Professional Documents
Culture Documents
Buerger Disease
Uploaded by
M Ali AdrianCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Buerger Disease
Uploaded by
M Ali AdrianCopyright:
Available Formats
Endovascular Treatment of Critical Limb Ischemia in Buerger
Disease (Thromboangiitis Obliterans) With Midterm Follow-Up:
A Viable Option When Bypass Surgery Is Not Feasible
Sadık Ahmet Uyanık, MD1, Umut Öğüşlü, MD1, Ibrahim Sani Aminu, MD2, Bırnur Yılmaz, MD1, Halime Çevik, MD1,
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
Eray Atlı, MD1, Burçak Gümüş, MD1
Inter ventional Radiology · Original Research
Keywords
OBJECTIVE. Thromboangiitis obliterans (TAO) is an occlusive inflammatory disease
Buerger disease, endovascular treatment,
thromboangiitis obliterans affecting small- and medium-sized vessels that causes decrease in life quality and even-
tually limb loss. The only proven treatment method is smoking cessation, but it may be
Submitted: Feb 25, 2020 insufficient for limb salvage in patients with critical limb ischemia. In this single-cen-
Revision requested: Apr 4, 2020 ter retrospective study, the feasibility and efficiency of endovascular treatment in TAO
Revision received: Apr 23, 2020 were evaluated.
Accepted: May 8, 2020 MATERIALS AND METHODS. After approval of the local institutional review
board, 41 patients who underwent endovascular treatment of TAO between Janu-
The authors declare that they have no ary 2014 and June 2019 were evaluated retrospectively. Technical success and proce-
disclosures relevant to the subject matter of dure-related complications were recorded. Decrease in Rutherford classification score,
this article.
relief of pain, and wound healing were evaluated to determine clinical success. Primary
patency, limb salvage rate, and amputation-free survival were also evaluated.
RESULTS. A total of 45 limbs were treated during the study period. Technical suc-
cess was achieved in 82.2% of procedures. Mean follow-up was 29.8 months. Clinical
improvement was achieved in 35 limbs. Three patients underwent major amputation
and 12 patients underwent minor amputation. Amputation-free survival and limb sal-
vage were both 93.3% at both 1 and 2 years. Reintervention was performed in 14 pa-
tients because of occlusion and clinical relapsing of the symptoms.
CONCLUSION. Endovascular treatment of TAO is feasible, has a potential to prevent
limb amputation in patients with critical limb ischemia, and has acceptable technical
success and limb salvage rates. Because there is no consensus in treatment of TAO, pro-
spective comparative studies are needed to determine the effectiveness of an endo-
vascular approach.
Thromboangiitis obliterans (TAO), or Buerger disease, is an occlusive inflammatory
vascular disease that affects predominantly small- and medium-sized vessels in the ex-
tremities, leading to loss of perfusion in the affected area and eventually resulting in am-
putation [1]. TAO is more prevalent in the younger male population, and its incidence cor-
responds with tobacco exposure. TAO is also more prevalent in Asian and Middle Eastern
countries compared with Western Europe [2].
The pathophysiologic mechanisms of TAO are still unclear; however, the disease con-
sists of an acute inflammatory phase followed by a chronic fibrotic phase. The prognosis
of the disease is dependent on the progression to the latter phase [3]. As the disease pro-
gresses, ischemic signs ranging from intermittent claudication, cyanosis, and Raynaud
phenomenon to paresthesia, rest pain, and phlebitis migrans begin to manifest [2, 4, 5].
It may eventually lead to life-limiting claudication and limb-threatening ischemia, which
are two main indications for treatment of TAO. Infrapopliteal vessels are predominantly
affected in TAO. Although femoropopliteal vessels may be included, distal crural arteries
are the most commonly affected vessels [6].
There is still no consensus over the treatment of TAO, and the only accepted effective
Uyanik et al. treatment is the cessation of smoking [1, 5, 7]. Nevertheless, for patients with critical limb
Endovascular Treatment of Critical Limb Ischemia
Interventional Radiology ischemia, revascularization should be considered in addition to cessation of smoking be-
cause critical limb ischemia results in decreases in productivity and quality of life [8]. Al-
Original Research
though methods such as surgical bypass, lumbar sympathectomy, spinal cord stimulation,
Uyanik SA, Öğüşlü U, Aminu IS, et al. and prostaglandin analogs have been reported in the literature, endovascular treatment
of TAO is gaining focus paralleling the advancements in endovascular techniques [9–13].
doi.org/10.2214/AJR.20.23023
AJR 2021; 216:1–7 1
Department of Radiology, Okan University Hospital, Aydınlı Cad No 2, Okan Universitesi Hastanesi İçmeler, Tuzla,
ISSN-L 0361–803X/21/2162–1 Istanbul, Turkey 34947. Address correspondence to S. A. Uyanik (drsadikahmetuyanik@gmail.com).
