Professional Documents
Culture Documents
Garnacho Montero2005
Garnacho Montero2005
Uploaded by
EviOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Garnacho Montero2005
Garnacho Montero2005
Uploaded by
EviCopyright:
Available Formats
Effect of critical illness polyneuropathy on the withdrawal from
mechanical ventilation and the length of stay in septic patients*
Jose Garnacho-Montero, MD, PhD; Rosario Amaya-Villar, MD; Jose Luis García-Garmendía, MD, PhD;
Juan Madrazo-Osuna, MD; Carlos Ortiz-Leyba, MD, PhD
Objectives: No previous study has demonstrated whether crit- mechanical ventilation was significantly higher in patients who
ical illness polyneuropathy itself lengthens mechanical ventilation had developed critical illness polyneuropathy (median 34 days vs.
or whether this prolonged duration of ventilatory support is ex- 14 days, p < .001). The duration of the weaning period was also
plained by concomitant risk factors for weaning failure. Our significantly greater in patients with critical illness polyneurop-
objectives were to evaluate the impact of critical illness polyneu- athy (median 15 days vs. 2 days, p < .001) even though factors
ropathy on the length of mechanical ventilation after controlling suspected to influence the weaning process did not differ be-
for coexisting risk factors for weaning failure and to assess the tween these two groups. Multiple logistic regression analysis
impact of critical illness polyneuropathy on the length of the stay indicated that critical illness polyneuropathy was the only risk
in a cohort of septic patients. factor independently associated with weaning failure (odds ratio,
Design: Prospective cohort study. 15.4; 95% confidence interval, 4.55, 52.3; p < .001). Lengths of
Setting: Intensive care unit of a tertiary hospital. intensive care unit and hospital stays were significantly higher in
Patients: All patients with severe sepsis or septic shock who patients with critical illness polyneuropathy.
required mechanical ventilation for >7 days who were considered Conclusions: In critically ill septic patients, critical illness
ready to discontinue mechanical ventilation. polyneuropathy significantly increases the duration of mechanical
Interventions: Patients underwent a neurophysiologic evalua- ventilation and prolongs the lengths of intensive care unit and
tion at onset of weaning from mechanical ventilation. hospital stays. (Crit Care Med 2005; 33:349 –354)
Measurements and Main Results: Sixty-four critically ill septic KEY WORDS: sepsis; critical illness polyneuropathy; weaning;
patients were enrolled, and 34 developed critical illness polyneu- mechanical ventilation
ropathy (53.1%; 95% confidence interval, 40.2– 65.7%). Length of
C omplications that can delay Commonly, CIP is manifest by a fail- hospital stay, especially if patients are
recovery from critical illness ure to wean from mechanical ventilation. evaluated only after improvement from
are a major concern to critical In fact, it was originally described in pa- the acute illness and initiation of wean-
care physicians. Neuromuscu- tients with difficult weaning from venti- ing. In this subgroup of patients we can
lar disturbances are now well recognized latory support (2, 3). Various studies have certainly assess the clinical consequences
as complications that can affect long- attempted to determine whether CIP pro- of this neurologic disorder.
term ventilated patients, and the number longs the duration of mechanical ventila- We performed a prospective clinical
of reports has risen markedly in the last tion, and conflicting data have been ob- study enrolling patients with severe sep-
decades. Although diverse disorders can tained. We and others found that the sis or septic shock who required mechan-
afflict the peripheral nervous system in duration of mechanical ventilation was ical ventilation for ⱖ7 days who were
these patients, critical illness polyneu- significantly longer in patients suffering considered ready to discontinue mechan-
ropathy (CIP) is the most clearly defined from CIP compared with those who did ical ventilation. Our primary objective
neuromuscular complication in these pa- not (4 –7). In contrast, other studies was to evaluate the impact of CIP on the
tients (1). found that CIP did not prolong the dura- length of mechanical ventilation after
tion of mechanical ventilation or the controlling for coexisting risk factors for
length of the weaning time (8, 9). Never- weaning failure. Our secondary objectives
theless, to the best of our knowledge, were to assess the impact of CIP on the
*See also p. 452. length of the stay as well as to determine
From the Intensive Care Unit (JG-M, RA-V, CO-L) none of these previous studies have dem-
and Department of Clinical Neurophysiology (CO-L), onstrated that CIP itself prolongs me- the costs associated with this neurologic
Hospital Universitario Virgen del Rocío, Sevilla. Spain; chanical ventilation or whether this pro- complication.
