Psychiatry Notes Overview
Uploaded by
Noman ButtPsychiatry Notes Overview
Uploaded by
Noman Butt- Introduction to Psychiatry Notes: Introduces the scope and purpose of the psychiatry notes related to medical studies.
- Alcohol Withdrawal and Related Disorders: Covers symptoms and treatments associated with alcohol withdrawal and related disorders like anorexia nervosa and bulimia nervosa.
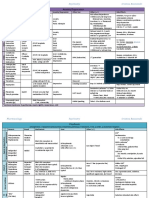
- Antipsychotics in Treatment: Discusses different types of antipsychotic medications used in psychiatric treatment and their side effects.
- Depression and Anxiety: Explains distinguishing features and treatments for depression and anxiety disorders, emphasizing evidence-based approaches.
- Insomnia and Related Conditions: Addresses causes, risk factors, and management strategies for insomnia and its various forms.
- Obsessive-Compulsive and Related Disorders: Provides insight into obsessive-compulsive disorder (OCD) and other related mental health conditions.
- Personality Disorders: Offers details about different types of personality disorders, including symptomatic and therapeutic insights.
- Schizophrenia and Psychotic Disorders: Discusses schizophrenia and other psychotic disorders, covering diagnostic criteria and treatment options.
- Pharmacology and Interaction Management: Outlines pharmacological interventions and interaction considerations for psychiatric medications.
- Dementia Types and Management: Explores various forms of dementia and recommended management strategies, focusing on cognitive health.
- Novel Treatments and Advances: Highlights emerging treatments and recent advances in psychiatric treatment methods.
lOMoARcPSD|6265699
Psychiatry Notes
Medicine (Queen Mary University of London)
StuDocu is not sponsored or endorsed by any college or university
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Alcohol withdrawal say you are thing? Does food dominate your
life? Yes >2 = AN or bulimia
Mechanism - Features: Due to starvation or vomiting:
chronic alcohol consumption enhances Fatigue, reduced cognition, altered sleep cycle,
GABA mediated inhibition in the CNS sensitivity to cold, enlarged salivary glands,
hypotension
(similar to benzodiazepines) and inhibits - Red flags: BMI <13 or below 2nd centile, wt loss
NMDA-type glutamate receptors >1kg/wk, temp <34.5, BP <80/50, pulse <40,
alcohol withdrawal is thought to be lead O2 < 92%, limbs = blue and cold, no muscle
strength, ECG: long QT, flat T waves, purpura,
to the opposite (decreased inhibitory K<2.5, Na<130, PO4 <0.5
GABA and increased NMDA glutamate o Refer to EDU, re-feed
transmission) - Tx: Individual eating-disorder-focused cognitive
behavioural therapy (CBT-ED), wight gain
0.5kg-1kg, final BMI = 20-25, Maudsley
Features Anorexia Nervosa Treatment for Adults
symptoms start at 6-12 hours: tremor, (MANTRA), specialist supportive clinical
management (SSCM), fluozetine
sweating, tachycardia, anxiety - In children and young people, NICE
peak incidence of seizures at 36 hours recommend 'anorexia focused family therapy'
peak incidence of delirium tremens is at as the first-line treatment. The second-line
treatment is cognitive behavioural therapy.
48-72 hours: coarse tremor, confusion,
delusions, auditory and visual
Bulimia nervosa
hallucinations, fever, tachycardia - Episodes of binge eating then vomiting or
using laxatives or diuretics or exercising, BMI
Management >17.5, preoccupation with body weight
control.
patients with a history of complex - Episodes occur on average once a week for
withdrawals from alcohol (i.e. delirium three months.
tremens, seizures, blackouts) should be - Tx = Mild: Supportive (CBT-ED, FT-BN), refer to
EDU if no response, moderate/severe: SSRI
admitted to hospital for monitoring until (fluoxetine), CBT
withdrawals stabilised
first-line: benzodiazepines e.g. chlordiazep
oxide. Lorazepam may be preferable in Antipsychotics
patients with hepatic failure. Typically
given as part of a reducing dose protocol Antipsychotics are a group of drugs used in the
carbamazepine also effective in treatment management of schizophrenia and other forms of
of alcohol withdrawal psychosis, mania and agitation. They are usually
divided into typical and atypical antipsychotics. The
phenytoin is said not to be as effective in
atypical antipsychotics were developed due to
the treatment of alcohol withdrawal the problematic extrapyramidal side-effects which
seizures are associated with the first generation of typical
antipsychotics.
Typical antipsychotics
Anorexia nervosa
- Common cause of admission to children and
Mechanism of Dopamine D2 receptor antagonists, blocking dopam
adolescent psych wards. F>M action transmission in the mesolimbic pathways
- DSM5 criteria: Adverse effects Extrapyramidal side-effects and hyperprolactinaemia
o Weight <85% of predicted
o Intense fear of gaining weight with
behaviour that interferes with
Examples Haloperidol
weight gain
Chlopromazine
o Feeling fat when thin
- SCOFF questionnaire: Make yourself sick? Lost
control over eating? Lost more than one stone
in 3 months? Believe you are fat hen others The rest of this section will focus on typical
antipsychotics, with atypical antipsychotics covered
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
elsewhere. top of the clinical follow-up that such patients
clearly require. The BNF advises the following*:
Extrapyramidal side-effects (EPSEs)
Test
Full blood count (FBC), urea and electrolytes (U&E), liver
Parkinsonism function tests (LFT)
acute dystonia
o sustained muscle
contraction (e.g. torticollis, oculo
gyric crisis)
o may be managed with
procyclidine Lipids, weight
akathisia (severe restlessness)
tardive dyskinesia (late onset of
choreoathetoid movements, abnormal,
involuntary, may occur in 40% of
patients, may be irreversible, most Fasting blood glucose, prolactin
common is chewing and pouting of jaw)
The Medicines and Healthcare products Regulatory
Blood pressure
Agency has issued specific warnings when
antipsychotics are used in elderly patients:
Electrocardiogram
increased risk of stroke
increased risk of venous
thromboembolism
Cardiovascular risk assessment
Other side-effects
*please see the BNF for more details. There are a
antimuscarinic: dry mouth, blurred number of specific recommendations for individual
vision, urinary retention, constipation drugs, the above is a general summary
sedation, weight gain
raised prolactin
o may result in galactorrhoea Atypical antipsychotics
o due to inhibition of the
dopaminergic tuberoinfundibular
pathway Atypical antipsychotics should now be used first-
impaired glucose tolerance line in patients with schizophrenia, according to
neuroleptic malignant syndrome: pyrexia, 2005 NICE guidelines. The main advantage of the
muscle stiffness atypical agents is a significant reduction in
reduced seizure threshold (greater with extrapyramidal side-effects.
atypicals)
prolonged QT interval (particularly Adverse effects of atypical antipsychotics
haloperidol)
Antipsychotics: monitoring weight gain
clozapine is associated
with agranulocytosis (see below)
The monitoring requires for patients taking hyperprolactinaemia
antipsychotic medication are extensive. This is on
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
The Medicines and Healthcare products Regulatory Dose adjustment of clozapine might be necessary
Agency has issued specific warnings when if smoking is started or stopped during treatment.
antipsychotics are used in elderly patients:
Benzodiazepines
increased risk of stroke
Benzodiazepines enhance the effect of the
increased risk of venous
inhibitory neurotransmitter gamma-aminobutyric
thromboembolism
acid (GABA) by increasing the frequency of
chloride channels. They therefore are used for a
variety of purposes:
Examples of atypical antipsychotics
sedation
clozapine
hypnotic
olanzapine: higher risk of dyslipidemia
anxiolytic
and obesity
anticonvulsant
risperidone
muscle relaxant
quetiapine
amisulpride
aripiprazole: generally good side-effect
Patients commonly develop a tolerance and
profile, particularly for prolactin elevation
dependence to benzodiazepines and care should
therefore be exercised on prescribing these drugs.
The Committee on Safety of Medicines advises that
benzodiazepines are only prescribed for a short
Clozapine period of time (2-4 weeks).
Clozapine, one of the first atypical agents to be The BNF gives advice on how to withdraw a
developed, carries a significant risk benzodiazepine. The dose should be withdrawn in
of agranulocytosis and full blood count monitoring steps of about 1/8 (range 1/10 to 1/4) of the daily
is therefore essential during treatment. For this dose every fortnight. A suggested protocol for
reason, clozapine should only be used in patients patients experiencing difficulty is given:
resistant to other antipsychotic medication. The
BNF states:
switch patients to the equivalent dose of
diazepam
Clozapine should be introduced if schizophrenia is reduce dose of diazepam every 2-3 weeks
not controlled despite the sequential use of two or in steps of 2 or 2.5 mg
more antipsychotic drugs (one of which should be time needed for withdrawal can vary from
a second-generation antipsychotic drug), each for 4 weeks to a year or more
at least 6–8 weeks.