© American Roentgen Ray Society School of Medicine, Okan University, Istanbul, Turkey.
2
AJR:216, February 2021 www.ajronline.org | 1
Uyanik et al.
revious studies have reported surgical bypass as an effective
P lar treatment were included in this study. Inclusion criteria were
method for limb salvage. Unfortunately, severe multisegmental a diagnosis of TAO according to the Shionoya criteria (Appen-
below-the-knee involvement of the disease results in the lack of a dix 1) and angiographic findings compatible with TAO, Ruther-
suitable artery for anastomosis, and coexisting phlebitis may less- ford classification 4 or higher (rest pain, minor ulceration, major
en the chance for autogenous graft usage. In addition, patency of ulceration, or gangrene), and not being eligible for surgical re-
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
the bypass grafts in TAO is lower than for atherosclerotic occlusive vascularization because of a lack of suitable venous conduit or
disease, which may be attributed to on-going inflammation be- distal nondiseased artery for anastomosis [23]. Exclusion crite-
cause of the nature of TAO [14–17]. Previously, endovascular treat- ria were patients with a history of allergic reaction precluding
ment of TAO has been shown to be feasible, but the data are still angiography, patients with a main presentation of claudication
being accumulated [4, 18–22]. The primary aim of this single-cen- (Rutherford class 3 or less), and patients who were candidates
ter study is to evaluate the technical and clinical outcomes of endo- for bypass surgery.
vascular treatment in TAO and contribute to the growing literature Demographic features of the patients included in the study are
supporting endovascular treatment in patients with TAO who are presented in Table 1.
not candidates for bypass surgery.
Interventional Procedure
Materials and Methods The procedures were performed under local anesthesia and
Patient Population mild to moderate sedation. An antegrade 5-French sheath was
This study was approved by the ethics committee of Okan placed in the ipsilateral common femoral artery and angiography
University Hospital, and informed consent was waived. A to- of the lower extremity was performed. After depiction of the le-
tal of 41 consecutive patients between January 2016 and June sions with angiography, IV 5000 IU heparin was administered and
2019 who had a TAO diagnosis and who underwent endovascu- 100 µg nitroglycerin was injected from the sheath if there was
no contraindication. All inflow lesions (superficial femoral artery
and popliteal artery) were targeted for recanalization as a rou-
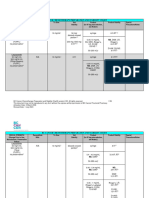
TABLE 1: Demographic Characteristics of the tine protocol. The decision on how many tibial vessels were tar-
Patients geted for treatment was made on a case basis according to the
main clinical presentation and condition of the wound if present.
Characteristic Value The main objective was to achieve at least one additional patent
Sex runoff artery to the foot. For patients with tissue loss, the prima-
Male 39 (95.1) ry target for revascularization was the artery of the related angio-
some. If direct revascularization of the target angiosome failed,
Female 2 (4.9)
indirect vascularization was attempted by treating other runoff
Age (y) arteries. Lesions were crossed with a 4-French support catheter
Mean 41.9 (NaviCross, Terumo Medical) and 0.035-inch hydrophilic guide-
Range 28–55 wire combination. Lesions were first attempted to be crossed
with an endoluminal approach. If this approach failed, a subinti-
Diabetes 0 (0)
mal technique was used. Retrograde pedal access was also used
Coronary artery disease 4 (9.8) when both techniques from the antegrade route failed.
Chronic renal disease 0 (0) After crossing of the lesion was successful, balloon dilatation was
applied for a specific length of time (mean, 3 minutes) and under
Hypertension 5 (12.2)
high pressure (18–24 atm). Primary stenting was avoided because
Hyperlipidemia 0 (0) of the underlying inflammatory nature of the disease and was re-
Smoking history (y) served for bail-out procedures. After angioplasty, if the control an-
Mean 20.9 giography showed straight inflow of the target arteries without
more than 50% residual stenosis or flow-limiting dissection, the
Range 10–31
procedure was terminated. A sample case is presented in Figure 1.
Current smoker 12 (29.3)
Previous endovascular intervention 7 (17.0) Follow-Up
Previous amputation After the procedure, patients received daily dual antiplatelet
therapy (acetylsalicylic acid and clopidogrel) during follow-up for 6
Major 0 (0)
months. Lifelong single antiplatelet therapy with acetylsalicylic acid
Minor 4 (9.7) was continued daily after 6 months. Control follow-up visits were
Rutherford classification scheduled at the first week, first month, and every 6-month inter-
vals after the procedure. At their follow-up visits, patients were eval-
4 21 (46.7)
uated with Doppler ultrasound, and clinical symptoms and condi-
5 13 (28.9) tion of the wound (if present) were also assessed. Wound care was
6 11 (24.4) performed by a wound care specialist. Aggressive antibiotic thera-
Note—Unless otherwise indicated, values are reported as number (%). Total py administered in infected wounds and extensive débridement of
number of patients was 41; total number of limbs was 45. necrotic tissues were done after endovascular therapy.
