) Guidelines: Peter Miranda 3 Year IM ResidentDocument32 pagesGlobal Initiative For Asthma (2021) Guidelines: Peter Miranda 3 Year IM ResidentPeter MirandaNo ratings yet
- Diagnosis and definition of severe refractory asthma consensusDocument9 pagesDiagnosis and definition of severe refractory asthma consensusFlavio GuillenNo ratings yet
- Asthma: For Use of A Registered Medical Practitioner OnlyDocument31 pagesAsthma: For Use of A Registered Medical Practitioner OnlyCCU FellowsNo ratings yet
- Bringing Asthma Care Into The Twenty-First Century: Review ArticleDocument11 pagesBringing Asthma Care Into The Twenty-First Century: Review ArticleliadiafaridaNo ratings yet
- Diagnosis of Asthma, COPD and asthma-COPD Overlap Syndrome (ACOS)Document20 pagesDiagnosis of Asthma, COPD and asthma-COPD Overlap Syndrome (ACOS)Linto JohnNo ratings yet
- Drug Selection Patterns in Asthma and Hyperre Active Airway Disease in ChildrenDocument16 pagesDrug Selection Patterns in Asthma and Hyperre Active Airway Disease in ChildrenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Asthm Seminar 1Document38 pagesAsthm Seminar 1Sol Gat ChupataNo ratings yet
- COPD Case Study Assessment and Care PlanDocument7 pagesCOPD Case Study Assessment and Care PlanMohammad KhalaylahNo ratings yet
- Anesthaesia and Intensive CareDocument139 pagesAnesthaesia and Intensive CareIvan Kurniadi100% (2)
- Asthma Copd OverlapDocument16 pagesAsthma Copd OverlapMaryam BurhanuddinNo ratings yet
- Asthma, COPD and Asthma-COPD Overlap Syndrome (GINA 2014)Document16 pagesAsthma, COPD and Asthma-COPD Overlap Syndrome (GINA 2014)dinh son myNo ratings yet
- Cough: Diagnosis and ManagementDocument5 pagesCough: Diagnosis and Managementkomalasari -No ratings yet
- 01-Obstractihe Pulmonary Diseases (Asthma) PDFDocument50 pages01-Obstractihe Pulmonary Diseases (Asthma) PDFsima.koye2005No ratings yet
- ICU Sepsis Management GuideDocument139 pagesICU Sepsis Management GuideMuhammad Farid100% (1)
- COPD Case Study GuideDocument5 pagesCOPD Case Study GuideMohammad KhalaylahNo ratings yet
- GINA 2014: Dr. Trình Thị NgàDocument34 pagesGINA 2014: Dr. Trình Thị NgàEphy HaningNo ratings yet
- NSAIDs-in-ASthma-2020.v8-final-1Document6 pagesNSAIDs-in-ASthma-2020.v8-final-1suleapikogluNo ratings yet
- Long-Term Azithromycin With Severe CopdDocument8 pagesLong-Term Azithromycin With Severe Copdlaksono_adeNo ratings yet
- Whats New in GINA 2021 FinalDocument47 pagesWhats New in GINA 2021 FinalHeriestian eriesNo ratings yet
- Anesthesia For Adult Patients With Asthma - UpToDateDocument43 pagesAnesthesia For Adult Patients With Asthma - UpToDateKatiaNo ratings yet
- Plenary Discussion Scenario 3Document8 pagesPlenary Discussion Scenario 3RifaiNo ratings yet
- Safety of N Acetylcysteine at High Doses in Chronic Respiratory Diseases: A ReviewDocument18 pagesSafety of N Acetylcysteine at High Doses in Chronic Respiratory Diseases: A Reviewkaroline SernadesNo ratings yet
- Gold and Gina Guideline For Copd and AsthmaDocument56 pagesGold and Gina Guideline For Copd and AsthmaSomnath Das GuptaNo ratings yet
- Managing The Paediatric Patient With An Acute Asthma ExacerbationDocument6 pagesManaging The Paediatric Patient With An Acute Asthma ExacerbationafsajghfdNo ratings yet
- Pediatric Asthma PDFDocument12 pagesPediatric Asthma PDFzie_luph_taz13No ratings yet
- BY Dr. Rajeev Ranjan GuptaDocument66 pagesBY Dr. Rajeev Ranjan Guptarajiv vijarNo ratings yet
- Severe Asthma Phenotypes - UpToDateDocument9 pagesSevere Asthma Phenotypes - UpToDateSilvana ReyesNo ratings yet
- Management of Severe Acute Asthma in The Emergency DepartmentDocument7 pagesManagement of Severe Acute Asthma in The Emergency DepartmentOskar MartinezNo ratings yet
- GINA Pocket2013 May15Document0 pagesGINA Pocket2013 May15David BarzalloNo ratings yet
- Factors Related To Severe Acute Asthma Attack and Treatment: IJPSR (2012), Vol. 3, Issue 08 (Research Article)Document4 pagesFactors Related To Severe Acute Asthma Attack and Treatment: IJPSR (2012), Vol. 3, Issue 08 (Research Article)Tanvir HayderNo ratings yet
- Stable COPD - Initial Pharmacologic Management - UpToDateDocument32 pagesStable COPD - Initial Pharmacologic Management - UpToDateLiz CampoverdeNo ratings yet
- 2000 Journal of The California Dental AssociationDocument20 pages2000 Journal of The California Dental AssociationUnyar LeresatiNo ratings yet