Adverse effects of clozapine If patients withdraw too quickly from
benzodiazepines they may experience
benzodiazepine withdrawal syndrome, a condition
agranulocytosis (1%), neutropaenia (3%) very similar to alcohol withdrawal syndrome. This
reduced seizure threshold - can induce may occur up to 3 weeks after stopping a long-
seizures in up to 3% of patients acting drug. Features include:
constipation
myocarditis: a baseline ECG should be
taken before starting treatment insomnia
hypersalivation irritability
anxiety
tremor
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
loss of appetite hypomania describes decreased or
tinnitus increased function for 4 days or more
perspiration from an exam point of view the key
perceptual disturbances differentiation is psychotic symptoms
seizures (e.g.delusions of grandeur or auditory
hallucinations) which suggest mania
GABAA drugs
Management
benzodiazipines increase the frequency of
chloride channels psychological interventions specifically
barbiturates increase the duration of designed for bipolar disorder may be
chloride channel opening helpful
lithium remains the mood stabilizer of
choice. An alternative is valproate
Frequently Bend - During Barbeque management of mania: consider stopping
antidepressant if the patient takes one;
...or... antipsychotic therapy e.g. olanzapine or
haloperidol
Barbidurates increase duration management of depression: talking
& Frendodiazepines increase frequency therapies (see above); fluoxetine is the
antidepressant of choice
address co-morbidities - there is a 2-3
Bipolar disorder times increased risk of diabetes,
cardiovascular disease and COPD
Bipolar disorder is a chronic mental health disorder
characterised by periods of mania/hypomania Primary care referral
alongside episodes of depression.
Epidemiology
if symptoms suggest hypomania then
NICE recommend routine referral to the
community mental health team (CMHT)
typically develops in the late teen years if there are features of mania or severe
life time prevalence: 2% depression then an urgent referral to the
CMHT should be made
Two types of bipolar disorder are recognised:
Charles-Bonnet syndrome
type I disorder: mania and depression
(most common)
type II disorder: hypomania and Charles-Bonnet syndrome (CBS) is characterised by
depression persistent or recurrent complex hallucinations
(usually visual or auditory), occurring in clear
consciousness. This is generally against a
background of visual impairment (although visual
What is mania/hypomania?
impairment is not mandatory for a diagnosis).
Insight is usually preserved. This must occur in the
absence of any other significant neuropsychiatric
both terms relate to abnormally elevated disturbance.
mood or irritability
with mania there is severe functional Risk factors include:
impairment or psychotic symptoms for 7
days or more
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Advanced age Factors suggesting diagnosis of depression over
Peripheral visual impairment dementia:
Social isolation Short history, rapid onset
Sensory deprivation Biological symptoms e.g. Weight
Early cognitive impairment loss, sleep disturbance
Patient worried about poor memory
Reluctant to take tests, disappointed with
CBS is equally distributed between sexes and does results
not show any familial predisposition. The most Mini-mental test score: variable
common ophthalmological conditions associated Global memory loss (dementia
with this syndrome are age-related macular characteristically causes recent memory
degeneration, followed by glaucoma and cataract. loss)
Well-formed complex visual hallucinations are Depression: management of subthreshold
thought to occur in 10-30 per cent of individuals depressive symptoms or mild depression
with severe visual impairment. Prevalence of CBS
in visually impaired people is thought to be
between 11 and 15 per cent. NICE produced updated guidelines in 2009 on the
management of depression in primary and
Around a third find the hallucinations themselves secondary care. Patients are classified according to
an unpleasant or disturbing experience. In a large the severity of the depression and whether they
study published in the British Journal of have an underlying chronic physical health
Ophthalmology, 88% had CBS for 2 years or more, problem.
resolving in only 25% at 9 years (thus it is not
generally a transient experience). Please note that due to the length of the 'quick'
reference guide the following is a summary and we
Cox (2014) Negative outcome Charles Bonnet would advise you follow the link for more detail.
Syndrome. Br J Ophthalmol.
Cotard syndrome Persistent subthreshold depressive symptoms or
mild to moderate depression
Cotard syndrome is a rare mental disorder where
General measures
the affected patient believes that they (or in some
cases just a part of their body) is either dead or
non-existent. This delusion is often difficult to treat
and can result in significant problems due to sleep hygiene
patients stopping eating or drinking as they deem active monitoring for people who do want
it not necessary. an intervention
Cotard syndrome is associated with severe
depression and psychotic disorders. Drug treatment
De Clerambault's syndrome do not use antidepressants routinely but
consider them for people with:
a past history of moderate or severe
De Clerambault's syndrome, also known as
depression or
erotomania, is a form of paranoid delusion with an
initial presentation of subthreshold
amorous quality. The patient, often a single
depressive symptoms that have been
woman, believes that a famous person is in love
present for a long period (typically at least
with her.
2 years) or
subthreshold depressive symptoms or
Depression vs. Dementia
mild depression that persist(s) after other
interventions
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
if a patient has a chronic physical health focus on sharing experiences and feelings
problem and mild depression complicates associated with having a chronic physical
the care of the physical health problem health problem
consist typically of 1 session per week
over 8-12 weeks
The following 'low-intensity psychosocial
interventions' may be useful:
Depression: management of unresponsive,
Intervention moderate and severe depression
Individual guided self-help based on CBT Interventions should:
principles NICE produced updated guidelines in 2009 on the
management of depression in primary and
(Includes behavioural activation and include written materials
secondary (or alternative
care. Patients media) according to
are classified
problem-solving techniques) be supported by a trained
the severity of thepractitioner
depressionwhoand reviews
whetherprogress
they
consist ofhave
up toan6-8 sessions (face-to-face
underlying andhealth
chronic physical by telephone) over 9-12
weeks, including
problem.follow-up
Computerised CBT Please note that due to the length of the 'quick'
Interventions should:
reference guide the following is a summary and we
would advise you follow the link for more detail.
explain the CBT model, encourage tasks between sessions, and use
thought-
Persistent subthreshold depressive symptoms or
challenging and active monitoring of behaviour, thought patterns and
mild to moderate depression with inadequate
outcomes
response to initial interventions, and moderate
be supported by a trained practitioner who reviews progress and outcome
and severe depression
typically take place over 9-12 weeks, including follow-up
A structured group physical activity For these patients NICE recommends an
Interventions should:
programme antidepressant (normally a selective serotonin
reuptake inhibitor, SSRI)
typically consist of 3 sessions
The following per weekpsychological
'high-intensity (lasting 45 minutes to 1 hour) over
10-14 weeks
interventions' may be useful:
An alternative is group-based CBT
typicall
be based on a model such as 'Coping with consider 3-4 fol
depression' for moderate or severe dep
be delivered by two trained and
competent practitioners
Individual CBT
consist of 10-12 meetings of 8-10
participants Interpersonal therapy (IPT) Delivery
typically take place over 12-16 weeks,
including follow-up
typically 16-20 sessions over 3-
for severe depression, consider
For patients with chronic physical health problems
NICE also recommend considering a group-based Behavioural activation Delivery
peer support programme:
typically 16-20 sessions over 3-
consider 3-4 follow-up sessions
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
A 'yes' answer to either of the above should
prompt a more in depth assessment.
consider 3-4 follow-up sessions over the next 3-6 months
Assessment
for moderate or severe depression, consider 2 sessions per week for the first 2-3
Individual CBT There are many tools to assess the degree of
depression
for moderate or severe including
depression, the
consider Hospital per
2 sessions Anxiety
weekand
for the first 3-4 weeks
Depression (HAD) scale and the Patient Health
Questionnaire (PHQ-9).
