Professional Documents
Culture Documents
The Hip Joint Arthroscopic Procedures An
The Hip Joint Arthroscopic Procedures An
Uploaded by
wladjaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Hip Joint Arthroscopic Procedures An
The Hip Joint Arthroscopic Procedures An
Uploaded by
wladjaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/6906157
The Hip Joint: Arthroscopic Procedures and Postoperative Rehabilitation
Article in Journal of Orthopaedic and Sports Physical Therapy · August 2006
DOI: 10.2519/jospt.2006.2138 · Source: PubMed
CITATIONS READS
66 100
6 authors, including:
Keelan R Enseki Bryan T. Kelly
UPMC Hospital for Special Surgery
26 PUBLICATIONS 379 CITATIONS 221 PUBLICATIONS 7,665 CITATIONS
SEE PROFILE SEE PROFILE
Marc J Philippon Mara L Schenker
Steadman Philippon Research Institute Emory University
312 PUBLICATIONS 8,619 CITATIONS 32 PUBLICATIONS 2,507 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Gluteus Medius Tears View project
CSM 2016 View project
All content following this page was uploaded by Keelan R Enseki on 29 May 2014.
The user has requested enhancement of the downloaded file.
Journal of Orthopaedic & Sports Physical Therapy
Official Publication of the Orthopaedic and Sports Physical Therapy Sections of the American Physical Therapy Association
Supplemental Video Available at www.jospt.org
The Hip Joint: Arthroscopic Procedures
and Postoperative Rehabilitation
Keelan R. Enseki, PT, MS, ATC, SCS, CSCS 1
RobRoy L. Martin, PT, PhD, CSCS 2
Peter Draovitch, PT, MS, ATC 3
Bryan T. Kelly, MD 4
Marc J. Philippon, MD 5
Mara L. Schenker, BS 6
Recent technological improvements have resulted in a greater number of surgical options available Correction of other abnormalities
for individuals with hip joint pathology. These options are particularly pertinent to the relatively of the joint associated with, or
younger and more active population. The diagnosis and treatment of acetabular labral tears have contributing to, the underlying
become topics of particular interest. Improvements in diagnostic capability and surgical technol- cause of a labral tear, including
ogy have resulted in an increased number of arthroscopic procedures being performed to address
capsular laxity, femoral-acetabular
acetabular labral tears and associated pathology. Associated conditions include capsular laxity,
femoral-acetabular impingement, and chondral lesions. Arthroscopic techniques include labral tear
impingement (FAI), and chondral
resection, labral repair, capsular modification, osteoplasty, and microfracture procedures. Postop- lesions, through recent advances
erative rehabilitation following arthroscopic procedures of the hip joint carries particular concerns can now also be performed
regarding range of motion, weight-bearing precautions, and initiation of strength activities. through arthroscopic procedures.
Postoperative rehabilitation protocols that have been typically used for surgeries such as total hip Arthroscopic procedures have
arthroplasty are often not sufficient for the population of patients undergoing arthroscopic evolved in the last decade to ad-
procedures of the hip joint. Postoperative rehabilitation should be based upon the principles of dress labral tears and associated
tissue healing as well as individual patient characteristics. As arthroscopic procedures to address pathologies and are typically per-
acetabular labral tears and associated pathology evolve, physical therapists have the opportunity
formed on young, active individu-
to play a significant role through the development of corresponding rehabilitation protocols.
J Orthop Sports Phys Ther 2006;36(7):516-525. doi:10.2519/jospt.2006.2138
als. As a result, traditional hip
rehabilitation protocols have been
Key Words: clinical research, hip, labrum, lower extremity adapted to meet the demands of
this patient population. Rehabilita-
tion for individuals having a total
T
he advancement of diagnostic procedures along with the
development of improved arthroscopic instrumentation and hip arthroplasty (THA) or surgical
techniques has broadened the range of treatment options procedures to address fractures
for individuals with hip joint pathology. Recently, the have typically focused on gait
surgical treatment of acetabular labral tears has been of training, weight-bearing status,
particular interest. Treatment options have evolved from simple resec- range of motion (ROM) precau-
tion of the torn tissue to more advanced labral repair procedures. tions, and activity modification,
with a goal of returning to specific
1
activities of daily living, but most
Orthopaedic Physical Therapy Residency Program Director, Centers for Rehab Services, University of
Pittsburgh Center for Sports Medicine, Department of Physical Therapy, University of Pittsburgh School of often not strenuous labor or com-
Health and Rehabilitation Sciences, Pittsburgh, PA. petitive sport.9,22,59 The active
2
Assistant Professor, Department of Physical Therapy, Duquesne University, Pittsburgh, PA. population of patients undergoing
3
Physical Therapist, Centers for Rehab Services, University of Pittsburgh Center for Sports Medicine,
Pittsburgh, PA. hip arthroscopy raise additional
4
Assistant Professor of Orthopaedic Surgery, Hospital for Special Surgery, New York-Presbyterian concerns regarding increased joint
Hospital, Weill Medical College of Cornell University, New York, NY. load demands, proprioception,
5
Orthopaedic Surgeon, Steadman-Hawkins Clinic, Steadman-Hawkins Research Foundation, Vail, CO.
6
Research Assistant, Steadman-Hawkins Research Foundation, Vail, CO. muscle imbalances, lumbopelvic
There is no financial affiliation or involvement of any commercial organization that has a direct financial stability, strenuous occupation de-
interest in any matter included in this manuscript. mands, and possibly return to
Address correspondence to Keelan R. Enseki, Centers for Rehab Services, UPMC Sports Medicine
Complex, 3200 South Water Street, Pittsburgh, PA 15203. E-mail: ensekikr@upmc.edu competition. As surgeries to cor-
516 Journal of Orthopaedic & Sports Physical Therapy
rect disorders of the acetabular labrum and associ- tion force is applied under fluoroscopic evaluation,
ated pathology are performed more often, along with gentle traction to the contralateral limb to
CLINICAL COMMENTARY
postoperative protocols must reflect the evolution of provide a counterforce. Typically 11.3 to 22.6 kg of
these procedures and the demands of the patient force is required to create the minimum 8 to 10 mm
population. of hip joint distraction necessary to perform
arthroscopy and reduce the risk of iatrogenic
Indications chondral or labral injury. Flexible instrumentation
now allows access to the deeply recessed joint struc-
Potential candidates for arthroscopic procedures to tures for arthroscopic intervention. Though numer-
address acetabular labral tears and associated pathol- ous variations have been described, 3 basic portals
ogy should be identified through clinical and diag- are most commonly utilized: anterolateral, anterior,
nostic testing. Initially, an attempt should be made to and posterolateral.
determine if the cause of symptoms is extra-articular, Systematic arthroscopic examination of the hip can
intra-articular, or from a structure other than the hip be performed through 2 portals: anterolateral and
joint (referred pain). The examination includes the anterior.28 The anterolateral portal is placed approxi-
assessment of ROM, strength, and special tests for the mately 1 to 2 cm superior and 1 to 2 cm anterior to
hip joint, as well as lower-quarter–screening compo- the anterosuperior portion of the greater trochanter.
nents to rule out lumbosacral spine or knee joint The anterolateral portal allows examination of nu-
involvement. Identifying a labral tear through clinical merous structures within the joint, including the
examination may be difficult and, therefore, diagnos- anterior and superior labrum, the anterior femoral
tic imaging may be necessary. Imaging modalities are head and neck, the cotyloid fossa, and ligamentum
most effective when their selection is based upon a teres. The psoas tendon, also visible through this
complete history and physical examination.3 Plain- portal, most commonly lies medially to a thin barrier
film radiographs may include supine anterior- of capsular tissue and can be palpated with a probe.
