Professional Documents
Culture Documents
Clinical Reasoning in Manual Therapy
Uploaded by
Khushboo PakhraniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Reasoning in Manual Therapy
Uploaded by
Khushboo PakhraniCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/21700582
Clinical Reasoning in Manual Therapy
Article in Physical Therapy · January 1993
DOI: 10.1093/ptj/72.12.875 · Source: PubMed
CITATIONS READS
162 9,029
1 author:
Mark Jones
University of South Australia
63 PUBLICATIONS 2,684 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Textbook Clinical Reasoning in Musculoskeletal Practice View project
All content following this page was uploaded by Mark Jones on 17 February 2015.
The user has requested enhancement of the downloaded file.
Clinical Reasoning in Manual Therapy
Clinical reasoning refers to the cognitive processes or thinking used in the evalua- Mark A Jones
tion and management of a patient. In this article, clinical reasoning research
and expert-novice studies are examined to provide insight into the growing un-
derstanding of clinical reasoning and the nature of expertise. Although
bypothetic~deductivemethod of reasoning are used by clinicians at all leuels of
experience, experts appear to poses a superior otganization of knowledge. Ex-
perts oflen reach a diagnosis based on pure pattern recognition of clinical pat-
terns. With a n atypical problem, however, the expert, like the novice, appears to
rely more on bypotheticedeductive clinical reasoning. Five categories of hypothe-
ses are pmposed for physical therapists wing a bypothetico-deductivemethod of
clinical reasoning. A model of the clinical reasoning proces for physical therapists
is presented to bring attention to the hypothesisgeneration, testing, and modijica-
tion that I feel should take place through all aspects of the patient encounter.
Examples of common errors in clinical reasoning are highlighted, and sugges-
tionsfor facilitating clinical reasoning in our students are made. [JonesMA.
Clinical reasoning in manual therapy. Pbys Ther 1992;72:875-884.]
Key Words: Clinical competence, Decision making, Diagnosis, Manual therapy.
There is an increasing demand for observations and the hypotheses are are increasing,'-5 research in clinical
accountability of physical therapists then tested through subsequent data reasoning within physical therapy is
from within the profession as well as collection and modified as a result of still sparse.- Considerable research,
outside, including funding agencies, the outcome of the test. Similarly, however, has been conducted in the
competing health practitioners, and physical therapists should b e taught to area of thinkingkeasoning and the
the increasingly more health con- use clinical reasoning skills in their nature of expertise in such diverse
scious consumer. This demand is met examination and management of fields as medicine, nursing, psychol-
in part by the profession's ongoing patients. But what reasoning skills ogy, artificial intelligence, program-
efforts to teach and conduct scientific should we teach? And how should ming, law, mathematics, engineering,
inquiry with the aim of improving this be balanced against the teaching and physics.S13This article will
and validating physical therapy prac- of knowledge? Understanding the briefly highlight research findings that
tice. Equally important, physical thera- cognitive components of clinical rea- provide insight into the growing un-
pists must apply the methods of scien- soning and in particular the differenti- derstanding of clinical reasoning and
tific inquiry to the examination and ating features between experts and the nature of expertise relevant to
management of patient problems. novices should enable us to critically physical therapy. Although further
Accountability sufferswhen therapists evaluate our own reasoning and de- research is needed to clarify the na-
unquestioningly follow examination sign educational activities to facilitate ture of clinical reasoning, the majority
and treatment routines without con- improved reasoning. of clinical reasoning literature sug-
sidering and exploring alternatives. gests that expert clinicians have a
Scientific reasoning often includes the Although theoretical discussions and highly developed organization of
hypothetico-deductive method, in educational suggestions on aspects of knowledge and use a hypothetico-
which hypotheses are generated from clinical reasoning in physical therapy deductive method in their clinical
reasoning.14 A model of a clinical
reasoning process for physical thera-
-
pists is presented that emphasizes a
MA Jones, PT, is Cwrdinator, Post Graduate Manipulative Physiotherapy Programmes, School of hypothesis testing approach to clinical
Physiotherapy, University of South Australia, North Terrace, Adelaide, South Australia, Australia
5000. reasoning. Clinical reasoning that is
Physical Therapy /Volume 72, Number 12December 1992
hypothetico-deductive will assist clini- In a review of research in medical rected. This finding of the importance
cians in avoiding common errors of clinical reasoning, Feltovich and Bar- of good hypotheses highlights the
reasoning and enhance their recogni- rows15 described hypotheses and data crucial role the clinician's knowledge
tion of clinical patterns and organiza- gathering that were considered in the base has in the clinical reasoning
tion of knowledge. clinical reasoning studies. The vari- process. The importance of knowl-
ables affecting hypothesis generation edge and its organization are also
Cllnkal Reasonlng included the percentage of patient reflected in the seminal work of El-
data items or the time it took to cre- stein and colleagues,16in which clini-
Clinical reasoning can be defined as ation of the first hypothesis. The total cal reasoning performance was shown
the cognitive processes, or thinking number of hypotheses considered to vary greatly across cases. That is,
used in the evaluation and manage- and number of hypotheses actively clinical reasoning is specific to one's
ment of a patient. Other terms includ- considered at any one time were also area of work (eg, orthopedics, neurol-
ing "clinical decision making,"l "clini- studied. There was no difference in ogy, and so forth), dependent on the
cal problem solving,"8 and "clinical any of these variables across different clinician's organization of knowledge
judgrnent"l0 also appear in the litera- specialties or across different levels of in the particular area.
ture and frequently are used inter- experience within the same specialty.
changeably. Clinical decision making Although these hypothesis-related These early medical studies provide
and clinical judgment focus on the variables are common to all clinicians, an overall picture of a clinical reason- ,
diagnostic decision-making aspect of their importance to effective clinical ing process that is hypothetico-
the clinical reasoning process, reasoning was unclear, as none were deductive and universally applied by
whereas problem solving typically consistently predictive of the quality clinicians at all levels of experience.
refers to the steps involved in work- of outcome (eg, correct diagnosis and The process involves collecting and
ing toward a problem solution. Prob- management plan). analyzing information, generating
lem solving also infers the therapist's hypotheses concerning the cause or
aim is to solve the patient's problem. The data-gathering variables centered nature of the patient's condition, in-
Some patient problems, however, are on the general themes of thorough- vestigating or testing these hypotheses
"unsolvable." Our profession's aim is ness, efficiency (ie, important to non- through further data collection, and
to evaluate the patient problem, iden- important information collected), determining the optimal diagnostic
tifylng factors amenable to physical activeness (ie, extent to which data and treatment decisions based on the
therapy to effectively manage the collected are evaluated in relationship data obtained.
