Professional Documents
Culture Documents
Nursing Care Plan: Subjective
Uploaded by
Alimansor M. Darping0 ratings0% found this document useful (0 votes)
47 views6 pagesThe nursing care plan summarizes the care for a patient with decreased cardiac output related to positive-pressure ventilation. Short term goals include maintaining adequate cardiac output and heart rate between 60-100 bpm within 8 hours. Long term goals include normal cardiac output and no reported chest pain. Interventions include monitoring vital signs, assessing blood pressure/heart rate, consciousness level, and signs of low cardiac output. The plan is to notify the physician of any decreases in output and anticipate possible ventilator setting changes.
Original Description:
Original Title
Education material
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe nursing care plan summarizes the care for a patient with decreased cardiac output related to positive-pressure ventilation. Short term goals include maintaining adequate cardiac output and heart rate between 60-100 bpm within 8 hours. Long term goals include normal cardiac output and no reported chest pain. Interventions include monitoring vital signs, assessing blood pressure/heart rate, consciousness level, and signs of low cardiac output. The plan is to notify the physician of any decreases in output and anticipate possible ventilator setting changes.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
47 views6 pagesNursing Care Plan: Subjective
Uploaded by
Alimansor M. DarpingThe nursing care plan summarizes the care for a patient with decreased cardiac output related to positive-pressure ventilation. Short term goals include maintaining adequate cardiac output and heart rate between 60-100 bpm within 8 hours. Long term goals include normal cardiac output and no reported chest pain. Interventions include monitoring vital signs, assessing blood pressure/heart rate, consciousness level, and signs of low cardiac output. The plan is to notify the physician of any decreases in output and anticipate possible ventilator setting changes.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 6
University of Southern Mindanao
College of Health Sciences
Department of Nursing
NURSING CARE PLAN
Name of Patient: ______________________________________Age: ______ Sex: _____ Room: ________Date:
__________________________
Admitting Diagnosis: _________________________________Attending Physician: _________________________Diet: __________________
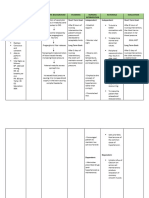
Assessment Nursing Planning Intervention Rationale Evaluation
Diagnosis
Subjective: 1. Establish rapport. 1. To gain patient's trust.
"Sumisikip Risk For Short term goal: 2. Monitor vital signs. 2. To have baseline data Short term goal:
daw po yung Decreased After 8hrs of 3. Assess client's blood 3. Mechanical ventilation can Goal met
dibdib nya" Cardiac nursing care, pressure and heart rate. produce a decreased venous After 8hrs of nursing
as stated by Output related client will return to the heart, resulting in care, client maintained
the watcher. to Positive- maintain decreased BP, compensatory adequate cardiac output
Objective: Pressure adequate increased heart rate, and and HR to 60 to 100
BP-130/90 Ventilation cardiac output decreased cardiac output. This beats per minute with
mmHg and HR to 60 to 4. Assess the client’s level may happen abruptly with regular rhythm.
100 beats per of consciousness. ventilator changes: rate, tidal
HR- 108
minute with volume, or positive-pressure Long term goal:
bpm
regular rhythm. ventilation. Goal met
Altered
Long term goal: 4. The level of consciousness will Client had a normal
myocardial
Client will have 5. Assess the capillary decrease if cardiac output is cardiac output and report
contractility
normal cardiac refill, skin temperature, severely compromised. Therefore no chest pain.
Extra heart output and and peripheral pulses. close monitoring during ventilator
sounds report no chest changes is imperative.
Decreased pain.
urine output 5. Pulses are weak with reduced
Diminished stroke volume and cardiac output.
peripheral 6. Monitor for Capillary refill is slow with reduced
pulses dysrhythmias. cardiac output. Cold, pale, clammy
Cool, ashy skin is secondary to compensatory
skin; 7. Monitor fluid balance sympathetic nervous system
diaphoresis and urine output. stimulation and associated with low
Wheezes cardiac output and oxygen
Tachypnea desaturation.