posterior pelvis, frog-lateral, cross-table lateral, In approximately 20% of the population, the psoas
and/or false-profile views. Magnetic resonance imag- tendon and/or bursa may be intra-articular.43
ing (MRI) may be performed to evaluate soft tissue The anterior portal is placed directly inferior to the
injuries, including chondral and labral pathologies.37 anterior superior iliac spine at the horizontal inter-
Gadolinium-enhanced magnetic resonance arthrogra- section of the anterolateral portal. It allows a detailed
phy may also be used to image labral and chondral view of structures, including the anterior acetabular
pathology in the hip. If history, physical examination, rim, posterior labrum, ligamentum teres, and cotyloid
and medical imaging analysis lead to suspicion of a fossa. Placement of this portal requires precise knowl-
labral tear, an attempt should also be made to edge of the anatomy of the region to avoid potential
determine the presence of associated joint laxity, FAI, damage to numerous neurovascular structures, in-
or joint degeneration. cluding the lateral femoral cutaneous nerve, lateral
After clinical and diagnostic evidence is evaluated, femoral circumflex artery, and femoral neurovascular
candidacy for arthroscopic surgery is determined. bundles.12
Individuals who suffer from persistent hip pain that The third portal (posterolateral) can be placed 2
has not responded to conservative intervention pro- to 3 cm posterior to the tip of the greater trochanter
vided for longer than 4 weeks and who show signs of at the same level as the anterolateral portal. The
intra-articular hip pathology are considered to be sciatic nerve needs to be carefully avoided during the
potential candidates for hip arthroscopy. 29 placement of this portal.29 Visualization of the poste-
Contraindications for hip arthroscopy include hip rior aspect of the femoral head, the posterior labrum,
fusion, cellulitis, severe acetabular dysplasia, femoral posterior capsule, and the inferior edge of the
neck stress fracture, stable avascular necrosis, inability ischiofemoral ligament is possible from this portal.12
or unwillingness to comply with rehabilitation proto- The posterolateral portal can also be useful for the
cols, arthrofibrosis, and advanced joint degeneration. removal of loose bodies.
An association between the presence of advanced Other portals may be established as needed for
cartilage degeneration and poor outcomes following visualization and treatment of otherwise inaccessible
hip arthroscopy has been suggested.36 Individuals in regions of the joint.
this category may be better suited for a trial of
conservative treatment, with a focus on manual Labral Resection
therapy.25 If satisfactory results are still not achieved,
the patient may be a candidate for a THA procedure. Recent advances in arthroscopic technology have
resulted in an increased number of treatment options
for individuals with labral pathology of the hip. The
Arthroscopic Examination
choice of surgical technique can vary depending on
Arthroscopy of the hip may be performed with the the type, size, location, and degenerative condition of
patient in the supine or lateral position.7,21 A distrac- the labral tear. As with the debridement of a meniscal
J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006 517
undergoing arthroscopic labral resection had good to
A
excellent results at 1-year follow-up, if they did not
have significant preoperative hip arthritis. Byrd and
Jones8 performed a prospective analysis of patients
undergoing arthroscopic procedures for tears of the
acetabular labrum. They reported a significant im-
provement of symptoms in patients on the MHHS
during a 2-year follow-up after arthroscopic labrum
resection. A number of the studies presented in Table
1 are case series. Therefore, these results should be
considered, while acknowledging that case series have
been noted to overestimate the therapeutic effects of
interventions.53
Labral Repair
The ability to perform labral repairs has recently
B been reported.28,46 Individuals with a labrum that is
partially detached from the bony acetabulum or who
have intrasubstance tears are considered candidates
for repair. A repair is chosen over resection to avoid
significant disruption of joint mechanics.15-16 In the
case of detachment, a bioabsorbable suture anchor is
placed on the rim of the acetabulum. After the
anchor is established, suture material is passed
through the labrum twice to create a vertical mattress
suture. When an intrasubstance split in the labrum is
observed, a bioabsorbable suture is passed around
the split, utilizing a suture lasso or similar instrumen-
tation. Once the suture is tied, the split labral tissue
is reapproximated. Repairs of the acetabular labrum
share common concerns with meniscal repairs for the
knee regarding vascularity and healing potential.
McCarthy et al35 found limited vascularization occur-
ring in the labrum-capsular sulcus and the junction
between the acetabulum and fibrocartilagenous
FIGURE 1. (A) normal acetabular labrum under arthroscopic exami-
nation; (B) frayed acetabular labrum. labrum. Flap or frayed tears, as well as tears with
considerable degeneration, are not considered to be
tear in the knee, it is believed that mechanical repairable. These tears should be debrided, leaving as
symptoms and immediate pain will be relieved by much healthy tissue as possible. Early results for
removing the unstable portion of the labrum. Once a arthroscopic labral repair procedures appear to be
labral tear has been identified, resection of the favorable. Leunig33 reported preliminary data com-
unhealthy labral tissue is performed. An attempt is paring labral resection and repair using an open
made to spare as much stable tissue as possible procedure. They showed significantly better subjective
to preserve the mechanical integrity of the joint outcomes in patients undergoing repair as compared
(Figure 1).15-16 to resection.
A number of studies have reported favorable out-
comes following debridement of a labral tear (Table Osteoplasty and Rim Trimming
1).13,17,24,31,42,47,51 Potter et al47 recently performed a
study examining the association of Short Form-36 FAI has been recognized as a cause of acetabular
and disability status with outcomes of arthroscopic labral tears and chondral injuries that may eventually
acetabular debridement. Twenty-eight months lead to joint degeneration.4,20,39,57 A decreased offset
postsurgery, they found arthroscopic debridement of the femoral head-neck junction secondary to
yielded good or excellent results on the Modified abnormalities of the femoral head (cam impinge-
Harris Hip Score (MHHS) in 68% of patients, with ment) or acetabulum (pincer impingement), or a
84% being very or somewhat satisfied, when patients combination cam and pincer impingement, has been
undergoing military disability evaluations were ex- observed.20,26,41,48 The decreased clearance between
cluded. Farjo et al13 found that 71% of patients the femoral head-neck region and the acetabulum
518 J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006
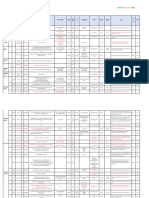
TABLE 1. Reported outcomes and average follow-up after procedures of the hip joint intended to address acetabular labral tears and/or
femoral-acetabular impingement.
