Professional Documents
Culture Documents
Hypertension 2006 Ryan 988 93
Uploaded by
lm_catalinaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertension 2006 Ryan 988 93
Uploaded by
lm_catalinaCopyright:
Available Formats
Insulin Resistance and Obesity in Lupus
Insulin Resistance and Obesity in a Mouse Model of
Systemic Lupus Erythematosus
Michael J. Ryan, Gerald R. McLemore Jr, Steven T. Hendrix
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
AbstractAccumulating data indicate that metabolic syndrome is an inflammatory condition. Systemic lupus erythematosus (SLE) is an autoimmune disorder associated with nephritis and cardiovascular disease. Evidence suggests that
individuals with SLE are at risk for developing insulin resistance; however, this has not been directly examined. Using
an established mouse strain with SLE (NZBWF1), we examined whether SLE is associated with increased body weight
and fat deposition. Mean arterial pressure was significantly increased (1404 versus 1142 mm Hg; n5) in SLE mice
by 36 weeks of age compared with control mice (NZW/LacJ). Body weight in SLE mice was higher at each age
compared with controls by 12%, 22%, and 34% (n30). Visceral adipose tissue weight was increased in SLE by 44%,
74%, and 117% at 8, 20, and 36 weeks, respectively (n12). Plasma leptin was increased in SLE mice (8.61.0 versus
24.72.2 ng/mL; n5), and renal and adipose tissue exhibited macrophage infiltration. Fasted insulin was higher in
SLE mice (0.60.1 versus 1.40.3 ng/mL; n10), but fasted glucose was not different (945 versus 809; n9). A
glucose tolerance test caused a significantly greater and longer increase in blood glucose from mice with SLE compared
with control mice. Food intake was not different between control and SLE mice. However, mice with SLE demonstrated
lower levels of nighttime activity than controls. These data show that the NZBWF1 strain may be an important model
to study the effects of obesity and insulin resistance on SLE-associated hypertension. (Hypertension. 2006;48:988-993.)
Key Words: SLE autoimmune inflammation insulin adipose leptin glucose
etabolic syndrome can be characterized by a group of
metabolic risk factors that includes central obesity,
insulin resistance, dyslipidemia, increased blood pressure,
and endothelial dysfunction.1 Individuals with metabolic
syndrome are at a markedly increased risk for developing
hypertension and renal disease. Recent evidence indicates
that inflammatory cytokines are elevated in patients with
metabolic syndrome,2 4 thus suggesting a role for chronic
inflammation as an underlying mechanism for progression of
this disease.
Systemic lupus erythematosus (SLE) is a chronic inflammatory disorder that predominantly affects women during
their reproductive years. The presence of autoantibodies
(typically antinuclear antibodies) is used diagnostically, and
although SLE can influence many organ systems, the skin,
joints, and kidneys are typically affected. Like metabolic
syndrome, a large percentage of individuals with SLE are
hypertensive. Evidence suggests that individuals with SLE
are also at increased risk for developing insulin resistance5
and changes in body mass composition6; however, this has
not been adequately examined.
The purpose of the present study was to test whether the
progression of SLE is associated with changes in body
composition, insulin sensitivity, and other characteristics of
the metabolic syndrome. To examine this, we used a genetic
mouse model of SLE (NZBWF1) that exhibits many features
of human SLE, including a complex genetic origin, a bias for
the female sex, immune complex glomerulonephritis, and the
presence of antinuclear antibodies. We reported recently that
these mice have hypertension and impaired endothelialdependent relaxation.7 The results of the present study show
that NZBWF1 mice also have several other characteristics of
the metabolic syndrome that may contribute to the hypertension, including central obesity, insulin resistance, and hyperleptinemia. These data show that the NZBWF1 strain may be
an important model to study the effects of obesity and insulin
resistance on SLE-associated hypertension.
Methods
Animals
Female NZBWF1 (SLE) and NZW/LacJ (control) obtained from
Jackson Laboratories (Bar Harbor, ME) were maintained on a
12-hour light/dark cycle, normal chow, and water ad libitum. Mice
were studied at 8 (7.80.7 weeks), 20 (21.20.3 weeks), and 36
(36.40.1 week) weeks of age. These ages correspond with the onset
of sexual maturity, pre-SLE, and full SLE, respectively. At 36 weeks
of age, female mice are fully capable of reproduction, and a decline
in ovarian hormones would be expected to improve or delay the
onset of SLE in NZBWF1 females. All of the studies were performed
Received July 26, 2006; first decision August 13, 2006; revision accepted August 21, 2006.
This paper was sent to Ernesto L. Schiffrin, associate editor, for review by expert referees, editorial decision, and final disposition.
From the Department of Physiology, University of Mississippi Medical Center, Jackson, Miss.
Correspondence to Michael J. Ryan, Department of Physiology and Biophysics, University of Mississippi Medical Center, 2500 North State St,
Jackson, MS 39216. E-mail mjryan@physiology.umsmed.edu
2006 American Heart Association, Inc.
Hypertension is available at http://www.hypertensionaha.org
DOI: 10.1161/01.HYP.0000243612.02929.df
988
Ryan et al
Insulin Resistance, Obesity, and SLE
989
with the approval of the University of Mississippi Medical Center
Institutional Animal Care and Use Committee and in accordance
with National Institutes of Health guidelines.
Physical Characteristics
Body weight (in grams) was measured for all of the mice. A
subgroup was euthanized and dissected for measurement of total
visceral adipose (omentalovarian/uterineretroperitoneal) and to
weigh individual adipose depots (ovarian/uterine, retroperitoneal,
and thermogenic). Mice were acclimated for 5 days to being individually housed before daily food intake was measured (in grams)
and normalized to grams per 24 hours. The effect of leptin on food
intake was also measured in 36-week-old mice. Mouse leptin (R&D
Systems) was administered via intraperitoneal injection (30 g,
twice daily) for 3 days. Intraperitoneal injection of vehicle (saline)
was used as a control.
