Professional Documents
Culture Documents
Service Excellence 2012
Uploaded by
FifiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Service Excellence 2012
Uploaded by
FifiCopyright:
Available Formats
ORIGINAL CONTRIBUTION
Scan for Author
Audio Interview
Association Between Hospital Recognition
for Nursing Excellence and Outcomes
of Very Low-Birth-Weight Infants
Eileen T. Lake, PhD, RN Context Infants born at very low birth weight (VLBW) require high levels of nursing
Douglas Staiger, PhD intensity. The role of nursing in outcomes for these infants in the United States is not
Jeffrey Horbar, MD known.
Robyn Cheung, PhD, RN Objective To examine the relationships between hospital recognition for nursing ex-
cellence (RNE) and VLBW infant outcomes.
Michael J. Kenny, MS
Design, Setting, and Patients Cohort study of 72 235 inborn VLBW infants weigh-
Thelma Patrick, PhD, RN ing 501 to 1500 g born in 558 Vermont Oxford Network hospital neonatal intensive
Jeannette A. Rogowski, PhD care units between January 1, 2007, and December 31, 2008. Hospital RNE was de-
termined from the American Nurses Credentialing Center. The RNE designation is
O
NE IN 4 VERY LOW-BIRTH- awarded when nursing care achieves exemplary practice or leadership in 5 areas.
weight (VLBW) infants Main Outcome Measures Seven-day, 28-day, and hospital stay mortality; noso-
(⬍1500 g) dies in the first comial infection, defined as an infection in blood or cerebrospinal fluid culture occur-
year of life; nearly all ring more than 3 days after birth; and severe (grade 3 or 4) intraventricular hemor-
deaths (87%) occur in the first month.1 rhage.
Infant mortality in the United States is Results Overall, the outcome rates were as follows: for 7-day mortality, 7.3% (5258/
concentrated in this population. Al- 71 955); 28-day mortality, 10.4% (7450/71 953); hospital stay mortality, 12.9% (9278/
though they account for only 1.5% of 71 936); severe intraventricular hemorrhage, 7.6% (4842/63 525); and infection, 17.9%
births, these infants account for more (11 915/66 496). The 7-day mortality was 7.0% in RNE hospitals and 7.4% in non-
than half of infant deaths.1 Very low- RNE hospitals (adjusted odds ratio [OR], 0.87; 95% CI, 0.76-0.99; P=.04). The 28-
birth-weight infants who survive have day mortality was 10.0% in RNE hospitals and 10.5% in non-RNE hospitals (adjusted
OR, 0.90; 95% CI, 0.80-1.01; P=.08). Hospital stay mortality was 12.4% in RNE hos-
higher rates of morbidity and disabil-
pitals and 13.1% in non-RNE hospitals (adjusted OR, 0.90; 95% CI, 0.81-1.01; P=.06).
ity, including developmental delays and Severe intraventricular hemorrhage was 7.2% in RNE hospitals and 7.8% in non-RNE
cognitive impairment, than infants with hospitals (adjusted OR, 0.88; 95% CI, 0.77-1.00; P=.045). Infection was 16.7% in
normal birth weights.2-5 RNE hospitals and 18.3% in non-RNE hospitals (adjusted OR, 0.86; 95% CI, 0.75-
Neonatal intensive care unit (NICU) 0.99; P=.04). Compared with RNE hospitals, the adjusted absolute decrease in risk of
infants are among the most nurse- outcomes in RNE hospitals ranged from 0.9% to 2.1%. All 5 outcomes were jointly
intensive patients, with recom- significant (P⬍.001). The mean effect across all 5 outcomes was OR, 0.88 (95% CI,
mended patient-nurse ratios of at most 0.83-0.94; P⬍.001). In a subgroup of 68 253 infants with gestational age of 24 weeks
2 to 1 for neonates needing intensive or older, the ORs for RNE for all 3 mortality outcomes and infection were statistically
significant.
care.6,7 To intervene before the onset of
life-threatening problems, nurses must Conclusion Among VLBW infants born in RNE hospitals compared with non-RNE
make complex assessments, imple- hospitals, there was a significantly lower risk-adjusted rate of 7-day mortality, noso-
comial infection, and severe intraventricular hemorrhage but not of 28-day mortality
ment highly intensive therapies, and
or hospital stay mortality.
make immediate adjustments depen-
JAMA. 2012;307(16):1709-1716 www.jama.com
For editorial comment see p 1750. Author Affiliations are listed at the end of this article.
dent on infant response.8 Maintaining Corresponding Author: Eileen T. Lake, PhD, RN, Uni-
Author Audio Interview available at versity of Pennsylvania School of Nursing, 418 Curie
optimal respiratory, cardiac, and feed- Blvd, Philadelphia, PA 19104-6096 (elake@nursing
www.jama.com. ing status may result in improved de- .upenn.edu).
©2012 American Medical Association. All rights reserved. JAMA, April 25, 2012—Vol 307, No. 16 1709
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
velopment and behavior, lower levels an extensive and rigorous process that families. VON hospitals are located in
of morbidity, and shorter hospitaliza- generally takes 2 years. Recognition is 47 states, Washington, DC, and 22 for-
tion.9 Nurse handling of an infant and at the hospital level but all units must eign countries. The VON database con-
recognition and response to subtle cues meet criteria. The hospital pays a tains detailed uniform clinical and treat-
that an infant is distressed may sup- sliding-scale application fee, conducts ment information on all VLBW infants
port infant hemodynamic stability and an extensive self-evaluation followed cared for by network hospitals. By 2008,
reduce the likelihood of intraventricu- by an analysis to identify the gaps in the US VON database comprised 578
lar hemorrhage.10 Aseptic technique and achieving standards, works with a hospitals, which included approxi-
scrupulous hand hygiene by nurses dur- consultant to implement organiza- mately 65% of NICUs and 80% of all
ing infant care, especially in the main- tional changes to fulfill numerous rec- VLBW infants born in the United States.
tenance of central lines, decrease the ognition of nursing excellence (RNE) This cross-sectional study included 558
risk of infants acquiring a nosocomial standards, and is evaluated by outside VON hospitals with inborn infants in
infection.11,12 appraisers through a site visit of sev- 2007 and 2008. The remaining 20 were
The American Nurses Credentialing eral days.15 Hospitals are required to children’s hospitals that had only out-
Center developed the Magnet Recog- undergo a redesignation process every born infants.
nition Program to recognize health 4 years. Interim reporting is also The study population consisted of
care organizations for quality patient required. 72 235 inborn infants who weighed be-
care, nursing excellence, and innova- Recognition for nursing excellence tween 501 and 1500 g. Infants who died
tions in professional nursing prac- is uncommon. Only 7% of US hospi- in the delivery department or else-
tice.13 Organizations are evaluated for tals achieve this. Very few lose it (⬍10 where in the hospital were included
evidence of achieving 5 program ele- since the program’s inception in 1994); even if they were not admitted to the
ments: transformational leadership; however, approximately 20% of hos- NICU. Infants who weighed 500 g or
structural empowerment; exemplary pitals with a NICU have this recogni- less were excluded for consistency with
professional practice; new knowledge, tion (authors’ tabulations of American prior studies. Infants with incomplete
innovations, and improvements; Hospital Association Annual Survey data on infant characteristics (n=599)
and empirical outcomes. Exemplary data and American Nurses Credential- were excluded to yield a consistent
professional practice is achieved ing Center public listing). sample for multivariable models. In
when “nurses have significant [profes- Patient outcomes in RNE hospitals analyses of mortality, an additional 299
sional] control . . . and work in have been understudied.16,17 The objec- infants were excluded for missing data
collaboration with interdisciplinary tive of this study was to examine the as- on death. Institutional review board ap-
partners to achieve high-quality sociation of hospital RNE status with proval was obtained from the Univer-
patient outcomes.” 14(p28) The other VLBW infant outcomes. We analyzed sity of Medicine and Dentistry of New
4 elements support and maintain mortality, severe intraventricular hem- Jersey and the University of Vermont,
nursing excellence. For instance, orrhage (SIVH), and nosocomial infec- including a waiver of informed con-
structural empowerment means “the tion because we hypothesized these out- sent. The University of Pennsylvania in-
flow of information and decision- comes would be influenced by nursing stitutional review board judged the
making is bi-directional and horizon- care and prior research has indicated that project exempt.
