Professional Documents
Culture Documents
Methacholine Challenge Test
Uploaded by
Hafiz Hari NugrahaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Methacholine Challenge Test
Uploaded by
Hafiz Hari NugrahaCopyright:
Available Formats
Methacholine
Challenge Test (MCT)
What is Methacholine Challenge Test (MCT)?
The methacholine challenge test (MCT) is used to measure whether your
airways narrow after inhaling a specific provoking agent – methacholine
in this instance. The degree of resultant airway narrowing is dependent on
each individual’s susceptibility and the airway narrowing will be assessed
objectively by measuring the changes in lung function before and after
inhalation of the methacholine in progressively larger doses. Increased
airway hyper-responsiveness is usually a hallmark feature of asthma.
Why do I need this test?
Your doctor may use this test to establish
the diagnosis of asthma if initial lung
function tests did not show any
conclusive results. If you have a
history of asthma, your doctor may
recommend doing a MCT from time to
time to assess how well your asthma
medication is working. Please clarify with
your doctor if you are unsure why you
need to undergo this test.
How do I prepare myself for the test?
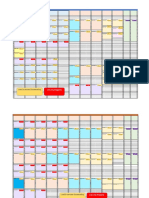
How long before the test? Avoid:
2 hours Heavy meals
8 hours Alcohol
Day of test • Smoking
• Exercise
• Wearing tight clothing that will restrict your
breathing or movement
The doctor will advise you on the medications to temporarily discontinue
before the test as they can affect the test results. Please clarify with your
doctor if you are on any other medication for your breathing that is not listed
here so that they can advise you accordingly.
1 | Methacholine Challenge Test (MCT)
Inhaled medication containing only corticosteroids such as Beclomethasone,
Budesonide, Fluticasone, Triamcinolone, or Mometasone may be continued.
Please confirm with your doctor if there is any need to stop these
medications.
How long before Avoid: Examples
the test?
8 hours Inhaled beta-agonists Albuterol or Salbutamol
– Short acting (Ventolin)
12 hours Inhaled anticholinergics Ipratropium bromide
– Short acting (Atrovent)
Oral Theophylline Nuelin
(Non-SR)
24 hours Oral Theophylline (SR) Nuelin SR
48 hours Inhaled beta-agonists Formoterol
– Long acting (e.g. Symbicort, Flutiform)
Salmeterol (e.g. Seretide)
Inhaled beta-agonists Indacaterol
– Ultra-long acting (Onbrez & Ultibro Breezhaler)
Olodaterol
(Striverdi & Spiolto Respimat)
Vilanterol
(Anoro, Relvar & Trelegy
Ellipta)
1 week Inhaled anticholinergics Glycopyrronium
– Long acting (Seebri & Ultibro Breezhaler)
Tiotropium
(Spiriva & Spiolto Respimat)
Umeclidinium
(Incruse, Anoro & Trelegy
Ellipta)
Aclidinium
Methacholine Challenge Test (MCT) | 2
How is the test done?
Our clinical physiologist will guide you through the three stages of the MCT,
estimated to take about 30 to 45 minutes.
1. You will need to undergo a baseline lung function assessment first. You
will be asked to use maximal effort to blow out and breathe in through the
equipment. This step helps to ensure that your baseline lung function is
not too low to proceed with the rest of the test.
2. You will then be asked to inhale progressively larger doses of
methacholine, which is tasteless and odourless, from a machine. The lung
function assessment will be repeated after each dose to see if there is
significant change in your lung function from the baseline readings. If
there is no significant change, you will be asked to inhale the next dose of
methacholine, for up to 5 doses. If there is a significant change, you will
not be asked to inhale the next dose of methacholine.
3. You will be given inhaled bronchodilator medication to re-open your
airways if there is significant airway narrowing during the course of the
test. Lung function assessments will be repeated thereafter to ensure that
your lungs and breathing have returned to normal.
The entire procedure is estimated
to take about 30-45mins.
3 | Methacholine Challenge Test (MCT)
What are the possible risks from this test?
This is generally a safe test.
You may feel breathless or light-headed for a short while (usually lasting
only for a few seconds) after the test is performed as the lung function
assessments require some exertion during the breathing manoeuvres.