and the Intensive Care Unit (JLG-G), Hospital San Juan longation of mechanical ventilation is the
de Dios del Aljarafe, Sevilla, Spain. MATERIALS AND METHODS
Supported, in part, by grant 154/97 from Conse-
effect of concurrent risk factors for wean-
jería de Salud de la Junta de Andalucía. ing failure. Hospital. This is a prospective study car-
Copyright © 2005 by the Society of Critical Care Until now, little information has been ried out in the intensive care unit (ICU) of the
Medicine and Lippincott Williams & Wilkins available concerning the impact of CIP on Hospital Virgen del Rocio from July 1, 1999, to
DOI: 10.1097/01.CCM.0000153521.41848.7E in-hospital mortality and the length of December 31, 2002. This is a medical-surgical
Crit Care Med 2005 Vol. 33, No. 2 349
unit in a large university hospital. Trauma and chanical ventilation was not possible, a percu- The protocol of study has been described
neurosurgical patients are admitted to an- taneous tracheostomy was performed (12). elsewhere (7). Briefly, the study included mea-
other unit, and these patients were not in- The duration of mechanical ventilation surement of motor nerve conduction (median,
cluded in this protocol. Written consent was was recorded. The day of the beginning of peroneal, and tibial nerves); calculation of
obtained from patients’ relatives, and the Eth- mechanical ventilation, the date of the onset conduction velocities, amplitude, and shape of
ical Committee of the Hospital Virgen del Ro- of weaning from mechanical ventilation, the the compound muscle action potential; mea-
cio approved this study. date of disconnection from the ventilator, and surement of distal latencies; and repetitive
Patients. All patients with severe sepsis or the need of reintubation were recorded. The nerve stimulation. In addition, sensory nerve
septic shock following American College of reason for reintubation was also noted (13). action potential and velocity conduction of the
Chest Physicians/Society of Critical Care Med- Extubation or spontaneous ventilation sural nerve and the sensory median nerve
icine criteria (10) who required mechanical through a tracheostomy marked the end of were also recorded. Signs of denervation, such
ventilation for ⱖ7 days were evaluated. A pa- mechanical ventilation. The weaning failure as fibrillation potentials and positive waves in
tient was included in this study when the group consisted of all patients in whom, after muscles, were also sought in four muscles
attending physician considered that the pa- trials of extubation, a tracheostomy was per- (deltoid, quadriceps femoris, first dorsal inter-
tient was stabilized and ready to be weaned formed because of the impossibility of discon- osseus, and tibialis anterior muscle) using
from the ventilator. The patients included in tinuation from mechanical ventilation and needle electromyography.
this protocol were followed up until death or those patients in whom extubation failed and CIP was diagnosed when signs of acute
hospital discharge. who required reintubation (14). axonal injuries were present: reduced com-
Excluded were patients ⬍18 yrs old; preg- Demographic variables of all patients en- pound muscle action potential and sensory
nant patients; patients intubated for exacerba- rolled in this study were recorded: age, gender, nerve action potential amplitudes, preserva-
tion of chronic obstructive pulmonary disease; and dates of admission and discharge from the tion of the speed of impulse conduction and
patients with a history of neuromuscular dis- ICU and the hospital. Severity of illness was the distal latencies, and signs of denervation
ease, liver cirrhosis, and end-stage renal dis- evaluated by the Acute Physiology and in at least one of the explored muscles (20).
ease; and patients infected with human immu- Chronic Health Evaluation (APACHE) II score Statistical Analysis. Comparisons between
nodeficiency virus. Routinely, the patient or, patients with CIP and without CIP were ac-
(15) considering the worst data point of the
most frequently, close relatives were asked complished using unpaired Student’s t-test for
first 24 hrs in the ICU. At the time of admis-
about signs and symptoms of preexisting neu- parametric continuous variables after correc-
sion, severity of organ failure was evaluated by
romuscular disease, and the patient was ex- tion for equality of variance (Levene’s test) and
the Sequential Organ Failure Assessment
cluded from the study if previous symptoms Mann-Whitney U test for nonparametric con-
(SOFA) score (16). Both scores were also re-
were reported. tinuous variables. Categorical variables were
corded at the onset of weaning.
