Professional Documents
Culture Documents
Mechanisms of Sleep Deprivation-Induced Hepatic Steatosis and Insulin Resistance in Mice
Uploaded by
Nazan ElmaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mechanisms of Sleep Deprivation-Induced Hepatic Steatosis and Insulin Resistance in Mice
Uploaded by
Nazan ElmaCopyright:
Available Formats
Am J Physiol Endocrinol Metab 315: E848–E858, 2018.
First published July 10, 2018; doi:10.1152/ajpendo.00072.2018.
RESEARCH ARTICLE Translational Physiology
Mechanisms of sleep deprivation-induced hepatic steatosis and insulin
resistance in mice
Fumika Shigiyama,1 X Naoki Kumashiro,1 Yousuke Tsuneoka,2 Hiroyuki Igarashi,1 Fukumi Yoshikawa,1
Saori Kakehi,3,4 Hiromasa Funato,2 and Takahisa Hirose1
1
Division of Diabetes, Metabolism, and Endocrinology, Department of Medicine, Toho University Graduate School of
Medicine, Tokyo, Japan; 2Department of Anatomy, Toho University Graduate School of Medicine, Tokyo, Japan;
3
Department of Metabolism and Endocrinology, Juntendo University Graduate School of Medicine, Tokyo, Japan; and
4
Sportology Center, Juntendo University Graduate School of Medicine, Tokyo, Japan
Submitted 22 February 2018; accepted in final form 28 June 2018
Shigiyama F, Kumashiro N, Tsuneoka Y, Igarashi H, resistance (3, 59). In a rodent model, it was reported that sleep
Yoshikawa F, Kakehi S, Funato H, Hirose T. Mechanisms of sleep disorders were associated with increased food intake (16, 48)
deprivation-induced hepatic steatosis and insulin resistance in mice. and reduced whole-body energy expenditure (43). However, in
Am J Physiol Endocrinol Metab 315: E848 –E858, 2018. First pub- the above studies, it was not clear whether glucose intolerance
lished July 10, 2018; doi:10.1152/ajpendo.00072.2018.—Sleep depri-
vation is associated with increased risk for type 2 diabetes mellitus.
was due to the changes in food intake or energy expenditure or
However, the underlying mechanisms of sleep deprivation-induced to the sleep deprivation itself. Thus, the exact underlying
glucose intolerance remain elusive. The aim of this study was to mechanisms remain undetermined.
investigate the mechanisms of sleep deprivation-induced glucose In the present study, we adopted the single 6-h sleep depri-
intolerance in mice with a special focus on the liver. We established vation technique by the gentle handling method (19, 47).
a mouse model of sleep deprivation-induced glucose intolerance using Especially in this study, to mimic the metabolic disorders seen
C57BL/6J male mice. A single 6-h sleep deprivation by the gentle in lifestyle disturbances in humans, mice were fed a high-fat
handling method under fasting condition induced glucose intolerance. diet and provided with sucrose water for 2 wk, and then we
Hepatic glucose production assessed by a pyruvate challenge test was compared the effects of sleep deprivation in fasting and move-
significantly increased, as was hepatic triglyceride content (by 67.9%) ment-restricted C57BL/6J mice and freely sleeping (accord-
in the sleep deprivation group, compared with freely sleeping control
mice. Metabolome and microarray analyses were used to evaluate
ingly noneating and nonmoving) mice. Thus, the model al-
hepatic metabolites and gene expression levels and to determine the lowed for the assessment of the effects of sleep deprivation on
molecular mechanisms of sleep deprivation-induced hepatic steatosis. glucose intolerance independent of hyperphagia and behavioral
Hepatic metabolites, such as acetyl coenzyme A, 3-hydroxybutyric patterns. In addition, we assessed the animals immediately
acid, and certain acylcarnitines, were significantly increased in the after a single 6-h sleep deprivation so as to avoid any effects of
sleep deprivation group, suggesting increased lipid oxidation in the deep sleep recovery. Our model is different from the mouse
liver. In contrast, fasted sleep-deprived mice showed that hepatic gene model of genetic mutation or ablation of molecular clock genes
expression levels of elongation of very long chain fatty acids-like 3, and thus allowed us to assess the physiological effects of sleep
lipin 1, perilipin 4, perilipin 5, and acyl-CoA thioesterase 1, which are deprivation. Considering that metabolic disorders occur with
known to play lipogenic roles, were 2.7, 4.5, 3.7, 2.9, and 2.8 times, lifestyle disturbances, it is important to assess the effect of
respectively, those of the fasted sleeping control group, as assessed by
quantitative RT-PCR. Sleep deprivation-induced hepatic steatosis and
sleep deprivation without genetic modification.
hepatic insulin resistance seem to be mediated through upregulation of The pathogenesis of type 2 diabetes mellitus is associated
hepatic lipogenic enzymes. with hepatic and peripheral muscle insulin resistance caused by
ectopic lipid accumulation in the liver and skeletal muscle (50,
hepatic insulin resistance; hepatic steatosis; sleep deprivation 56). In mammals, it is also reported that the liver encompasses
a biological circadian clock system (11, 19). In this regard, the
liver plays an important physiological role in energy metabo-
INTRODUCTION lism, the diurnal processing of nutrients (57, 60). Thus, it
seems important to investigate the underlying mechanisms of
Sleep is one of the most important lifestyle components. The sleep deprivation-induced glucose intolerance with special fo-
quality and quantity of sleep correlate with physical and mental cus on the liver. In the present study, hepatic metabolome and
health and homeostasis (43). Sleep disorders are also closely microarray analyses were performed to identify the molecular
associated with serious complications, such as hypertension mechanisms of sleep deprivation-induced hepatic insulin resis-
and type 2 diabetes mellitus (25). In this regard, several clinical tance and hepatic steatosis.
and experimental studies have demonstrated the association
between sleep disorders and glucose intolerance or insulin MATERIALS AND METHODS
Animals. Male C57BL/6J mice (CLEA Japan Inc., Tokyo, Japan)
Address for reprint requests and other correspondence: N. Kumashiro, aged 13 wk were used in all experiments. They were individually
6-11-1 Omori-Nishi, Ota-ku, Tokyo, Japan 143-8541 (e-mail: naoki. housed in plastic cages under a 12-h light/12-h dark cycle (lights on
kumashiro@med.toho-u.ac.jp). at 0800) at controlled ambient temperature (24 ⫾ 1°C) and were
E848 0193-1849/18 Copyright © 2018 the American Physiological Society http://www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER E849
provided with food and water ad libitum. During the 14-day habitu- overnight. After an overnight, they slept in the small plastic cage
ation period, mice received a high-fat diet (D12451, Research Diets, while fasting for 6 h, and then ipGTT or tissue sampling was
Inc., New Brunswick, NJ) and 5% sucrose water. All procedures performed.
described in this study were approved by the Institutional Animal Tissue sampling. Tissues were immediately dissected out at the end
Care and Use Committee of Toho University School of Medicine. of the sleep deprivation period, wrapped in aluminum foil, flash-
Sleep deprivation and fasting protocol. Mice were visually moni- frozen in liquid nitrogen, and preserved in a ⫺80°C refrigerator.
tored continuously for signs of sleep for 6 h from 0800 to 1400 on the Laboratory tests. Blood glucose concentrations were measured by
day of the experiment. To avoid any stress, handling or touching of a portable glucose meter using Accu-Chek Aviva Nano (Roche, Basel,
mice was minimized. For mice of the sleep deprivation group, they Switzerland). Plasma insulin was measured using an ELISA kit
were physically handled or gently touched once they started to close (Morinaga, Kanagawa, Japan). Glucagon concentration was measured
their eyes and recline. On the other hand, mice of the control group by a radioimmunoassay kit (Euro-Diagnostica AB, Malmö, Sweden).
were allowed to sleep undisrupted. Unless otherwise stated, the Corticosterone and adrenocorticotropic hormone (ACTH) were mea-
procedure of sleep deprivation was applied only once per animal in sured by electrochemiluminescence immunoassay kit (Roche Diag-
this study. Mice of both groups were fasted during the 6-h sleep nostic K.K., Tokyo, Japan).
deprivation period and also maintained in small individual plastic ipGTT and pyruvate challenge test. At the end of the sleep
cages (Natsume Seisakusho Co., Tokyo, Japan) to limit their physical deprivation and fasted period for 6 h, 20% glucose (2.0 g/kg body wt)
activity during the sleep deprivation period. Tissue and blood sam- or pyruvate (1.5 g/kg body wt) was injected intraperitoneally for
pling, intraperitoneal glucose tolerance test (ipGTT), and pyruvate ipGTT or for the pyruvate challenge test, respectively, as described
challenge test were performed immediately after the 6-h sleep depri- previously (26, 28, 61). Blood samples were collected from the tail
vation period. For the chronic assessment, 6 h of sleep deprivation vein at the indicated time on the figures, and plasma glucose and
was conducted daily over 5 consecutive days under the same labora- insulin levels were measured with the portable glucose meter and
tory conditions, and then ipGTT was performed at the end of the 5-day ELISA kit, respectively, as described above.
sleep deprivation period. For the recovery sleep assessment, after a Hepatic triglyceride assay. Hepatic triglyceride content was deter-
single 6-h sleep deprivation period, the mice of the recovery group mined by using the triglyceride assay kit (Triglyceride E-test WAKO,
were released into the usual plastic cage and stayed ad libitum Tokyo, Japan) and a method adapted as described previously (26, 27,
Fig. 1. A and B: intraperitoneal glucose tolerance test (ipGTT).
