Professional Documents
Culture Documents
Wernickesencephalopathy 170412164215
Wernickesencephalopathy 170412164215
Uploaded by
Fithry Rahma0 ratings0% found this document useful (0 votes)
5 views22 pagesOriginal Title
wernickesencephalopathy-170412164215
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views22 pagesWernickesencephalopathy 170412164215
Wernickesencephalopathy 170412164215
Uploaded by
Fithry RahmaCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 22
Acute neurological disorder induced by
Thiamine deficiency(Vitamin B1)
More prevalent in males (1.7: 1)
Average onset age is 50 years
(range: 30-70 years)
First described in 1881 by Dr. Carl Wernicke
Rate has been found to be significantly
higher in specific populations, i.e., homeless
people, older people (especially those living
alone or in isolation), and psychiatric
inpatients, where alcohol use and poor
nutritional states predominate.
Prevalence at autopsy exceeds clinical
detection.
Water soluble vitamin absorbed from the gut.
Serves as a cofactor to several enzymes that
are responsible for lipid and carbohydrate
metabolism, production of amino acids and
production of glucose derived
neurotransmitters.
Also have a role in axonal conduction esp. of
acetylcholinergic and serotoninergic
neurons.
Cellular impairment and injury occur within 2-
3 weeks of decreased intake and thiamine
depletion.
Acute thiamine deficiency leads to
mitochondrial dysfunction resulting in
oxidative toxicity in areas of brain.
Chronic alcoholism
Malnutrition or prolonged starvation
Hyperemesis Gravidarum
Bariatric surgery
Gastric malignancy (inflammatory bowel
disease)
Intestinal obstruction (abscess)
Thyrotoxicosis
Iatrogenic (IV glucose without thiamine
supplement or chronic hemodialysis)
Systemic diseases (AIDS, disseminated TB)
Thiamine deficient formula/ breastfeeding by
mothers with inadequate thiamine intake
Infection( precipitating factor)- pneumonia,
meningitis
Clinical Triad - ocular abnormalities (29%)
- encephalopathy (82%)
- ataxia (23%)
Occurs in 1/3 of cases.
Hallmark of WE
Nystagmus, bilateral rectal
palsies and conjugate gaze
palsies (involvement of
oculomotor, abducens and
vestibular nuclei)
Less common manifestations
are pupillary abnormalities,
ptosis, sctomata and
anisocoria
Global confusion state, disinterest,
inattentiveness or agitation.
Most common presentation is mental state
changes.
Stupor and coma observed in severe cases
Due to polyneuropathy, cerebellar damage
and vestibular paresis.
Wide based stance
Slow and uncertain short stepped gait.
Inability to walk without support in severe
cases.
Peripheral neuropathy (weakness, foot drop
& decreased proprioception)
GI symptoms (nausea, vomiting, lactic
acidosis)
Hypotension
Hypothermia
Memory disturbances
Acute symmetrical lesions in thalamus,
mamillary bodies, tectal plate,
periaqueductal area, floor of 4th ventricle
(includes oculomotor and vestibular nuclei
and cerebellar vermis)
Lesions are in form of vascular congestion,
microglial proliferation and petechial
hemorrhages.
Chronic complication of WE
Occurs in 2/3 of patients with untreated WE
Only 25% of patients fully recover.
Lesions are similar to WE expect they are
not hemorrhagic.
Results in cerebellar atrophy (irreversible
change).
Characteristics:
Anterograde amnesia (inability to form new
memories)
Retrograde amnesia ( inability to recall past
events)
Confabulations
Detailed patient history
Physical and neurological examination
Laboratory evaluation
CBC (rule out infections, severe anemia)
Serum thiamine levels
Erythrocyte transketolase levels
Serum glucose levels
Toxic drug screening
Lumbar puncture (rule out CNS infections)
Imaging
MRI (fluid attenuated inversion recovery
{FLAIR} images)
CT ( not specific)
EEG ( rule out non- convulsive status
epilepticus)
Hepatic encephalopathy
Hypoglycemia
Anorexia nervosa
Alcohol related psychosis
Withdrawal syndromes
Delirium tremens
Considered a medical emergency
Emergency care : Parenteral Thiamine (multiple
daily doses – 500mg/dose)
Alcohol withdrawal
In case of WKS, use of oral Thiamine to prevent
further complications.
Parenteral magnesium sulfate in case of
hypomagnesaemia
Balanced diet with high thiamine containing
foods.
THANK YOU..