6. Cardiac dysrhythmias may result
from the low perfusion state,
8. Notify the physician acidosis, or hypoxia.
immediately of signs of a 7. Optimal hydration status is
decrease in cardiac needed to maintain effective
output, and anticipate circulating blood volume and
possible ventilator setting counteract the ventilatory effects
changes. on cardiac output. With positive
pressure ventilation, pressure from
9. Maintain an optimal fluid the diaphragm decreases blood
balance. flow to the kidneys and could result
in a drop in urine output.
8. Vigilant monitoring reduces the
risk for complications. Hypotension
and decreased cardiac output may
10. Administer be related to positive-pressure
medications as ordered ventilator itself or use of positive
(diuretics, inotropic end-expiratory pressure (PEEP)
agents). mode.
9. Volume therapy may be
required to maintain adequate
filling pressures and optimize
cardiac output. However, if PADP
and/or pulmonary capillary wedge
pressure rises and cardiac output
remains low, fluid restriction may
be necessary.
10. Diuretics may be useful to
maintain fluid balance if fluid
retention is a problem. Inotropic
agents may be useful to increase
cardiac output.
NURSING CARE PLAN
Name of Patient: ______________________________________________________ Age: _________ Sex: ______ Room:
____________Date:________________
Admitting Diagnosis: ___________________________________________________ Attending physician: _________________________Diet:
________________
Assessment Nursing Planning Intervention Rationale Eva
Diagnosis
O:Vital signs: Risk for trauma The patient will remain free of 1. Assess client’s temperature. 1. Fever may be a Goal me
T: 37.3°C and infection infection, as evidenced by normal 2. Assess skin integrity under tracheal manifestation of an
PR: 79 bpm related to temperature, absence of purulent ties. infection or inflammatory The pati
RR: 17 endotracheal drainage around the stoma, and 3. Observe the stoma for erythema, color, process. from an
BP: 110/70 intubation or clear breath sounds. exudates, and crusting lesions. If 2. This is a common site for symptom
tracheostomy present, culture the stoma and notify infection and skin infection
the physician. breakdown. manifest
4. Monitor white blood cell (WBC) count. 3. The buildup of mucus and absence
5. Maintain an inflated tracheostomy cuff the rubbing of the
at the lowest pressure possible to tracheostomy tube can
maintain an adequate seal for irritate the skin and serve
ventilation. as a site for infection.
6. Keep a tracheal obturator taped at the Culture and sensitivity
head of the bed for emergency use. reports guide the antibiotic
7. Keep a spare tracheostomy tube of selection.
same size and brand at the bedside. 4. An increasing WBC
8. Do not allow secretions to pool around indicates the body’s effort
the stoma. Suction the area, or wipe to combat pathogen.
with aseptic technique. Keep the skin 5. An inflated cuff protects the
under the tracheostomy ties and back airway and is required for
of the neck clean and dry. mechanical ventilation.
9. Provide stoma care Cuffs should be kept at the
10. If signs of infection are present, apply lowest pressure to prevent
an antifungal or antibacterial tracheal erosion. Clients
medication, as prescribed. are not able to vocalize
while the cuff is properly
inflated.
6. The tracheal obturator is
used to reinsert the
tracheostomy.
7. Being prepared for an
emergency helps prevent
future complications.
8. These steps keep the
stoma clean and dry. The
back of the neck should be
checked carefully in
bedridden clients because
secretions tend to flow to
the back of the neck.
Clean, dry skin helps
prevent skin irritation.
9. Frequent stoma care is
required for postoperative
clients. Care for clients with
long-term stoma placement
is based on need.
10. These agents are either
toxic to the pathogen or
retard its growth.