The 6-h sleep deprivation was induced by the gentle handling
method. A: plasma glucose level at 60 min was significantly
higher in mice of the sleep deprivation group (n ⫽ 8) than the
control group (n ⫽ 8). B: area under the curve (AUC) of
glucose calculated for individual mice and averaged for the two
groups. The AUC of glucose was significantly higher in the
sleep deprivation group. C and D: ipGTT of the chronic model
with 6 h of sleep deprivation for 5 days. C: six-hours of sleep
deprivation was induced by the gentle handling method and
repeated for 5 days. Plasma glucose concentrations at 0 and 60
min were significantly lower in the sleep deprivation group
(n ⫽ 8) than the control group (n ⫽ 8). D: AUC of plasma
glucose concentration during ipGTT was comparable between
the two groups (n ⫽ 8 per group). E and F: ipGTT after 24-h
recovery period, including sleep recovery. E: ipGTT was per-
formed after 24-h recovery period, including sleep recovery
after 6 h of sleep deprivation. In detail, mice of the recovery
group were released into the plastic cage and stayed ad libitum
overnight. Then, they were fasted in the small plastic cage and
slept freely for 6 h, and then ipGTT was performed. Fasting
plasma glucose was significantly higher in the recovery group
than the sleep deprivation group (n ⫽ 8 per group). F: recovery
group had a smaller increase in plasma glucose compared with
the sleep deprivation group, specifically significant at 120 min
(n ⫽ 8 per group). Data are means ⫾ SD. Differences among
groups were assessed by two-way ANOVA followed by the
Tukey post hoc (in A, C, E, and F) or by the unpaired t-test (in
B and D). *P ⬍ 0.05.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
E850 HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER
gene ontology analyses were performed by the KURABO Bio-Med-
A 150
ical Department using the Affymetrix GeneChip Mouse Gene 2.0 ST
Array (Affymetrix, Inc., Santa Clara, CA). Genes with a more than
Δblood glucose (mg/dL) * twofold change in their expression levels (sleep deprivation vs.
100 * control) (P ⬍ 0.05) were selected as differentially expressed genes. P
values and fold changes between the two groups were calculated using
the Moderated t-test. A heat map with hierarchical clustering was
50 constructed for the genes that showed different expression levels in
the sleep deprivation and control groups. Gene expression data of each
sample were analyzed using hierarchical clustering, and each color in
0 the heat map indicates gene expression intensity (Log2). In this
0 30 60 analysis, red color reflects much higher than the average standardized
expression level, whereas blue color represents lower than average
expression. Hierarchical clustering analysis was performed using
-50 Time (min) GeneSpring version 14 software (Agilent Technologies, Santa Clara,
B 5000 *
AUC Δblood glucose
4000
3000
2000
1000
0
Control Sleep deprivation
Fig. 2. Pyruvate challenge test. Blood glucose concentrations were measured
following intraperitoneal pyruvate injection (1.5 g/kg) after 6 h of fasting (n ⫽
8 per group). A: Delta (⌬, change in) blood glucose, as an index of extent of
gluconeogenesis. B: area under the curve (AUC) of delta glucose was calcu-
lated for the individual mouse and averaged for each group. Data are
means ⫾ SD. Differences among groups were assessed by two-way ANOVA
followed by the Tukey post hoc test. *P ⬍ 0.05.
29). Briefly, around 100 mg of liver tissues were used to extract liver
triglycerides. Tissues were homogenized in 2:1 chloroform/methanol
on cold ice, and lipids were extracted by shaking for 3– 4 h at room
temperature. After the addition of sulfuric acid to 100 mM, the
samples were vortexed and centrifuged to separate the solution phase.
The organic phase was collected and used for analysis of triglyceride
content.
Oil red O staining. Mice were deeply anesthetized with sodium
pentobarbital (15 mg/kg ip) and then perfused transcardially with 4%
paraformaldehyde in 0.01 M phosphate᎑buffered saline (PBS) (pH
7.4). The livers were removed immediately and postfixed in 4%
paraformaldehyde/PBS at 4°C overnight, followed by cryoprotection
in 30% (wt/vol) sucrose in PBS. The tissue blocks were embedded in
Surgipath (FSC22, Leica Biosystems, Wetzlar, Germany), and then
stored at ⫺80°C until cryosectioning. Livers were cryosectioned into
10-m thick sections and mounted on MAS-coated slides. The sec-
tions were stained with 0.3% Oil red O solution, counterstained with
hematoxylin, and coverslipped with aqueous mountant.
Measurement of liver metabolites. Metabolome analysis was con-
ducted by the Dual Scan package of Human Metabolome Technolo-
gies Inc. (Tsuruoka, Japan) using capillary electrophoresis time-of-
flight mass spectrometry and liquid chromatography time-of-flight
mass spectrometry, based on the methods described in detail previ-
ously (37, 40). The migration time, retention time, and mass-to-charge
ratio were compared with authentic standards to identify the metab-
olites in the liver tissue samples. In addition to the quantification of Fig. 3. Plasma corticosterone, glucagon, and adrenocorticotropic hormone
the metabolites, their peak areas were compared with those of authen- (ACTH) levels after 6 h of sleep deprivation. Plasma corticosterone (A),
tic standards. glucagon (B), and ACTH (C) were measured in both groups (n ⫽ 8 per group).
Gene expression microarray and data analysis. To determine the Data are means ⫾ SD. Differences among groups were assessed by the
genetic and signaling pathways involved in the liver, microarray and unpaired t-test. *P ⬍ 0.05.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER E851
*
We further examined the effects of 6 h of sleep deprivation
2 = Control group conducted daily over 5 consecutive days under the same
laboratory conditions. ipGTT was performed at the end of the
= Sleep deprivation group 5-day sleep deprivation period. The results of the latter tests
Relative mRNA expression
showed significantly lower plasma glucose concentrations at
times 0 and 60 min of ipGTT in the sleep deprivation group
(Fig. 1C). However, in these tests, the area under the curve of
plasma glucose concentration was comparable between the two
1 groups (Fig. 1D). We also evaluated the effect of sleep recov-
ery on glucose tolerance and found that a 24-h recovery period,
including sleep recovery, improved the impaired glucose tol-
erance (Fig. 1, E and F).
Next, we investigated the mechanisms of sleep deprivation-
induced glucose intolerance with a special focus on the liver.
To assess hepatic gluconeogenic capacity that reflects hepatic
0 insulin sensitivity, the pyruvate challenge test was performed.
G6Pase FBP1 PC PEPCK1 Sleep deprivation was associated with significant increase in
Fig. 4. Comparison of mRNA expression levels of four hepatic gluconeogen- glucose level after pyruvate loading compared with the control
esis-related genes between the control and sleep deprivation groups (n ⫽ 7 per group (Fig. 2, A and B). This result was supported by the
group). The average mRNA expression level of the control group was set as 1. finding of significantly higher plasma concentrations of corti-
Data are means ⫾ SD. Differences among groups were assessed by the
unpaired t-test. *P ⬍ 0.05. FBP1, fructose-1,6-bisphosphatase; G6Pase, glu-
costerone and glucagon, which increase hepatic glucose pro-
cose-6-phosphatase; PC, pyruvate carboxylase; PEPCK1, phosphoenolpyru- duction, in the sleep deprivation group compared with the
vate carboxykinase 1. control group (Fig. 3, A and B). We also assessed plasma
ACTH, which is usually released from the pituitary gland and
stimulates corticosterone production from the adrenal glands.
CA). The gene expression values on the heat map were normalized by
the RMA-Sketch method. A complete set of microarray data was Plasma ACTH level tended to be higher in the sleep depriva-
deposited into the Gene Expression Omnibus repository (https:// tion group than the control group (Fig. 3C), albeit insignifi-
www.ncbi.nlm.nih.gov/geo/) under accession number GSE92913. cantly. Furthermore, hepatic mRNA expression level of glu-
Gene ontology analysis was performed using Fisher’s exact test. cose 6-phosphatase, which is one of the gluconeogenic en-
Real-time polymerase chain reaction. Total RNA was extracted zymes, was significantly higher in the sleep deprivation group
from flash-frozen ~15 mg liver tissue using the RNeasy mini kit than the control group (Fig. 4).
(Qiagen, Tokyo, Japan). RNA was reverse-transcribed into cDNA Sleep deprivation induces hepatic steatosis accompanied by
using the QuantiTect Reverse Transcription kit (Qiagen, Hilden, increased hepatic lipid oxidation and lipogenesis. Since he-
Germany). The abundance of transcripts was assessed by real-time patic insulin resistance is associated with hepatic steatosis (27,
polymerase chain reaction (PCR) on an Applied Biosystems 7500 Fast
62), we assessed hepatic triglyceride content. Interestingly, a
Real-Time PCR System (Thermo Fisher Diagnostics, Tokyo, Japan)
with a Fast SYBR Green Master Mix (Thermo Fisher Diagnostics). single 6-h sleep deprivation increased hepatic triglyceride con-
The expression level of each gene of interest was normalized for the tent by 67.9% compared with the control group (Fig. 5, P ⬍
efficiency of amplification with TATA box binding protein mRNA as 0.05). To confirm the increase in hepatic triglyceride level, a
the invariant control, as determined by a standard curve. histological examination of liver tissue was conducted using
Statistical analysis. All data are expressed as means ⫾ SD unless Oil red O staining. Consistent with the above results of bio-
otherwise indicated. Differences among groups were assessed by chemical analysis, larger numbers and areas of lipid droplets
two-way ANOVA followed by the Tukey post hoc test (for ipGTT were observed in the sleep deprivation group than the control
and pyruvate challenge test), and by the unpaired t-test for other
parameters. P values ⬍0.05 were defined as statistically significant.