problem. The term "clinical reason- to hypotheses being considered to
ing" has broader connotations and is test appropriateness of hypotheses), The Nature of Expertise
used in this article to refer to the and accuracy in interpretation (ie,
cognitive processes used in achieving correctness of interpretations as sup- "Experts" in the early medical educa-
this aim of evaluating and managing porting or not to hypotheses). The tion research were typically those
the patient's problem. value of the data-gathering measures selected by peer nomination, whereas
to reveal important aspects of clinical "novices" were usually students at
Cllnlcal Reasonlng In reasoning were also questionable, as varying levels of their education.lb20
Medlclne: A Unhrersal they did not discriminate among Pate1 and Groen21 have suggested that
Process clinicians from different specialties o r expertise be considered along the
clinicians with different levels of expe- dual continuum of both generic and
A summary of findings from early rience or peer-judged proficiency. specialized knowledge. They define a
medical education research in clinical The importance of these data- novice as an individual who has the
reasoning highlights some universal gathering variables to the products of prerequisite knowledge assumed by
aspects of clinical reasoning and the the rea5oning process was also ques- the domain. A subexpert, according to
significance that the organization of tioned. With the exception of "accura- Pate1 and Groen, is an individual with
one's knowledge has to the differenti- cy in interpretation,"16 no other data- generic knowledge, but inadequate
ation of expert clinicians and novices. gathering variable correlated with specialized knowledge of the domain,
Early medical education studies ana- quality of diagnosis and management and an expert is defined as an individ-
lyzed clinicians' thoughts (eg, percep plan. ual with specialized knowledge of the
tions, interpretations, plans), either domain. These definitions provide
retrospectively as the clinicians The best indicator of the correctness sufficient distinctions for interpreting
thought aloud while being prompted of diagnosis and management plan the expert-novice literature cited in
by a video or audio playback of a was the quality (as judged by expert this article. Although I will not suggest
patient examination just completed or standards) of hypotheses consid- my own expert-novice distinction for
concurrently as the clinicians read a ered.17-20If the appropriate hypothe- physical therapy, I do feel the full
patient's unfolding clinical history. ses were not considered from the range of competencies inherent to
start, the clinician's subsequent inqui- physical therapy including knowledge,
ries would presumably be misdi- interpersonal, manual, and clinical
Physical Therapy /Volume 72, Number 12December 1992
reasoning skills should b e incorpo- radiographs.z8This superior ability to zation of knowledge. Experts make
rated into any expert-novice see meaningful patterns is not the significantly more inferences about
distinction. result of superior perceptual or mem- clinically relevant information and
ory skills; rather it reflects a more chunk information into recognizable
Expert clinicians have a superior highly organized knowledge base.2" patterns.32 Novices make more verba-
organization of knowledge and use a tim recall of the surface features of a
combination of hypothetico-deductive These representations of the problem problem and have less developed and
reasoning and pattern recognition o r will in turn influence the subsequent fewer variations of patterns stored in
forward reasoning.16J1.22 Support for search for a solution. The expert their memory. For example, a novice
the importance of one's organization chess player's conceptualization of the may recall the specific, yet superficial,
of knowledge is available from the game into strengths and vulnerabili- detail that the patient's shoulder hurt
literature of cognitive psychology.23~24 ties lessens the number of appropri- with attempted elevation in early
Experts acquire efficient ways of rep- ate moves to consider. When the activities. Further details such as the
resenting information in their work- physicist characterizes a problem as exact site of pain and position of the
ing memory. Studies of problem an example of a physics law, the law patient's neck, shoulder, and arm may
solving and expert-novice differences itself substantially directs the form not have been sought o r attended to
in fields other than medicine have and application of equations that will if the clinical patterns implicated by
pointed to the importance of an indi- be used. Similarly, the physical thera- this additional information were not
vidual's problem representation for pist's representation of the problem known to the student. The novice
guiding reasoning and determining (as determined by each individual's must rely on black and white text-
successful problem solution. A prob- personal perspective and organization book patterns and lacks information
lem representation is the solver's of knowledge) will influence the on the relationships and shared fea-
internal model of the problem, con- subsequent reasoning and search for tures across dfierent clinical pat-
taining the solver's conception of the a solution. For example, physical terns.3" This creates difficulty for the
problem elements, his or her knowl- therapists who adhere to the concept novice when confronted with irrele-
edge of those elements, and the rela- of "adverse neural tissue tension" as vant and unrelated information or
tionship the different problem ele- described by Elvey29 and Butler 30 will patient presentations containing over-
ments have to each other.25 The conceptually approach the examina- lapping problems and gray, nontext-
depth and organization of knowledge tion and treatment of a patient differ- book variations.
between novices and experts has ently than therapists without this par-
consistently been found to differ. ticular organization of knowledge. An example of the novice's risk of
Recognition of the continuity of the missing overlapping problems is the
Chess experts recognize patterns nervous system29,30will influence patient whose lateral elbow pain is
reflecting areas of strategic strength therapists' attention and weighting of aggravated by resisted extension of
and vulnerability and positions sup- patient clues and their subsequent the wrist. The novice may recognize
porting maneuvers of attack and de- search for supporting and negating this typical feature of injury to the
fense. Although the chess expert can data. common extensor origin yet fail to
replicate a chessboard when viewed exclude (through inquiry and physical
for only 5 seconds, there is a dramatic Using a method of propositional anal- tests) other potentially coexisting
drop-off in this ability below the level ysis to determine a clinician's mental disorders that may share o r predis-
of chess master. N o differences, how- representation of a case, Pate1 and pose to this clinical presentation (eg,
ever, are found when the chess pieces colleagues31-3' have found analogous involvement of C5-6 musculoskeletal
are randomly arranged, demonstrating results when comparing medical structures, adverse neural tissue ten-
the chess master's superior ability to clinicians at various levels of exper- sion, radiohumeral joint and local
perceive patterns in chess posi- tise. Typically, subjects are presented radial nerve entrapment).
ti0ns.26.~7Expert physics problem with a written patient description and
solvers represent problems as in- then asked to recall the facts in writ- Bordage and colleagues39~4~ have
stances of major laws of physics appli- ing, followed by their explanation of demonstrated other more qualitative
cable to the specific situation in the patient's underlying pathophysiol- differences in the organization of
which novices' problem representa- ogy and lastly their diagnosis. Proposi- novice and expert knowledge.
tion are more literal, fragmented, and tional analysis is a system of noting Whereas the novice's knowledge is
tied to overt features of the problem and classifying the clinician's observa- centered purely on disjointed lists of
such as the use of a spring or a pul- tions, findings, interpretations, and signs and symptoms, the stronger
ley.25 Similar results demonstrating inferences derived from the infoma- diagnosticians make use of abstract
experts' recognition of patterns have tion contained in the text. These stud- relationships such as proximal-distal,
been replicated in several other do- ies consistently demonstrated differ- deep-superficial, and gradual-sudden,
mains such as in the game of GO, in ences between experts' and novices' which assist to categorize similar and
reading circuit diagrams, in reading conceptualization of a problem, with opposing bits of information in
architectural plans, and in interpreting experts possessing a superior organi- memory.
Physical Therapy /Volume 72, Number 12Pecember 1992
One's organization of knowledge not lar. That is, in an attempt to under- be directed at the source of the symp-
only appears to determine what labels stand and manage the patient's prob- toms or toward contributing factors. If
are given to recognizable patterns of lem, I contend that therapists obtain passive movement is used, examples
information, but also includes "pro- information regarding the following of considerations include whether
duction rules," which specify what five categories of hypotheses: physiological or accessory movements
actions should be taken in different (1) source of the symptoms o r are used; whether pain should be
situations.23~32.41
Experts are thought dysfunction, (2) contributing factors, provoked o r avoided; and what direc-
to have a large number of such rules (3) precautions and contraindications tion, amplitude, speed, and duration
specific to their area of experience. to physical examination and treat- of movement should be applied.44
ment, (4) management, and
The end result of the expert's supe- (5) prognosis. Whereas epidemiological studies
rior organization of knowledge is the provide insight into the probable
ability to reason inductively in a for- These hypothesis categories are not course of different diseases and inju-
ward manner from the information peculiar to any particular approach or ries,45 physical therapists should be
presented and to achieve superior philosophy of manual therapy. Any able to inform patients to what extent
diagnostic accuracy. That is, when clinician who uses hypothetico- their disorder appears amenable to
confronting a familiar presentation, deductive clinical reasoning should physical therapy and to give an esti-
experts can utilize rules of action be considering hypotheses within mate of the time frame for which
found reliable in their own clinical each of these categories. recovery can be expected. Hypotheses
experience to reach a diagnosis based regarding "prognosis" in this sense
on pure pattern recognition. When "Source of the symptoms o r dysfunc- can only be made on the basis of
faced with an atypical problem o r a tion" refers to the actual structure each patient's individual presentation.
problem out of their area of exper- from which symptoms are emanating.
tise, however, experts, like novices, "Contributing factors" are any predis- Information leading to the different
must rely more on the hypothetico- posing or associated factors involved hypothesis categories is obtained
deductive (ie, hypothesis testing) in the development or maintenance throughout the subjective and physi-
method of reasoning.22.42~~3 of the patient's problem, whether cal examination, with any single piece
environmental, behavioral, emotional, of information often contributing to
The organization of knowledge rele- physical, or biomechanical. For exam- more than one hypothesis category.