Blood Glucose, Insulin, and Leptin
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
Thirty-six-week-old NZBWF1 and NZW/LacJ mice were fasted for
6 hours before collecting blood samples with EDTA through
retro-orbital punctures in lightly anesthetized animals (isoflurane).
Fifteen microliters were used with the Accuchek Advantage glucometer (Roche) to measure blood glucose in milligrams per deciliter.
Remaining blood samples were centrifuged, and plasma samples
were stored at 80C.
Fasted insulin (nanograms per milliliter) was measured using a
Rat/Mouse Insulin ELISA kit (Linco Research). Plasma leptin levels
(nanograms per milliliter) were measured using the Quantikine
Mouse Leptin Immunoassay (R&D Systems).
Glucose tolerance was tested in 36-week-old NZBWF1 and
NZW/LacJ mice. Carotid artery catheters were implanted as described previously.8 10 The next day mice were fasted for 6 hours at
which time a 15-L sample of blood was analyzed for basal blood
glucose levels. Each mouse was administered an intraperitoneal
injection of isosmotic glucose (317 mmol/L). Fifteen-microliter
blood samples were taken through the carotid catheter, and glucose
was measured at 20, 40, 60, 120, and 180 minutes postinjection. This
method has been reported previously.11
Mean Arterial Pressure
Mean arterial pressure (MAP) was measured with indwelling carotid artery catheters attached to an external force displacement
transducer as described previously.9,12 Mice were allowed 48 hours
to recover before measurements were made. Surgeries were performed under isoflurane anesthesia, and bupivacaine (subcutaneous)
was used postoperatively as an analgesic.
Animal Activity
Radiotelemeters (PAC10 or PAC20, DSI) were implanted in
NZBWF1 and NZW/LacJ mice at 8, 20, and 36 weeks of age as
described previously.7 Mice recovered for 1 week before measuring activity continuously (24 hours per day) for 4 consecutive days.
Measurements are a relative measure of locomotor activity (high
counts means the animal was active) and cannot be used to calculate
distance or type of activity.
Figure 1. MAP is increased at 36 weeks of age in SLE mice
compared with controls. Pressure was measured by indwelling
carotid artery catheters in conscious freely moving mice.
(*P0.05, 1-way ANOVA).
control and 6 SLE mice were incubated with Oil-Red-O to test for
the presence of hepatic liver accumulation. Sections were counterstained with hematoxylin/eosin.
Statistics
A 1-way ANOVA with StudentNewmanKeuls post hoc test for all
of the pairwise comparisons was used to assess differences across
different age groups and between control and SLE animals. A
Student t test was used to assess statistical significance when
comparing only control and SLE groups. Significance was accepted
at P0.05.
Results
As we have reported recently,7 SLE mice are hypertensive
compared with control animals by 36 weeks of age (Figure 1).
Body weight in female SLE (NZBWF1) mice at 8, 20, and 36
weeks of age was significantly greater than control mice
(NZW/LacJ) and by a progressively larger margin (12%,
21%, and 34%) at each age (Figure 2 and Table). Weights,
indexed for body length (excluding tail), were significantly
higher in SLE mice compared with controls at 36 weeks of
age (0.360.00 versus 0.400.02 g/cm2; P0.01, Student
t test). Visceral adipose tissue from SLE mice was significantly increased by 20 weeks of age with a progressively
larger margin (73% to 117%; Table). Adipose tissue weight
from individual depots, including ovarian/uterine, retroperitoneal, and thermogenic (brown), was also measured. Thermogenic adipose tissue was not different between control and
Histology
Ovarian/uterine adipose or kidneys were fixed in 10% neutral
buffered formalin and paraffin embedded for histological analysis.
Sections were incubated with F4/80 rat anti-mouse antigen (1:10 in
normal rabbit serum overnight, Serotec), biotinylated with rabbit
anti-rat IgG, incubated with avidin-biotin complex (mouse avidin
biotin Vectastain, Vector), and visualized with diaminobenzidine
substrate (Vector) to detect the presence of monocytes/macrophage.
Slides were counterstained with Harris hematoxylin. At least 10
randomly selected fields were analyzed per slide from each animal,
and data are presented as a percentage (total number of macrophage/
total number of adipose cells counted). Frozen liver sections from 6
Figure 2. Body weight in control and SLE mice at 8, 20, and 36
weeks of age. *8-week control mice, #greater than all groups
except 36-week SLE, greater than all groups (P0.01, 1-way
ANOVA). Control body weight was not different from 20 to 36
weeks of age.
990
Hypertension
November 2006
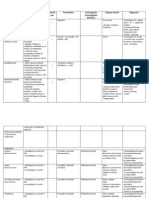
Body Weight, Food Intake, Activity, and Adipose Weight
Age,
wk
Strain
Weight, g
Food Intake,
g per 24 h
Activity, Counts
per min
Visceral
Fat, g
Uterine/Ovarian
Fat, g
RP
Fat, g
Brown
Fat, g
NZW/LacJ
24.10.4
3.90.1
10.01.5
0.90.1
0.60.1
0.110.01
0.110.01
n33
n5
n5
n10
n4
n4
n4
27.10.5
3.90.1
7.50.9
1.30.1
1.00.1
0.170.01
0.130.01
n34*
n5
n4
n12
n5
n5
n5
32.30.3
3.10.2
6.90.6
1.90.2
1.20.1
0.210.02
0.280.03
n55
n5
n5
n15
n4
n4
n4
39.30.8
3.00.2
5.70.5
3.30.2
3.80.3
0.480.06
0.270.04
n48*
n5
n13*
n5*
n5*
n5
34.10.4
3.20.1
8.50.7
2.30.2
2.60.2
0.470.08
0.170.02
n79
n5
n7
n31
n4
n4
n4
45.70.6
3.30.2
5.50.7
5.00.3
5.70.6
0.870.08
0.320.09
n97*
n5
n8*
n46*
n5*
n5*
n5
NZBWF1
20
NZW/LacJ
NZBWF1
36
NZW/LacJ
NZBWF1
n5
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
RP indicates retroperitoneal.