CLINICAL COMMENTARY
Average
Study Length of
Study Author(s) Description/Subjects (n) Follow-up Outcomes
5
Beck et al Retrospective case series of pa- 4.0-5.2 y 13 hips rated as good to excel-
tients undergoing open bony lent on the Merle d’Aubigné́
resection to address femoral- and Postel Hip Score; 5 had
acetabular impingement (n = subsequent total hip
19) arthroplasty
Byrd and Jones8 Prospective study of patients 2y Significant symptom improve-
undergoing hip arthroscopy ment on the Modified Harris
(n = 35) Hip Score (MHHS); best results
occurring for labral tears and
removal of loose bodies
Farjo et al13 Retrospective case series of pa- 13-100 mo 71% of patients without
tients who had hip preoperative arthritic findings
arthroscopy performed for had good to excellent results
debridement of a labral tear on a numeric self-report scor-
(n = 28) ing system compared to 21%
for those with arthritis
Hase and Ueo24 Retrospective case report review 15-68 mo 8 patients had arthroscopic re-
of patients diagnosed with section of the torn labrum and
labral tears (n = 10) were symptom free at follow-
up; 2 patients did not recover
with conservative treatment
Murphy et al38 Prospective study of patients 2-12 y 15 hips functioning well on the
undergoing open bony Merle d’Aubigné́ and Postel
debridement as treatment to Hip Score without further inter-
address femoral-acetabular vention; 7 converted to total
impingement (n = 23) hip arthroplasty; no subjects
developed osteonecrosis
Oleary et al42 Retrospective study comparing Average, 30 mo; 91% of patients having
results of arthroscopy of the minimum, 20 mo arthroscopy for labral tears re-
hip for osteonecrosis com- ported significant improvement
pared to other diagnoses (n = through self report, compared
86) (43% osteonecrosis, 20% to 40% for osteonecrosis, and
labral injury, 10% 44% for degenerative joint dis-
osteoarthritis, 10% Legg- ease
Calvé́-Perthes disease, 10%
loose bodies)
Potter et al47 Retrospective case series of pa- 13-55 mo Patient self-reported satisfaction
tients undergoing arthroscopic rates were 70% overall; 50%
acetabular labrum debride- for those undergoing military
ment (n = 40) disability evaluations versus
84% for those who were not
Santori and Villar51 Case series review of patients 24-61 mo Of the 58 cases remaining at
undergoing arthroscopy to ad- follow-up, 67.3% reported be-
dress acetabular labral tears ing pleased with the results of
(n = 76) their operation (mean MHHS,
89.8); 32.7% were not satisfied
(mean MHHS, 49.5)
results in impingement between the bony structures, have advanced degeneration of the joint (Table
particularly in hip positions of flexion and internal 1).4,5,38 It should be noted that the Merle d’Aubigné
rotation. Labral and chondral injuries have been and Postel Hip Score, utilized as outcome measures
shown to be associated with FAI. An open surgical in a number of studies, was originally designed to
dislocation approach to the decompression of FAI has measure pain, mobility, and ambulation characteris-
been described.19,32 The open technique has pro- tics in individuals following THA. Therefore, it may
duced favorable outcomes in individuals who do not overestimate the functional status of individuals who
J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006 519
are typically more active in comparison to this popu-
lation.
Current advances now allow for osteoplasty of cam
impingement and rim trimming of pincer impinge-
ment to be performed through arthroscopy.46,45 This
method avoids surgical dislocation and thus reduces
the risk of developing avascular necrosis, infection, or
nonunion of the greater trochanter. In the
osteoplasty technique, the femoral head-neck offset is
improved by removing any significant nonspherical
portion of the femoral head (Figure 2). The rim-
trimming technique allows resection of the anterior
acetabular overcoverage.5 Resection or repair of the
damaged labrum can be performed during the same
procedure. Outcome studies comparing arthroscopic
osteoplasty to the conventional open dislocation pro-
cedures do not exist at this time. FIGURE 3. Microfracture procedure for chondral lesion of the
acetabulum: a surgical awl is used to create lesions in the
subchondral bone.
Capsular Modification
tensioned at the margin between the iliofemoral and
As with FAI, capsular laxity has been associated
ischiofemoral ligaments. Plication of the iliofemoral
with labral lesions. Injury to the labrum or attenua-
ligament and repair of the labrum to address recur-
tion of the capsuloligamentous structures can result
in a disturbance of the buffer mechanism of hip rent anterior instability of the hip joint can be
stability. This may create a disproportionate load compared to a Bankart procedure performed for
distribution and resulting injury to both structures. shoulder instability and glenoid labrum compromise.
Rotational instability, particularly in the athletic popu- Data on long-term effectiveness of plication proce-
lation, is associated with sports involving axial loading dures for the hip joint are needed.
and external rotation, and is likely related to elonga-
tion of the iliofemoral ligament. Procedures includ-
ing thermal capsulorrhaphy or plication may be
Microfracture Procedures
performed to address capsular laxity.52 In a small
study (n = 11 hips) of professional athletes who McCarthy et al36 observed that 74% of patients
underwent labral resection and capsular thermal with a frayed or torn labrum also had chondral
modification of the hip, 81% returned to preinjury lesions. Arthroscopic observation suggested an asso-
level of competition with minimal or no pain.44 ciation between progression of labral lesions and
Recently, arthroscopic plication of the iliofemoral progression of anterior articular cartilage lesions of
ligament has been performed on patients demon- the acetabulum.34 Though not completely under-
strating significant redundancy and capsular laxity.29 stood, cartilage damage may play a detrimental role
During this procedure, a bioabsorbable suture is in the outcomes of patients undergoing arthroscopic
procedures of the hip joint.36,39 Often found in
conjunction with labral tears, medium-sized, full-
thickness articular lesions of the femoral head and
acetabulum can be addressed through arthroscopic
microfracture procedures.29 Microfractures are cre-
ated in the subchondral bone in an attempt to
facilitate the growth of hyaline-like fibrocartilage
(Figure 3). Though there are no current outcome
studies regarding patients undergoing microfracture
procedures for the hip joint, functional improvement
and decreased pain have been reported with the use
of the microfracture techniques in the knee.56 In the
hip, the microfracture technique is currently recom-
mended for well-contained chondral defects in the
acetabulum and the femoral head up to 400 mm2.
The authors make this recommendation based upon
the reported outcomes following microfracture proce-
FIGURE 2. Postosteoplasty view of the femoral head-neck junction. dures of the knee.56
520 J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006
Complications prescribed nonsteroidal anti-inflammatory drugs
(NSAIDs), ice, and compression. The authors utilize
CLINICAL COMMENTARY
The reported complication rate associated with a motorized cuff system (Cryo/Cuff AutoChill Sys-
arthroscopy of the hip joint ranges from 1.3% to
tem; Aircast, Summit, NJ) to continuously deliver
1.6%.6,11,23 In comparison, complication rates for
compression with water kept cold in a reservoir of
arthroscopic procedures of the knee and shoulder
ice. The progression of weight-bearing, ROM, and
have been reported in the ranges of 1.29% to
strengthening activities is dictated by current knowl-
8.2%54,55 and 5.8% to 9.5%,58 respectively. Potential
complications are most often related to joint distrac- edge of the tissue-healing response for each specific
tion, joint entry, and fluid management.11,40,50 surgery (Table 2).
Pudendal, sciatic, and femoral neuropraxias have Limited ROM activities are initiated early after
been reported.11,18,23,50 The vast majority of these surgery. Patients are issued a brace (Post-op Hip
neuropraxias are transient in nature,11,40 and may be Brace; Bledsoe, Grand Prairie, TX) to protect the
related to the total time spent in traction.50 Less joint and limit ROM, particularly hip abduction and
common complications that have been reported in- rotation. The brace is worn during ambulation for
clude instrument breakage, heterotopic ossification, approximately 10 postoperative days. The brace is set
reflex sympathetic dystrophy, labia majora hematoma, at a neutral position to approximately 80° of flexion
trochanteric bursitis, and infection.6,11,18,23,30 in the sagittal plane. Rotation precaution boots (KAF
positioning kit; Bledsoe, Grand Prairie, TX) are worn
Preoperative Rehabilitation at night to prevent the hips from falling into external
rotation during sleep. External rotation places the
Griffin et al22 noted the importance of preopera- anterior capsuloligamentous structures under in-
tive rehabilitation in patients undergoing creased tension. Avoiding prolonged periods of in-
arthroscopic hip procedures. Goals in common with creased tension is of particular importance, especially
preoperative therapy for many other orthopaedic
for individuals undergoing capsular modification pro-
surgeries include maximizing ROM, strength, and
cedures. These individuals may be directed to utilize
endurance, without exacerbating the patient’s symp-
the immobilization system for up to 4 weeks
toms. During this time, patients who may not be
postsurgery. A continuous passive motion (CPM)
compliant with the prescribed therapeutic protocol
may also be identified. These individuals would not device is prescribed to be used for up to 8 hours per
typically be considered good candidates for surgery. day for 2 to 4 weeks in all patients undergoing hip
Preoperative therapy also gives the therapist an op- arthroscopy to reduce the risk of developing postop-
portunity to explain multiple aspects of the postop- erative adhesions and to encourage early postopera-
erative rehabilitation process, including weight- tive healing. This is the same CPM device utilized
bearing restrictions, as well as duration and frequency after surgical procedures of the knee joint. The initial
of therapy. setting provides movement between 30° and 70° of
flexion. This can be increased as tolerated, with an
Postoperative Rehabilitation eventual goal of movement between full extension
and maximally tolerated flexion.