vant to clinical manual therapy would ple, a subacromial structure may be A more detailed discussion of what
include the facts (eg, anatomy, patho- the source of the symptoms, whereas information can be considered for the
physiology, and so forth), procedures poor force production by the scapular different categories of hypotheses is
(eg, examination and treatment strate- rotators may b e the contributing fac- available in Jones5 and Jones and
gies), concepts (eg, instability, adverse tor responsible for the development Jones.46
neural tissue tension), and patterns of or maintenance of an "impingement"
presentation. This knowledge is uti- syndrome. Rothstein and Echternachj~~~ have
lized with the assistance of rules or proposed a useful hypothesis-oriented
principles (eg, selection of the grade Hypotheses regarding "precautions algorithm for clinicians. In highlight-
of passive movement and technique) and contraindications to physical ing the all-too-frequent occurrence of
to acquire, interpret, infer, and collate examination and treatment" serve to clinicians carrying out routine treat-
patient information. determine the extent of physical ex- ment plans that are unrelated to the
amination (ie, whether specific move- preceding patient examination, these
Clinlcal Reasoning in ments are performed or taken up to authors make a case for the need for
Physkal Therapy or into ranges of movement in which physical therapists to acquire clinical
pain is provoked and how many reasoning skills. They provide a clear
Whereas research in medical educa- movements are tested), whether phys- set of steps that appropriately high-
tion has emphasized diagnosis, I be- ical treatment is indicated, and, if so, light the importance of utilizing data
lieve that physical therapists must be whether there are constraints to phys- from the patient interview to generate
concerned with additional categories ical treatment (eg, the use of passive a problem statement and establish
of hypotheses in order to deliver movement without provoking any measurable goals. The algorithm
physical therapy effectively and safely. discomfort versus passive movement continues with the physical examina-
Therapists with different training will that provokes the patient's pain). tion and the generation of hypotheses
ask different questions and perform about the cause(s) of the patient's
different tests in accordance with the Hypotheses regarding "management" problem. They note that testing crite-
significance they give to the subjective include consideration of whether ria for each hypothesis should be
and physical information available physical therapy is indicated and, if considered and that all treatments
from the patient. I propose, however, so, what means should be trialed. If should relate to the hypotheses made.
that despite these differences, the manual therapy is warranted, it must The second part of their hypothesis-
aims of therapists' inquiries are simi- be decided whether treatment should oriented algorithm provides an or-
Physical Therapy /Volume 72, Number 12December 1992
patient shows obvious difficulty in
removing his o r her arm from a
jacket, the therapist will already be
forming initial hypotheses or working
INFORMATION
interpretations regarding the source
PERCEPTION
and of the problem and degree of involve-
INTERPRETATION ment. Further information (ie, data
collection) is then sought throughout
DATA the subjective and physical examina-
INITIAL CONCEPT ,or@ COLLECTION tion with these working hypotheses in
and ~nformatlon, ' s ~ b l e c t l v e mind.
MULTIPLE mdrd Interview
HYPOTHESES physlcal Although certain categories of infor-
examlnatlon
mation (eg, site, behavior, and history
of symptoms) are scanned in all pa-
EVOLVING tients, the specific questions pursued
CONCEPT 4
of the PROBLEM Information are tailored to each patient and the
(hypotheses therapist's evolving hypotheses. For
knowledge base modlfled) example, when the patient with d f i -
cognltlve skllls culty removing the jacket describes an
metacognltlve area of ache in the supraspinous fossa
skllls and an area of pain in the anterior
DECISION
dlagnostlc shoulder just lateral to the coracoid
management process, the initial hypothesis of a
"shoulder problem" is already modi-
fied. For me, two different symptoms,
an ache and a pain, are indicated,
PHYSICAL THERAPY each warranting consideration and
INTERVENTION
further inquiry. I would consider both
4 local and spinal structures as potential
REASSESSMENT sources o r contributing factors. The
patient's response to open questions
regarding what aggravates and what
Flgure. Clinical reasoning model for physical therapists. (Adaptedfrom Barrows eases the pain should then be inter-
and T ~ r n b l y n . ~ ~ ) preted with these hypotheses in mind.
dered series of steps for reassessing ing management. I have also Maitland**~~9 uses the phrase "make
the effects of the treatment imple- attempted to depict the cyclical char- the features fit" to encourage thera-
mented. This algorithm is useful in acter of the clinical reasoning process pists to inquire in the mode de-
teaching the hypothetico-deductive and to highlight key factors that influ- scribed here where information is
method of clinical reasoning and ence the various phases of clinical interpreted for its support or "fit"
assisting clinicians in recognizing reasoning. The process begins with with existing information (ie, working
when their actions have not been the therapist's obsavation and inter- hypotheses). When features do not fit,
logically formulated. pretation of initial cues from the or in this terminology your hypothe-
patient. Even in the opening moments sis is not supported by the new infor-
I have adapted a diagram from Bar- of greeting a patient, the therapist will mation, further inquiry is needed. For
rows and Tamblyn48 to depict the observe specific cues such as the example, an impingement of either
clinical reasoning process of physical patient's age, appearance, facial ex- contractile o r noncontractile struc-
therapists (Figure). This is not a sub- pressions, movement patterns, resting tures may be considered in the pa-
stitute for the hypothesis-oriented posture, and any spontaneous com- tient I have described. If further ques-
algorithm of Rothstein and Echter- ments. These initial cues from the tioning revealed that the patient had
nach.3.47 Rather, this model is pre- patient should cause the therapist to no difficulty lifting any weight below
sented to bring attention to the hy- develop an iniiial concept of the 90 degrees while movements across
pothesis generation, testing, and problem that includes prelimina y the body into horizontal flexion were
modification that I feel should take working hypotheses for consideration limited by the anterior pain, this
place through all aspects of the pa- through the rest of the examination would not, in my view, support a
tient encounter including the inter- and throughout ongoing management contractile tissue lesion but would
view, physical examination, and ongo- of the patient. For example, if the implicate an impingement of noncon-
tractile structures or an acromioclavic-
Physical Therapy /Volume 72, Number 12iDecember 1992
ular source to this pain. I would ques- additional examination, reanalysis of Errors of Clinlcal Reasonlng
tion and reason in this manner to data obtained, referral to another
assess the involvement of other struc- health care practitioner). Successful management of a patient's
tures in the anterior pain, such as problem requires a multitude of
cervical structures and neural tissues, Factors lnfluenclng Cllnlcal skills. Working from the patient's
and I would pay equal attention to Reasonlng account of the problem, the therapist
the ache. must be able to efficiently observe
The clinical reasoning process is influ- and extract information, distinguish
Similarly, the physical examination is enced by the therapist's knowledge relevant from irrelevant information,
not simply a routine series of tests. base, cognitive skills (eg, data analysis make correct interpretations, weigh
There may be specific physical tests and ~ynthesis),~6~*~~5~ and metacogni- and collate information, and draw
that are used for different areas, but tive skills (ie, awareness and monitor- correct inferences and deductions.
these should be seen as an extension ing of thinking processes).5l These Errors of reasoning may occur at any
of the data collection and hypothesis factors influence all aspects of the stage of the clinical reasoning process
testing performed through the subjec- clinical reasoning process and can including errors of perception, in-
tive e ~ a m i n a t i o nFor
. ~ ~example, re- themselves be improved when thera- quiry, interpretation, synthesis, plan-
ports of painful "clicking" in the pists consciously reflect on the sup- ning, and reflection. Application of
shoulder and sensations of apprehen- porting and negating information on hypothesis-oriented clinical reasoning
sion indicate the need for instability which their inquiries and clinical as encouraged by the clinical reason-
and labral integrity testing, but these decisions are based. For example, ing model portrayed in the Figure
tests may not be warranted in the consideration of the features of the and the hypothesis-oriented algorithm
next patient who has similar patient's presentation that fit and do described by Rothstein and Echter-
symptoms. not fit existing patterns recognized by nach4' should assist clinicians in
therapists will enable therapists to avoiding errors of reasoning.