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NarcanDocument1 pageNarcanKatie McPeekNo ratings yet
- Oral Medication Doses: Asha Russel Asst. Science Tutor A'Document45 pagesOral Medication Doses: Asha Russel Asst. Science Tutor A'AshaNo ratings yet
- Barangay Annual Gad Plan and Budget SampleDocument22 pagesBarangay Annual Gad Plan and Budget SampleAnaliza LabsangNo ratings yet
- Targeted Public Distribution SystemDocument20 pagesTargeted Public Distribution SystemTanushka shuklaNo ratings yet
- Right of HumanDocument39 pagesRight of HumanjeyasinghNo ratings yet
- CV Bu VonyDocument4 pagesCV Bu Vonydwi jayantiNo ratings yet
- Diagnostic Product Guide-MDIDocument24 pagesDiagnostic Product Guide-MDIAnh NguyenNo ratings yet
- WHO - Traditional Medicine - Growing Needs & PotentialDocument6 pagesWHO - Traditional Medicine - Growing Needs & PotentialDonny LoNo ratings yet
- CARBON AmAir C AmAir CSAAFOxi AmAir SAAFOxi AmAir CP GPF1118Document4 pagesCARBON AmAir C AmAir CSAAFOxi AmAir SAAFOxi AmAir CP GPF1118FRAJCO9248No ratings yet
- Ramos V CA (MR)Document41 pagesRamos V CA (MR)nobocNo ratings yet
- 10 1016@j Accpm 2019 10 019Document6 pages10 1016@j Accpm 2019 10 019Sri NingsihNo ratings yet
- The Pathophysiology of Sepsis - 2021 Update - Part 2, Organ Dysfunction and AssessmentDocument13 pagesThe Pathophysiology of Sepsis - 2021 Update - Part 2, Organ Dysfunction and AssessmentValerie ZimmermannNo ratings yet
- Mcmillan Sample Print Out1Document3 pagesMcmillan Sample Print Out1CrizarNo ratings yet
- Umbilical Cord ProlapseDocument5 pagesUmbilical Cord Prolapseangga hergaNo ratings yet
- V2 N2 JITED P03 - Uma Devi T - Stress ManagementDocument19 pagesV2 N2 JITED P03 - Uma Devi T - Stress ManagementDev UdiataNo ratings yet
- Information Technology (IT) and The Healthcare Industry: A SWOT AnalysisDocument19 pagesInformation Technology (IT) and The Healthcare Industry: A SWOT AnalysisTuan PhanNo ratings yet
- Iso 14001:1996Document22 pagesIso 14001:1996Adhi SyukriNo ratings yet
- Training Report GaganDocument18 pagesTraining Report GaganYaman VermaNo ratings yet
- Fix A Nator A Fixed Bionator Technique ArticleDocument6 pagesFix A Nator A Fixed Bionator Technique ArticleOrtho OrganizersNo ratings yet
- St. Paul University Philippines: Tuguegarao City, Cagayan 3500Document35 pagesSt. Paul University Philippines: Tuguegarao City, Cagayan 3500Hazel FlorentinoNo ratings yet
- Material Safety Data Sheet: Remove DebonderDocument4 pagesMaterial Safety Data Sheet: Remove DebonderSales OnlineNo ratings yet
- Unit 1: Leisure ActivitiesDocument4 pagesUnit 1: Leisure ActivitiesThao Nguyen ThuNo ratings yet
- Sally Rogers Dinner Conference: Clinical and Developmental Aspects of AutismDocument1 pageSally Rogers Dinner Conference: Clinical and Developmental Aspects of Autismaaspen3190No ratings yet
- Fotona Dynamis Brochure Fotona 2 WebDocument21 pagesFotona Dynamis Brochure Fotona 2 WebAferNo ratings yet
- Skeletal and Muscular SystemDocument118 pagesSkeletal and Muscular SystemMark Kevin AguilarNo ratings yet
- Woman Centred Care: A Concept AnalysisDocument37 pagesWoman Centred Care: A Concept AnalysisArdin MunrekNo ratings yet
- Animal Research - Reporting in Vivo Experiments - The ARRIVE GuidelinesDocument3 pagesAnimal Research - Reporting in Vivo Experiments - The ARRIVE GuidelinesFellicia RachmadianaNo ratings yet
- Takashima 2016Document15 pagesTakashima 2016Fatih HarisNo ratings yet
- Pangestuti, Arifin - 2018 - Medicinal and Health Benefit Effects of Functional Sea CucumbersDocument11 pagesPangestuti, Arifin - 2018 - Medicinal and Health Benefit Effects of Functional Sea CucumbersGREESTYNo ratings yet
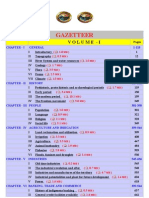
- Puducherry Gazetteer ContentsDocument9 pagesPuducherry Gazetteer Contentsvillipdy0% (1)