tal . . . among professional nurses at they may be affected.18-21 In addition to
the bedside, the leadership team, and hospital stay mortality, 2 other mortal- Variables
the chief nursing officer (CNO).14(p44) ity time frames were predefined: within All patient- and NICU-level measures
New knowledge includes “establishing the critical first week of life and within were obtained or derived from the VON
new ways of achieving high-quality, 28 days of birth. Death in the first week database. VON data are collected using
effective, and efficient care.” 14(p32) of life accounts for the majority of neo- standardized definitions. The data are
Transformational leadership requires natal (71%) and in-hospital (57%) mor- subjected to extensive range, logic, and
that “the CNO in a Magnet organiza- tality in VLBW infants. Death within 28 consistency checks when submitted and
tion . . . develops a strong vision and days, or neonatal mortality, is a com- are reviewed and verified annually. In-
well-articulated philosophy, profes- monly reported statistic. fant characteristics were measured at
sional practice model, and strategic birth.
and quality plans in leading nursing METHODS The key outcome measures were
services.”14(p42) Empirical outcomes Sites and Patient Sample death (within 7 days, 28 days, and the
document achievement in all of these The Vermont Oxford Network (VON) hospital stay), nosocomial infection,
areas. These criteria are expected to is a voluntary collaborative network of and SIVH. Nosocomial infection was
assist health care organizations in hospitals with a NICU dedicated to im- defined as an infection in blood or ce-
achieving high-quality nursing care for proving the quality and safety of medi- rebrospinal fluid culture occurring
all patients. The route to recognition is cal care for newborn infants and their more than 3 days after birth. The da-
1710 JAMA, April 25, 2012—Vol 307, No. 16 ©2012 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
tabase includes information on 3 based on maternal race and ethnicity as account for a secular trend. We esti-
culture-proven infections: coagulase- recorded in the birth certificate or medi- mated random-effects models by the
negative Staphylococcus, the most com- cal record. Maternal socioeconomic sta- maximum likelihood method. This
mon bacterial infection in the NICU; tus was not available in the VON da- method includes an unobserved hos-
other bacterial infections; and fungal in- tabase and could not be geocoded. pital-level component (the random
fections. Severe intraventricular hem- Previous research did not find an ef- effect) that captures any omitted hos-
orrhage was defined as the presence of fect of maternal socioeconomic status pital-level factors that systematically
grade 3 or 4 intraventricular hemor- on mortality using earlier years of the increase or decrease the likelihood of
rhage on a cranial ultrasound per- VON database.24 The risk-adjustment each outcome for all infants in that hos-
formed within the first 28 days.22 Grades model had area under the receiver op- pital. Inclusion of this random effect
3 and 4 hemorrhages are the most se- erating characteristic curves of 0.88 for corrects the standard errors for the
vere and are more likely to be associ- mortality, 0.82 for SIVH, and 0.75 for resulting within-hospital correlation (ie,
ated with long-term neurodevelopmen- infection. clustering) in patient outcomes. When
tal sequelae. Of the sample, 14.6% of Two NICU-level variables were in- there are multiple outcomes and all are
the infants were transferred and 3.7% cluded consistent with prior re- hypothesized to be important, a joint
were readmitted to the birth hospital. search.24-26 Volume was measured as the significance test computes the average
The final disposition (discharge alive mean number of VLBW infants admit- effect to summarize the overall pat-
or dead) is tracked for all infants and ted to the hospital in 2007 and 2008. tern. The joint F test accounts for cor-
attributed to the birth hospital regard- Due to the presence of high-volume relation between the 3 mortality mea-
less of transfer status. If an infant was NICUs, the data were transformed to sures. To determine whether RNE status
readmitted to the birth hospital after a the natural log of volume for a more was significantly related to all 5 out-
transfer, SIVH and infection were col- normally distributed measure. NICU comes, we tested the hypothesis that all
lected for the entire stay, including at level was obtained from the VON’s an- 5 odds ratios (ORs) were jointly equal
the transfer hospital, and attributed to nual survey. The VON classifies NICUs to 1 and also tested whether the mean
the birth hospital. These data were not into levels A (restriction on ventila- OR across all 5 outcomes was equal to
collected on infants transferred out and tion; no surgery), B (major surgery), 1. Confidence intervals and P values for
not readmitted. However, since SIVH and C (cardiac surgery), correspond- these tests were based on the boot-
occurs principally in the first few days ing to high level II and level III units strap method to account for correla-
of life, the 23-day median age of trans- in the American Academy of Pediat- tion between the estimates.28 To explore
fer implies that SIVH is unlikely to oc- rics NICU classification. The universe the possibility that RNE may have a dif-
cur in a transfer hospital. In 2009, VON of US NICUs was identified from the ferent association with outcomes for
data were collected on infection loca- American Hospital Association sur- VLBW infant subgroups, such as those
tion and indicated that among read- vey27 by nonzero values for neonatal above a viability threshold, we repeated
mitted infants, 4% of infections were intensive care beds. Two hospital our regression analyses in subgroups
contracted at the transfer hospital; in characteristics, hospital ownership stratified by gestational age of 24 weeks
this analysis, those would be attrib- (not-for-profit, for-profit, or public) and or older vs younger than 24 weeks and
uted to the hospital of birth. teaching status (membership in the birth weight of 1000 g or more vs less
The independent variable, hospital Council of Teaching Hospitals), were than 1000 g (extremely low birth
RNE designation in 2008, was ob- also obtained from the American Hos- weight). The analyses were conducted
tained from a public website listing des- pital Association survey. using Stata software, version 10.1.29 The
ignated hospitals’ original and most re- a priori significance level was P⬍.05
cent year of redesignation.23 Patient risk Data Analysis for a 2-sided significance test.
adjusters consisted of infant character- Our focus in this study was on hospi-
istics that were developed for the VON tal RNE and VLBW infant outcomes. We RESULTS
risk-adjustment model.23 These covar- first examined the bivariate relation- Of the sample, 21% of hospitals had
iates included gestational age in weeks ship between RNE and each outcome. RNE status compared with 19% of US
(and its square); small for gestational Tests of bivariate comparisons adjusted hospitals with a NICU; 16% of sample
age; 1-minute Apgar score; race and eth- for infant clustering within hospitals. hospitals provided the highest level of
nicity (non-Hispanic black, non- We then estimated 3 logistic regres- care (level C). Compared with the uni-
Hispanic white, or other [including His- sions for each outcome. The first verse of hospitals with a NICU, our
panic]); sex; multiple birth; presence included only RNE status as the inde- sample contains somewhat more teach-
of a major birth defect; vaginal deliv- pendent variable. The second added ing hospitals (33% vs 27%) and larger
ery; and whether the mother received patient risk adjusters. The third added units (a mean of 28 beds vs 22 beds).
