Professional Documents
Culture Documents
Nurse Protocol Article
Nurse Protocol Article
Uploaded by
Mohamed Abd El MonemCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nurse Protocol Article
Nurse Protocol Article
Uploaded by
Mohamed Abd El MonemCopyright:
Available Formats
The development of a stroke nurse protocol for delivering thrombolyti...
for patients with acute ischaemic stroke in United Kingdom hospitals
Thrombolysis for acute ischaemic stroke: the development of a
nurse protocol in the United Kingdom
IST-3 Stroke Nurse Collaborative Group (see appendix for list of collaborators and
participating hospitals)
Abstract
This paper describes a nursing protocol for patients treated with thrombolysis for acute
ischaemic stroke developed during the Stroke Association phase of the Third International
Stroke Trial (IST-3), a randomised controlled trial of recombinant tissue plasminogen
activator for acute ischaemic stoke.
The IST-3 Nurse collaborative group met three times over three years. The meetings consisted
of educational updates on stroke thrombolysis, training on trial procedures, presentations by
participating nurses and discussions of good practice, local initiatives and sharing common
problems.
Lack of knowledge, fear of bleeding complications and lack of appropriate NHS beds were
common barriers. Core nursing requirements suggested by this research included:
fast-tracking of patients; access to trained stroke physicians; acute physiological monitoring
and nursing intervention; effective communication and support of patients and carers;
knowledge of complications and actions to be taken; transfer to an appropriately skilled stroke
unit environment and successful discharge planning to home or rehabilitation.
INTRODUCTION
This article summarises the reasons why thrombolytic therapy is a promising treatment for
acute ischaemic stroke and describes the development of the core nursing implications of
introducing thrombolytic therapy in selected United Kingdom hospitals. In 2002, the Committee
for Proprietary Medicinal Products for the European Union, agreed a framework to allow
national drug licensing bodies of individual European Union countries to grant a licence for
alteplase (a recombinant tissue plasminogen activator thrombolytic agent known as rt-PA). This
may lead to a license being granted in the UK for patients treated up to three hours following an
ischaemic stroke (at the time of writing this was still awaited). Consequently, there is an urgent
need to establish and refine appropriate nursing guidelines for NHS hospitals.
Stroke is a major problem in the United Kingdom
In the UK, about 150,000 people have a stroke each year (110,000 being first-ever strokes)
(Bamford et al, 1988). The underlying pathology in 85% of patients with stroke is cerebral
ischaemia (infarction), and therefore treatments directed at this subgroup will have greatest
impact (Bamford et al, 1990). Stroke is an important illness, as 30% of patients are dead within
6 months and a further 30% are dependent in activities of living. (Bamford et al, 1990). In
addition, stroke consumes about 5% of all NHS resources and places a considerable burden on
family and carers. (Isard and Forbes, 1992; Department of Health (DOH), 2001). It remains a
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (1 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
major health problem for Europe, with a stroke rate of about 1 million a year, and globally, with
over 5 million stroke deaths around the world. (Sandercock et al, 1992).
As the population ages, stroke is likely to become more frequent even if stroke incidence rates
remain constant or decline. It is, therefore, likely that stroke will represent a significant health
problem for many decades to come. Important research investment in stroke is needed to
tackle this problem. There needs to be effective stroke prevention and improvement in stroke
management through greater availability of stroke units to provide acute treatment and
rehabilitation and facilitate research. (DOH, 2001; Rothwell 2001)
Better treatments needed for acute stroke
Few treatments are effective for acute stroke. Aspirin treatment (150-300mg daily, orally or
rectally, started immediately after acute ischaemic stroke confirmed) has only modest benefit
(approximately 12 more independent survivors per 1,000 treated).(Chen et al, 2000) In
contrast, thrombolytic therapy, which works by dissolving the thrombus causing the ischaemic
stroke, can potentially re-open the occluded artery and reverse the stroke. Research has
demonstrated that some patients with severely disabling stroke (e.g. aphasia, dense
hemiparesis and hemianopia) recover quickly after emergency with thrombolysis, and are
discharged home within days, with little or no residual disability. (The National Institute of
Neurological Disorders and Stroke rt-PA Stroke Study Group 1995) Without effective treatment,
such patients usually require months of in-patient rehabilitation, have a high risk of dying and
often need long-term institutional care. (Stroke Unit Trialists' 2001)
Why is thrombolytic therapy the promising treatment to evaluate for acute ischaemic
stroke?
There have now been 18 completed randomised controlled trials involving 5721 patients, of
thrombolytic therapy for acute ischaemic stroke and the results from these trials have been
systematically reviewed in the Cochrane Library. (Wardlaw et al. 2003) This Library provides
high quality systematic reviews of medical treatment (and management strategies) and is
widely available in medical libraries and the Internet (http://www.update-software.com/cochrane).
Table 5 lists references for the trials.
Four different thrombolytic agents have been evaluated but about half of the data come from
trials of alteplase (recombinant tissue plasminogen activator or rt-PA for short). Sixteen trials
used the intravenous route of administration, with only two using the more complex intra-arterial
route. The time window from onset of stroke symptoms to treatment varied between trials but
almost all patients were treated within six hours of the onset of stroke symptoms.
In the following sections the overall results of thrombolytic therapy from the systematic review
are summarised.
RESULTS OF THROMBOLYTIC THERAPY
Reduction in "death or dependency".
Thrombolytic treatment significantly reduced the number of patients dead or dependent from
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (2 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
58% in control patients to 53.3% in treated patients. (Wardlaw et al, 2003) This is equivalent to
an additional 43 independent survivors for every 100 patients treated (95% Confidence Interval
13 to 71). This is a substantial and worthwhile benefit.