It should be emphasized that arthroscopic proce- Hip ROM activities are introduced based on the
dures of the hip joint have only become more healing properties of the involved tissues (compara-
popular in recent times and continue to rapidly tive healing rates of bone, labral tissue,
evolve. At this time minimal evidence exists regarding capsuloligamentous structures, and cartilage). The
postoperative rehabilitation for these procedures. The factors to be considered are the pliability potential
guidelines suggested in this commentary are highly versus the risk of tissue damage.10 ROM activities can
based on the authors’ combined clinical experience be initiated in a fairly aggressive manner for individu-
gained from working with more than 500 patients als undergoing isolated resection or repair of the
undergoing these procedures. These guidelines will labrum. In the majority of cases, a patient will utilize
hopefully provide a foundation from which clinical a stationary bike without resistance the day of sur-
studies can be designed. gery. Excessive hip flexion or abduction should be
Though the postoperative rehabilitation program avoided to prevent discomfort often noted to occur
varies depending on the nature of procedure and during these ranges of motion. In the authors’
patient characteristics, general recommendations can experience, excessive flexion or abduction early in
be made. In our experience, 10 to 12 weeks of the rehabilitation process can result in the patient
supervised therapy is sufficient for an individual reporting a well-defined ‘‘pinching’’ sensation that is
undergoing arthroscopic resection or repair of the often followed by a period of general soreness in the
labrum as well as any of the previously mentioned anterior thigh or lateral hip region. Full passive
conjunct procedures. The immediate goal of therapy ROM, as dictated by patient tolerance, is typically
is to control postoperative inflammation through allowed at 14 days after surgery. If an anterior
J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006 521
capsular modification procedure was also performed, formed, and if other procedures were performed
hip external rotation and extension beyond 10° involving the articular cartilage or bony structures.
should be limited for 21 to 28 days to protect the Most patients are instructed to use crutches, allowing
anterior portion of the capsule. The need for protect- approximately 9.1 kg of flat-foot weight bearing. If a
ing the anterior capsuloligamentous structures is microfracture or osteoplasty procedure is performed,
comparable to the postoperative scenario following partial weight-bearing status is usually preferred over
anterior capsular reconstruction of the shoulder.27 complete non-weight bearing for the hip joint. This
Gentle, repetitive hip internal rotation ROM exercise demonstrates an application of Wolff’s Law; the goal
is stressed early in the rehabilitation process to being application of appropriate mechanical stress,
prevent adhesions of the joint capsule and subse- optimizing bone formation to manage compressive
quent loss of motion. In the authors’ experience, loads.2 A partial weight-bearing status also decreases
most patients can tolerate stretching of all muscles the load placed upon the upper extremities during
that cross the hip joint approximately 28 days after ambulation, compared to a non–weight-bearing sta-
surgery. tus. This is particularly relevant in the relatively active
Weight-bearing considerations are dependent on population who may undergo arthroscopic surgical
the area of the lesion (weight bearing versus non– procedures of the hip joint. This group of patients
weight-bearing region), nature of the procedure per- will likely desire a relatively higher level of mobility
TABLE 2. Rehabilitation guidelines after selected arthroscopic procedures of the hip joint.
Rehabilitation Weight-Bearing Range-of-Motion
Surgical Procedure Concerns Precautions (ROM) Precautions Strength Issues
Labral resection Avoiding initiation of Partial weight bearing for Avoid excessive early Gentle isometrics on day
joint inflammation 10-14 d flexion and abduction 2; active range of mo-
to prevent inflamma- tion (AROM) at 2 wk;
tion of affected tissue; weight-bearing progres-
full passive range of sive resisted exercises
motion (PROM) by 2 (PREs) as tolerated after
wk full weight bearing
Labral repair Avoiding initiation of Partial weight bearing for Avoid excessive early Gentle isometrics on day
joint inflammation 10-28 d flexion and abduction 2; AROM at 2 wk;
to prevent inflamma- weight-bearing PREs as
tion of affected tissue; tolerated after full
full PROM by 2 wk weight bearing
Osteoplasty/rim trimming Avoid excessive com- Partial weight bearing Avoid excessive early Gentle isometrics on day
procedure pressive and tensile (approximately 9.1 kg) flexion and abduction 2; AROM at 2 wk; cau-
forces to femoral neck for 4-6 wk to prevent inflamma- tion with sagittal plane
and head-neck junc- tion of affected tissue; straight leg raise sec-
tion; protect exposed full PROM by 2 wk ondary to increased
bone compressive forces;
gentle weight bearing
PREs by 4-6 wk
Capsular modification: Avoid excessive tension Partial weight bearing for Avoid excessive early Gentle isometrics on day
thermal assisted, plica- of affected capsular 10-14 d flexion and abduction; 2; limited AROM at 3
tion tissue (usually anterior avoid forced external wk; weight-bearing PREs
region); avoid capsular rotation and extension as tolerated after full
inflammation for 3-4 wk to protect weight bearing
anterior capsule;
progress external rota-
tion and extension after
3 wk; full PROM al-
lowed by 4 wk
Microfracture Avoid reinitiation of in- Partial weight bearing Avoid excessive early Gentle isometrics on day
flammatory response (approximately 9.1 kg) flexion and abduction 2; AROM at 2 weeks;
and protect early for 4-6 wk to prevent inflamma- caution with sagittal
fibrocartilage formation tion of affected tissue; plane straight leg raise
by limiting early com- full PROM by 2 wk secondary to increased
pression and shear compressive forces;
forces gentle weight-bearing
PREs by 4-6 wk
* For combined procedures the most conservative guidelines for each aspect of rehabilitation are observed.
522 J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006
and typically be ambulating greater average distances Emphasis is placed on eliminating substitution pat-
compared to individuals receiving THA procedures. A terns and progressing activities into specific func-
CLINICAL COMMENTARY
partial weight-bearing status allows application of a tional movement patterns. Lumbopelvic stabilization
controlled progressive stimulus for healing, while activities are progressed in parallel to PREs of the hip
promoting a relatively normal gait pattern. joint. Due to the proximity of the hip joint to the
An individual undergoing an isolated labral resec- lumbopelvic complex, the importance of trunk stabil-
tion or repair typically utilizes crutches for 10 to 28 ity has been noted.3 The authors suggest a useful
days before progressing to weight bearing as toler- analogy may be made between the need for
ated. Individuals undergoing repair procedures may lumbopelvic stabilization after hip surgery and
be required to maintain partial weight bearing for scapular stabilization after surgical procedures of the
shoulder.
the longer period to protect the repaired tissue and
Balance and functional activities are initiated as
promote healing. If a patient also has a microfracture
allowed by weight-bearing precautions and patients’
procedure or osteoplasty procedure performed, the
symptomatic presentation. During balance activities,
weight-bearing progression may be prolonged for 28
particular attention is directed towards proper re-
to 42 days. Primary concerns with the microfracture
cruitment of the gluteus medius muscle group, as
procedure are avoiding reinitiation of the inflamma-
well as continued incorporation of the more proximal
tor y process and protection of the forming
lumbopelvic stabilization musculature. Activities chal-
fibrocartilage. Alford and Cole1 noted the importance
of patient compliance to rehabilitation recommenda- lenging the patient in all planes of motion should be
tions following microfracture to the articular surfaces utilized. As previously mentioned, rotational instabil-
of the knee joint. They recommended non-weight ity is a preoperative finding in a number of patients
bearing for 6 weeks for procedures performed on the with labral and capsular compromise of the hip joint.