prenatal care. Race and ethnicity were NICU- and hospital-level covariates. All Compared with non-RNE hospi-
classified into standard VON options models controlled for birth year to tals, the RNE hospitals with a NICU are
©2012 American Medical Association. All rights reserved. JAMA, April 25, 2012—Vol 307, No. 16 1711
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
mostly not-for-profit (87% vs 71%) and (eTable 1; available at http://www.jama fants with higher-risk characteristics
have more registered nurse hours (10.5 .com). such as lower Apgar score, multiple
vs 9.3 hours per patient-day at the hos- Sample infants had a mean birth birth, and white race. It is well known
pital level); twice as many are teach- weight of 1056 g and a gestational age in this literature that black infants have
ing hospitals (55% vs 27%) (TABLE 1). of 28.2 weeks (Table 1). The racial and a survival advantage, which differs from
Few RNE hospitals are for-profit com- ethnic composition of the entire sample most other populations.30 The mean
pared with non-RNE hospitals (3% vs was 47% non-Hispanic white, 29% non- predicted probability of death was
13%). The RNE hospitals care for a Hispanic black, and 24% other, while 13.0% in RNE hospitals and 12.6% in
larger volume of VLBW infants than the composition of infants in RNE hos- non-RNE hospitals controlling for in-
non-RNE hospitals (93 vs 74 VLBW in- pitals was disproportionately non- fant factors.
fants, respectively). Also, RNE hospi- Hispanic white (54%) (P ⬍ .001). The The percentage of eligible infants
tal NICUs are disproportionately level risk profile of RNE hospitals was higher with each outcome was as follows:
C (32% vs 12%) rather than level A than for non-RNE hospitals based on 7-day mortality, 7.3% (n = 5258/
(23% vs 33%) compared with non- the characteristics of VLBW infants 71 955); 28-day mortality, 10.4%
RNEs. These RNE/non-RNE differ- born in those hospitals. The RNE hos- (n = 7450/71 953); hospital stay mor-
ences mirrored those of US NICUs pitals had disproportionately more in- tality, 12.9% (n=9278/71 936); SIVH,
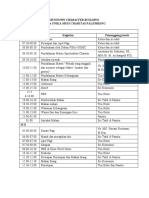
Table 1. Hospital, NICU, and Infant Characteristics
Participants a
Characteristics Total RNE Hospitals Non-RNE Hospitals P Value b
Hospital characteristics N = 558 n = 119 n = 439
Hospital ownership
Public 85 (15) 13 (11) 72 (16)
For-profit 60 (11) 3 (3) 57 (13) .001
Not-for-profit 413 (74) 103 (87) 310 (71)
Member, Council of Teaching Hospitals 185 (33) 66 (55) 119 (27) ⬍.001
Hospital nursing characteristics
RNE hospital 119 (21) 119 (100) 0
Registered nurse hours per adjusted patient-day, 9.6 (3.0) 10.5 (2.9) 9.3 (2.9) ⬍.001
mean (SD) c
NICU characteristics
NICU level
A 171 (31) 27 (23) 144 (33)
B 296 (53) 54 (45) 242 (55) ⬍.001
C 91 (16) 38 (32) 53 (12)
Annual volume of very low-birth-weight admissions, 78 (60.4) 93 (58.9) 74 (60.3) ⬍.001
mean (SD)
Infant characteristics n = 72 235 n = 17 455 n = 54 780
Birth weight, mean (SD), g 1056 (287) 1056 (286) 1056 (287) .89
Gestational age, mean (SD), wk 28.2 (2.9) 28.2 (2.9) 28.2 (2.9) .96
1-Minute Apgar score, mean (SD) 5.4 (2.5) 5.3 (2.5) 5.5 (2.5) ⬍.001
Small for gestational age 13 916/72 216 (19) 3345/17 449 (19) 10 571/54 767 (19) .70
Multiple birth 20 616/72 224 (29) 5284/17 454 (30) 15 332/54 770 (28) ⬍.001
Congenital malformation 3439/72 194 (5) 840/17 449 (5) 2599/54 745 (5) .72
Vaginal delivery 19 972/72 230 (28) 4817/17 452 (28) 15 155/54 778 (28) .87
Had prenatal care 69 124/72 025 (96) 16 817/17 421 (97) 52 307/54 604 (96) ⬍.001
Male 36 341/72 211 (50) 8869/17 451 (51) 27 472/54 760 (50) .13
Race/ethnicity n = 72 040 n = 17 410 n = 54 630
Non-Hispanic white 33 541 (47) 9426 (54) 24 115 (44)
Non-Hispanic black 21 164 (29) 4588 (26) 16 576 (30) ⬍.001
Other d 17 335 (24) 3396 (20) 13 939 (26)
Year of birth 2008 37 116/72 235 (51) 9132/17 455 (52) 27 984/54 780 (51) ⬍.001
Abbreviations: NICU, neonatal intensive care unit; RNE, recognition for nursing excellence.
a Data are expressed as No. (%) of participants unless otherwise indicated.
b The 2 test was used for comparison of categorical variables and the unpaired 2-tailed t test for continuous variables.
c Calculated by the authors from the 2008 American Hospital Association Annual Hospital Survey.27
d All other races/ethnicities, including Hispanic.
1712 JAMA, April 25, 2012—Vol 307, No. 16 ©2012 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
Table 2. Very Low-Birth-Weight Infant Outcomes, 2007-2008
Infants, No./Total (%)
All Hospitals RNE Hospitals Non-RNE Hospitals
Outcomes (N = 558) (n = 119) (n = 439)
No. of infants 72 235 17 455 54 780
Death within 7 d 5258/71 955 (7.3) 1215/17 415 (7.0) 4043/54 540 (7.4)
Death within 28 d 7450/71 953 (10.4) 1740/17 415 (10.0) 5710/54 538 (10.5)
Death before discharge home 9278/71 936 (12.9) 2159/17 414 (12.4) 7119/54 522 (13.1)
Nosocomial infection 11 915/66 496 (17.9) 2706/16 221 (16.7) 9209/50 275 (18.3)
Severe intraventricular hemorrhage 4842/63 525 (7.6) 1109/15 482 (7.2) 3733/48 043 (7.8)
Abbreviation: RNE, recognition for nursing excellence.
7.6% (4842/63 525); and infection, SIVH. Birth in an RNE hospital was COMMENT
17.9% (11 915/66 496) (T ABLE 2). associated with odds of death in the Hospital RNE status was found to be as-
The 7-day mortality was 7.0% in RNE first week of life of 0.87 (95% CI, sociated with significantly lower rates
hospitals vs 7.4% in non-RNE hospi- 0.76-0.99), an odds of infection of of 7-day mortality, nosocomial infec-
tals (difference, 0.4%); 28-day mortal- 0.86 (95% CI, 0.75-0.99), and an tion, and SIVH in VLBW infants. Rates
ity was 10.0% in RNE hospitals vs odds of SIVH of 0.88 (95% CI, 0.78- of 7-day mortality (7%), SIVH (8%), and
10.5% in non-RNE hospitals (differ- 1.00). The 28-day and in-hospital nosocomial infection (18%) were high
ence, 0.5%); and hospital stay mortal- mortality had similar ORs (0.90) but in these patients. There was a 12% to
ity was 12.4% in RNE hospitals vs were not statistically significant. Com- 14% difference in the odds of these out-
13.1% in non-RNE hospitals (differ- pared with non-RNE hospitals, the comes between RNE and non-RNE hos-
ence, 0.7%). The incidence of SIVH adjusted absolute decrease in risk of pitals, with 95% confidence limits close
was 7.2% in RNE hospitals and 7.8% outcomes in RNE hospitals ranged to 1, which translates to relatively small
in non-RNE hospitals (difference, from 0.9% to 2.1%. All 5 outcomes adjusted absolute risk differences of
0.6%). Infection occurred in 16.7% of were jointly significant (P ⬍ .001). 0.9% to 2.1%. For neonatal and in-
VLBW infants in RNE hospitals and The mean effect across all 5 outcomes hospital mortality, the findings were not
18.3% in non-RNE hospitals (differ- was an OR of 0.88 (95% CI, 0.83- significant. Although the significant
ence, 1.6%). 0.94; P ⬍ .001). Infants cared for in mortality difference between the 2 hos-
T ABLE 3 shows the relationships type A NICUs had an OR for infection pital groups disappeared by 28 days of
between RNE status and infant out- of 0.74 (95% CI, 0.60-0.92; P = .005) life, it remained significant in older-
comes in logistic regression models. relative to type C NICUs. Infants born gestational-age infants.
