Professional Documents
Culture Documents
Significance of Extreme Leukocytosis in Evaluation of Febrile Children Aged 3-36 Months: A Single Center Experience
Uploaded by
silpayOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Significance of Extreme Leukocytosis in Evaluation of Febrile Children Aged 3-36 Months: A Single Center Experience
Uploaded by
silpayCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/312304062
Significance of extreme leukocytosis in evaluation of febrile children aged 3-36
months: A single center experience
Article in Iraqi Journal of Hematology · January 2016
DOI: 10.4103/2072-8069.198121
CITATIONS READS
3 1,177
3 authors, including:
Rabab Baaker Nabeeha N. Akram
Al-Mustansiriya University Al-Mustansiriya University
3 PUBLICATIONS 3 CITATIONS 4 PUBLICATIONS 3 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Knowledge of medical students on diagnosis and management of diabetes mellitus View project
characteristics and outcome of children hospitalized with COVID-19 in child’scentral teaching hospital : A single center experience. View project
All content following this page was uploaded by Nabeeha N. Akram on 17 May 2021.
The user has requested enhancement of the downloaded file.
[Downloaded free from http://www.ijhonline.org on Monday, May 17, 2021, IP: 185.51.223.113]
Original Article
Access this article online
Quick Response Code:
Significance of extreme leukocytosis
in evaluation of febrile children
aged 3–36 months: A single center
experience
Website:
www.ijhonline.org Sadek H. Ghani, Rabab H. Baaker1, Nabeeha N. Akram
DOI:
10.4103/2072-8069.198121
Abstract:
BACKGROUND: Emergency department evaluation of young febrile children often includes measurement of
white blood cell (WBC) count. Although a high WBC count is associated with an increased likelihood of infection,
the clinical significance of extreme leukocytosis (EL) (a WBC count of ≥25,000/mm3), has not been well studied.
OBJECTIVE: The aim of this study is to study the correlation between the level of WBC and the cause of fever
in febrile children and to assess if WBC level helpful in predicting the seriousness of febrile illness.
PATIENTS AND METHODS: A cross‑sectional case series study conducted over 5 months from August 01 to
December 31, 2015, in the emergency department at child central teaching hospital in Baghdad city in Iraq. The
study was evaluating children aged 3–36 months admitted to the emergency department for fever. WBC count
was done either manually or a complete blood count by automated hematologic analyzer.
RESULTS: Of those 129 febrile children were enrolled in this study, 42 patients with EL were identified and
compared with 87 patients with moderate leukocytosis (ML). Pneumonia was the only diagnosis found to be
significantly higher in EL group 17 cases (40.5%) versus 15 cases (17.2%) in ML group with P value (0.004).
Meningitis was higher in patient with ML with P value (0.03). Finally, EL was associated with higher rates of
admission to hospital (P < 0.036).
CONCLUSIONS: The presence of EL indicates a higher risk of having pneumonia. The degree of
leukocytosis (extreme or moderate) does not affect the rates of serious bacterial infection.
Key words:
Children, leukocytosis, significance
A cute febrile illness in an infant or a young
child is a common clinical scenario that
can be a diagnostic challenge. The evaluation is
37.5 and 38.3°C (99.5 and 100.9°F).[4] Fever is
generally agreed to be present if the elevated
temperature is caused by a raised set point:
guided by the history and physical examination, • Temperature in the anus (rectum/rectal) is
along with judiciously selected screening tests. at or over 37.5–38.3°C (99.5–100.9°F)[4]
The overwhelming majority of nontoxic, but • Temperature in the mouth (oral) is at or
febrile infants and young children have a viral over 37.7°C (99.9°F)[5]
Department of infection. The physician’s primary task is to • Temperature under the arm (axillary) or in
Neonatology, Childs identify the infant or child who is at risk for the ear is at or over 37.2°C (99.0°F).[6]
Central Teaching serious bacterial infection (SBI).[1] The occurrence
Hospital, 1Department of fever is one of the most common reasons for A fever can be caused by many medical
of pediatrics, children seeking medical attention, both in the conditions ranging from simple to potentially
Almustansiriya community and in the pediatric emergency serious one. This includes viral, bacterial, and
University College of unit.[2] Fever is defined as having a temperature parasitic infections such as the common cold,
Medicine, Baghdad, Iraq above the normal range due to an increase in urinary tract infection (UTI), and meningitis
the body’s temperature set‑point.[3] There is no among others. Noninfectious causes include
Address for single agreement on the upper limit for normal vasculitis, side effects of medication, and cancer
correspondence: temperature with sources using values between among others.[3] Viral infection is the cause of
Dr. Sadek H. Ghani,
Child’s Central Teaching This is an open access article distributed under the terms of the
Hospital, Baghdad, Iraq. Creative Commons Attribution‑NonCommercial‑ShareAlike 3.0 How to cite this article: Ghani SH, Baaker RH,
E‑mail: alsaadidoctor@ License, which allows others to remix, tweak, and build upon the Akram NN. Significance of extreme leukocytosis
yahoo.com work non‑commercially, as long as the author is credited and the in evaluation of febrile children aged 3-36 months:
new creations are licensed under the identical terms.
A single center experience. Iraqi J Hematol
Submission: 09‑10‑2016 2016;5:167-72.