2 AJR:216, February 2021
E n d o v a s c u l a r Tr e a t m e n t o f C r i t i c a l L i m b I s c h e m i a
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
A B C
D E F
G H I
Fig. 1—35-year-old man with ischemic rest pain.
A–C, Diagnostic angiography shows long segmental occlusions of superficial femoral artery (A) and crural arteries (B and C).
D–F, After crossing lesions, balloon angioplasty was performed on superficial femoral artery (D), peroneal artery (E), and posterior tibial artery (F).
G–I, Control angiography shows recanalization of superficial femoral artery (G), peroneal artery (H), and posterior tibial artery (I).
Outcomes defined as wound healing, relief of pain, and decrease in Ruther-
Primary outcomes of this study were technical success, clini- ford classification of at least 1 point. Limb salvage was defined as
cal success, limb salvage, and amputation-free survival. Technical the time from the procedure to time of major amputation. Ampu-
success was defined as achieving direct inflow in the target vessel tation-free survival was defined as the time from the procedure
without residual stenosis greater than 30%. Clinical success was to the time of death or major amputation. Major amputation was
AJR:216, February 2021 3
Uyanik et al.
glycerin injection. Another three patients did not respond to in-
TABLE 2: Procedural Details
traarterial vasodilators, which resulted in failure of the procedure.
Procedure Detail No. of Procedures One patient with vessel perforation and one patient with arte-
riovenous fistulation were treated with prolonged balloon dila-
Treated artery
tion and were relieved without any further therapy. There were
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
SFA 10 no thrombosis or embolic complications. Procedural details are
Popliteal artery 17 summarized in Table 2.
ATA 30 Mean follow-up of the patients was 29.8 months (range, 8–61
months). The median Rutherford score before treatment was 5
PTA 32
(range, 4–6) and 3 after treatment (range, 2–6). Changes in Ruth-
Peroneal artery 11 erford scores were statistically significant (p < 0.001). Clinical im-
Plantar artery 21 provement was reported in 35 limbs. Wound healing was report-
Total 121 ed in 19 limbs and pain relief was reported in 33 limbs. There was
no change in rest pain in two patients although endovascular
Technical success 37/45 (82.2)
treatment was successful.
Transpedal access 9/45 (20.0) Primary patency was 64.2% at 1 year and 60.0% at 2 years. Four-
Complication teen patients underwent reintervention during the follow-up pe-
riod because of relapsing of the symptoms and occlusion of the
Vasospasm 6 (13.3)
treated vessels. After reintervention, patency was achieved in all
Perforation 1 (2.2) of the patients and secondary patency was 88.6% at 1 year and
Arteriovenous fistula 1 (2.2) 80.9% at 2 years.
Note—Total number of patients was 41; total number of limbs involved was 45. During the follow-up, three patients with technical failure un-
SFA = superficial femoral artery, ATA = anterior tibial artery, PTA = posterior derwent major amputation. Twelve of the patients underwent
tibial artery. minor amputation because of established necrosis of the toes.
There were no mortalities. Amputation-free survival and limb sal-
defined as amputation above the ankle level, and minor amputa- vage rates were 93.3% at 1 year and 2 years. Kaplan-Meier curves
tion was defined as amputation below the ankle level. of amputation-free survival, limb salvage, primary patency, and
Complications are classified according to descriptions of the So- secondary patency are presented in Figure 2.
ciety of Interventional Radiology Clinical Practice Guidelines [24].
Discussion
Statistical Analysis TAO is a disabling peripheral artery disease with poor progno-
Descriptive statistics were evaluated as mean, SD, median, fre- sis and high risk of amputation [25]. The underlying pathologic
quency, percentage, minimum, and maximum. The difference of mechanism is still not understood, and thus there is no consensus
Rutherford scores before and after the procedure were evaluated on the most effective treatment method. The only proven effec-
with Wilcoxon test. A p value less than 0.05 was considered sta- tive treatment is cessation of tobacco use [1, 5, 7]. Nevertheless, in
tistically significant. Limb salvage, amputation-free survival, and patients with critical limb ischemia, cessation of smoking only is
patency rates were evaluated with Kaplan-Meier analysis. not enough to avoid limb loss, and further intervention is needed
for better outcomes [8].