The lower rates of adverse outcomes in for-profit hospitals had an OR for These morbidities have serious con-
in RNE hospitals observed in Table 2 infection of 1.24 (95% CI, 1.02-1.49; sequences. Development of an infec-
understate the differences between P = .03) relative to not-for-profit hos- tion more than doubles the mortality
these hospital types. From the unad- pitals. The OR for the log volume of rate among VLBW infants.31 In our
justed OR to the OR adjusted for VLBW infants for 7-day mortality was sample, among infants who survived 3
infant risk, the ORs associated with 0.90 (95% CI, 0.82-0.99; P=.02). days, 13.8% of those with nosocomial
RNE status decreased on average by The 2 gestational age subgroups ex- infection died compared with 5.5%
0.07 (range, 0-0.12). This is because hibited marked differences in the ORs without infection. Even more striking
somewhat higher-risk infants are for the mortality variables but not for are the implications of SIVH for mor-
born in RNE hospitals, so unadjusted infection and SIVH. In the older ges- tality. In our sample, 36.4% of infants
models confound RNE status with tational age subgroup (ⱖ24 weeks), the with SIVH died compared with 5.9%
patient risk. Adjusting for patient ORs for all 3 mortality outcomes were without SIVH. There are important
risk, RNE hospitals had statistically smaller than in the full cohort, rang- long-term consequences of SIVH for
significant ORs of 0.84 to 0.87 for ing from 0.83 to 0.87, and were statis- brain development, including neuro-
mortality and SIVH, but the OR of tically significant (TABLE 4). In the cognitive impairment, cerebral palsy,
0.88 (95% CI, 0.76-1.00) for infec- younger gestational age subgroup (⬍24 and developmental delays.32,33
tion was not statistically significant. weeks), the ORs for all 3 mortality out- Among VLBW infants born at 24
Three infant outcomes exhibited comes were weaker (ie, closer to or ex- weeks of gestational age or more, the
statistically significant associations ceeding 1.00), with P⬎.60 (eTable 2). ORs for all 3 mortality measures were
with RNE status in models that also The results of analyses in birth-weight stronger (0.83 to 0.87) and statisti-
controlled for NICU and hospital vari- subgroups mirrored the overall find- cally significant. The exclusion of the
ables: 7-day mortality, infection, and ings (eTable 3 and eTable 4). extremely premature subgroup (⬍24
©2012 American Medical Association. All rights reserved. JAMA, April 25, 2012—Vol 307, No. 16 1713
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
weeks) sharpened the RNE associa- tified by reputation as a good place to agement level, and developing new
tion with mortality in the remaining in- practice nursing and for a record of re- knowledge about how to achieve high-
fants. Infants born before 24 weeks are cruiting and retaining professional quality, effective, and efficient care. Im-
at the lower limit of viability. Some nurses in a competitive market com- proving the quality of care for vulner-
families and physicians of these in- pared with a matched sample of hos- able infants was emphasized in the
fants will choose not to use assisted ven- pitals.34 Another study of 2004 data Institute of Medicine report on pre-
tilation and instead provide comfort found a 5% lower patient fall rate in term birth,37 which pointed to nursing
care. Thus, RNE status was more RNE vs non-RNE hospitals.16 as a promising avenue for developing
strongly associated with survival for In the decade since Crossing the Qual- NICU quality measures, and the focus
infants in the gestational age range ity Chasm,35 there have been numer- on infants was reinforced by a March
in which intensive care is usually ous calls to improve the quality of the of Dimes report. 38 One way to in-
applied. health care system. The Quality Health crease the number of infants that re-
Our study identified larger differ- Outcomes Model links system-level fac- ceive high-quality care would be to in-
ences in the odds of outcomes than did tors to patient outcomes.36 Recogni- crease the number of hospitals with
the few studies that have identified simi- tion of nursing excellence status is a RNE. Our results suggest benefit for the
lar associations between hospital RNE system-level factor encompassing pro- VLBW infant population, but other
and adult outcomes. The earliest study fessional control, interdisciplinary col- hospitalized patients may also benefit,
documented a 5% lower Medicare mor- laboration, decision making shared as suggested by the limited empirical
tality rate in 1988 in 39 hospitals iden- from the bedside to the highest man- evidence.
Table 3. Odds Ratios Estimating the Association of Hospital RNE Status and NICU and Hospital Variables With Very Low-Birth-Weight Infant
Outcomes a
Odds Ratio (95% CI)
Adjusted for Patient,
Adjusted for Patient NICU, and Hospital
Outcomes Unadjusted P Value Characteristics P Value Characteristics P Value
Mortality
Within 7 d 0.96 (0.86-1.06) .41 0.84 (0.74-0.96) .01 0.87 (0.76-0.99) .04
Within 28 d 0.96 (0.87-1.05) .35 0.87 (0.77-0.98) .02 0.90 (0.80-1.01) .08
Before discharge 0.95 (0.87-1.03) .21 0.87 (0.78-0.97) .01 0.90 (0.81-1.01) .06
Morbidity
Nosocomial infection 0.88 (0.78-1.01) .06 0.88 (0.76-1.00) .06 0.86 (0.75-0.99) .04
Severe intraventricular hemorrhage 0.90 (0.80-1.00) .05 0.84 (0.75-0.95) .01 0.88 (0.78-1.00) .045
Abbreviations: NICU, neonatal intensive care unit; RNE, recognition for nursing excellence.
a Odds ratios and 95% CIs were derived from random-effects logistic regression models. All models control for year of birth. Infant risk adjusters were gestational age, gestational
age squared, 1-minute Apgar score, small for gestational age, multiple birth, congenital malformation, vaginal delivery, prenatal care, race/ethnicity, and sex. NICU characteristics
were adjusted for the natural log of volume of very low-birth-weight infants and level of care. Hospital characteristics were adjusted for hospital ownership and membership in the
Council of Teaching Hospitals.