Accepted: 08‑11‑2016 For reprints contact: reprints@medknow.com
© 2016 Iraqi Journal of Hematology | Published by Wolters Kluwer - Medknow 167
[Downloaded free from http://www.ijhonline.org on Monday, May 17, 2021, IP: 185.51.223.113]
Ghani, et al.: Significance of extreme leukocytosis in febrile children
fever in most infants and young children. Clinical appearance Patients with extreme leukocytosis (EL) have an increased risk
rather than the height of fever is a more powerful predictor of of bacteremia, the risk of bacteremia increases from 0.5% for
serious illness.[7,8] Differentiating young children with SBI from WBC counts <15,000 per mm3 (15 × 109/L) to >18% for WBC
those with self‑limited viral illnesses has been quite difficult,[9] counts over 30,000 per mm3 (30 × 109/L).[23]
SBI include meningitis, sepsis, bone and joint infections, UTIs,
pneumonia, enteritis.[10] In moderate and EL, the majority of cells are neutrophils.[24,25]
Neutrophilia may be caused by increased release from marrow
Approximately, 10% of well‑appearing young infants with stores, increased production, extended survival or demargination
a temperature higher than 38°C (100.4°F) harbor a serious within the blood vessels. It is considered a nonspecific measure of
bacterial infection or meningitis.[11‑13] In contrast, fewer than inflammation, being associated with bacterial and fungal infection
2% of well‑appearing older infants and young children with a and with almost any medical condition that causes stress. Some
temperature higher than 39°C (102.2°F) manifest bacteremia, medications including steroids, beta agonists, and lithium may
with widespread immunization against Haemophilus influenzae elevate the neutrophil count.[26] Neutrophilia alone or with an
infection, Streptococcus pneumoniae has become the predominant increased band count had variable sensitivity and specificity in
cause of SBI in infants and young children. Streptococcal numerous studies as a possible predictor of bacteremia in young
bacteremia affects fewer than 2% of well‑appearing older children with fever; there is a significantly positive correlation
infants and young children with a temperature above 39°C.[14] between the frequency of blood cultures positive for Streptococcus
Most children in this age group clear streptococcal bacteremia pneumoniae and the WBC and absolute neutrophil counts.[23]
without antibiotic therapy.[1]
The aims of this study were to study the correlation between
Approximately, 10% of infants and young children with the level of WBC and the etiology of fever in febrile child and
fever and S. pneumoniae bacteremia progress to an SBI, and to assess if WBC level helpful in predicting the seriousness of
from 3% to 6% progress to meningitis (i.e., approximately febrile illness.
one case per 1000–2500 of these febrile children. [15,16]
Approximately, 30% of febrile children 3 months to 3 years Patients and Methods
of age have no localizing signs of infection. Risk factors
indicating increased probability of occult bacteremia A cross‑sectional case series study conducted over 5 months
include temperature >39°C, white blood cell (WBC) count from August 01 to December 31, 2015, in the emergency
>15,000/mm3, or an elevated absolute neutrophil count, department at child central teaching hospital in Baghdad city
band count, erythrocyte sedimentation rate, or C‑reactive in Iraq. One hundred and twenty‑nine febrile children (axillary
protein. The incidence of bacteremia among infants temperature 38°C or more) aged 3–36 months admitted to the
3–36 months of age increases as the temperature and WBC emergency department were included in the study regardless
count increase. Socioeconomic status, race, gender, and age of the associated signs and symptoms. Children with a known
(within the range of 3–36 months) do not appear to affect underlying chronic illness (e.g., malignancy, sickle cell anemia,
the risk for occult bacteremia.[17] immunodeficiency, cystic fibrosis, asthma) were excluded from
the study also children who recently received a drug known to
Leukocytosis is increase in the number of circulating WBCs cause leukocytosis (e.g., steroid) also were excluded.
above the normal range. Leukocytosis is defined as WBCs count
>11,000 per mm3, is frequently found in the course of routine Detailed history and complete physical examination was done
laboratory testing.[18] Reference ranges for leukocyte counts in for all children enrolled in the study to find out the cause of
children and adults are shown in Table 1.[19] fever. Temperature was taken by electronic thermometer in
the axilla. All patients were sent for WBC count either manual
Types of leukocytosis: There are five principal types of or complete blood count (CBC) by automated hematologic
leukocytosis.[20] analyzer (RUBY®).
• Neutrophilia
• Lymphocytosis According to WBC count results, patients were divided
• Monocytosis into two groups: 42 patients who found to have WBC count
• Eosinophilia ≥25.000/mm3 defined as EL, whereas 87 patients who have
• Basophilia. had WBC count 15.000–24.999/mm3 considered as moderate
leukocytosis (ML).
Extreme leukocytosis
It is defined as a peripheral WBC count ≥25,000/mm3. A higher Chest X‑ray (CXR), blood culture and sensitivity (C/S), general
WBC count has been associated with an increased likelihood urine examination was obtained in all patients, whereas urine
of infection in studies that have focused on well‑appearing C/S were done by bladder catheterization only in those who
children at risk for occult bacteremia.[21] found to have ≥5WBC in urinalysis and lumber puncture was
done for those who was suspected to have central nervous
The leukemoid reaction is an extremely high white cell system infection based on history and/or clinical examination.
count resembling leukemia. Previous authors have used The final diagnosis and treatment plan with the need for
the terms “leukemoid reaction” and “extreme granulocytic admission was recorded for all patients.