Risk of major intracranial haemorrhage.
The main risk of thrombolytic therapy for stroke is fatal intracranial haemorrhage (ICH). The
data in the Cochrane review showed that treatment increased the absolute risk of fatal ICH
from 0.9% in control patients to 5.1% in treated patients (2p<0.00001, a highly significant
result). The risk of symptomatic ICH (including fatal bleeds) increased from about 2.3% to 8.7%
(2p<0.00001).(Wardlaw, de Zoppo, Yamaguchi, & Berge2003)
The risks of alteplase were somewhat less and the benefits somewhat more and thus alteplase
appears to be one of the more promising thrombolytic agents to evaluate in further trials.
(Wardlaw, de Zoppo, Yamaguchi, & Berge2003)
Overall, this evidence suggests that thrombolytic therapy may increase independent survival in
many patients despite causing intracranial haemorrhage in others. Whilst it is already clear that
some highly selected patients with stroke will benefit from thrombolytic therapy there is far less
data on thrombolytic therapy for stroke than, for example, for myocardial infarction (MI).
(Fibrinolytic Therapy Trialists' (FTT) Collaborative Group 1994) By the time thrombolysis for MI
was routine, some 60,000 patients had been included in the major trials. (Fibrinolytic Therapy
Trialists' (FTT) Collaborative Group 1994) The relative lack of stroke data has resulted in very
little use of thrombolytic therapy in the UK. Treatment remains controversial and doctors are
uncertain of the benefits of treatment. It is with this background that a further trial evaluating
thrombolysis has been developed and this trial, the Third International Stroke Trial (IST-3),
started recruitment in May 2000 in the UK.
The Third International Stroke Trial (IST-3)
The third International Stroke Trial is an international collaborative trial funded independently
from the pharmaceutical industry with a trial co-ordinating office based at the University of
Edinburgh. A detailed protocol for the IST-3 is available on the Internet
(http://www.dcn.ed.ac.uk/ist3), but in brief, this trial is a randomised controlled trial evaluating
alteplase (rt-PA) for patients with acute ischaemic stroke.
The main eligibility criteria for the IST-3 are shown in Table 2
Table 2. Main eligibility criteria for the Third International Stroke Trial (IST-3)
Clinically definite stroke with a known time of onset
Computerised tomography (CT) brain scanning has excluded intracranial haemorrhage and
mimics of acute stroke (e.g. brain tumour)
Appropriate consent has been obtained
Treatment started as early as possible, and no later than 6 hours after stroke onset
Trial treatment consists of alteplase in a dose of 0.9mg/kg up to a maximum of 90mg
given as a 10% intravenous bolus and the rest of the dose as a 1-hour intravenous
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (3 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
infusion. Control patients were given matching placebo in the early phase of the trial
described in this paper (2000 – 2002).
Non-trial thrombolytic treatment
In the absence of a license for alteplase for acute stroke in the United Kingdom, few
patients receive routine thrombolysis treatment. However, there is a licence for stroke,
for patients who can treated within 3 hours of stroke onset, in the United States of
America, Germany and Canada. Treatment has to be administered within 3 hours of
stroke onset and published guidelines from North America are available.(Special Writing
Group of the Stroke Council of the American Heart Association 1996) These guidelines
provide some useful information but are difficult to implement in the United Kingdom
(UK), as the health services, and stroke services differ so much between North America
and the UK. This prompted research to develop core nursing standards appropriate to
the NHS, based on the North American guidelines and the experience of implementing
thrombolysis (mainly in the context of the IST-3) in UK centres.
Nursing requirements are exactly the same whether patients receive trial (e.g. IST-3
treatment), with a 50% chance of receiving alteplase, or routine treatment, with 100%
receiving alteplase.
METHODS
The Stroke Association funded pilot and service development phase of the IST-3 covers
the period from February 2000 to January 2003. Multicentre Research Ethics Approval
was obtained in 1999. During this period centres in the United Kingdom (and abroad)
with local ethics committee approval developed fast-track thrombolysis protocols and
sought appropriate patients for the trial. Centres in the UK were asked to nominate a
member of nursing staff with an interest in stroke. There was some financial aid (from
the Stroke Association grant) to assist NHS staff support this research, which was about
0.1 whole time equivalent funding per centre.
The IST-3 Nurse Collaborative Group consisted of the Principal Investigator, Trial
Manager and Medical Research Fellow for the trial and one or more nurses from each UK
centre. The collaborative group met three times. The meetings were structured with
presentations by each participant, and there was ample time for discussion. The
prespecified aims of the meetings were to share knowledge, disseminate good practice
and to learn from the experiences of others. Core nursing standards, appropriate for
thrombolysis in the UK, were discussed, agreed and redrafted by the collaborative
group.
RESULTS
The Stroke Association start-up phase of the IST-3 commenced in Edinburgh in May
2000 and 11 UK centres obtained full ethics approval. The first two meetings of the
collaborative groups discussed the local barriers to recruiting patients in the IST-3.