Behavioural couples Delivery
therapy
Hospital Anxiety and Depression (HAD) scale
typically 15-20 sessions over 5-6 months
consists of 14 questions, 7 for anxiety and
7 for depression
For people who decline the options above, each item is scored from 0-3
consider: produces a score out of 21 for both
anxiety and depression
severity: 0-7 normal, 8-10 borderline, 11+
counselling for people with persistent case
subthreshold depressive symptoms or patients should be encouraged to answer
mild to moderate depression; offer 6-10 the questions quickly
sessions over 8-12 weeks
short-term psychodynamic psychotherapy
for people with mild to moderate Patient Health Questionnaire (PHQ-9)
depression; offer 16-20 sessions over 4-6
months
asks patients 'over the last 2 weeks, how
often have you been bothered by any of
For patients with chronic physical health problems the following problems?'
the following should be offered: 9 items which can then be scored 0-3
includes items asking about thoughts of
self-harm
group-based CBT depression severity: 0-4 none, 5-9 mild,
individual CBT 10-14 moderate, 15-19 moderately
severe, 20-27 severe
Depression: screening and assessment
NICE use the DSM-IV criteria to grade depression:
Screening
1. Depressed mood most of the day,
The following two questions can be used to screen nearly every day
for depression 2. Markedly diminished interest or
pleasure in all, or almost all, activities
most of the day, nearly every day
'During the last month, have you often 3. Significant weight loss or weight gain
been bothered by feeling down, when not dieting or decrease or increase
depressed or hopeless?' in appetite nearly every day
'During the last month, have you often 4. Insomnia or hypersomnia nearly every
been bothered by having little interest or day
pleasure in doing things?' 5. Psychomotor agitation or retardation
nearly every day
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
6. Fatigue or loss of energy nearly every
day Switching from citalopram, escitalopram,
7. Feelings of worthlessness or excessive sertraline, or paroxetine to venlafaxine
or inappropriate guilt nearly every day
8. Diminished ability to think or
concentrate, or indecisiveness nearly cross-taper cautiously. Start venlafaxine
every day 37.5 mg daily and increase very slowly
9. Recurrent thoughts of death, recurrent
suicidal ideation without a specific plan,
or a suicide attempt or a specific plan for
Switching from fluoxetine to venlafaxine
committing suicide
withdraw and then start venlafaxine at
Subthreshold depressive
37.5 mg each day and increase very slowly
symptoms
Mild depression Few, if any, symptoms in excess of the 5 required to make the diagnosis, and symptoms result in
only minor functional impairment
*this means gradually reduce the dose then stop
Moderate depression Symptoms or functional impairment are between 'mild' and 'severe'
Severe depression Most symptoms, and the symptoms markedly interfere
Electroconvulsive therapywith functioning. Can occur with or
without psychotic symptoms
Depression: switching antidepressants Electroconvulsive therapy is a useful treatment
option for patients with severe depression
refractory to medication (e.g. catatonia) those with
The following is based on the Clinical Knowledge psychotic symptoms. The only absolute
Summaries depression guidelines, which in turn contraindications is raised intracranial pressure.
are based on the Maudsley hospital guidelines.
Short-term side-effects
Switching from citalopram, escitalopram,
sertraline, or paroxetine to another SSRI
headache
nausea
the first SSRI should be withdrawn* short term memory impairment
before the alternative SSRI is started memory loss of events prior to ECT
cardiac arrhythmia
Switching from fluoxetine to another SSRI
Long-term side-effects
withdraw then leave a gap of 4-7 days (as
it has a long half-life) before starting a some patients report impaired memory
low-dose of the alternative SSRI
Generalised anxiety disorder
Switching from a SSRI to a tricyclic antidepressant
(TCA)
Management
cross-tapering is recommend (the current
drug dose is reduced slowly, whilst the SSRI anti-depressants
dose of the new drug is increased slowly) buspirone (5-HT1A partial agonist)
beta-blockers
- an exceptions is fluoxetine which should be benzodiazepines: use longer acting
withdrawn prior to TCAs being started preparations e.g. diazepam, clonazepam
cognitive behaviour therapy
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
thinking and self-harm. Weekly follow-up
Generalised anxiety disorder and panic disorder is recommended for the first month
Anxiety is a common disorder that can present in
multiple ways. NICE define the central feature as
Management of panic disorder
an 'excessive worry about a number of different
events associated with heightened tension.'
Again a stepwise approach:
Always look for a potential physical cause when
considering a psychiatric diagnosis. In anxiety
disorders, important alternative causes include step 1: recognition and diagnosis
hyperthyroidism, cardiac disease and medication- step 2: treatment in primary care - see
induced anxiety (NICE). Medications that may below
trigger anxiety include salbutamol, theophylline, step 3: review and consideration of
corticosteroids, antidepressants and caffeine alternative treatments
step 4: review and referral to specialist
mental health services
Management of generalised anxiety disorder step 5: care in specialist mental health
(GAD) services
NICE suggest a step-wise approach:
Treatment in primary care
step 1: education about GAD + active
monitoring NICE recommend either cognitive
step 2: low intensity psychological behavioural therapy or drug treatment
interventions (individual non-facilitated SSRIs are first-line. If contraindicated or no
self-help or individual guided self-help or response after 12 weeks then imipramine
psychoeducational groups) or clomipramine should be offered
step 3: high intensity psychological
interventions (cognitive behavioural
therapy or applied relaxation) or drug Grief reaction
treatment. See drug treatment below for
more information
step 4: highly specialist input e.g. Multi It is normal for people to feel sadness and grief
agency teams following the death of a loved one and this does
not necessarily need to be medicalised. However,
having some understanding of the potential stages
Drug treatment a person may go through whilst grieving can help
determine whether a patient is having a 'normal'
grief reaction or is developing a more significant
problem.
NICE suggest sertraline should be
considered the first-line SSRI One of the most popular models of grief divides it
if sertraline is ineffective, offer into 5 stages.
an alternative SSRI or a serotonin–
noradrenaline reuptake inhibitor (SNRI)
o examples of SNRIs include
duloxetine and venlafaxine Denial: this may include a feeling of
If the person cannot tolerate SSRIs or numbness and also pseudohallucinations
SNRIs, consider offering pregabalin of the deceased, both auditory and visual.
interestingly for patients under the age of Occasionally people may focus on physical
30 years NICE recommend you warn objects that remind them of their loved
patients of the increased risk of suicidal one or even prepare meals for them
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Anger: this is commonly directed against
other family members and medical Speech and thought
professionals
Bargaining
Depression pressured
Acceptance flight of ideas: characterised by rapid
speech with frequent changes in topic
based on associations, distractions or
It should be noted that many patients will not go word play
through all 5 stages. poor attention
Abnormal, or atypical, grief reactions are more
likely to occur in women and if the death is sudden Behaviour
and unexpected. Other risk factors include a
problematic relationship before death or if the
patient has not much social support.
insomnia
Features of atypical grief reactions include: loss of inhibitions: sexual promiscuity,
overspending, risk-taking
increased appetite
delayed grief: sometimes said to occur
when more than 2 weeks passes before
Insomnia
grieving begins
prolonged grief: difficult to define. Normal
grief reactions may take up to and beyond
Insomnia is one of the most commonly reported
12 months
problems in primary care, and can be associated
with other physical and mental health complaints.
In the DSM-V, insomnia is defined as difficulty
Hypomania vs. mania initiating or maintaining sleep, or early-morning
awakening that leads to dissatisfaction with sleep
quantity or quality. This is despite adequate time
Mania and opportunity for sleep and results in impaired
daytime functioning.
Lasts for at least 7 days - Causes severe
functional impairment in social and work setting Insomnia may be considered acute or chronic.
May require hospitalization due to risk of harm Acute insomnia is more typically related to a life
to self or others event and resolves without treatment. Chronic
May present with psychotic symptoms insomnia may be diagnosed if a person has trouble
falling asleep or staying asleep at least three nights
per week for 3 months or longer.
Therefore, the length of symptoms, severity and
Patients typically present with decreased daytime
presence of psychotic symptoms (e.g. delusions of
functioning, decreased periods of sleep (delayed
grandeur, auditory hallucinations) helps
sleep onset or awakening in the night) or increased
differentiates mania from hypomania.
accidents due to poor concentration. Often the
partner's rest will also suffer. It is important to
The following symptoms are common to both
identify the aetiology of the insomnia, as
hypomania and mania
management can differ.
Mood
The following features are associated with
insomnia:
predominately elevated
irritable
Female gender
Increased age
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Lower educational attainment Identify any potential causes e.g. mental/
Unemployment physical health issues or poor sleep
Economic inactivity hygiene.
Widowed, divorced, or separated status Advise the person not to drive while
sleepy.
Advise good sleep hygiene: no screens
Other risk factors include: before bed, limited caffeine intake, fixed
bed times etc.
ONLY consider use of hypnotics if daytime
impairment is severe.
Alcohol and substance abuse
Stimulant usage
Medications such as corticosteroids
Poor sleep hygiene There is good evidence for the efficacy of hypnotic
Chronic pain drugs in short-term insomnia. However, there are
Chronic illness: patients with illnesses many adverse effects e.g. daytime sedation, poor
such as diabetes, CAD, hypertension, motor coordination, cognitive impairment and
heart failure, BPH and COPD have a higher related concerns about accidents and injuries. In
prevalence of insomnia than the general addition, tolerance to the hypnotic effects of
population. benzodiazepines may be rapid (within a few days
Psychiatric illness: anxiety and depression or weeks of regular use).
are highly correlated with insomnia.