Table 4. Odds Ratios Estimating the Association of Hospital RNE Status and NICU and Hospital Variables With Very Low-Birth-Weight Infant
Outcomes Among Infants With Gestational Age of 24 Weeks or More at Birth a
Odds Ratio (95% CI)
Adjusted for Patient,
Adjusted for Patient NICU, and Hospital
Outcomes Unadjusted P Value Characteristics P Value Characteristics P Value
Mortality (n = 67 497-67 517)
Within 7 d 0.91 (0.81-1.02) .10 0.81 (0.70-0.93) .004 0.83 (0.72-0.96) .01
Within 28 d 0.92 (0.83-1.02) .11 0.85 (0.75-0.95) .01 0.87 (0.77-0.99) .03
Before discharge 0.91 (0.83-1.00) .06 0.85 (0.76-0.96) .01 0.87 (0.78-0.98) .02
Morbidity
Nosocomial infection (n = 64 201) 0.87 (0.77-1.0) .04 0.87 (0.75-0.99) .04 0.86 (0.74-0.99) .03
Severe intraventricular hemorrhage 0.89 (0.80-1.00) .06 0.84 (0.74-0.96) .01 0.88 (0.77-1.00) .05
(n = 61 030)
Abbreviations: NICU, neonatal intensive care unit; RNE, recognition for nursing excellence.
a Odds ratios and 95% CIs were derived from random-effects logistic regression models. All models control for year of birth. Infant risk adjusters were gestational age, gestational
age squared, 1-min Apgar score, small for gestational age, multiple birth, congenital malformation, vaginal delivery, prenatal care, race/ethnicity, and sex. NICU characteristics
were adjusted for volume of very low-birth-weight infants and level of care. Hospital characteristics were adjusted for hospital ownership and membership in the Council of Teach-
ing Hospitals.
1714 JAMA, April 25, 2012—Vol 307, No. 16 ©2012 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
The better outcomes observed in did not differ substantially by hospital Funding/Support: This study was supported by a Rob-
ert Wood Johnson Foundation Interdisciplinary Nurs-
VLBW infants in RNE hospitals may type (12% for RNE and 15% for non- ing Quality Research Initiative grant (to Dr Lake) and
reflect higher-quality NICU and RNE). Also, the cross-sectional re- grant R01NR010357 (to Dr Rogowski) from the Na-
tional Institute of Nursing Research, National Insti-
obstetric care. Perhaps RNE hospitals search design prevents causal infer- tutes of Health.
have a broad, long-standing commit- ences. There may be unobserved Role of the Sponsors: The funding organizations had
ment to quality care that is reflected quality-related characteristics of RNE no role in the design and conduct of the study; in the
collection, analysis, and interpretation of the data; or in
in other aspects of care, such as hospitals that are differentially associ- the preparation, review, or approval of the manuscript.
excellent physician care, respiratory ated with outcomes. Future research Disclaimer: The content is solely the responsibility of
the authors and does not necessarily represent the of-
care, or infection control, that are should focus on NICU nursing care, in- ficial views of the National Institute of Nursing Re-
not directly related to RNE but that cluding the roles of specific factors (eg, search or the National Institutes of Health.
Online-Only Material: eTables 1 through 4 and the
may independently contribute to bet- nurse staffing and experience), as well Author Audio Interview are available at http://www
ter outcomes for VLBW infants. as physicians and other health care pro- .jama.com.
Additional Contributions: We thank the 578 institu-
Thus, RNE status may serve as a fessionals. tions that participated in the Vermont Oxford Net-
marker for an institution-wide com- Our study focused on hospitals that work database, whose work made this research possible.
mitment to optimizing outcomes. met criteria for organizational excel-
Recognition for nursing excellence lence in nursing through comprehen- REFERENCES
status has been included as a crite- sive standards that are documented and 1. Mathews TJ, Miniño AM, Osterman MJK, Strobino
rion for a high-quality institution by continuously monitored. Meeting these DM, Guyer B. Annual summary of vital statistics: 2008.
the national groups US News & criteria was associated with better out- Pediatrics. 2011;127(1):146-157.
2. Eichenwald EC, Stark AR. Management and out-
World Report Best Hospitals (since comes for high-risk infants. comes of very low birth weight. N Engl J Med. 2008;
2004)39 and Leapfrog (since 2011).40 358(16):1700-1711.
Author Affiliations: Center for Health Outcomes and 3. Boardman JD, Powers DA, Padilla YC, Hummer
The practical importance of our find- Policy Research, School of Nursing, Department of So- RA. Low birth weight, social factors, and develop-
ings is influenced by the accessibility ciology, and Leonard Davis Institute of Health Eco- mental outcomes among children in the United States.
nomics, University of Pennsylvania, Philadelphia (Dr Demography. 2002;39(2):353-368.
of existing RNE hospitals to mothers at Lake); Department of Economics, Dartmouth Col- 4. Hack M, Flannery DJ, Schluchter M, Cartar L,
high risk of preterm birth. Currently, lege, Hanover, New Hampshire (Dr Staiger); Na- Borawski E, Klein N. Outcomes in young adulthood
access is limited because only 1 in 5 tional Bureau of Economic Research, Cambridge, Mas- for very-low-birth-weight infants. N Engl J Med. 2002;
sachusetts (Drs Staiger and Rogowski); Departments 346(3):149-157.
hospitals with a NICU has RNE. This of Pediatrics (Dr Horbar) and Medical Biostatistics (Mr 5. Maternal and Child Health Bureau, Health Re-
is a particular source of concern for ra- Kenny), University of Vermont, and Vermont Ox- sources and Services Administration, US Department
ford Network (Dr Horbar), Burlington; UK Health- of Health and Human Services. Child health USA 2010.
cial and ethnic minorities because dis- care Enterprise, Lexington, Kentucky (Dr Cheung); Col- http://www.mchb.hrsa.gov/chusa10/hstat/hsi/pages
proportionately few minority infants are lege of Nursing, Ohio State University, Columbus /203vlbw.html. Accessed March 29, 2012.
(Dr Patrick); and Department of Health Systems and 6. Inpatient perinatal care services. In: Lemnos JA,
born in hospitals with RNE. Policy, School of Public Health, University of Medi- Lockwood CJ, eds; American Academy of Pediatrics;
Our study has limitations. The VON cine and Dentistry of New Jersey, Piscataway (Dr American College of Obstetricians and Gynecologists.
is not fully representative of US hospi- Rogowski). Guidelines for Perinatal Care. 6th ed. Elk Grove Vil-
Author Contributions: Dr Lake had full access to all lage, IL: American Academy of Pediatrics and Ameri-
tals with a NICU. Our results may un- the data in the study and takes responsibility for can College of Obstetricians and Gynecologists; 2007:
derestimate the ‘‘true’’ RNE associa- the integrity of the data and the accuracy of the data chap 2.
analysis. 7. Association of Women’s Health Obstetric and Neo-
tions. The comparison hospitals in this Study concept and design: Lake, Staiger, Horbar, natal Nurses. Guidelines for Professional Registered
sample participate in a network dedi- Patrick, Rogowski Nurse Staffing for Perinatal Units. Washington, DC:
Acquisition of data: Lake, Staiger, Horbar, Cheung, Association of Women’s Health Obstetric and Neo-
cated to improving the quality and Patrick, Rogowski. natal Nurses; 2010.
safety of neonatal care; therefore, they Analysis and interpretation of data: Lake, Staiger, 8. Boxwell G, ed. Neonatal Intensive Care Nursing.