Barriers to the introduction of thrombolysis for ischaemic stroke in the NHS
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (4 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
The practical barriers to the introduction of thrombolysis for ischaemic stroke in the UK
included:
● Lack of nursing knowledge about thrombolysis for stroke
● Lack of necessary skill mix in stroke centre
● Lack of fast-track organisation
● Nursing fears of the intracranial haemorrhagic side effects
● Lack of appropriate stroke unit beds
● Consent issues
Lack of knowledge about thrombolysis for stroke:
A lack of knowledge about thrombolysis was a considerable barrier to the introduction
of a thrombolysis service in most UK hospitals. Indeed, many of the group admitted
uncertainties themselves. Stroke unit staff needed to keep up to date with the current
information about thrombolysis. Nursing staff were often unaware of the promising data
to support the use of thrombolysis for some highly selected patients (Wardlaw et al
2003) e.g. younger (< 80 years) patients who can be treated within 3 hours of stroke
onset), and that thrombolysis may be beneficial for many more patients (such as those
suitable for the IST-3 trial). (Wardlaw at al, 2003). The group rapidly realised that stroke
thrombolysis teams had an ongoing responsibility to educate all staff including nursing
staff.
Necessary skill mix on stroke unit:
Thrombolysis for stroke can have serious complications and at present it can only be
recommended for organised stroke services, e.g. hospitals with a stroke unit. The
introduction of thrombolysis is an important service development for acute stroke
services. Thrombolysis services will need to be funded (i.e. with health improvement
plans or research and development funding). Local co-ordinators, in discussion with
nurse managers need to ensure that a suitable skill mix is available to safely deliver a
thrombolysis service. In some centres, this may mean limiting thrombolysis to "office
hours" when more support is immediately available. Acute stroke unit areas will need to
be developed. Each shift should include at least one staff nurse who has been trained in
stroke thrombolysis.
In addition many centres have only one stroke consultant prepared to supervise a
thrombolysis service. This is a major barrier. The National Service Framework for Older
People emphasised the importance of a stroke consultant in every hospital but there are
a lack of suitably trained physicians in the UK (DoH, 2001) .This situation should
improve; in the meantime, stroke physicians should consider involving other physicians
or neurologists to share the caseload. This is especially important for out-of-hours
consultant support for nursing and medical staff.
Lack of fast-track organisation:
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (5 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
The three centres with the best recruitment (Western General Hospital, Edinburgh,
Addenbrookes Hospital, Cambridge and Arrowe Park Hospital, The Wirral) had
organised fast-track stroke systems. The Western General Hospital had an integrated
care pathway that was developed by a multidisciplinary task force and was very effective
in identifying suitable patients for the acute stroke team. Arrowe Park hospital had an
acute stroke pathway, and its stroke service was awarded an NHS Beacon.
Addenbrookes hospital had an acute stroke pathway. Organisation of stroke admissions
by pathways of care, agreed by multi-disciplinary members is key to successful acute
stroke assessment.
Fear of side effects and medico-legal protection for nursing staff:
Both doctors and nurses fear the haemorrhagic complications of thrombolytic treatment,
especially major extra cranial bleeding (e.g. massive gastrointestinal bleeding) or
intracranial bleeding (e.g. severe or fatal recurrent stroke or deterioration). However, the
frequency of these risks is similar to the frequency of complications in the natural
history of a major ischaemic stroke. (Bamford et al, 1990) In legal terms this is called
"minimal risk". Although the risks of thrombolysis are greater than many typical medical
treatments, the risks of the natural history of stroke are greater than many typical
medical conditions. (Bamford, et al,1990) The risks of thrombolysis can, therefore, be
compared to the risks of cerebral oedema in some patients with untreated ischaemic
stroke. Consumer work has emphasised that older people are comfortable with a risk of
death IF there is a chance of future independence.(Koops & Lindley 2002). A simple
analogy is to compare thrombolysis for stroke to major surgery. There are definite risks,
but potential major advantages. In Koops’s study, older people supported research for
thrombolysis despite these increased risks. If patients are given alteplase treatment, it is
very important that informed consent is obtained from the patient (and relatives if
medically appropriate). The IST-3 has strictly controlled consent procedures with full UK
Multi-Centre Research Ethics approval. NHS Trusts should provide management
approval for non-licensed use of alteplase and management approval is mandatory for
clinical trials such as IST-3. These formal approval mechanisms help provide
medico-legal protection for nursing staff.
Lack of appropriate beds:
Many acute NHS hospitals (and stroke units) have average bed occupancy of greater
than 95%, which predicts regular bed crises. (Bagust, et al, 1999) Stroke thrombolysis
needs to be given the priority afforded to thrombolysis for acute MI. Ideally, acute stroke
units need to keep a bed for the next potential thrombolysis patient, or have a strategy
for clearing a bed within an hour. This has been a recurring problem in the IST-3 hospital
centres. However, liaison with bed management, a written protocol and a dedicated
stroke unit bed are some solutions to this problem. It is vital that a bed is protected for
stroke thrombolysis to ensure that treatment is always given in a safe environment with
trained and experienced staff.
Consent issues:
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (6 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
Consent for thrombolysis creates unique ethical dilemmas and there are considerable
problems to overcome.(Lindley 1998) However, the unique consumer involvement in the
design of the IST-3 has created a streamlined and ethical consent process that has
worked well so far. (Koops & Lindley, 2002)
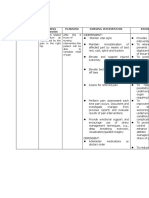
Core Nursing Requirements
There are 10 requirements for the safe delivery of thrombolysis for patients with acute
stroke. These are shown in Table 3 and are discussed below:
Table 3. Core nursing requirements for safe thrombolysis
Triage nursing in the emergency room
Urgent skilled medical assessment in a safe environment
Communication and support
Quick and safe transfer to Computerised tomographic (CT) brain scanning
Monitoring and nursing prior to treatment
Treatment
Monitoring and nursing during and after treatment
Comprehensive assessment in a stroke unit
Preventing and treating complications
Hospital Discharge or transfer to rehabilitation
Triage nursing in the emergency room:
"Time is brain" is a useful phrase to help persuade health professionals identify suitable
patients quickly. Emergency room triage nurses need to follow an appropriate
"fast-track" protocol to activate the acute stroke team. The triage guideline for the
Western General Hospital, Edinburgh, is shown in Table 4.