People with manic episodes or PTSD will Guidance on using hypnotics:
also complain of extended periods of
sleeplessness.
The hypnotics recommended for treating
insomnia are short-acting
Less common diagnostic factors may include: benzodiazepines or non-benzodiazepines
(zopiclone, zolpidem and zaleplon).
Diazepam is not recommended but can be
useful if the insomnia is linked to daytime
Daytime napping
anxiety.
Enlarged tonsils or tongue
Use the lowest effective dose for the
Micrognathia (small jaw) and retrognathia
shortest period possible.
Lateral narrowing of oropharynx
If there has been no response to the first
hypnotic, do not prescribe another. You
should make the patient aware that
Investigations: repeat prescriptions are not usually given.
It is important to review after 2 weeks and
consider referral for cognitive behavioural
Diagnosis is primarily made through therapy (CBT).
patient interview, looking for the presence
of risk factors.
Sleep diaries and actigraphy may aid Other sedative drugs (such as antidepressants,
diagnosis. Actigraphy is a non-invasive antihistamines, choral hydrate, clomethiazole and
method for monitoring motor activity. barbiturates) are not recommended for managing
Polysomnography is not routinely insomnia.
indicated. It may be considered in patients
with suspected obstructive sleep apnoea Lithium
or periodic limb movement disorder, or
when insomnia is poorly responsive to
conventional treatment. Lithium is mood stabilising drug used most
commonly prophylactically in bipolar disorder but
also as an adjunct in refractory depression. It has a
Short-term management of insomnia: very narrow therapeutic range (0.4-1.0 mmol/L)
and a long plasma half-life being excreted primarily
by the kidneys.
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Mental state examination
Mechanism of action - not fully understood, two
theories:
Thought disorders
Circumstantiality is the inability to answer a
interferes with inositol triphosphate
question without giving excessive, unnecessary
formation
detail. However, this differs from tangentiality in
interferes with cAMP formation
that the person does eventually return the original
point.
Adverse effects
Tangentiality refers to wandering from a topic
without returning to it.
nausea/vomiting, diarrhoea Neoligisms are new word formations, which might
fine tremor include the combining of two words.
nephrotoxicity: polyuria, secondary to
nephrogenic diabetes insipidus Clang associations are when ideas are related to
thyroid enlargement, may lead each other only by the fact they sound similar or
to hypothyroidism rhyme.
ECG: T wave flattening/inversion
weight gain Word salad is completely incoherent speech where
idiopathic intracranial hypertension real words are strung together into nonsense
leucocytosis sentences.
hyperparathyroidism and resultant
hypercalcaemia Knight's move thinking is a severe type of
loosening of associations, where there are
unexpected and illogical leaps from one idea to
Monitoring of patients on lithium therapy another. It is a feature of schizophrenia.
Flight of ideas, a feature of mania, is thought
disorder where there are leaps from one topic to
inadequate monitoring of patients taking
another but with discernible links between them.
lithium is common - NICE and the
National Patient Safety Agency (NPSA)
Perseveration is the repetition of ideas or words
have issued guidance to try and address
despite an attempt to change the topic.
this. As a result it is often an exam hot
topic
Echolalia is the repetition of someone else's
when checking lithium levels, the sample
speech, including the question that was asked.
should be taken 12 hours post-dose
after starting lithium levels should be
Mirtazapine
performed weekly and after each dose
change until concentrations are stable
once established, lithium blood level
Mirtazapine is an antidepressant that works by
should 'normally' be checked every 3
blocking alpha2-adrenergic receptors, which
months
increases the release of neurotransmitters.
after a change in dose, lithium levels
should be taken a week later and weekly
Mirtazapine has fewer side effects and interactions
until the levels are stable.
than many other antidepressants and so is useful
thyroid and renal function should be
in older people who may be affected more or be
checked every 6 months
taking other medications. Two side effects of
patients should be issued with an
mirtazapine, sedation and an increased appetite,
information booklet, alert card and record
can be beneficial in older people that are suffering
book
from insomnia and poor appetite.
It is generally taken in the evening as it can be
sedative.
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Monoamine oxidase inhibitors The aetiology is multifactorial but possible factors
include:
Overview
genetic
psychological trauma
serotonin and noradrenaline are pediatric autoimmune neuropsychiatric
metabolised by monoamine oxidase in disorder associated with streptococcal
the presynaptic cell infections (PANDAS)
Non-selective monoamine oxidase inhibitors Associations
e.g. tranylcypromine, phenelzine depression (30%)
used in the treatment of atypical schizophrenia (3%)
depression (e.g. hyperphagia) and other Sydenham's chorea
psychiatric disorder Tourette's syndrome
not used frequently due to side-effects anorexia nervosa
Adverse effects of non-selective monoamine Management
oxidase inhibitors
If functional impairment is mild
hypertensive reactions with tyramine o low-intensity psychological
containing foods e.g. cheese, pickled treatments: cognitive
herring, Bovril, Oxo, Marmite, broad behavioural therapy (CBT)
beans including exposure and response
anticholinergic effects prevention (ERP)
o If this is insufficient or can’t
engage in psychological therapy,
Obsessive-compulsive disorder then offer choice of either a
course of an SSRI or more
intensive CBT (including ERP)
Obsessive-compulsive disorder (OCD) is If moderate functional impairment
characterised by the presence of either obsessions o offer a choice of either a course
or compulsions, but commonly both. The of an SSRI (any SSRI for OCD but
symptoms can cause significant functional fluoxetine specifically for body
impairment and/ or distress. dysmorphic disorder) or more
intensive CBT (including ERP)
An obsession is defined as an unwanted intrusive If severe functional impairment
thought, image or urge that repeatedly enters the o offer combined treatment with
person's mind. Compulsions are repetitive an SSRI and CBT (including ERP)
behaviours or mental acts that the person feels
driven to perform. A compulsion can either be
overt and observable by others, such as checking Notes on treatments
that a door is locked, or a covert mental act that
cannot be observed, such as repeating a certain
phrase in one's mind.
ERP is a psychological method which
It is thought that 1 to 2% of the population have involves exposing a patient to an anxiety
OCD, although some studies have estimated 2 to provoking situation (e.g. for someone
3%. with OCD, having dirty hands) and then
stopping them engaging in their usual
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
safety behaviour (e.g. washing their Disorder Features
hands). This helps them confront their Physical appearance used for attention seeking purposes
anxiety and the habituation leads to the Impressionistic speech lacking detail
eventual extinction of the response Self dramatization
if treatment with SSRI is effective then Relationships considered to be more intimate than they are
continue for at least 12 months to preventNarcissistic Grandiose sense of self importance
relapse and allow time for improvement Preoccupation with fantasies of unlimited success, power, or beauty
If SSRI ineffective or not tolerated try Sense of entitlement, taking advantage of others to achieve own needs
Lack of empathy
either another SSRI
Excessive need for admiration
Chronic envy
Arrogant and haughty attitude
Othello's syndrome Obsessive- Is occupied with details, rules, lists, order, organization, or agenda to the
compulsive Demonstrates perfectionism that hampers with completing tasks
Is extremely dedicated to work and efficiency to the elimination of spare ti
Othello's syndrome is pathological jealousy where Is meticulous, scrupulous, and rigid about etiquettes of morality, ethics, o
a person is convinced their partner is cheating on Is not capable of disposing worn out or insignificant things even when the
them without any real proof. This is accompanied Is unwilling to pass on tasks or work with others except if they surrender t
by socially unacceptable behaviour linked to these Takes on a stingy spending style towards self and others; and shows stiffn
claims. Paranoid Hypersensitivity and an unforgiving attitude when insulted
Unwarranted tendency to questions the loyalty of friends
Reluctance to confide in others
Personality Disorders Preoccupation with conspirational beliefs and hidden meaning
Disorder Features Unwarranted tendency to perceive attacks on their character
Antisocial Failure to conform to social norms with respect to lawful behaviorsIndifference
Schizoid as indicatedtobypraise
repeatedly performing acts that are grounds for
and criticism
arrest; Preference for solitary activities
More common in men; Lack of interest in sexual interactions
Deception, as indicated by repeatedly lying, use of aliases, or conning
Lackothers for personal
of desire profit or pleasure;
for companionship
Impulsiveness or failure to plan ahead; Emotional coldness
Irritability and aggressiveness, as indicated by repeated physical fights
Feworinterests
assaults;
Reckless disregard for safety of self or others; Few friends or confidants other than family
Consistent irresponsibility, as indicated by repeated failure to sustain consistent work behavior or honor financial obligations;
Schizotypal Ideas of reference (differ from delusions in that some insight is retained)
Lack of remorse, as indicated by being indifferent to or rationalizing having hurt, mistreated, or stolen from another
Odd beliefs and magical thinking
Avoidant Avoidance of occupational activities which involve significant interpersonal
Unusual contact duedisturbances
perceptual to fears of criticism, or rejection.