femoral condyle or tibial plateau. For the reasons For these individuals, activities focusing on re-
previously discussed, modified partial weight-bearing establishing dynamic rotational stability and motor
recommendations have been suggested for individuals control should be emphasized.
undergoing microfracture procedures of the hip The time for return to function varies depending
joint. In the case of an osteoplasty or rim-trimming on the extent of the surgical procedure and the
procedure, avoiding excessive compressive or tensile demand of the activities in which the patient wishes
forces at the femoral head-neck junction or to participate. Individual morphological characteris-
acetabulum is a priority. The transient compromise of tics may also play a role in the amount of time
bony integrity that occurs with an osteoplasty proce- required to return to desired activities. In the case of
dure creates a concern for the development of an isolated procedure for the labrum, jogging may be
femoral neck fractures during the early recovery initiated as early as 8 to 10 weeks if symptoms permit.
period. The authors have found aquatic ambulation If a microfracture or FAI procedure was also per-
to be useful for developing gait symmetry and at- formed, this time period will be extended signifi-
tempting to create an environment of optimal joint cantly. A return to manual labor activities can be
loading for patients undergoing any of the discussed expected in 10 to 24 weeks, depending on the
procedures. complexity of the case. A select few athletes undergo-
Gentle resisted exercises can be initiated the day ing resection of a small labral tear have returned to
after surgery. Such activities include isometric exer- sport activities as soon as 8 weeks postsurgery. Typi-
cises performed in a neutral position focusing on cally, athletes can return to a competitive environ-
extension, abduction, and adduction. In addition, ment in 10 to 32 weeks. The extended time range
quadriceps isometrics, and gentle lumbopelvic stabili- exists to account for those individuals undergoing
zation activities may be initiated. Active ROM is complex procedures that involve the articular carti-
usually initiated 14 days after surgery. A particular lage or bony components. In rare cases, when the
focus is placed on strengthening the gluteus medius postoperative integrity of the joint is questionable, it
muscle. For individuals who had a partial release of may be recommended that an athlete change the
the iliopsoas tendon, straight leg raises in the sagittal training regimen or even consider refraining from
plane are not allowed for at least 28 days. In the specific activities. Early establishment of realistic pa-
authors’ experience, early initiation of sagittal plane tient goals in relation to known joint integrity will
straight leg raise exercise is often associated with an help to minimize disappointment and frustration for
increased inflammatory response and may be related both the patient and therapist alike.
to the development of postoperative hip flexor
tendinitis. It has been noted that the hip joint
CONCLUSION
experiences a force greater than several times an The improvement of diagnostic technology and
individual’s body weight during a straight leg raise surgical technique has resulted in an expansion of
maneuver.22,49 Weight-bearing progressive resistance the options available to individuals suffering from
activities (PREs) are introduced when appropriate. pathological conditions of the hip joint. There has
J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006 523
been a particular interest in the detection and 14. Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular
surgical treatment of acetabular labral tears and labrum seal: a poroelastic finite element model. Clin
Biomech (Bristol, Avon). 2000;15:463-468.
associated lesions. Surgical procedures include labral
15. Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro
resection, labral repair, capsular modification, investigation of the acetabular labral seal in hip joint
osteoplasty, rim trimming, and microfracture. The mechanics. J Biomech. 2003;36:171-178.
common goal remains to decrease patient symptoms, 16. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of
improve functional outcomes, and restore long-term the acetabular labrum on hip joint cartilage consolida-
mechanical integrity of the joint. Initial results from a tion: a poroelastic finite element model. J Biomech.
2000;33:953-960.
number of these procedures appear promising. How- 17. Fitzgerald RH, Jr. Acetabular labrum tears. Diagnosis
ever, continued outcome studies are necessary to and treatment. Clin Orthop Relat Res. 1995;60-68.
validate their long-term success. Future studies must 18. Funke EL, Munzinger U. Complications in hip
focus on the effectiveness of newly developed proce- arthroscopy. Arthroscopy. 1996;12:156-159.
dures, as well as defining the ideal surgical candidate. 19. Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N,
Berlemann U. Surgical dislocation of the adult hip a
Physical therapists have the opportunity to play a technique with full access to the femoral head and
substantial role in the evolution of arthroscopic hip acetabulum without the risk of avascular necrosis.
procedures. Rehabilitation protocols, as with the sur- J Bone Joint Surg Br. 2001;83:1119-1124.
gical procedures, are still new in the field of 20. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H,
orthopaedics, and are constantly evolving. The devel- Siebenrock KA. Femoroacetabular impingement: a
cause for osteoarthritis of the hip. Clin Orthop Relat
opment of effective evidence-based rehabilitation
Res. 2003;112-120.
guidelines may prove to be a crucial factor in the 21. Glick JM, Sampson TG, Gordon RB, Behr JT, Schmidt E.
success of surgical procedures to address acetabular Hip arthroscopy by the lateral approach. Arthroscopy.
labral tears and associated pathologies. 1987;3:4-12.
22. Griffin DR, Villar RN. Complications of arthroscopy of
the hip. J Bone Joint Surg Br. 1999;81:604-606.
23. Griffin KM, Henry CO, Byrd JWT. Rehabilitation after
hip arthroscopy. J Sport Rehabil. 2000;9:77-88.
REFERENCES 24. Hase T, Ueo T. Acetabular labral tear: arthroscopic
1. Alford JW, Cole BJ. Cartilage restoration, part 2: tech- diagnosis and treatment. Arthroscopy. 1999;15:138-141.
niques, outcomes, and future directions. Am J Sports 25. Hoeksma HL, Dekker J, Ronday HK, et al. Comparison
of manual therapy and exercise therapy in osteoarthritis
Med. 2005;33:443-460.
of the hip: a randomized clinical trial. Arthritis Rheum.
2. Anderson MW, Greenspan A. Stress fractures. Radiol-
2004;51:722-729.
ogy. 1996;199:1-12.
26. Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R.
3. Anderson K, Strickland SM, Warren R. Hip and groin
Femoroacetabular impingement and the cam-effect. A
injuries in athletes. Am J Sports Med. 2001;29:521-533.
MRI-based quantitative anatomical study of the femoral
4. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology
head-neck offset. J Bone Joint Surg Br. 2001;83:171-
influences the pattern of damage to the acetabular
176.
cartilage: femoroacetabular impingement as a cause of
27. Jobe FW, Glousman RE. Anterior capsulolabral recon-
early osteoarthritis of the hip. J Bone Joint Surg Br.
struction. In: Paulos LE, Tibone JE, eds. Operative
2005;87:1012-1018. Technique in Shoulder Surgery. Gaithersburg, MD: As-
5. Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz pen Publishing; 1992.
R. Anterior femoroacetabular impingement: part II. Mid- 28. Kelly BT, Weiland DE, Schenker ML, Philippon MJ.
term results of surgical treatment. Clin Orthop Relat Arthroscopic labral repair in the hip: surgical technique
Res. 2004;67-73. and review of the literature. Arthroscopy.
6. Byrd JW. Complications associated with hip 2005;21:1496-1504.
arthroscopy. In: Byrd JW, ed. Operative Hip 29. Kelly BT, Williams RJ, 3rd, Philippon MJ. Hip
Arthroscopy. New York, NY: Thieme; 1998:171-176. arthroscopy: current indications, treatment options, and
7. Byrd JW. Hip arthroscopy utilizing the supine position. management issues. Am J Sports Med. 2003;31:1020-
Arthroscopy. 1994;10:275-280. 1037.
8. Byrd JW, Jones KS. Prospective analysis of hip 30. Kim SJ, Choi NH, Kim HJ. Operative hip arthroscopy.
arthroscopy with 2-year follow-up. Arthroscopy. Clin Orthop Relat Res. 1998;156-165.
