Professional Documents
Culture Documents
Paulsen 2014
Uploaded by
MOHAMMAD JOFA RACHMAN PUTERACopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paulsen 2014
Uploaded by
MOHAMMAD JOFA RACHMAN PUTERACopyright:
Available Formats
VOLUME 32 䡠 NUMBER 29 䡠 OCTOBER 10 2014
JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Efficacy of Methylprednisolone on Pain, Fatigue, and Appetite
Loss in Patients With Advanced Cancer Using Opioids:
A Randomized, Placebo-Controlled, Double-Blind Trial
Ørnulf Paulsen, Pål Klepstad, Jan Henrik Rosland, Nina Aass, Eva Albert, Peter Fayers, and Stein Kaasa
See accompanying editorial on page 3210; listen to the podcast by Drs Vardy and Agar at
Ørnulf Paulsen, Telemark Hospital www.jco.org/podcasts
Trust, Skien; Ørnulf Paulsen, Pål Klep-
stad, Peter Fayers, and Stein Kaasa, A B S T R A C T
Norwegian University of Science and
Technology; Pål Klepstad and Stein
Purpose
Kaasa, St Olavs Hospital, Trondheim
Corticosteroids are frequently used in cancer pain management despite limited evidence. This
University Hospital, Trondheim; Jan
Henrik Rosland, Haraldsplass Deacon-
study compares the analgesic efficacy of corticosteroid therapy with placebo.
ess Hospital and University of Bergen,
Bergen; Nina Aass, Oslo University
Patients and Methods
Hospital and University of Oslo, Oslo;
Adult patients with cancer receiving opioids with average pain intensity ⱖ 4 (numeric rating scale
Eva Albert, Sørlandet Hospital Kris- [NRS], 0 to 10) in the last 24 hours were eligible. Patients were randomly assigned to methylpred-
tiansand, Kristiansand, Norway; and nisolone (MP) 16 mg twice daily or placebo (PL) for 7 days. Primary outcome was average pain
Peter Fayers, University of Aberdeen, intensity measured at day 7 (NRS, 0 to 10); secondary outcomes were analgesic consumption (oral
Aberdeen, United Kingdom. morphine equivalents), fatigue and appetite loss (European Organisation for Research and Treatment
Published online ahead of print at of Cancer–Quality of Life Questionnaire C30, 0 to 100), and patient satisfaction (NRS, 0 to 10).
www.jco.org on July 7, 2014.
Results
Supported by unrestricted grants from
A total of 592 patients were screened; 50 were randomly assigned, and 47 were analyzed. Baseline opioid
the Telemark Hospital Trust and the
South-Eastern Norway Regional Health
level was 269.9 mg in the MP arm and 160.4 mg in the PL arm. At day-7 evaluation, there was no difference
Authority. between the groups in pain intensity (MP, 3.60 v PL, 3.68; P ⫽ .88) or relative analgesic consumption (MP,
1.19 v PL, 1.20; P ⫽ .95). Clinically and statistically significant improvements were found in fatigue (⫺17 v
Presented in abstract form and orally at
the 13th World Congress of the Euro-
3 points; P .003), appetite loss (⫺24 v 2 points; P ⫽ .003), and patient satisfaction (5.4 v 2.0 points; P ⫽ .001)
pean Association for Palliative Care, in favor of the MP compared with the PL group, respectively. There were no differences in adverse effects
Prague, Czech Republic, May 30-June between the groups.
2, 2013, and as a poster at the 2013
European Cancer Congress, Amster- Conclusion
dam, the Netherlands, September MP 32 mg daily did not provide additional analgesia in patients with cancer receiving opioids, but
28-October 1, 2013. it improved fatigue, appetite loss, and patient satisfaction. Clinical benefit beyond a short-term
The study sponsors had no role in the effect must be examined in a future study.
planning of the study, study design,
collection of data, analysis or interpreta- J Clin Oncol 32:3221-3228. © 2014 by American Society of Clinical Oncology
tion of data, writing of the report, or deci-
sion to submit the report for publication.
the adjuvant pain medications, according to the
Terms in blue are defined in the glos- INTRODUCTION
sary, found at the end of this article
treatment guidelines.4-7
and online at www.jco.org. Pain is a prevalent symptom in patients with can- Inflammation is a significant pain-modulating
Authors’ disclosures of potential conflicts cer,1 and providing pain relief is a challenge. Cancer factor. Proinflammatory cytokines and chemo-
of interest and author contributions are pain is complex, involving inflammatory, neuro- kines can directly modulate neuronal activity in
found at the end of this article.
pathic, ischemic, and compression mechanisms.2 both the peripheral and CNSs.8 Glia cells play a
Clinical trial information: NCT00676936;
Pain may be caused by a mixture of these mecha- major role in pain regulation, in part by releasing
EudraCT 2007-005617-19.
nisms in the individual patient, occurring at multi- proinflammatory cytokines.9 Corticosteroids are
Corresponding author: Ørnulf Paulsen,
MD, Telemark Hospital Trust, Palliative
ple sites and changing over time.2 potentanti-inflammatorydrugs,inhibitarangeofpro-
Care Unit, Ulefossveien, N-3710 Skien, Careful assessment of pain and titration of inflammatory molecules,10 and are recommended
Norway; e-mail: ornulf.paulsen@sthf.no. nonopioid and opioid analgesics comprise the basis therapy as an adjunct for postoperative pain.11 In
© 2014 by American Society of Clinical of cancer pain treatment. In addition, the WHO and two randomized trials, analgesic effect in patients
Oncology
European Association for Palliative Care pain man- with cancer was reported.12,13 Corticosteroids can
0732-183X/14/3229w-3221w/$20.00
agement recommendations state that adjuvant pain also mediate pain relief by reducing tumor-related
DOI: 10.1200/JCO.2013.54.3926 medications should be considered at each step of the edema in brain metastases14 or by directly reducing
WHO analgesic ladder.3 Corticosteroids are one of tumor burden (eg, in prostate cancer).15
© 2014 by American Society of Clinical Oncology 3221
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Paulsen et al
Corticosteroids are used in a large proportion of patients with metastases. Production of study drugs was performed at the hospital pharmacy
cancer pain. A European survey of 3,030 patients admitted to palliative at the Telemark Hospital Trust. Randomization was blinded for all parties
until the completion of data collection.