leukocytosis,” variously implying a leukocytosis in excess
of 25–50 × 109/L in the absence of known hematological Patients considered having SBI if the child found to have
disease.[22] one of the following (meningitis, osteomyelitis, bacteremia,
168 Iraqi Journal of Hematology - Vol 5, Issue 2, Jul-Dec 2016
[Downloaded free from http://www.ijhonline.org on Monday, May 17, 2021, IP: 185.51.223.113]
Ghani, et al.: Significance of extreme leukocytosis in febrile children
Table 1: Reference ranges for leukocyte counts in children and adults
Age Total leukocytes Neutrophils Lymphocytes Monocytes Eosinophil
Mean Range Mean Range Percentage Mean Range Percentage Mean Percentage Mean Percentage
Birth 18.1 9.0300 11.0 6.0260 61 5.5 2.0110 31 1.1 6 0.4 2
12 h 22.8 13.030 15.5 6.0280 68 5.5 2.0110 24 1.2 5 0.5 2
24 h 18.9 9.4340 11.5 5.0210 61 5.8 2.0115 31 1.1 6 0.5 2
1 week 12.2 5.0210 5.5 1.5100 45 5.0 2.0170 41 1.1 9 0.5 4
2 weeks 11.4 5.0200 4.5 1.09.5 40 5.5 2.0170 48 1.0 9 0.4 3
1 month 10.8 5.0195 3.8 1.09.0 35 6.0 2.5165 56 0.7 7 0.3 3
6 months 11.9 6.0175 3.8 1.08.5 32 7.3 4.0135 61 0.6 5 0.3 3
1 year 11.4 6.0175 3.5 1.58.5 31 7.0 4.0105 61 0.6 5 0.3 3
2 years 10.6 6.0170 3.5 1.58.5 33 6.3 3.09.5 59 0.5 5 0.3 3
4 years 9.1 5.5155 3.8 1.58.5 42 4.5 2.08.0 50 0.5 5 0.3 3
6 years 8.5 5.0145 4.3 1.58.0 51 3.5 1.57.0 42 0.4 5 0.2 3
8 years 8.3 4.5135 4.4 1.58.0 53 3.3 1.56.8 39 0.4 4 0.2 2
10 years 8.1 4.5135 4.4 1.88.0 54 3.1 1.56.5 38 0.4 4 0.2 2
16 years 7.8 4.5130 4.4 1.88.0 57 2.8 1.25.2 35 0.4 5 0.2 3
21 years 7.4 4.5110 4.4 1.87.7 59 2.5 1.04.8 34 0.3 4 0.2 3
UTIs, pneumonia, and cellulitis). Hence, in this study, Proven 40
SBI was defined as the presence of positive culture (blood,
cerebral spinal fluid [CSF], urine) obtained from the patients 39.5
at emergency department diagnosed as cases of (bacteremia,
bacterial meningitis, UTI), respectively.
Temperature (C° )
39
38.93
38.74
We created the category of probable SBI to include those
infections that were probably bacterial in origin and 38.5
treated as such although not proven by culture. This
category included pneumonia (considered bacterial in origin 38
when CXR shows alveolar infiltrations particularly lobar
consolidation identified by pediatric radiologist and CBC shows 37.5
neutrophilia), cellulitis (diagnosed clinically by the presence
of redness, tenderness, swelling), osteomyelitis (diagnosed 37
by magnetic resonance imaging), meningitis with negative Extreme Leukocytosis (n=42) Moderate Leukocytosis (n=87)
CSF culture (neutrophilic pleocytosis and low glucose level WBC count
in CSF analysis).
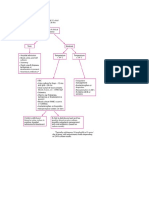
Figure 1: Comparison of the degree of temperatures at time of admission between
Statistical analysis patients with extreme and moderate leukocytosis
Each patient assigned a serial identification number. The data
were reviewed and analyzed using Statistical Package for Social versus (54%) in ML group, whereas female percentage in EL
Sciences version 20 (IBM Corp. Armonk, NY, USA). Categorical was (40.5%) versus (46%) in ML group. The male to female
data represented by frequency and percentages. The Chi‑square ratio was 1:1.47 in EL group and 1:1.17 in ML group. The
test was used to assess the association between the categorical distribution of the patients according to their age and gender
data. The Shapiro–Walk test was used to test data distribution. in this study were statistically not significant between patient
The continuous variables were presented as mean, standard with EL and those with ML with P values (>0.5) for both as
deviation, median, and range accordingly. shown in Table 2.
Results CXR was positive for pneumonia in 17 (40.5%) in EL group VS
15 (17.2%) in ML group so it was statistically significant in
A total of 129 children aged 3–36 months with fever and EL with (P = 0.004). In addition, Blood C/S was positive in
leukocytosis (WBC >14,999 mm3) were identified, 42 patients 6 (15.4%) in EL group versus 9 (10.5%) in ML group found
with EL were compared to 87 patients with ML. The mean to be statistically not significant with (P = 0.4) as shown in
body temperature of the patients at the time of admission to the Table 3.
emergency department was (38.9 ± 0.6) in EL versus (38.7 ± 0.7)
in ML P value (0.1); it was not significantly different in the two Urine culture done in 113 patients (39 in EL and 74 in ML),
groups as shown in Figure 1. urine C/S were positive in 5 (12.8%) in EL versus 15 (20.3%)
in ML so was not significant with (P = 0.3) as noted in Table 3.
The mean age and standard deviation for case group
were (13.07 ± 10.55), whereas it was (12.11 ± 8.55) for Cerebrospinal fluid analysis and culture obtained in
control group. Male percentage in EL group was (59.5%) 83 patients (26 in EL vs. 57 in ML). It was positive in 8 (30.8%)
Iraqi Journal of Hematology - Vol 5, Issue 2, Jul-Dec 2016 169
[Downloaded free from http://www.ijhonline.org on Monday, May 17, 2021, IP: 185.51.223.113]
Ghani, et al.: Significance of extreme leukocytosis in febrile children
in EL vs. 33 (57.9%) in ML which was significant in ML group From 129 cases included in this study, only one case died
with (P = 0.022). There was no difference between both groups during hospitalization in EL group and no death was recorded
in frequency with which these studies were performed as in patients with ML.
