Professional Documents
Culture Documents
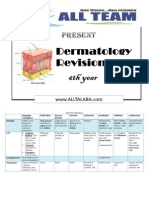
Dermatology in Tables
Dermatology in Tables
Uploaded by
Ahmed Mansour100%(1)100% found this document useful (1 vote)
17 views7 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
17 views7 pagesDermatology in Tables
Dermatology in Tables
Uploaded by
Ahmed MansourCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
Bacterial infections
Impetigo Folliculitis Sycosis Furncle Carbuncle Erythiplas Cellulitis erythrasma
contagiosa barbae
Etiology Cocci + poor Stap aureus ( Staph aureus ( Infection of Diabetes Inflammation INF of lower Corynebactrium
hygiene & infection of folliculitis of lower part of of upper dermis ( staph minutissimum (
moisture or upper part of the beard area the hair dermis ( B aureus – strpt DM )
scabies & hair follicle ) follicle hemolytic stept pyogenes
pediculosis )
C/P 1- Ordinary Follicular Follicular Red papules Multiple deep Erythrematous As erythiplas Reddish brown
2- Bullous : new pustules pustules & boils open on tender swollen but illdefined patches in
born – staph papules surface by area with border interriginous
infection – fistulae sharp border areas /
may be fatal + Give red
3- Circinate : constitutional S fluorescence
extension of with wood’s
ordinary light
4- Ulcerative :
crust & scars
Complications Post streptococcal Lymphedema
glomerulonephritis
Treatment Topical antiseptics Same Same Same Incision & Erythromycin Aggressive Topical AB and
+ topical drainage + AB antifungal ?
antibiotics and systemic AB systemic AB
systemic if sever
Viral infections
Herpes simplex Herpes zoster Warts Mollascum contagiosum
Aetioligy HSV I : herpes libialis Varicella Zoster virus Human papilloma virus Pox virus
HSV II : herpes progenitalis
C/P 1- HSV I : Vesilces along distribution of a 1- Common warts : Dome shaped papule with
a. superficial vesicles sensory nerve + local LNs verroucus papules central umblication and
perioroficail → ulcers → enlargement – leave scar – give 2- Plane warts : flat topped white chessy material if
swollen gums & permenant immunity papules squeezed – can be sexual
lymphadenopathy + 3- Filiform warts :
constitutional manifestations DANGEROUS in : peduculated
b. recurrent attacks in lips & face Bilateral 4- Digitiform warts : finger
less sever Old age like
c. ocular type Gangrenous 5- Planter warts : foot =
d. herpitic witlow : in fingers Recurrent tender – grow inward
very painful 6- Genital warts : moist
2- HSV II : vesicles on genitals foul smelling in MM &
and ulcers / if pregnant → CS skin
Complications 2ry infections / eye cimolications / Eye complication ? post herpitic Oncogenicity ( cervical cancer )
CNS : encephalitis / erythema neuralgia
multiforme / cancer cervix
Treatment Antiseptic lotions 1- Topical : drying AS lotion 1- Cautery : electro- cryo – Cauterization
Acyclovir cream 5 times / Acyclovir cream laser – chemical
daily 5 days 2- Systemic : Acyclovir 800 2- Podophyllon resin in
IDU for eye lesions mg 5 X 7 - Analgesics alcohol : for veneral
Acyclovir tab 200 mg 5 X 5 3- Radiotherapy
4- Autosuggestion
Fungal infections
Dermatophytes Yeasts
Tinea capitis Tinea circinata Tinea pedis Other types Pityriasis versicolor Candidiasis
Cause Trichophyta & Trichophyta & Trichophyta & 1- Tinea cruris : Malassezia furfur Candida albicans
microspore microspore epidermophyta scrotum not the pathogenic form
involed of pityrrosporum