care programs showed that 39% used corticosteroids.1 A Swedish
survey showed that 50% of patients with cancer in palliative care Intervention
received corticosteroids, and pain was the indication for treatment in After baseline assessment, patients received identical-looking capsules of
the study drug containing either methylprednisolone 16 mg or placebo twice
25% of the cases.16 However, in a recently published systematic liter- daily for 7 days. Patients were contacted daily by a study nurse during the
ature review, we found little evidence for an analgesic effect of corti- treatment period to ensure compliance with the protocol.
costeroids in the treatment of cancer pain.17 This review calls into
Instruments
question the widespread use of corticosteroids for cancer pain.17 Medical and sociodemographic data. Patient demographics, medica-
The most common indications for starting corticosteroids in the tions, clinical characteristics, and pain categories, as judged by clinical evalua-
Swedish survey were appetite loss (37%), fatigue (36%), and poor tion, were recorded at baseline (Table 1). Daily analgesic consumption, which
well-being (33%).16 An expert working group of the European Asso- was a secondary outcome in the trial, was recorded in a diary and converted to
oral morphine equivalents.20
ciation for Palliative Care stated that steroids might be effective in Symptom assessment. Primary end point was average pain intensity
relieving fatigue for a short period of time, but the documentation was (NRS, 0 [no pain] to 10 [worst imaginable pain]), as measured by the Brief
weak.18 A systematic review of the treatment of cancer-associated Pain Inventory21 at day 7. Secondary outcomes were daily pain intensity at rest
anorexia and weight loss reported evidence to support the use of measured by the Edmonton Symptom Assessment System (NRS, 0 to 10),
corticosteroids in short courses as an appetite stimulant.19 reported as area under the curve22; change in fatigue and appetite loss from
Against this background, we performed a randomized controlled
trial with the primary aim of comparing the analgesic effects of oral
methylprednisolone 32 mg with placebo administrated for 7 days in Table 1. Patient Demographic and Clinical Characteristics at Inclusion (N ⫽ 49)
patients with cancer pain using opioids. Secondary aims were to eval- Methylprednisolone Placebo
(n ⫽ 26) (n ⫽ 23)
uate the effects of corticosteroids regarding fatigue, appetite loss, sat-
isfaction with treatment, and tolerance of this medication. Characteristic No. % No. %
Sex
Female 13 11
PATIENTS AND METHODS Male 13 12
Age, years
Mean 62.5 66.0
Study Design
95% CI 59.0 to 65.9 60.8 to 71.2
The study was a randomized, placebo-controlled, double-blind, parallel-
Karnofsky score (0 to 100)
group, multicenter phase III trial of oral corticosteroids in patients with cancer
Mean 66.4 65.7
experiencing pain. The trial was conducted according to Good Clinical Prac-
95% CI 60.8 to 72.2 59.7 to 71.6
tice guidelines, monitored independently by staff members from Oslo Univer-
Cancer diagnosis
sity Hospital, and registered in ClinicalTrial.gov on May 8, 2008. The study was
Breast 1 4 1 5
approved by the Regional Committee for Medical Research Ethics and Nor-
Prostate 3 12 3 14
wegian Directorate of Health. The procedures were conducted in accordance
GI 6 23 5 23
with the Declaration of Helsinki, as revised in 1983. The technical appendix,
Lung 6 23 5 23
statistical code, and complete anonymized data set are available from the
Gynecologic 5 19 5 23
corresponding author.
Other 7 27 4 18
Patients Metastasis
Patients with cancer, age ⱖ 18 years with average pain ⱖ 4 (numeric No 1 4 1 5
rating scale [NRS], 0 to 10) in the last 24 hours, with ⬎ 4 weeks expected Liver 11 42 6 27
survival and receiving an opioid for moderate or severe cancer pain, were CNS 2 8 0 0
eligible for the study. Exclusion criteria were as follows: excruciating pain Bone 9 35 6 27
(average pain NRS ⱖ 8 in last 24 hours), use of corticosteroids in the last 4 Lung 4 16 3 14
weeks, diabetes mellitus, peptic ulcer disease, concurrent medication with Other 15 58 18 82
nonsteroidal anti-inflammatory drugs, radiotherapy or systemic cancer treat- Mini Mental State Examination score
ment started ⬍ 4 weeks before entering the study or planned to start within the Mean 27.1 27.0
study period, spinal cord compression or need of bone surgery, and severe Concomitant disease
cognitive impairment. No changes in the current scheduled opioid medication Total 16 62 13 59
were allowed for the last 48 hours before inclusion or throughout the study Cardiac 4 16 4 18
period. Patients could use additional opioid for breakthrough pain. In- and Vascular 5 19 8 36
outpatients were screened for participation at five palliative care units and Lung 3 12 4 18
outpatient oncology services in Norway: Telemark Hospital, Haraldsplass GI/hepatic 4 16 1 5
Deaconess Hospital, Sørlandet Hospital, St Olav’s University Hospital, and Other 8 31 10 43
Oslo University Hospital. Written informed consent was obtained before any Ongoing cancer treatment
study-related procedures were performed. Radiotherapy 0 0 0 0
Chemotherapy 4 16 3 14
Randomization and Masking Hormonal therapy 3 12 3 14
Computerized randomization was provided by Norwegian University of None 19 73 17 77
Science and Technology by personnel not otherwise involved in the study.