If your airways tighten after inhalation of methacholine, you may experience
symptoms similar to an asthmatic attack, such as chest tightness, shortness
of breath, wheezing or coughing. These symptoms are usually mild, transient,
and you will be given inhaled bronchodilator medication to relieve your
symptoms. There will be no symptoms if your airways do not tighten.
Please inform the clinical physiologist if you experience any discomfort
during the test. Generally, it would be extremely rare to have persistent
symptoms or develop new symptoms after the test. The test is done in
our Pulmonary Function Laboratory with trained staff and there will be
appropriate medical assistance available whenever necessary.
The risks and complications
listed here are not intended to
be exhaustive. There may be
uncommon risks or those that are
specifically applicable to you due
to individual risk factors. Please
check with your doctor if you have
any concerns about this.
Methacholine Challenge Test (MCT) | 4
What can I expect after the test?
After the test, you can resume the medication(s) that you have stopped
for the purpose of the test unless your doctor had given you other prior
instructions. You can also go back to your usual diet and activities.
You will be given an appointment to see your doctor who will discuss the test
results with you and answer any questions that you may have about
your condition.
Are there alternatives to MCT?
Clinical guidelines recommend that asthma should be diagnosed based
on presence of typical asthma symptoms and objective evidence of airflow
limitation, usually obtained from lung function assessments.
Our doctor may recommend other alternatives to MCT in certain situations
(e.g. if you are deemed unsuitable to undergo MCT).
Pre- and Post-Bronchodilator Spirometry
Our doctor may recommend pre-and post-bronchodilator spirometry (which
is another form of lung function test) to elicit a significant response to an
inhaled bronchodilator medication to confirm diagnosis of asthma. This test
may be repeated if needed.
Other forms of airway provocation tests
Other methods such as exercise challenge test can produce similar effects of
inducing airway narrowing. However, the effects are dependent on individual
susceptibility and may be considered in certain situations (e.g. if your
respiratory symptoms are solely exercise-induced).
5 | Methacholine Challenge Test (MCT)
Is there a chance that I may not be able to have
the test?
You may not be able to undergo the test in certain scenarios such as the
following:
If you are pregnant or nursing
If you had a recent heart attack or stroke within the last 3 months
If you have a known blood vessel problem
If you have uncontrolled high blood pressure
If your baseline lung function prior to inhalation of the methacholine is
too low
If you are allergic to methacholine
Please inform your doctor if you have any of these conditions that may
preclude you from undergoing the test, so that alternative plans or tests
can be arranged.
Can I take the test if I am not feeling well?
You should not proceed with the test if you have a fever, cold, respiratory
tract infection or feeling unwell. Generally, you are advised to take the test
one month after recovery for a more accurate test result.
Please call the CGH Appointment Centre at 6850 3333 to reschedule your
appointment. Do check with your doctor if you have any concerns.
Methacholine Challenge Test (MCT) | 6
2 Simei Street 3 Singapore 529889
Tel: 6788 8833 Fax: 6788 0933
Reg No 198904226R
CGH Appointment Centre
For appointments and enquiries,
please call: (65) 6850 3333
Operating hours:
8.30 am to 8.00 pm (Monday to Friday)
8.30 am to 12.30 pm (Saturday & Sunday)
Closed on Public Holiday
For more information, please visit www.cgh.com.sg
facebook.com/ChangiGeneralHospital
Information is valid as of October 2020 and subject to revision without prior notice.
All information provided within this publication is intended for general information and is provided
on the understanding that no surgical and medical advice or recommendation is being rendered.
Please do not disregard the professional advice of your doctor.