Table 4. An example of an emergency room triage nurse protocol for thrombolysis
Clinical signs of definite acute stroke Yes/No
Time of onset known Yes/No, if yes state time __: __ (24 hour clock)
Time from stroke onset < 5 hours Yes/No
If Yes to all three questions contact acute stroke team
Initial triage nursing includes functional documentation of airway, breathing and
circulation. Blood pressure, pulse, oxygen saturation and blood glucose estimation
should be performed, and abnormalities treated according to local protocol and medical
advice. An important stroke mimic is hypoglycaemia (Libman et al 1995). The Glasgow
Coma Scale (GCS) should be recorded and vital signs monitored regularly. A peripheral
Intravenous catheter should be inserted. Patients who are in acute urinary retention
should be catheterised. Aspirin and heparin treatment should be avoided during the first
24 hours after treatment with thrombolysis. (The National Institute of Neurological
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (7 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
Disorders and Stroke rt-PA Stroke Study Group 1995)
Urgent skilled medical assessment in a safe environment:
Patients who are being considered for thrombolytic treatment need an expert medical
assessment to document the time of stroke onset and to determine the severity of the
stroke. Other mimics of acute stroke include migraine, seizures, metabolic disturbances
and brain tumours. (Libman et al. 1995) An important part of the clinical assessment is
getting a confirmatory history from relatives (or ambulance staff). Relatives should be
advised to remain with the patient until the medical staff have spoken with them and
obtained consent for treatment if appropriate. During this time the nursing priorities
should include monitoring oxygen saturation, documenting blood pressure, pulse and
temperature.
Communication and support:
During this early period it is essential to prepare the patient and relatives for the next
stage of assessment with clear and simple advice. Written information is helpful, for
example, the IST-3 trial information leaflet (available on the British Medical Journal
website at: http://bmj.com/cgi/content/full/325/7361/415/DC1). Relatives should be
encouraged to accompany the patient until eventual arrival on the stroke unit, as they
are often required to help with consent issues for those who are drowsy, aphasic or
confused. Nurses have an important role in relieving anxiety in the patients and relatives
by the provision of information (both verbal and written), reassurance and explanation.
Transfer to CT brain scanning:
If the medical staff assess that the patient is potentially eligible for thrombolytic therapy
an urgent computerised tomogram (CT) brain scan must be obtained. Patients should be
transferred on a trolley (not a chair, even if only a mild stroke deficit) to facilitate transfer
onto the CT scanning table. Valuable time is saved if patients can be transferred easily
from trolley to CT scanning table and back onto the trolley at the end of the procedure. A
nurse must accompany the patient to monitor his/her neurological status, vital signs and
to assist in the transfers.
Monitoring and nursing care prior to treatment :
Vital signs need to be rechecked before treatment with thrombolytic therapy. American
guidelines suggest that thrombolytic therapy is contraindicated if blood pressure is
greater than 185/110 mmHg. (Adams Jr. et al, 1996) Some clinicians will initiate
emergency blood pressure lowering in this situation, but this policy is controversial, as
there is some data to suggest that lowering blood pressure in the acute phase of stroke
is harmful. (Brott et al, 1998) Nursing staff have an important role in facilitating
communication at all stages of the fast-tracking process.
Treatment with thrombolysis:
When patients are eligible and have consented to thrombolytic therapy, treatment must
be given without delay. Consideration should be given to where therapy is started. If the
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (8 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
acute stroke unit is a short distance away, patients should be urgently transferred to the
unit. If the acute stroke unit is some distance from the CT scanner, a convenient
treatment room should be identified. The treatment room should provide 24-hour access
to alteplase (or trial treatment packs), giving set equipment and an intravenous infusion
pump. Alteplase is given by an intravenous bolus injection followed by a 1-hour
infusion. The dose is calculated at 0.9mg/kg body weight up to a maximum of 90mg, 10%
is given over 1-2 minutes and the remaining 90% is infused intravenously over 1 hour.
The patients’ weight should be estimated to calculate the correct dose. While the bolus
dose is being administered over 1 - 2 minutes, the 1-hour infusion should be prepared.
The infusion is best given by a syringe driver.
Monitoring and nursing care during and after treatment:
Blood pressure and pulse should be monitored at the start of treatment, at 30 minutes
and at the end of treatment at 1 hour. Our experience has shown blood pressure cuffs
can sometimes cause petechial subcutaneous bleeding; therefore automated blood
pressure machines, that use high-inflation pressures, should be avoided. We, therefore,
recommend that a handheld manual sphygmomanometer be used during thrombolytic
treatment and in the 24 hours following treatment. The patient’s neurological status
should be directly observed during the first 24-48 hours. The GCS should be part of a
minimum nursing assessment and recorded on a bedside chart. The medical staff
should be called if the GCS falls during this period. In our experience patients rarely
deteriorate during the actual alteplase infusion but if the neurological deficit worsens, or
if the patient becomes haemodynamically unstable, the infusion should be halted and
the doctor called. The main risk of thrombolytic treatment is intracranial haemorrhage
and if the patient deteriorates neurologically (Adams et al 1996) (e.g. the GCS falls)
during or after treatment, an urgent CT brain scan should be performed to exclude
haemorrhagic transformation of the cerebral infarct, or other intracranial bleeds.