Randomization was stratified for study center and pain related to verified bone
3222 © 2014 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Methylprednisolone RCT for Cancer Pain, Fatigue, and Appetite Loss
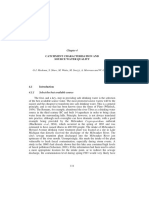
Assessed for eligibility
(N = 592)
Not eligible (n = 542)
Not meeting inclusion criteria (n = 60)
Declined to participate (n = 13)
Exclusion criteria (n = 462)
Receiving corticosteroids (n = 169)
Systemic cancer treatment (n = 125)
Pain ≥ 8 (n = 33)
Opioid dose change last 48 hours (n = 19)
Diabetes mellitus (n = 30)
Cognitive impairment (n = 11)
Other exclusion criteria (n = 75)
Other reasons (n = 7)
Randomly allocated
(n = 50)
Allocated to methylprednisolone (n = 26) Allocated to placebo (n = 24)
Received methylprednisolone (n = 26) Received placebo (n = 23)
Did not receive methylprednisolone (n = 0) Did not receive placebo (n = 1)
(patient withdrew consent before any study
procedures were done)
Lost to follow-up (n = 0) Lost to follow-up (n = 0)
Discontinued methylprednisolone (n = 1) Discontinued placebo (n = 1)
(SAE, withdrawn day 5 as a result of malignant (SAE, patient died day 4 as a result of
bowel obstruction) disease progression)
Analyzed (n = 25) Analyzed (n = 22)
Excluded from analysis (n = 0) Excluded from analysis (n = 0)
(1 patient SAE, withdrawn day 5, received
methylprednisolone, kept in analysis)
Fig 1. CONSORT flow diagram. SAE, serious adverse effect.
baseline to day 7, both measured by the European Organisation for Research SPSS statistical software (versions 15.0 and 19.0; SPSS, Chicago, IL) was used
and Treatment of Cancer–Quality of Life Questionnaire C3023; and overall for all statistical analyses. Statistical analyses were performed according to
satisfaction with the intervention (NRS, 0 [no benefit] to 10 [major benefit]) intention-to-treat principles.
measured at day 7. Fatigue and appetite loss scores were calculated according
to guidelines,24 with scores ranging from 0 to 100; a higher score represented a
higher level of symptoms (ie, worse). A difference of 10, corresponding to 1 on RESULTS
the NRS (0 to 10) scales, was considered clinically significant.25
Adverse effects. The presence of adverse effects (AEs) was assessed by the Study Population
investigator at day 7 through semistructured interviews (presence of edema, A total of 592 patients with cancer and average pain intensity ⱖ 4
sleeplessness, restlessness, anxiety, muscle weakness, psychological changes, in the last 24 hours were identified and screened for eligibility at five
dyspepsia, mouth symptoms, and other [yes v no]). The complete protocol is
available at http://www.ntnu.edu/prc/projects.
outpatient oncology services and palliative care programs. Fifty pa-
tients were recruited during the period from April 2008 to January
Statistical Analysis 2012. The reasons for excluding patients are shown in Figure 1. The
The trial was designed to detect a difference in average pain intensity of
two treatment groups had some minor differences in characteristics at
1.5 (NRS, 0 to 10) between the intervention and placebo groups measured at
day-7 evaluation.26 With a standard deviation of 1.5,12 two-sided t test, baseline (Tables 1 and 2). These were corrected for in the data analyses.
power of 0.90, and significance level of .05, the estimated sample size was 22 Three patients did not complete the study period: one withdrew con-
evaluable patients in each group. A total of 50 patients were recruited to sent before any study procedures were performed, one died as a result
allow for dropouts. of disease progression, and one was withdrawn because of malignant
All data are reported as means, 95% CIs, ranges, medians, or frequencies bowel obstruction. In addition, one patient was withdrawn because of
as appropriate. In the comparison between the two groups, the independent rapidly increasing back pain at day 5. This patient received methyl-
student’s t test was used for continuous variables. In addition, regression and
covariate analyses were performed to adjust for pain intensity and other
prednisolone 48 mg daily on an open basis because of clinical suspi-
differences between the groups at baseline, with the stratification factor of pain cion of spinal cord compression. The patient remained in the analysis,
related to verified bone metastasis and study center. Mann-Whitney U test was according to the principles of the intention-to-treat analysis. No pa-
used for noncontinuous variables. A P value ⱕ .05 was defined as significant. tients were withdrawn or discontinued the study because of AEs.
www.jco.org © 2014 by American Society of Clinical Oncology 3223
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Paulsen et al
Treatment effect on fatigue, appetite loss, and overall satisfaction.
Table 2. Pain Characteristics and Pain Medication at Inclusion (N ⫽ 49)
At day 7, there were significant improvements in fatigue and appetite
Methylprednisolone Placebo loss in the corticosteroid group compared with the placebo group.
(n ⫽ 26) (n ⫽ 23)
Reported as change from baseline, fatigue improved 17 points (95%
Characteristic No. % No. % CI, ⫺27 to ⫺6) in the corticosteroid arm versus a deterioration of 3
Pain category points (95% CI, ⫺5 to 11) in the placebo group (P ⫽ .003). Appetite
Bone 6 23 5 23 improved 24 points (95% CI, ⫺38 to ⫺11) in the corticosteroid group
Visceral 11 42 9 41
versus a deterioration of 2 points (95% CI, ⫺8 to 11) in the placebo
Soft tissue 1 4 6 27
Neuropathic 5 19 1 5
group (P ⫽ .003). Regression analyses using the same variables as for
Mixed 3 12 2 9 pain intensity did not change the results (data not shown). Overall
Breakthrough pain 14 54 17 77 satisfaction with treatment was significantly higher in the corticoste-
Opioids roid group compared with the placebo group (5.4; 95% CI, 4.1 to 6.7 v
Morphine 8 31 7 32 2.0; 95% CI, 0.7 to 3.3; P ⫽ .001; Table 3; Fig 2).