*P0.05, 1-way ANOVA, vs age-matched NZW/LacJ.
SLE; however, reproductive and retroperitoneal adipose depots were significantly greater beginning at 20 weeks of age
in SLE compared with controls (Table).
Food intake was not different between control and SLE
mice at any age tested (Table). Data using radiotelemeters
indicate that locomotor activity (during the night cycle)
tended to be lower in SLE mice at 8 (P0.14) and 20
(P0.11) weeks of age. At 36 weeks, the age with the
greatest disparity in weight and adipose, activity is significantly lower in SLE mice (P0.02). Activity data in the
Table represent the average nighttime activity over the course
of the 4 days. Because the greatest differences in activity,
body, and adipose weight were observed at 36 weeks, the
remaining experiments were performed at this age.
Given the increased central adiposity, it was not surprising
to find that plasma leptin levels in 36-week-old mice were
significantly elevated compared with controls (Figure 3a).
The elevated leptin and similar food intake led to the con-
sideration of leptin resistance, at least centrally. To assess
this, the effect of intraperitoneal leptin administration on food
intake was tested in 36-week-old mice (Figure 3b). Leptin
significantly reduced food intake to the same degree in both
control and SLE mice, suggesting that the SLE mice are not
resistant to its appetite-suppressing effects. In addition, the
reduction in body weight caused by leptin injection was not
different between control and SLE mice (2.60.2 g versus
3.00.4 g; n5; P0.33 Student t test). Injection of
vehicle (saline) did not affect food intake in either strain (data
not shown).
The ovarian/uterine adipose tissue depot isolated from
36-week-old SLE mice had significant macrophage infiltration, an indication of inflammation, when compared with
control mice (Figure 4). Similarly, sections of renal cortex
from SLE mice exhibited macrophage infiltration, whereas
those from control mice did not (Figure 5). Macrophage
infiltration was not notable in the medulla (data not shown).
Figure 3. Plasma leptin levels are increased
in 36-week SLE mice compared with controls. (A) P0.001 compared with control
(Student t test). Twice daily intraperitoneal
injections of 30 g of leptin in saline lead to
a similar reduction in food intake in both
control and SLE mice. (B) P0.05 compared
with basal food intake (1-way ANOVA).
Ryan et al
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
Figure 4. Visceral adipose tissue from 36-week-old SLE mice
(B) had macrophage infiltration, whereas control adipose tissue
did not (A). Percentage of macrophage (per total number of
cells) was significantly increased in SLE mice compared with
controls (C). P0.03.
Frozen liver sections from SLE mice exhibited marked lipid
accumulation in 5 of 6 mice studied compared with 0 of 6
controls (Figure 6).
Although fasted blood glucose levels were not different
(Figure 7a), fasted insulin levels were significantly increased
in SLE mice when compared with controls (Figure 7b).
Moreover, when isosmotic glucose was administered after a
6-hour fast, SLE mice demonstrated a greater increase in
blood glucose that took longer to return to basal levels
(Figure 7c). These data indicate that the SLE mice are insulin
resistant.
Discussion
The major new finding of this study is that an established
model of SLE with hypertension has several characteristics of
the metabolic syndrome. Therefore, the NZBWF1 strain may
prove to be an important model for examining the connection
between chronic inflammation and the metabolic syndrome.
Specific findings include the following: (1) a hypertensive
mouse model of SLE has increased body weight and central
adiposity; (2) adipose tissue from SLE mice has monocyte/
macrophage infiltrates as a marker of inflammation; (3)
reduced physical activity may contribute to the increased
body weight and adipose, but increased food intake does not;
(4) SLE mice do not seem to be resistant to the satiating
Insulin Resistance, Obesity, and SLE
991
effects of leptin; and (5) the NZBWF1 model of SLE is insulin
resistant.
Several risk factors comprise metabolic syndrome, including central obesity, insulin resistance, endothelial dysfunction, hypertension, inflammation, and dyslipidemia. The
present data demonstrate that this model of SLE exhibits
many of these features. For example, numerous other studies
have reported an important role for inflammatory cytokines in
the progression of SLE in NZBWF1 mice.1315 Recent evidence from our laboratory demonstrated that NZBWF1 mice
are hypertensive, have impaired endothelial dependent relaxation, and have albuminuria by 36 weeks of age.7 The
pressure data from the present study measured by indwelling
carotid catheters are consistent with the recently reported
telemetry pressures. Although it is not yet clear, the impaired
endothelial function7 and elevated circulating leptin may be
potential contributors to elevated blood pressure in this
model. Although they were not measured in the present
experiments, data from the literature indicate that these mice
have dyslipoproteinemia.16 The NZBWF1 strain has been
widely used to examine the progression of SLE. These mice
closely mimic human SLE, including the presence of antinuclear antibodies, glomerulonephritis, inflammatory cytokines,
and a female predilection.13,15,17,18, Despite 4 decades of
experimentation, this is the first study to report characteristics of the metabolic syndrome in this model. One potential
limitation of this model is that the obesity and insulin
resistance may be comorbid with SLE. Further examination
will be required to establish a link between chronic inflammation in this model and the metabolic syndrome.
The relationship between SLE and changes in glucose
handling or body composition has not been widely studied. In
rare clinical cases, patients with SLE develop antibodies to
the insulin receptor, which cause insulin resistance (type B
insulin resistance).19 Independent of these case studies, currently available data suggest that humans with SLE are at an
increased risk to develop insulin resistance and obesity. For
example, it has been reported that individuals with SLE
have significantly increased body mass index at a 10-year
follow-up compared with healthy controls.20 In addition,
women with SLE have an increased likelihood of developing
insulin resistance5 and changes in body fat distribution and
composition.6,20 The reason for increased body weight and
adiposity in the NZBWF1 model is not yet clear; however,
one possible mechanism seems to be a reduced physical
activity level.