Results Treatment of TAO is challenging. Various additional treatment
A total of 45 limbs were treated in 41 patients. Target vessels methods have been used. Pharmacologic treatment with prosta-
for angioplasty were superficial femoral artery in 10 limbs, popli- cyclin and prostaglandin analogs has been reported to improve
teal artery in 17, anterior tibial artery in 30, posterior tibial artery pain and ulcer healing in previous studies, but these studies did
in 32, peroneal artery in 11, and plantar artery in 21. For each pa- not report long-term outcomes such as limb salvage and ampu-
tient, the mean number of treated runoff arteries was 1.6 ± 0.49 tation-free survival, and data are still lacking to support their rou-
(SD) (range, 1–2 arteries). Retrograde pedal access was used in tine usage [9, 10, 13]. Lumbar sympathectomy and spinal cord
nine cases because of failure of lesion crossing via the antegrade stimulation have been used to decrease high sympathetic activ-
path. Technical success was achieved in 37 of 45 procedures ity causing vasospasm in TAO. Sympathectomy improves blood
(82.2%). The reasons for technical failure were inability of reentry flow by decreasing peripheral resistance of the regional blood
to true lumen in five cases and insufficient response to balloon vessels; however, this method of treatment is beneficial only in
angioplasty in three cases, which were assumed to be because of the short term (approximately 6 months) before symptoms re-
vasospasm. Before treatment, 13 limbs had no runoff artery and turn and sexual and autonomic dysfunction are reported [26, 27].
32 limbs had one runoff artery. After treatment, one limb ended Although spinal cord stimulation has promising results, it has not
with no runoff artery, 10 limbs ended with one runoff artery, 29 been not studied in randomized controlled studies [11, 12]. A re-
limbs ended with two runoff arteries, and five limbs ended with cent study of endovascular sympathectomy with radiofrequency
three runoff arteries. ablation showed clinical improvement in TAO without sexual and
There were no major procedural complications. Eight minor autonomic dysfunction [28].
complications were reported. In six of the procedures there was In this study, we presented our single-center experience of en-
vasospasm, three of which were treated with intraarterial nitro- dovascular treatment in TAO. Our midterm results showed that
4 AJR:216, February 2021
E n d o v a s c u l a r Tr e a t m e n t o f C r i t i c a l L i m b I s c h e m i a
1.0 1.0
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
0.8 0.8
Amputation-Free Survival
0.6 0.6
Limb Salvage
0.4 0.4
0.2 0.2
Survival function Survival function
0 Censored 0 Censored
0 500 1000 1500 2000 0 500 1000 1500 2000
Time Since Treatment (d) Time Since Treatment (d)
A B
1.0 1.0
0.8 0.8
Secondary Patency
Primary Patency
0.6 0.6
0.4 0.4
0.2 0.2
Survival function Survival function
0 Censored 0 Censored
0 500 1000 1500 2000 0 500 1000 1500 2000
Time Since Treatment (d) Time Since Treatment (d)
C D
Fig. 2—Kaplan-Meier curves for patients with thromboangiitis obliterans.
A–D, Graphs show Kaplan-Meier curves demonstrating amputation-free survival (A), limb salvage (B), primary patency (C), and secondary patency (D).
endovascular treatment of TAO is feasible, and in patients with traindications, we administered nitroglycerin before starting the
critical limb ischemia it has a potential to lower amputation rates procedure and used hydrophilic 0.035-inch guidewires initially in
when used in addition to smoking cessation. Smoking cessation lesion crossing if possible, and then 0.018-inch guidewires in the
is key to the long-term treatment of TAO. In our clinic, patients are distal crural segment. Dedicated total occlusion guidewires cause
instructed to quit smoking or any form of tobacco use at least 1 severe vasospasm in this group of patients and should be avoid-
month before any endovascular procedure. We believe that this ed during the crossing of the lesions. Second, because of the ad-
adequately prevents inflammatory reactions in the blood vessels. vanced involvement of distal runoff arteries, lesion crossing and
Endovascular treatment of TAO presents several challenges. reentry into the true lumen at the distal level (which is crucial for a
First, there is an increased tendency of vasospasm during catheter successful procedure) is difficult. Although technically successful
and guidewire manipulation. For that reason, if there were no con- lesion crossing and reentry may be achieved, response to balloon
AJR:216, February 2021 5
Uyanik et al.
angioplasty may be inadequate. Prolonged balloon inflation and compromise future endovascular treatment of the effected vessel,
incremental increase in pressure and balloon size may overcome and revision of the surgery has higher morbidity.
this adversity, but in some cases all efforts may be fruitless. Last, The only prospective study that has reported on endovascular
depending on the pathologic mechanism of TAO, there may be treatment of TAO was by Ghoneim et al. [28]. In that study, the au-
an increased risk of acute thrombosis and embolic events during thors reported the outcomes of 39 patients; 15 were managed en-
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
endovascular therapy and thrombolytic treatment, which may in- dovascularly, 15 were treated medically, five were treated surgical-
crease morbidity, mortality, and hospital stay. ly, and four were treated by sympathectomy. They reported lower
Few studies have investigated the efficiency of endovascular technical success and patency rates than previous studies and
treatment of TAO. Graziani et al. [19] first reported a case series comparable limb salvage rates. There was no comparison between
of 17 patients in 2012, and they achieved a technical success of the treatment groups, and the study was lacking randomization.