You might also like
- Albuterol VentolinDocument3 pagesAlbuterol VentolinKristi WrayNo ratings yet
- ECT PharmacologyDocument29 pagesECT PharmacologySangkaran KumarNo ratings yet
- NURS 5 Clinical Medications WorksheetsDocument1 pageNURS 5 Clinical Medications WorksheetsMichael KuzbytNo ratings yet
- ECT - Patient LeafletDocument4 pagesECT - Patient LeafletSarah GrixtiNo ratings yet
- Allergy Skin Testing Patient Consent FormDocument3 pagesAllergy Skin Testing Patient Consent FormchinchouNo ratings yet
- Solved Second Sessional Question Paper of Pharmacology-II Theory (BP503T)Document12 pagesSolved Second Sessional Question Paper of Pharmacology-II Theory (BP503T)ANUJ KUMARNo ratings yet
- Abdulaziz Hisham Al GainDocument69 pagesAbdulaziz Hisham Al GainMostafa ElbagouryNo ratings yet
- Preparation of Drug Profile of AtropineDocument8 pagesPreparation of Drug Profile of AtropineSufian AhmadNo ratings yet
- Endo Case No. 3Document2 pagesEndo Case No. 3Deinielle Magdangal RomeroNo ratings yet
- Lsuhsc Nursing Licensed Personnel Inpatient RN Pharmacology Exam InstructionsDocument10 pagesLsuhsc Nursing Licensed Personnel Inpatient RN Pharmacology Exam Instructionskellly100% (1)
- Chemical Pathology UnitDocument22 pagesChemical Pathology UnitLee Yann Na IbrahimNo ratings yet
- Contraception 14 April 2014Document74 pagesContraception 14 April 2014danielNo ratings yet
- Pharm RemediationDocument5 pagesPharm RemediationAudrey WatsonNo ratings yet
- NLN Pharmacology Study Guide Final 6-3-2013Document65 pagesNLN Pharmacology Study Guide Final 6-3-2013الأغا محمد زكارنة100% (2)
- PST OpDocument90 pagesPST OpBSRT1A BERBANO, IAN JEWEL M.No ratings yet
- NLN Pharmacology Study GuideDocument65 pagesNLN Pharmacology Study GuideLauraysha McMillanNo ratings yet
- Pharmacology Made EasyDocument43 pagesPharmacology Made EasyGauthaman KarunakaranNo ratings yet
- Meptin® Swinghaler®: Dry Powder InhalerDocument9 pagesMeptin® Swinghaler®: Dry Powder InhalerYusuf HadiNo ratings yet
- Operation UeueueueDocument210 pagesOperation UeueueueBSRT1A BERBANO, IAN JEWEL M.No ratings yet
- trelegy-ellipta-epar-product-information_enDocument44 pagestrelegy-ellipta-epar-product-information_enandricmilovan888No ratings yet
- 2020 Respiratory Drugs DentistryDocument27 pages2020 Respiratory Drugs DentistryVisayan Alliah GailNo ratings yet
- Codiene-Acetaminophen Tylenol 3Document1 pageCodiene-Acetaminophen Tylenol 3Kristi WrayNo ratings yet
- Boston Food Allergy Center Immunotherapy Info SheetDocument3 pagesBoston Food Allergy Center Immunotherapy Info SheetAndres ANo ratings yet
- Step 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionFrom EverandStep 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionNo ratings yet
- Ventilator Management ProtocolDocument15 pagesVentilator Management Protocolihtisham1No ratings yet
- Clen GuideDocument19 pagesClen Guidemilad bigdeliNo ratings yet
- Psychiatric Informed Consent - Augmented PsychotherapyDocument6 pagesPsychiatric Informed Consent - Augmented PsychotherapyNicolas Berasain OcaresNo ratings yet
- Fasting and Thyroid Test ResultsDocument4 pagesFasting and Thyroid Test ResultsRosNo ratings yet
- The 2 Keys to Continued Growth and Size Post CycleDocument9 pagesThe 2 Keys to Continued Growth and Size Post CycleJohnnie DahiyaNo ratings yet