Figure 5. The renal cortex from
36-week-old SLE mice (B) exhibit macrophage infiltration, whereas the renal cortex from control mice did not.
992
Hypertension
November 2006
Figure 6. Liver sections from 3 control (A
to C) and 3 SLE mice (D and E) stained
with Oil-Red-O show increased hepatic
lipid accumulation (red droplets) in SLE
mice.
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
This new model of metabolic syndrome is potentially interesting, because previous genetic models typically have
alterations in the leptin gene, its receptor, or its signaling
pathways in the brain.2124 The NZBWF1 model of SLE is
unique in that the cause of the metabolic syndrome is not
clear. Although the present data suggest that the satiety actions of leptin in the brain are not different between control
and SLE, the data do not rule out the possibility of selective
leptin resistance.25 In addition, it is equally plausible that the
increased leptin may provide some benefit by maintaining
normal blood glucose26,27 and preventing even greater lipid
accumulation in nonadipose tissues.25 The findings of hepatic
lipid accumulation are consistent with what has been observed in human metabolic syndrome.
The role of leptin and its contributions to obesity in rodent
models has been studied extensively. Interestingly, leptin is
important for promoting immune system function. Leptin
(ob/ob) or leptin receptor (db/db) knockout mice are protected against the development of autoimmune diseases,
including arthritis, inflammatory bowel disease, and multiple
sclerosis.28 30 There is also compelling evidence in humans
that leptin may be important for the pathogenesis of autoimmune disease. For example, after a 7-day fasting period, 10
individuals with rheumatoid arthritis showed significant clinical improvement.31 Another study demonstrated that women
with SLE have significantly elevated plasma leptin when
compared with age-, sex-, and body mass indexmatched
controls.32 Therefore, it is possible that the elevated leptin in
NZBWF1 may be a contributing factor to the chronic inflam-
mation and progression of SLE in this model. Future studies
will be required to determine the role of leptin in promoting
autoimmunity and SLE hypertension.
Perspectives
Chronic inflammation is increasingly considered as a potential underlying mechanism for the progression of hypertension, insulin resistance, and the metabolic syndrome. SLE is
a chronic autoimmune inflammatory disorder with a high
incidence of hypertension. Evidence suggests that the incidence of insulin resistance, obesity, and lipodystrophy is
higher in individuals with SLE; however, the mechanisms for
this have not been investigated. The present study shows for
the first time that a widely used mouse model of SLE has
characteristics of the metabolic syndrome, including central
adiposity, fatty liver, elevated leptin, and insulin resistance.
Therefore, NZBWF1 may be an important model to examine
the relationship between chronic inflammation during SLE
and how this leads to insulin resistance and altered body
composition.
Acknowledgments
We acknowledge the University of Mississippi Medical Center
Department of Physiology Histology Core (Lisa Henegar and
Stephanie Evans) for assistance with adipose tissue and liver
histology.
Sources of Funding
This work was supported by an American Heart Association Scientist Development Grant to M.J.R (0630089N), as well as the National
Institutes of Health (PO1HL-51971).
Figure 7. Fasted blood glucose was not
different between 36-week-old control
and SLE mice (A). Fasted plasma insulin
was significantly increased in 36-week
SLE mice vs controls (B). P0.05. A glucose tolerance test showed that fasted
glucose was significantly greater in
36-week SLE mice after an intraperitoneal injection of isosmotic glucose and
took longer to return to basal levels (C).
P0.05 vs time-matched control (1-way
ANOVA).
Ryan et al
Disclosures
None.
References
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
1. Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R. Metabolic
syndrome: a comprehensive perspective based on interactions between
obesity, diabetes, and inflammation. Circulation. 2005;111:1448 1454.
2. Fernandez-Real JM, Ricart W. Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev. 2003;24:278 301.
3. Lebovitz HE. The relationship of obesity to the metabolic syndrome. Int
J Clin Pract Suppl. 2003;18 27.
4. Wisse BE. The inflammatory syndrome: the role of adipose tissue cytokines in metabolic disorders linked to obesity. J Am Soc Nephrol. 2004;
15:27922800.
5. Tso TK, Huang HY, Chang CK, Liao YJ, Huang WN. Clinical evaluation
of insulin resistance and beta-cell function by the homeostasis model
assessment in patients with systemic lupus erythematosus. Clin
Rheumatol. 2004;23:416 420.
6. Kipen Y, Strauss BJ, Morand EF. Body composition in systemic lupus
erythematosus. Br J Rheumatol. 1998;37:514 519.
7. Ryan MJ, McLemore GR Jr. Hypertension and impaired vascular
function in a female mouse model of systemic lupus erythematosus. Am J
Physiol Regul Integr Comp Physiol. epub (August 3, 2006). doi: 10.1152/
ajpregu.00168.2006
8. Didion SP, Ryan MJ, Didion LA, Fegan PE, Sigmund CD, Faraci FM.
Increased superoxide and vascular dysfunction in CuZnSOD-deficient
mice. Circ Res. 2002;91:938 944.
9. Ryan MJ, Didion SP, Davis DR, Faraci FM, Sigmund CD. Endothelial
dysfunction and blood pressure variability in selected inbred mouse
strains. Arterioscler Thromb Vasc Biol. 2002;22:42 48.
10. Ryan MJ, Jernigan NL, Drummond HA, McLemore GR Jr, Rimoldi JM,
Poreddy SR, Gadepalli RS, Stec DE. Renal vascular responses to
CORM-A1 in the mouse. Pharmacol Res. 2006;54:24 29.
11. Edvell A, Lindstrom P. Vagotomy in young obese hyperglycemic mice:
effects on syndrome development and islet proliferation. Am J Physiol.
1998;274:E1034 E1039.
12. Ryan MJ, Didion SP, Mathur S, Faraci FM, Sigmund CD. PPAR(gamma)
agonist rosiglitazone improves vascular function and lowers blood
pressure in hypertensive transgenic mice. Hypertension. 2004;43:661
666.