95% and a limb salvage rate of 100% with no complications. The Surgical revascularization has reported acceptable limb sal-
authors proposed that endovascular treatment is a feasible, safe, vage rates between 91.4% and 95% [14–16, 29–31]. The most lim-
and effective treatment method in TAO. Another study by Moda- iting issues with surgical revascularization are the absence of a
ghegh and Hafezi [22] reported a technical success rate and limb suitable venous conduit and a patent distal runoff artery for anas-
salvage rate of 92% in 13 patients. Kawarada et al. [21] treated 20 tomosis. Unfortunately, most patients with TAO lack these two
lower limbs and five upper limbs endovascularly in 20 patients conditions because of extensive runoff artery disease and coex-
with TAO. They also investigated intravascular ultrasound find- isting phlebitis migrans [16]. In addition, the patency of bypass
ings in these patients and found some typical findings correlat- conduits is lower in TAO than atherosclerotic disease, resulting
ing the underlying pathologic changes in the vessel wall. Similar in a need for early reintervention and morbidity. Although the
to other studies, they achieved a limb salvage rate of 100% with reported patency rates were longer than for endovascular ther-
high technical success (96%). They reported an acute thrombosis apy, surgical revascularization carries more complication rates
in one patient that was treated endovascularly with administra- than endovascular therapy and requires surgical reintervention
tion of thrombolytics. There were 12 reocclusions in their series because early failure increases the morbidity of patients. For this
and seven required reintervention. In the largest case series of 44 reason, in addition to the feasibility of surgical intervention in pa-
patients by Kim et al. [3], technical success was reported in 80%, tients, it is still debatable whether endovascular treatment or sur-
and the limb salvage rate was reported to be 86.7% at 5 years. gical treatment is the most suitable option for revascularization
Fifteen patients needed reintervention during follow-up, and re- in patients with TAO. Two studies compare results of endovascu-
intervention and amputation-free survival was 62.7% at 5 years. lar treatment and surgery in the literature. Lee et al. [4] compared
In the present study, we achieved an 82.2% technical success 33 consecutive cases with critical limb ischemia (22 endovascular
rate, which is lower than most of the previous reports. In three procedures vs 11 inframalleolar bypass surgeries). Limb salvage
cases there was evident vasospasm that did not respond to va- rates and patency rates were both similar between the groups.
sodilators, and in five cases an inability to reenter true lumen at The other study by Ye et al. [32] again compared endovascu-
the plantar artery was the cause of technical failure. We believe lar treatment and bypass surgery results and showed that both
our lower technical success rate may be a result of extensive in- limb-salvage rate and major reintervention rates were similar in
volvement of the plantar artery in the patient population. The both groups. In both studies, primary patency was significantly
limb salvage rate in our study was 93.3% and compatible with the longer and ulcer healing was faster in the surgery group than en-
mentioned reports. Firat and Igus [18] reported a case series of 28 dovascular treatment group. However, these results must be in-
patients who underwent 40 procedures, and they achieved a limb terpreted carefully because patients in the surgery group were
salvage rate of 96.8% at 2 years. They also reported primary pa- also candidates for endovascular treatment, but patients in the
tency rates of 84%, 78%, and 75% at 1, 2, and 3 years, respectively. endovascular group were not candidates for surgery. This reflects
In eight patients in whom antegrade lesion crossing failed, retro- that the baseline involvement of the endovascular group was
grade transpedal access was used and they showed that a com- more advanced so the comparison is of two unmatched groups.
bined antegrade and retrograde approach is feasible in techni- There are some limitations in this study. First is the retrospective
cally challenging cases of TAO. Similarly, Kaçmaz et al. [20] used a design of the study with a limited number of patients. This case se-
retrograde crossing technique in two cases in their study. We used ries study lacks a control group so there is no comparison of endo-
retrograde access in nine patients in whom antegrade crossing of vascular treatment with medical therapy or other interventions. In
the occlusion failed, and we achieved success in all of them. Retro- addition, an approach with the combination of other therapies to
grade access is promising in suitable patients, but it is not always endovascular recanalization may achieve better outcomes.
possible because of occlusion of the classic pedal access sites at
ankle level. Puncture of the occluded vessels may be an option in Conclusion
TAO, and we used the technique in one of our patients. Previous Endovascular treatment of TAO is a feasible and viable option
studies reported reintervention rates between 25–35% because for patients with critical limb ischemia who are not candidates
of reocclusion [3, 18, 19, 21, 22]. There was a need for reinterven- for bypass surgery with acceptable limb salvage rates and clinical
tion in 14 patients in the present study and they were all treated improvement of symptoms. There is still a lack of data comparing
successfully with an endovascular approach similar to the previ- endovascular therapy with other treatment methods, and pro-
ous reports. Repeatability of endovascular treatment may be ac- spective randomized studies are needed to determine the clin-
cepted as superior to surgery because surgery has a potential to ical benefits of endovascular therapy.