This process of data collection contin- learn about different clinical patterns
ues as hypotheses are refined and and their variations and to broaden Examples of reasoning errors extrapo-
reranked and new ones considered in their knowledge base. I contend that lated from Nickerson et alsl are given
the therapist's "evolving concept" of therapists with good clinical reason- below with the physical therapy appli-
the problem. The clinical reasoning ing skills will reflect as they interact cations derived by this author.
through the patient examination con- with the patient, improvising their
tinues until sufficient idormation is actions in accordance with the unfold- 1. Adding pragmatic inferences. Mak-
obtained to make a "diagnostic" and ing patient findings much like a musi- ing assumptions is an error of
management decbion. cian adjusts his o r her performance reasoning. For example, a patient
when participating in an improvisa- with pain in the supraspinous fossa
The clinical reasoning process does tional session with other musicians.52 will often describe this as "pain in
not stop at completion of the patient my shoulder." It is a misrepresen-
examination. Rather, the therapist will As reasoning is only as good as the tation of the facts to assume the
have reached the management deci- information on which it occurs, any patient's "shoulder pain" is actually
sions of whether to treat o r not treat; factor influencing the reliability and within the shoulder itself without
whether to address the source(s) o r validity of information obtained (eg, specific clarification of the site.
contributing factor@),or both, ini- communication/interpersonal and
tially; which mode of treatment to use manual skills) will also influence the 2. Considering too fa0 hypotheses. By
initially; and, if passive movement effectiveness of one's clinical reason- prematurely limiting the hypotheses
treatment is to be used, whether to ing. For example, leading questions in considered, discovery of the correct
provoke symptoms and the direction a patient interview often elicit re- hypothesis may be missed or de-
and grade of movement. Every treat- sponses that support the examiner's layed. This can occur when inqui-
ment, whether it is hands-on o r ad- assertion. Other less tangible factors ries and physical tests are only
vice, should be a form of hypothesis influencing clinical reasoning include directed to the local sources of a
testing. Continual reassessment is environmental contingencies such as patient's symptoms, as with the
essential and provides the evidence group norms and time constraints.*l patient reporting "shoulder pain
on which hypotheses are accepted or That is, working environments of with any lifting." To interpret this
rejected. Reassessmmt should contrib- overextended case loads and peer or automatically as a shoulder problem
ute to the therapist's evolving concept self-imposed pressure to exclusively or, worse yet, a "frozen shoulder"
of the patient's problem. When treat- adopt the latest treatment fad are not without considering other hypothe-
ment has not had the expected effect, conducive to clinical reasoning that is ses is an error of reasoning.
the therapist's concept of the problem hypothesis oriented.
and its management may be altered, 3. Failure to sample enough irzformu-
leading to a change in treatment o r tion. It is an error to make a gen-
further inquiry (eg, reexamination, eralization based o n limited data.
Physical Therapy 'Volume 72, Number 12Pecember 1992
This is seen in judgments regard- time as a central neck pain is insuf- lesions, there will typically be pain
ing the success o r failure of a par- ficient to judge the relationship of on resisted isometric testing; how-
ticular management approach these symptoms. A full understand- ever, this does not mean that all
based on only a few experiences. ing of the relationship between painful resisted isometric tests are
Closely linked to this error is the these two symptoms requires in- necessarily intrinsic rotator cuff
failure to sample information in an quiry of when both occur together, lesions.
unbiased way. Although this is when the neck pain occurs without
typically controlled for in formal the scapular pain, when the scapu- A second form of deductive rea-
research, the practicing therapist lar pain occurs without the neck soning states: If A, then B; not B,
will rely on memory of previous pain, and when neither neck nor therefore not A. For example, if
experiences as the sample on scapular pain are occurring. you have shoulder pain referred
which views are based. The error from the cervical spine, you will
occurs when only those cases are 6. Confusing covariance with causal- have cervical signs; if you do not
recalled that support one view ity. When two factors have been have cervical signs, it is not cervical
while confounding evidence is found to covary, it is an error to referred shoulder pain. It is a de-
forgotten. deduce the factors are necessarily ductive error to reason: If A, then
causally related. For example, if the B; not A, therefore not B. For ex-
4. Confirmution bias. Another error scapular pain in the above example ample, if you have shoulder pain
of reasoning related to a biased only occurs when the cervical pain referred from the cervical spine,
sample of information occurs when is present, this does not prove the you will have cervical signs; if
therapists only attend to those two symptoms are from the same there is no cervical referred shoul-
features that support their favorite source (eg, cervical disk). Although der pain, there will not be cervical
hypotheses while neglecting the this is a reasonable hypothesis, signs.
negating features. This can lead to another possibility is that two dif-
incorrect clinical decisions and ferent structures (eg, cenical and 8. Premise conversion. It is a deduc-
hinder the therapist's opportunity thoracic) are simultaneously tive error of reasoning to reverse a
to learn different variations of clini- stressed by the same activity or statement of categorization. That is,
cal patterns. For example, a pre- posture. all A are B does not mean all B are
sentation of central low back pain A. For example, all shoulder im-
aggravated by slouched sitting may 7 . Conjksion between deductive and pingements are subacromial (or
be quickly interpreted by some inductive logic. Deductive reason- subcoracoid) does not mean
therapists to be a "diskogenic" ing involves logical inference. One all subacromial pains are
disorder. Further clarification that draws conclusions that are a logi- impingements.
the patient's pain provocation was cal, necessary consequence of the
not time dependent and that move- premises without going beyond the These examples represent only a
ment from a sitting to a standing information contained in the prem- sample of the reasoning errors a
position was not hindered, regard- ises. Correct deductive reasoning is therapist can make. Errors in reason-
less of the speed at which it was independent of the truth of the ing are also not confined to the less
performed, could represent negat- premises o r the conclusion. In experienced, as even "experts" have
ing features to the "diskogenic" contrast, inductive reasoning in- been shown to overemphasize posi-
diagnosis. Attention to such varia- volves going beyond the informa- tive findings, ignore or misinterpret
tions in presentation will assist tion given. Every time we make a negative findings, deny findings that
therapists' recognition of clinical generalization based on specific conflict with a favorite hypothesis, and
variations within the same diagno- observations, this is an induction. obtain redundant information.16.52-54
sis, which in turn should lead to A valid form of deductive reason- The As and Bs of logic may appear to
recognition of optimal treatment ing states: If A, then B; A, therefore be nothing more than semantics. If
strategies for the respective B. For example, if you have an the inductive generalizations preva-
presentations. acromioclavicular joint problem, lent in manual therapy are not recog-
horizontal flexion is likely to be nized for what they are, however,
5. E m r s in detecting covariance. To symptomatic. It is a deductive error therapists are prone to accept these
make a judgment about the rela- to reason: If A, then B; B, therefore generalizations as fact and fail to look
tionship of two factors requires A. For example, if you get pain for alternative explanations.
understanding of how the two with horizontal flexion you have an
factors covary with one another. It acromioclavicular joint problem. Bordage and c o l l e a g ~ e s ~ ~suggest
,5~5~
is an error to make this judgment This may be inductively reasonable that most diagnostic errors are not
based solely on one combination based on past experience; how- the result of inadequate medical
of covariance. For example, know- ever, it is deductively wrong, as knowledge as much as an inability to
ing that the patient's medial scapu- other structures may be responsi- retrieve relevant knowledge already
lar pain is experienced at the same ble. Similarly, with rotator cuff stored in memory. That is, the
Physical Therapy /Volume 72, Number
amount of knowledge appears less physical therapy organization of closely linked to the accessibility of
relevant than the organization of that knowledge necessitates further inves- one's knowledge. Knowledge that is
knowledge. When knowledge is not tigation of potential differences in acquired in the context for which it
organized in clinically relevant pat- clinical reasoning and associated will be used becomes more accessi-
terns, it becomes less accessible in factors. ble.72,73Although clinical knowledge
the clinical setting. is typically presented in the context of
Facllltating Cllnlcal Reasoning patient problems, this is less com-
Having given the impression that in Our Students monly the case with the basic sci-
good clinical reasoning will assist ences (eg, pathophysiology). Ap-
therapists in recognizing clinical pat- As physical therapists have taken proaches to physical therapy
terns, a word of caution regarding greater responsibility in patient man- education in which the acquisition of
excessive attention to clinical patterns agement, especially with the increased knowledge is facilitated by teaching
I
is needed. Clinical patterns are at risk autonomy associated with first-contact centered on patient problems pro-
of becoming rigidly established when practice, physical therapy education vide, in my opinion, the ideal envi-
the patterns themselves control our ha. respbnded with efforts to produce ronment for building an accessible I
attention. I believe this leads to errors more "thinking" therapists. Although organization of knowledge and foster- I
of limited hypotheses and insufficient attention to clinical reasoning skills ing clinical reasoning ~kills.67~68,7-1
sampling where anything that has any has presumably always been inherent
resemblance to a standard pattern will in our physical therapy education, Learning the hypothesis testing ap-
be seen as that pattern. For example, there has been a more recent interest proach also enables students to con-
the information that a patient has pain in providing more formal and focused tinue to learn beyond their formal
in the area of the greater trochanter learning experiences specifically education. Rather than relying on a
aggravated by functional movements aimed at facilitating clinical reasoning text or more experienced colleague
involving flexion or adduction of the in physical therapy students.*.5aGS69 to learn new clinical patterns, the
hip may cause some therapists to therapist who actively reasons
hypothesize the existence of a "hip Facilitating students' clinical reasoning through and reflects on patient prob-
joint" disorder. Limiting one's hypoth- requires making them aware of their lems will continually challenge exist-
eses to what may appear to be the own reasoning process and designing ing patterns and in the process ac-
most obvious hypothesis without learning experiences that promote all quire new ones.