Thrombolysis with rt-PA is clot specific, i.e. it mainly exerts its effect within the
thrombus (The National Institute of Neurological Disorders and Stroke rt-PA Stroke
Study Group (1995) so although the rt-PA has a very short half-life in the circulation
(minutes), the drug will continue to act in a thrombosis for many hours. Therefore the
potential haemorrhagic complications may be delayed for 24-48 hours.
At about 24-48 hours following thrombolysis treatment the excess risks of bleeding start
to diminish and it is common practice to obtain a second CT brain scan to help exclude
any intracranial bleeding complications. If there have been no bleeding complications,
aspirin is usually started (or recommenced) (Chen et al 2000). Heparin is not used
routinely as there is no evidence that early anticoagulation is required after
thrombolysis for stroke, and early anticoagulation is not effective for ischaemic stroke.
(Gubitz et al 2003)
Comprehensive assessment in a stroke unit:
The benefits of stroke unit care are applicable to patients with all types of stroke and it is
important that all patients who are considered for thrombolysis have access to stroke
unit care (or stroke team care). The treatment benefits of being in a stroke unit are
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (9 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
considerable (equivalent to about 60 per 1,000 extra independent survivors compared to
about 20-30 per thousand survivors for early thrombolysis of acute myocardial
infarction). (Stroke Unit Trialists'2001) (Fibrinolytic Therapy Trialists' (FTT) Collaborative
Group 1994) Hospitals without a stroke unit should invest in stroke services prior to
setting up a stroke thrombolysis service. A major feature of the stroke units in the
randomised controlled trials was comprehensive assessment by trained
multi-disciplinary staff.(Stroke Unit Trialists'2001)
Preventing and treating complications:
Nurses have a major role to play in the prevention of complications following
thrombolysis for acute ischaemic stroke. Patients need to be carefully observed to
identify any signs of bleeding or bruising. Invasive procedures such as urinary
catheterisation should be avoided if possible, to avoid causing any trauma which might
result in bleeding. Care must be taken when removing indwelling intravenous catheters,
as there may be excessive bleeding. During this risky period nursing care plans or
nursing pathways need to pay particular attention to patient safety. This is especially
important if the patient has sensory inattention or neglect. Consideration should be
given to providing one-to-one nursing for the initial 24 hours of treatment. In general,
there should be no restrictions on usual early rehabilitation strategies for patients.
Hospital Discharge or transfer to rehabilitation:
Patients who continue to need nursing support and rehabilitation should be nursed in a
stroke rehabilitation unit. Hospitals without well-organised stroke services need to
invest in these before even considering introducing thrombolytic therapy. If this unit is
off the main acute hospital site it is very important to ensure a good handover of care.
Patients who regain full independence on the acute stroke unit will need information
about their stroke, counselling regarding modifiable risk factors e.g. smoking and this
can be reinforced using written material and videos from the Stroke Association and
Chest, Heart and Stroke, Scotland.
CONCLUSIONS
This paper has outlined the rationale for introducing thrombolysis for acute ischaemic
stroke in the UK and has discussed the nursing issues that need to be considered when
writing a local protocol and developing a thrombolysis service. Education was an
important theme to emerge from our research, and new stroke services should ensure
that resources are allocated for continued professional development for stroke nurses.
The introduction of a thrombolysis service will also need investment in nursing time and
expertise, with appropriate staffing levels to manage the detailed nursing described in
this paper. The continued development of stroke units within the United Kingdom should
facilitate the introduction of a thrombolysis service.
We would welcome comments and contributions from other with similar experience in
the UK.
Acknowledgements
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (10 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
This work was supported by the Stroke Association grant TSA04/99 "Thrombolysis for
acute ischaemic stroke: pilot and service development phase of the Third International
Stroke Trial (IST-3)", University of Edinburgh and the Scottish National Health Service
(Dr Lindley).
We thank the patients and their relatives who agreed to participate in IST-3 and to the
many hundreds of NHS and University staff who have contributed their time and effort to
this project.
Key Points
● Thrombolysis for acute ischaemic stroke is a promising treatment requiring
further development before becoming a routine treatment in UK hospitals.
● In the UK, the Third International Stroke Trial (IST-3) is the major ongoing trial
of alteplase, the most promising thrombolytic agent.
● This study identified many barriers to a routine stroke thrombolysis service in the
UK NHS, including lack of available beds, knowledge and perceived fears of
treatment.
● Solutions to many of the identified barriers were identified and implemented, such
as regular education updates for stroke service staff and the routine use of stroke
pathways or protocols.
● This research has led to the development of core nursing requirements that are
practicable for the UK NHS.
Appendix: IST-3 Stroke Nurse Collaborative Group
Julie Rycarte, Addenbrookes Hospital, Cambridge
Pamela Beattie, Royal Victoria Hospital, Belfast
Diane Day, Addenbrookes Hospital, Cambridge
Sandra Aitcheson, Ulster Hospital, Belfast
Annemarie Hunter, Royal Victoria Hospital, Belfast
Ruth Plant, Arrowe Park Hospital, Wirral
Diane Rennie, Western General Hospital, Edinburgh
Pat Taylor, Western General Hospital, Edinburgh
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (11 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
Doreen Shaw, Western General Hospital, Edinburgh
Denise Shave, Royal Bournemouth Hospital
Ally Graham, Royal Bournemouth Hospital
Karen Innes, Trial Manager, Edinburgh
Peter Hand, Research Fellow, Edinburgh
Richard Lindley, Principal Investigator, Edinburgh
Steve Duckworth, King’s College Hospital, London
Diane Thompson, Royal Hallamshire Hospital, Sheffield
Emma Jackson, St James’s University Hospital, Leeds
Karen Coyle, University Hospital Aintree, Liverpool
Tracy McCormick, University Hospital Aintree, Liverpool
Cheryl Utecht, Leicester Royal Infirmary, Leicester
References
Adams HPJr, Brott TG, Furlan A J et al (1996) Guidelines for thrombolytic therapy for
acute stroke: a supplement to the guidelines for the management of patients with acute
ischemic stroke. A statement for healthcare professionals from a Special Writing Group
of the Stroke Council, American Heart Association Circulation 94:1167-74.