shown in Table 3. Pneumonia was the only diagnosis found
to be significantly higher in EL group 17 cases (40.5%) versus Discussion
15 cases (17.2%) in ML group with P value (0.004). Meningitis
was more common in ML 33 (37.9%) than EL 8 (19%) with In evaluating febrile children aged 3–36 months many
P value of (0.03). No significant difference was found among physicians use WBC counts for screening febrile children
both groups in regard to frequencies of other diagnoses (P value to check for underlying bacterial infection. An increased
for all >0.05) as noted in Table 4. WBC count in a well‑appearing febrile child between 3 and
36 months of age is associated with an increased risk of occult
In this study, SBI (proven and probable) found in 36 (85.7%) bacteremia.[27]
in EL group versus 68 (87.1%) in ML group with (P = 0.3), the
most common SBI in the EL patient was pneumonia (47.2%) In this study, there was no statistically significant difference
as shown in Figure 2. between patients with EL and those with ML regarding degree
of fever and gender with P value (0.1) and (0.5), respectively,
Hospitalization was significantly greater in EL than patients this result was similar to study by Shah et al.[21] The current
with ML 83.3% versus 65.5% with (P = 0.036) as shown in study shows that there are no differences in the frequency
Table 5. of diagnoses between a patient with moderate or EL groups
with exception of pneumonia and meningitis. Pneumonia
was significantly higher in EL17 (40.5%) versus 15 (17.2%) in
ML group with P value (0.004). Meningitis was higher in ML
33 (37.9%) than those with EL 8 (19%) with P value (0.03), while
Shah et al.[21] found that all diagnoses were not significantly
different between EL and ML groups finding could be explain
by short study time in the current study while Shah et al. study
performed over 3 years although both studies carried out at
similar settings (emergency department of an urban tertiary
hospital).
Pneumonia was the most prevalent diagnosis in patient with
EL (40.5%) this is similar to result found by Bachur et al.[28] and
Lawrence et al.[22] with percentages (28% and 30%), respectively.
While Shah et al. found that pneumonia account for only (13%)
of patient with EL. This finding suggests that child 3–36 m
Figure 2: Comparison of percentage of different types of serious bacterial infection with fever and with EL should be evaluated thoroughly and
in patients with extreme versus moderate leukocytosis (P = 0.306 [significant at
0.05 level])
CXR should be considered to exclude pneumonia similar
recommendation made by Bachur et al. and also to that given
by the UK’s national institute for health and clinical on fever
Table 2: The distribution of patients according to their in children ≤5 years.[29] In our study, Otitis media found in
age and gender only (4.8%) of patient with EL while Shah et al. found that
Variables Leukocytosis P otitis media was the most common diagnosis in patient with
EL (n=42) ML (n=87) EL (40.7%), this could be attributed to the fact that cases of
Age (months), median±SD 13.07±10.55 12.11±8.55 0.5a otitis media in our hospital usually not admitted to emergency
Gender (%) department (the place where our study conducted) unless
Male 25 (59.5) 47 (54) 0.5b patient had complication and/or unable to take oral treatment.
Female 17 (40.5) 40 (46)
Male to female ratio 1:1.47 1:1.17 The risk of bacteremia in febrile children increase as WBC count
a
Student’s t‑test, bChi‑square test, *Significant at 0.05 levels. ML = Moderate increase,[1] Lee and Harper found that the risk of bacteremia
leukocytosis, EL = Extreme leukocytosis, SD = Standard deviation increases from (0.5%) for WBC <15,000 mm 3 to greater
Table 3: Laboratory test performed in patient with extreme leukocytosis and moderate leukocytosis groups
Laboratory tests Leukocytosis P
EL (n=42) ML (n=87)
Done in n (%) Positive result, n (%) Done in n (%) Positive result, n (%)
Blood culture 42 (100) 6 (15.4) 87 (100) 9 (10.5) 0.4
CXR 42 (100) 20 (47.6) 87 (100) 16 (18.4) 0.001*
Urine culture 39 (92.8) 5 (12.8) 74 (94.8) 15 (20.3) 0.3
CSF analysis and culture 26 (61.9) 8 (30.8) 57 (65.5) 33 (57.9) 0.022*
*Significant at 0.05 levels. ML = Moderate leukocytosis, EL = Extreme leukocytosis, CXR = Chest X‑ray, CSF = Cerebral spinal fluid
170 Iraqi Journal of Hematology - Vol 5, Issue 2, Jul-Dec 2016
[Downloaded free from http://www.ijhonline.org on Monday, May 17, 2021, IP: 185.51.223.113]
Ghani, et al.: Significance of extreme leukocytosis in febrile children
Table 4: Number and percentage of cases, according Conclusions
to leukocytosis and final diagnosis
Final Number of leukocytosis P In febrile children aged 3–36 months, the presence of EL
diagnosis Extreme Moderate indicates a higher risk of having pneumonia. Otherwise, it is
variable (n=42), n (%) (n=87), n (%) not helpful alone in finding out the cause of fever. The degree
Pneumonia 17 (40.5) 15 (17.2) 0.004* of leukocytosis (extreme or moderate) does not affect the rates
Meningitis 8 (19) 33 (37.9) 0.03* of SBI. EL is good indicator for need for hospital admission
UTI 4 (9.5) 12 (13.8) 0.4 rather than outpatient management.
Otitis media 2 (4.8) 5 (5.7) 0.8
Osteomyelitis 1 (2.4) 2 (2.3) 0.9
Financial support and sponsorship
Nil.
Pertussis 3 (7.1) 7 (8) 0.8
Cellulitis 1 (2.4) 1 (1.1) 0.5
Conflicts of interest
Bacteremia 5 (11.9) 5 (5.7) 0.2
There are no conflicts of interest.
Others 1 (2.4) 7 (8) 0.2
*Significant at 0.05 levels. Other includes 1 kalazar and 7 cases of amoebic
dysentery. UTI = Urinary tract infection References
1. Luszczak M. Evaluation and management of infants and young
Table 5: Admission rates among patients with extreme children with fever. Am Fam Physician 2001;64:1219‑26.
and moderate leukocytosis 2. Nelson DS, Walsh K, Fleisher GR. Spectrum and frequency of
Management plan EL (n=42), n (%) ML (n=87), n (%) P pediatric illness presenting to a general community hospital
Inpatient 35 (83.3) 57 (65.5) 0.036* emergency department. Pediatrics 1992;90(1 Pt 1):5‑10.