pursuing additional supporting o r aspects of the clinical reasoning pro-
negating evidence prevents the thera- cess while exposing the errors in Summary
pist from ever learning the pattern of reasoning that occur. This requires
other disorders that may share fea- access to students' thoughts and feed- Early research in medical education
tures with a disorder of the hip (eg, back on thinking processes. That is, provided a picture of a clinical rea-
lumbar spine, sacroiliac joint, adverse students should be taught to think soning process that was hypothetico-
neural tissue tension) or the full and to think about their thinking.70 deductive and universally applied by
range of presentations a hip joint This can be achieved by promoting clinicians at all levels of experience.
disorder can manifest. students' use of reflection to encour- The differentiating feature of expert
I age awareness and promote integra- diagnosticians and novices appears to
Implkatlons for Physkal tion of existing versus new knowl- lie in their organization of knowl-
Therapists edge. When combined with a better edge. Experts have a superior organi-
awareness of one's own cognitive zation of knowledge that enables
Physlcal Therapy Research in processes (ie, metacognition), the them to reason inductively in a form
Cllnlcal Reasoning students' processing of information is of pattern recognition. When con-
enhanced and clinical reasoning is fronted with unfamiliar problems, the
Consideration of the clinical reason- facilitated. Learning experiences to expert, like the novice, will rely on
ing literature outside of physical ther- facilitate clinical reasoning using both the more basic hypothesis testing
apy assists in developing an under- reflection and metacognition are approach to clinical reasoning.
standing of this topic while providing described else~here.5~71
educational and clinical extrapolations Research to better understand the
to our profession. Debate continues The process of reasoning should not, clinical reasoning and nature of ex-
in the medical literature, however, in my view, be addressed to the ne- pertise in physical therapy can assist
regarding the nature of expertise and glect of knowledge. Rather, facilitating us in designing learning experiences
the appropriate methodology to use the clinical reasoning process will to facilitate clinical reasoning. Clinical
in research.4015-3 Although some assist the students' acquisition of reasoning is now being given specific
evidence does exist suggesting that knowledge. In turn, good organiza- attention in some physical therapy
medical and physical therapy clinical tion of knowledge leads to better education programs. The aims of
reasoning processes are similar,- the clinical reasoning. The importance of these programs should be to increase
potential differences in medical and one's organization of knowledge is students' awareness of their clinical
Physical Therapy,/Volume 72, Number 12December 1992
reasoning and to foster development Therapy, May 17-22, 1987; Sydney, New South 24 Newell A, Simon HA. Human Problem
Wales, Australia. 1987:543-551. Solving. Englewood Cliffs, NJ: Prentice-Hall;
of both reasoning and knowledge 1972.
8 Thomas-Edding D. Clinical problem solving
through learning experiences cen- in physical therapy and its implications for 25 Chi MTH, Feltovich PJ, Glaser R. Categori-
tered on patient problems. This re- curriculum development. In: Proceedings of zation and representation of physics problems
quires accessing students' thoughts the Tenth International Congress of the World by experts and novices. Cognitive Science.
Confederation for Physical Therapy; May 17- 1981;5:121-152.
during and after a patient encounter 22, 1987; Sydney, N m South Wales, Australia. 26 DeGrcmt AD. Thought a n d Choice in Chess.
and providing feedback on errors of 1987:10@104. New York, NY Basic Books; 1965.
reasoning that emerge. Teaching 9 Benner P. From Novice to Expert: Excellence 27 Chase WG, Simon HA. Perception in chess.
students skills of reflection and meta- a n d Power in Clinical Nursing Practice. Cognitive Psychology 1973;4:5541.
Menlo Park, Calif: Addison-Wesley; 1984. 28 Glaser R, Chi MTH. Overview. In: Chi
cognition should improve their clini- 10 Downie J, Elstein AS, eds. Profesn'onal MTH, Glaser R, Farr MJ, eds. The Nature of
cal reasoning now and equip them Judgment: A Reader in Clinical Decision Mak- Expertise. Hillsdale, NJ: Lawrence Erlbaum As-
with the: means to continue learning ing. New York, W, Cambridge University sociates Inc; 1988:xv-xxxvi.
Press; 1988. 29 Elvey RL. Treatment of arm pain associated
from future patient problems. Thera-
11 Nickerson RS, Perkins DN, Smith EE. The with abnormal brachial plexus tension. Austra-
pists can improve their own clinical Teaching of Thinking. Hillsdale, NJ: Lawrence lian Journal of ~ b ~ s i o t h k r 1986;32:224
a~~.
reasoning by stopping at various Erlbaum Associates Inc; 1985. 229.
points through a patient examination 12 Chi MTH, Glaser R, Farr MJ, eds. The Nu- 30 Butler DS. Mobilization of the Nervous
and the ongoing management period ture of Expertise. Hillsdale, NJ: Lawrence Ed- System. Melbourne, Victoria, Australia: Church-
baum Associates Inc; 1988. ill Livingstone: 1991.
to consciously reflect on hypotheses 1 3 Thomas SA, Wearing AJ, Bennett MJ. Clini- 31 Patel VL, Frederiksen CH. Cognitive p r e
being considered, implications of cal Decision Making for Nurses a n d Health cesses in comprehension and knowledge ac-
those hypotheses, and, in hindsight, Professionals. Sydney, New South Wales, Aus- quisition by medical students and physicians.
tralia: Harcourt Brace Jovanovich; 1991. In: Schmidt HG, DeVolder ML, eds. Tutorials
where e:rrors of reasoning occurred. in Problem-Based Learning. Assen, the Nether-
14 Elstein AS. Cognitive processes in clinical
Clinical reasoning that is hypothesis inference and decision making. In: Turk DC, lands: Van Gorcum BV; 1984;14>157.
directed and open-minded can add to Salovey P, eds. Reasoning, Inference, a n d 32 Pate1 VL, Groen GJ. Knowledge-based solu-
our organization of knowledge and Judgment in Clinical Psychology. New York, tion strategies in medical reasoning. Cognitive
NY: The Free Press; 1988:17-50. Science. 1986;10:91-108.
enhance the quality and accountability 15 Feltovich PJ, Barrows HS. Issues of general- 33 Patel VL, Groen GJ, Frederiksen CH. Differ-
of our patient care. ity in medical problem solving. In: Schmidt ences between medical students and doctors
HG, DeVolder ML, eds. Tutorials in Problem- in memory for clinical cases. Med Educ. 1986;
Acknowledgment Based Learning Assen, the Netherlands: Van 20:3-9.
Gorcum BV; 1984:128-141. 34 Coughlan LD, Patel VL. Processing of criti-
1 6 Elstein AS, Shulman IS,Sprafka SS. Medi- cal information by physicians and medical stu-
I would like to thank Dr Joy Higgs, cal Problem Solving: An Analysis of Clinical dents. J Med Educ. 1987;62:81&828.
Head, School of Physiotherapy, Fac- Reasoning. Cambridge, Mass; Harvard Univer- 35 Patel VL, Evans DA, Groen GJ. Biomedical
ulty of Health Sciences, University of sity Press; 1978. knowledge and clinical reasoning. In: Evans
Sydney, for her review and sugges- 17 Barrows HS, Feightner JW, Neufeld VR, DA, Patel VL, eds. Cognitive Science in Medi-
Norman GR. Analysis of the Clinical Methods cine. London, England: The MIT Press Ltd;
tions in the development of this of Medical Students a n d Physicians: Final Re- 1989:53-112.
manuscript. port. Hamilton, Ontario, Canada: Ontario De- 36 Patel VL, Evans DA, Kaufman DR. A cogni-
partment of Health; 1978. tive framework for doctor-patient interaction.