All patients received standard supportive analyzed with Pearson’s chi-square test, ex-
Detailed information of total doses of sed-
treatment including surgical treatment of the cept where small samples required the use of
ative drugs administered since admission to
focus of infection if necessary, fluid resuscita- Fisher’s exact test. The ␣ level was set at .05.
the ICU was recorded. Intravenous midazolam
tion, vasoactive drugs, antimicrobial therapy, All p values were two-sided.
was interrupted when the patient’s clinical The Kaplan-Meier method was used to
and nutritional support. The sedation protocol
condition had improved and weaning was con- compare the duration of weaning period and
included intravenous midazolam (Dormicum,
sidered indicated. The following conditions the length of hospital stay between patients
Roche, Madrid, Spain) plus morphine both in
that were judged to be clinically valuable as with and without CIP; comparisons between
continuous drips. Muscle relaxant use was left
factors that could hinder the weaning from groups were made using log-rank tests.
to the discretion of the physician in charge of
the patient. mechanical ventilation were also noted: previ- Univariate analysis comparing weaning
Study Design. Weaning from the ventila- ous history of chronic obstructive pulmonary failure group with successful weaning group
tory support was initiated when the attending disease as defined by the APACHE II score was performed as previously indicated. A mul-
physician considered that the patient was sta- (15), active smoker (17), cardiac insufficiency tivariate analysis using logistic regression
bilized and ready to be weaned from the ven- (as defined by the APACHE II score), morbid analysis was used to evaluate independent risk
tilator. Daily the attending physician assessed obesity (body mass index ⬎40), and under- factors for weaning failure. The variables in-
the patient’s readiness for liberation from me- weight (body mass index ⬍20) (18). Body mass cluded in the multivariate analysis were those
chanical ventilation. index was defined as the ratio of weight in with significance levels of p ⬍ .10 in univari-
General criteria to be enrolled in this study kilograms divided by the square of height in ate analysis. The model was constructed using
were adequate gas exchange (arterial oxygen meters. a forward stepwise method with the likelihood
saturation ⱖ90% for an inspired oxygen frac- The occurrence of ventilator-associated ratio test. The presence of collinearity in the
tion ⱕ0.4, with a positive end-expiratory pres- pneumonia was also recorded. Ventilator- model was evaluated using the tolerance and
sure ⱕ5 cm H2O), body temperature ⬍38°C, associated pneumonia diagnosis required ra- variance inflation factor analysis followed by
hemoglobin level ⬎9 g/dL, and ability to fol- diographic appearance of a new and persistent testing the condition indexes. No condition
low simple commands. Patients were sitting in pulmonary infiltrate and at least two of the index ⬎15 was found, so the variance propor-
their beds at 45° from the horizontal, and following criteria: temperature ⬎38°C or tions were not examined. The odds ratio and
weaning was performed by a 2-hr trial of spon- ⬍35.5°C, leukocytosis ⬎12,000 cells/mm3 or corresponding 95% confidence intervals were
taneous (T-piece) breathing following the pro- leukopenia ⬍4,000 cells/mm3, and purulent also calculated (21).
tocol described by Esteban et al. (11). If extu- bronchial secretions. In these patients, a bron-
bation was not achieved with this method, the choscopy with protected brush or a quantita-
weaning could be continued either with T- tive tracheal aspirate was carried out to obtain RESULTS
piece trials or with pressure-support ventila- microbiological documentation (19).
Description of Patients. During the
tion: progressive reduction of pressure sup- Neurophysiologic Studies. A neurophysio-
logic study (electroneurogram and needle study period, 139 patients fulfilled inclu-
port in steps of 2 cm of water every 2 hrs until
a pressure of 5 cm of water was reached. Two electromyography) was performed at onset of sion criteria and underwent mechanical
different ventilators were used throughout the weaning from mechanical ventilation. The ventilation for ⱖ7 days. Sixty-nine pa-
study period: Servo Ventilator 300 (Siemens, same investigator (JMO), who was unaware of tients (44 males and 25 females) died
Madrid, Spain) and EVITA2 dura (Dräger, Ma- the patient’s medical condition, carried out all before discontinuation from mechanical
drid, Spain). When discontinuation from me- these studies. ventilation could be started. The mean
350 Crit Care Med 2005 Vol. 33, No. 2
APACHE II score on admission of these dian, 22 hrs; range, 1, 96) whereas only cation: 27 of 34 (79.4%) vs. six of 30
69 patients was 22.2 (6.5). Therefore, six- four (13.3%) of the patients without CIP (20%, p ⬍ .0001).