6 AJR:216, February 2021
E n d o v a s c u l a r Tr e a t m e n t o f C r i t i c a l L i m b I s c h e m i a
References bypass in Buerger’s disease. Ann Vasc Surg 1994; 8:248–257
1. Olin JW. Thromboangiitis obliterans (Buerger’s disease). N Engl J Med 2000; 18. Firat A, Igus B. Endovascular recanalization of thromboangiitis obliterans
343:864–869 (Buerger’s disease) in twenty-eight consecutive patients and combined
2. Vijayakumar A, Tiwari R, Kumar Prabhuswamy V. Thromboangiitis obliterans antegrade-retrograde intervention in eight patients. Cardiovasc Intervent
Downloaded from www.ajronline.org by Goteborgs Universitetsbibl. on 12/16/20 from IP address 130.241.16.16. Copyright ARRS. For personal use only; all rights reserved
(Buerger’s disease): current practices. Int J Inflamm 156905 [Epub 2013 Sep 11] Radiol 2019; 42:820–828
3. Kim DH, Ko YG, Ahn CM, et al. Immediate and late outcomes of endovascu- 19. Graziani L, Morelli L, Parini F, et al. Clinical outcome after extended endo-
lar therapy for lower extremity arteries in Buerger disease. J Vasc Surg 2018; vascular recanalization in Buerger’s disease in 20 consecutive cases. Ann
67:1769–1777 Vasc Surg 2012; 26:387–395
4. Lee CY, Choi K, Kwon H, et al. Outcomes of endovascular treatment versus 20. Kaçmaz F, Kaya A, Keskin M, et al. Clinical outcomes of extended endovas-
bypass surgery for critical limb ischemia in patients with thromboangiitis cular recanalization of 16 consecutive Buerger’s disease patients. Vascular
obliterans. PLoS One 2018; 13:e0205305 2019; 27:233–241
5. Shionoya S. Diagnostic criteria of Buerger’s disease. Int J Cardiol 1998; 21. Kawarada O, Kume T, Ayabe S, et al. Endovascular therapy outcomes and
66(suppl 1):S243–S245; discussion, S247 intravascular ultrasound findings in thromboangiitis obliterans (Buerger’s
6. Ketha SS, Cooper LT. The role of autoimmunity in thromboangiitis obliter- disease). J Endovasc Ther 2017; 24:504–515
ans (Buerger’s disease). Ann N Y Acad Sci 2013; 1285:15–25 22. Modaghegh MS, Hafezi S. Endovascular treatment of thromboangiitis ob-
7. Papa MZ, Rabi I, Adar R. A point scoring system for the clinical diagnosis of literans (Buerger’s Disease). Vasc Endovascular Surg 2018; 52:124–130
Buerger’s disease. Eur J Vasc Endovasc Surg 1996; 11:335–339 23. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Ra-
8. Sugimoto M, Miyachi H, Morimae H, et al. Fate of ischemic limbs in patients diology clinical practice guidelines. J Vasc Interv Radiol 2003; 14:S199–
with Buerger’s disease based on our 30-year experience: does smoking have S202
a definitive impact on the late loss of limbs? Surg Today 2015; 45:466–470 24. Börner C, Heidrich H. Long-term follow-up of thromboangiitis obliterans.
9. The European TAO Study Group. Oral iloprost in the treatment of thrombo- Vasa 1998; 27:80–86
angiitis obliterans (Buerger’s disease): a double-blind, randomised, place- 25. Chander J, Singh L, Lal P, Jain A, Lal P, Ramteke VK. Retroperitoneoscopic
bo-controlled trial. Eur J Vasc Endovasc Surg 1998; 15:300–307 lumbar sympathectomy for Buerger’s disease: a novel technique. JSLS
10. Bozkurt AK, Köksal C, Demirbas MY, et al.; Turkish Buerger’s Disease Re- 2004; 8:291–296
search Group. A randomized trial of intravenous iloprost (a stable prosta- 26. Nesargikar PN, Ajit MK, Eyers PS, Nichols BJ, Chester JF. Lumbar chemical
cyclin analogue) versus lumbar sympathectomy in the management of sympathectomy in peripheral vascular disease: does it still have a role? Int
Buerger’s disease. Int Angiol 2006; 25:162–168 J Surg 2009; 7:145–149
11. Donas KP, Schulte S, Ktenidis K, Horsch S. The role of epidural spinal cord stim- 27. Tang J, Gan S, Zheng M, Jiang Y, Feng Y, Miao J. Efficacy of endovascular
ulation in the treatment of Buerger’s disease. J Vasc Surg 2005; 41:830–836 radiofrequency ablation for thromboangiitis obliterans (Buerger’s dis-
12. Fabregat G, Villanueva VL, Asensio JM, De Andrés J, López D. Spinal cord ease). Ann Vasc Surg 2017; 42:78–83
