Professional Documents
Culture Documents
CCPH Presentation 1
Uploaded by
api-561982212Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CCPH Presentation 1
Uploaded by
api-561982212Copyright:
Available Formats
Region V Public Health Training Center 5/15/2019
Culturally Competent Public
Health Practice for Deaf and
Hard of Hearing Populations
Communication Access Center for
the Deaf and Hard of Hearing
Diana McKittrick
dmckittrick@cacdhh.org
810-250-7010
Statistics
• About 2 to 3 out of every 1,000 children in the United States are born with a detectable level of
hearing loss in one or both ears.
• More than 90 percent of deaf children are born to hearing parents.
• 70 percent of parents who have deaf children cannot communicate with their deaf child.
• Approximately 15% of American adults (37.5 million) aged 18 and over report some trouble hearing.
• Among adults aged 20-69, the overall annual prevalence of hearing loss dropped slightly from 16
percent (28.0 million) in the 1999-2004 period to 14 percent (27.7 million) in the 2011–2012 period.
• Age is the strongest predictor of hearing loss among adults aged 20-69, with the greatest amount of
hearing loss in the 60 to 69 age group.
• Men are almost twice as likely as women to have hearing loss among adults aged 20-69.
• One in eight people in the United States (13 percent, or 30 million) aged 12 years or older has hearing
loss in both ears, based on standard hearing examinations.
• About 2 percent of adults aged 45 to 54 have disabling hearing loss. The rate increases to 8.5 percent
for adults aged 55 to 64. Nearly 25 percent of those aged 65 to 74 and 50 percent of those who are
75 and older have disabling hearing loss.
• Roughly 10 percent of the U.S. adult population, or about 25 million Americans, has experienced
tinnitus lasting at least five minutes in the past year.
• About 28.8 million U.S. adults could benefit from using hearing aids.
• Among adults aged 70 and older with hearing loss who could benefit from hearing aids, fewer than
one in three (30 percent) has ever used them. Even fewer adults aged 20 to 69 (approximately 16
percent) who could benefit from wearing hearing aids have ever used them.
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 1
Region V Public Health Training Center 5/15/2019
Reactions of people involved in a
typical medical related interaction
• Reaction of the Deaf/HH/DB person
attempting to obtain health care services
• Reaction of front line medical personnel
when approached by Deaf/HH individuals
• Reaction of Physicians and Nurses providing
health care services
Labels We See: We Use:
• Deaf • Deaf
• Deaf-Mute
• Hard of Hearing
• Deaf and Dumb
• Hearing
• Hard of Hearing
• Almost Hearing
• Hearing Challenged
• Dummy
• Mute
• Hearing Impaired
• Speech Impaired
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 2
Region V Public Health Training Center 5/15/2019
What is the difference?
Deaf
The individual is part of the deaf community, uses
American Sign Language and embraces the
concept that deafness is normal way of life.
deaf
The individual is not part of the deaf
community. Perceives self as flawed and need
to be fixed. Views self as disabled.
Different groups within the
Deaf Community Influences
Communication Approaches
• Generational Deaf
• Deaf who attended state residential school for the deaf
• Deaf with hearing parents that have not learned to sign or can sign
• Ethnic groups- Black Deaf, Asian Deaf, Hispanic Deaf, etc…
• Hard of Hearing
• Oral Deaf
• LGBTQ
• Senior Citizens
• CODA/KODA
• Late Deafened
• Cochlear Implanted Deaf
• Limited Language Deaf
• Deaf with other disabilities
• DeafBlind
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 3
Region V Public Health Training Center 5/15/2019
Cultural Tendencies
• Starts conversation from general to specific
• Long good-byes
• Always let people know where you are going
• Hugging/Touching
• Blunt/Straight talk
• Visual noise
• Sharing information
• Whispers
Deaf People Can:
Get married
Can drive
Raise hearing children
Can work/have jobs/careers
Handle their own finances
Have a social life
Make phone calls to hearing friends,
family members or businesses
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 4
Region V Public Health Training Center 5/15/2019
Barriers that Deaf
Community face
• Inadequate education
• Low reading skills
• Low health literacy knowledge
• Service providers not willing to provide
effective communication
• Discrimination
• Audism
• Paternalism
Language and
Communication
• American Sign Language (ASL) is the
preferred language used in North America
• ASL is not universal
• ASL has regional variations
• ASL is a living language and
additions/changes occur over time
• ASL is a visual language with its own
syntax and grammar
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 5
Region V Public Health Training Center 5/15/2019
Different Types of Sign
Language Modalities
Manually Coded English (MCE)
• Created by hearing people to make English visible
for students to improve their reading and writing
skills
• It is not a language
• Different types of MCE are: SEE, SEE1, LOVE,
CASE, Rochester Method
• PSE - Pidgin Sign Language/Contact Sign
Language
• Rochester method- all fingerspelling except for
sign “AND”
Degree of competency in
use of English and ASL
• Balanced bilingual - equally competent in
English and ASL
• ASL Dominant - has skills in both but ASL use
is preferred and stronger than English
• English Dominant - has skills in both but
English word order is preferred and
proficient in use of written English
• Minimal Language - does not have skills in
English or ASL - illiterate
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 6
Region V Public Health Training Center 5/15/2019
Comparison of English and ASL
ASL: English:
Woman leave Did the woman
book? leave book?