Oxycodone 9 35 10 45
AEs. There were no differences between number of AEs in the
Fentanyl 7 27 6 27
Other 2 8 0 0
corticosteroid group compared with the placebo group (average number,
Oral morphine equivalents 1.08; 95% CI, 0.52 to 1.64 v 1.55; 95% CI, 0.85 to 2.24, respectively; P ⫽
(mg per day) .28; Table 4). The most frequent AEs were oral symptoms, restlessness,
Mean 269.9 160.3 and sleeplessness. The two latter were more frequent in the corticosteroid
95% CI 168.0 to 371.8 90.2 to 230.5 group (restlessness, six v three; sleeplessness, four v three). Three serious
Nonopioids
AEs were reported during the treatment period: one in the placebo group,
Paracetamol 22 85 22 100
Pregabalin 3 12 3 14
whereapatientdiedatday4becauseofdiseaseprogression,andtwointhe
Gabapentin 6 23 0 0 corticosteroid group, where one patient was withdrawn on day 5 because
Amitriptyline 1 4 2 9 of malignant bowel obstruction, and another was withdrawn on day 5
Ketamine 1 4 0 0 because of clinical suspected spinal cord compression. None of these were
suspected to have been caused by the study medication.
DISCUSSION
Twenty-five patients were evaluable in the corticosteroid group, and
22 patients in the placebo group (Fig 1). This study found no evidence of any additional analgesic effect of meth-
ylprednisolone 32 mg daily for 7 days in patients with advanced cancer
Efficacy Analyses treated with opioids. Patients receiving corticosteroids reported less fa-
Treatment effect on pain relief. At day 7, there were no differences tigue, better appetite, and better overall satisfaction with the treatment
in average pain intensity (mean difference, ⫺0.08; 95% CI, ⫺0.97 to compared with the placebo group. The medication was well tolerated.
1.13; corticosteroid arm, 3.6; 95% CI, 2.8 to 4.4; placebo arm, 3.7; 95% The evidence for analgesic effects of corticosteroids in patients
CI, 3.0 to 4.4; P ⫽ .88). Similarly, there were no significant differences with cancer was recently evaluated in a systematic literature review
in pain intensity between the groups when measured as change from published by our research group.17 Four randomized controlled trials
baseline (⫺0.48; 95% CI, ⫺1.43 to 0.47; corticosteroid arm, ⫺1.16; were identified, but only one of these performed an adequate assess-
95% CI, ⫺1.96 to ⫺0.35; placebo group, ⫺0.68; 95% CI, ⫺1.28 to ment of outcomes,12 and the quality of evidence was rated low. Ac-
⫺0.08; P ⫽ .50; Table 3; Fig 2). Correcting for differences between cordingly, only a weak recommendation was made: “Evidence
groups in baseline pain intensity, allowing for covariates, reduced the supports that a moderate dose of corticosteroid, such as methylpred-
difference between the groups to ⫺0.33 (95% CI, ⫺1.33 to 0.67). nisolone 32 mg, may contribute to analgesia and seems to be well
There were no differences between the groups concerning opioid tolerated.”17(p104) In addition, concern about serious AEs associated
consumption. The opioid dose increased similarly in both groups with continued high-dose treatment with corticosteroids was raised.
(relative consumption day 7 v day 0: corticosteroid arm, 1.19; 95% CI, In a cross-over study by Bruera et al,12 a difference in pain inten-
1.00 to 1.38; placebo arm, 1.20; 95% CI, 0.90 to 1.51; P ⫽ .95; Table 3; sity of 13 (visual analog scale, 0 to 100) in favor of the corticosteroid
Fig 3). Daily registrations of pain intensity at rest (area under curve) period compared with the placebo period was found (CIs not pro-
were also similar between the study groups (Table 3). vided). The intervention was similar to that in our study: methylpred-
Regression analyses were also performed adjusting for differ- nisolone 16 mg twice daily. However, the two studies differ in some
ences in baseline characteristics between the groups (Tables 1 and 2): respects. In our study, patients used on average 222 mg oral morphine
baseline opioid dose, presence of breakthrough pain, use of gabapen- equivalents at baseline, had advanced cancer disease, and a mean
tin or pregabalin, soft tissue pain, liver metastases, and other metasta- Karnofsky performance score of 66, approximately equal to an Eastern
ses. Regression analyses did not change the results. Interactions of Cooperative Oncology Group performance status of 2.27 In the study
treatment with pain categories and cancer type were explored using by Bruera et al, the 28 evaluated patients used propoxyphene equaling
linear regression analyses and showed no evidence of important inter- approximately 36 mg of oral morphine equivalents,28 and patients had
actions; the  coefficients for medication and for the main effects of a mean Eastern Cooperative Oncology Group performance status of
the prognostic factors were substantially unchanged when the inter- 3.5. This indicates that the two studies represent two different cancer
action terms were included and excluded from the model. pain populations.
3224 © 2014 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Methylprednisolone RCT for Cancer Pain, Fatigue, and Appetite Loss
Table 3. Primary and Secondary Outcomes
Methylprednisolone Placebo
(n ⫽ 25) (n ⫽ 22)
Outcome Mean 95% CI Mean 95% CI Pⴱ
Average pain intensity†‡
Day 0 4.76 4.33 to 5.19 4.36 3.88 to 4.85 .21
Day 7 3.60 2.79 to 4.41 3.68 2.99 to 4.37 .88
Mean difference ⫺1.16 ⫺1.96 to ⫺0.35 ⫺0.68 ⫺1.28 to ⫺0.08 .50
Morphine consumption (OMEs), mg§
Day 0 273.8 167.8 to 379.8 165.8 93.1 to 238.5 .09
Day 7 318.6 192.3 to 444.8 188.2 103.2 to 273.2 .08
Mean difference 44.8 ⫺16.0 to 105.6 22.4 ⫺5.6 to 50.4 .51
Relative difference (day 7/day 0) 1.19 1.00 to 1.38 1.20 0.90 to 1.51 .95
Pain intensity at rest (day 1 to 7)‡§储
AUC 19.9 14.4 to 25.4 17.9 12.2 to 23.6 .60
Fatigue§储¶
Day 0 77.1 68.3 to 85.9 67.2 56.3 to 78.1 .15
Day 7 60.4 49.7 to 71.2 70.5 61.4 to 79.6 .16
Mean difference ⫺16.7 ⫺27.0 to ⫺6.3 3.3 ⫺4.5 to 11.1 .003
Appetite loss§储¶
Day 0 73.3 60.2 to 86.5 63.6 50.8 to 76.5 .28
Day 7 49.3 34.9 to 63.7 65.2 51.9 to 78.4 .10
Mean difference -24.0 ⫺37.5 to ⫺10.5 1.5 ⫺8.1 to 11.2 .003
Patient satisfaction with treatmentठ5.4 4.05 to 6.70 2.0 0.71 to 3.29 .001
Abbreviations: AUC, area under the curve; OME, oral morphine equivalent.