Unwillingness to be involved unless certain of being liked Paranoid ideation and suspiciousness
Preoccupied with ideas that they are being criticised or rejected in social situationsbehaviour
Odd, eccentric
Restraint in intimate relationships due to the fear of being ridiculedLack of close friends other than family members
Reluctance to take personal risks doe to fears of embarrassment Inappropriate affect
Views self as inept and inferior to others Odd speech without being incoherent
Social isolation accompanied by a craving for social contact - Tx: TT, dialectical behavioural therapy,
Borderline Efforts to avoid real or imagined abandonment mentalization, therapeutic communities
Unstable interpersonal relationships which alternate between idealization and devaluation
Unstable self image
Impulsivity in potentially self damaging area (e.g. Spending, sex,Post-concussion
substance abuse)syndrome
Recurrent suicidal behaviour
Affective instability
Chronic feelings of emptiness Post-concussion syndrome is seen after even minor
Difficulty controlling temper head trauma
Quasi psychotic thoughts
Dependent Difficulty making everyday decisions without excessive reassurance Typical
fromfeatures
others include
Need for others to assume responsibility for major areas of their life
Difficulty in expressing disagreement with others due to fears of losing support
Lack of initiative
Unrealistic fears of being left to care for themselves headache
Urgent search for another relationship as a source of care and support fatigue
when a close relationship ends
Extensive efforts to obtain support from others anxiety/depression
Unrealistic feelings that they cannot care for themselves dizziness
Histrionic Inappropriate sexual seductiveness
Need to be the centre of attention
Rapidly shifting and shallow expression of emotions Post-traumatic stress disorder
Suggestibility
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Post-traumatic stress disorder (PTSD) can develop
in people of any age following a traumatic event, Pseudohallucinations
for example, a major disaster or childhood sexual
abuse. It encompasses what became known as
'shell shock' following the first world war. One of ICD10 definition of hallucination: false sensory
the DSM-IV diagnostic criteria is that symptoms perception in the absence of an external stimulus.
have been present for more than one month. Maybe organic, drug-induced or associated with
mental disorder.
Features
The definition of a pseudohallucination is harder to
pin down. There is no mention of
pseudohallucinations in either the ICD10 nor the
re-experiencing: flashbacks, nightmares,
DSM-5. However, there is a generally accepted
repetitive and distressing intrusive images
definition that a pseudohallucination is a false
avoidance: avoiding people, situations or
sensory perception in the absence of external
circumstances resembling or associated
stimuli when the affected is aware that they are
with the event
hallucinating.
hyperarousal: hypervigilance for threat,
exaggerated startle response, sleep
There is disagreement among specialists about not
problems, irritability and difficulty
only the definition but also the role in the
concentrating
treatment of pseudohallucinations. Many
emotional numbing - lack of ability to
specialists feel that it is more appropriate to think
experience feelings, feeling detached
about hallucinations on a spectrum from mild
sensory disturbance to hallucinations to prevent
from other people
symptoms from being mistreated or misdiagnosed.
An example of a pseudohallucination is a
depression hypnagogic hallucination which occurs when
drug or alcohol misuse transitioning from wakefulness to sleep. These are
anger experienced vivid auditory or visual hallucinations
unexplained physical symptoms which are fleeting in duration and may occur in
anyone. These are pseudohallucinations as the
affected person is able to determine that the
Management hallucination was not real.
The relevance of pseudohallucinations in practice
is that patients may need reassurance that these
following a traumatic event single-session
experiences are normal and do not mean that they
interventions (often referred to as
will develop a mental illness.
debriefing) are not recommended
watchful waiting may be used for mild
Pseudohallucinations commonly occur in people
symptoms lasting less than 4 weeks
who are grieving.
military personnel have access to
treatment provided by the armed forces
Psychosis
trauma-focused cognitive behavioural
therapy (CBT) or eye movement
desensitisation and reprocessing (EMDR)
Psychosis is a term used to describe a person
therapy may be used in more severe cases
experiencing things differently from those around
drug treatments for PTSD should not be
them.
used as a routine first-line treatment for
adults. If drug treatment is used
Psychotic features include:
then venlafaxine or a selective serotonin
reuptake inhibitor (SSRI), such as
sertraline should be tried. In severe cases,
NICE recommends that risperidone may hallucinations (e.g. auditory)
be used delusions
thought disorganisation
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
o alogia: little information parent has schizophrenia = 10-15%
conveyed by speech sibling has schizophrenia = 10%
o tangentiality: answers diverge no relatives with schizophrenia = 1%
from topic
o clanging
o word salad: linking real words Other selected risk factors for psychotic disorders
incoherently → nonsensical include:
content
Black Caribbean ethnicity - RR 5.4
Associated features: Migration - RR 2.9
Urban environment- RR 2.4
Cannabis use - RR 1.4
agitation/aggression
neurocognitive impairment (e.g. in
memory, attention or executive function) Schizophrenia: epidemiology
depression
thoughts of self harm
The strongest risk factor for developing a psychotic
disorder (including schizophrenia) is family history.
Psychotic symptoms may occur in a number of Having a parent with schizophrenia leads to a
conditions: relative risk (RR) of 7.5.
Risk of developing schizophrenia
schizophrenia
depression (psychotic depression, a
subtype more common in elderly monozygotic twin has schizophrenia =
patients) 50%
bipolar disorder parent has schizophrenia = 10-15%
puerperal psychosis sibling has schizophrenia = 10%
brief psychotic disorder: where symptoms no relatives with schizophrenia = 1%
last less than a month
neurological conditions e.g. Parkinson's
disease, Huntington's disease Other selected risk factors for psychotic disorders
prescribed drugs e.g. corticosteroids include:
certain illicit drugs e.g. cannabis,
phencyclidine
Black Caribbean ethnicity - RR 5.4
Migration - RR 2.9
The peak age of first-episode psychosis is around Urban environment- RR 2.4
15-30 years. Cannabis use - RR 1.4
Schizophrenia: epidemiology
Schizophrenia: features
The strongest risk factor for developing a psychotic
disorder (including schizophrenia) is family history. Schneider's first rank symptoms may be divided
Having a parent with schizophrenia leads to a into auditory hallucinations, thought disorders,
relative risk (RR) of 7.5. passivity phenomena and delusional perceptions:
Risk of developing schizophrenia Auditory hallucinations of a specific type:
monozygotic twin has schizophrenia = two or more voices discussing the patient
50% in the third person
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
thought echo NICE published guidelines on the management of
voices commenting on the patient's schizophrenia in 2009.
behaviour
Key points:
Thought disorder*:
oral atypical antipsychotics are first-line
cognitive behavioural therapy should be
thought insertion offered to all patients
thought withdrawal close attention should be paid to
thought broadcasting cardiovascular risk-factor modification
due to the high rates of cardiovascular
disease in schizophrenic patients (linked
Passivity phenomena: to antipsychotic medication and high
smoking rates)
bodily sensations being controlled by
Schizophrenia: prognostic indicators
external influence
actions/impulses/feelings - experiences
which are imposed on the individual or
Factors associated with poor prognosis
influenced by others
Delusional perceptions strong family history
gradual onset
low IQ
prodromal phase of social withdrawal
a two stage process) where first a normal lack of obvious precipitant
object is perceived then secondly there is
a sudden intense delusional insight into
the objects meaning for the patient e.g.
Seasonal affective disorder
'The traffic light is green therefore I am
the King'.