Statistical analyses were performed with PRISM.7 software (Graph-
Pad Software, La Jolla, CA). 40
*
Hepatic triglyceride content
RESULTS
30
Single 6-h sleep deprivation episode induces glucose intol-
(mg / g-liver)
erance and hepatic insulin resistance. To evaluate the effect of
sleep deprivation on glucose metabolism, each mouse under- 20
went ipGTT after the sleep deprivation period. Figure 1A
shows a significant increase in plasma glucose level in the
sleep deprivation group after only one session of 6 h of sleep 10
deprivation. The area under the curve of glucose in ipGTT was
significantly higher in the sleep deprivation group (Fig. 1B),
despite the lack of increase in body weight (26.3 ⫾ 2.4 vs. 0
25.9 ⫾ 2.5 g, control vs. sleep deprivation, respectively). There Control Sleep deprivation
was no difference in plasma insulin level at 60 min of ipGTT Fig. 5. Hepatic triglyceride content in the control and sleep deprivation groups
between the two groups (0.29 ⫾ 0.3 vs. 0.54 ⫾ 0.4 U/ml, (n ⫽ 7 per group). Data are means ⫾ SD. Differences among groups were
control vs. sleep deprivation group, respectively, P ⫽ 0.18). assessed by the unpaired t-test. *P ⬍ 0.05.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
E852 HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER
group (Fig. 6). We also evaluated the effect of sleep recovery firmed overexpression of hepatic genes known to be involved
on hepatic lipid accumulation and found that only a 24-h in promoting lipogenesis, such as elongation of very long chain
recovery period, including sleep recovery, improved hepatic fatty acids-like 3 (Elovl3), lipin 1 (Lpin1), perilipin 4 (Plin4),
lipid accumulation (14.4 ⫾ 7.6 vs. 29.2 ⫾ 9.0 mg/g liver for perilipin 5 (Plin5), and acyl-CoA thioesterase 1 (Acot1) (Fig.
recovery group vs. sleep deprivation group, respectively). 9A). On the other hand, the same method showed downregu-
To determine the underlying mechanism of hepatic steatosis, lation of the genes known to be involved in the sterol regula-
metabolome analysis was performed using frozen liver tissues. tory element-binding protein-1c (SREBP1c), another lipogenic
Interestingly, 3-hydroxybutyric acid, acetyl coenzyme A enzyme. With regard to the genes that promote lipid oxidation,
(CoA), and acylcarnitines were significantly increased in mice ATP-binding cassette subfamily D member 2 (ABCD2) was
of the sleep deprivation group compared with those of the significantly lower, whereas acetyl-CoA carboxylase 2 was
control group (Fig. 7, A–C). We also assessed hepatic mRNA higher in the sleep deprivation group compared with the
expression levels using microarray analysis and RT-PCR. A control group (Fig. 9B).
total of 34,474 genes were screened by microarray analysis
using liver samples. Of the entire group, the expression levels DISCUSSION
of 58 genes were significantly different between the sleep
deprivation group and control group (Fig. 8). Next, we per- In this study, 6 h of sleep deprivation was associated with
formed gene ontology analysis to estimate multiplicity between the development of glucose intolerance and increased hepatic
gene ontology functional classes of the gene sets and genes that glucose production, suggestive of hepatic insulin resistance.
were differentially expressed genes on microarray analysis. Interestingly, this was also accompanied by hepatic steatosis
The results showed that genes involved in the lipid metabolic without weight gain. Comprehensive analysis using metabo-
process, steroid metabolic process, and regulation of fatty acid lome suggested that sleep deprivation-induced hepatic steatosis
metabolic process were significantly different between the two was mediated by increased lipid oxidation in the liver. In
groups (Table 1). Furthermore, quantitative RT-PCR con- contrast, the expression levels of certain hepatic lipogenic
A B
C D
Fig. 6. Oil red O staining of liver sections.
A–C: control group. D–F: sleep deprivation
group. n ⫽ 3 per group; scale bar ⫽ 100 m.
E F
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER E853
A 0.03 C
3-Hydroxybutyric acid
(Relative area)
0.02
0.01
Number of Carbon
Fig. 7. Results of metabolome analysis. A:
3-hydroxybutyric acid. B: acetyl CoA. C:
0.00 acylcarnitines. The levels of 3-hydroxybu-
tyric acid, acetyl-CoA, and some acylcar-
Control Sleep deprivation nitines were significantly higher in the sleep
deprivation group compared with control
B 0.0006 group (n ⫽ 7 per group). Data are
means ⫾ SD of the relative area calculated
as described in M ETHODS . Differences
among groups were assessed by the unpaired
t-test. *P ⬍ 0.05.
(Relative area)
Acetyl CoA
0.0004
0.0002
= Control group
= Sleep deprivation group
0.0000
Control Sleep deprivation Number of Double bond
genes were significantly increased in the fasted sleep-deprived due to severe physical stress caused by continuous sleep
mice compared with the control sleeping mice, as assessed by deprivation, and it may explain the significant decrease in
microarray and quantitative RT-PCR. Taken together, our data plasma glucose concentration. Based on these observations, we
suggest that the mechanisms of sleep deprivation-induced he- did not perform experiments with chronic sleep deprivation for
patic steatosis and insulin resistance include, at least in part, more than 5 days. Furthermore, in this study, to mimic the
overexpression of certain lipogenic genes, such as Elovl3. metabolic disorders in humans associated with lifestyle distur-
Several rodent sleep deprivation models have already been bances, we provided mice with a high-fat diet and sucrose
described (5, 14, 16 –19, 34, 38, 43, 47, 48, 53, 66). With water for 2 wk during the habituation period.
regard to the model selection, we considered it was important In our model, the 6 h of sleep deprivation significantly
to assess the effect of sleep deprivation without genetic mod- increased hepatic triglyceride content and induced hepatic
ification, considering that metabolic disorders occur with life- insulin resistance. Hepatic gluconeogenesis in vivo was
style disturbances. Ferrell and Chiang (19) favored gentle significantly increased in the sleep deprived mice, as as-
stimulation with physical contact as a technique of circadian sessed by the pyruvate challenge test and, consistently,
system disturbance or sleep disruption rather than genetic increased glucose 6-phosphatase gene expression, as con-
mutation or ablation of molecular clock genes in mice. In the firmed by RT-PCR. In this regard, previous studies reported
present study, we also simultaneously fasted mice of both the that sleep restriction or fragmentation leads to insulin resis-
sleep deprivation and control groups and restricted their phys- tance in rodents (4, 14, 66) and humans (13, 15, 22, 35, 46,
ical activity at comparable levels to assess the direct effects of 58). In addition, Hsieh et al. (24) reported the association of
sleep deprivation on glucose intolerance independent of hy- short sleep duration with fatty liver in human. It has also
perphagia and behavioral pattern. Then, body weight was not been demonstrated that several genetic variants of the clock
increased, but glucose intolerance was induced by the applied genes correlate with hepatic steatosis (32). In general, he-
technique of sleep deprivation. Our model is also different patic steatosis is considered to induce hepatic insulin resistance
from the chronic sleep deprivation model (3) and has been used (27, 62). Thus, sleep deprivation seems to induce hepatic
to evaluate the direct and immediate effects of sleep depriva- steatosis, and this, in turn, increases hepatic glucose produc-
tion on metabolism in vivo, avoiding the effects of sleep tion, reflecting hepatic insulin resistance, at least in part, finally
recovery (2, 14) and chronic compensatory metabolic changes leading to glucose intolerance.
(4). In this study, we also tested the chronic model, but body To determine the underlying molecular mechanisms, we
weight tended to decrease in the sleep deprivation group performed metabolome and microarray analyses. Hepatic
compared with the control group (27.7 vs. 30.2 g, sleep metabolome analysis showed significantly higher levels of
deprivation vs. control, n ⫽ 8 vs. 8, P ⫽ 0.054, respectively). acetyl-CoA, 3-hydroxybutyric acid, and acylcarnitine in the
Such body weight reduction in the sleep deprived mice may be sleep deprived mice. Acetyl-CoA is known to catalyze the
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
E854 HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER
01.SD
02.SD
03.SD
05.SD
06.SD
10.SD
13.SD
04.CT
07.CT
08.CT
09.CT
11.CT
12.CT
14.CT
Lpin1
Elovl3
Mfsd2a
St3gal5
Gm19958 Edv Gm3579
Gm19958 Edv Gm3579
Gm19958 Edv Gm3579
Gm19958 Edv Gm3579
E330011021Rik
Erbb4
Lgr5
Dsg1c
Abcd2
Pparg
Sult1c2
1700040L02Rik
Cxcl1
Clec2h
Bcl6
Sc4mol
Per3
Fig. 8. Differentially expressed genes in the Gsap
Car1
control and sleep deprivation groups (n ⫽ 7 Fzd8
per group), assessed by microarray analysis. Sort1
Cdkn1a
Gene expression data of each sample were Ddit4
analyzed using hierarchical clustering. Each Gm15889
Tmc7
color in the heat map indicates the gene Gm19958 Edv Gm3579
expression intensity (Log2). The colors are Gm19958 Edv Gm3579
derived from color range (1). Each fold- Scara5
E030018B12Rik
change score (Log2) between the control Mir344d-2 mmu-mir-344d-2
group and sleep deprivation group is also Fam107a
Cyp2b10
colored. The colors are located on the right Plin4
side of the heat map. The colors were derived Fgf21 LOC100862558
Cidec
from color range (2). Arntl
Srebf1
Apol7a
Ugt2b35
Acot1
Lyve1
Slc45a3
Tbc1d8
Lipg
Fam35a
Slc35g1
LOC100862287 Fkbp5
Ppp1r3c
Cyp39a1
Cyp17a1
Insig2
Plin5
Igfbp1
Ankhd1 Eif4ebp3
Color range(1) Color range(2)
Gene Expression Intensity (Log2) Fold Change (Log2)
CT=Control group
SD=Sleep deprivation group
gluconeogenic function of pyruvate carboxylase (44, 50). In to increased hepatic glucose production. With regard to the
our model, pyruvate carboxylase was not increased at the gene increased levels of hepatic 3-hydroxybutyric acid, a ketone
expression level, but its gluconeogenic function was likely body, Chikahisa et al. (10) also reported that 6 h of sleep
increased by the increased hepatic acetyl-CoA content, leading deprivation in mice increased plasma ketone body levels. They
Table 1. Distribution of gene ontology biological process groups for genes that showed significant difference in their
expression levels
Count in Selection Count in Total
Accession GO Term (Numerator) (Denominator) P Value
GO:0006629 lipid metabolic process 13 1032 0.0050
GO:0015074 DNA integration 3 8 0.0050
GO:0004523/GO:0004524 RNA-DNA hybrid ribonuclease activity 3 9 0.0050
GO:0007169 transmembrane receptor protein, tyrosine kinase signaling pathway 7 295 0.0203
GO:0032868 response to insulin 6 196 0.0203
GO:0008202 steroid metabolic process 6 229 0.0351
GO:0019217/GO:0006632 regulation of fatty acid metabolic process 4 64 0.0351
Data are results of gene ontology (GO) analysis for genes of the sleep deprivation group/control group. GO Term criteria is P value of the Fisher exact test
of ⬍0.05.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER E855
= Control group regulate numerous hepatic genes (41), including SREBP1c,
* *
A = Sleep deprivation group fatty acid synthase, and acetyl-CoA carboxylase 1 (7, 41), but
these do not seem to be involved in sleep deprivation-induced
*
Relative mRNA expression
5
hepatic steatosis based on the results of the present study.