2- Tinea axillaris orbiculare
C/P 1- Scaly type :child – Annular patches Sodden white 3- Tinea barbae Macule hypo or 1- Cutaneous
bal patch with with active edge and macerated skin with 4- Tinea mannum : hyper pigmented candidiasis :
scales healing centre – bad dour between in palm with fine scales in a. Intertrigo :
2- Black dot : hair itching is common toes 5- Tinea uguium : upper chest arms – i. Axilla & groin
breaks leave dots on exposed surfaces onchomycosis → In summer ii. Eriosio
3- Kerion : also adult thickened interdigitalis
with boggy greenish nails mastocytica
swelling & iii. Angular
pustules → chelitis
cicatricial alopecia iv. Napkin
4- Favus : diffuse dermatitis
loss of hair with b. Paronychia : nail
mousy odour fold tender – nail
yellow crusts → corrugated
cicatricail alopecia 2- Mucosalcandidiasis :
oral thrush – vulvo
vaginitis - balanitis
Diagnosis 1- Wood’s : DD : herald patch Wood’s light gives
green yellow
2- LM Parker ink stain :
3- Culture on spagitti & meatballs
saburoud appearance
Treatment Topical alone is Topical antifungal 2 1- Tincture iodine 1-Systemic : 1- Topical : castellani
useless daily + systemic 1% ketoconazole paint – nystatin
( ketoconazole grisofulvin for 3 W 2- Systemic 200X10 oint
shampoo + antifunal in 2-Topical : Na 2- Systemic :
griseofulvin tab for 2 sever cases hyposulphide – mycostatin oral
months imidazole – zinc drops – Azoles –
pyrithione – white amphotericin B in
field – tincture sever
iodine
Scaly erythematous lesions
Psoriasis Lichen planus Discoid Lupus erythematousus Pityriasis rosea
Etiology Lack of UV rays - Psychological Chronic scaly erythematous Considered exanthematous
- Hemolytic infection - Liver disease eruption in skin reaction for upper respiratory
- Hypocalcemia - Sunrays viral infection ( HHV 6-7 )
- Pregnancy - Antimalairial – gold
- Trauma / psychogenic
C/P Erythematous papule with Flat topped polyangular Erythematous plaques + adherent Herald patch ( outer
shiny scales – lossely adherent violaceous itchy papules with scales + dilated pilosebaceous erythematous zone –
– bleed on removal ( Auspiz ) adherent scales in flexor areas orifices ( stippling ) + intermediate scaly one –
with sever pruritis telangectesia + thin atrophic scar healing center ) parallel to rib
→ cicatricial alopecia in sun / 2ry eruption give
exposed areas chrismats tree appearance &
jacket with short sleeves
Clinical types 1- Psoriasis vulgaris 1- Ordinary LP 1- Ordinary type
a. Skin : in extensors – back 2- Actinic LP : in sun exposed 2- Inverted type : occur
b. Scalp psoriasis area in summer distal
c. Nail psoriasis : bi;aterla 3- Mucosal : reticulate network 3- Abortive type : only
pitting hyperkeratotic nail – ulcerative laesion – herald
d. Flexural type : scaling is precancerous 4- Papular type : more
absent 4- LP of the scalp : cicatricai elevated
2- Erythrodermic alopecia 5- Flexural type
3- Arthropathic
4- Pustular : sterile pustules
Treatment 1- Local : coal tar – Anthralin 1- Antihistaminics 1- Sun screens 1- PT reassurance
0.5% - corticosteroids – 2- Steroids & aalcylic loacally 2- Systemic photoprotectives ( 2- Avoid hot baths
salicylic acid 5% - 3- Steroids – retinoids and chloroquine ) 3- Calamine lotion
calcipotriol – PUVA – laser cyclosporine systemically 3- Corticosteroids ( local – 4- Oral antihistaminics ,
2- Systemic : for extensive 4- Actinic : sunscreens 0 systemic – intralesional ) topical corticosteroids and