Bibliography:
You might also like
- Nursing Care Plan For HypertensionDocument3 pagesNursing Care Plan For HypertensionFranco Razon100% (2)
- Assessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGDocument11 pagesAssessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGGrape JuiceNo ratings yet
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For Hypertensionmariejo89% (84)
- HypertensionDocument2 pagesHypertensionRodel Yacas0% (1)
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For HypertensionJessy MalloNo ratings yet
- Risk For Decreased Cardiac Output NCPDocument2 pagesRisk For Decreased Cardiac Output NCPMae Denn LabordoNo ratings yet
- NCP Risk For Decreased CO 1 PDFDocument2 pagesNCP Risk For Decreased CO 1 PDFdubsNo ratings yet
- Nursing Care Plan For HypertensionDocument2 pagesNursing Care Plan For HypertensionFranco Razon100% (1)
- Activity 11 Cardiac Tamponade NCPDocument3 pagesActivity 11 Cardiac Tamponade NCPCloe CorpuzNo ratings yet
- NCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountDocument6 pagesNCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountMabelle SorianoNo ratings yet
- NCP BeeaDocument3 pagesNCP BeeaKiko BernardinoNo ratings yet
- Nursing Care Plan For HypertensionDocument6 pagesNursing Care Plan For HypertensionArian May MarcosNo ratings yet
- NCPDocument4 pagesNCPElbert Vierneza100% (2)
- Nursing Care Plan: Assessment Cues Nursing DiagnosisDocument4 pagesNursing Care Plan: Assessment Cues Nursing DiagnosisKristil ChavezNo ratings yet
- Nursing Care PlanDocument19 pagesNursing Care PlanChic Dian UsmanNo ratings yet
- Hypertension NCPDocument4 pagesHypertension NCPChristian Karl B. Llanes0% (2)
- Preeclampsia NCPDocument4 pagesPreeclampsia NCPKhan Hans100% (1)
- Tams NCP and DrugDocument5 pagesTams NCP and DrugNicholas Xavier VenturaNo ratings yet
- Nursing Care Plan. HypertensionDocument2 pagesNursing Care Plan. HypertensionKiara Shanelle Posadas AbrioNo ratings yet
- Nursing Care Plan 1Document4 pagesNursing Care Plan 1Kiko BernardinoNo ratings yet
- Nursing Care Plan. HypertensionDocument2 pagesNursing Care Plan. HypertensionKiara Shanelle Posadas AbrioNo ratings yet
- CHFDocument3 pagesCHFMary AllizaNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- Cues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Background Knowledge Goals of Care Intervention Rationale EvaluationCharles Dave AgustinNo ratings yet
- CVD HypertensionDocument15 pagesCVD HypertensionAbigail BascoNo ratings yet
- Rationale EvaluationDocument1 pageRationale EvaluationAshraf DalumaNo ratings yet
- NCP HypertensionDocument2 pagesNCP HypertensionRea LynNo ratings yet
- NCPDocument2 pagesNCPJonathan LiscanoNo ratings yet
- Decrease Carsiac Outpit NCP CADDocument3 pagesDecrease Carsiac Outpit NCP CADJayvee CornelioNo ratings yet
- Stroke NCPDocument5 pagesStroke NCPChantal Caragan100% (1)
- Drug StudyDocument5 pagesDrug StudySharies ArgelNo ratings yet
- Nursing Care Plan AnswerDocument6 pagesNursing Care Plan Answercoosa liquorsNo ratings yet
- Decreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To CardiomyopathyDocument2 pagesDecreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To Cardiomyopathywen_pil75% (8)
- Cardiac Rehab Phase3Document15 pagesCardiac Rehab Phase3Evangelin MelvinNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- Decreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To CardiomyopathyDocument2 pagesDecreased Cardiac Output Related To Decreased Myocardial Contractility Secondary To CardiomyopathySoniaMarieBalanayNo ratings yet
- NCP Sa Sinus Tachycardia FinalDocument13 pagesNCP Sa Sinus Tachycardia FinalMYKRISTIE JHO MENDEZNo ratings yet