13. Brennan DC, Yui MA, Wuthrich RP, Kelley VE. Tumor necrosis factor
and IL-1 in New Zealand Black/White mice. Enhanced gene expression
and acceleration of renal injury. J Immunol. 1989;143:3470 3475.
14. Finck BK, Chan B, Wofsy D. Interleukin 6 promotes murine lupus in
NZB/NZW F1 mice. J Clin Invest. 1994;94:585591.
15. Ryffel B, Car BD, Gunn H, Roman D, Hiestand P, Mihatsch MJ. Interleukin-6 exacerbates glomerulonephritis in (NZB NZW)F1 mice. Am J
Pathol. 1994;144:927937.
16. Jacobson MS, Trachtman H, Feldman J, Samuel P, Ilowite NT. Dyslipoproteinemia in murine systemic lupus erythematosus. Atherosclerosis.
1989;79:205211.
Insulin Resistance, Obesity, and SLE
993
17. Burnett R, Ravel G, Descotes J. Clinical and histopathological progression of lesions in lupus-prone (NZB NZW) F1 mice. Exp Toxicol
Pathol. 2004;56:37 44.
18. Kiberd BA. Murine lupus nephritis. A structure-function study. Lab Invest.
1991;65:5160.
19. Gehi A, Webb A, Nolte M, Davis J Jr. Treatment of systemic lupus
erythematosus-associated type B insulin resistance syndrome with cyclophosphamide and mycophenolate mofetil. Arthritis Rheum. 2003;48:
10671070.
20. Kipen Y, Briganti EM, Strauss BJ, Littlejohn GO, Morand EF. Three year
follow-up of body composition changes in pre-menopausal women with
systemic lupus erythematosus. Rheumatology (Oxford). 1999;38:59 65.
21. Chlouverakis C, White PA. Obesity and insulin resistance in the obesehyperglycemic mouse (obob). Metabolism. 1969;18:998 1006.
22. Huszar D, Lynch CA, Fairchild-Huntress V, Dunmore JH, Fang Q,
Berkemeier LR, Gu W, Kesterson RA, Boston BA, Cone RD, Smith FJ,
Campfield LA, Burn P, Lee F. Targeted disruption of the melanocortin-4
receptor results in obesity in mice. Cell. 1997;88:131141.
23. Lee GH, Proenca R, Montez JM, Carroll KM, Darvishzadeh JG, Lee JI,
Friedman JM. Abnormal splicing of the leptin receptor in diabetic mice.
Nature. 1996;379:632 635.
24. Bowles L, Kopelman P. Leptin: of mice and men? J Clin Pathol. 2001;
54:13.
25. Mark AL, Correia ML, Rahmouni K, Haynes WG. Loss of leptin actions
in obesity: two concepts with cardiovascular implications. Clin Exp
Hypertens. 2004;26:629 636.
26. Toyoshima Y, Gavrilova O, Yakar S, Jou W, Pack S, Asghar Z, Wheeler
MB, LeRoith D. Leptin improves insulin resistance and hyperglycemia in
a mouse model of type 2 diabetes. Endocrinology. 2005;146:4024 4035.
27. Da Silva AA, Tallam LS, Liu J, Hall JE. Chronic antidiabetic and
cardiovascular actions of leptin: role of CNS and increased adrenergic
activity. Am J Physiol Regul Integr Comp Physiol. epub (June 15, 2006).
doi: 10.1152/ajpregu.00187.2006.
28. Busso N, So A, Chobaz-Peclat V, Morard C, Martinez-Soria E,
Talabot-Ayer D, Gabay C. Leptin signaling deficiency impairs humoral
and cellular immune responses and attenuates experimental arthritis.
J Immunol. 2002;168:875 882.
29. Matarese G, Di GA, Sanna V, Lord GM, Howard JK, Di TA, Bloom SR,
Lechler RI, Zappacosta S, Fontana S. Requirement for leptin in the
induction and progression of autoimmune encephalomyelitis. J Immunol.
2001;166:5909 5916.
30. Peelman F, Waelput W, Iserentant H, Lavens D, Eyckerman S, Zabeau L,
Tavernier J. Leptin: linking adipocyte metabolism with cardiovascular
and autoimmune diseases. Prog Lipid Res. 2004;43:283301.
31. Fraser DA, Thoen J, Reseland JE, Forre O, Kjeldsen-Kragh J. Decreased
CD4 lymphocyte activation and increased interleukin-4 production in
peripheral blood of rheumatoid arthritis patients after acute starvation.
Clin Rheumatol. 1999;18:394 401.
32. Garcia-Gonzalez A, Gonzalez-Lopez L, Valera-Gonzalez IC, CardonaMunoz EG, Salazar-Paramo M, Gonzalez-Ortiz M, Martinez-Abundis E,
Gamez-Nava JI. Serum leptin levels in women with systemic lupus erythematosus. Rheumatol Int. 2002;22:138141.
Insulin Resistance and Obesity in a Mouse Model of Systemic Lupus Erythematosus
Michael J. Ryan, Gerald R. McLemore, Jr and Steven T. Hendrix
Downloaded from http://hyper.ahajournals.org/ by guest on August 16, 2016
Hypertension. 2006;48:988-993; originally published online September 18, 2006;
doi: 10.1161/01.HYP.0000243612.02929.df
Hypertension is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright 2006 American Heart Association, Inc. All rights reserved.