ⴱ
t test.
†Primary outcome.
‡Numeric rating scale, 0 to 10.
§Secondary outcome.
储Higher score in symptom assessment represents higher level of symptom (ie, worse).
¶Eastern Cooperative Oncology Group performance status, 0 to 100.
We observed a beneficial effect from corticosteroids on appetite with fatigue as the primary end point. Participants were outpa-
loss and fatigue. A Cochrane review from 2010 found no research tients with advanced cancer. The study demonstrated a significant
on corticosteroids with fatigue as the primary outcome.29 In 2013, improvement of 5.9 points (Functional Assessment of Chronic
Yennurajalingam et al30 published a randomized controlled trial Illness Therapy–Fatigue subscale, range, 0 to 52) in the corticosteroid
10 100 10
Day 0 Day 0 Day 0
Day 7 Day 7 Day 7
9 90 9
P = .50 P = .003 P = .003 P = .001
8 80 8
7 70 7
No. of Patients
No. of Patients
No. of Patients
6 60 6
5 50 5
4 40 4
3 30 3
2 20 2
1 10 1
0 0 0
CS PL CS PL CS PL CS PL
Average Pain Intensity Fatigue Appetite Patient Satisfaction
Fig 2. Main results: average pain intensity in last 24 hours (numeric rating scale [NRS], 0 to 10), fatigue and appetite (European Organisation for Research and
Treatment of Cancer–Quality of Life Questionnaire C30, 0 to 100) on days 0 and 7, and patient satisfaction (NRS, 0 to 10) on day 7. CS, corticosteroid; PL, placebo.
www.jco.org © 2014 by American Society of Clinical Oncology 3225
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Paulsen et al
These effects may, in long-term use, counteract the positive effects on
Analgesic consumption CS Analgesic consumption PL
fatigue and appetite. Indeed, the trial by Bruera et al indicated that the
Pain now CS Pain now PL
appetite-stimulating effect of corticosteroids diminishes over time.
350 10 This underlines the need for larger long-term studies. Nevertheless,
(mean oral morphine equivalents)
9 the reported results support a short-term trial of corticosteroids in
Mean Analgesic Consumption
300
8
patients with cancer-related fatigue or loss of appetite.
Pain Intensity at Rest
To our knowledge, ours is the first randomized, controlled,
250 7
double-blind study investigating the analgesic properties of corticoste-
200
6 roids in a population of patients with advanced cancer using opioids.
5 Although the majority of patients included had metastatic disease, the
150 number of dropouts and amount of missing data were low. All out-
4
comes for pain intensity and analgesic consumption showed in a
100 3 consistent way that there were no differences between the intervention
2 and control groups. It was known that a large proportion of the patient
50 group screened already used corticosteroids or had received systemic
1
cancer treatment. Therefore, it was necessary to screen a large number
0 0 of patients to reach the target of 50 eligible patients. The recruitment
0
period was 45 months. This may have introduced a possible selection
ay
ay
ay
ay
ay
ay
ay
ay
D
bias. The corticosteroid group had higher levels of pain intensity,
Fig 3. Mean analgesic consumption and pain intensity at rest (numeric rating morphine consumption, fatigue, and loss of appetite at baseline com-
scale, 0 to 10) as measured day by day. CS, corticosteroid; PL, placebo.
pared with the placebo group, although none of these differences were
statistically significant. Regression analyses did not change the results.
Our trial did not show any analgesic effects from corticosteroids.
group receiving dexamethasone 4 mg twice daily compared with the
The small sample size is reflected by the wide 95% confidence limits.
placebo group. The improvements were significant after both 8 and 15
However, the clinical difference of interest was above the upper bound
days. Both the corticosteroid doses used as well as the results demon-
of the 95% CI, which confirms that there is unlikely to have been a
strated are comparable to the findings in our study. Several randomized
clinically useful effect. The outcomes of fatigue and appetite loss showed
controlled trials have demonstrated a short-term positive effect on appe-
bothclinicallyandstatisticallysignificantimprovement.Thissuggeststhat
tite loss12,13,30-33; only one study did not demonstrate this effect.34
the lack of analgesic effect in the study was not a small-sample effect and
The number of AEs was low in our study, with no difference
supports the main conclusion. However, the sample size was too small to
between the two groups. This finding coincides with the studies by
perform a subgroup analysis, which could have been of clinical interest.
Bruera et al12 and Yennurajalingam.30,34 It is generally agreed that
Lack of analgesic effect in the this study should not preclude the
corticosteroid toxicity is related to the total cumulative dose of corti-
use of corticosteroids in cancer pain syndromes where specific mech-
costeroids as well as the duration of their use.7,35 AEs accumulate with
anisms of action from these drugs are effective. Examples of such
long-term use, and development of cushingoid habitus with moon
mechanisms are reduction of edema in patients with cerebral metas-
face and skin atrophy, osteoporosis, hyperglycaemia, increased risk of
tases and tumor reduction in patients with lymphoma.
infection, and neuropsychological effects36 may interfere with health-
In conclusion, our study found no evidence of an analgesic effect
related quality of life in this patient group. Furthermore, corticoste-
of methylprednisolone 32 mg daily in patients with advanced cancer
roids are known to promote muscle atrophy37,38 and myopathy.39
treated with opioids. Thus, this study provides no support for cancer
pain in general as an indication for starting treatment with corticoste-
roids. Patients who received corticosteroids had clinically significant
Table 4. AEs reduced fatigue and increased appetite, as well as a significantly higher
Methylprednisolone Placebo level of treatment satisfaction, suggesting a symptomatic benefit from
(n ⫽ 25) (n ⫽ 22) the treatment. Clinical benefit beyond short-term effects must be
Predefined AE Category No. % No. % examined in a future study.