psoriasis : Methotrexate – chloroquine 200mg /day UVB
retinoids – cyclosporine – 5- Mucosal : steroids – acitrtin –
corticosteroids – PUVA oral chloroquine
Allergic Dermatoses
Eczema urticaria Erythema multiforms Drug eruptions
May be genetic in types as atopic & 1- Exogenous : foods as fish- 1- Genetic factors Allergy to the drug
allergic contact dermatitis chocolate / drugs as penicillin 2- Infections : HSV
injected or ingested / pollens
3- DRUGS : NSAIDs
2- Endogenous : infection –
parasites – SLE – lymphoma – 4- Autoimmune : SLE
pregnancy 5- Malignancy : lymph
1- Contact dermatitis : 1- Ordinary urticaria 1- EM minor : only 1- Urticarial &
a. 1ry irritant dermatitis : any individual 2- Facticious : very mild – limmted to skin – no angioedema
b. Allergic contact dermatitis : type IV
in genetic susceptile
follow trauma or mild mucosal 2- Erythroderma (
2- Discoid eczema : well defined 3- Cholinergic : itchy involvement – no exfoliative dermatitis )
3- Atopic eczema : genetic with FH sensation after sweating systemic involvement 3- Photosensitive drug
a. Infantile : on cheeks & hands with wheals on scalp –neck 2- EM major : extensive reaction
b. Childhood : on flexures upper chest mucosal and systemic 4- Acneform eruptions
c. Adult : hyperpigmentation &
lichenification
4- Physical : either solar – involvement → death ( steroids )
4- Stasis eczema : venous insufficiency → pressure – cold –heat 5- Fixed drug eruption
edema oozing vesiculation itching 5- Popular : due to insect bite : with sulfonamides &
5- Seborrheic eczema : by malassezia in infants & children / NSAIDs / fixed to the
furfur wheal then papule over it drug & site /
a. Infantile type : scales on scalp &
diaper area
permengnate colored
b. Aadult : from androgens on macule vesicles &
sebaceous glands eruption
-acute eczema : erythema –swelling – Sudden appearance of elevated Primary lesion : iris ( target ) Acute atypical inflammatory
vesicles edematous lesion varies in size lesion erythematous annukar eruptions suside after
-chronic eczema : lichenification & transient for few hours ring with central vesicle / in stoppage of drug
excoriations mucosa : may form painful
HGE bullae & erosions
1- Acute : drying antiseptic lotion & 1- local : cold 3- Local : compresses –
corticosteroid cream witth compresses –calamine calamine lotion –
hydrous base – systemic lotion – steroids steroids – antiseptics
antihistaminics & corticosteroids 2- Systemic : oral 4- Systemic :
2- Chronic : local corticosteroids antihistaminic → antihistaminics –
cream parentral AH → oral steroids – antibiotics
3- Atopic : + topical steroids → parentral 5- Major needs
immunomodulators & UVB steroids → adrenaline hospitalization and
4- Seborrheic : antidandruff SC or IM TTT of complications
shampoo
Vitiligo ALopecia Acne
Etiology Melanocytes are destroyed and disappear 1- Cicatricial : mechanical trauma – Block of follicular opening by KCs –
from epidermis due to : fungal inection DLE – lichen planus dilatation of the lower part – disruption
1- Autoimmune : antimelanocyte AB 2- Non cicatricial : of the epithelium – discharge into the
precipitated by psycho or a. Telogen : postpartum – dermis – inflammation especially with
mechanical trauma nutritional deficiency propionobacterium acnes lead to papule
2- Neurogenic L melanocytotoxic b. Anagen : cytotoxic – pastule nodulocystic lesions