Print ISSN: 0194-911X. Online ISSN: 1524-4563
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://hyper.ahajournals.org/content/48/5/988
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Hypertension can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Hypertension is online at:
http://hyper.ahajournals.org//subscriptions/
You might also like
- Complementary and Alternative Medical Lab Testing Part 18: PsychiatryFrom EverandComplementary and Alternative Medical Lab Testing Part 18: PsychiatryRating: 5 out of 5 stars5/5 (1)
- Jvs 16 113Document8 pagesJvs 16 113Emmanuel Ricardo Marín LópezNo ratings yet
- Grupo 3 Obesity InflammationDocument9 pagesGrupo 3 Obesity InflammationJeisonAlejandroÁlvarezVergaraNo ratings yet
- Consumption of Isoflavone-Rich Soy Protein Does Not Alter Homocysteine or Markers of Inflammation in Postmenopausal WomenDocument7 pagesConsumption of Isoflavone-Rich Soy Protein Does Not Alter Homocysteine or Markers of Inflammation in Postmenopausal WomenmerikasorNo ratings yet
- 1 s2.0 0165380681900717 Main PDFDocument8 pages1 s2.0 0165380681900717 Main PDFJean Pierre Chastre LuzaNo ratings yet
- Insulin Resistance in The Spontaneously Hypertensive Rat: BopyrightDocument3 pagesInsulin Resistance in The Spontaneously Hypertensive Rat: BopyrightDawn KentNo ratings yet
- PHD Thesis: University of Medicine and Pharmacy CraiovaDocument10 pagesPHD Thesis: University of Medicine and Pharmacy CraiovapaulNo ratings yet
- Obesity - 2012 - Sampey - Cafeteria Diet Is A Robust Model of Human Metabolic Syndrome With Liver and Adipose InflammationDocument10 pagesObesity - 2012 - Sampey - Cafeteria Diet Is A Robust Model of Human Metabolic Syndrome With Liver and Adipose InflammationRodrigoNo ratings yet
- 2008_Chamy_Biol Res -sometido-07-11-04P-PDFDocument17 pages2008_Chamy_Biol Res -sometido-07-11-04P-PDFEva Montserrat MadridNo ratings yet
- Primacy of Hepatic Insulin Resistance in The Development of The Metabolic Syndrome Induced by An Isocaloric Moderate-Fat Diet in The DogDocument8 pagesPrimacy of Hepatic Insulin Resistance in The Development of The Metabolic Syndrome Induced by An Isocaloric Moderate-Fat Diet in The DogBlagojeNo ratings yet
- No. 2 Art7Document9 pagesNo. 2 Art7Joko Swasono Adi AdiekNo ratings yet
- 61 10 09 s3 ArticleDocument6 pages61 10 09 s3 ArticlekasabeNo ratings yet
- The EffectDocument6 pagesThe EffectDavid IsuNo ratings yet
- Zini E Et Al., 2010Document8 pagesZini E Et Al., 2010Ojhn SmithNo ratings yet
- Karatsoreos Et Al 2010Document11 pagesKaratsoreos Et Al 2010zacharymweil100% (1)
- Wan Et Al 2019 PDFDocument8 pagesWan Et Al 2019 PDFEdgar Huerta CardenasNo ratings yet
- Mechanisms of Sleep Deprivation-Induced Hepatic Steatosis and Insulin Resistance in MiceDocument11 pagesMechanisms of Sleep Deprivation-Induced Hepatic Steatosis and Insulin Resistance in MiceNazan ElmaNo ratings yet
- Prepuberal Stress and Obesity Effects On Serum Corticosterone Prolactin and Precancerous Prostate Leisons in Adults RatsDocument8 pagesPrepuberal Stress and Obesity Effects On Serum Corticosterone Prolactin and Precancerous Prostate Leisons in Adults RatsAntares Basulto NathNo ratings yet
- Essah 2011Document6 pagesEssah 2011ThormmmNo ratings yet
- (1479683X - European Journal of Endocrinology) Subcutaneous Adipocytes From Obese Hyperinsulinemic Women With Polycystic Ovary Syndrome Exhibit Normal Insulin Sensitivity But ReducedDocument5 pages(1479683X - European Journal of Endocrinology) Subcutaneous Adipocytes From Obese Hyperinsulinemic Women With Polycystic Ovary Syndrome Exhibit Normal Insulin Sensitivity But ReduceddfdfffffNo ratings yet
- 1 Predict NeoDocument5 pages1 Predict NeoGary Carhuamaca LopezNo ratings yet
- Female Rats Are Protected Against Fructose-Induced Changes in Metabolism and Blood PressureDocument7 pagesFemale Rats Are Protected Against Fructose-Induced Changes in Metabolism and Blood PressureMarta SandeNo ratings yet
- HFD MiceDocument5 pagesHFD Micechar462No ratings yet
- Social Isolation Affects The Development of Obesity and Type 2 Diabetes in MiceDocument9 pagesSocial Isolation Affects The Development of Obesity and Type 2 Diabetes in MiceNovita WulandariNo ratings yet
- Evaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)Document6 pagesEvaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)soledadDC329No ratings yet
- Kim 2009Document7 pagesKim 2009edelinNo ratings yet
- Chronic Inflammation in Fat Plays A Crucial Role in The Development of Obesity-Related Insulin ResistanceDocument10 pagesChronic Inflammation in Fat Plays A Crucial Role in The Development of Obesity-Related Insulin ResistanceRachel Lalaine Marie SialanaNo ratings yet
- PCOS and Metabolic SyndromeDocument21 pagesPCOS and Metabolic SyndromeHAVIZ YUADNo ratings yet
- To Fat Mass and Tumor Necrosis Factor - (Alpha) System Plasma Interleukin-8 Concentrations Are Increased in Obese Subjects and RelatedDocument6 pagesTo Fat Mass and Tumor Necrosis Factor - (Alpha) System Plasma Interleukin-8 Concentrations Are Increased in Obese Subjects and RelatedadnanakilNo ratings yet