Outpatient 7 (16.7) 30 (34.5) 3. Tamas RP, Gus MG. Fever in adults. In: Garmel Gus M, editor.
*Significant at 0.05 levels. ML = Moderate leukocytosis, EL = Extreme leukocytosis An Introduction to Clinical Emergency Medicine. 2nd ed. United
Kingdom: Cambridge University Press; 2012. p. 5‑375.
4. Axelrod YK, Diringer MN. Temperature management in acute
than (18%) for WBC more than 30,000/mm3.[23] In our study, neurologic disorders. Neurol Clin 2008;26:585‑603, xi.
(15.4%) of a patient with EL had bacteremia, however, the risk
5. Barone JE. Fever: Fact and fiction. J Trauma 2009;67:406‑9.
of bacteremia was not statistically significant from those with
6. Barton DS. Fever in childhood. Pediatrics 1984;74:929.
ML which is similar to that found by Shah et al.
7. Trautner BW, Caviness AC, Gerlacher GR, Demmler G,
Macias CG. Prospective evaluation of the risk of serious bacterial
In our study, the overall rate of SBI in patient with EL infection in children who present to the emergency department
was (85.7%) This percentage is much higher than results with hyperpyrexia (temperature of 106 degrees F or higher).
found by Brauner et al. (39%)[30] and Mazur et al. (18%),[31] Shah Pediatrics 2006;118:34‑40.
et al. (25%) for proven SBI and (52%) for combined proven and 8. Press S. Association of hyperpyrexia with serious disease in
probable SBI, Danino et al.[32] (39%). This could be explained by children. Clin Pediatr (Phila) 1994;33:19‑25.
a probable over diagnosis of SBI in our study as a result of lack 9. Belfer RA, Gittelman MA, Muñiz AE. Management of febrile
of some confirmatory tests like lack of colony count in urine infants and children by pediatric emergency medicine and
culture results in considering any case with the growth of any emergency medicine: Comparison with practice guidelines.
pathogenic bacteria in urine culture as UTI and treated as such. Pediatr Emerg Care 2001;17:83‑7.
10. Baraff LJ, Bass JW, Fleisher GR, Klein JO, McCracken GH,
Powell JK. Practice guideline for the management of infants
The risk of SBI in EL group was not significantly higher than
and children 0 to 36 months of age with fever without source.
that in a patient with ML (P = 0.309), a result similar to that Pediatrics 1993;92:1‑12.
found by Shah et al. but different to what found by Brauner
11. Chiu CH, Lin TY, Bullard MJ. Identification of febrile neonates
et al. and Mazur et al. unlikely to have bacterial infections. Pediatr Infect Dis J 1997;16:59‑63.
12. Baskin MN. The prevalence of serious bacterial infections by age
Mazur et al. found that the risk of proven SBI was higher in in febrile infants during the first 3 months of life. Pediatr Ann
children with EL compared with those with ML. The incidence 1993;22:462‑6.
of proven SBI from the Mazur et al. study was even higher 13. Jaskiewicz JA, McCarthy CA, Richardson AC, White KC,
with a WBC count of ≥35,000/mm3 as the cutoff value. Shah Fisher DJ, Dagan R, et al. Febrile infants at low risk for serious
et al. found that the overall rate of proven SBI was comparable bacterial infection – An appraisal of the Rochester criteria and
with that found by Mazur et al. but the incidence of proven implications for management. Febrile Infant Collaborative Study
and combined proven or probable SBI in children with EL, did Group. Pediatrics 1994;94:390‑6.
not differ from the incidence in children with ML. The rates 14. Alpern ER, Alessandrini EA, Bell LM, Shaw KN, McGowan KL.
of proven SBI were similar between EL (25%) and ML (17%) Occult bacteremia from a pediatric emergency department:
Current prevalence, time to detection, and outcome. Pediatrics
patients. Differences in the combined rates of proven or
2000;106:505‑11.
probable SBI between the EL (52%) and ML (35%) patients were
15. Rothrock SG, Harper MB, Green SM, Clark MC, Bachur R,
not statistically significant. The most common SBI in patient McIlmail DP, et al. Do oral antibiotics prevent meningitis and
with EL in our study was pneumonia which agrees with what serious bacterial infections in children with Streptococcus
found by Danino et al. and Shah et al. The need for hospital pneumoniae occult bacteremia? A meta‑analysis. Pediatrics
admission was significantly higher in patient with EL (83.3%) 1997;99:438‑44.
similar to that found by Shah et al. and to Lawrence et al. (49%, 16. Baraff LJ, Oslund S, Prather M. Effect of antibiotic therapy and
100%) respectively. etiologic microorganism on the risk of bacterial meningitis in
Iraqi Journal of Hematology - Vol 5, Issue 2, Jul-Dec 2016 171
[Downloaded free from http://www.ijhonline.org on Monday, May 17, 2021, IP: 185.51.223.113]
Ghani, et al.: Significance of extreme leukocytosis in febrile children
children with occult bacteremia. Pediatrics 1993;92:140‑3. Diagnosis and outcome of 100 consecutive patients with extreme
17. Nield LS, Kamat D, Fever without focus .In: Kliegman RM, granulocytic leukocytosis. Am J Med 1998;104:12‑6.
Stanton BF, St. Geme III JW, Schor NF eds. Nelson textbook of 26. Holland SM, Gallin JI. Disorders of granulocytes and monocytes.
pediatrics, 20th ed. Canada. Elsevier 2016:1280-82. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL,
18. Shapiro MF, Greenfield S. The complete blood count and leukocyte Jameson JL, editors. Harrison’s Principles of Internal Medicine.
differential count. An approach to their rational application. Ann 16 th ed. New York: McGraw-Hill Medical Publishing;2004.