Seasonal affective disorder (SAD) describes
depression which occurs predominately around
Other features of schizophrenia include the winter months. SAD should be treated the
same way as depression, therefore as per the NICE
guidelines for mild depression, you would begin
impaired insight with psychological therapies and follow up with
incongruity/blunting of affect the patient in 2 weeks to ensure that there has
(inappropriate emotion for circumstances) been no deterioration. Following this an SSRI can
decreased speech be given if needed. In seasonal affective disorder,
neologisms: made-up words you should not give the patient sleeping tablets as
catatonia this can make the symptoms worse. Finally, the
negative symptoms: incongruity/blunting evidence for light therapy is limited and as such it
of affect, anhedonia (inability to derive is not routinely recommended.
pleasure), alogia (poverty of speech),
avolition (poor motivation) Sectioning under the Mental Health Act
*occasionally referred to as thought alienation This is used for someone over the age of 16 years
who will not be admitted voluntarily. Patients who
Schizophrenia: management are under the influence of alcohol or drugs are
specifically excluded
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Section 2
Section 17a
admission for assessment for up to 28
days, not renewable Supervised Community Treatment
an Approved Mental Health Professional (Community Treatment Order)
(AMHP) or rarely the nearest relative (NR) can be used to recall a patient to hospital
makes the application on the for treatment if they do not comply with
recommendation of 2 doctors conditions of the order in the community,
one of the doctors should be 'approved' such as complying with medication
under Section 12(2) of the Mental Health
Act (usually a consultant psychiatrist)
treatment can be given against a patient's Section 135
wishes
a court order can be obtained to allow the
Section 3 police to break into a property to remove
a person to a Place of Safety
admission for treatment for up to 6
months, can be renewed Section 136
AMHP along with 2 doctors, both of which
must have seen the patient within the
past 24 hours
someone found in a public place who
treatment can be given against a patient's
appears to have a mental disorder can be
wishes
taken by the police to a Place of Safety
can only be used for up to 24 hours, whilst
a Mental Health Act assessment is
Section 4 arranged
72 hour assessment order Selective serotonin reuptake inhibitors
used as an emergency, when a section 2
would involve an unacceptable delay
a GP and an AMHP or NR Selective serotonin reuptake inhibitors (SSRIs) are
often changed to a section 2 upon arrival considered first-line treatment for the majority of
at hospital patients with depression.
Section 5(2) citalopram (although see below re: QT
interval) and fluoxetine are currently the
preferred SSRIs
a patient who is a voluntary patient in sertraline is useful post myocardial
hospital can be legally detained by a infarction as there is more evidence for its
doctor for 72 hours safe use in this situation than other
antidepressants
SSRIs should be used with caution
Section 5(4) in children and adolescents. Fluoxetine is
the drug of choice when an
antidepressant is indicated
similar to section 5(2), allows a nurse to
detain a patient who is voluntarily in
Adverse effects
hospital for 6 hours
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
gastrointestinal symptoms are the most continue on treatment for at least 6 months after
common side-effect remission as this reduces the risk of relapse.
there is an increased risk of
gastrointestinal bleeding in patients taking When stopping a SSRI the dose should be gradually
SSRIs. A proton pump inhibitor should be reduced over a 4 week period (this is not necessary
prescribed if a patient is also taking a with fluoxetine). Paroxetine has a higher incidence
NSAID of discontinuation symptoms.
patients should be counselled to be
vigilant for increased anxiety and agitation Discontinuation symptoms
after starting a SSRI
fluoxetine and paroxetine have a higher
propensity for drug interactions increased mood change
restlessness
difficulty sleeping
Citalopram and the QT interval unsteadiness
sweating
gastrointestinal symptoms: pain,
the Medicines and Healthcare products cramping, diarrhoea, vomiting
Regulatory Agency (MHRA) released a paraesthesia
warning on the use of citalopram in 2011
it advised that citalopram and
escitalopram are associated with dose- SSRIs and pregnancy
dependent QT interval prolongation and - BNF says to weigh up benefits and risk when
should not be used in those with: deciding whether to use in pregnancy.
congenital long QT syndrome; known pre- - Use during the first trimester gives a small
existing QT interval prolongation; or in increased risk of congenital heart defects
combination with other medicines that - Use during the third trimester can result
prolong the QT interval in persistent pulmonary hypertension of the
the maximum daily dose is now 40 mg for newborn
adults; 20 mg for patients older than 65 - Paroxetine has an increased risk of congenital
years; and 20 mg for those with hepatic malformations, particularly in the first trimester
impairment
Serotonin and noradrenaline reuptake inhibitors
Interactions
Serotonin and noradrenaline reuptake inhibitor
(SNRI's) are a class of relatively new
antidepressants. Inhibiting the reuptake increases
NSAIDs: NICE guidelines advise 'do not
the concentrations of serotonin and noradrenaline
normally offer SSRIs', but if given co-
in the synaptic cleft leading to the effects.
prescribe a proton pump inhibitor
Examples include venlafaxine and duloxetine. They
warfarin / heparin: NICE guidelines
are used to treat major depressive disorders,
recommend avoiding SSRIs and
generalised anxiety disorder, social anxiety
considering mirtazapine
disorder and panic disorder and menopausal
aspirin: see above
symptoms.
triptans - increased risk of serotonin
syndrome
Sleep paralysis
monoamine oxidase inhibitors (MAOIs) -
increased risk of serotonin syndrome
Sleep paralysis is a common condition
characterized by transient paralysis of skeletal
Following the initiation of antidepressant therapy muscles which occurs when awakening from sleep
patients should normally be reviewed by a doctor or less often while falling asleep. It is thought to be
after 2 weeks. For patients under the age of 30 related to the paralysis that occurs as a natural
years or at increased risk of suicide they should be part of REM (rapid eye movement) sleep. Sleep
reviewed after 1 week. If a patient makes a good paralysis is recognised in a wide variety of cultures
response to antidepressant therapy they should
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Features Interactions
paralysis - this occurs after waking up or NSAIDs: NICE guidelines advise 'do not
shortly before falling asleep normally offer SSRIs', but if given co-
hallucinations - images or speaking that prescribe a proton pump inhibitor
appear during the paralysis warfarin / heparin: NICE guidelines
recommend avoiding SSRIs and
considering mirtazapine
Management aspirin: see above
triptans: avoid SSRIs
if troublesome clonazepam may be used
Following the initiation of antidepressant therapy
patients should normally be reviewed by a doctor
after 2 weeks. For patients under the age of 30
SSRI: side-effects
years or at increased risk of suicide they should be
reviewed after 1 week. If a patient makes a good
response to antidepressant therapy they should
Adverse effects
continue on treatment for at least 6 months after
remission as this reduces the risk of relapse.
gastrointestinal symptoms are the most When stopping a SSRI the dose should be gradually
common side-effect reduced over a 4 week period (this is not necessary
there is an increased risk of with fluoxetine). Paroxetine has a higher incidence
gastrointestinal bleeding in patients taking of discontinuation symptoms.
SSRIs. A proton pump inhibitor should be
prescribed if a patient is also taking a Discontinuation symptoms
NSAID
hyponatraemia
patients should be counselled to be
increased mood change
vigilant for increased anxiety and agitation
restlessness
after starting a SSRI
difficulty sleeping
fluoxetine and paroxetine have a higher
unsteadiness
propensity for drug interactions
sweating
gastrointestinal symptoms: pain,
cramping, diarrhoea, vomiting
Citalopram and the QT interval
paraesthesia
the Medicines and Healthcare products Suicide: risk factors
Regulatory Agency (MHRA) released a
warning on the use of citalopram in 2011
it advised that citalopram and The risk stratification of psychiatric patients into
escitalopram are associated with dose- 'high', 'medium' or 'low risk' is common in clinical
dependent QT interval prolongation and practice. Questions based on a patient's suicide
should not be used in those with: risk are therefore often seen. However, it should be
congenital long QT syndrome; known pre- noted that there is a paucity of evidence
existing QT interval prolongation; or in addressing the positive predictive value of
combination with other medicines that individual risk factors. An interesting review in the
prolong the QT interval BMJ (BMJ 2017;359:j4627) concluded that 'there is
the maximum daily dose is now 40 mg for no evidence that these assessments can usefully
adults; 20 mg for patients older than 65 guide decision making' and noted that 50% of
years; and 20 mg for those with hepatic suicides occur in patients deemed 'low risk'.
impairment
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Whilst the evidence base is relatively weak, there used widely in the treatment of neuropathic pain,
are a number of factors shown to be associated where smaller doses are typically required.
with an increased risk of suicide
Common side-effects
male sex (hazard ratio (HR) approximately
2.0) drowsiness
history of deliberate self-harm (HR 1.7) dry mouth
alcohol or drug misuse (HR 1.6) blurred vision
history of mental illness constipation
o depression urinary retention
o schizophrenia: NICE estimates lengthening of QT interval
that 10% of people with
schizophrenia will complete
suicide Choice of tricyclic
history of chronic disease
advancing age
unemployment or social isolation/living low-dose amitriptyline is commonly used
alone in the management of neuropathic pain
being unmarried, divorced or widowed and the prophylaxis of headache (both
tension and migraine)
lofepramine has a lower incidence of
If a patient has actually attempted suicide, there toxicity in overdose
are a number of factors associated with an amitriptyline and dosulepin (dothiepin)
increased risk of completed suicide at a future are considered the most dangerous in
date: overdose
efforts to avoid discovery More sedative
planning
Amitriptyline Im
leaving a written note
Clomipramine Lof
final acts such as sorting out finances
Dosulepin No
violent method
Trazodone*
*trazodone is technically a 'tricyclic-related
antidepressant'
Unexplained symptoms
Protective factors
There are, of course, factors which reduce the risk There are a wide variety of psychiatric terms for
of a patient committing suicide. These include patients who have symptoms for which no organic
cause can be found:
Somatisation disorder
family support
having children at home
religious belief
multiple physical SYMPTOMS present for
at least 2 years
patient refuses to accept reassurance or
Tricyclic antidepressants
negative test results
Tricyclic antidepressants (TCAs) are used less
commonly now for depression due to their side- Illness anxiety disorder (hypochondriasis)
effects and toxicity in overdose. They are however
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
persistent belief in the presence of an Z drugs have similar effects to benzodiazepines but
underlying serious DISEASE, e.g. cancer are different structurally. They act on the α2-
patient again refuses to accept subunit of the GABA receptor.