- Serum Vaspin Concentrations in Human Obesity and Type 2 DiabetesDocument6 pagesSerum Vaspin Concentrations in Human Obesity and Type 2 DiabetesDianPertiwiSNo ratings yet
- (Doi 10.1089/neu.2014.3497) A. D. Sauerbeck J. L. Laws V. v. Bandaru P. G. Popovich N. J - Spinal Cord Injury Causes Chronic Liver Pathology in RatsDocument11 pages(Doi 10.1089/neu.2014.3497) A. D. Sauerbeck J. L. Laws V. v. Bandaru P. G. Popovich N. J - Spinal Cord Injury Causes Chronic Liver Pathology in RatsDitaIsnainiNo ratings yet
- DM Tipe 1Document6 pagesDM Tipe 1Mutiara Kristiani PutriNo ratings yet
- Plasma Leptin Levels in Rats With PancreatitisDocument6 pagesPlasma Leptin Levels in Rats With PancreatitisAndykaYayanSetiawanNo ratings yet
- Schreyer 1998Document8 pagesSchreyer 1998Jocilene Dantas Torres NascimentoNo ratings yet
- MD 1 Section E2 Group 3 Biochem REVISEDDocument10 pagesMD 1 Section E2 Group 3 Biochem REVISEDParadoxistNo ratings yet
- The Effect of Aloin in Blood Glucose and Antioxidants in Male Albino Rats With Streptozotocin-Induced DiabeticDocument18 pagesThe Effect of Aloin in Blood Glucose and Antioxidants in Male Albino Rats With Streptozotocin-Induced DiabeticJunaid MinhasNo ratings yet
- Research Article: Improving The Reliability and Utility of Streptozotocin-Induced Rat Diabetic ModelDocument15 pagesResearch Article: Improving The Reliability and Utility of Streptozotocin-Induced Rat Diabetic ModelSipend AnatomiNo ratings yet
- Original Article Evidence of Anti-Obesity Effects of The Pomegranate Leaf Extract in High-Fat Diet Induced Obese MiceDocument7 pagesOriginal Article Evidence of Anti-Obesity Effects of The Pomegranate Leaf Extract in High-Fat Diet Induced Obese MiceAisy Savira anizarNo ratings yet
- Stress Oxy 5 DatifDocument19 pagesStress Oxy 5 DatifImene KadiNo ratings yet
- Infertility and Eating Disorders YmobDocument1 pageInfertility and Eating Disorders Ymobps.paulayanezNo ratings yet
- Obesity Is Associated With Macrophage Accumulation in Adipose TissueDocument13 pagesObesity Is Associated With Macrophage Accumulation in Adipose TissueRachel Lalaine Marie SialanaNo ratings yet
- 2016 Adipose Tissue Hyperplasia With Enhanced Adipocyte-Derived Stem Cell Activity in Tc1 (C8orf4) - Deleted MiceDocument10 pages2016 Adipose Tissue Hyperplasia With Enhanced Adipocyte-Derived Stem Cell Activity in Tc1 (C8orf4) - Deleted MiceFrancisco Antonó Castro WeithNo ratings yet
- Clinical Case Study: Questions To ConsiderDocument3 pagesClinical Case Study: Questions To Considerالشهيد محمدNo ratings yet
- AerobicDocument7 pagesAerobicMayra PereiraNo ratings yet
- 133 Full-2Document10 pages133 Full-2Emilian EmNo ratings yet
- Sex-Dependent Metabolic, Neuroendocrine, and Cognitive Responses To Dietary Energy Restriction and ExcessDocument16 pagesSex-Dependent Metabolic, Neuroendocrine, and Cognitive Responses To Dietary Energy Restriction and ExcessBillard StéphaneNo ratings yet
- 2006_Publicación final BRDocument8 pages2006_Publicación final BREva Montserrat MadridNo ratings yet
- Effect of Chickpea On GlucoseDocument7 pagesEffect of Chickpea On GlucoseMia DragostinNo ratings yet
- Effect of Intermittent Fasting On Brain Neurotransmitters, Neutrophils Phagocytic Activity, and Histopathological Finding in Some Organs in RatsDocument8 pagesEffect of Intermittent Fasting On Brain Neurotransmitters, Neutrophils Phagocytic Activity, and Histopathological Finding in Some Organs in RatsBrian ColborneNo ratings yet
- Lipasa Pancreatica LeidoDocument6 pagesLipasa Pancreatica LeidoJessica MerloNo ratings yet
- Fatty pancreas disease linked to obesityDocument7 pagesFatty pancreas disease linked to obesitykurnia fitriNo ratings yet
- Onion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsDocument8 pagesOnion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsRizky Agustian HadiNo ratings yet
- 8 HalamansdbDocument14 pages8 HalamansdbbanglarkNo ratings yet
- 2-Heremans-Schmid Glycoprotein: Fetuin-A Is Associated With Insulin Resistance and Fat Accumulation in The Liver in HumansDocument5 pages2-Heremans-Schmid Glycoprotein: Fetuin-A Is Associated With Insulin Resistance and Fat Accumulation in The Liver in HumansOcto IndradjajaNo ratings yet
- A Suprachiasmatic Nucleus Generated Rhythm in Basal GlucoseDocument11 pagesA Suprachiasmatic Nucleus Generated Rhythm in Basal GlucoseD Gonzalez GarciaNo ratings yet
- Diabetesmellitusinelkhoundsisassociatedwith DiestrusandpregnancyDocument7 pagesDiabetesmellitusinelkhoundsisassociatedwith DiestrusandpregnancyBea GonzalvoNo ratings yet
- Reduced Total Antioxidant Status in Postterm Pregnancies: Kaya S, Keskin HL, Kaya B, Ustuner I, Avsar AFDocument5 pagesReduced Total Antioxidant Status in Postterm Pregnancies: Kaya S, Keskin HL, Kaya B, Ustuner I, Avsar AFMaulidianaIndahNo ratings yet
- 10253890.2021(1)Document12 pages10253890.2021(1)diego.battiatoNo ratings yet