Intern Med 1987;106:65‑74. p. 349‑57.
19. Curnutte JT, Coates TD. Disorders of phagocytic function and 27. Jamuna R, Srinivasan S, Harish BN. Factors predicting occult
number. In: Hoffman Hematology: Basic Principles and Practice. bacteremia in young children. Indian J Pediatr 2000;67:709‑11.
3rd ed. St. Louis, MO: Elsevier Churchill Livingstone; 2000. 28. Bachur R, Perry H, Harper MB. Occult pneumonias: Empiric chest
p. 721‑2520. radiographs in febrile children with leukocytosis. Ann Emerg Med
20. Zorc JJ. Leukocytosis. In: Schwartzs Clinical Handbook of 1999;33:166‑73.
Pediatrics. 4th ed. Philadelphia: Wolters Kluwer, Lippincott 29. National Collaborating Center for Women’s and Children’s
Williams and Wilkins; 2009. p. 559. Health. Feverish Illness in Children: Assessment and Initial
21. Shah SS, Shofer FS, Seidel JS, Baren JM. Significance of extreme Management in Children Younger Than 5 Years. Clinical
leukocytosis in the evaluation of febrile children. Pediatr Infect Guideline No. 47. London: National Institute for Health and
Dis J 2005;24:627‑30. Clinical Excellence; 2007. p. 142.
22. Lawrence YR, Raveh D, Rudensky B, Munter G. Extreme 30. Brauner M, Goldman M, Kozer E. Extreme leucocytosis and the
leukocytosis in the emergency department. QJM risk of serious bacterial infections in febrile children. Arch Dis
2007;100:217‑23. Child 2010;95:209‑12.
23. Lee GM, Harper MB. Risk of bacteremia for febrile young children 31. Mazur LJ, Kline MW, Lorin MI. Extreme leukocytosis in patients
in the post‑Haemophilus influenzae type b era. Arch Pediatr presenting to a pediatric emergency department. Pediatr Emerg
Adolesc Med 1998;152:624‑8. Care 1991;7:215‑8.
24. Wenz B, Gennis P, Canova C, Burns ER. The clinical utility of the 32. Danino D, Rimon A, Scolnik D, Grisaru‑Soen G, Glatstein M. Does
leukocyte differential in emergency medicine. Am J Clin Pathol extreme leukocytosis predict serious bacterial infections in infants
1986;86:298‑303. in the post‑pneumococcal vaccine era? The experience of a large,
25. Reding MT, Hibbs JR, Morrison VA, Swaim WR, Filice GA. tertiary care pediatric hospital. Pediatr Emerg Care 2015;31:391‑4.
172 Iraqi Journal of Hematology - Vol 5, Issue 2, Jul-Dec 2016
View publication stats
You might also like
- Feverinthepediatricpatient: Robyn Wing,, Maya R. Dor,, Patricia A. McquilkinDocument24 pagesFeverinthepediatricpatient: Robyn Wing,, Maya R. Dor,, Patricia A. McquilkinAzkiaNo ratings yet
- Evaluacion Niño Con FiebreDocument24 pagesEvaluacion Niño Con FiebredanielentuxtlaNo ratings yet
- Fever in The Pediatric Patient PDFDocument24 pagesFever in The Pediatric Patient PDFSABASA1012No ratings yet
- Genetics and The Evaluation of The Febrile Child: EditorialDocument2 pagesGenetics and The Evaluation of The Febrile Child: EditorialYRRVNo ratings yet
- Fever Without A Source in Children 3 To 36 Months of Age: Evaluation and ManagementDocument30 pagesFever Without A Source in Children 3 To 36 Months of Age: Evaluation and ManagementAndreea BanicaNo ratings yet
- Fever Without A Source in Children 3 To 36 Months of Age - Evaluation and Management - UpToDateDocument50 pagesFever Without A Source in Children 3 To 36 Months of Age - Evaluation and Management - UpToDateThảo Nguyên Phan NguyễnNo ratings yet
- Vol 21 No 1 - SANTOS - Clinical Risk Score FinalDocument12 pagesVol 21 No 1 - SANTOS - Clinical Risk Score FinalAnnsh Hadji EliasNo ratings yet
- IntJMycobacteriol63258-523108 000843Document6 pagesIntJMycobacteriol63258-523108 000843Andrés UribeNo ratings yet
- Ishimine2013fiebre SignosDocument26 pagesIshimine2013fiebre SignosAnirisulNo ratings yet
- Infectious Mononucleosis Due To Epstein-Barr Virus Infection in Children - A Profile From Eastern IndiaDocument7 pagesInfectious Mononucleosis Due To Epstein-Barr Virus Infection in Children - A Profile From Eastern IndiaEmilia LunguNo ratings yet
- Jurnal 2Document12 pagesJurnal 2zingioNo ratings yet
- New Tool For TB DX and Drug Resistance-2018Document5 pagesNew Tool For TB DX and Drug Resistance-2018OclyDaviraPutriNo ratings yet
- Dengue Infection in Children in Ratchaburi, Thailand: A Cohort Study. II. Clinical ManifestationsDocument11 pagesDengue Infection in Children in Ratchaburi, Thailand: A Cohort Study. II. Clinical ManifestationsMey KhNo ratings yet
- IPIntJMedPaediatrOncol 7 1 41 45Document5 pagesIPIntJMedPaediatrOncol 7 1 41 45Angelo FanusanNo ratings yet
- Fever Without A Source in Children 3 To 36 Months of AgeDocument19 pagesFever Without A Source in Children 3 To 36 Months of AgeRajiv KabadNo ratings yet
- A Thesis Proposal Submitted in Partial Fulfillment For The Requirements of MD inDocument13 pagesA Thesis Proposal Submitted in Partial Fulfillment For The Requirements of MD inMohamed HassanNo ratings yet