2000;16:578-587. 31. Lage LA, Patel JV, Villar RN. The acetabular labral tear:
9. Canale ST. Campbell’s Operative Orhtopaedics. 9th ed. an arthroscopic classification. Arthroscopy. 1996;12:
New York, NY: Mosby; 1998. 269-272.
10. Cantu R. Soft tissue healing considerations after surgery. 32. Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R,
In: Maxey LM, ed. Rehabilitation for the Postsurgical Leunig M. Anterior femoroacetabular impingement: part
Orthopedic Patient. St Loius, MO: Mosby; 2001. I. Techniques of joint preserving surgery. Clin Orthop
11. Clarke MT, Arora A, Villar RN. Hip arthroscopy: com- Relat Res. 2004;61-66.
plications in 1054 cases. Clin Orthop Relat Res. 33. Leunig M. [waiting for au reply]. Third Symposium on
2003;84-88. Joint Preserving and Minimally Invasive Surgery of the
12. Dvorak M, Duncan CP, Day B. Arthroscopic anatomy of Hip. Montreal, Canada: 2004.
the hip. Arthroscopy. 1990;6:264-273. 34. Leunig M, Werlen S, Ungersbock A, Ito K, Ganz R.
13. Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for Evaluation of the acetabular labrum by MR
acetabular labral tears. Arthroscopy. 1999;15:132-137. arthrography. J Bone Joint Surg Br. 1997;79:230-234.
524 J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006
35. McCarthy J, Noble P, Aluisio FV, Schuck M, Wright J, disability status with outcomes of arthroscopic
Lee JA. Anatomy, pathologic features, and treatment of acetabular labral debridement. Am J Sports Med.
acetabular labral tears. Clin Orthop Relat Res. 2003;38-
CLINICAL COMMENTARY
2005;33:864-870.
47. 48. Reynolds D, Lucas J, Klaue K. Retroversion of the
36. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. acetabulum. A cause of hip pain. J Bone Joint Surg Br.
The Otto E. Aufranc Award: The role of labral lesions to 1999;81:281-288.
development of early degenerative hip disease. Clin 49. Rydell N. Forces acting on the femoral head-prosthesis:
Orthop Relat Res. 2001;25-37. a study on strain gauge supplied prostheses in living
37. Mintz DN, Hooper T, Connell D, Buly R, Padgett DE, persons. Acta Orthop Scand. 1966;37(Suppl 88):1-132.
Potter HG. Magnetic resonance imaging of the hip: 50. Sampson TG. Complications of hip arthroscopy. Clin
detection of labral and chondral abnormalities using
Sports Med. 2001;20:831-835.
noncontrast imaging. Arthroscopy. 2005;21:385-393.
38. Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. 51. Santori N, Villar RN. Acetabular labral tears: result of
Debridement of the adult hip for femoroacetabular arthroscopic partial limbectomy. Arthroscopy.
impingement: indications and preliminary clinical re- 2000;16:11-15.
sults. Clin Orthop Relat Res. 2004;178-181. 52. Schenker ML, Philippon MJ. The role of flexible
39. Murphy SB, Barsoum W. Preliminary clinical results of radiofrequency energy probes in hip arthroscopy. Tech
ceramic-ceramic bearings in total hip arthroplasty. Orthop. 2005;20:37-44.
Orthop J Harv Med Sch. 2001;3:92-94. 53. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical
40. Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular evidence of bias. Dimensions of methodological quality
labrum and its tears. Br J Sports Med. 2003;37:207-211. associated with estimates of treatment effects in con-
41. Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber trolled trials. JAMA. 1995;273:408-412.
K, Hodler J. The contour of the femoral head-neck 54. Sherman OH, Fox JM, Snyder SJ, et al. Arthroscopy—
junction as a predictor for the risk of anterior impinge- ‘‘no-problem surgery’’. An analysis of complications in
ment. J Bone Joint Surg Br. 2002;84:556-560. two thousand six hundred and forty cases. J Bone Joint
42. O’Leary J A, Berend K, Vail TP. The relationship Surg Am. 1986;68:256-265.
between diagnosis and outcome in arthroscopy of the 55. Small NC. Complications in arthroscopic surgery per-
hip. Arthroscopy. 2001;17:181-188. formed by experienced arthroscopists. Arthroscopy.
43. Philippon MJ. Debridement of acetabular tears with 1988;4:215-221.
associated thermal capsulorrhaphy. Oper Tech Sports 56. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ,
Med. 2002;10:215-218. Rodkey WG. Outcomes of microfracture for traumatic
44. Philippon MJ. The role of arthroscopic thermal chondral defects of the knee: average 11-year follow-
capsulorrhaphy in the hip. Clin Sports Med. up. Arthroscopy. 2003;19:477-484.
2001;20:817-829. 57. Tanzer M, Noiseux N. Osseous abnormalities and early
45. Philippon MJ, Schenker ML. Hip arthroscopy for the osteoarthritis: the role of hip impingement. Clin Orthop
treatment of femoroacetabular impingement in the ath- Relat Res. 2004;170-177.
lete. Clin Sports Med. In press. 58. Weber SC, Abrams JS, Nottage WM. Complications
46. Philippon MJ, Schenker ML. A new method for associated with arthroscopic shoulder surgery.
acetabular rim trimming and labral repair. Clin Sports Arthroscopy. 2002;18:88-95.
Med. 2006;25:293-297, ix. 59. Wegener ST, Belza BL, Gall EP. Clinical Care in
47. Potter BK, Freedman BA, Andersen RC, Bojescul JA, Rheumatic Diseases. Atlanta, GA: American College of
Kuklo TR, Murphy KP. Correlation of Short Form-36 and Rhematology; 1996.