ASL: English:
Woman leave The woman didn’t
book (NEG) leave her book.
ASL: English:
Woman leave The woman left
book (NODDING) her book.
Translation Activity
Limited Language User
• Earl John HOUSE WHITE LOOK
• Earl John BOOK PLEASE OK?
• M-A-R-Y FRIDAY 6:00 PARTY YES OK?
• SCHOOL FINISH Earl John GO GO GO YES.
• TALK CURVE CURVE ALL TIME NOT STRAIGHT
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 7
Region V Public Health Training Center 5/15/2019
Communication Methods
Used by Service Providers
• Writing back and forth
• Lipreading
• Using an “signer” instead of Certified
Interpreter
• Using family to interpret
• Waiting until the last minute to call for sign
language interpreter
• Video Remote Interpreting (VRI)
• Onsite Certified Interpreter
Lack of Effective
Communication Access
Communication difficulties
Altered Health care utilization
Misunderstanding about medical condition
Misunderstanding of treatment process
Misunderstanding of medication use
Sense of unease by both parties
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 8
Region V Public Health Training Center 5/15/2019
Risk to the Deaf/HH/DB
Individual
• Error in understanding all symptoms
• Error in decision on diagnosis
• Error in development of appropriate
treatment plan
• Non compliance of treatment plan
• Choice of making informed decision
about health care is compromised
Potential Problems
• Possible return to emergency room/primary
care provider for same problem.
• Non compliance with treatment plan
• Cost of repeat visits
• Time wasted
• Patient and doctor relationship and trust
issues
• Possible lawsuit for failure to provide
accommodation
ADA- Americans with Disabilities Act
Section 504 Rehabilitation Act
PA204 amended 2007 (Deaf Person’s Interpreter Act)
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 9
Region V Public Health Training Center 5/15/2019
Communication
Strategies Typically Used
• Sign Language Interpreter on site
• Video Remote Interpreting
• Writing back and forth
• Speechreading/lipreading
• Visual drawings/pictures
Michigan Interpreters
PA 204 amended 2007
(known as Deaf Individual
Interpreter Act)
• Must be registered with LARA
• Must Have Interpreter Certification
• Must have Medical Endorsement to
do medical/mental health
interpreting assignments.
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 10
Region V Public Health Training Center 5/15/2019
How Do You Know?
• Ask to see Identification card
issued by State of Michigan
which has their credentials and
endorsements
• Use Michigan Online
Interpreter Directory
• Use of waivers - typically
indicate underqualified
interpreter
• Responses to questions not
make sense
Do
• Talk directly to the Deaf/HH/DB Individual.
• Talk at a normal pace
• Realize that head nodding does not mean
agreement or understanding of what was
conveyed
• Realize that the interpreter may ask for
clarification to ensure full understanding of
what was said
• Maintain eye contact throughout the
interaction
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 11
Region V Public Health Training Center 5/15/2019
Don’t
• Ask the interpreter not to interpret what you
said
• Say “Tell him” or “Tell her”
• Ask the interpreter to give information about
the deaf/hh individual.
• Continue if you see that communication is
not effective between the interpreter and
deaf individual - How do you know?
Goal
• Positive experience for the deaf/hh/db
patient and family
• Appropriate medical diagnosis and
treatment given
• Better compliance with treatment plan
• Reduce return visits for the same problem
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 12
Region V Public Health Training Center 5/15/2019
Questions???