- Feverinthepediatricpatient: Robyn Wing,, Maya R. Dor,, Patricia A. McquilkinDocument24 pagesFeverinthepediatricpatient: Robyn Wing,, Maya R. Dor,, Patricia A. McquilkinSebastian SalinasNo ratings yet
- Fever in Pediatric Primary Care: Occurrence, Management, and OutcomesDocument9 pagesFever in Pediatric Primary Care: Occurrence, Management, and OutcomesAlbertNo ratings yet
- Etiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesDocument11 pagesEtiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesAlexandra Duque-DavidNo ratings yet
- s13256 021 02698 5Document5 pagess13256 021 02698 5meth holaNo ratings yet
- Hypothermie NigeriaDocument5 pagesHypothermie NigeriaMadina NacroNo ratings yet
- 12 IauujDocument9 pages12 IauujFaiz Yunanto MangoendiprodjoNo ratings yet
- A Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsDocument28 pagesA Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsPatrick NunsioNo ratings yet
- Clinical Characteristic Covid ChildrenDocument8 pagesClinical Characteristic Covid ChildrenEstirahayuNo ratings yet
- Bloodstream Infections in Hospitalized Children: Epidemiology and Antimicrobial SusceptibilitiesDocument4 pagesBloodstream Infections in Hospitalized Children: Epidemiology and Antimicrobial SusceptibilitiesrasioputraNo ratings yet
- 182208-Article Text-464354-1-10-20190121Document7 pages182208-Article Text-464354-1-10-20190121NuurNo ratings yet
- Children: Fever in Children: Pearls and PitfallsDocument19 pagesChildren: Fever in Children: Pearls and PitfallsKelvin George Huayllazo MerelNo ratings yet
- 2010 Fiebre Sin FocoDocument29 pages2010 Fiebre Sin FocoHerminia CastilloNo ratings yet
- Microbiological Profiles of Neonatal Sepsis in Northern EgyptDocument12 pagesMicrobiological Profiles of Neonatal Sepsis in Northern EgyptAhmed AmerNo ratings yet
- 30182-Article Text-56587-1-10-20211025Document8 pages30182-Article Text-56587-1-10-20211025hamdi.mus.mh10No ratings yet
- JurnalDocument6 pagesJurnalAchmad YunusNo ratings yet
- Ref 8 Pneumonia in ALLDocument7 pagesRef 8 Pneumonia in ALLmuarifNo ratings yet
- Bab IiDocument7 pagesBab IiRaden HasanusiNo ratings yet
- 868 4051 1 PBDocument4 pages868 4051 1 PBVhievien ChiaNo ratings yet
- Warming Up For A Better Fever: A Randomized Pilot Study in Pediatric OncologyDocument10 pagesWarming Up For A Better Fever: A Randomized Pilot Study in Pediatric OncologyhcuasnawatiNo ratings yet
- The Optimum Cut Off Value of The Nelwan Score To Diagnose Typhoid Fever in AdultsDocument18 pagesThe Optimum Cut Off Value of The Nelwan Score To Diagnose Typhoid Fever in AdultsDwiky AmarullahNo ratings yet
- Clinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-AnalysisDocument8 pagesClinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-AnalysisArina Al-KhaqNo ratings yet
- 10 1001@jamapediatrics 2020 2430Document7 pages10 1001@jamapediatrics 2020 2430rianza hutasuhutNo ratings yet
- Trevisan U To 2018Document7 pagesTrevisan U To 2018linamaria.pedNo ratings yet
- Laboratory Findings of COVID-19 Infection Are Conflicting in Different Age Groups and Pregnant Women: A Literature ReviewDocument5 pagesLaboratory Findings of COVID-19 Infection Are Conflicting in Different Age Groups and Pregnant Women: A Literature Reviewtrisna amijayaNo ratings yet
- Emergency Department Management of Adults With Infectious MeningitisDocument24 pagesEmergency Department Management of Adults With Infectious MeningitisJuan Carlos Navarro GarcíaNo ratings yet
- Dengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesDocument12 pagesDengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesYono FabiandiNo ratings yet
- The Incidence and Consequences of Neonatal Hypothermia in Babies Presenting To A Tertiary Care Hospital: An Observational StudyDocument6 pagesThe Incidence and Consequences of Neonatal Hypothermia in Babies Presenting To A Tertiary Care Hospital: An Observational StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Fiebre Sin Foco Aparente 3 A 36 Meses DynaMedDocument41 pagesFiebre Sin Foco Aparente 3 A 36 Meses DynaMedAna Maria Guerron CabreraNo ratings yet
- Value of Widal Test in The Diagnosis of Typhoid Fever: Original ArticleDocument5 pagesValue of Widal Test in The Diagnosis of Typhoid Fever: Original ArticleguemadiNo ratings yet
- Articulo 5Document7 pagesArticulo 5Diana OlivaresNo ratings yet
- Journal Pone 0248838Document11 pagesJournal Pone 0248838helentika AvianaNo ratings yet
- Mec y VacunasDocument7 pagesMec y Vacunaskaty gradosNo ratings yet
- Sciencedirect: Hong-Jie Kuo, Ing-Kit Lee, Jien-Wei LiuDocument9 pagesSciencedirect: Hong-Jie Kuo, Ing-Kit Lee, Jien-Wei LiuzihanNo ratings yet