substances from nerve endings retinoids – mercury
3- Chemical : melanocytotoxic c. Familial baldness :
substances from rubber gloves etc overactivity 5alfa reductase
4- UV rays d. Areata : genetic factors –
immunological actors
Types 1- Focal vitilgo 1- Cicatricial 1- Mild ; comedones – no papules
2- Unilateral vitilgo 2- Non cicatricail : telogen effulfium – 2- Moderate : comedones – paules –
3- Generalized vitilgo anagen effluvium – androgenitic pustules
4- Universal vitiligo alopecia – alopecia areata ( patchy – 3- Sever : nodules & cysts
marginaalis – ophiasis – totalis –
universalis )
DD DD : tinea versicolor – pityriasis alba-
postinflammatory hypopigmentation
Tratment 1- Phoyototherapy : PUVA 1- topical ; local irritants – 1- topical : erythromycin lotion –
2- Steroids & immunomodulators corticosteroids cream – PUVA – retinoids – benzyl peroxide –
3- Surgical : punch gafting & tissue minoxidil azelic acid
culture 2- systemic : antidepressant – 2- systemic : antibiotics (tetracycline)
4- camouflage corticosteroids + retinoids – dapsone & steroids (
sever )
The following topics has to be studied from the department book : leprosy & protozoal infections
Prepared by
Mahmoud abdel Ghany Behairy
You might also like
- Dermatology BookDocument479 pagesDermatology BookBharath Magesh100% (2)
- Dermatology in 2hrsDocument222 pagesDermatology in 2hrslarisaP100% (4)
- Physical Examination in DermatologyDocument117 pagesPhysical Examination in Dermatologykykyrisky100% (5)
- Nail Changes: III-A '07 - Derma MegatableDocument21 pagesNail Changes: III-A '07 - Derma MegatableAileen Peña100% (2)
- ABC of DermatologyDocument149 pagesABC of DermatologyAndreea Alexandru100% (15)
- Dermatology: Dr. N. Shear Blaise Clarkson and Elana Lavine, Chapter Editors Harriette Van Spall, Associate EditorDocument44 pagesDermatology: Dr. N. Shear Blaise Clarkson and Elana Lavine, Chapter Editors Harriette Van Spall, Associate EditorKassim Junior Duale100% (2)
- Dermatology Class NotesDocument48 pagesDermatology Class Notesapi-26938624100% (6)
- DermatologyDocument44 pagesDermatologyakufahaba100% (2)
- Dermatology MnemonicDocument16 pagesDermatology MnemonicAhmed Rami100% (1)
- Dermatology NotesDocument59 pagesDermatology NotesAbdullah Matar Badran50% (2)
- Dermatology PDFDocument37 pagesDermatology PDFanabananan100% (2)
- PATHOPHYS - DermatologyDocument19 pagesPATHOPHYS - Dermatologyaagioaa100% (1)
- Viva Questions DermatologyDocument5 pagesViva Questions DermatologyRavva0% (1)
- Dermatology QuestionsDocument8 pagesDermatology QuestionsDrMubashir ShaikhNo ratings yet
- What Is Hybrid Annuity ModelDocument2 pagesWhat Is Hybrid Annuity Modelisquare77No ratings yet
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessFrom EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanNo ratings yet
- Dermatology RevisionDocument7 pagesDermatology RevisionmksharmaaNo ratings yet
- DermatologyDocument6 pagesDermatologygnuzzo100% (3)
- Complete Dermatology NotesDocument41 pagesComplete Dermatology NotesSetlhare Motsamai100% (1)
- Epigenetics and DermatologyFrom EverandEpigenetics and DermatologyQianjin LuRating: 3 out of 5 stars3/5 (1)
- Dermatology - Papulosquamous DisordersDocument34 pagesDermatology - Papulosquamous DisordersskNo ratings yet
- Dermatology Notes for Medical StudentsFrom EverandDermatology Notes for Medical StudentsRating: 4 out of 5 stars4/5 (5)