- Generic Name, Dose, Indications, Side Effects, Nursing Care, Rationale, Patient Teaching (38Document7 pagesGeneric Name, Dose, Indications, Side Effects, Nursing Care, Rationale, Patient Teaching (38Joanna Marie Datahan EstomoNo ratings yet
- Single-Dose Oral Phenytoin in GTC Status EpilepticusDocument19 pagesSingle-Dose Oral Phenytoin in GTC Status EpilepticusPutri Senna RahayuNo ratings yet
- Auspar Valdoxan PDFDocument87 pagesAuspar Valdoxan PDFPandroshaNo ratings yet
- Cardiopulmonary Exercise Testing (CPET)Document2 pagesCardiopulmonary Exercise Testing (CPET)frandi wirajayaNo ratings yet
- NR 446 Week 6 ATI Weekly Tips Mental HealthDocument16 pagesNR 446 Week 6 ATI Weekly Tips Mental HealthChristine LansdownNo ratings yet
- (Why Med Ordered) Contraindications/warnings/interactionsDocument6 pages(Why Med Ordered) Contraindications/warnings/interactionsJita SinghNo ratings yet
- Anorectal Physiology - Information For Patients: Why Do I Need This Test?Document2 pagesAnorectal Physiology - Information For Patients: Why Do I Need This Test?soudrackNo ratings yet
- Symph A To Mimetic SDocument27 pagesSymph A To Mimetic Sjl frusaNo ratings yet
- Use of methotrexate to treat pregnancy of unknown location and ectopic pregnancy_NBT002435Document12 pagesUse of methotrexate to treat pregnancy of unknown location and ectopic pregnancy_NBT002435autokucamatijevic1No ratings yet
- Drug LipitorDocument1 pageDrug LipitorSrkocherNo ratings yet
- Prescribed Drug Study Dosage and AdministrationDocument9 pagesPrescribed Drug Study Dosage and AdministrationKaren GonzalesNo ratings yet
- Pulmonary Function TestDocument9 pagesPulmonary Function TestMarivic DianoNo ratings yet
- SLP Thyroid Function TestDocument9 pagesSLP Thyroid Function TestMuhd ArsyadNo ratings yet
- SAT and SBT Protocol DefinitionsDocument11 pagesSAT and SBT Protocol DefinitionsI C JNo ratings yet
- Drug Study ArraDocument5 pagesDrug Study ArraPaul ManaloNo ratings yet
- RESPIRATORY CASE - Sol - GargantielDocument4 pagesRESPIRATORY CASE - Sol - GargantielMaryglen GargantielNo ratings yet
- 4 Min MiraclesDocument8 pages4 Min MiraclesmanncsageNo ratings yet
- Protocol for managing pesticide poisoningDocument6 pagesProtocol for managing pesticide poisoningJesicca SNo ratings yet
- ThyroidectomyDocument3 pagesThyroidectomyhahahahaaaaaaaNo ratings yet
- Chapter-3 Drug ProfileDocument2 pagesChapter-3 Drug ProfileRajivNo ratings yet
- Airway Management in TransportDocument46 pagesAirway Management in TransportArtha PutuNo ratings yet
- Dr. Thomas - Tatalaksana ESODocument38 pagesDr. Thomas - Tatalaksana ESOsuryaniNo ratings yet
- Case StudyDocument3 pagesCase StudyAJ BayNo ratings yet
- Exercise Stress Test: Presented By: Ns. Rifa'atul MahmudahDocument14 pagesExercise Stress Test: Presented By: Ns. Rifa'atul MahmudahRifa'atul MahmudahNo ratings yet
- Buteyko Breathing ExercisesDocument14 pagesButeyko Breathing Exercisesvolonterneboja100% (4)
- Intravenous Anesthetic Agents: by Miss Maidah MehtabDocument49 pagesIntravenous Anesthetic Agents: by Miss Maidah MehtabLuqman QadirNo ratings yet
- The Practical Book For Pharmacology & Physiology Laboratory ExperimentsDocument11 pagesThe Practical Book For Pharmacology & Physiology Laboratory ExperimentstiruchanurNo ratings yet
- APSRLive OndemandDocument2 pagesAPSRLive OndemandHafiz Hari NugrahaNo ratings yet
- ReadmeDocument1 pageReadmeHafiz Hari NugrahaNo ratings yet