* *
Although it is reported that SREBP1c activity is modulated by
4
nutrients and circadian rhythm (21, 31), the mechanisms of
decreased SREBP1c expression by sleep deprivation need to be
3
*
further investigated. In contrast, Elovl3, whose expression was
2
significantly altered by sleep deprivation, is considered to be
strongly linked to circadian rhythm (1). Other studies also
1
reported that hepatic Elovl3 mRNA expression exhibited a
diurnal rhythm and was induced by exposure to glucocorticoids
0 (8). The results also described a potential functional crosstalk
SRBP1c Elovl3 Lpin1 Plin4 Plin5 Acot1 FAS between Elovl3 and ABCD2 (8). Interestingly, significantly
higher plasma corticosterone concentrations and significantly
B higher expression levels of Elovl3 and lower expression levels
*
Relative mRNA expression
3
of ABCD2 hepatic mRNA were noted in the sleep deprived
mice in the present study compared with the control. These
results suggest that sleep deprivation seems to increase plasma
2
* glucocorticoid concentration, leading to upregulation of Elovl3
and downregulation of ABCD2. To date, some animal and
human studies have reported a direct stimulatory effect of sleep
1 loss on the hypothalamic pituitary adrenal axis (23, 33, 36, 54).
In addition, Patel et al. (42) suggested previously that elevated
glucocorticoid levels modulate hepatic gene expressions in-
0 volved in lipolysis and lipogenesis and contribute to hepatic
ABCD2 PPARα ACC1 ACC2 ACO steatosis. Thus, the high corticosterone levels could be respon-
Fig. 9. Comparison of hepatic mRNA expression levels of genes involved in sible, at least in part, for the sleep deprivation-induced lipid
lipogenesis and lipid oxidation between the control and sleep deprivation accumulation in the liver. We are currently engaged in research
groups (n ⫽ 7 per group). A: lipogenesis-related genes. B: lipid oxidation-
related genes. The average of the control group was set as 1. Data are
on loss of function using metyrapone to suppress glucocorti-
means ⫾ SD. Differences among groups were assessed by the unpaired t-test. coid production in our sleep deprivation model. This research
*P ⬍ 0.05. ABCD2, ATP-binding cassette subfamily D member 2; ACC1/2, is designed to address the question of whether lipid accumu-
acetyl-CoA carboxylase 1/2; ACO, acyl-CoA oxidase; Acot1, acyl-CoA thio- lation is abolished when sleep deprivation is uncoupled with
esterase 1; Elovl3, elongation of very long chain fatty acids-like 3; FAS, fatty stress-induced glucocorticoid levels.
acid synthase; Lpin1, lipin 1; Plin4/5, perilipin 4/5; PPAR␣, peroxisome
proliferator-activated receptor ␣; SREBP1c, sterol regulatory element-binding In addition to Elovl3, our results detected upregulation of
protein-1c. Lpin1, Plin4, Plin5, and Acot1, suggesting their potential
involvement in the sleep deprivation-induced hepatic steatosis
suggested that ketone body was associated with sleep/wake (20, 30, 39). Sengupta et al. (53) also reported that sleep
regulation in the brain. However, the effects of changes in restriction induced lipogenesis metabolic switches in the rat
hepatic ketone bodies on brain sleep homeostasis or vice versa liver. Of note, because our sleep deprived mice were fasted,
are not well established. Some studies reported the association any decrease in the expression of lipogenic genes and increase
of sleep curtailment with increased acylcarnitine levels in in the expression of lipid oxidation-related genes could be
humans (6, 12, 63, 65). Increased acylcarnitine level is caused by fasting, but the increased expression levels of
considered to be a sign of mitochondrial dysfunction and a lipogenic genes, such as Elovl3, Lpin1, Plin4, Plin5, and
marker of altered metabolic processes (63). Altered mito- Acot1, or decreased expression levels of lipid oxidation-related
chondrial parameters are thought to be linked to insulin genes, such as ABCD2, could be caused by sleep deprivation.
resistance (45, 63). Our group has also reported that mito- Combining the metabolome and microarray data, there
chondrial dysfunction is associated with hepatic insulin seems to be an increase in lipid oxidation and lipogenesis in
resistance in nonalcoholic fatty liver disease in humans (55). our acute sleep deprivation model. In this regard, a previous
In addition, increased acylcarnitine levels may play a causal review suggested that patients with fatty liver exhibit both
role in the development of insulin resistance through their increased triglyceride synthesis and increased -oxidation
proinflammatory effects (49). (51). In addition, Bugianesi et al. (9) reported that hepatic lipid
Using microarray data, the results of gene ontology analysis content, as assessed in liver biopsies, correlated significantly
suggested that sleep deprivation significantly affects the met- with lipid oxidation in patients with nonalcoholic fatty liver
abolic processes of lipid metabolism, steroids, and regulation disease. Thus, lipid accumulation in the liver seems to be
of fatty acid. We also used quantitative RT-PCR to examine associated with increased hepatic lipid oxidation. Steatosis
the upregulated genes involved in lipid metabolism. Interest- could result from increased delivery of circulating fatty acids to
ingly, sleep deprivation was associated with significant de- the liver (64); part of the excess fatty acids would be oxidized,
crease in the well-known SREBP1c, a master regulator of and the remainder could be esterified to triglyceride in the
lipogenesis. In this regard, circadian rhythm is known to liver.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
E856 HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER
The present study has several limitations. First, hepatic and, as such, has full access to all study data and takes responsibility for the
steatosis was evaluated in this study by increased hepatic integrity of the data and accuracy of data analysis.
triglycerides content. Because sometimes hepatic triglycerides
become inert storage and hepatic insulin-sensitive fatty liver REFERENCES
exists in humans (55), future studies should assess other lipid 1. Anzulovich A, Mir A, Brewer M, Ferreyra G, Vinson C, Baler R.
species, such as diacylglycerol and ceramide, which have been Elovl3: a model gene to dissect homeostatic links between the circadian
implicated in mediating insulin resistance (27, 52). Second, no clock and nutritional status. J Lipid Res 47: 2690 –2700, 2006. doi:10.
causality can be ascertained due to the lack of gain or loss of 1194/jlr.M600230-JLR200.
function analysis. Therefore, intervention studies designed to 2. Arthaud S, Varin C, Gay N, Libourel PA, Chauveau F, Fort P, Luppi
PH, Peyron C. Paradoxical (REM) sleep deprivation in mice using the
prevent sleep deprivation-induced hepatic steatosis and insulin small-platforms-over-water method: polysomnographic analyses and mel-
resistance should be performed in the future. Third, our pro- anin-concentrating hormone and hypocretin/orexin neuronal activation
tocol of sleep deprivation included sleep deprivation and pos- before, during and after deprivation. J Sleep Res 24: 309 –319, 2015.
sibly stress. Finally, the asleep/awake status was monitored doi:10.1111/jsr.12269.
3. Barf RP, Meerlo P, Scheurink AJ. Chronic sleep disturbance impairs
visually. Similar studies are needed in which the sleep/wake
glucose homeostasis in rats. Int J Endocrinol 2010: 819414, 2010. doi:
cycle is monitored by electroencephalography, electrooculog- 10.1155/2010/819414.
raphy, and electromyography. 4. Baud MO, Magistretti PJ, Petit JM. Sustained sleep fragmentation
In conclusion, the molecular mechanisms of hepatic steato- affects brain temperature, food intake and glucose tolerance in mice. J
sis and hepatic insulin resistance induced by sleep deprivation Sleep Res 22: 3–12, 2013. doi:10.1111/j.1365-2869.2012.01029.x.
5. Baud MO, Magistretti PJ, Petit JM. Sustained sleep fragmentation
were investigated comprehensively using metabolome and mi- induces sleep homeostasis in mice. Sleep 38: 567–579, 2015. doi:10.5665/
croarray analyses in our mouse model. A single session of 6 h sleep.4572.
of sleep deprivation was associated with the development of 6. Bell LN, Kilkus JM, Booth JN III, Bromley LE, Imperial JG, Penev
hepatic steatosis and hepatic insulin resistance under fasting PD. Effects of sleep restriction on the human plasma metabolome. Physiol
condition without weight gain. Sleep deprivation-induced he- Behav 122: 25–31, 2013. doi:10.1016/j.physbeh.2013.08.007.
7. Brewer M, Lange D, Baler R, Anzulovich A. SREBP-1 as a transcrip-
patic steatosis and hepatic insulin resistance are probably tional integrator of circadian and nutritional cues in the liver. J Biol
mediated through upregulation of hepatic lipogenic enzymes. Rhythms 20: 195–205, 2005. doi:10.1177/0748730405275952.
8. Brolinson A, Fourcade S, Jakobsson A, Pujol A, Jacobsson A. Steroid
ACKNOWLEDGMENTS hormones control circadian Elovl3 expression in mouse liver. Endocrinol-
ogy 149: 3158 –3166, 2008. doi:10.1210/en.2007-1402.