J Orthop Sports Phys Ther • Volume 36 • Number 7 • July 2006 525
View publication stats
You might also like
- AACP Acupuncture Point Reference Manual PDFDocument100 pagesAACP Acupuncture Point Reference Manual PDFRadhakrishnan Kasthuri100% (4)
- Orthopedic Surgery Clerkship A Quick Reference Guide For Senior Medical StudentsDocument750 pagesOrthopedic Surgery Clerkship A Quick Reference Guide For Senior Medical StudentsGreenIron9100% (1)
- Cerebral Palsy Special Tests and Corrective ProceduresDocument11 pagesCerebral Palsy Special Tests and Corrective ProceduresOj AlimbuyuguenNo ratings yet
- Exercises and Stretches For Ankylosing Spondylitis Back PainDocument7 pagesExercises and Stretches For Ankylosing Spondylitis Back PainBGNo ratings yet
- Gait BiomechanicsDocument35 pagesGait BiomechanicsHeena Awais100% (1)
- Rehabilitation For Hip Arthros PDFDocument4 pagesRehabilitation For Hip Arthros PDFMónica Sabogal JaramilloNo ratings yet
- Evidence-Based Treatment Choices For Acute Lateral Ankle Sprain: A Comprehensive Systematic ReviewDocument9 pagesEvidence-Based Treatment Choices For Acute Lateral Ankle Sprain: A Comprehensive Systematic ReviewMilton RezzaNo ratings yet
- 0269215511423557Document10 pages0269215511423557Jose Maria DominguezNo ratings yet
- Anterior Cruciate Ligament Reconstruction, Rehabilitation, and Return To Play: 2015 UpdateDocument12 pagesAnterior Cruciate Ligament Reconstruction, Rehabilitation, and Return To Play: 2015 UpdateAulida Arum MNo ratings yet
- Willmore Smith 2016 Scapular Dyskinesis EvolutiontowardsandsystemsbasedapproachDocument11 pagesWillmore Smith 2016 Scapular Dyskinesis EvolutiontowardsandsystemsbasedapproachAhmed TawfiqNo ratings yet
- 2014 Rehabilitación Después de Una Cirugía Por Estenosis Espinal Lumbar. RevisiónDocument12 pages2014 Rehabilitación Después de Una Cirugía Por Estenosis Espinal Lumbar. Revisiónjuan pabloNo ratings yet
- The Effect of Rim Preparation, Labral Augmentation, and Labral Reconstruction On The Suction Seal of The HipDocument9 pagesThe Effect of Rim Preparation, Labral Augmentation, and Labral Reconstruction On The Suction Seal of The HipGökhan PehlivanoğluNo ratings yet
- Eliasson 2018Document11 pagesEliasson 2018seriesediversosNo ratings yet
- What's New in Spine Surgery: Specialty UpdateDocument11 pagesWhat's New in Spine Surgery: Specialty UpdatePoliceNo ratings yet
- Does Total Knee Replacement Restore NormDocument9 pagesDoes Total Knee Replacement Restore NormSahithya MNo ratings yet
- The Effectiveness of Shoulder Stretching and Joint Mobilizations On Posterior Shoulder TightnessDocument8 pagesThe Effectiveness of Shoulder Stretching and Joint Mobilizations On Posterior Shoulder TightnessKlgo. Fernando HuertaNo ratings yet
- Traction PDFDocument31 pagesTraction PDFrushaliNo ratings yet
- OUtcome After Limted or Extensive BursectomyDocument8 pagesOUtcome After Limted or Extensive BursectomySeno adipNo ratings yet
- 1 s2.0 S0003999319303892 MainDocument8 pages1 s2.0 S0003999319303892 MainRizkyrafiqoh afdinNo ratings yet
- Giray 2019Document13 pagesGiray 2019Felix LoaizaNo ratings yet
- Resurfacing For Perthes DiseaseDocument6 pagesResurfacing For Perthes Diseaseyarimar hoyosNo ratings yet
- Rehabilitationafter Arthroscopic Decompressionfor Femoroacetabular ImpingementDocument9 pagesRehabilitationafter Arthroscopic Decompressionfor Femoroacetabular ImpingementEricNo ratings yet
- 1 - General Indications and Contraindications - 2019 - Lumbar Interbody FusionsDocument12 pages1 - General Indications and Contraindications - 2019 - Lumbar Interbody FusionsSergiu MalinNo ratings yet
- Luthringer 2019Document14 pagesLuthringer 2019Cristian Diaz KooNo ratings yet
- CV4 EfectDocument21 pagesCV4 EfectNicole HermosillaNo ratings yet
- Rehab JournalDocument11 pagesRehab JournalMae DoctoleroNo ratings yet
- A Systematic Review of Outcomes Reporting For Brachial Plexus ReconstructionDocument6 pagesA Systematic Review of Outcomes Reporting For Brachial Plexus ReconstructionAndrés Urrego NietoNo ratings yet
- GR Up: SM Orthopedics & Muscular SystemDocument6 pagesGR Up: SM Orthopedics & Muscular SystemValerie BpNo ratings yet
- Rajiv Gandhi University of Health Sciences Bengaluru, Karnataka Proforma For Registration of Subjects For DissertationDocument10 pagesRajiv Gandhi University of Health Sciences Bengaluru, Karnataka Proforma For Registration of Subjects For DissertationRachnaNo ratings yet
- Okc Vs CKC in PfpsDocument10 pagesOkc Vs CKC in PfpsABDUL NASAR.MNo ratings yet
- SiaiDocument8 pagesSiaimassimo bertoniNo ratings yet
- Vergelijking Versneld Vs NT Versneld Revalidatie Na ACLDocument14 pagesVergelijking Versneld Vs NT Versneld Revalidatie Na ACLEllen&Koen WalravensNo ratings yet
- The "Ligamentization" Process in Anterior Cruciate Ligament ReconstructionDocument9 pagesThe "Ligamentization" Process in Anterior Cruciate Ligament Reconstructionmarcelogascon.oNo ratings yet
- Physical Therapy in The Postoperative of Proximal Femur Fracture in Elderly. Literature ReviewDocument4 pagesPhysical Therapy in The Postoperative of Proximal Femur Fracture in Elderly. Literature ReviewEcsekiel MirandaNo ratings yet
- FIRST2020Document10 pagesFIRST2020Jeisson Daniel Barrera AlvarezNo ratings yet
- Ankle Stabilization With Arthroscopic Versus Open With Suture Tape Augmentation Techniques X1D XJ. George DeVries PDFDocument5 pagesAnkle Stabilization With Arthroscopic Versus Open With Suture Tape Augmentation Techniques X1D XJ. George DeVries PDFcrpcsxfdkgNo ratings yet
- Sternotomi PDFDocument11 pagesSternotomi PDFHeri PrasetyoNo ratings yet
- Management Sprain AnkleDocument10 pagesManagement Sprain AnkledwiNo ratings yet
- Mulligan Knee TapingDocument8 pagesMulligan Knee TapingVinicius MascarenhasNo ratings yet
- Early Versus Delayed Passive Range of Motion Exercise For Arthroscopic Rotator Cuff RepairDocument9 pagesEarly Versus Delayed Passive Range of Motion Exercise For Arthroscopic Rotator Cuff RepairJane Elisabeth WauranNo ratings yet
- O Fortalecimento Combinado Do Abdutor Do Quadril e Do Rotador Externo e o Alongamento Do Rotador Interno Do Quadril Melhoram A Dor e A Função em Pacientes Com Síndrome Da Dor Femoropatelar Um EnsaiDocument6 pagesO Fortalecimento Combinado Do Abdutor Do Quadril e Do Rotador Externo e o Alongamento Do Rotador Interno Do Quadril Melhoram A Dor e A Função em Pacientes Com Síndrome Da Dor Femoropatelar Um EnsaiLeticia ZaniniiNo ratings yet
- Ijspt 12 1150 IliopsoasDocument13 pagesIjspt 12 1150 Iliopsoasnikhilmascarenhas07No ratings yet
- Physiotherapy After Tibial Plateau Fracture Fixation A Systematic Review of The Literature - PMCDocument1 pagePhysiotherapy After Tibial Plateau Fracture Fixation A Systematic Review of The Literature - PMCmf6wj6ccxqNo ratings yet
- Willmore, 2016 - Scapular Dyskinesia (Evolution Towards A Systems Based Approach)Document10 pagesWillmore, 2016 - Scapular Dyskinesia (Evolution Towards A Systems Based Approach)Ana Teixeira MartinsNo ratings yet
- Randomized, Controlled Clinical Trial of Treatment For Shoulder PainDocument8 pagesRandomized, Controlled Clinical Trial of Treatment For Shoulder PainRoy TukaNo ratings yet