Oral symptoms 6 24 7 32
Restlessness 6 24 3 14
Psychic change 2 8 3 14 AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS
Anxiety 2 8 3 14 OF INTEREST
Edema 1 4 5 23
Muscle weakness 1 4 3 14 The author(s) indicated no potential conflicts of interest.
Sleeplessness 4 16 3 14
Dyspepsia 3 12 4 18
Other 2 8 3 14 AUTHOR CONTRIBUTIONS
Total 27 34
Mean No. of AEs 1.08 1.55
P .28
Conception and design: Ørnulf Paulsen, Pål Klepstad, Peter Fayers,
Stein Kaasa
Abbreviation: AE, adverse effect. Financial support: Ørnulf Paulsen
Administrative support: Ørnulf Paulsen, Stein Kaasa
3226 © 2014 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Methylprednisolone RCT for Cancer Pain, Fatigue, and Appetite Loss
Provision of study materials or patients: Ørnulf Paulsen, Jan Henrik Data analysis and interpretation: Ørnulf Paulsen, Pål Klepstad, Peter
Rosland, Nina Aass, Eva Albert Fayers, Stein Kaasa
Collection and assembly of data: Ørnulf Paulsen, Jan Henrik Rosland, Manuscript writing: All authors
Nina Aass, Eva Albert Final approval of manuscript: All authors
controlled, multicenter study—The Methylpred- 27. Buccheri G, Ferrigno D, Tamburini M: Karnof-
REFERENCES nisolone Preterminal Cancer Study Group. Eur J sky and ECOG performance status scoring in lung
Cancer Clin Oncol 25:1817-1821, 1989 cancer: A prospective, longitudinal study of 536
1. Klepstad P, Kaasa S, Cherny N, et al: Pain and 14. Ryan R, Booth S, Price S: Corticosteroid-use patients from a single institution. Eur J Cancer
pain treatments in European palliative care units: A in primary and secondary brain tumour patients: A 32A:1135-1141, 1996
cross sectional survey from the European Associa- review. J Neurooncol 106:449-459, 2012 28. Twycross R, Wilcock A: Dextropropoxyphene:
tion for Palliative Care Research Network. Palliat 15. Tannock I, Gospodarowicz M, Meakin W, et Palliative Care Formulary. Nottingham, United King-
Med 19:477-484, 2005 al: Treatment of metastatic prostatic cancer with dom, Palliativedrugs.com, 2011, pp 337-340
2. Raphael J, Ahmedzai S, Hester J, et al: Cancer low-dose prednisone: Evaluation of pain and quality 29. Peuckmann V, Elsner F, Krumm N, et al:
pain: Part 1—Pathophysiology; oncological, pharma- of life as pragmatic indices of response. J Clin Oncol Pharmacological treatments for fatigue associated
cological, and psychological treatments: A perspec- 7:590-597, 1989
with palliative care. Cochrane Database Syst Rev
tive from the British Pain Society endorsed by the 16. Lundström SH, Fürst CJ: The use of cortico-
11:CD006788, 2010
UK Association of Palliative Medicine and the Royal steroids in Swedish palliative care. Acta Oncol 45:
30. Yennurajalingam S, Frisbee-Hume S, Palmer JL,
College of General Practitioners. Pain Med 11:742- 430-437, 2006
et al: Reduction of cancer-related fatigue with dexa-
764, 2010 17. Paulsen Ø, Aass N, Kaasa S, et al: Do cortico-
methasone: A double-blind, randomized, placebo-
3. World Health Organization: WHO’s cancer steroids provide analgesic effects in cancer pa-
pain ladder for adults. http://www.who.int/cancer/ tients? A systematic literature review. J Pain controlled trial in patients with advanced cancer. J Clin
palliative/painladder/en/ Symptom Manage 46:96-105, 2013 Oncol 31:3076-3082, 2013
4. Knotkova H, Pappagallo M: Adjuvant analge- 18. Radbruch L, Strasser F, Elsner F, et al: Fatigue 31. Moertel CG, Schutt AJ, Reitemeier RJ, et al:
sics. Anesthesiol Clin 25:775-786, vi, 2007 in palliative care patients: An EAPC approach. Palliat Corticosteroid therapy of preterminal gastrointesti-
5. Fallon M, Hanks G, Cherny N: Principles of Med 22:13-32, 2008 nal cancer. Cancer 33:1607-1609, 1974
control of cancer pain. BMJ 332:1022-1024, 2006 19. Yavuzsen T, Davis MP, Walsh D, et al: Sys- 32. Popiela T, Lucchi R, Giongo F: Methylpred-
6. Swarm RA, Abernethy AP, Anghelescu DL, et tematic review of the treatment of cancer- nisolone as palliative therapy for female terminal
al: Adult cancer pain. J Natl Compr Canc Netw associated anorexia and weight loss. J Clin Oncol cancer patients: The Methylprednisolone Female
11:992-1022, 2013 23:8500-8511, 2005 Preterminal Cancer Study Group. Eur J Cancer Clin
7. Lussier D, Portenoy RK: Adjuvant analgesics 20. Caraceni A, Hanks G, Kaasa S, et al: Use of Oncol 25:1823-1829, 1989
in pain management, in Hanks G, Cherny NI, Christa- opioid analgesics in the treatment of cancer pain: 33. Willox JC, Corr J, Shaw J, et al: Prednisolone
kis NA, et al (eds): Oxford Textbook of Palliative Evidence-based recommendations from the EAPC. as an appetite stimulant in patients with cancer. Br
Medicine (ed 4). New York, NY, Oxford University Lancet Oncol 13:e58-e68, 2012 Med J (Clin Res Ed) 288:27, 1984
Press, 2010, pp 706-734 21. Cleeland CS, Ryan KM: Pain assessment: 34. Bruera E, Moyano JR, Sala R, et al: Dexameth-
8. Zhang JM, An J: Cytokines, inflammation, and Global use of the Brief Pain Inventory. Ann Acad asone in addition to metoclopramide for chronic
pain. Int Anesthesiol Clin 45:27-37, 2007 Med Singapore 23:129-138, 1994 nausea in patients with advanced cancer: A random-
9. Watkins LR, Hutchinson MR, Milligan ED, et 22. Bruera E, Kuehn N, Miller MJ, et al: The ized controlled trial. J Pain Symptom Manage 28:
al: “Listening” and “talking” to neurons: Implications Edmonton Symptom Assessment System (ESAS): 381-388, 2004
of immune activation for pain control and increasing A simple method for the assessment of palliative 35. Stanbury RM, Graham EM: Systemic cortico-
the efficacy of opioids. Brain Res Rev 56:148-169, care patients. J Palliat Care 7:6-9, 1991
steroid therapy: Side effects and their management.
