Professional Documents
Culture Documents
Key Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation Problems
Key Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation Problems
Uploaded by
ay254Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Key Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation Problems
Key Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation Problems
Uploaded by
ay254Copyright:
Available Formats
Key recommendations for clinical practice
• Anaphylaxis is a potentially life-threatening allergic reaction.
• Recognise anaphylaxis based on:
o sudden onset and rapid progression of symptoms
o Airway and/or Breathing and/or Circulation problems
o skin and/or mucosal changes (flushing, urticaria, angioedema) –
but these may be absent in up to 20% of cases.
The diagnosis is supported if a patient has been exposed to an allergen known to
affect them.
• Treat life-threatening features, using the Airway, Breathing, Circulation,
Disability, Exposure (ABCDE) approach.
• Adrenaline is the first-line treatment for anaphylaxis. Give intramuscular (IM)
adrenaline early (in the anterolateral thigh) for Airway/Breathing/Circulation
problems.
o A single dose of IM adrenaline is well-tolerated and poses minimal
risk to an individual having an allergic reaction. If in doubt, give IM
adrenaline.
o Repeat IM adrenaline after 5 minutes if Airway/Breathing/Circulation
problems persist.
• Intravenous (IV) adrenaline must be used only in certain specialist
settings, and only by those skilled and experienced in its use.
o IV adrenaline infusions form the basis of treatment for refractory
anaphylaxis: seek expert help early in patients whose respiratory and/or
cardiovascular problems persist despite 2 doses of IM adrenaline.
• Follow the National Institute for Health and Care Excellence (NICE) guideline
for the assessment and referral of patients suspected to have had
anaphylaxis. Specifically:
o All patients should be referred to a specialist clinic for allergy
assessment.
o Offer patients (or, if appropriate, their parent and/or carer) an
appropriate adrenaline injector as an interim measure before the
specialist allergy assessment (unless the reaction was drug-
induced).
o Patients prescribed adrenaline auto-injectors (and/or their
parents/carers) must receive training in their use, and have an
emergency management or action plan
• Further research is needed to better identify and treat patients at greatest
risk of severe anaphylaxis.
Emergency treatment of anaphylaxis | May 2021
o Anaphylaxis reactions should be reported to the UK Anaphylaxis
Registry at www.anaphylaxie.net (to register, email
anaphylaxis.registry@ic.ac.uk).
o Follow guidance for reporting and debriefing of adverse events.
Emergency treatment of anaphylaxis | May 2021
Summary of changes from previous guideline
This guideline replaces the previous guideline from Resuscitation Council UK (RCUK):
Emergency treatment of anaphylactic reactions – Guidelines for healthcare providers
(originally published January 2008, annotated July 2012 with links to NICE guidance).1
• Greater emphasis on intramuscular adrenaline to treat anaphylaxis, and repeated
after 5 minutes if Airway/Breathing/Circulation problems persist.
• A specific dose of adrenaline is now included for children below 6 months of
age.
• Increased emphasis on the importance of avoiding sudden changes in posture
and maintaining a supine position (or semi-recumbent position if that makes
breathing easier for the patient) during treatment.
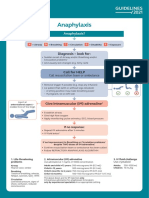
• There are 2 algorithms:
o Initial treatment of anaphylaxis, with emphasis on repeating the dose
of adrenaline after 5 minutes and giving an IV fluid bolus if
Airway/Breathing/Circulation problems persist.
o Treatment of refractory anaphylaxis, defined as anaphylaxis where
there is no improvement in respiratory or cardiovascular symptoms
despite two appropriate doses of IM adrenaline.
• IV fluids are recommended for refractory anaphylaxis, and must be given
early if hypotension or shock is present.
• Antihistamines are considered a third-line intervention and should not be used to
treat Airway/Breathing/Circulation problems during initial emergency treatment.
o Non-sedating oral antihistamines, in preference to chlorphenamine,
may be given following initial stabilisation especially in patients with
persisting skin symptoms (urticaria and/or angioedema).
• Corticosteroids (e.g. hydrocortisone) are no longer advised for the routine
emergency treatment of anaphylaxis.
• New guidance is offered relating to the duration of observation following
anaphylaxis, and timing of discharge.