- Pims 2020Document8 pagesPims 2020diegoarenasleytonNo ratings yet
- Background: Pneumonia Arthritis Osteomyelitis SepsisDocument53 pagesBackground: Pneumonia Arthritis Osteomyelitis SepsisWuwun NurulhidayatiNo ratings yet
- 2016 Article 645Document10 pages2016 Article 645Betharia TriayuNo ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofrizki agusmaiNo ratings yet
- Serum Ionic Calcium Levels and Hypocalcemia in DenDocument5 pagesSerum Ionic Calcium Levels and Hypocalcemia in DenJoko Purnomo HNo ratings yet
- Shah Neonatal SepsisDocument10 pagesShah Neonatal SepsistioNo ratings yet
- Symptoms of SARS-CoV-2Document13 pagesSymptoms of SARS-CoV-2dhairyasheelNo ratings yet
- Lucas 2014Document8 pagesLucas 2014Prima YosiNo ratings yet
- Immunological Aspects of Chronic and Recurrent Acute Rhinosinusitis in ChildrenDocument5 pagesImmunological Aspects of Chronic and Recurrent Acute Rhinosinusitis in ChildrenCentral Asian StudiesNo ratings yet
- Thesis VasundharaDocument56 pagesThesis VasundharapanugantigireeshraiNo ratings yet
- Chronic Viral Hepatitis:: Always Be Current!Document14 pagesChronic Viral Hepatitis:: Always Be Current!silpayNo ratings yet
- With Row 1990Document2 pagesWith Row 1990silpayNo ratings yet
- FrenectomiaDocument5 pagesFrenectomiasilpayNo ratings yet
- Cleghorn2010 PDFDocument28 pagesCleghorn2010 PDFsilpayNo ratings yet
- Periodontal Approach To Esthetic Dentistry: February 2015Document6 pagesPeriodontal Approach To Esthetic Dentistry: February 2015silpayNo ratings yet
- Vaccine: What You Need To Know: Haemophilus Influenzae Type B (Hib)Document2 pagesVaccine: What You Need To Know: Haemophilus Influenzae Type B (Hib)mpersiNo ratings yet
- Management of Unconscious PatientDocument51 pagesManagement of Unconscious PatientEmenike Donald Ejieji50% (2)
- AC IO L: Oral Revalida 5Document38 pagesAC IO L: Oral Revalida 5OT312 CBRNo ratings yet
- Nursing Care Plan LeptospirosisDocument2 pagesNursing Care Plan Leptospirosisderic85% (20)
- Dr. G. M. Taori: Curriculum VitaeDocument12 pagesDr. G. M. Taori: Curriculum Vitaesrajan sahuNo ratings yet
- Signs & Symptoms of Strep B in InfantsDocument59 pagesSigns & Symptoms of Strep B in InfantsAbdul Ghaffar AbdullahNo ratings yet
- Meningismus Vs MeningitisDocument19 pagesMeningismus Vs MeningitisRanna HertenizaNo ratings yet
- Bacterial Meningitis in Children Older Than One MonthDocument23 pagesBacterial Meningitis in Children Older Than One MonthMario Mendoza TorresNo ratings yet
- MicroorganismsDocument12 pagesMicroorganismsMiggy GNo ratings yet
- Hanson Infectious Diseases - Anamneza I StatusDocument33 pagesHanson Infectious Diseases - Anamneza I StatusSilvia KesegNo ratings yet
- CoC ExamDocument29 pagesCoC Examanteneh67% (3)
- Chapter SixDocument182 pagesChapter Sixtadele10No ratings yet
- CNS questions-WPS OfficeDocument39 pagesCNS questions-WPS OfficeEvidence ChaibvaNo ratings yet
- Cefotaxime and Ceftriaxone PDFDocument7 pagesCefotaxime and Ceftriaxone PDFDwi FitriyaniNo ratings yet
- MCQ April 2015Document15 pagesMCQ April 2015Sylphana Astharica LawalataNo ratings yet
- Hospital Antibiotic Policy: ST Helens and Knowsley Hospitals TrustDocument72 pagesHospital Antibiotic Policy: ST Helens and Knowsley Hospitals TrustDimas RfNo ratings yet
- Undergraduate Pathology NotesDocument77 pagesUndergraduate Pathology Notesraul sinatoNo ratings yet
- Col Medical Surgical 30.06.2016-1Document66 pagesCol Medical Surgical 30.06.2016-1Sibelle Bou NassifNo ratings yet
- Immunoglobulin G4-Related Hypertrophic Pachymeningitis: A Case-Oriented ReviewDocument11 pagesImmunoglobulin G4-Related Hypertrophic Pachymeningitis: A Case-Oriented ReviewErnesto ColqueNo ratings yet
- HIV-Associated Opportunistic Infections of The CNSDocument13 pagesHIV-Associated Opportunistic Infections of The CNSmauroignacioNo ratings yet
- Algoritma Fever, DLLDocument4 pagesAlgoritma Fever, DLLVanDoctor JerseyNo ratings yet
- MeningitisDocument5 pagesMeningitisliesel_12100% (1)
- Meningitis ViralDocument7 pagesMeningitis ViralTia Gustiani Poplei ViolaNo ratings yet
- Clinical Aspects of Headache in HIVDocument8 pagesClinical Aspects of Headache in HIVnatacha479No ratings yet
- 16 Microbiology MCQsDocument9 pages16 Microbiology MCQsomaromran0% (1)
- Miliary TB R)Document15 pagesMiliary TB R)Krishna VidhuriNo ratings yet
- 3 s2.0 B9781455748013003301 MainDocument120 pages3 s2.0 B9781455748013003301 MainInzamam Ul HaqNo ratings yet
- Microbial Diseases of The Nervous SystemDocument7 pagesMicrobial Diseases of The Nervous SystemAnaNo ratings yet
- Specimen Collection HenrysDocument17 pagesSpecimen Collection HenrysLeonNo ratings yet
- DiseasesDocument3 pagesDiseasesBarani KingNo ratings yet