2007 23. Aaronson NK, Ahmedzai S, Bergman B, et al:
Br J Ophthalmol 82:704-708, 1998
10. Mensah-Nyagan AG, Meyer L, Schaeffer V, et The European Organisation for Research and Treat-
36. Fardet L, Kassar A, Cabane J, et al:
al: Evidence for a key role of steroids in the modu- ment of Cancer QLQ-C30: A quality-of-life instru-
Corticosteroid-induced adverse events in adults:
lation of pain. Psychoneuroendocrinology 34:S169- ment for use in international clinical trials in
Frequency, screening and prevention. Drug Saf 30:
S177, 2009 (suppl 1) oncology. J Natl Cancer Inst 85:365-376, 1993
861-881, 2007
11. Salerno A, Hermann R: Efficacy and safety of 24. Fayers P, Aaronson N, Bjordal K, et al: EORTC
steroid use for postoperative pain relief: Update and QLQ-C30 Scoring Manual. http://groups.eortc.be/ 37. Braun TP, Zhu X, Szumowski M, et al: Central
review of the medical literature. J Bone Joint Surg qol/manuals nervous system inflammation induces muscle atro-
Am 88:1361-1372, 2006 25. Osoba D, Rodrigues G, Myles J, et al: Inter- phy via activation of the hypothalamic-pituitary-
12. Bruera E, Roca E, Cedaro L, et al: Action of preting the significance of changes in health-related adrenal axis. J Exp Med 208:2449-2463, 2011
oral methylprednisolone in terminal cancer patients: quality-of-life scores. J Clin Oncol 16:139-144, 1998 38. Schakman O, Gilson H, Kalista S, et al: Mech-
A prospective randomized double-blind study. Can- 26. Kaasa S, Apolone G, Klepstad P, et al: Expert anisms of muscle atrophy induced by glucocorti-
cer Treat Rep 69:751-754, 1985 conference on cancer pain assessment and classifi- coids. Horm Res 72:36-41, 2009 (suppl 1)
13. Della Cuna GR, Pellegrini A, Piazzi M: Effect of cation: The need for international consensus— 39. Dietrich J, Rao K, Pastorino S, et al: Cortico-
methylprednisolone sodium succinate on quality of Working proposals on international standards. BMJ steroids in brain cancer patients: Benefits and pit-
life in preterminal cancer patients: A placebo- Support Palliat Care 1:281-287, 2011 falls. Expert Rev Clin Pharmacol 4:233-242, 2011
■ ■ ■
www.jco.org © 2014 by American Society of Clinical Oncology 3227
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Paulsen et al
GLOSSARY TERMS
chemokines: cytokines that are responsible for chemotactic Eastern Cooperative Oncology Group performance sta-
responses. Chemokines are heparin-binding proteins, which play tus: criteria used by doctors and researchers to define the progression
a role in a variety of biologic processes, the most important being of a patient’s disease, assessing how the disease affects daily living habits,
leukocyte chemotaxis. Their classification as C, CC, CXC, and and to assist in the determination of the appropriate treatment and
CX3C is based on the position of cysteine residues that form two prognosis.
disulfide bonds. Typically, chemokines mediate their effects
through G protein– coupled seven-transmembrane domain re- Karnofsky performance score: a standard way of measuring the
ceptors, which belong to four families on the basis of their affin- ability of patients with cancer to perform ordinary tasks. Karnofsky per-
ity for a given chemokine–CXCR1 to CXCR5, CCR1 to CCR9, formance scores range from 0 to 100. A higher score means the patient
XCR1, and CX3CR1. is better able to carry out daily activities. The Karnofsky performance
score may be used to determine a patient’s prognosis, measure changes
in a patient’s ability to function, or decide whether a patient could be
included in a clinical trial.
cytokines: cell communication molecules that are secreted in stratification factor: a factor used to separate data into subgroups
response to external stimuli. to determine whether that factor is significant.
ASCO’s Cancer Genetics Program
ASCO University has developed a comprehensive eLearning program that is focused on hereditary cancer genetics. Take
this expert-led program to gain greater competence in recording and interpreting family history and to know when to refer
for counseling and testing. Members save 20% at asco.org/store.
3228 © 2014 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
Methylprednisolone RCT for Cancer Pain, Fatigue, and Appetite Loss
Acknowledgment
We thank Sebastian von Hofacker, Arve Nordbø, Frode Skanke, Erik Hellem, Katrin Rut Sigurdardottir, and Morten Thronæs (site
investigators who recruited patients and gathered data); Marianne Aamand and Ragnhild Thormodsrød (coordinating study nurses who
performed follow-up at study centers); Grethe Skorpen Iversen, Bente Elisabeth Marum, Bente Miriam Christiansen, Cinzia Marini, Torbjørn
Øvreness, and Ingunn Eriksen (study nurses); Karin Tulluan and Marianne Bjelkåsen (randomization); Gunnhild Jacobsen (assistance with
database design and SPSS statistical software); Lone Nielsen (pharmacist); and staff and patients for participation.
www.jco.org © 2014 by American Society of Clinical Oncology
Information downloaded from jco.ascopubs.org and provided by at Univ of Chicago Library on October 9, 2014 from
Copyright © 2014 American Society of Clinical Oncology. All rights reserved.