We thank Azusa Fujimura, Sachiko Mizuno, Hikari Taka, and Naoko Kaga
9. Bugianesi E, Gastaldelli A, Vanni E, Gambino R, Cassader M, Baldi
for the excellent technical assistance.
S, Ponti V, Pagano G, Ferrannini E, Rizzetto M. Insulin resistance in
non-diabetic patients with non-alcoholic fatty liver disease: sites and
GRANTS mechanisms. Diabetologia 48: 634 –642, 2005. doi:10.1007/s00125-005-
This research was supported by the Japan Society for the Promotion of 1682-x.
Science KAKENHI (Grant nos. 25893260, 26702032, and JP17H02180) and 10. Chikahisa S, Shimizu N, Shiuchi T, Séi H. Ketone body metabolism and
by a research grant from Kanae Foundation for the Promotion of Medical sleep homeostasis in mice. Neuropharmacology 79: 399 –404, 2014.
Science. doi:10.1016/j.neuropharm.2013.12.009.
11. Damiola F, Le Minh N, Preitner N, Kornmann B, Fleury-Olela F,
DISCLAIMERS Schibler U. Restricted feeding uncouples circadian oscillators in periph-
eral tissues from the central pacemaker in the suprachiasmatic nucleus.
The funding agencies and corporations had no role in study design, data Genes Dev 14: 2950 –2961, 2000. doi:10.1101/gad.183500.
collection and analysis, decision to publish, or writing of the manuscript. 12. Davies SK, Ang JE, Revell VL, Holmes B, Mann A, Robertson FP,
Cui N, Middleton B, Ackermann K, Kayser M, Thumser AE,
DISCLOSURES Raynaud FI, Skene DJ. Effect of sleep deprivation on the human
metabolome. Proc Natl Acad Sci USA 111: 10761–10766, 2014. doi:10.
T. Hirose received research funds from AstraZeneca; Boehringer Ingelheim 1073/pnas.1402663111.
Pharmaceuticals, Inc.; Astellas Pharma Inc.; Ono Pharmaceutical Co., Ltd.;
13. De Bernardi Rodrigues AM, da Silva CC, Vasques AC, Camilo DF,
Novo Nordisk Inc; Sanofi-Aventis Deutschland GmbH; Daiichi-Sankyo Co.,
Barreiro F, Cassani RS, Zambon MP, Antonio MA, Geloneze B;
Ltd.; Eli Lilly Japan K.K.; Takeda Pharmaceutical Company Limited; Mit-
Brazilian Metabolic Syndrome Study (BRAMS) Investigators. Asso-
subishi Tanabe Pharma Corporation; Dainippon Sumitomo Pharma Co., Ltd.;
ciation of sleep deprivation with reduction in insulin sensitivity as assessed
Kissei Pharmaceutical Co., Ltd.; and Johnson & Johnson and received lecture
by the hyperglycemic clamp technique in adolescents. JAMA Pediatr 170:
fees from Sanofi-Aventis Deutschland GmbH; Eli Lilly Japan K.K., Novo
487–494, 2016. doi:10.1001/jamapediatrics.2015.4365.
Nordisk Inc; Takeda Pharmaceutical Company Limited; Daiichi-Sankyo Co.,
14. de Oliveira EM, Visniauskas B, Sandri S, Migliorini S, Andersen ML,
Ltd.; Mitsubishi Tanabe Pharma Corporation; Merck & Co., Inc,; Dainippon
Sumitomo Pharma Co., Ltd.; Novartis Pharma K.K.; Kissei Pharmaceutical Tufik S, Fock RA, Chagas JR, Campa A. Late effects of sleep restric-
Co., Ltd.; Boehringer Ingelheim Pharmaceuticals, Inc.; Ono Pharmaceutical tion: potentiating weight gain and insulin resistance arising from a high-fat
Co., Ltd.; and AstraZeneca. The authors declare no conflicts of interest in diet in mice. Obesity (Silver Spring) 23: 391–398, 2015. doi:10.1002/oby.
relation to the work described in this manuscript. 20970.
15. Donga E, van Dijk M, van Dijk JG, Biermasz NR, Lammers GJ, van
Kralingen KW, Corssmit EP, Romijn JA. A single night of partial sleep
AUTHOR CONTRIBUTIONS deprivation induces insulin resistance in multiple metabolic pathways in
F.S., N.K., and H.F. conceived and designed research; F.S., N.K., H.I., F.Y., healthy subjects. J Clin Endocrinol Metab 95: 2963–2968, 2010. doi:10.
and S.K. performed experiments; F.S. and N.K. analyzed data; F.S., N.K., 1210/jc.2009-2430.
Y.T., H.F., and T.H. interpreted results of experiments; F.S. and N.K. prepared 16. Everson CA, Szabo A. Recurrent restriction of sleep and inadequate
figures; F.S. and N.K. drafted manuscript; F.S. and N.K. edited and revised recuperation induce both adaptive changes and pathological outcomes. Am
manuscript; F.S., N.K., Y.T., H.I., F.Y., S.K., H.F., and T.H. approved final J Physiol Regul Integr Comp Physiol 297: R1430 –R1440, 2009. doi:10.
version of manuscript. 1152/ajpregu.00230.2009.
The authors are fully responsible for all the content and editorial decisions, 17. Everson CA, Szabo A. Repeated exposure to severely limited sleep
were involved in all stages of the study and manuscript development, and results in distinctive and persistent physiological imbalances in rats. PLoS
approved the final version of the manuscript. N.K. is the guarantor of this work One 6: e22987, 2011. doi:10.1371/journal.pone.0022987.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER E857
18. Febinger HY, George A, Priestley J, Toth LA, Opp MR. Effects of 35. Nedeltcheva AV, Kessler L, Imperial J, Penev PD. Exposure to recur-
housing condition and cage change on characteristics of sleep in mice. J rent sleep restriction in the setting of high caloric intake and physical
Am Assoc Lab Anim Sci 53: 29 –37, 2014. inactivity results in increased insulin resistance and reduced glucose
19. Ferrell JM, Chiang JY. Short-term circadian disruption impairs bile acid tolerance. J Clin Endocrinol Metab 94: 3242–3250, 2009. doi:10.1210/jc.
and lipid homeostasis in mice. Cell Mol Gastroenterol Hepatol 1: 664 – 2009-0483.
677, 2015. doi:10.1016/j.jcmgh.2015.08.003. 36. Novati A, Roman V, Cetin T, Hagewoud R, den Boer JA, Luiten PG,
20. Finck BN, Gropler MC, Chen Z, Leone TC, Croce MA, Harris TE, Meerlo P. Chronically restricted sleep leads to depression-like changes in
Lawrence JC Jr, Kelly DP. Lipin 1 is an inducible amplifier of the neurotransmitter receptor sensitivity and neuroendocrine stress reactivity
hepatic PGC-1alpha/PPARalpha regulatory pathway. Cell Metab 4: 199 – in rats. Sleep 31: 1579 –1585, 2008. doi:10.1093/sleep/31.11.1579.
210, 2006. doi:10.1016/j.cmet.2006.08.005. 37. Ohashi Y, Hirayama A, Ishikawa T, Nakamura S, Shimizu K, Ueno Y,
21. Gilardi F, Migliavacca E, Naldi A, Baruchet M, Canella D, Le Tomita M, Soga T. Depiction of metabolome changes in histidine-starved
Martelot G, Guex N, Desvergne B; CycliX Consortium. Genome-wide Escherichia coli by CE-TOFMS. Mol Biosyst 4: 135–147, 2008. doi:10.
analysis of SREBP1 activity around the clock reveals its combined 1039/B714176A.
dependency on nutrient and circadian signals. PLoS Genet 10: e1004155, 38. Oishi K, Yamamoto S, Itoh N, Miyazaki K, Nemoto T, Nakakita Y,
2014. doi:10.1371/journal.pgen.1004155. Kaneda H. Disruption of behavioral circadian rhythms induced by psy-
22. González-Ortiz M, Martínez-Abundis E, Balcázar-Muñoz BR, chophysiological stress affects plasma free amino acid profiles without
Pascoe-González S. Effect of sleep deprivation on insulin sensitivity and affecting peripheral clock gene expression in mice. Biochem Biophys Res
cortisol concentration in healthy subjects. Diabetes Nutr Metab 13: 80 –83, Commun 450: 880 –884, 2014. doi:10.1016/j.bbrc.2014.06.083.
2000. 39. Okumura T. Role of lipid droplet proteins in liver steatosis. J Physiol
23. Guyon A, Morselli LL, Balbo ML, Tasali E, Leproult R, L’Hermite- Biochem 67: 629 –636, 2011. doi:10.1007/s13105-011-0110-6.
Balériaux M, Van Cauter E, Spiegel K. Effects of insufficient sleep on 40. Ooga T, Sato H, Nagashima A, Sasaki K, Tomita M, Soga T, Ohashi
pituitary-adrenocortical response to CRH stimulation in healthy men. Y. Metabolomic anatomy of an animal model revealing homeostatic
Sleep 40: zsx064, 2017. doi:10.1093/sleep/zsx064. imbalances in dyslipidaemia. Mol Biosyst 7: 1217–1223, 2011. doi:10.
24. Hsieh SD, Muto T, Murase T, Tsuji H, Arase Y. Association of short 1039/c0mb00141d.
sleep duration with obesity, diabetes, fatty liver and behavioral factors 41. Panda S, Antoch MP, Miller BH, Su AI, Schook AB, Straume M,
in Japanese men. Intern Med 50: 2499 –2502, 2011. doi:10.2169/ Schultz PG, Kay SA, Takahashi JS, Hogenesch JB. Coordinated tran-
internalmedicine.50.5844. scription of key pathways in the mouse by the circadian clock. Cell 109:
25. Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic 307–320, 2002. doi:10.1016/S0092-8674(02)00722-5.
consequences of sleep deprivation. Sleep Med Rev 11: 163–178, 2007. 42. Patel R, Williams-Dautovich J, Cummins CL. Minireview: new molec-
doi:10.1016/j.smrv.2007.01.002. ular mediators of glucocorticoid receptor activity in metabolic tissues. Mol
26. Kumashiro N, Beddow SA, Vatner DF, Majumdar SK, Cantley JL, Endocrinol 28: 999 –1011, 2014. doi:10.1210/me.2014-1062.