This updated guideline has been developed according to the GRADE Evidence to
Decision (EtD) frameworks for adoption, adaptation, and de novo development of
trustworthy recommendations (GRADE-ADOLOPMENT).2 The evidence tables and
conclusions have been peer-reviewed and published.3
Emergency treatment of anaphylaxis | May 2021
Download this algorithm:
https://www.resus.org.uk/sites/default/files/2021-04/Anaphylaxis%20algorithm%202021.pdf
Emergency treatment of anaphylaxis | May 2021
Download this algorithm:
https://www.resus.org.uk/sites/default/files/2021-04/Refractory%20anaphylaxis%20algorithm%202021.pdf
Emergency treatment of anaphylaxis | May 2021
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- OET WRITING ConnectorsDocument3 pagesOET WRITING Connectorsmarine gns88% (8)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- WCLC2021 Abstract Book - Final 16310719983133277Document1,066 pagesWCLC2021 Abstract Book - Final 16310719983133277Shawn Gaurav Jha100% (1)
- Anxiety Disorders: Presented byDocument38 pagesAnxiety Disorders: Presented byRudra prasad Sahu100% (1)
- ALL in 1Document1 pageALL in 1Shawn Gaurav JhaNo ratings yet
- Neet PG Result All India CandidatesDocument2,919 pagesNeet PG Result All India CandidatesShawn Gaurav Jha0% (1)
- RO-DBT in Service 11 18Document24 pagesRO-DBT in Service 11 18Ela Barszcz50% (2)
- Cardiac Rhythms and DysrhythmiasDocument14 pagesCardiac Rhythms and DysrhythmiasShawn Gaurav Jha100% (1)
- Tinnitus Important History Questions and Interpretation. For Use by Physicians, Gps and CliniciansDocument1 pageTinnitus Important History Questions and Interpretation. For Use by Physicians, Gps and CliniciansShawn Gaurav JhaNo ratings yet
- Discussing DNACPR: Before You Begin .Document5 pagesDiscussing DNACPR: Before You Begin .Shawn Gaurav JhaNo ratings yet
- START Info For Potential New Regional Centres 21Document9 pagesSTART Info For Potential New Regional Centres 21Shawn Gaurav JhaNo ratings yet
- Mechanical Thrombectomy For Acute Ischaemic Stroke: An Implementation Guide For The UKDocument99 pagesMechanical Thrombectomy For Acute Ischaemic Stroke: An Implementation Guide For The UKShawn Gaurav JhaNo ratings yet
- Stroke Information Pack: Information For Patients, Families and CarersDocument56 pagesStroke Information Pack: Information For Patients, Families and CarersShawn Gaurav JhaNo ratings yet
- Neet PG 2019 - DR AzamDocument17 pagesNeet PG 2019 - DR AzamShawn Gaurav Jha75% (4)
- ADT Form Sample Prescription ChartDocument6 pagesADT Form Sample Prescription ChartShawn Gaurav JhaNo ratings yet
- E-Portfolio Guidance For Foundation Year 1 Doctors: August 2015 - July 2016Document17 pagesE-Portfolio Guidance For Foundation Year 1 Doctors: August 2015 - July 2016Shawn Gaurav JhaNo ratings yet
- Anaphylaxis Algorithm 2021Document1 pageAnaphylaxis Algorithm 2021Shawn Gaurav JhaNo ratings yet
- BTS Guideline For Long Term Macrolide UseDocument35 pagesBTS Guideline For Long Term Macrolide UseShawn Gaurav JhaNo ratings yet
- Hospital Passport Template Example From South West London Access To Acute GroupDocument9 pagesHospital Passport Template Example From South West London Access To Acute GroupShawn Gaurav JhaNo ratings yet
- Respiratory System 2Document8 pagesRespiratory System 2Shawn Gaurav JhaNo ratings yet
- Optho Diams QDocument5 pagesOptho Diams QShawn Gaurav JhaNo ratings yet
- You May Find Useful Some of My Pathology Notes. Markos Greece. You May Find Useful Some of My Pathology Notes. Markos Greece. (10557)Document3 pagesYou May Find Useful Some of My Pathology Notes. Markos Greece. You May Find Useful Some of My Pathology Notes. Markos Greece. (10557)Shawn Gaurav JhaNo ratings yet
- PELVIS, Student FileDocument52 pagesPELVIS, Student FileShawn Gaurav JhaNo ratings yet