128.135.12.127
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Magic Frequencies: Excerpted From The Mixing Engineer's HandbookDocument5 pagesMagic Frequencies: Excerpted From The Mixing Engineer's HandbookmehmetkurtulusNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Moors Sovereign Dollarium 500 Gold Backed Dollarium PicautoDocument2 pagesMoors Sovereign Dollarium 500 Gold Backed Dollarium Picautoakil kemnebi easley elNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Permaculture - Plants Suitable For Ground Cover (P) - Plants For A FutureDocument2 pagesPermaculture - Plants Suitable For Ground Cover (P) - Plants For A Futurecontadino_impazzitoNo ratings yet
- Blood Physiology 2022Document116 pagesBlood Physiology 2022Gurmessa FekaduNo ratings yet
- A. A. Allen The Price of Gods Miracle Working PowerDocument52 pagesA. A. Allen The Price of Gods Miracle Working Powerprijiv86% (7)
- Training Sinal PDFDocument15 pagesTraining Sinal PDFlobitoferoz81No ratings yet
- Graha YuddhaDocument10 pagesGraha YuddhaHeather WilliamsNo ratings yet
- Mary Szybist On Visual Poetry Compressed PDFDocument5 pagesMary Szybist On Visual Poetry Compressed PDFcarlos.enrique.fonseca1440No ratings yet
- Lymphatic System PowerpointDocument20 pagesLymphatic System Powerpointabisantiago6131No ratings yet
- Consideration of Some Other Specific Indications: BacteremiaDocument18 pagesConsideration of Some Other Specific Indications: BacteremiaMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Management of Hypoparathyroidism: Summary Statement and GuidelinesDocument11 pagesManagement of Hypoparathyroidism: Summary Statement and GuidelinesMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Pengantar Reproduksi Menstruasi: Fisiologi DR - Susy OliviaDocument34 pagesPengantar Reproduksi Menstruasi: Fisiologi DR - Susy OliviaMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Pharmacology: Management of Acute Agitation in The Emergency DepartmentDocument13 pagesPharmacology: Management of Acute Agitation in The Emergency DepartmentMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Diagnosis: Systemic Inflamatory Response Syndrome (SIRS) : Assess Haematological & Metabolic StateDocument10 pagesDiagnosis: Systemic Inflamatory Response Syndrome (SIRS) : Assess Haematological & Metabolic StateMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Seizure Focal SeizuresDocument8 pagesSeizure Focal SeizuresMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Gangguan Akibat Kekurangan Iodium: Dr. Idawati Karjadidjaja Ms. SPGKDocument22 pagesGangguan Akibat Kekurangan Iodium: Dr. Idawati Karjadidjaja Ms. SPGKMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Tachycardia Ventricular: - 3 or More Consecutive Ectopic Ventricular ComplexesDocument2 pagesTachycardia Ventricular: - 3 or More Consecutive Ectopic Ventricular ComplexesMOHAMMAD JOFA RACHMAN PUTERANo ratings yet
- Concept Paper Group 1Document9 pagesConcept Paper Group 1Kaime KeilarNo ratings yet
- Catchment CharacterisationDocument48 pagesCatchment CharacterisationSherlock BaileyNo ratings yet
- EngineeringDocument107 pagesEngineeringSuezakumeNo ratings yet
- Cramers Rule 3 by 3 Notes PDFDocument4 pagesCramers Rule 3 by 3 Notes PDFIsabella LagboNo ratings yet
- 2005 Removing Aland RegeneratingDocument6 pages2005 Removing Aland RegeneratingHebron DawitNo ratings yet
- Ix T7AM-CAN - Beijer ElectronicsDocument1 pageIx T7AM-CAN - Beijer ElectronicsKen VikstromNo ratings yet
- The Laws of Motion ¿ ¿ Cengage LearningDocument57 pagesThe Laws of Motion ¿ ¿ Cengage LearningNguyễn Khắc HuyNo ratings yet
- QuizBowl QuestionsDocument84 pagesQuizBowl QuestionsJowel MercadoNo ratings yet
- Scientific Approaches For Impurity Profiling in New Pharmaceutical Substances and Its Products-An OverviewDocument18 pagesScientific Approaches For Impurity Profiling in New Pharmaceutical Substances and Its Products-An OverviewsrichainuluNo ratings yet
- CekocideDocument1 pageCekocideKaren Claire HorcaNo ratings yet
- WBMDocument90 pagesWBMMiguel RegisNo ratings yet
- Design and Fabrication of Single Cylinder Solenoid EngineDocument7 pagesDesign and Fabrication of Single Cylinder Solenoid EngineVIVA-TECH IJRINo ratings yet
- NUTRACEUTICALDocument8 pagesNUTRACEUTICALShubham GuptaNo ratings yet
- International StandardDocument8 pagesInternational Standardnazrul islamNo ratings yet
- Hemiplegia Case 18.12.21Document5 pagesHemiplegia Case 18.12.21Beedhan KandelNo ratings yet
- BCA 5005 Minor Project Synopsis Format & GuidelinesDocument7 pagesBCA 5005 Minor Project Synopsis Format & GuidelinesAnu VermaNo ratings yet
- Case Report - Anemia Ec Cervical Cancer Stages 2bDocument71 pagesCase Report - Anemia Ec Cervical Cancer Stages 2bAnna ListianaNo ratings yet
- 5754 Aluminum CircleDocument2 pages5754 Aluminum Circlewei huaNo ratings yet
- J-20 Stealth Fighter Design Balances Speed and Agility - Defense Content From Aviation WeekDocument9 pagesJ-20 Stealth Fighter Design Balances Speed and Agility - Defense Content From Aviation WeekMahesNo ratings yet
- A Novel Wastewater Derived BiodieselDocument13 pagesA Novel Wastewater Derived BiodieselYuri ClaroNo ratings yet
- Coord Angle and BearingDocument18 pagesCoord Angle and BearingvNo ratings yet