reassurance or negative test results
They can be divided into 3 groups:
Conversion disorder
Imidazopyridines: e.g. zolpidem
Cyclopyrrolones: e.g. zopiclone
typically involves loss of motor or sensory Pyrazolopyrimidines: e.g. zaleplon
function
the patient doesn't consciously feign the
symptoms (factitious disorder) or seek Adverse effects
material gain (malingering)
patients may be indifferent to their
apparent disorder - la belle indifference - similar to benzodiazepines
although this has not been backed up by increase the risk of falls in the elderly
some studies
Dissociative disorder Acute confusional state (Delirium)
dissociation is a process of 'separating off' Acute confusional state is also known as delirium
certain memories from normal or acute organic brain syndrome.
consciousness
in contrast to conversion disorder involves Predisposing factors include:
psychiatric symptoms e.g. Amnesia, Age > 65 years
fugue, stupor Background of dementia
dissociative identity disorder (DID) is the Significant injury e.g. Hip fracture
new term for multiple personality Frailty or multimorbidity
disorder as is the most severe form of Polypharmacy
dissociative disorder
The precipitating events are often multifactorial
and may include:
Factitious disorder Infection: particularly urinary tract
infections
Metabolic: e.g. Hypercalcaemia,
hypoglycaemia, hyperglycaemia,
also known as Munchausen's syndrome
dehydration
the intentional production of physical or
Change of environment
psychological symptoms
Any significant cardiovascular, respiratory,
neurological or endocrine condition
Severe pain
Malingering Alcohol withdrawal
Constipation
fraudulent simulation or exaggeration of Features - a wide variety of presentations
symptoms with the intention of financial Cognitive functions:
or other gain o memory disturbances (loss of
short term > long term)
Perception - Auditory or visual
Z drugs hallucination
Physical function - reduced morbidity,
reduce movement, restlessness, agitation
changes in appetite, sleep disturbance
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
Social behaviour - may be very agitated or point cognitive screener (10-CS), 6-Item
withdrawn, Lack of cooperation cognitive impairment test (6CIT)
assessment tools not recommended by
Management NICE for the non-specialist setting include
- treatment of the underlying cause the abbreviated mental test score (AMTS),
- modification of the environment General practitioner assessment of
- the 2006 Royal College of Physicians cognition (GPCOG) and the mini-mental
publication 'The prevention, diagnosis and state examination (MMSE) have been
management of delirium in older people: widely used. A MMSE score of 24 or less
concise guidelines' out of 30 suggests dementia
recommended haloperidol 0.5 mg as the
first-line sedative
- the 2010 NICE delirium guidelines Management
advocate the use of haloperidol or
olanzapine IM (SE - alteration in blood
pressure, stroke, insomnia, dyspepsia)
in primary care, a blood screen is usually
- management can be challenging in
sent to exclude reversible causes (e.g.
patients with Parkinson's disease, as
Hypothyroidism). NICE recommend the
antipsychotics can often worsen
following tests: FBC, U&E, LFTs, calcium,
Parkinsonian symptoms
glucose, TFTs, vitamin B12 and folate
- careful reduction of the Parkinson
levels. Patients are now commonly
medication may be helpful
referred on to old-age psychiatrists
- if symptoms require urgent treatment
(sometimes working in 'memory clinics').
then the atypical
in secondary care, neuroimaging is
antipsychotics quetiapine and clozapine
performed* to exclude other reversible
are preferred
conditions (e.g. Subdural haematoma,
normal pressure hydrocephalus) and help
differential diagnosis:
provide information on aetiology to guide
- withdrawal from alcohol or drugs
prognosis and management
- mania
- psychosis or anxiety
Dementia vs Delirium *in the 2011 NICE guidelines structural imaging
was said to be essential in the investigation of
dementia
Factors favouring delirium over dementia
Impairment of consciousness
Fluctuation of symptoms: worse at night, Dementia: causes
periods of normality
Abnormal perception (e.g. Illusions and
hallucinations) Common causes
Agitation, fear
Delusions
Alzheimer's disease
Dementia cerebrovascular disease: multi-infarct
dementia (c. 10-20%)
Lewy body dementia (c. 10-20%)
Common cause of dementia in the UK is
Alzheimer's disease followed by vascular and Lewy
body dementia. These conditions may coexist. Rarer causes (c. 5% of cases)
Features
Huntington's
diagnosis can be difficult and is often
CJD
delayed
Pick's disease (atrophy of frontal and
assessment tools recommended by NICE
temporal lobes)
for the non-specialist setting include: 10-
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
HIV (50% of AIDS patients)
Risk factors
Important differentials, potentially treatable
History of stroke or transient ischaemic
attack (TIA)
hypothyroidism, Addison's Atrial fibrillation
B12/folate/thiamine deficiency Hypertension
syphilis Diabetes mellitus
brain tumour Hyperlipidaemia
normal pressure hydrocephalus Smoking
subdural haematoma Obesity
depression Coronary heart disease
chronic drug use e.g. Alcohol, barbiturates A family history of stroke or
cardiovascular
Vascular dementia
Rarely, VD can be inherited as in the case of
Vascular dementia (VD) is the second most CADASIL (cerebral autosomal dominant
common form of dementia after Alzheimer arteriopathy with subcortical infarcts and
disease. It is not a single disease but a group of leukoencephalopathy.
syndromes of cognitive impairment caused by
different mechanisms causing ischaemia or Patients with VD typically presents with
haemorrhage secondary to cerebrovascular
disease. Vascular dementia has been increasingly
recognised as the most severe form of the Several months or several years of a
spectrum of deficits encompassed by the term history of a sudden or stepwise
vascular cognitive impairment (VCI). Early deterioration of cognitive function.
detection and an accurate diagnosis are important
in the prevention of vascular dementia.
Symptoms and the speed of progression vary but
Epidemiology
may include:
VD is thought to account for around 17%
Focal neurological abnormalities e.g.
of dementia in the UK
visual disturbance, sensory or motor
Prevalence of dementia following a first
symptoms
stroke varies depending on location and
The difficulty with attention and
size of the infarct, definition of dementia,
concentration
interval after stroke and age among other
Seizures
variables. Overall, stroke doubles the risk
Memory disturbance
of developing dementia.
Gait disturbance
Incidence increases with age
Speech disturbance
Emotional disturbance
The main subtypes of VD:
Diagnosis is made based on:
Stroke-related VD – multi-infarct or single-
infarct dementia
A comprehensive history and physical
Subcortical VD – caused by small vessel
examination
disease
Formal screen for cognitive impairment
Mixed dementia – the presence of both
Medical review to exclude medication
VD and Alzheimer’s disease
cause of cognitive decline
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
MRI scan – may show infarcts and There is no specific pharmacological
extensive white matter changes treatment approved for cognitive
symptoms
Only consider AChE inhibitors or
National Institute for health and care excellence memantine for people with vascular
(NICE) recommends that diagnosis be made using dementia if they have suspected
the NINDS-AIREN criteria for probable vascular comorbid Alzheimer’s disease, Parkinson’s
dementia disease dementia or dementia with Lewy
bodies.
Presence of cognitive decline that interferes with activities of daily living, not due to secondary effects of the
cerebrovascular event There is no evidence that aspirin is
effective in treating patients with a
diagnosis of vascular dementia.
No randomized trials found evaluating
established using clinical examination and neuropsychological testing
statins for vascular dementia
Cerebrovascular disease Lewy body dementia
defined by neurological signs and/or brain imaging Lewy body dementia is an increasingly recognised
cause of dementia, accounting for up to 20% of
cases. The characteristic pathological feature is
A relationship between the above two disorders inferred by:
alpha-synuclein cytoplasmic inclusions (Lewy
bodies) in the substantia nigra, paralimbic and
neocortical areas.
the onset of dementia within three months following a recognised stroke
an abrupt deterioration in cognitive functions The relationship between Parkinson's disease and
fluctuating, stepwise progression of cognitive deficits
Lewy body dementia is complicated, particularly as
dementia is often seen in Parkinson's disease. Also,
up to 40% of patients with Alzheimer's have Lewy
General management bodies.