Horbar, Cheung, Kenny, Patrick, Rogowski. 2nd ed. New York, NY: Routledge; 2010.
most likely give greater attention to Drafting of the manuscript: Lake, Staiger, Horbar, 9. Becker PT, Grunwald PC, Moorman J, Stuhr S. Out-
quality improvements and monitor- Patrick, Rogowski. comes of developmentally supportive nursing care for
ing. In addition, the VON dispropor- Critical revision of the manuscript for important in- very low birth weight infants. Nurs Res. 1991;
tellectual content: Lake, Staiger, Horbar, Cheung, 40(3):150-155.
tionately lacks the smallest NICUs, Kenny, Patrick, Rogowski. 10. Volpe J. Intracranial hemorrhage. In: Neurology
where prior research shows that out- Statistical expertise: Staiger, Kenny. of the Newborn. 5th ed. Philadelphia, PA: Saunders;
Obtained funding: Lake, Staiger, Horbar, Patrick, 2001.
comes are the worst.25 In addition, we Rogowski. 11. Kilbride HW, Wirtschafter DD, Powers RJ, Sheehan
excluded 20 network hospitals with- Administrative, technical, or material support: Lake, MB. Implementation of evidence-based potentially bet-
Cheung. ter practices to decrease nosocomial infections.
out inborn infants. Outborn infants may Study supervision: Lake. Pediatrics. 2003;111(4 pt 2):e519-e533.
acquire morbidities before admission, Conflict of Interest Disclosures: All authors have com- 12. McCourt M. At risk for infection: the very-low-
thus confounding the role of RNE sta- pleted and submitted the ICMJE Form for Disclosure birth-weight infant. J Perinat Neonatal Nurs. 1994;
of Potential Conflicts of Interest. Dr Lake received an 7(4):52-64.
tus in these outcomes. By restricting to honorarium for plenary remarks at the 2010 Ameri- 13. American Nurses Credentialing Center. Magnet
inborn infants, we excluded some free- can Nurses Credentialing Center Research Sympo- recognition program overview. http://www
sium. Dr Staiger holds an equity interest in ArborMet- .nursecredentialing.org/Magnet/ProgramOverview
standing children’s hospitals. Infec- ric Inc, a company that sells efficiency measurement .aspx. Accessed March 29, 2012.
tion and SIVH were not recorded for systems and consulting services to insurers and hos- 14. American Nurses Credentialing Center. Applica-
pitals. Dr Horbar is chief executive and scientific offi- tion Manual: Magnet Recognition Program. Silver
some infants who were transferred out. cer for the Vermont Oxford Network. No other dis- Spring, MD: American Nurses Credentialing Center;
However, transfer rates were low and closures were reported. 2011.
©2012 American Medical Association. All rights reserved. JAMA, April 25, 2012—Vol 307, No. 16 1715
Downloaded From: http://jamanetwork.com/ on 07/11/2017
NURSING EXCELLENCE RECOGNITION AND VLBW INFANT OUTCOMES
15. American Nurses Credentialing Center. Journey organizations with Magnet-recognized nursing services. mental and growth impairment among extremely
to Magnet excellence. http://www.nursecredentialing http://www.nursecredentialing.org/Magnet low-birth-weight infants with neonatal infection.
.org/MagnetJourney.aspx. Accessed July 30, 2011. /FindAMagnetFacility.aspx. Accessed March 29, 2012. JAMA. 2004;292(19):2357-2365.
16. Lake ET, Shang J, Klaus S, Dunton NE. Patient falls: 24. Rogowski JA, Horbar JD, Staiger DO, Kenny M, 33. Vohr BR, Wright LL, Poole WK, McDonald SA.
association with hospital Magnet status and nursing Carpenter J, Geppert J. Indirect vs direct hospital qual- Neurodevelopmental outcomes of extremely low birth
unit staffing. Res Nurs Health. 2010;33(5):413- ity indicators for very low-birth-weight infants. JAMA. weight infants ⬍32 weeks’ gestation between 1993
425. 2004;291(2):202-209. and 1998. Pediatrics. 2005;116(3):635-643.
17. Hickey P, Gauvreau K, Connor J, Sporing E, Jenkins 25. Phibbs CS, Baker LC, Caughey AB, Danielsen B, 34. Aiken LH, Smith HL, Lake ET. Lower Medicare mor-
K. The relationship of nurse staffing, skill mix, and Mag- Schmitt SK, Phibbs RH. Level and volume of neona- tality among a set of hospitals known for good nurs-
net recognition to institutional volume and mortality tal intensive care and mortality in very-low-birth- ing care. Med Care. 1994;32(8):771-787.
for congenital heart surgery. J Nurs Adm. 2010; weight infants. N Engl J Med. 2007;356(21):2165- 35. Institute of Medicine. Crossing the Quality Chasm:
40(5):226-232. 2175. A New Health System for the 21st Century. Wash-
18. Hamilton KES, Redshaw ME, Tarnow-Mordi W. 26. Chung J, Phibbs C, Boscardin W, et al. Examin- ington, DC: National Academy Press; 2001.
Nurse staffing in relation to risk-adjusted mortality in ing the effect of hospital-level factors on mortality of 36. Mitchell PH, Ferketich S, Jennings BM; Ameri-
neonatal care. Arch Dis Child Fetal Neonatal Ed. 2007; very low birth weight infants using multilevel modeling. can Academy of Nursing Expert Panel on Quality
92(2):F99-F103. J Perinatol. 2011;31(12):770-775. Health Care. Quality health outcomes model. Image
19. Grandi C, González A, Meritano J; Grupo Co- 27. American Hospital Association. AHA Annual Sur- J Nurs Sch. 1998;30(1):43-46.
laborativo Neocosur. Patient volume, medical and nurs- vey Database. 2008 ed. Chicago, IL: American Hos- 37. Institute of Medicine. Preterm Birth: Causes, Con-
ing staffing and its relationship with risk-adjusted out- pital Association; 2010. sequences, and Prevention. Washington, DC: Na-
comes of VLBW infants in 15 Neocosur neonatal 28. Efron B, Gong G. A leisurely look at the boot- tional Academies Press; 2006.
network NICUs. Arch Argent Pediatr. 2010;108 strap, the jackknife, and cross-validation. Am Stat. 38. March of Dimes. Towards Improving the Out-
(6):499-510. 1983;37:36-48. come of Pregnancy III: Enhancing Perinatal Health
20. Cimiotti JP, Haas J, Saiman L, Larson EL. Impact 29. Stata Corp. Stata Statistical Software: Release 10.1 Through Quality, Safety and Performance Initiatives.
of staffing on bloodstream infections in the neonatal [computer program]. College Station, TX: Stata Corp; White Plains, NY: March of Dimes; 2010.
intensive care unit. Arch Pediatr Adolesc Med. 2006; 2007. 39. Murphy J, Geisen E, Olmsted MG, et al. Meth-
160(8):832-836. 30. Medlock S, Ravelli ACJ, Tamminga P, Mol BWM, odology: US News & World Report Best Hospitals
21. Pollack MM, Koch MA; NIH–District of Colum- Abu-Hanna A. Prediction of mortality in very prema- 2011-12. July 19, 2011. http://static.usnews.com
bia Neonatal Network. Association of outcomes with ture infants: a systematic review of prediction models. /documents/health/best-hospitals-methodology
organizational characteristics of neonatal intensive care PLoS One. 2011;6(9):e23441. .pdf?s_cid=related-links:TOP. Accessed August 1,
units. Crit Care Med. 2003;31(6):1620-1629. 31. Stoll BJ, Hansen N, Fanaroff AA, et al. Late- 2011.