- Deepti - 2016 Effects of Retrowalking On Osteoarthritis of Knee in GeriatricDocument7 pagesDeepti - 2016 Effects of Retrowalking On Osteoarthritis of Knee in Geriatricnur pratiwiNo ratings yet
- The Role of Biomechanical Applications in Muasculoskeletal and Neurological Rehabilitation: Review ArticleDocument7 pagesThe Role of Biomechanical Applications in Muasculoskeletal and Neurological Rehabilitation: Review ArticleGSL SMART LABNo ratings yet
- 2015 OJSM ProximalHamstringRepairStrength ABiomechanicalAnalysisat3HipFlexionAnglesDocument6 pages2015 OJSM ProximalHamstringRepairStrength ABiomechanicalAnalysisat3HipFlexionAnglesMaria Elena AguileraNo ratings yet
- Open Kinetic Chain Exercises in A Restricted Range of Motion After Anterior Cruciate Ligament Reconstruction - Fukuda2013Document8 pagesOpen Kinetic Chain Exercises in A Restricted Range of Motion After Anterior Cruciate Ligament Reconstruction - Fukuda2013Adriano SantosNo ratings yet
- Massive Rotator Cuff Tears: Pathomechanics, Current Treatment Options, and Clinical OutcomesDocument13 pagesMassive Rotator Cuff Tears: Pathomechanics, Current Treatment Options, and Clinical OutcomesFillipe AgraNo ratings yet
- Colgan 2016Document6 pagesColgan 2016Wahyu InsanNo ratings yet
- LowerDocument16 pagesLowerLucaNo ratings yet
- The Relationship of Suture Design To Bio-MechanicaDocument11 pagesThe Relationship of Suture Design To Bio-MechanicaantoanetaNo ratings yet
- Open Kinetic Chain Exercises in Restricted ROM After ACL Reconstruction AJSM 2013Document8 pagesOpen Kinetic Chain Exercises in Restricted ROM After ACL Reconstruction AJSM 2013Michele GonçalvesNo ratings yet
- Beynnon2011 RCTDocument14 pagesBeynnon2011 RCTNaeema MosaNo ratings yet
- To Rry EffusionDocument14 pagesTo Rry EffusionLINANo ratings yet
- 45 Llps Vs HlbsDocument4 pages45 Llps Vs HlbsSudhir MishraNo ratings yet
- Reduced Muscle Fiber Force ProductionDocument9 pagesReduced Muscle Fiber Force ProductionRaeni Dwi PutriNo ratings yet
- Fsurg 08 662720Document6 pagesFsurg 08 662720Deborah SalinasNo ratings yet
- Birth Brachial Plexus Palsy UpdateDocument8 pagesBirth Brachial Plexus Palsy UpdateDyah SafitriNo ratings yet
- Comparison of Aggressive and Traditional Postoperative Rehabilitation Protocol After Rotator Cuff Repair: A Meta-AnalysisDocument6 pagesComparison of Aggressive and Traditional Postoperative Rehabilitation Protocol After Rotator Cuff Repair: A Meta-AnalysisNico BrantesNo ratings yet
- PRP Versus Aspirado de MedulaDocument9 pagesPRP Versus Aspirado de Medulajulionline7No ratings yet
- El Akkawi2017Document7 pagesEl Akkawi2017Nurfitrianti ArfahNo ratings yet
- Evidence To Practice Review Best Practices in Patellar Tendinopathy ManagementDocument8 pagesEvidence To Practice Review Best Practices in Patellar Tendinopathy ManagementLeandroNo ratings yet
- Operative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesFrom EverandOperative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesAlexander Y. ShinNo ratings yet
- Chiropractic and Spinal Manipulation Red Flags: A Comprehensive Review Sam HomolaDocument20 pagesChiropractic and Spinal Manipulation Red Flags: A Comprehensive Review Sam HomolawladjaNo ratings yet
- Symposium Fikkert KoopmanDocument2 pagesSymposium Fikkert KoopmanwladjaNo ratings yet
- Acetabular Labral Tears Diagnosis RepairDocument13 pagesAcetabular Labral Tears Diagnosis RepairwladjaNo ratings yet
- Physical Examination Tests For Hip Dysfunction and Injury: March 2015Document8 pagesPhysical Examination Tests For Hip Dysfunction and Injury: March 2015wladjaNo ratings yet
- Assessment of Strength Flexibility and RDocument6 pagesAssessment of Strength Flexibility and RwladjaNo ratings yet
- Anatomy of The Deep Fascia of The UpperDocument8 pagesAnatomy of The Deep Fascia of The UpperwladjaNo ratings yet
- Manipulation According To Maigne: Roger Baecher, MDDocument69 pagesManipulation According To Maigne: Roger Baecher, MDwladjaNo ratings yet
- Interventions in Chronic Pain ManagementDocument4 pagesInterventions in Chronic Pain ManagementwladjaNo ratings yet
- Groin DissectionDocument19 pagesGroin Dissectiondewiswahyu100% (1)
- 1.05 Understand The Functions and Disorders of The Muscular SystemDocument49 pages1.05 Understand The Functions and Disorders of The Muscular SystemanneNo ratings yet
- Shoulder Arthroplasty: Types - Indication - RehabilitationDocument35 pagesShoulder Arthroplasty: Types - Indication - RehabilitationPerjalanan SukarNo ratings yet
- Ultrasonografia em EquinosDocument8 pagesUltrasonografia em EquinosIngrid MachadoNo ratings yet
- Skeletal Muscles of A Toad/FrogDocument2 pagesSkeletal Muscles of A Toad/FrogAuroraNo ratings yet
- Dermatome, Myotome, SclerotomeDocument4 pagesDermatome, Myotome, SclerotomeElka Rifqah100% (3)
- Study Guide For Students of Tong's AcupunctureDocument63 pagesStudy Guide For Students of Tong's AcupuncturemattNo ratings yet
- Muscles of The Gluteal RegionDocument2 pagesMuscles of The Gluteal RegionYogi drNo ratings yet
- Human Anatomy Lab Manual 1535056949Document187 pagesHuman Anatomy Lab Manual 1535056949HalluxNo ratings yet
- Elbow Anatomy: DR Paul Bundi Karau (BSC, MBCHB) Lecturer, Human AnatomyDocument30 pagesElbow Anatomy: DR Paul Bundi Karau (BSC, MBCHB) Lecturer, Human AnatomyGish KioiNo ratings yet
- 6 Day Female Training Program PDFDocument1 page6 Day Female Training Program PDFSmyle KatariaNo ratings yet
- Catatan Bedah SarafDocument3 pagesCatatan Bedah SarafNo NamedNo ratings yet
- BTEC Sport - Anatomy - Muscle GroupsDocument18 pagesBTEC Sport - Anatomy - Muscle Groupsbenjenkins21No ratings yet
- Biomechanics of Knee Joint PDFDocument32 pagesBiomechanics of Knee Joint PDFAli NoumanNo ratings yet
- Osteology I: Bones of The Upper LimbDocument26 pagesOsteology I: Bones of The Upper LimbNaufalNo ratings yet
- 18 Vascular Anatomy of The Lower LimbsDocument15 pages18 Vascular Anatomy of The Lower Limbsroyvillafranca100% (1)
- Anatomy of Hip JointDocument5 pagesAnatomy of Hip JointSneha ParveenNo ratings yet
- FSFCS36 PDFDocument8 pagesFSFCS36 PDFSatbir KarwasraNo ratings yet
- Review Pub MedicineDocument2 pagesReview Pub Medicinestylesh828No ratings yet
- 00.+27788676511,. Contact the Official ILLUMINATI AGENT in SOUTH AFRICA,,,Botswana,Uganda ,UK, Canada, Harare.. ,Zambia,Swaziland,Canada,Guyana,France,Germany,Spain,Poland,Switzerland,Romania,Bulgaria,Denmark,Finland,Netherlands,Norway,SwedenDocument1 page00.+27788676511,. Contact the Official ILLUMINATI AGENT in SOUTH AFRICA,,,Botswana,Uganda ,UK, Canada, Harare.. ,Zambia,Swaziland,Canada,Guyana,France,Germany,Spain,Poland,Switzerland,Romania,Bulgaria,Denmark,Finland,Netherlands,Norway,Swedenjona tumukundeNo ratings yet
- Muscle Extremitas SuperiorDocument57 pagesMuscle Extremitas SuperiorDewi NurpratiwiNo ratings yet
- Common Sports Injuries: August 2016Document8 pagesCommon Sports Injuries: August 2016Binte SajjadNo ratings yet
- Darkroom Procedures QuestionDocument12 pagesDarkroom Procedures QuestionSatish Paswan100% (1)
- The Language of AnatomyDocument4 pagesThe Language of Anatomyjava_biscocho122950% (2)
- SOAL Rehab 2010 Kak NelfiDocument5 pagesSOAL Rehab 2010 Kak Nelfifarid akbarNo ratings yet