Guebre-Egziabher F, Fat I, Guigni B, Jurczak MJ, Birkenfeld AL, 43. Penev PD. Update on energy homeostasis and insufficient sleep. J Clin
Endocrinol Metab 97: 1792–1801, 2012. doi:10.1210/jc.2012-1067.
Kahn M, Perler BK, Puchowicz MA, Manchem VP, Bhanot S, Still
44. Perry RJ, Camporez JG, Kursawe R, Titchenell PM, Zhang D, Perry
CD, Gerhard GS, Petersen KF, Cline GW, Shulman GI, Samuel VT.
CJ, Jurczak MJ, Abudukadier A, Han MS, Zhang XM, Ruan HB,
Targeting pyruvate carboxylase reduces gluconeogenesis and adiposity
Yang X, Caprio S, Kaech SM, Sul HS, Birnbaum MJ, Davis RJ, Cline
and improves insulin resistance. Diabetes 62: 2183–2194, 2013. doi:10.
GW, Petersen KF, Shulman GI. Hepatic acetyl CoA links adipose tissue
2337/db12-1311.
inflammation to hepatic insulin resistance and type 2 diabetes. Cell 160:
27. Kumashiro N, Erion DM, Zhang D, Kahn M, Beddow SA, Chu X, Still
745–758, 2015. doi:10.1016/j.cell.2015.01.012.
CD, Gerhard GS, Han X, Dziura J, Petersen KF, Samuel VT, Shul-
45. Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI. Impaired
man GI. Cellular mechanism of insulin resistance in nonalcoholic fatty
mitochondrial activity in the insulin-resistant offspring of patients with
liver disease. Proc Natl Acad Sci USA 108: 16381–16385, 2011. doi:10.
type 2 diabetes. N Engl J Med 350: 664 –671, 2004. doi:10.1056/
1073/pnas.1113359108. NEJMoa031314.
28. Kumashiro N, Tamura Y, Uchida T, Ogihara T, Fujitani Y, Hirose T, 46. Rao MN, Neylan TC, Grunfeld C, Mulligan K, Schambelan M,
Mochizuki H, Kawamori R, Watada H. Impact of oxidative stress and Schwarz JM. Subchronic sleep restriction causes tissue-specific insulin
peroxisome proliferator-activated receptor gamma coactivator-1alpha in resistance. J Clin Endocrinol Metab 100: 1664 –1671, 2015. doi:10.1210/
hepatic insulin resistance. Diabetes 57: 2083–2091, 2008. doi:10.2337/ jc.2014-3911.
db08-0144. 47. Rasmussen S, Miller MM, Filipski SB, Tolwani RJ. Cage change
29. Kumashiro N, Yoshimura T, Cantley JL, Majumdar SK, Guebre- influences serum corticosterone and anxiety-like behaviors in the mouse.
Egziabher F, Kursawe R, Vatner DF, Fat I, Kahn M, Erion DM, J Am Assoc Lab Anim Sci 50: 479 –483, 2011.
Zhang XM, Zhang D, Manchem VP, Bhanot S, Gerhard GS, Petersen 48. Rechtschaffen A, Bergmann BM. Sleep deprivation in the rat: an update
KF, Cline GW, Samuel VT, Shulman GI. Role of patatin-like phospho- of the 1989 paper. Sleep 25: 18 –24, 2002. doi:10.1093/sleep/25.1.18.
lipase domain-containing 3 on lipid-induced hepatic steatosis and insulin 49. Rutkowsky JM, Knotts TA, Ono-Moore KD, McCoin CS, Huang S,
resistance in rats. Hepatology 57: 1763–1772, 2013. doi:10.1002/hep. Schneider D, Singh S, Adams SH, Hwang DH. Acylcarnitines activate
26170. proinflammatory signaling pathways. Am J Physiol Endocrinol Metab
30. Kwon EY, Jung UJ, Park T, Yun JW, Choi MS. Luteolin attenuates 306: E1378 –E1387, 2014. doi:10.1152/ajpendo.00656.2013.
hepatic steatosis and insulin resistance through the interplay between the 50. Samuel VT, Shulman GI. The pathogenesis of insulin resistance: inte-
liver and adipose tissue in mice with diet-induced obesity. Diabetes 64: grating signaling pathways and substrate flux. J Clin Invest 126: 12–22,
1658 –1669, 2015. doi:10.2337/db14-0631. 2016. doi:10.1172/JCI77812.
31. Matsumoto E, Ishihara A, Tamai S, Nemoto A, Iwase K, Hiwasa T, 51. Saponaro C, Gaggini M, Carli F, Gastaldelli A. The subtle balance
Shibata S, Takiguchi M. Time of day and nutrients in feeding govern between lipolysis and lipogenesis: a critical point in metabolic homeosta-
daily expression rhythms of the gene for sterol regulatory element-binding sis. Nutrients 7: 9453–9474, 2015. doi:10.3390/nu7115475.
protein (SREBP)-1 in the mouse liver. J Biol Chem 285: 33028 –33036, 52. Schmitz-Peiffer C. Targeting ceramide synthesis to reverse insulin resis-
2010. doi:10.1074/jbc.M109.089391. tance. Diabetes 59: 2351–2353, 2010. doi:10.2337/db10-0912.
32. Mazzoccoli G, Vinciguerra M, Oben J, Tarquini R, De Cosmo S. 53. Sengupta A, Rhoades SD, Kim EJ, Nayak S, Grant GR, Meerlo P,
Non-alcoholic fatty liver disease: the role of nuclear receptors and circa- Weljie AM. Sleep restriction induced energy, methylation and lipogenesis
dian rhythmicity. Liver Int 34: 1133–1152, 2014. doi:10.1111/liv.12534. metabolic switches in rat liver. Int J Biochem Cell Biol 93: 129 –135, 2017.
33. Meerlo P, Koehl M, van der Borght K, Turek FW. Sleep restriction doi:10.1016/j.biocel.2017.08.014.
alters the hypothalamic-pituitary-adrenal response to stress. J Neuroendo- 54. Sgoifo A, Buwalda B, Roos M, Costoli T, Merati G, Meerlo P. Effects
crinol 14: 397–402, 2002. doi:10.1046/j.0007-1331.2002.00790.x. of sleep deprivation on cardiac autonomic and pituitary-adrenocortical
34. Miyazaki K, Itoh N, Ohyama S, Kadota K, Oishi K. Continuous stress reactivity in rats. Psychoneuroendocrinology 31: 197–208, 2006.
exposure to a novel stressor based on water aversion induces abnormal doi:10.1016/j.psyneuen.2005.06.009.
circadian locomotor rhythms and sleep-wake cycles in mice. PLoS One 8: 55. Shigiyama F, Kumashiro N, Furukawa Y, Funayama T, Takeno K,
e55452, 2013. doi:10.1371/journal.pone.0055452. Wakui N, Ikehara T, Nagai H, Taka H, Fujimura T, Uchino H,
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
E858 HEPATIC STEATOSIS AND INSULIN RESISTANCE BY SLEEP DISORDER
Tamura Y, Watada H, Nemoto T, Shiraga N, Sumino Y, Hirose T. 62. Utzschneider KM, Kahn SE. Review: The role of insulin resistance in
Characteristics of hepatic insulin-sensitive nonalcoholic fatty liver disease. nonalcoholic fatty liver disease. J Clin Endocrinol Metab 91: 4753–4761,
Hepatol Commun 1: 634 –647, 2017. doi:10.1002/hep4.1077. 2006. doi:10.1210/jc.2006-0587.
56. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest 106: 63. van den Berg R, Mook-Kanamori DO, Donga E, van Dijk M, van Dijk
171–176, 2000. doi:10.1172/JCI10583. JG, Lammers GJ, van Kralingen KW, Prehn C, Adamski J, Romijn
57. Sinturel F, Gerber A, Mauvoisin D, Wang J, Gatfield D, Stubblefield JA, van Dijk KW, Corssmit EP, Rensen PC, Biermasz NR. A single
JJ, Green CB, Gachon F, Schibler U. Diurnal oscillations in liver mass night of sleep curtailment increases plasma acylcarnitines: Novel insights
and cell size accompany ribosome assembly cycles. Cell 169: 651– in the relationship between sleep and insulin resistance. Arch Biochem
663.e14, 2017. doi:10.1016/j.cell.2017.04.015. Biophys 589: 145–151, 2016. doi:10.1016/j.abb.2015.09.017.
58. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic 64. Vatner DF, Majumdar SK, Kumashiro N, Petersen MC, Rahimi Y,
and endocrine function. Lancet 354: 1435–1439, 1999. doi:10.1016/
Gattu AK, Bears M, Camporez JP, Cline GW, Jurczak MJ, Samuel
S0140-6736(99)01376-8.
VT, Shulman GI. Insulin-independent regulation of hepatic triglyceride
59. Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and
short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol 5: synthesis by fatty acids. Proc Natl Acad Sci USA 112: 1143–1148, 2015.
253–261, 2009. doi:10.1038/nrendo.2009.23. doi:10.1073/pnas.1423952112.