Bagust A, Place M, Posnett J (1999) Dynamics of bed use in accommodating emergency
admissions: stochastic simulation model. Br Med J 319:155-8
Bamford J, Sandercock P, Dennis M et al (1998) A prospective study of acute
cerebrovascular disease in the community: the Oxfordshire Community Stroke
Project1981-6. 1, Methodology, demography and incident cases of first-ever stroke.J
Neurol, Neurosurgery Psychiatry 51: 1373-80.
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (1990) A prospective study of
acute cerebrovascular disease in the community: the Oxfordshire Community Stroke
Project 1981-1986. 2; Incidence, case fatality and overall outcome at one year of cerebral
infarction, primary intracerebral haemorrhage and subarachnoid haemorrhage", Journal
of Neurology, Neurosurgery and Psychiatry, vol. 53, pp. 16-22.
Brott, T. Lu M, Kothari R et al (1998) Hypertension and its treatment in the NINDS rt-PA
Stroke Trial. Stroke 29:1504-9.
Councell, C, Collins, NINDS rt_PA Stroke Study Group (1998) Stroke 29: 1504-9.
Chen ZM, Sandercock P, Pan et al (2000) Indications for early aspirin use in acute
ischemic stroke: a combined analysis of 40 000 randomised patients from the Chinese
acute stroke trial and the international stroke trial. On behalf of the CAST and IST
collaborative groups. Stroke 31:1240-9.
DoH (2001) Standard five: stroke. In: National Service Framework for Older People. DoH,
London.
Fibrinolytic Therapy Trialists' (FTT) Collaborative Group (1994) Indications for
fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (12 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
early mortality of early mortality and major morbidity results from all randomised trials
of more than 1000 patients. Lancet 343: 311-22.
Gubitz G, Counsell C, Sandercock P, Signorini D. (2003) Anticoagulants for acute
ischaemic stroke (Cochrane Review). 1 edn, Update Software, Oxford.
Isard PA, Forbes JF (1992) The Cost of Stroke to the NHS in Scotland. Cerebrovascular
Dis 2: 47-50.
Koops L, Lindley RI (2002) Thrombolysis for acute ischaemic stroke: consumer
involvement in design of new randomised controlled trial. Br Med J 325: 415-17.
Libman RB, Wirkowski E, Alvir J, Rao H (1995) Conditions that mimic stroke in the
emergency department: implications for acute stroke trials Arch Neurol 52: 1119-22.
Lindley RI 1998,Thrombolytic treatment for acute ischaemic stroke: consent can be
ethical. Br Med J 316:1005-7.
Rothwell PM (2001) The high cost of not funding stroke research: a comparison with
heart disease and cancer. Lancet 357:1612-16.
Sandercock PAG, Celani MG, Ricci S (1992) The likely public health impact in Europe of
simple treatments for acute ischaemic stroke. Cerebrovascular Dis 2: 236.
Special Writing Group of the Stroke Council of the American Heart Association (1996)
Guidelines for thrombolytic therapy for acute stroke: a supplement to the guidelines for
the management of patients with acute ischaemic stroke. Stroke, 27: 711-18.
Stroke Unit Trialists C (2001) Organised inpatient (stroke unit) care for stroke, Cochrane
Database of Systematic Reviews 1: 2001.
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group
(1995) Tissue plasminogen activator for acute ischemic stroke. New Engl J Med 333:
1581-7.
Wardlaw JM, de Zoppo G, Yamaguchi T, Berge, E (2003) Thrombolysis for Ischaemic
Stroke (Cochrane Review). 1 edn, Update Software, Oxford.
Table 5 Trials of thrombolysis for acute ischaemic stroke.
Abe 1981 (Abe 1981)
Atarashi 1985 (Atarashi et al. 1985)
Ohtomo (Atarashi, Otomo, Araki, Itoh, Togi, & Matsuda1985)
Mori (Mori et al. 1992)
Haley (Haley et al. 1993)
JTSG (Yamaguchi et al. 1993)
ECASS 1 (European Cooperative Acute Stroke Study Group 1995)
Morris (Morris et al. 1995)
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (13 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
MAST Italy (Multicentre Acute Stroke Trial - Italy (MAST-I) Group 1995)
NINDS (The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group 1995)
ASK 1996 (Donnan et al. 1996)
MAST Europe (The Multicenter Acute Stroke Trial - Europe Study Group 1996)
PROACT (del Zoppo et al. 1998)
ECASS 2 (Hacke et al. 1998)
ATLANTIS B (Clark et al. 1999)
PROACT II (Furlan et al. 1999)
ATLANTIS A (Clark et al. 2000)
Chinese UK Trial (full publication awaited) (Wardlaw et al. 2003)
Detailed summaries of the trials are available in the Cochrane Library review (Wardlaw, de Zoppo,
Yamaguchi, & Berge2003)
References
Abe, T. 1981, "Clinical evaluation for efficacy of tissue cultured urokinase on cerebral
thrombosis by means of multi-centre double blind study", Blood and Vessel, vol. 12, pp.
321-341.