stimulation for the treatment of Buerger disease: a report on 3 cases. Clin 28. Ghoneim BM, Karmota AG, Abuhadema AM, et al. Management of Buerg-
J Pain 2011; 27:819–823 er’s disease in endovascular era. Int J Angiol 2019; 28:173–181
13. Fiessinger JN, Schäfer M. Trial of iloprost versus aspirin treatment for criti- 29. Ates A, Yekeler I, Ceviz M, et al. One of the most frequent vascular diseases
cal limb ischaemia of thromboangiitis obliterans. The TAO Study. Lancet in northeastern of Turkey: thromboangiitis obliterans or Buerger’s disease
1990; 335:555–557 (experience with 344 cases). Int J Cardiol 2006; 111:147–153
14. Bozkurt AK, Beşirli K, Köksal C, et al. Surgical treatment of Buerger’s dis- 30 Ohta T, Ishioashi H, Hosaka M, Sugimoto I. Clinical and social consequences
ease. Vascular 2004; 12:192–197 of Buerger disease. J Vasc Surg 2004; 39:176–180
15. Dilege S, Aksoy M, Kayabali M, Genc FA, Senturk M, Baktiroglu S. Vascular re- 31. Shindo S, Matsumoto H, Ogata K, et al. Arterial reconstruction in Buerger’s
construction in Buerger’s disease: is it feasible? Surg Today 2002; 32:1042–1047 disease: by-pass to disease-free collaterals. Int Angiol 2002; 21:228–232
16. Sasajima T, Kubo Y, Inaba M, Goh K, Azuma N. Role of infrainguinal bypass 32. Ye K, Shi H, Qin J, et al. Outcomes of endovascular recanalization versus
in Buerger’s disease: an eighteen-year experience. Eur J Vasc Endovasc Surg autogenous venous bypass for thromboangiitis obliterans patients with
1997; 13:186–192 critical limb ischemia due to tibioperoneal arterial occlusion. J Vasc Surg
17. Sasajima T, Kubo Y, Izumi Y, Inaba M, Goh K. Plantar or dorsalis pedis artery 2017; 66:1133–1142
APPENDIX 1: Shionoya Criteria
• Smoking history
• Onset before the age of 50 years
• Infrapopliteal occlusions
• Upper extremity involvement or phlebitis migrans
• Absence of atherosclerotic risk factors other than smoking
AJR:216, February 2021 7
You might also like
- An Occurrence of Steinstrasse in (SIRS)Document14 pagesAn Occurrence of Steinstrasse in (SIRS)M Ali AdrianNo ratings yet
- Assocoition of KidneyDocument9 pagesAssocoition of KidneyM Ali AdrianNo ratings yet
- The Effect of Preoperative UreteralDocument7 pagesThe Effect of Preoperative UreteralM Ali AdrianNo ratings yet
- Admin, 085 - 799 - Ivan Master Worung - GalleyDocument5 pagesAdmin, 085 - 799 - Ivan Master Worung - GalleyM Ali AdrianNo ratings yet
- Ultrasound Guided Involuntary Motion Compensation of Kidney StonesDocument7 pagesUltrasound Guided Involuntary Motion Compensation of Kidney StonesM Ali AdrianNo ratings yet
- PDF Slide Ca RektiDocument14 pagesPDF Slide Ca RektiM Ali AdrianNo ratings yet
- Aca 19 225Document6 pagesAca 19 225M Ali AdrianNo ratings yet
- Acute Upper Limb Ischemia As A Complication of Tunneled Hemodialysis Catheter Placement Via The Right Internal Jugular VeinDocument3 pagesAcute Upper Limb Ischemia As A Complication of Tunneled Hemodialysis Catheter Placement Via The Right Internal Jugular VeinM Ali AdrianNo ratings yet
- Thyroglossal Duct Cyst Carcinoma WithDocument8 pagesThyroglossal Duct Cyst Carcinoma WithM Ali AdrianNo ratings yet
- Intrathoracic Hibernoma: Brief Communication Communication AbrégéeDocument2 pagesIntrathoracic Hibernoma: Brief Communication Communication AbrégéeM Ali AdrianNo ratings yet
- PIIS0003497514019808Document6 pagesPIIS0003497514019808M Ali AdrianNo ratings yet
- The Importance of Mean Platelet Volume To Lymphocyte Ratio in Predicting Atrial Fibrillation After Coronary Bypass OperationsDocument5 pagesThe Importance of Mean Platelet Volume To Lymphocyte Ratio in Predicting Atrial Fibrillation After Coronary Bypass OperationsM Ali AdrianNo ratings yet
- Research ArticleDocument6 pagesResearch ArticleM Ali AdrianNo ratings yet
- Laparoscopic Cholecystectomy Perioperative Management: An UpdateDocument6 pagesLaparoscopic Cholecystectomy Perioperative Management: An UpdateM Ali AdrianNo ratings yet