60. Tahara Y, Shibata S. Circadian rhythms of liver physiology and disease: 65. Weljie AM, Meerlo P, Goel N, Sengupta A, Kayser MS, Abel T,
experimental and clinical evidence. Nat Rev Gastroenterol Hepatol 13: Birnbaum MJ, Dinges DF, Sehgal A. Oxalic acid and diacylglycerol
217–226, 2016. doi:10.1038/nrgastro.2016.8. 36:3 are cross-species markers of sleep debt. Proc Natl Acad Sci USA 112:
61. Tamura Y, Ogihara T, Uchida T, Ikeda F, Kumashiro N, Nomiyama 2569 –2574, 2015. doi:10.1073/pnas.1417432112.
T, Sato F, Hirose T, Tanaka Y, Mochizuki H, Kawamori R, Watada 66. Zhang SX, Khalyfa A, Wang Y, Carreras A, Hakim F, Neel BA, Brady
H. Amelioration of glucose tolerance by hepatic inhibition of nuclear MJ, Qiao Z, Hirotsu C, Gozal D. Sleep fragmentation promotes NADPH
factor kappaB in db/db mice. Diabetologia 50: 131–141, 2007. doi:10. oxidase 2-mediated adipose tissue inflammation leading to insulin resis-
1007/s00125-006-0467-1. tance in mice. Int J Obes 38: 619 –624, 2014. doi:10.1038/ijo.2013.139.
AJP-Endocrinol Metab • doi:10.1152/ajpendo.00072.2018 • www.ajpendo.org
Downloaded from journals.physiology.org/journal/ajpendo (194.027.203.180) on March 8, 2021.
You might also like
- Chronic Sleep Disorder Induced by Psychophysiological Stress InducesDocument6 pagesChronic Sleep Disorder Induced by Psychophysiological Stress InducesRicardo VegaNo ratings yet
- Leptin: Regulation and Clinical ApplicationsFrom EverandLeptin: Regulation and Clinical ApplicationsSam Dagogo-Jack, MDNo ratings yet
- Jejum IntermitenteDocument11 pagesJejum IntermitenteJohn Talmid De Yeshua HamashiachNo ratings yet
- Effect of Intermittent Fasting On Brain Neurotransmitters, Neutrophils Phagocytic Activity, and Histopathological Finding in Some Organs in RatsDocument8 pagesEffect of Intermittent Fasting On Brain Neurotransmitters, Neutrophils Phagocytic Activity, and Histopathological Finding in Some Organs in RatsBrian ColborneNo ratings yet
- Jurnal InternationalDocument9 pagesJurnal InternationalAngelNo ratings yet
- G4 TEMA REPRODUCCIÓN Dieta y ReproducciónDocument10 pagesG4 TEMA REPRODUCCIÓN Dieta y ReproducciónJorge EscobarNo ratings yet
- Social Isolation Affects The Development of Obesity and Type 2 Diabetes in MiceDocument9 pagesSocial Isolation Affects The Development of Obesity and Type 2 Diabetes in MiceNovita WulandariNo ratings yet
- Efecto Hipotalamico Lira2016-ObesityDocument8 pagesEfecto Hipotalamico Lira2016-ObesitylucilaNo ratings yet
- Circadian Rhythms, Metabolism, and Chrononutrition in Rodents and HumansDocument8 pagesCircadian Rhythms, Metabolism, and Chrononutrition in Rodents and HumansFranklin Howley-Dumit SerulleNo ratings yet
- Metabolic Changes in Serum Metabolome in Response To A MealDocument11 pagesMetabolic Changes in Serum Metabolome in Response To A MealmarcusmattosantosNo ratings yet
- Journal of Steroid Biochemistry & Molecular Biology: A A A A A A A A A B C 1 A 1Document8 pagesJournal of Steroid Biochemistry & Molecular Biology: A A A A A A A A A B C 1 A 1Fuada Haerana RifaiNo ratings yet
- Efecto Del Sueño en LeptinaDocument10 pagesEfecto Del Sueño en LeptinaLuiz Henrique De Oliveira LeiteNo ratings yet
- Alterations in Peripheral Purinergic and Muscarinic Signaling of Rat Bladder After Long-Term Fructose-Induced Metabolic SyndromeDocument13 pagesAlterations in Peripheral Purinergic and Muscarinic Signaling of Rat Bladder After Long-Term Fructose-Induced Metabolic SyndromeThalia KarampasiNo ratings yet
- NP2008 646919Document9 pagesNP2008 646919Mauricio Mondaca HerreraNo ratings yet
- Timothy H. Moran, Laura F. Katz, Carlos R. Plata-Salaman and Gary J. SchwartzDocument9 pagesTimothy H. Moran, Laura F. Katz, Carlos R. Plata-Salaman and Gary J. SchwartzSandra WithingtonNo ratings yet
- 61 10 09 s3 ArticleDocument6 pages61 10 09 s3 ArticlekasabeNo ratings yet
- MD 1 Section E2 Group 3 Biochem REVISEDDocument10 pagesMD 1 Section E2 Group 3 Biochem REVISEDParadoxistNo ratings yet
- Hons2009 PDFDocument11 pagesHons2009 PDFBkash ShahNo ratings yet
- Jcinvest00248 0177 PDFDocument11 pagesJcinvest00248 0177 PDFluis morales garzaNo ratings yet
- Auto0606 0702Document9 pagesAuto0606 0702sister girlfriendNo ratings yet
- Takenouchi 20151Document13 pagesTakenouchi 20151Angelique R. AltamiranoNo ratings yet
- Chrononutrition: Summary Well-Regulated Eating Habits Are Said To Be Important For Health. A MajorDocument3 pagesChrononutrition: Summary Well-Regulated Eating Habits Are Said To Be Important For Health. A MajorFranklin Howley-Dumit SerulleNo ratings yet
- 9048 FullDocument5 pages9048 FullFelia AlyciaNo ratings yet
- A Suprachiasmatic Nucleus Generated Rhythm in Basal GlucoseDocument11 pagesA Suprachiasmatic Nucleus Generated Rhythm in Basal GlucoseD Gonzalez GarciaNo ratings yet
- Effect of Intermittent Fasting and Refeeding On Insulin Action in Healthy MenDocument9 pagesEffect of Intermittent Fasting and Refeeding On Insulin Action in Healthy Mendgh3No ratings yet
- Best Practice & Research Clinical Endocrinology & MetabolismDocument16 pagesBest Practice & Research Clinical Endocrinology & MetabolismvipereejayNo ratings yet
- Obesity - 2012 - Sampey - Cafeteria Diet Is A Robust Model of Human Metabolic Syndrome With Liver and Adipose InflammationDocument10 pagesObesity - 2012 - Sampey - Cafeteria Diet Is A Robust Model of Human Metabolic Syndrome With Liver and Adipose InflammationRodrigoNo ratings yet
- Intermittent Fasting and Refeeding On Insulin Dependant MenDocument10 pagesIntermittent Fasting and Refeeding On Insulin Dependant MenTyrone PenningNo ratings yet
- Gutman Et Al 2008Document10 pagesGutman Et Al 2008Roee GutmanNo ratings yet
- Intermittent Fasting Induces Hypothalamic Modifications Resulting in Low Feeding Efficiency, Low Body Mass and Overating 2014Document11 pagesIntermittent Fasting Induces Hypothalamic Modifications Resulting in Low Feeding Efficiency, Low Body Mass and Overating 2014Camila VidigalNo ratings yet
- Perfil Das Citocinas de Ratos Alimentados Com Dieta de CamarãoDocument8 pagesPerfil Das Citocinas de Ratos Alimentados Com Dieta de CamarãoApolosclayograndelutador GrandelutadorNo ratings yet
- Gutman Et Al 2011cDocument4 pagesGutman Et Al 2011cRoee GutmanNo ratings yet
- Hypertension 2006 Ryan 988 93Document7 pagesHypertension 2006 Ryan 988 93lm_catalinaNo ratings yet
- Enmet DM AntioxDocument9 pagesEnmet DM AntioxAreef MuarifNo ratings yet
- Physiological Effects of Melatonin On Leptin, Testosterone and Biochemical Parameters in Albino RatsDocument6 pagesPhysiological Effects of Melatonin On Leptin, Testosterone and Biochemical Parameters in Albino RatsIOSR Journal of PharmacyNo ratings yet
- PDF 5Document40 pagesPDF 5agung krisNo ratings yet
- 12 - AsurDocument8 pages12 - AsurFujiko SaavedraNo ratings yet
- Sherman Et Al 2011bDocument15 pagesSherman Et Al 2011bRoee GutmanNo ratings yet
- Structure Kestose and NystoseDocument6 pagesStructure Kestose and NystoseJavier MendozaNo ratings yet
- Effects of Dietary Carbohydrate Restriction With High Protein Intake On Protein Metabolism and The Somatotropic AxisDocument7 pagesEffects of Dietary Carbohydrate Restriction With High Protein Intake On Protein Metabolism and The Somatotropic Axisthe bungalowvideotapesNo ratings yet
- Effect of A Hyper-Protein Diet On Wistar Rats Development and Intestinal FunctionDocument6 pagesEffect of A Hyper-Protein Diet On Wistar Rats Development and Intestinal FunctionhafizNo ratings yet
- Ni Hms 958771Document31 pagesNi Hms 958771Cem Tunaboylu (Student)No ratings yet
- SSRN Id3309237Document10 pagesSSRN Id3309237Bima Anugrah WijayaNo ratings yet
- Caffeine and Sleep Deprivation Mediated Changes in Open Field Be 2016 SleepDocument8 pagesCaffeine and Sleep Deprivation Mediated Changes in Open Field Be 2016 SleepIngrid DíazNo ratings yet
- Sleep and Circadian Rhythms: Key Components in The Regulation of Energy MetabolismDocument10 pagesSleep and Circadian Rhythms: Key Components in The Regulation of Energy MetabolismAacg MeryendNo ratings yet
- Seminario 5 Degradacion de Proteinas 2012Document9 pagesSeminario 5 Degradacion de Proteinas 2012pau_sebNo ratings yet
- Diabetes PDFDocument12 pagesDiabetes PDFDANIELA MALAGÓN MONTAÑONo ratings yet
- Effect and Interactions of Pueraria-Rehmannia and Aerobic Exercise On MetabolicDocument9 pagesEffect and Interactions of Pueraria-Rehmannia and Aerobic Exercise On Metabolicyhenti widjayantiNo ratings yet
- Onion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsDocument8 pagesOnion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsRizky Agustian HadiNo ratings yet