22. Papile LA, Burstein J, Burstein R, Koffler H. Inci- onset sepsis in very low birth weight neonates: the ex- 40. Leapfrog Group. The Leapfrog Group will pub-
dence and evolution of subependymal and intraven- perience of the NICHD Neonatal Research Network. licly report on nursing excellence: 2011 hospital rat-
tricular hemorrhage: a study of infants with birth Pediatrics. 2002;110(2 pt 1):285-291. ings will include Magnet status for the first time [press
weights less than 1500 gm. J Pediatr. 1978;92 32. Stoll BJ, Hansen NI, Adams-Chapman I, et al; Na- release]. July 27, 2011. http://www.leapfroggroup
(4):529-534. tional Institute of Child Health and Human Develop- .org/news/leapfrog_news/4801927. Accessed March
23. American Nurses Credentialing Center. Health care ment Neonatal Research Network. Neurodevelop- 29, 2012.
1716 JAMA, April 25, 2012—Vol 307, No. 16 ©2012 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/ on 07/11/2017
You might also like
- Congenital Malformations in The Newborn Population: A Population Study and Analysis of The Effect of Sex and PrematurityDocument6 pagesCongenital Malformations in The Newborn Population: A Population Study and Analysis of The Effect of Sex and PrematuritydentsavvyNo ratings yet
- Admission of Term Infants To The NicuDocument6 pagesAdmission of Term Infants To The NicucarlsonrenovatioNo ratings yet
- Common Problems in the Newborn Nursery: An Evidence and Case-based GuideFrom EverandCommon Problems in the Newborn Nursery: An Evidence and Case-based GuideGilbert I. MartinNo ratings yet
- Pediatrics 2012 Yee E298 304Document9 pagesPediatrics 2012 Yee E298 304Amber CarterNo ratings yet
- AripiDocument9 pagesAripiberthad33No ratings yet
- Knowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhanaDocument10 pagesKnowledge Level and Determinants of Neonatal Jaundice A Cross-Sectional Study in The Effutu Municipality of GhananicloverNo ratings yet
- Inter-Hospital Variations in Labor Induction and OutcomesDocument9 pagesInter-Hospital Variations in Labor Induction and OutcomesStéphanieNo ratings yet
- Pediatric Nasogastric Tube Placement and Verification: Best Practice Recommendations From The NOVEL Project: CONSENSUS RecommendationsDocument9 pagesPediatric Nasogastric Tube Placement and Verification: Best Practice Recommendations From The NOVEL Project: CONSENSUS RecommendationsDoraNo ratings yet
- Early Enteral Feeding and Nosocomial Sepsis in Very Low Birthweight InfantsDocument4 pagesEarly Enteral Feeding and Nosocomial Sepsis in Very Low Birthweight InfantsaripbudiboyNo ratings yet
- Wales 2004Document6 pagesWales 2004Subha ManivannanNo ratings yet
- Neonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkDocument14 pagesNeonatal Outcomes of Extremely Preterm Infants From The NICHD Neonatal Research NetworkKattia FloresNo ratings yet
- RCP y Resultados A Corto Plazo en Prematuros. JPedDocument8 pagesRCP y Resultados A Corto Plazo en Prematuros. JPedSheila Patricia Castro ErazoNo ratings yet
- Am J Perinatol. 2007 Jun24 (6) 373-6Document4 pagesAm J Perinatol. 2007 Jun24 (6) 373-6Ivan Osorio RuizNo ratings yet
- Less Is More Modern NeonatologyDocument11 pagesLess Is More Modern NeonatologyEN BUNo ratings yet
- Pneumonia and Pregnancy Outcomes: A Nationwide Population-Based StudyDocument7 pagesPneumonia and Pregnancy Outcomes: A Nationwide Population-Based StudyAdrin Mahmuddin HarahapNo ratings yet
- Agulnik 2016Document8 pagesAgulnik 2016Karma SetiyawanNo ratings yet
- Brue Antes AlteDocument12 pagesBrue Antes Altehacek357No ratings yet
- 2016 Relacion ANEMIA Con NEC y TransfusionesDocument9 pages2016 Relacion ANEMIA Con NEC y TransfusionesnadisjaviNo ratings yet
- Morfologi PlasentaDocument6 pagesMorfologi PlasentayueldiNo ratings yet
- JAMA. 2016 : in ReplyDocument3 pagesJAMA. 2016 : in Replydella psNo ratings yet
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- Diabetes in Children and Adolescents: A Guide to Diagnosis and ManagementFrom EverandDiabetes in Children and Adolescents: A Guide to Diagnosis and ManagementNo ratings yet
- Risk Factor For Sever Postpartum Hemorrhage A Case Control StudyDocument9 pagesRisk Factor For Sever Postpartum Hemorrhage A Case Control StudyAhmad SyaukatNo ratings yet
- Shankaran 2019Document11 pagesShankaran 2019Desmiyati AdoeNo ratings yet
- Skin Care For Pediatric2Document7 pagesSkin Care For Pediatric2Sri Nauli Dewi LubisNo ratings yet
- Predicting In-Hospital Length of Stay For Very-Low-Birth-Weight Preterm Infants Using Machine Learning TechniquesDocument8 pagesPredicting In-Hospital Length of Stay For Very-Low-Birth-Weight Preterm Infants Using Machine Learning TechniquesGabriel Ferreira MassonNo ratings yet
- Pediatrics 2002 Mortality in Low Birth Weight Infants According To Level of Neonatal Care at Hospital BirthDocument7 pagesPediatrics 2002 Mortality in Low Birth Weight Infants According To Level of Neonatal Care at Hospital Birthafrizal_deafzNo ratings yet
- Population Case-Control Study of Cerebral Palsy: Neonatal Predictors For Low-Risk Term SingletonsDocument9 pagesPopulation Case-Control Study of Cerebral Palsy: Neonatal Predictors For Low-Risk Term SingletonsFirdaus Septhy ArdhyanNo ratings yet
- 114 How Parents To Technology Dependent Children Experience The Transition From A Hospital Stay To Professional Home Care NursingDocument1 page114 How Parents To Technology Dependent Children Experience The Transition From A Hospital Stay To Professional Home Care NursingDaniella AwurumibeNo ratings yet
- Jeng2011 PDFDocument5 pagesJeng2011 PDFMeita AskudeNo ratings yet
- Management of The Febrile Young Infant: Cme R ADocument6 pagesManagement of The Febrile Young Infant: Cme R AsarabisimonaNo ratings yet
- AAP Guia Practica Liquidos IVDocument12 pagesAAP Guia Practica Liquidos IVMiroslaba Avila DiazNo ratings yet
- Medical and Obstetric Outcomes Among Preg Wpman With Cpngenital Hart DseeeDocument9 pagesMedical and Obstetric Outcomes Among Preg Wpman With Cpngenital Hart DseeeZahed UllahNo ratings yet
- JurnalDocument6 pagesJurnalDevi DaryaningsihNo ratings yet
- PIIS1472648318300427Document11 pagesPIIS1472648318300427Thanh Binh TranNo ratings yet
- 1 s2.0 S0022347621002900 MainDocument10 pages1 s2.0 S0022347621002900 MainFarah PramestyNo ratings yet
- Does This Child Have Appendicitis?: The Rational Clinical ExaminationDocument14 pagesDoes This Child Have Appendicitis?: The Rational Clinical ExaminationTrys RobledoNo ratings yet