- Toronto Notes DermatologyDocument52 pagesToronto Notes Dermatologyalphabeta101100% (1)
- Market Research Bags PhilippinesDocument173 pagesMarket Research Bags PhilippinesDaniel Israel Sta Rosa100% (1)
- Dermatology Venereology LeprosyDocument86 pagesDermatology Venereology LeprosyDolamani RohidasNo ratings yet
- Dermatology MemoryDocument7 pagesDermatology MemoryBenny PojerNo ratings yet
- Dermatology Slides - Introduction To Clinical DermatologyDocument34 pagesDermatology Slides - Introduction To Clinical DermatologyAzry Mustapa100% (1)
- Dermoscopy in General DermatologyDocument16 pagesDermoscopy in General DermatologyMaestro JadNo ratings yet
- Dermatology Essentials for Medical AssistantsFrom EverandDermatology Essentials for Medical AssistantsRating: 4 out of 5 stars4/5 (1)
- 0 Basic Principles of DermatologyDocument42 pages0 Basic Principles of Dermatologymusatii100% (1)
- Finance Risk Manager CV TemplateDocument3 pagesFinance Risk Manager CV TemplateАна ЈеленковићNo ratings yet
- Annual Report Powerpoint TemplateDocument40 pagesAnnual Report Powerpoint TemplateTeam Advertising HARDIANNo ratings yet
- Dermatology Atlas for Medical StudentsFrom EverandDermatology Atlas for Medical StudentsRating: 4 out of 5 stars4/5 (6)
- Cards+Against+Paediatric+Dermatology+-+Vickie+Wells+&+Emma+Buxton+ (v1 0)Document146 pagesCards+Against+Paediatric+Dermatology+-+Vickie+Wells+&+Emma+Buxton+ (v1 0)Donna Ricotta100% (1)
- Clinical Dermatology: Differential DiagnosisDocument73 pagesClinical Dermatology: Differential DiagnosisHalim MaherNo ratings yet
- Bhaktamar Stotra in English With MeaningsDocument11 pagesBhaktamar Stotra in English With MeaningsPrachi Sasture100% (2)
- Imaging in DermatologyFrom EverandImaging in DermatologyMichael R. HamblinNo ratings yet
- All Dermatology PicturesDocument140 pagesAll Dermatology PicturesAshty RzgarNo ratings yet
- Clinical Laboratory Investigator: Passbooks Study GuideFrom EverandClinical Laboratory Investigator: Passbooks Study GuideNo ratings yet
- Aesthetic Procedures: Nurse Practitioner's Guide to Cosmetic DermatologyFrom EverandAesthetic Procedures: Nurse Practitioner's Guide to Cosmetic DermatologyNo ratings yet
- Fire Effect On ConcreteDocument19 pagesFire Effect On ConcreteHesham MohamedNo ratings yet
- SDG - PHDocument4 pagesSDG - PHBaby CometNo ratings yet
- Study Guide-Dermatology 2021Document14 pagesStudy Guide-Dermatology 2021Nasir RafieNo ratings yet
- Case Studies in Advanced Skin Cancer Management: An Osce Viva ResourceFrom EverandCase Studies in Advanced Skin Cancer Management: An Osce Viva ResourceNo ratings yet
- An Atlas of the Commoner Skin Diseases: With 153 Plates Reproduced by Direct Colour Photography from the Living SubjectFrom EverandAn Atlas of the Commoner Skin Diseases: With 153 Plates Reproduced by Direct Colour Photography from the Living SubjectRating: 4 out of 5 stars4/5 (4)
- CLINICAL DERMATOLOGY (NXPowerLite)Document119 pagesCLINICAL DERMATOLOGY (NXPowerLite)api-3710926No ratings yet
- Dermatology FinalDocument16 pagesDermatology FinalMelinda100% (2)
- Wood Lamp DermatologyDocument6 pagesWood Lamp Dermatologyindriyanti natasya ayu utami kotten100% (1)
- Dermatology Review NotesDocument8 pagesDermatology Review Notesnmb1986No ratings yet
- Manual of Skin Surgery: A Practical Guide to Dermatologic ProceduresFrom EverandManual of Skin Surgery: A Practical Guide to Dermatologic ProceduresRating: 1 out of 5 stars1/5 (1)