Atarashi, J., Otomo, E., Araki, G., Itoh, E., Togi, H., & Matsuda, T. 1985, "Clinical utility of
urokinase in the treatment of acute stage of cerebral thrombosis (Multicentre
double-blind study in comparison with placebo)", Clinical Evaluation, vol. 13, pp.
659-709.
Clark, W. M., Albers, G. W., Madden, K. P., Hamilton, S., & for the Thrombolytic Therapy
in Acute Ischaemic Stroke Study Investigators 2000, "The rt-PA (Alteplase) 0- to 6- hour
Acute Stroke Trial, Part A (A027g). Results of a double-blind, placebo-controlled,
multicentre study.", Stroke, vol. 31, pp. 811-816.
Clark, W. M., Wissman, S., Albers, G. W., Jhamandas, J., Madden, K., & Hamilton, S.
1999, "Recombinant tissue-type plasminogen activator (Alteplase) form ischaemic
stroke 3 to 5 hours after symptom onset. The Atlantis Study: a randomised controlled
trial", JAMA, vol. 282, pp. 2019-2026.
del Zoppo, G., Higashida, R. T., Furlan, A. J., Pessin, M. S., Rowley, H. A., Gent, M., & and
the PROACT Investigators 1998, "A phase II randomised trial of recombinant
pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke", Stroke,
vol. 29, pp. 4-11.
Donnan, G. A., Davis, S. M., Chambers, B. R., Gates, P. C., Hankey, G. J., McNeil, J. J.,
Rosen, D., Stewart-Wynne, E. G., Tuck, R. R., & for the Australian Streptokinase (ASK)
Trial Study Group 1996, "Streptokinase for acute ischemic stroke with relationship to
time of administration", JAMA, vol. 276, pp. 961-966.
European Cooperative Acute Stroke Study Group 1995, "European Cooperative Acute
Stroke Study (ECASS). Intravenous thrombolysis with recombinant tissue plasminogen
activator for acute hemispheric stroke", JAMA, vol. 274, pp. 1017-1025.
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (14 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
Furlan, A. J., Higashida, R. T., Wechsler, L., Gent, M., Rowley, H. A., Kase, C., Pessin, M.,
Ahuja, A., Callahan, F., Clark, W. M., Silver, F., Rivera, F., & for the PROACT Investigators
1999, "Intraarterial Pro-Urokinase for acute ischaemic stroke. The PROACT II Study: A
randomised controlled trial", JAMA, vol. 282, pp. 2003-2011.
Hacke, W., Kaste, M., Fieschi, C., von Kummer, R., Davalos, A., Meier, D., Larrue, V.,
Bluhmki, E., Davis, S., Donnan, G., Schneider, D., Diez-Tejedor, E., Trouillas, P., & for
second European-Australasian Acute Stroke Study Investigators 1998, "Randomised
double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase
in acute ischaemic stroke (ECASS II)", The Lancet, vol. 352, pp. 1245-1251.
Haley, E. C., Brott, T. G., Sheppard, G. L., Barsan, W., Broderick, J., Marler, J. R.,
Kongable, G. L., Spilker, J., Massey, S., Hansen, C. A., Torner, J. C., & for the TPA
Bridging Study Group 1993, "Pilot randomised trial of tissue plasminogen activator in
acute ischaemic stroke", Stroke, vol. 24, pp. 1000-1004.
Mori, E., Yoneda, Y., Tabuchi, M., Yoshida, T., Ohkawa, S., Ohsumi, Y., Kitano, K.,
Tsutsumi, A., & Yamadori, A. 1992, "Intravenous recombinant tissue plasminogen
activator in acute carotid artery territory stroke", Neurology, vol. 42, pp. 976-982.
Morris, A. D., Ritchie, C., Grosset, D. G., Adams, F. G., & Lees, K. R. 1995, "A pilot study
of streptokinase for acute cerebral infarction", Quarterly Journal of Medicine, vol. 88, pp.
727-731.
Multicentre Acute Stroke Trial - Italy (MAST-I) Group 1995, "Randomised controlled trial
of streptokinase, aspirin, and combination of both in treatment of acute ischaemic
stroke", The Lancet, vol. 346, pp. 1509-1514.
The Multicenter Acute Stroke Trial - Europe Study Group 1996, "Thrombolytic therapy
with streptokinase in acute ischemic stroke", The New England Journal of Medicine, vol.
335, pp. 145-150.
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group
1995, "Tissue plasminogen activator for acute ischemic stroke", The New England
Journal of Medicine, vol. 333, pp. 1581-1587.
Wardlaw, J. M., de Zoppo, G., Yamaguchi, T., & Berge, E. 2003, Thrombolysis for
ischaemic stroke (Cochrane Review), 1 edn, Update Software, Oxford.
Yamaguchi, T., Hayakawa, T., Kiuchi, H., & for the Japanese Thrombolysis Study Group
1993, "Intravenous tissue plasminogen activator ameliorates the outcome of hyperactue
embolic stroke", Cerebrovascular Diseases, vol. 3, pp. 269-272.