- Nursing Care Plan # 5Document5 pagesNursing Care Plan # 5Tin DuapaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermDocument5 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermJA BerzabalNo ratings yet
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersDocument8 pagesJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonNo ratings yet
- Cues: Subjective/ Objective Background of The Disease Nursing Diagnosis Goal/ Objectives Intervention Rationale EvaluationDocument3 pagesCues: Subjective/ Objective Background of The Disease Nursing Diagnosis Goal/ Objectives Intervention Rationale EvaluationMaria Margaret Macasaet0% (1)
- B. Inggris PPT NCP Kel. 6Document9 pagesB. Inggris PPT NCP Kel. 6Emi LestariNo ratings yet
- Nursing Diagnoses of A Client With CHDDocument19 pagesNursing Diagnoses of A Client With CHDNG CHEUK HEI 2018 Graduates 6B28No ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Cues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationMiggy SikatNo ratings yet
- Assessmen T Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssessmen T Diagnosis Planning Intervention Rationale EvaluationPeter Emmil GonzalesNo ratings yet
- Sheryl Ann B. Pedines Bsn-IvDocument2 pagesSheryl Ann B. Pedines Bsn-IvSheryl Ann Barit PedinesNo ratings yet
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For Hypertensionanon_9189425950% (2)
- HypertensionDocument13 pagesHypertensionkennedy1434450% (4)
- Chapter 14: Nursing Management: Patients With Coronary Vascular DisordersDocument13 pagesChapter 14: Nursing Management: Patients With Coronary Vascular DisorderskingNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care PlanJoanna Marie PacanoNo ratings yet
- NCP SGHDocument2 pagesNCP SGHdaniloabautista44No ratings yet
- Hypertension Nursing Care PlanDocument3 pagesHypertension Nursing Care Plangeng gengNo ratings yet
- Geria Day 2 NCP 2Document5 pagesGeria Day 2 NCP 2karl davidNo ratings yet
- Dash Diet Cookbook: Easy and Healthy Dash Diet Recipes to Lower Your Blood Pressure. 7-Day Meal Plan and 7 Simple Rules for Weight LossFrom EverandDash Diet Cookbook: Easy and Healthy Dash Diet Recipes to Lower Your Blood Pressure. 7-Day Meal Plan and 7 Simple Rules for Weight LossNo ratings yet
- Mitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandMitral Valve Regurgitation, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesFrom EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesRating: 4 out of 5 stars4/5 (1)
- Pulmonary Hypertension, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandPulmonary Hypertension, A Simple Guide to the Condition, Treatment and Related DiseasesNo ratings yet
- The Perceived Stress Scale (14 Items) - Cohen Et Al, 1983Document4 pagesThe Perceived Stress Scale (14 Items) - Cohen Et Al, 1983Alimansor M. DarpingNo ratings yet
- Part 1 Darping, Alimansor .Document3 pagesPart 1 Darping, Alimansor .Alimansor M. DarpingNo ratings yet
- NCP (Darping, Alimansor M. 4BSN-C)Document14 pagesNCP (Darping, Alimansor M. 4BSN-C)Alimansor M. DarpingNo ratings yet
- Socsci2 Lesson 3 (Akmad)Document5 pagesSocsci2 Lesson 3 (Akmad)Alimansor M. DarpingNo ratings yet
- Acitivity 8 - AKMADDocument6 pagesAcitivity 8 - AKMADAlimansor M. DarpingNo ratings yet
- Statement Frequen CY (n-50) Percenta GEDocument1 pageStatement Frequen CY (n-50) Percenta GEAlimansor M. DarpingNo ratings yet
- Maguindanaon CultureDocument23 pagesMaguindanaon CultureAlimansor M. DarpingNo ratings yet
- DARPING, A. (MBTI Personality Test)Document1 pageDARPING, A. (MBTI Personality Test)Alimansor M. DarpingNo ratings yet
- Graphic Organizer (Persuasion Map)Document1 pageGraphic Organizer (Persuasion Map)Alimansor M. DarpingNo ratings yet