Features
Treatment is mainly symptomatic with the
aim to address individual problems and
provide support to the patient and carers progressive cognitive impairment
Important to detect and address o in contrast to Alzheimer's, early
cardiovascular risk factors – for slowing impairments in attention and
down the progression executive function rather than
just memory loss
o cognition may be fluctuating, in
Non-pharmacological management contrast to other forms of
dementia
o usually develops before
parkinsonism
Tailored to the individual
parkinsonism
Include: cognitive stimulation
visual hallucinations (other features such
programmes, multisensory stimulation,
as delusions and non-visual hallucinations
music and art therapy, animal-assisted
may also be seen)
therapy
Managing challenging behaviours e.g.
address pain, avoid overcrowding, clear
communication Diagnosis
Pharmacological management usually clinical
single-photon emission computed
tomography (SPECT) is increasingly used.
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
It is currently commercially known as a by personality change and impaired social conduct.
DaTscan. Dopaminergic iodine-123- Other common features include hyperorality,
radiolabelled 2-carbomethoxy-3-(4- disinhibition, increased appetite, and
iodophenyl)-N-(3-fluoropropyl) perseveration behaviours.
nortropane (123-I FP-CIT) is used as the
radioisotope. The sensitivity of SPECT in Focal gyral atrophy with a knife-blade appearance
diagnosing Lewy body dementia is around is characteristic of Pick's disease.
90% with a specificity of 100%
Macroscopic changes seen in Pick's disease
include:-
Management
Atrophy of the frontal and temporal lobes
both acetylcholinesterase inhibitors (e.g.
donepezil, rivastigmine) and memantine
can be used as they are in Alzheimer's. Microscopic changes include:-
NICE have made detailed
recommendations about what drugs to
use at what stages. Please see the link for Pick bodies - spherical aggregations of tau
more details protein (silver-staining)
neuroleptics should be avoided in Lewy Gliosis
body dementia as patients are extremely Neurofibrillary tangles
sensitive and may develop irreversible Senile plaques
parkinsonism. Questions may give a
history of a patient who has deteriorated
following the introduction of an
Management
antipsychotic agent
Frontotemporal lobar degeneration
NICE do not recommend that AChE
inhibitors or memantine are used in
Frontotemporal lobar degeneration (FTLD) is the people with frontotemporal dementia
third most common type of cortical dementia after
Alzheimer's and Lewy body dementia.
There are three recognised types of FTLD CPA
Here the chief factor is non fluent speech. They
Frontotemporal dementia (Pick's disease) make short utterances that are agrammatic.
Progressive non fluent aphasia (chronic Comprehension is relatively preserved.
progressive aphasia, CPA)
Semantic dementia
Semantic dementia
Common features of frontotemporal lobar dementias
Here the patient has a fluent progressive aphasia.
Onset before 65 The speech is fluent but empty and conveys little
Insidious onset meaning. Unlike in Alzheimer's memory is better
Relatively preserved memory and visuospatial skills for recent rather than remote events.
Personality change and social conduct problems
Alzheimer's disease: management
Pick's disease
Alzheimer's disease is a progressive degenerative
disease of the brain accounting for the majority of
This is the most common type and is characterised dementia seen in the UK
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
lOMoARcPSD|6265699
is relatively contraindicated in patients
Non-pharmacological management with bradycardia
adverse effects include insomnia
NICE recommend offering 'a range of
activities to promote wellbeing that are
tailored to the person's preference'
NICE recommend offering group cognitive
stimulation therapy for patients with mild
and moderate dementia
other options to consider include group
reminiscence therapy and cognitive
rehabilitation
https://passmedicine.com/database/dbnotes.php
Pharmacological management
NICE updated it's dementia guidelines in
2018
the three acetylcholinesterase inhibitors
(donepezil, galantamine and rivastigmine)
as options for managing mild to moderate
Alzheimer's disease
memantine (an NMDA receptor
antagonist) is in simple terms the 'second-
line' treatment for Alzheimer's, NICE
recommend it is used in the following
situation reserved for patients with
o moderate Alzheimer's who are
intolerant of, or have a
contraindication to,
acetylcholinesterase inhibitors
o as an add-on drug to
acetylcholinesterase inhibitors
for patients with moderate or
severe Alzheimer's
o monotherapy in severe
Alzheimer's
Managing non-cognitive symptoms
NICE does not recommend
antidepressants for mild to moderate
depression in patients with dementia
antipsychotics should only be used for
patients at risk of harming themselves or
others, or when the agitation,
hallucinations or delusions are causing
them severe distress
Donepezil
Downloaded by Noman Ajmal (nomanbutt8895@gmail.com)
You might also like
- Descriptive Psychopathology (Synopsis of Symptoms of The Mind)No ratings yetDescriptive Psychopathology (Synopsis of Symptoms of The Mind)35 pages
- Geriatric Psychiatry Case Studies and InsightsNo ratings yetGeriatric Psychiatry Case Studies and Insights77 pages
- Laboratory Testing and Imaging Studies in Psychiatry100% (1)Laboratory Testing and Imaging Studies in Psychiatry54 pages
- Psychopharmacology for Medically Ill PatientsNo ratings yetPsychopharmacology for Medically Ill Patients21 pages
- SSRIs, TCAs, MAOIs, and Atypical Antipsychotics Overview100% (3)SSRIs, TCAs, MAOIs, and Atypical Antipsychotics Overview4 pages
- K P Differential Diagnosis Pyramid: OPMAPS: Sychiatry Evision100% (2)K P Differential Diagnosis Pyramid: OPMAPS: Sychiatry Evision36 pages
- Laboratory Tests and Imaging in Psychiatry100% (2)Laboratory Tests and Imaging in Psychiatry29 pages
- Clinical Interviewing. BMA 2017 Psychiatry Book of The Year0% (1)Clinical Interviewing. BMA 2017 Psychiatry Book of The Year2 pages
- Assessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MD100% (1)Assessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MD85 pages
- Psychiatric Work-Up Template For StudentsNo ratings yetPsychiatric Work-Up Template For Students2 pages
- ANCC PMHNP Board Exam Content Outline 2019No ratings yetANCC PMHNP Board Exam Content Outline 20193 pages
- 1.02 Psychiatric History and Mental Status Examination PDF100% (1)1.02 Psychiatric History and Mental Status Examination PDF4 pages
- Psychiatry Notes: Psychotic & Mood Disorders100% (1)Psychiatry Notes: Psychotic & Mood Disorders20 pages
- Gillman’s Antidepressant Treatment AlgorithmNo ratings yetGillman’s Antidepressant Treatment Algorithm50 pages
- Overview of Anxiety and Schizophrenia Disorders100% (2)Overview of Anxiety and Schizophrenia Disorders17 pages
- Interviewing and Assessment of The Psychiatric Patient: Interviewing TechniquesNo ratings yetInterviewing and Assessment of The Psychiatric Patient: Interviewing Techniques41 pages
- Psychiatric History and Mentafafafal Status Exam (Fixed)100% (1)Psychiatric History and Mentafafafal Status Exam (Fixed)7 pages
- Venlafaxine and Alcohol Interaction RisksNo ratings yetVenlafaxine and Alcohol Interaction Risks38 pages
- Barret 2008 Manic Defenses Against Loneliness in AdolescenceNo ratings yetBarret 2008 Manic Defenses Against Loneliness in Adolescence23 pages
- Sex Differences in Unipolar Depression: Evidence and Theory: Susan Nolen-HoeksemaNo ratings yetSex Differences in Unipolar Depression: Evidence and Theory: Susan Nolen-Hoeksema24 pages
- Medicine Card Questions 2025 - Srijan Sarker (DCIMC 9)No ratings yetMedicine Card Questions 2025 - Srijan Sarker (DCIMC 9)25 pages
- Model Exit Exam of Hawassa University-1No ratings yetModel Exit Exam of Hawassa University-136 pages
- Mood Disorder Epidemiology and TreatmentNo ratings yetMood Disorder Epidemiology and Treatment53 pages
- Understanding Mental Illness and Treatments79% (19)Understanding Mental Illness and Treatments5 pages
- K1661148609yoswaal CBSE 12th Psychology - Practice Paper-2No ratings yetK1661148609yoswaal CBSE 12th Psychology - Practice Paper-24 pages
- Bipolar Disorder and Sleep Issues ExplainedNo ratings yetBipolar Disorder and Sleep Issues Explained12 pages
- Attention Deficit Hyperactivity Disorder (ADHD) in Adults With Intellectual DisabilityNo ratings yetAttention Deficit Hyperactivity Disorder (ADHD) in Adults With Intellectual Disability45 pages