18 Barrows HS, Norman GR, Neufeld VR, In: Evans DA, Patel VL, eds. Cognitive Science
References Feightner JW. The clinical reasoning of ran- in Medicine. London, England: The MIT Press
domly selected physicians in general medical Ltd; 1989:257-312.
practice. Clin Invest Med. 1982;5:49-55. 37 Patel VL, Groen GJ, Arocha JF. Medical ex-
1 Wolf SL, ed. Clinical Decision Making in
Physical Therapy. Philadelphia, Pa: FA Davis 19 Neufeld VR, Norman GR, Feightner JW, pertise as a Function of task difficulty. Memory
Barrows HS. Clinical problem-solving by medi- a n d Cognition. 1990;18:394-406,
Co; 1985.
cal students: a cross-sectional and longitudinal 3 8 Feltovich PJ, Johnson PE, Moller JH, Swan-
2 Grant R, Jones MA, Maitland GD. Clinical analysis. Med Educ. 1981;15:315-322.
decision making in upper quadrant dysfunc- son DB. LCS: the role and development of
tion. In: Grant R, ed. Physical Therapy of the 20 Norman GR, Tugwell P, Feightner JW.A medical knowledge in diagnostic expertise. In:
Cervical a n d Thoracic Spine. New York, NY: comparison of resident performance on real Clancey WJ, Shortliffe EH, eds. Readings in
Churchill Livingstone Inc; 1988:51-79. and simulated patients. J Med Educ. 1982;57: Medical Ar12Jicial InleN@ence: The Firsl Dec-
708-715. ade. Reading, Mass: Addison-Wesley; 1983:275
3 Echternach JL, Rothstein JM. Hypothesis-
21 Patel VL, Groen GJ. The general and spe- 319.
oriented algorithms. Phys Ther 1989;69:559-
564. cific nature of medical expertise: a critical 39 Bordage G, Lemieux MA. Some cognitive
look. In: Ericsson A, Smith J, eds. Toward a characteristics of medical students with and
4 Shepard KF, Jensen GM. Physical therapist General Theory of Expertise: Prospects a n d without diagnostic reasoning difficulties. In:
curricula for the 1990s: educating the reflec- Limits. New York, NY: Cambridge University Proceedings of the 25th Annual Conference
tive pracl.itioner.Phys Ther. 1990;70:566-577. Press; 1991:93-125. o n Research in Medical Education; 1986;New
5 Jones MA. Clinical reasoning process in ma- 22 Groen GJ, Pate1 VL. A view from medicine. Orleans, Louisiana. 1986:185-190.
nipdative therapy. In: Boyling JD, Palastanga In: Smith M, ed. Toward a UniJied Theory of 40 Bordage G, Grant J, Marsden P. Quantita-
N, eds. Modern Manual Therapy: The Vertebral Problem Solving: Views from Content Do- tive assessment of diagnostic ability. Med Educ.
Column. 2nd ed. London, England: Churchill mains. Hillsdale, NJ: Lawrence Erlbaum Associ- 1990;24:413425.
Livingstone. In press. ates Inc; 1990:35-44. 41 Patel VL, Groen GJ. Developmental ac-
6 Payton OD. ClinicaI reasoning process in 23 Greeno JG, Simon HA. Problem solving counts of the transition from medical student
physical therapy. Phys T k . 1985;65:92&928. and reasoning. In: Atkinson RC, Hernstein R, to doctor: some problems and suggestions.
7 Dennis JK, May BJ. Practice in the year 2000: Lindsey G, Luce RD, eds. Steven's Handbook of Med Educ. 1991;25:527-535.
expert decision making in physical therapy. In: Experimental Psychology, Volume 2: Learning 42 Elstein AS. Shulman LS, Sprafka SA. Medi-
Proceedings of the Tenth International Con- a n d Cognition. 2nd ed. New York, NY: John cal problem solving: a ten-year retrospective.
gress of the World Confederation for Physical Wiley & Sons Inc; 1986:589-572.
Physical Therapy /Volume 72, Number 12December 1992
Evaluation and the Health Profes~ions.1990; atory study. In: Proceedings of the 21sr Confer- 69 Terry W, Higgs J. Educational programs to
13:>36. ence on Research in Medical Education; 1982; develop clinical reasoning skills. Australian
43 Barrows HS, Feltovich PJ. The clinical rea- Washington, DC.1982:171-176. Journal of Physiotherapy. In press.
soning pmess. Med Educ. 1987;21:8691. 56 Bordage G, Zacks R. The structure of medi- 7 0 Schon DA. Educating the Refective Practi-
44 Maitland GD. Peripheral Manipulation. 3rd cal knowledge in the memories of medical tioner. San Francisco, Calif: Jossey-Bass Pub-
ed. London, England: Butterwonh & Co (Pub- students and general practitioners: categories lishers; 1990.
lishers) Ltd; 1991. and prototypes. Med Educ. 1984;18:406416. 7 1 Higgs J. Developing knowledge: a process
45 Jeffreys E. Prognosis in Musculoskeletal 5 7 Bordage G, Lemieux M. Semantic struc- of construction, mapping and review. New
Injury: A Handbook for Doctors and Lawyers. tures and diagnostic thinking of experts and Zealand Journal of Physiotherapy. In press.
London, England: Butterwonh & Co (Publish- novices. Acad Med. 1991;66(suppI):S7&S72. 72 Tulving E, Thomson DM. Encoding speci-
ers) Ltd; 1991. 5 8 Berner ES. Paradigms and problem-solving: ficity and retrieval processes in episodic mem-
46 Jones MA, Jones HM. Principles of the a literature review. J Med Educ. 1984;59:62> ory. Psycho1 Rev. 1973;80:352-373.
physical examination. In: Boyling JD, Pa- 633. 7 3 Rumelhan DE, Onony E. The representa-
lastanga N, eds. Modern Manual Therapy: The 59 McGuire C. Medical problem-solving: a tion of knowledge in memory. In: Anderson
Vertebral Column. 2nd ed. London, England: critique of the literature. In: Proceedings of the RC, Spiro RJ, Montague WE, eds. Schooling
Churchill Livingstone. In press. 23rd Annual Conference on Research in Medi- and the Acquisition of Knowledge. Hillsdale,
47 Rothstein JM, Echternach JL. Hypothesis- cal Education; 1984; Washington, DC 1984:3- NJ: Lawrence Erlbaum A5sociates Inc; 1977':s-
oriented algorithm for clinicians: a method for 12. 135.
evaluation and treatment planning. Phys Ther. 6 0 Groen GJ, Patel VL. Medical problem- 74 Barr JS. A problem-solving curriculum de-
1986;66:138%1394. solving: some questionable assumptions. Med sign in physical therapy. Phys Ther. 1977;57:
48 Barrows HS, Tamblyn RM. Problem-Based Edw. 1985;19:95-100. 262-270.
Learning: An Approach to Medical Education. 6 1 Norman GR. Problem-solving skills, solving 75 May BJ. An integrated problem-solving cur-
New York, NY:Springer-Verlag New York Inc; problems and problem-based learning. Med riculum design for physical therapy education.
1980. Educ. 1988;22:279-286. Phys Ther. 1977;57:807-813.
49 Maitland GD. Vertebral Manipulation. 5th 62 Barrows HS. Inquiry: the pedagogical im- 7 6 May BJ. Evaluation in a competency-based
ed. London, England: Butterwonh & Co (Pub- portance of a skill central to clinical practice. educational system. Phys Ther. 1977;57:2%33.
lishers) Ltd; 1986. Med Educ. 1930;24:3-5. 7 7 Olsen SL. Teaching treatment planning. a
50 Gale J. Some cognitive components of the 6 3 Norman GR, Pate1 VL, Schmidt HG. Clinical problem-solving model. Phys Ther 1983;63:
diagnostic thinking process. Br J Educ Psychol. inquiry and scientific inquiry. Med Educ. 1990; 526529.
1982;52:64-76. 24:396399. 7 8 Titchen AC. Design and implementation of
51 Nickerson RS, Perkins DN, Smith EE. The 64 Denton B, Jensen GM. Reflective inquiry: a a problem-based continuing education pro-
Teaching of Thinking. Hillsdale, NJ: Lawrence suggestion for clinical education. Phys Ther. gramme. Physiotherapy. 1987;73:31%323.