- Jurnal BEDocument6 pagesJurnal BEM Ali AdrianNo ratings yet
- PTX 3Document9 pagesPTX 3M Ali AdrianNo ratings yet
- Renal CancerDocument7 pagesRenal CancerM Ali AdrianNo ratings yet
- The Quality of Life in The Treatment of Maxillofacial Fractures Using Open Reduction: A Prospective StudyDocument5 pagesThe Quality of Life in The Treatment of Maxillofacial Fractures Using Open Reduction: A Prospective StudyM Ali AdrianNo ratings yet
- Pone 0228947Document12 pagesPone 0228947M Ali AdrianNo ratings yet
- International Journal of SurgeryDocument6 pagesInternational Journal of SurgeryM Ali AdrianNo ratings yet
- Medicine: Epidemiological Pattern of Maxillofacial Fractures in Northern ChinaDocument7 pagesMedicine: Epidemiological Pattern of Maxillofacial Fractures in Northern ChinaM Ali AdrianNo ratings yet
- @MedicalBooksStore 2017 VascularDocument951 pages@MedicalBooksStore 2017 VascularM Ali AdrianNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Minimental QuirogaDocument12 pagesMinimental QuirogaLeonardo Rodrigo Vivanco PazNo ratings yet
- 8BreathingExercises Calmhappyhealthy PDFDocument10 pages8BreathingExercises Calmhappyhealthy PDFlunn100% (1)
- Psychiatric Rating Scales: Sajatovic and Ramirez, 2006Document11 pagesPsychiatric Rating Scales: Sajatovic and Ramirez, 2006Putri Tamara DasantosNo ratings yet
- WMBVGVBWMB GJG: Shinamycin LaDocument1 pageWMBVGVBWMB GJG: Shinamycin LaSharfina Akter BithiNo ratings yet
- Nursing Physical AssessmentDocument2 pagesNursing Physical AssessmentJenNo ratings yet
- Coass V-Ear TumorsDocument32 pagesCoass V-Ear TumorsErshine Villany100% (1)
- LaryngitisDocument29 pagesLaryngitisL'deo Dwi InsaniNo ratings yet
- Letter - Physical ExamDocument6 pagesLetter - Physical ExamLaurence LesmorasNo ratings yet
- 10.daftar PustakaDocument4 pages10.daftar PustakaInka SitiNo ratings yet
- CardiomyopathyDocument17 pagesCardiomyopathysarguss1450% (2)
- Glycerol BlankingDocument4 pagesGlycerol BlankingDiah Puspita RiniNo ratings yet
- Discharge PlanDocument2 pagesDischarge PlanHannah ChiuNo ratings yet
- Anthony Ortiz: Education ObjectiveDocument2 pagesAnthony Ortiz: Education Objectiveapi-404285262No ratings yet
- CAMBRADocument5 pagesCAMBRASarah KahilNo ratings yet
- Checklists For Heat and Cold ApplicationDocument5 pagesChecklists For Heat and Cold ApplicationJay Harold Cordero PanlilioNo ratings yet
- Chapter 22, PharmacologyDocument25 pagesChapter 22, PharmacologyDurgaNadellaNo ratings yet
- Seborrheic Dermatitis: Fitzpatrick Dermatology in General Medicine 7 EditionDocument19 pagesSeborrheic Dermatitis: Fitzpatrick Dermatology in General Medicine 7 EditionAdhe RidhoNo ratings yet
- Effect of Diet On Type 2 Diabetes MellitusDocument14 pagesEffect of Diet On Type 2 Diabetes MellitusPriya bhattiNo ratings yet
- Chemo Stability Chart - LtoZDocument59 pagesChemo Stability Chart - LtoZdr.am.s3edNo ratings yet
- StoppFrail PaperDocument8 pagesStoppFrail PaperEric LiangNo ratings yet
- Mumbai Claim FormDocument5 pagesMumbai Claim FormsunsangraNo ratings yet
- Gengigel For GingivitisDocument7 pagesGengigel For GingivitisIka Dewi RahmawatiNo ratings yet
- Nursing Research ReportDocument15 pagesNursing Research Reportapi-546467833No ratings yet
- Drug Abuse: Short-Term EffectsDocument2 pagesDrug Abuse: Short-Term EffectsYeonjin ChoiNo ratings yet
- Sample CollectionDocument8 pagesSample CollectionwillowmaecayabyabNo ratings yet
- Chapter 22Document6 pagesChapter 22Danielle ShullNo ratings yet
- MINT Lift Easy MINT Lift Fine: Handling BookDocument16 pagesMINT Lift Easy MINT Lift Fine: Handling BookEstemalatya FahrikayahanNo ratings yet
- NSQHS Standards Fact Sheet Standard 7Document2 pagesNSQHS Standards Fact Sheet Standard 7Annette LowryNo ratings yet
- Treatment of Jwara Roga With Ayurvedic HerbsDocument2 pagesTreatment of Jwara Roga With Ayurvedic HerbsSN WijesinheNo ratings yet
- Curs IRADocument124 pagesCurs IRAFloreaAndreiNo ratings yet