- Intertrigo, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandIntertrigo, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Derma Transcribed Table FormDocument9 pagesDerma Transcribed Table FormGerlyn MarcelinoNo ratings yet
- General Pathology Lecture Eyes and Skin Part IDocument5 pagesGeneral Pathology Lecture Eyes and Skin Part IMae GonzalesNo ratings yet
- Skin PDFDocument13 pagesSkin PDFLanaAmerieNo ratings yet
- Gingival & Periodontal DiseasesDocument9 pagesGingival & Periodontal DiseasesMostafaargoun FifaargounNo ratings yet
- Lichen Planus, Nitidus, Striatus, Sclerosus (Dr. Cruz)Document9 pagesLichen Planus, Nitidus, Striatus, Sclerosus (Dr. Cruz)Riena Austine Leonor NarcillaNo ratings yet
- Job AdvertisementDocument4 pagesJob AdvertisementMulenga DaviesNo ratings yet
- A Survey Report On Foreign Direct Investment in Nepal 2020 21Document28 pagesA Survey Report On Foreign Direct Investment in Nepal 2020 21Bhanu Bhakta AryalNo ratings yet
- EndNote 20 Training Guide For Mac 2023-2Document21 pagesEndNote 20 Training Guide For Mac 2023-2Rosalia EdwardNo ratings yet
- List of Exhibitor - Updated 150622Document3 pagesList of Exhibitor - Updated 150622dipak kambleNo ratings yet
- Stress Management Among Bank Employees: AbstractDocument10 pagesStress Management Among Bank Employees: AbstractJoy SathaNo ratings yet
- AR Ponemon 2009 PCI DSS Compliance SurveyDocument20 pagesAR Ponemon 2009 PCI DSS Compliance SurveyKhadir FayazNo ratings yet
- Reference Card UnixDocument2 pagesReference Card UnixmastersrikanthNo ratings yet
- AF 328 - Lovibond Colour ComparatorDocument1 pageAF 328 - Lovibond Colour Comparatorharsh421No ratings yet
- Final Demo PlanDocument8 pagesFinal Demo PlanRonnel Dela Rosa LacsonNo ratings yet
- Wired Network and Wireless Network.Document11 pagesWired Network and Wireless Network.Desi Manalu AgrifaNo ratings yet
- A4-C7 Engine Aug2013Document2 pagesA4-C7 Engine Aug2013tommy lanyonNo ratings yet
- Sigma 2 and Sigma 2 T Series Operation and Maintenance ManualDocument27 pagesSigma 2 and Sigma 2 T Series Operation and Maintenance ManualMedamriNo ratings yet
- Unit 2 Problem SheetDocument9 pagesUnit 2 Problem SheetTejas ArgulewarNo ratings yet
- Management A Focus On Leaders 2nd Edition Mckee Test BankDocument25 pagesManagement A Focus On Leaders 2nd Edition Mckee Test Bankwalterhubert6rl7mj100% (26)
- Placement of Loading Stations For Electric Vehicles: Allowing Small DetoursDocument9 pagesPlacement of Loading Stations For Electric Vehicles: Allowing Small DetoursTejas GhorpadeNo ratings yet
- Industrial Tour Report On (Four H Apparels LTD) : University of ChittagongDocument34 pagesIndustrial Tour Report On (Four H Apparels LTD) : University of ChittagongMandal SouvikNo ratings yet
- Ship Stability: Damaged Stability of ShipsDocument11 pagesShip Stability: Damaged Stability of ShipsgeorgesagunaNo ratings yet
- Letters To Gabriella - Leon KukkukDocument465 pagesLetters To Gabriella - Leon KukkukLeon KukkukNo ratings yet
- DSCR Ratio With ExampleDocument2 pagesDSCR Ratio With ExampleRanjeet SinghNo ratings yet
- Syllabus For Botany - PGDocument3 pagesSyllabus For Botany - PGSVB 2018No ratings yet
- LG FFH386Document14 pagesLG FFH386Abraham BautistaNo ratings yet
- Paper IDocument75 pagesPaper IThe AnarchistNo ratings yet
- Process-Product Matrix of TeslaDocument5 pagesProcess-Product Matrix of TeslaNavmeen KhanNo ratings yet