Erlbaum Associates Inc; 1985:10&109. 1989;69:407.Abstract. 79 Titchen AC. Problem-based learning: the
52 Schon DA. The Refective Practitioner: How 65 Jones MA. Clinical reasoning process in rationale for a new approach to physiotherapy
Professionals Think in Action. New York, NY: manipulative therapy. In: Proceedings of the continuing education ~hysiotherap~. 1987;73:
Basic Books; 1983. International Federation of Orthopaedic Ma- 324-327.
53 Lesgold A, Rubinson H, Feltovich P, et al. nipulative Therapists Congress;September 4-9, 8 0 Burnett CN, Pierson FM. Developing
Expenise in a complex skill: diagnosing x-ray 1988; Cambridge, England 1988:29-30. problem-solving skills in the classroom. Pbys
pictures. In: Chi MTH, Glaser R, Farr M, eds. 66 Jones MA. Clinical Reasoning in Manipula- Ther. 1988;69:441447.
The Nature of Expertise. Hillsdale, NJ: tive Therapy Education. Adelaide, South Aus- 81 Slaughter DS, Brown DS, Garder DL, Per-
Lawrence Erlbaum Associates Inc: 1981:311- tralia, Australia: South Australian Institute of ritt LJ. Improving physical therapy students'
342. Technology; 1989. Master's thesis. clinical problem-solving skills: an analytical
54 Voytovich AE, Rippey RM, Suffredini A. Pre- 67 Higgs J. Fostering the acquisition of clinical questioning model. Phys Ther 1989;69:441-
mature conclusions in diagnostic reasoning. reasoning skills. New Zealand Journal of Phys- 447.
J Med Educ. 1985;60:302-307. iotherapy. 1990;18:13-17.
55 Bordage G, Allen T.The etiology of diag- 68 Higgs J. Developing clinical reasoning
nostic errors: process or content? An explor- competencies. Physiotherapy. In press.
Physical Therapy/Volume 72, Number 12December 1992
View publication stats
You might also like
- Foundations of Professional Psychology: The End of Theoretical Orientations and the Emergence of the Biopsychosocial ApproachFrom EverandFoundations of Professional Psychology: The End of Theoretical Orientations and the Emergence of the Biopsychosocial ApproachNo ratings yet
- Dimensional PsychopathologyFrom EverandDimensional PsychopathologyMassimo BiondiNo ratings yet
- Clinical reasoning in manual therapyDocument10 pagesClinical reasoning in manual therapyPhooi Yee LauNo ratings yet
- Clinical Reasoning - Jones PDFDocument12 pagesClinical Reasoning - Jones PDFIsabelGuijarroMartinezNo ratings yet
- Clinical Reasoning: Linking Theory To Practice and Practice To TheoryDocument14 pagesClinical Reasoning: Linking Theory To Practice and Practice To Theorylumac1087831No ratings yet
- Original Research: Patterns of Clinical Reasoning in Physical Therapist StudentsDocument13 pagesOriginal Research: Patterns of Clinical Reasoning in Physical Therapist StudentsNishtha singhalNo ratings yet
- Clinical Reasoning Strategies in PTDocument19 pagesClinical Reasoning Strategies in PTamitesh_mpthNo ratings yet
- Single-Case Research Designs in Clinical Child Psychiatry: Journal of The American Academy of Child PsychiatryDocument10 pagesSingle-Case Research Designs in Clinical Child Psychiatry: Journal of The American Academy of Child PsychiatryKarla SuárezNo ratings yet
- He Clinical Integrative Puzzle For Teaching and Assessing Clinical Reasoning Preliminary Feasibility, Reliability, and Validity EvidenceDocument7 pagesHe Clinical Integrative Puzzle For Teaching and Assessing Clinical Reasoning Preliminary Feasibility, Reliability, and Validity EvidenceFrederico PóvoaNo ratings yet
- Pincus 2006Document9 pagesPincus 2006Claudio Andrés Olmos de AguileraNo ratings yet
- Understanding The Assessment of Clinical Reasoning: Omar S. LaynesaDocument20 pagesUnderstanding The Assessment of Clinical Reasoning: Omar S. Laynesaomar laynesaNo ratings yet
- Medscimonit 17 1 Ra12.pdf WT - SummariesDocument2 pagesMedscimonit 17 1 Ra12.pdf WT - SummariesRin VaelinarysNo ratings yet
- Clinical ReasoningDocument23 pagesClinical Reasoningathe_triiaNo ratings yet
- Physical Therapist As Critical InquirerDocument39 pagesPhysical Therapist As Critical InquirerMichels Garments S.H Nawaz HosieryNo ratings yet
- How Physicians Manage Medical Uncertainty: A Qualitative Study and Conceptual TaxonomyDocument17 pagesHow Physicians Manage Medical Uncertainty: A Qualitative Study and Conceptual TaxonomyAlexNo ratings yet
- Clinical reasoning for MSK PTsDocument48 pagesClinical reasoning for MSK PTsCatalina MusteațaNo ratings yet
- Assessment of Clinical Reasoning Three EvolutionsDocument6 pagesAssessment of Clinical Reasoning Three EvolutionsFrederico PóvoaNo ratings yet
- A Universal Model of Diagnostic Reasoning.14Document7 pagesA Universal Model of Diagnostic Reasoning.14Emília SantocheNo ratings yet
- Defining and Assessing Professional Competence: ReviewDocument10 pagesDefining and Assessing Professional Competence: ReviewJeaniee Zosa EbiasNo ratings yet
- UGML JAMA - I - How To Get StartedDocument3 pagesUGML JAMA - I - How To Get StartedAlicia WellmannNo ratings yet
- Context and Clinical ReasoningDocument8 pagesContext and Clinical ReasoningFrederico PóvoaNo ratings yet
- AConciseGuidetoClinicalReasoning PrepublicationDocument23 pagesAConciseGuidetoClinicalReasoning PrepublicationAlejandroNo ratings yet
- Timm Step by StepDocument6 pagesTimm Step by StepPutu WirasatyaNo ratings yet
- Critical Thinking in Respiratory Care Practice PDFDocument17 pagesCritical Thinking in Respiratory Care Practice PDFFernando MorenoNo ratings yet
- Evidence based-WPS OfficeDocument6 pagesEvidence based-WPS OfficeSalima HabeebNo ratings yet
- Defining and Assessing Professional Competence: JAMA The Journal of The American Medical Association February 2002Document11 pagesDefining and Assessing Professional Competence: JAMA The Journal of The American Medical Association February 2002NAYITA_LUCERONo ratings yet
- What S in A Case Formulation PDFDocument10 pagesWhat S in A Case Formulation PDFNicole Flores MuñozNo ratings yet
- Manual Therapy: Neil Langridge, Lisa Roberts, Catherine PopeDocument6 pagesManual Therapy: Neil Langridge, Lisa Roberts, Catherine PopeVizaNo ratings yet
- Piramide ClinicaDocument6 pagesPiramide ClinicaJASER MILTON ISMAEL MALDONADO GUERRERONo ratings yet
- Updated Integrated FrameworkDocument17 pagesUpdated Integrated FrameworkE. Jimmy Jimenez TordoyaNo ratings yet
- Updated Integrated Framework For Making Clinical Decisions Across The Lifespan and Health ConditionsDocument13 pagesUpdated Integrated Framework For Making Clinical Decisions Across The Lifespan and Health ConditionsmaryelurdesNo ratings yet
- Transdiagnostic FormulationDocument9 pagesTransdiagnostic FormulationMariela Del Carmen Paucar AlbinoNo ratings yet
- EBP in Adults FinalDocument20 pagesEBP in Adults FinalTony JacobNo ratings yet
- Facilitating Case Studies in Massage Therapy CliniDocument5 pagesFacilitating Case Studies in Massage Therapy ClinijorgenovachrolloNo ratings yet
- PublishedEBParticle JournalofAlliedHealth CardinDocument11 pagesPublishedEBParticle JournalofAlliedHealth Cardinag wahyudiNo ratings yet
- Critical Thinking Versus Clinical Reasoning Versus Clinical JudgmentDocument3 pagesCritical Thinking Versus Clinical Reasoning Versus Clinical JudgmentWinda ArfinaNo ratings yet