Organisations
Chest, Heart & Stroke Scotland
65 North Castle Street, Edinburgh EH2 3LT
Advice Line: 0845 077 6000
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (15 of 16) [13/05/2003 11:59:06]
The development of a stroke nurse protocol for delivering thrombolyti... for patients with acute ischaemic stroke in United Kingdom hospitals
Tel 0131 225 6963 Fax 0131 220 6313
E-mail: admin@chss.org.uk
Web: www.chss.org.uk
Stroke Association
Stroke House, 240 City Road, London, EC1V 2PR
Tel 020 7566 0300 Fax 020 7490 2686
http://www.stroke.org.uk/
info@stroke.org.uk
Correspondence Mrs Karen Innes, Trial Manager, IST-3
Bramwell Dott Building, University of Edinburgh, Western General Hospital
Edinburgh, EH4 2XU
Tel 0131 5372793 Fax 0131 332 5150
http://www.dcn.ed.ac.uk/newist3/nurse_protocol_article.htm (16 of 16) [13/05/2003 11:59:06]
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Casper Cheat SheetDocument3 pagesCasper Cheat SheetMichael Moore100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Teamwork Skill Communicating Effectively in GroupDocument21 pagesTeamwork Skill Communicating Effectively in Groupsiyalohia8No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Japanese Foods That Heal - Using Traditional Japanese Ingredients To Promote Health, Longevity, & Well-Being (PDFDrive)Document282 pagesJapanese Foods That Heal - Using Traditional Japanese Ingredients To Promote Health, Longevity, & Well-Being (PDFDrive)Stanislava KirilovaNo ratings yet
- Nursing ManagementDocument10 pagesNursing ManagementMohamed Abd El MonemNo ratings yet
- Adult Basic Life Support (BLS)Document50 pagesAdult Basic Life Support (BLS)Mohamed Abd El MonemNo ratings yet
- Nursing and Interdisciplinary of StrokeDocument36 pagesNursing and Interdisciplinary of StrokeMohamed Abd El MonemNo ratings yet
- NA Curriculum 01-16Document37 pagesNA Curriculum 01-16Mohamed Abd El MonemNo ratings yet
- Obat Program Puskesmas Des 2020Document28 pagesObat Program Puskesmas Des 2020WIWIK FADILAH AMIRNo ratings yet
- EPI 3.6 Qualitative ResearchDocument5 pagesEPI 3.6 Qualitative ResearchJoher MendezNo ratings yet
- Legal ComplianceDocument14 pagesLegal ComplianceArun FikdetcNo ratings yet
- NCP (Acute Pain)Document1 pageNCP (Acute Pain)Joan QuebalayanNo ratings yet
- SNEHADocument2 pagesSNEHAanishNo ratings yet
- MSDS X20 PlasterboardsDocument2 pagesMSDS X20 PlasterboardstantanNo ratings yet
- Sacandalfinal31 PDFDocument69 pagesSacandalfinal31 PDFJoshua KumayogNo ratings yet
- IELTS Essay - Public HealthDocument5 pagesIELTS Essay - Public HealthAnonymous j8Ge4cKINo ratings yet
- Elma-T3: Mammography SystemDocument12 pagesElma-T3: Mammography SystemKateNo ratings yet
- Blue and White Modern Creative Business PresentationDocument14 pagesBlue and White Modern Creative Business PresentationDaine GoNo ratings yet
- Module 1 HOME-ECONOMICS-LITERARCYDocument44 pagesModule 1 HOME-ECONOMICS-LITERARCYAaron Miguel Francisco100% (1)
- Safety Data Sheet: Product Name: MOBIL EAL 224HDocument10 pagesSafety Data Sheet: Product Name: MOBIL EAL 224HAnibal RiosNo ratings yet
- 20-Dialysis 2016Document10 pages20-Dialysis 2016duchess juliane mirambelNo ratings yet
- Technology PresentationDocument16 pagesTechnology Presentationabraralnaamani3No ratings yet
- Dr. Fixit Fastflex: High Performance Polymer Modified Cementitious CoatingDocument3 pagesDr. Fixit Fastflex: High Performance Polymer Modified Cementitious CoatingDeep GandhiNo ratings yet
- 09 7 Strategies For Effective TrainingDocument44 pages09 7 Strategies For Effective TrainingJaiDoms100% (1)
- Tugas Bahasa Inggris Ling Ling WeiDocument2 pagesTugas Bahasa Inggris Ling Ling WeiLing Ling Wei IINo ratings yet
- Colorectal Cancer EngDocument11 pagesColorectal Cancer Engrinadi_aNo ratings yet
- Disaster Management Regulatory FrameworkDocument38 pagesDisaster Management Regulatory FrameworkJames LoganNo ratings yet
- Warning: Company Profile Disclaimer of Warranties and Limitation of LiabilityDocument10 pagesWarning: Company Profile Disclaimer of Warranties and Limitation of Liabilitybman0051401No ratings yet
- HTP Technique Lecture Notes 1Document9 pagesHTP Technique Lecture Notes 1Rameen FatimaNo ratings yet
- Ferrous Sulphate - MSDSDocument6 pagesFerrous Sulphate - MSDSDyeing DyeingNo ratings yet
- The Role of Parents in Sex Education: How Can Parents Be Better Equipped To Provide Accurate and Comprehensive Information To Their Children?Document7 pagesThe Role of Parents in Sex Education: How Can Parents Be Better Equipped To Provide Accurate and Comprehensive Information To Their Children?RaashiNo ratings yet
- Assessing Special PopulationsDocument91 pagesAssessing Special PopulationsJAGATHESANNo ratings yet
- JSS Medical College Mysore: Admissions 2023, Courses Offerd, Fees Structure, Cutoff, CounsellingDocument27 pagesJSS Medical College Mysore: Admissions 2023, Courses Offerd, Fees Structure, Cutoff, CounsellingJustGetAdmissionNo ratings yet
- Reason For The Critical Equipment Maintenance (Tick One)Document1 pageReason For The Critical Equipment Maintenance (Tick One)Anil RainaNo ratings yet
- An Overview Storage of Pharmaceutical Products PDFDocument18 pagesAn Overview Storage of Pharmaceutical Products PDFVer OnischNo ratings yet