- Emergency Department Management of Acute Asthma ExacerbationsDocument32 pagesEmergency Department Management of Acute Asthma ExacerbationsFercho MedNo ratings yet
- Diskusi Topik 2 (PPOK) - Nafisa Zulpa Elhapidi - 406202067Document59 pagesDiskusi Topik 2 (PPOK) - Nafisa Zulpa Elhapidi - 406202067nafisa zulfaelNo ratings yet
- GINA Strategy 2021pocket GuideDocument16 pagesGINA Strategy 2021pocket GuideHossam HamzaNo ratings yet
- GINA 2016 Main Pocket GuideDocument29 pagesGINA 2016 Main Pocket GuideKaren Ceballos LopezNo ratings yet
- Chronic Cough Evaluation and Treatment GuideDocument13 pagesChronic Cough Evaluation and Treatment GuideRSU DUTA MULYANo ratings yet
- Hamza DissertDocument108 pagesHamza DissertMobin Ur Rehman KhanNo ratings yet
- Micro para OSCE For YL6 BacteriaDocument2 pagesMicro para OSCE For YL6 Bacteriagzldiwa100% (1)
- Sorbion SachetsDocument3 pagesSorbion SachetsReil_InsulaNo ratings yet
- Epidemiology of Sport-Related Spinal Cord Injuries: A Systematic ReviewDocument10 pagesEpidemiology of Sport-Related Spinal Cord Injuries: A Systematic Reviewanna widiaNo ratings yet
- Aap 2009Document538 pagesAap 2009toniassaf100% (1)
- Infections Diseases of The Central Nervous System: Chapter VI - J. RuscalledaDocument11 pagesInfections Diseases of The Central Nervous System: Chapter VI - J. RuscalledaArif BudimanNo ratings yet
- Walaa SNC Network List Mar 2021Document9 pagesWalaa SNC Network List Mar 2021ning yangNo ratings yet
- Introduction to Pathology of the Skeletal SystemDocument69 pagesIntroduction to Pathology of the Skeletal SystemSoleil SierraNo ratings yet
- USMLE Images For The BoardsDocument297 pagesUSMLE Images For The BoardsMulham Etki100% (3)
- Literature Review On PCRDocument6 pagesLiterature Review On PCRafdtzfutn100% (1)
- Jadwal Acara Konas Hiferi 8 UpdateDocument6 pagesJadwal Acara Konas Hiferi 8 Updatedaniel_alexander_susenoNo ratings yet
- Schizophrenia Case StudyDocument14 pagesSchizophrenia Case Studyapi-593859653No ratings yet
- PostsDocument6 pagesPostsQusaiBadrNo ratings yet
- Sdcep Anticoagulants Quick Reference Guide 2nd EditionDocument5 pagesSdcep Anticoagulants Quick Reference Guide 2nd EditionMeryem LahlouNo ratings yet
- WHO GHI Target Global Health ProblemsDocument17 pagesWHO GHI Target Global Health ProblemsKrisha Tañare-MalateNo ratings yet
- Importance of Health Appraisals for StudentsDocument10 pagesImportance of Health Appraisals for StudentsPantz Revibes PastorNo ratings yet
- 001 RCA FlipchartDocument40 pages001 RCA FlipchartAbd ZouhierNo ratings yet
- Viva Content of PsychiatricDocument152 pagesViva Content of PsychiatricMonika Joseph0% (1)
- Pediatrics Clerkship Online Daily Endorsements and PreceptorialsDocument33 pagesPediatrics Clerkship Online Daily Endorsements and PreceptorialsEVER MARY JOY ESCALERANo ratings yet
- Government College Nursing Anemia Nutritional DeficiencyDocument7 pagesGovernment College Nursing Anemia Nutritional Deficiencypriyanka100% (2)
- Pamphlet TemplateDocument2 pagesPamphlet TemplateZoe ColemanNo ratings yet
- Awareness of Mother With Baby PacifierDocument10 pagesAwareness of Mother With Baby PacifierIJAR JOURNALNo ratings yet
- Culture and ObesityDocument6 pagesCulture and ObesityShabi ZeeNo ratings yet
- Nursing Nclex ExamDocument11 pagesNursing Nclex ExamDenisa Viviana MaroNo ratings yet
- Chapter 7 - First Aid-1Document10 pagesChapter 7 - First Aid-1Pikapi PikachuNo ratings yet
- 17 TYPES OF GOOD BACTERIA - The List of Most Beneficial Species of Probiotics Lactobacillus and Bifidobacteria - Ecosh LifeDocument30 pages17 TYPES OF GOOD BACTERIA - The List of Most Beneficial Species of Probiotics Lactobacillus and Bifidobacteria - Ecosh LifeCarl MacCordNo ratings yet
- MRT1202 Course Resources 431Document47 pagesMRT1202 Course Resources 431Haytham AL-FaqihNo ratings yet
- SCREENING FOR DISEASEDocument15 pagesSCREENING FOR DISEASEDr. Radhay ShyamNo ratings yet
- Congenital Cholesteatoma TheoriesDocument14 pagesCongenital Cholesteatoma Theoriesapi-19500641No ratings yet
- A Systematic Review: The Influence of Social Media On Depression, Anxiety and Psychological Distress in AdolescentsDocument6 pagesA Systematic Review: The Influence of Social Media On Depression, Anxiety and Psychological Distress in AdolescentsShivani NeroyNo ratings yet
- Case StudyDocument44 pagesCase StudyPankaj AgrawalNo ratings yet