- Clinical ReasoningDocument3 pagesClinical ReasoningIvy VihNo ratings yet
- EBP Nursing ResearchDocument4 pagesEBP Nursing ResearchFrances BañezNo ratings yet
- Enhancing Patient Safety in Mental HealthDocument7 pagesEnhancing Patient Safety in Mental Healthruba azfr-aliNo ratings yet
- Needs Assessment For Holistic Health Providers Using Movement As MedicineDocument10 pagesNeeds Assessment For Holistic Health Providers Using Movement As Medicineapi-399928223No ratings yet
- Kazdin, 2008Document14 pagesKazdin, 2008CoordinacionPsicologiaVizcayaGuaymasNo ratings yet
- Case Formulation in PsychotherapyDocument5 pagesCase Formulation in PsychotherapySimona MoscuNo ratings yet
- Cooke2017 Transforming Medical AssessmentDocument6 pagesCooke2017 Transforming Medical AssessmentbrecheisenNo ratings yet
- 1 Running Head: Research Methods and ApproachesDocument6 pages1 Running Head: Research Methods and ApproachesGeorge MainaNo ratings yet
- Clinical Reasoning in Dentistry: A Conceptual Framework For Dental EducationDocument13 pagesClinical Reasoning in Dentistry: A Conceptual Framework For Dental EducationDrSanaa AhmedNo ratings yet
- Physical Therapy Research Paper SampleDocument8 pagesPhysical Therapy Research Paper Sampleaflbqewzh100% (1)
- 10 1111@jhn 12820Document10 pages10 1111@jhn 12820Federico CilloNo ratings yet
- The Use of Clinical Trials in Comparative Effectiv PDFDocument9 pagesThe Use of Clinical Trials in Comparative Effectiv PDFSilverio CasillasNo ratings yet
- Evidence-Based Practice in Pediatric Physical Therapy by BarryDocument14 pagesEvidence-Based Practice in Pediatric Physical Therapy by BarryFe TusNo ratings yet
- ActivityDocument2 pagesActivitysanchezanya34No ratings yet
- Methuselah-An Expert System For Diagnosis in Geriatric PsychiatryDocument12 pagesMethuselah-An Expert System For Diagnosis in Geriatric PsychiatryMilton MurilloNo ratings yet
- Meta Analysis Nursing Literature ReviewDocument10 pagesMeta Analysis Nursing Literature Reviewea46krj6100% (1)
- scholarly capstone paperDocument5 pagesscholarly capstone paperapi-738778945No ratings yet
- The Effect of Reducing The "Jumping To Conclusions"Document10 pagesThe Effect of Reducing The "Jumping To Conclusions"treyhanNo ratings yet
- Richards Et All (2020) Enseñanza ClínicaDocument33 pagesRichards Et All (2020) Enseñanza ClínicaCandela AriasNo ratings yet
- Van Scoyoc, S. (2017) - The Use and Misuse of Psychometrics in Clinical Settings. in B. Cripps (Ed.)Document17 pagesVan Scoyoc, S. (2017) - The Use and Misuse of Psychometrics in Clinical Settings. in B. Cripps (Ed.)susanvanscoyoc9870No ratings yet
- EBPDocument15 pagesEBPGaje SinghNo ratings yet
- ARTG - 2011 - PT Practice in Acute Care SettingDocument14 pagesARTG - 2011 - PT Practice in Acute Care SettingSM199021No ratings yet
- Current Perspectives: Research in Clinical Reasoning: Past History and Current TrendsDocument10 pagesCurrent Perspectives: Research in Clinical Reasoning: Past History and Current TrendsPablo IgnacioNo ratings yet
- 18 Hofmann & Hayes (In Press) The Future of Intervention Science - Process Based TherapyDocument41 pages18 Hofmann & Hayes (In Press) The Future of Intervention Science - Process Based TherapyCharles JacksonNo ratings yet
- Assignment Sheet Literature ReviewDocument3 pagesAssignment Sheet Literature ReviewMegan GuerreroNo ratings yet
- Shubham Gupta CVDocument2 pagesShubham Gupta CVPalash Ravi SrivastavaNo ratings yet
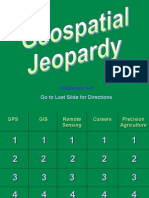
- Geospatial JeopardyDocument54 pagesGeospatial JeopardyrunnealsNo ratings yet
- Heidegger, Martin - On The Way To Language (Harper & Row, 1982) PDFDocument209 pagesHeidegger, Martin - On The Way To Language (Harper & Row, 1982) PDFammar RangoonwalaNo ratings yet
- Kohlbergs Moral DevelopmentDocument31 pagesKohlbergs Moral DevelopmentNiket RaikangorNo ratings yet
- Form - A5 - Student - REVISED PS 09012018 PDFDocument3 pagesForm - A5 - Student - REVISED PS 09012018 PDFLuis Daniel Córdoba AndradeNo ratings yet
- Curriculum Development: Process, Models and FoundationsDocument49 pagesCurriculum Development: Process, Models and FoundationsJhay Phee LlorenteNo ratings yet
- The 4 Sections and The 14 Principles of The Toyota WayDocument6 pagesThe 4 Sections and The 14 Principles of The Toyota WayJessica LaguatanNo ratings yet
- Lotf Argument EssayDocument4 pagesLotf Argument Essayapi-332982124No ratings yet
- Law and Poverty - The Legal System and PovertyDocument316 pagesLaw and Poverty - The Legal System and PovertyjitendraNo ratings yet
- Organisational Factors Affecting Employee Satisfaction in The Event IndustryDocument7 pagesOrganisational Factors Affecting Employee Satisfaction in The Event IndustryRitesh shresthaNo ratings yet
- BSA 4C 1 Factors Influenced The Decision of First Year Students of St. Vincent CollegeDocument44 pagesBSA 4C 1 Factors Influenced The Decision of First Year Students of St. Vincent CollegeVensen FuentesNo ratings yet
- Tarlac Agricultural University: Certificate of RegistrationDocument1 pageTarlac Agricultural University: Certificate of RegistrationMarian Kristina SabadoNo ratings yet
- Business Law SyllabusDocument11 pagesBusiness Law SyllabusTriệu Vy DươngNo ratings yet
- When Experience Turns Into NarrativeDocument87 pagesWhen Experience Turns Into NarrativeJudith SudholterNo ratings yet
- 21 Degrees SagittariusDocument11 pages21 Degrees Sagittariusstrength17No ratings yet
- Nexus Network Journal 2Document215 pagesNexus Network Journal 2Jelena MandićNo ratings yet
- EGCE 406 Bridge DesignDocument2 pagesEGCE 406 Bridge DesignNicole CollinsNo ratings yet
- Faculty Profile: 1. Work ExperienceDocument4 pagesFaculty Profile: 1. Work ExperienceMohana UMNo ratings yet
- Math 314 - LessonDocument17 pagesMath 314 - LessonNnahs Varcas-CasasNo ratings yet
- PHD Studentship - Predictive Modelling of Small Crack Formation in Superalloys at Cranfield UniversityDocument2 pagesPHD Studentship - Predictive Modelling of Small Crack Formation in Superalloys at Cranfield UniversityOzden IsbilirNo ratings yet
- 30 S. 2017Document7 pages30 S. 2017MaryroseNo ratings yet
- Apology Letter WorksheetDocument1 pageApology Letter WorksheetViral ShahNo ratings yet
- Simone de BeauvoirDocument20 pagesSimone de BeauvoirPrayogi AdiNo ratings yet
- The Ideology of PakistanDocument10 pagesThe Ideology of PakistanRaffay Malik MohsinNo ratings yet
- Celta Lesson Plan TP 3Document5 pagesCelta Lesson Plan TP 3mastro100100% (2)
- 2023 2024 Action Plan in ENGLISHDocument2 pages2023 2024 Action Plan in ENGLISHSa RahNo ratings yet
- SR - No Full Name Standard Seat Number Exam Time Medium SCH Code School NameDocument456 pagesSR - No Full Name Standard Seat Number Exam Time Medium SCH Code School NameBharat VyasNo ratings yet
- Barangay Ambassador: Republic of The Philippines Province of Benguet Municipality of TublayDocument3 pagesBarangay Ambassador: Republic of The Philippines Province of Benguet Municipality of TublayKathlyn Ablaza100% (1)
- Lesson 3-Cuentos de HadasDocument3 pagesLesson 3-Cuentos de Hadasapi-382813061No ratings yet