May 2019 Culturally Competent Public Health
Practice for Deaf & Hard of Hearing 13
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Establishment of The New Testament ChurchDocument7 pagesThe Establishment of The New Testament ChurchTytler Samuel Abiodun OlayinkaNo ratings yet
- Everyday Bias Identifying and Navigating Unconscious JudgmentsDocument2 pagesEveryday Bias Identifying and Navigating Unconscious Judgmentsapi-561982212No ratings yet
- Apocrypha Are Works, Usually Written Works, That Are of Unknown Authorship, or of DoubtfulDocument4 pagesApocrypha Are Works, Usually Written Works, That Are of Unknown Authorship, or of DoubtfulJas PalNo ratings yet
- Vendor PO & NPO Invoice Process Through VIM (Vendor Invoice Management) Two Type of Invoice ProcessDocument15 pagesVendor PO & NPO Invoice Process Through VIM (Vendor Invoice Management) Two Type of Invoice Processdivu_dhawan12100% (1)
- Software Architecture PatternsDocument54 pagesSoftware Architecture Patternsvenkata100% (1)
- English Prepositions 2Document22 pagesEnglish Prepositions 2Marcela Rodriguez0% (1)
- Class 10 Mental Ability Competitive Exams Book Good QuestionsDocument160 pagesClass 10 Mental Ability Competitive Exams Book Good Questionsrajeshsaran21No ratings yet
- Mini Project ReportDocument19 pagesMini Project Reportashim01100% (1)
- Introduction To NodejsDocument49 pagesIntroduction To NodejssiraleemNo ratings yet
- Sample Scraper Email PhoneDocument162 pagesSample Scraper Email PhoneNaveen PrabhuNo ratings yet
- Idaho Department of Health and WelfareDocument2 pagesIdaho Department of Health and Welfareapi-561982212No ratings yet
- Innova Foundation and United Way of North IdahoDocument3 pagesInnova Foundation and United Way of North Idahoapi-561982212No ratings yet
- Head Start Ted Talk 1Document1 pageHead Start Ted Talk 1api-561982212No ratings yet
- 25 Things All Great Communicators DoDocument3 pages25 Things All Great Communicators Doapi-561982212No ratings yet
- Competency Assessment Tier1 2014 PreDocument20 pagesCompetency Assessment Tier1 2014 Preapi-561982212No ratings yet
- Ks3 English Homework SheetsDocument6 pagesKs3 English Homework Sheetsafnahqfxahyjkj100% (1)
- OopTh Ass 01Document7 pagesOopTh Ass 01Saim KhanNo ratings yet
- Health Education Midterms ReviewerDocument5 pagesHealth Education Midterms ReviewerChihaya AyaseNo ratings yet
- Alasdair MacIntyre On Thomism and The STDocument24 pagesAlasdair MacIntyre On Thomism and The STHonny Pigai ChannelNo ratings yet
- Log Cat 1669029540894Document11 pagesLog Cat 1669029540894Mioratiana RandrianarisoaNo ratings yet
- The Project Gutenberg Ebook of Colloquies of ErasmusDocument415 pagesThe Project Gutenberg Ebook of Colloquies of ErasmusJuan RulfoNo ratings yet
- Cambridge International AS & A Level: Biology 9700/22 October/November 2022Document20 pagesCambridge International AS & A Level: Biology 9700/22 October/November 2022Milinda De SilvaNo ratings yet
- Clark & PaivioDocument62 pagesClark & PaivioGeléias Artesanais Fraga Delfino & KunzNo ratings yet
- Kathrin Seidl Gomez - The Creativity of DisplacementDocument390 pagesKathrin Seidl Gomez - The Creativity of DisplacementSantiago Ospina CelisNo ratings yet
- Philippine External Relations With Southeast AsiaDocument26 pagesPhilippine External Relations With Southeast AsiaKaren Gail JavierNo ratings yet
- Prueba de InglesDocument3 pagesPrueba de InglesAnyaly OSNo ratings yet
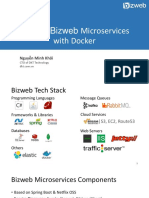
- Building Bizweb Microservices with Docker: Nguyễn Minh KhôiDocument25 pagesBuilding Bizweb Microservices with Docker: Nguyễn Minh KhôinguoinhenvnNo ratings yet
- Gang of Four Java Design Patterns Mock ExamDocument78 pagesGang of Four Java Design Patterns Mock ExamdesignpatternsNo ratings yet
- Ibn Abi Dunya and Yaqin - LibrandeDocument39 pagesIbn Abi Dunya and Yaqin - LibrandeAbul HasanNo ratings yet
- Applied Electronics Lab ReportDocument26 pagesApplied Electronics Lab ReportOdoch HerbertNo ratings yet
- Celebrations: Lesson B Festivals and HolidaysDocument55 pagesCelebrations: Lesson B Festivals and HolidaysAlessa GV.No ratings yet
- How To Embed A PDF File in An Excel WorksheetDocument7 pagesHow To Embed A PDF File in An Excel WorksheetNimish MadananNo ratings yet
- Farmer, ProfessionalismDocument11 pagesFarmer, ProfessionalismPatricia María Guillén CuamatziNo ratings yet
- Unit 1 DsaDocument55 pagesUnit 1 DsaRavishankar BhaganagareNo ratings yet
- Meaning and Circular Definitions (F. Orilia)Document16 pagesMeaning and Circular Definitions (F. Orilia)Daniel Rojas UNo ratings yet
- An Equivalent Pi Network Model For PDFDocument8 pagesAn Equivalent Pi Network Model For PDFWilson G SpNo ratings yet