- Toman'S Tuberculosis: Questions AND AnswersDocument351 pagesToman'S Tuberculosis: Questions AND AnswerschandanNo ratings yet
- JCM 09 02847 v2Document13 pagesJCM 09 02847 v2Hafiz Hari NugrahaNo ratings yet
- Rapid Progression To Acute Respiratory Distress Syndrome: Review of Current Understanding of Critical Illness From Coronavirus Disease 2019 (COVID-19) InfectionDocument11 pagesRapid Progression To Acute Respiratory Distress Syndrome: Review of Current Understanding of Critical Illness From Coronavirus Disease 2019 (COVID-19) InfectionVeloz RedNo ratings yet
- EBUS for Diagnosing and Staging Lung CancerDocument7 pagesEBUS for Diagnosing and Staging Lung CancerGio Mari MarcialNo ratings yet
- PIIS0012369220343142Document4 pagesPIIS0012369220343142Hafiz Hari NugrahaNo ratings yet
- Management of Respiratory Distress Syndrome Due To COVID-19 InfectionDocument6 pagesManagement of Respiratory Distress Syndrome Due To COVID-19 InfectionHafiz Hari NugrahaNo ratings yet
- Recent Advances in Diagnostic Bronchoscopy: Philip G. Ong, Labib G. Debiane, Roberto F. CasalDocument10 pagesRecent Advances in Diagnostic Bronchoscopy: Philip G. Ong, Labib G. Debiane, Roberto F. CasalHafiz Hari NugrahaNo ratings yet
- Early Versus Late Tracheal Intubation in COVID-19 Patients: A Pro-Con Debate Also Considering Heart-Lung InteractionsDocument28 pagesEarly Versus Late Tracheal Intubation in COVID-19 Patients: A Pro-Con Debate Also Considering Heart-Lung InteractionsHafiz Hari NugrahaNo ratings yet
- JTD 08 10 2758Document7 pagesJTD 08 10 2758Hafiz Hari NugrahaNo ratings yet
- Histamine and its receptorsDocument34 pagesHistamine and its receptorsHafiz Hari NugrahaNo ratings yet
- Drug-Resistant TB TreatmentDocument120 pagesDrug-Resistant TB TreatmentNadzhin15No ratings yet
- JTD 09 07 2178Document8 pagesJTD 09 07 2178Hafiz Hari NugrahaNo ratings yet
- Transbronchial Needle Aspiration Versus.6Document6 pagesTransbronchial Needle Aspiration Versus.6Hafiz Hari NugrahaNo ratings yet
- Nama Produk Harga Variasi Stok Total Stok S M L XL: All SizeDocument1 pageNama Produk Harga Variasi Stok Total Stok S M L XL: All SizeHafiz Hari NugrahaNo ratings yet
- WHO Consolidated On Tuberculosis: GuidelinesDocument106 pagesWHO Consolidated On Tuberculosis: GuidelinesHafiz Hari NugrahaNo ratings yet
- Nomor SampelDocument2 pagesNomor SampelHafiz Hari NugrahaNo ratings yet
- ScoreDocument8 pagesScoreHafiz Hari NugrahaNo ratings yet
- Sample Descriptions of OT AssessmentsDocument10 pagesSample Descriptions of OT AssessmentsHafiz Hari NugrahaNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaHafiz Hari NugrahaNo ratings yet
- AbstractDocument1 pageAbstractHafiz Hari NugrahaNo ratings yet
- FdgtyDocument1 pageFdgtyHafiz Hari NugrahaNo ratings yet
- Acute Appendicitis in Children - Diagnostic Imaging - UpToDateDocument28 pagesAcute Appendicitis in Children - Diagnostic Imaging - UpToDateHafiz Hari NugrahaNo ratings yet
- Distribusi Paritas IbuDocument10 pagesDistribusi Paritas IbuHafiz Hari NugrahaNo ratings yet
- Rsup Dr. Mohammad Hoesin Palembang Follow Up Dokter Muda IkkkDocument1 pageRsup Dr. Mohammad Hoesin Palembang Follow Up Dokter Muda IkkkHafiz Hari NugrahaNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- CV DiseaseDocument2 pagesCV DiseaseHafiz Hari NugrahaNo ratings yet
- Infection Control NHS PolicyDocument12 pagesInfection Control NHS PolicyYahya Salem100% (1)