- Ramadhan Et CancerDocument12 pagesRamadhan Et CancerSarah MellaliNo ratings yet
- Alkaline Phosphatase Activity of Duodenal Enterocytes After Neonatal Administration of Monosodium Glutamate To RatsDocument14 pagesAlkaline Phosphatase Activity of Duodenal Enterocytes After Neonatal Administration of Monosodium Glutamate To RatsGusti GandhaNo ratings yet
- Central Administration of Ghrelin Induces Conditi - 2017 - European NeuropsychopDocument7 pagesCentral Administration of Ghrelin Induces Conditi - 2017 - European NeuropsychopdanilomarandolaNo ratings yet
- Effect of Chickpea On GlucoseDocument7 pagesEffect of Chickpea On GlucoseMia DragostinNo ratings yet
- Wan Et Al 2019 PDFDocument8 pagesWan Et Al 2019 PDFEdgar Huerta CardenasNo ratings yet
- Lept in 012Document7 pagesLept in 012Carolina De Lima FerreiraNo ratings yet
- Xu 2010 Carbohydrate-To-Fat Ratio Affects Food Intake and Body Weight in Wistar RatsDocument6 pagesXu 2010 Carbohydrate-To-Fat Ratio Affects Food Intake and Body Weight in Wistar RatsPaul SimononNo ratings yet
- Articulo para Expo TraducirDocument6 pagesArticulo para Expo TraducirViki G PNo ratings yet
- Ness 2019Document27 pagesNess 2019Érica MunizNo ratings yet
- The Relationship Between Sleep Disturbances and DiabetesDocument15 pagesThe Relationship Between Sleep Disturbances and Diabeteskarar.hasan2000No ratings yet
- Free Radical Biology & Medicine: Lalini Ramanathan, Jerome M. SiegelDocument7 pagesFree Radical Biology & Medicine: Lalini Ramanathan, Jerome M. SiegelNazan ElmaNo ratings yet
- Bone Turnover Markers and Probable Advanced Nonalcoholic Fatty Liver Disease in MiddleAged and Elderly Men and Postmenopausal Women With Type 2 DiabetesDocument11 pagesBone Turnover Markers and Probable Advanced Nonalcoholic Fatty Liver Disease in MiddleAged and Elderly Men and Postmenopausal Women With Type 2 DiabetesNazan ElmaNo ratings yet
- Brain Research BulletinDocument7 pagesBrain Research BulletinNazan ElmaNo ratings yet
- Estrogens and Female Liver HealthDocument6 pagesEstrogens and Female Liver HealthNazan ElmaNo ratings yet
- Epithelial-Neuronal Communication in Thecolon - Implications For Visceral PainDocument12 pagesEpithelial-Neuronal Communication in Thecolon - Implications For Visceral PainNazan ElmaNo ratings yet
- Life Sciences: Haitham S. Mohammed, Yasser A. KhadrawyDocument9 pagesLife Sciences: Haitham S. Mohammed, Yasser A. KhadrawyNazan ElmaNo ratings yet
- Expression of Fibroblast Growth Factor 9 and Its.97885Document5 pagesExpression of Fibroblast Growth Factor 9 and Its.97885Nazan ElmaNo ratings yet
- S J H Biddle@lboro Ac UkDocument32 pagesS J H Biddle@lboro Ac UkNazan ElmaNo ratings yet
- Intranasal Injection of Recombinant Human Erythropoietin Improves Cognitive and Visual Impairments in Chronic Cerebral Ischemia RatsDocument7 pagesIntranasal Injection of Recombinant Human Erythropoietin Improves Cognitive and Visual Impairments in Chronic Cerebral Ischemia RatsNazan ElmaNo ratings yet
- AKUPUNKTURDocument12 pagesAKUPUNKTURNazan ElmaNo ratings yet
- The Effect of Pyruvate On The Development and Progression of Post-Stroke DepressionDocument12 pagesThe Effect of Pyruvate On The Development and Progression of Post-Stroke DepressionNazan ElmaNo ratings yet
- Additional English Handout For Printing 2nd BatchDocument4 pagesAdditional English Handout For Printing 2nd BatchCaracel Sobiono sub2sobNo ratings yet
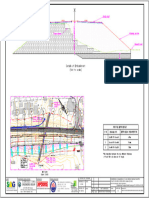
- Sag 011 5267 DSN PW em 24.380 24.520 Ol SG2 100 01Document1 pageSag 011 5267 DSN PW em 24.380 24.520 Ol SG2 100 01Sanjay SwamiNo ratings yet
- Canada Autos (DSC) (Panel)Document15 pagesCanada Autos (DSC) (Panel)Frontyardservices Uganda limitedNo ratings yet
- I Found The PathDocument72 pagesI Found The PathmasterrkNo ratings yet
- LL Module Barrowmaze 1 (Lv1-8, GG, 2012)Document87 pagesLL Module Barrowmaze 1 (Lv1-8, GG, 2012)Tony Helano100% (3)
- GE RT 3200 Advantage III Quick GuideDocument78 pagesGE RT 3200 Advantage III Quick GuideluisNo ratings yet
- Chemical Spill Kits ChecklistDocument14 pagesChemical Spill Kits ChecklistHaifaa ZakariaNo ratings yet
- Honeywell Question 1&2Document6 pagesHoneywell Question 1&2anon_909027967No ratings yet
- Glass Performance Days 2007Document5 pagesGlass Performance Days 2007Daren Talana0% (1)
- OSI Model and Its LayersDocument9 pagesOSI Model and Its LayersBakhtiyarNo ratings yet
- AutoSPRINK12InstallationWalkthrough PDFDocument2 pagesAutoSPRINK12InstallationWalkthrough PDFHai PhamNo ratings yet
- Example 1: Analytical Exposition TextDocument1 pageExample 1: Analytical Exposition Textlenni marianaNo ratings yet
- Leontief PDFDocument7 pagesLeontief PDFErvin ArrasyidNo ratings yet
- Technical Data: Rotax Kart Type R1, Model 2002Document2 pagesTechnical Data: Rotax Kart Type R1, Model 2002Gallego VilaNo ratings yet
- Multiple Choice Quiz Chapter 5Document4 pagesMultiple Choice Quiz Chapter 5gottwins05No ratings yet
- Black 2018 B Uploaded VersionDocument46 pagesBlack 2018 B Uploaded VersionOwais AhmedNo ratings yet
- VMTC RAII Presentation PDFDocument154 pagesVMTC RAII Presentation PDFDarwin Nacion ManquiquisNo ratings yet
- PTCL Internship Report 2020Document16 pagesPTCL Internship Report 2020Abdul WaheedNo ratings yet
- L7 Nonideal Flow Example ProblemsDocument33 pagesL7 Nonideal Flow Example ProblemsRicky JayNo ratings yet
- Seminar TopicsDocument21 pagesSeminar Topics123321No ratings yet
- Subject Orientation AP10Document26 pagesSubject Orientation AP10mikejones cotejoNo ratings yet
- 9bWJ4riXFBGGECh12 AutocorrelationDocument17 pages9bWJ4riXFBGGECh12 AutocorrelationRohan Deepika RawalNo ratings yet
- Calcium Silicate Bricks or Sand Lime BricksDocument4 pagesCalcium Silicate Bricks or Sand Lime Bricksmanhal alnoaimyNo ratings yet
- Assembly Drawing Tail Stock 2Document12 pagesAssembly Drawing Tail Stock 2Syech Maulana Malik100% (1)
- Electric Bike BatteryDocument3 pagesElectric Bike BatteryOrganic MechanicNo ratings yet
- SIP As A Stability Builder For A Retail InvestorDocument84 pagesSIP As A Stability Builder For A Retail InvestorprathamNo ratings yet
- Xtreet 250X 2017 Parts Catalogue 2016 08 16 1Document32 pagesXtreet 250X 2017 Parts Catalogue 2016 08 16 1JeovannyAlexanderMatamorosSanchezNo ratings yet
- Us District Court of Massachusetts Promotes Human and Constitutional Rights Violator Magistrate Judge Leo T. Sorokin To Chief Magistrate JudgeDocument98 pagesUs District Court of Massachusetts Promotes Human and Constitutional Rights Violator Magistrate Judge Leo T. Sorokin To Chief Magistrate Judgetired_of_corruptionNo ratings yet
- TAI PI 500 2018 FormattedDocument54 pagesTAI PI 500 2018 FormattedShinoharaNo ratings yet
- Abc Stock AcquisitionDocument13 pagesAbc Stock AcquisitionMary Joy AlbandiaNo ratings yet
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (5)
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (2)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodFrom EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNo ratings yet
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- The Noom Kitchen: 100 Healthy, Delicious, Flexible Recipes for Every DayFrom EverandThe Noom Kitchen: 100 Healthy, Delicious, Flexible Recipes for Every DayNo ratings yet
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (352)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- Ultrametabolism: The Simple Plan for Automatic Weight LossFrom EverandUltrametabolism: The Simple Plan for Automatic Weight LossRating: 4.5 out of 5 stars4.5/5 (28)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingFrom EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingRating: 5 out of 5 stars5/5 (61)
- Rapid Weight Loss Hypnosis: Deep Sleep Your Way to Rapid Weight Loss, Healing Your Body and Self Esteem with Guided Meditations and Positive AffirmationsFrom EverandRapid Weight Loss Hypnosis: Deep Sleep Your Way to Rapid Weight Loss, Healing Your Body and Self Esteem with Guided Meditations and Positive AffirmationsRating: 5 out of 5 stars5/5 (7)
- The Longevity Plan: Seven Life-Transforming Lessons from Ancient ChinaFrom EverandThe Longevity Plan: Seven Life-Transforming Lessons from Ancient ChinaNo ratings yet
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- Foods That Cause You to Lose Weight: The Negative Calorie EffectFrom EverandFoods That Cause You to Lose Weight: The Negative Calorie EffectRating: 3 out of 5 stars3/5 (5)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)