- Effect and Interactions of Pueraria-Rehmannia and Aerobic Exercise On MetabolicDocument9 pagesEffect and Interactions of Pueraria-Rehmannia and Aerobic Exercise On Metabolicyhenti widjayantiNo ratings yet
- Plasma Carboxy-Terminal Provasopressin (Copeptin) : A Novel Marker of Insulin Resistance and Metabolic SyndromeDocument7 pagesPlasma Carboxy-Terminal Provasopressin (Copeptin) : A Novel Marker of Insulin Resistance and Metabolic SyndromeFrisilia LeauaNo ratings yet
- Frequency of Fractures in Women With SysDocument9 pagesFrequency of Fractures in Women With Syslm_catalinaNo ratings yet
- Toxicologie Clinica Curs NR 3Document11 pagesToxicologie Clinica Curs NR 3lm_catalinaNo ratings yet
- Aquaporins at A GlanceDocument6 pagesAquaporins at A GlanceManu ElNo ratings yet
- Farma ClinicaDocument10 pagesFarma ClinicappvasileppNo ratings yet
- Aquaporins at A GlanceDocument6 pagesAquaporins at A GlanceManu ElNo ratings yet
- Scurta Clasificare ParazitiDocument8 pagesScurta Clasificare ParazitiIulia-Alexandra BenciuNo ratings yet
- Usmle Free 150Document44 pagesUsmle Free 150ironslave100% (1)
- Usmle Free 150Document44 pagesUsmle Free 150ironslave100% (1)
- Curs Engleza 10Document4 pagesCurs Engleza 10lm_catalinaNo ratings yet
- Aquaporins at A GlanceDocument6 pagesAquaporins at A GlanceManu ElNo ratings yet
- Does Altered Glucocorticoid HomeostasisDocument10 pagesDoes Altered Glucocorticoid HomeostasisandreNo ratings yet
- Ketogenic Diet IF-Philippine Lipid Society Consensus-Statement-20191108v4Document21 pagesKetogenic Diet IF-Philippine Lipid Society Consensus-Statement-20191108v4donmd98No ratings yet
- Daftar PustakaDocument5 pagesDaftar PustakaRusman Efendi100% (3)
- Diabetes Mellitus Surgical PatientDocument33 pagesDiabetes Mellitus Surgical PatientGerald AndersonNo ratings yet
- No Nonsense DoctorDocument2 pagesNo Nonsense DoctorDesikan NarayananNo ratings yet
- (2019) Metabolic Support Challenges With Obesity During Critical IllnessDocument8 pages(2019) Metabolic Support Challenges With Obesity During Critical IllnessAnna Maria Ariesta PutriNo ratings yet
- Teza de Doctorat - DR - Goel-SemnatDocument150 pagesTeza de Doctorat - DR - Goel-Semnatpopescu ancaNo ratings yet
- Impact of Coffee on Singapore Youth Health and LifestyleDocument8 pagesImpact of Coffee on Singapore Youth Health and LifestyleMun Yen LoiNo ratings yet
- Pomegranate Health BenefitsDocument27 pagesPomegranate Health BenefitscommuniversityNo ratings yet
- Osmun Case StudyDocument48 pagesOsmun Case StudyraffineeNo ratings yet
- Basics in Clinical Nutrition: Carbohydrate Metabolism: Luc TappyDocument4 pagesBasics in Clinical Nutrition: Carbohydrate Metabolism: Luc Tappymarliana100% (1)
- Diabetes Mellitus: (DM)Document84 pagesDiabetes Mellitus: (DM)Andika HNo ratings yet
- Beta BlockersDocument6 pagesBeta BlockersGopinath AgnihotramNo ratings yet
- Insulin ResistanceDocument12 pagesInsulin ResistancePrabhmeet GroverNo ratings yet
- Dept. of Medical and Clinical Biochemistry Upjš in Košice, Medical Faculty Eva Ďurovcová, Md. Phd. 5 GM CLBDocument48 pagesDept. of Medical and Clinical Biochemistry Upjš in Košice, Medical Faculty Eva Ďurovcová, Md. Phd. 5 GM CLBPaulina PaskeviciuteNo ratings yet
- Diabetes and Raising Awareness PowerpointDocument10 pagesDiabetes and Raising Awareness Powerpointapi-305921825No ratings yet
- Role of Heme Oxygenase in Inflammation, Insulin-SignallingDocument18 pagesRole of Heme Oxygenase in Inflammation, Insulin-SignallingAndri Praja SatriaNo ratings yet
- Etiology of HypertensionDocument7 pagesEtiology of HypertensionAdelia Maharani DNo ratings yet
- Diabetes MallitusDocument33 pagesDiabetes Mallitushammu hothi100% (2)
- Relationship Between Adiponectin, Obesity and Insulin ResistanceDocument9 pagesRelationship Between Adiponectin, Obesity and Insulin ResistanceSanthiya KunasegaranNo ratings yet
- Zaharia 2019Document11 pagesZaharia 2019Prashant BasukalaNo ratings yet
- Pathophysiology: Predisposing Factors: Precipitating FactorsDocument2 pagesPathophysiology: Predisposing Factors: Precipitating FactorsJemsMei Comparativo MensuradoNo ratings yet
- DIABETESDocument33 pagesDIABETESJamie IllmaticNo ratings yet
- Bio 12th ThesisDocument20 pagesBio 12th ThesisValli RamalingamNo ratings yet
- Swift 2018Document33 pagesSwift 2018Sam Steven Hernandez JañaNo ratings yet
- The Effects of Ginkgo Biloba On Metabolic SyndromeDocument14 pagesThe Effects of Ginkgo Biloba On Metabolic SyndromeVertigarden LondrinaNo ratings yet
- Diabetes Pregestacional ACOGDocument21 pagesDiabetes Pregestacional ACOGarturoNo ratings yet
- Non-Alcoholic Fatty Liver DiseaseDocument35 pagesNon-Alcoholic Fatty Liver Diseaserigueiram100% (1)
- DiabetesDocument352 pagesDiabetesbeltonNo ratings yet
- The Use of Zebrafish (Danio Rerio) As Biomedical Models: Feature ArticleDocument10 pagesThe Use of Zebrafish (Danio Rerio) As Biomedical Models: Feature ArticleJuniClaudia13No ratings yet