- Newborn InfantDocument62 pagesNewborn InfantShawn Gaurav Jha100% (1)
- A. Perform A Standard AppendectomyDocument2 pagesA. Perform A Standard AppendectomyShawn Gaurav JhaNo ratings yet
- A. Perform A Standard AppendectomyDocument2 pagesA. Perform A Standard AppendectomyShawn Gaurav JhaNo ratings yet
- Sound Energy A3 Poster in White Blue Illustrative StyleDocument1 pageSound Energy A3 Poster in White Blue Illustrative StyleAdiniy FikriyahNo ratings yet
- Definisi-Klasifikasi EpilepsiDocument40 pagesDefinisi-Klasifikasi Epilepsianita tri hastuti100% (1)
- Bio-Psycho-Social Formulation and Differential Diagnosis: Psychiatric Assessment With Helen M. Farrell, M.DDocument12 pagesBio-Psycho-Social Formulation and Differential Diagnosis: Psychiatric Assessment With Helen M. Farrell, M.DJ.C. GarzaNo ratings yet
- Dechoker Post Market Surveillance Report - Five Alleged UK Care Home Choking Rescue CasesDocument15 pagesDechoker Post Market Surveillance Report - Five Alleged UK Care Home Choking Rescue CasesACD SkepticNo ratings yet
- QM Episode 1 TranscriptDocument5 pagesQM Episode 1 TranscriptCandice NolanNo ratings yet
- The 13 Disability Categories Under IDEADocument4 pagesThe 13 Disability Categories Under IDEADavid SchneiderNo ratings yet
- Dissociative DisorderDocument44 pagesDissociative DisorderKiaraMaeRhiasNo ratings yet
- Addison & Cushing - Patho, Signs & TreatmentDocument1 pageAddison & Cushing - Patho, Signs & TreatmentVishalNo ratings yet
- Final Year Mbbs (2019-23) Question PapersDocument66 pagesFinal Year Mbbs (2019-23) Question PapersklenNo ratings yet
- InsomniaDocument4 pagesInsomniagladisNo ratings yet
- Test Report: Hemogram Test Name Units Results Bio. Ref. IntervalDocument19 pagesTest Report: Hemogram Test Name Units Results Bio. Ref. Intervalcs2015ok77No ratings yet
- Special Circumstances Guidelines ALSDocument19 pagesSpecial Circumstances Guidelines ALSHamzaMasoodNo ratings yet
- Bibliography Gian NewDocument2 pagesBibliography Gian NewDranlie LagdamenNo ratings yet
- Orthostatic Hypotension Medical StudentsDocument21 pagesOrthostatic Hypotension Medical StudentsRobMarvinNo ratings yet
- Newborn Screening, An Update: Learning ObjectivesDocument37 pagesNewborn Screening, An Update: Learning ObjectivesKrenz CatiboNo ratings yet
- Jama Marcus 2023 PG 220048 1676478924.2109Document1 pageJama Marcus 2023 PG 220048 1676478924.2109Mahmoud AbouelsoudNo ratings yet
- Instruction: Differentiate ARF and ARDS. Explain BrieflyDocument2 pagesInstruction: Differentiate ARF and ARDS. Explain BrieflyDuchess Juliane Jose MirambelNo ratings yet
- Safe T PDFDocument2 pagesSafe T PDFGd SuarantaNo ratings yet
- Midterm Exam: The Following Are Related To The Different Lobes of The CerebrumDocument13 pagesMidterm Exam: The Following Are Related To The Different Lobes of The CerebrumasdfasdfsadfsaNo ratings yet
- Literature ReviewDocument5 pagesLiterature Reviewapi-548937898No ratings yet
- Multiple Choice Questions For Part IVDocument18 pagesMultiple Choice Questions For Part IVTarek MohsenNo ratings yet
- Psychological-Assessment ScriptDocument9 pagesPsychological-Assessment ScriptCasas, Jo-an Pauline A.No ratings yet
- CACHO NCP NeuromuscularDocument3 pagesCACHO NCP NeuromuscularJaymee CachoNo ratings yet
- Bipolar DisorderDocument349 pagesBipolar Disorders3149521696100% (1)
- Unstable Angina - Cardiovascular Disorders - MSD Manual Professional EditionDocument1 pageUnstable Angina - Cardiovascular Disorders - MSD Manual Professional EditionboynextdoorpkyNo ratings yet
- NCP Preeclampsia TissueperfusionDocument2 pagesNCP Preeclampsia TissueperfusionMichael Angelo Seña100% (2)
- Actaapa 2020 39Document7 pagesActaapa 2020 39gretaNo ratings yet