- Zwi Ers 2016Document26 pagesZwi Ers 2016Medicpianist PVNo ratings yet
- Anemia de PrematDocument7 pagesAnemia de Prematmedibase12No ratings yet
- Pediatrics JournalDocument9 pagesPediatrics JournalDokter KarisNo ratings yet
- CDC 84627 DS1Document15 pagesCDC 84627 DS1Thu HoaiNo ratings yet
- Contemporary Cesarean Delivery Practice in The United StatesDocument17 pagesContemporary Cesarean Delivery Practice in The United StatesdedypurnamaNo ratings yet
- Unintended Pregnancy, Prenatal Care, Newborn Outcomes, and Breastfeeding in Women With EpilepsyDocument10 pagesUnintended Pregnancy, Prenatal Care, Newborn Outcomes, and Breastfeeding in Women With EpilepsyasfwegereNo ratings yet
- Articol 1Document7 pagesArticol 1nistor97No ratings yet
- Pi Is 0002937815011205Document9 pagesPi Is 0002937815011205Oki WihardiyantoNo ratings yet
- Intravenous Immunoglobulin in Neonates With RhesusDocument9 pagesIntravenous Immunoglobulin in Neonates With RhesusGabriel BuftiaNo ratings yet
- Piis0002937816321706 PDFDocument8 pagesPiis0002937816321706 PDFObgyn Unsrat2017No ratings yet
- Analysing Differences in Clinical Outcomes Between HospitalsDocument6 pagesAnalysing Differences in Clinical Outcomes Between Hospitalsujangketul62No ratings yet
- Bjo12636 PDFDocument9 pagesBjo12636 PDFLuphly TaluvtaNo ratings yet
- 18-American Journal of Reproductive Immunology 2019 SistiDocument5 pages18-American Journal of Reproductive Immunology 2019 SistiSara PaccosiNo ratings yet
- The NeoUpdates - DecDocument7 pagesThe NeoUpdates - DecDr Satish MishraNo ratings yet
- IUFDDocument12 pagesIUFDPitut T. PuspitasariNo ratings yet
- Incidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyDocument7 pagesIncidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyGusBlomkvistSomocurioNo ratings yet
- 33873-Article Text-121761-1-10-20170831Document6 pages33873-Article Text-121761-1-10-20170831AnggaNo ratings yet
- Maternal, Labor, Delivery, and Perinatal Outcomes Associated With Placental Abruption: A Systematic ReviewDocument23 pagesMaternal, Labor, Delivery, and Perinatal Outcomes Associated With Placental Abruption: A Systematic ReviewasfwegereNo ratings yet
- App Acog 2012Document10 pagesApp Acog 2012jimedureyNo ratings yet
- Parto en Casa Mayor MortalidadDocument12 pagesParto en Casa Mayor MortalidadDaniel Salazar OsorioNo ratings yet
- Piis002234760700594x PDFDocument1 pagePiis002234760700594x PDFraisyaNo ratings yet
- Smoking and CHDDocument19 pagesSmoking and CHDAnonymous NeRC5JYiSNo ratings yet
- JAMA Ophthalmology Volume Issue 2018 (Doi 10.1001 - Jamaophthalmol.2018.2753) Binenbaum, Gil Bell, Edward F. Donohue, Pamela Quinn, Graham - Development of Modified Screening Criteria For Retinop PDFDocument7 pagesJAMA Ophthalmology Volume Issue 2018 (Doi 10.1001 - Jamaophthalmol.2018.2753) Binenbaum, Gil Bell, Edward F. Donohue, Pamela Quinn, Graham - Development of Modified Screening Criteria For Retinop PDFKarthik CNo ratings yet
- Rundown Character BuildingDocument1 pageRundown Character BuildingFifiNo ratings yet
- MXQ 005Document12 pagesMXQ 005FifiNo ratings yet
- Young Risk of LBWDocument20 pagesYoung Risk of LBWFifiNo ratings yet
- Low Birth in South AsiaDocument19 pagesLow Birth in South AsiaFifiNo ratings yet
- Cost of LBWDocument75 pagesCost of LBWFifiNo ratings yet
- BarretDocument14 pagesBarretFifiNo ratings yet
- United Board Faculty Scholarship Program: 2021 - 2022 Application AnnouncementDocument2 pagesUnited Board Faculty Scholarship Program: 2021 - 2022 Application AnnouncementFifiNo ratings yet
- Nwogbe Love: Career ObjectivesDocument3 pagesNwogbe Love: Career ObjectivesArthur PentaxNo ratings yet
- Hospital Renovation Project Using PFI: October, 2016 Tsukuba UniversityDocument13 pagesHospital Renovation Project Using PFI: October, 2016 Tsukuba UniversityMike OptimusNo ratings yet
- An Internship Report OnDocument40 pagesAn Internship Report OnRaunak Thapa100% (6)
- Treatment of Distal Humerus FracturedDocument10 pagesTreatment of Distal Humerus Fracturedauliya ningsihNo ratings yet
- Glossary Mental Terms-FarsiDocument77 pagesGlossary Mental Terms-FarsiRahatullah AlamyarNo ratings yet
- Incentive SpirometryDocument3 pagesIncentive SpirometryNursidar Pascual MukattilNo ratings yet
- Soal UTS Bahasa Inggris Kelas 3 SD Semester 1 - (Nesabamedia - Com)Document9 pagesSoal UTS Bahasa Inggris Kelas 3 SD Semester 1 - (Nesabamedia - Com)Boboko NasiNo ratings yet
- Physical TherapyDocument123 pagesPhysical TherapyHari PrasadNo ratings yet
- Mac Peds Survival GuideDocument206 pagesMac Peds Survival GuideKatheryn100% (1)
- MAP Proposal 1.0Document4 pagesMAP Proposal 1.0Vaishnavi SrivathsanNo ratings yet
- Soul Surfer Movie Guide 1Document1 pageSoul Surfer Movie Guide 1Nayla Figueroa Etchelet100% (1)
- Forensic PsikiatriDocument13 pagesForensic PsikiatriLira Riana AkbarNo ratings yet
- NewsflashDocument109 pagesNewsflashTelmaNo ratings yet
- Physicians and Hospitals List Islamabad 2016Document11 pagesPhysicians and Hospitals List Islamabad 2016Zawar AliNo ratings yet
- An Intensive Review and Update of Neonatal-Perinatal MedicineDocument16 pagesAn Intensive Review and Update of Neonatal-Perinatal MedicinemaxamaxaNo ratings yet
- Practice Questions Chapter 7 & 13Document10 pagesPractice Questions Chapter 7 & 13jenniferhughesNo ratings yet
- Medical Reimbursement PDFDocument3 pagesMedical Reimbursement PDFOrlando WilliamsNo ratings yet
- Plaintiff'S Class Action Complaint Case SummaryDocument24 pagesPlaintiff'S Class Action Complaint Case SummaryCBS 11 News100% (1)
- Volume 15, Number 1 January 2011Document233 pagesVolume 15, Number 1 January 2011Nicolai BabaliciNo ratings yet
- PostFRCRFellowshipDocument16 pagesPostFRCRFellowshipMD Luthfy LubisNo ratings yet
- Degroat RN ResumeDocument1 pageDegroat RN Resumeapi-363089889No ratings yet
- Diamond Brochure PDFDocument3 pagesDiamond Brochure PDFSumit SinghNo ratings yet
- Nurse Guide April09Document136 pagesNurse Guide April09api-256209231No ratings yet
- Geremew OugaDocument71 pagesGeremew OugaDemisachew TenaNo ratings yet
- ResumeDocument2 pagesResumewella goNo ratings yet
- Golding BirdDocument21 pagesGolding BirdalecssterNo ratings yet
- Target BeneficiariesDocument6 pagesTarget BeneficiariesTommy SoleraNo ratings yet
- Carroll Resume RevisedDocument2 pagesCarroll Resume Revisedapi-652166364No ratings yet
- Error Prevention ToolsDocument2 pagesError Prevention Toolsedward2100% (1)
- 312 September 2017Document10 pages312 September 2017Cornwall and Isles of Scilly LMCNo ratings yet