- Activity 2 Direction: Answer Each Question Below Using The Space Provided ForDocument2 pagesActivity 2 Direction: Answer Each Question Below Using The Space Provided ForAlimansor M. DarpingNo ratings yet
- Hydraulic UrethralDocument2 pagesHydraulic UrethralMalgorzata LisowskaNo ratings yet
- Secondary Stroke PreventionDocument54 pagesSecondary Stroke PreventionHùng Phạm Lý ChíNo ratings yet
- Peripheral Nerve Block PresentationDocument50 pagesPeripheral Nerve Block PresentationShikha SoniNo ratings yet
- Cone Beam CT of The Head and Neck-An Anatomical Atlas (2011) PDFDocument76 pagesCone Beam CT of The Head and Neck-An Anatomical Atlas (2011) PDFJetter LeeNo ratings yet
- Drugs For The Heart in Perioperative When To Stop and When To StartDocument38 pagesDrugs For The Heart in Perioperative When To Stop and When To StartnureNo ratings yet
- Clinical Engineering II-2Document4 pagesClinical Engineering II-2Waltas KariukiNo ratings yet
- Instruments - Prof. ABM AbdullahDocument27 pagesInstruments - Prof. ABM Abdullahduniyajhaan19No ratings yet
- DR Danish Javed CBPACSDocument19 pagesDR Danish Javed CBPACSDrDanish JavedNo ratings yet
- Dutta 2Document671 pagesDutta 2Jeel GaralaNo ratings yet
- Urology IDocument34 pagesUrology IEbraheam HadiNo ratings yet
- Newly Diagnosed and Relapsed Epithelial Ovarian CancerDocument16 pagesNewly Diagnosed and Relapsed Epithelial Ovarian CancerDragos VrancianuNo ratings yet
- Heart Specialist in Haldwani - Google SearchDocument1 pageHeart Specialist in Haldwani - Google SearchManoj UpadhyayNo ratings yet
- Perioperative Teamwork For The Patient With A Shared AirwayDocument7 pagesPerioperative Teamwork For The Patient With A Shared AirwaysondiNo ratings yet
- 20 Q Arthroscopic Instruments PDFDocument11 pages20 Q Arthroscopic Instruments PDFEduardo BernardinoNo ratings yet
- Twin-To-Twin Transfusion Syndrome (TTTS) Pathogenesis, Diagnostics, Classification and Treatment OptionsDocument11 pagesTwin-To-Twin Transfusion Syndrome (TTTS) Pathogenesis, Diagnostics, Classification and Treatment OptionsArio DaniantoNo ratings yet
- Department of Nursing: AssessmentDocument2 pagesDepartment of Nursing: Assessmentjoshua canjaNo ratings yet
- Care of Chest Tube Drainage & Nursing Manangement SHDocument82 pagesCare of Chest Tube Drainage & Nursing Manangement SHJoanna RemollinoNo ratings yet
- 17corneal DystrophiesDocument15 pages17corneal Dystrophies2begeniusNo ratings yet
- Case Study 10 Hysterectomy: Hospital Costs and Outcomes Study For NSW HealthDocument68 pagesCase Study 10 Hysterectomy: Hospital Costs and Outcomes Study For NSW Healthkriesya riesyaNo ratings yet
- Osteoid Osteoma and Osteoblastoma: Review ArticleDocument12 pagesOsteoid Osteoma and Osteoblastoma: Review ArticleAnggi MartaNo ratings yet
- ArdsDocument32 pagesArdsMaxine HsuNo ratings yet
- Introduction To Emergency Nursing Concepts FinalDocument128 pagesIntroduction To Emergency Nursing Concepts FinalKarren FernandezNo ratings yet
- MS - Knee Arthroscopy - 1 - Slide16Document2 pagesMS - Knee Arthroscopy - 1 - Slide16testNo ratings yet
- Stoppa ModificadoDocument6 pagesStoppa ModificadomvortopediaNo ratings yet
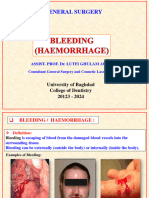
- Dentistry l4 BleedingDocument15 pagesDentistry l4 BleedingHadeer WasfyNo ratings yet
- Best Gynecologist Doctor in BangaloreDocument13 pagesBest Gynecologist Doctor in BangaloreAnjaly anjuNo ratings yet
- Supernumerary KidneysDocument8 pagesSupernumerary KidneysPedro Henrique SilveiraNo ratings yet
- Radiology ManualDocument24 pagesRadiology ManualQuality Manager100% (2)
- Ospe Du EntDocument114 pagesOspe Du Entmfshihab3352No ratings yet
- L&D PDFDocument2 pagesL&D PDFChandace JanineNo ratings yet