- Biochemistry Practical RGKSUDocument43 pagesBiochemistry Practical RGKSUmuhammad umer abdul moizNo ratings yet
- Understand LDL Cholesterol BetterDocument4 pagesUnderstand LDL Cholesterol BetterhealthcheckupNo ratings yet
- Presention SdaDocument13 pagesPresention SdaBikhu MatreNo ratings yet
- 2015 - Chronic Neck Pain Alters Muscle Activation Patterns To Sudden Movements (D. Falla)Document11 pages2015 - Chronic Neck Pain Alters Muscle Activation Patterns To Sudden Movements (D. Falla)romiromiromi123No ratings yet
- ECG MastersDocument644 pagesECG MastersJinnasit Tee100% (2)
- Sepsis Case StudiesDocument5 pagesSepsis Case StudiesRia Arcane0% (2)
- Deteksi Vibrio Multplex PCRDocument7 pagesDeteksi Vibrio Multplex PCRZulfana Fikru SifaNo ratings yet
- Presentation For Music Therapy CourseDocument13 pagesPresentation For Music Therapy CourseRodney HarrisNo ratings yet
- Rett Syndrome1Document4 pagesRett Syndrome1api-544862486No ratings yet
- Status of Fisheries and Aquaculture in the PhilippinesDocument11 pagesStatus of Fisheries and Aquaculture in the PhilippinesBAGaraNo ratings yet
- Nurse Collaborates With Jimmy to Reach Anxiety GoalDocument162 pagesNurse Collaborates With Jimmy to Reach Anxiety GoalAnn Claudette SyNo ratings yet
- Diabetes Mellitus FP NotebookDocument11 pagesDiabetes Mellitus FP NotebookDibyendunarayan BidNo ratings yet
- Pecinan 2016Document6 pagesPecinan 2016Faisar Dhamar KusumaNo ratings yet
- Telesom NewsLetter Issue 16 Mar 2013Document35 pagesTelesom NewsLetter Issue 16 Mar 2013Telesom CompanyNo ratings yet
- Supplements Who Needs Them?: A Behind The Headlines Report June 2011Document34 pagesSupplements Who Needs Them?: A Behind The Headlines Report June 2011Sa AsNo ratings yet
- Intravenous FluidsDocument19 pagesIntravenous Fluidsblack pink in ur area 21100% (1)
- Mhpss South Sudan HntpoDocument12 pagesMhpss South Sudan HntpoAnonymous BOsRleBNo ratings yet
- Trichuriasis 2Document18 pagesTrichuriasis 2Analeah MalayaoNo ratings yet
- J Parenter Enteral Nutr - 2017 - Worthington - When Is Parenteral Nutrition AppropriateDocument54 pagesJ Parenter Enteral Nutr - 2017 - Worthington - When Is Parenteral Nutrition AppropriateToño ZsucaritasNo ratings yet
- Doctor's Vaccine Safety WarrantyDocument4 pagesDoctor's Vaccine Safety WarrantyBrett AmbroseNo ratings yet
- Dermatology Slides - Introduction To Clinical DermatologyDocument34 pagesDermatology Slides - Introduction To Clinical DermatologyAzry Mustapa100% (1)
- Makalah B Inggris 2010Document36 pagesMakalah B Inggris 2010Adhi PradanaNo ratings yet
- Gastrointestinal MedicationsDocument3 pagesGastrointestinal MedicationsEllie ELLNo ratings yet
- Blood and Blood SpatterDocument24 pagesBlood and Blood Spatterapi-302019977No ratings yet
- IBM Explorys Therapeutic Datasets DeliveredDocument3 pagesIBM Explorys Therapeutic Datasets DeliveredCci Chu SetifNo ratings yet
- CCL-2 Product Sheet - HeLaDocument7 pagesCCL-2 Product Sheet - HeLaaricheNo ratings yet
- Abnormal Swallow Infantile and AdultDocument2 pagesAbnormal Swallow Infantile and Adultfinix33No ratings yet
- Drug Metabolism: A Pharmaceutical Industry PerspectiveDocument20 pagesDrug Metabolism: A Pharmaceutical Industry PerspectiveAndhika Bintang MahardhikaNo ratings yet
- Mindoro child with recurrent fever, chills, sweating has malariaDocument16 pagesMindoro child with recurrent fever, chills, sweating has malariaJiezl Abellano Afinidad100% (2)