ty-eight patients were assessed although required reintubation (median, 24 hrs; ICU mortality was not statistically dif-
only 64 were finally analyzed (39 males range, 5, 46) in the same period (p ⬍ .05). ferent (seven of 34 [20.6%] patients with
and 25 females): One patient was prema- Reasons for reintubation in these 18 pa- CIP vs. three of 30 [10%] patients with-
turely transferred to another hospital, tients are listed in Table 2. Tracheostomy out CIP; p ⫽ .31), whereas in-hospital
and in three patients the weaning process was performed in 21 patients (61.8%) mortality was significantly higher in pa-
was abandoned because of a complication with CIP and only in four (13.3%) of the tients with CIP (16 of 34 [47.1%)] vs. six
not related to disconnection from me- patients without CIP (p ⬍ .05). Weaning of 30 [20%]; p ⫽ 0.03).
chanical ventilation (suture leakage in failure was significantly more frequent in Lengths of ICU and hospital stays were
two patients and a pancreatic abscess that
patients who developed CIP than in those significantly higher in patients with CIP
required surgical drainage in one pa-
subjects who did not present this compli- (Table 3). Duration of hospitalization af-
tient).
All patients presented severe sepsis or
septic shock. The primary diagnoses were
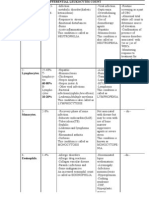
abdominal sepsis (n ⫽ 30), pneumonia (n Table 1. Univariate analysis comparing patients with and without critical illness polyneuropathy (CIP)
⫽ 21), urosepsis (n ⫽ 5), sepsis of un-
known origin (n ⫽ 5), and others (n ⫽ 3). CIP (n ⫽ 34) No CIP (n ⫽ 30) p
The mean APACHE II score on admission
Age, yrsa 61.1 (14.9) 61.5 (13.1) .9
was 18.6 (6.5) and the mean SOFA score APACHE II at admissiona 19.3 (6.9) 17.7 (5.9) .3
of the first 24 hrs in the unit was 7.2 (4). SOFA at admissiona 7.2 (4.3) 7.2 (3.5) 1
Comparison of CIP and Control Pa- APACHE II (onset of weaning)a 12.5 (4.6) 12.5 (4.4) 1
tients. CIP occurred in 34 (53.1%; 95% SOFA (onset of weaning)a 4 (2.5) 4 (2.4) 1
Total dose of midazolama,b 4306 (7267) 1728 (2589) .06
confidence interval, 40.2– 65.7%) of the Total dose of morphinea,b 616 (1114) 182 (141) .03
prospectively monitored critically ill pa- Muscle relaxantsa,b 10 (29.4)c 3 (10)d .055
tients. Patients with CIP exhibited typical COPDe 3 (8.8) 6 (20) .3
signs of an acute sensorimotor axonal Active smokere 9 (26.5) 11 (36.7) .4
neuropathy. Cardiac insufficiencye 1 (2.9) 2 (6.7) .6
Morbid obesitye 5 (14.7) 2 (6.7) .4
The mean time (SD) elapsed between Underweighte 2 (5.9) 1 (3.3) 1
the onset of mechanical ventilation and VAPe 17 (50) 8 (26.7) .056
the beginning of weaning was 16.4 (8.1)
days in patients with CIP and 11.3 (4.5) APACHE, Acute Physiology and Chronic Health Evaluation; SOFA, Sequential Organ Failure
days in patients without CIP (p ⬍ .05). Assessment; COPD, chronic obstructive pulmonary disease; VAP, ventilator-associated pneumonia.
a
Patients in both groups had similar age, Results are expressed as mean (SD); bdoses in milligrams; cseven patients received vecuronium,
two patients received vecuronium and atracurium, and one patient received exclusively atracurium;
APACHE II score, and SOFA score in the d
these three patients received vecuronium; eresults are expressed as n (%).
first 24 hrs. The total dose of midazolam
received did not differ between the two
groups, but the amount of morphine was
significantly higher in patients with CIP
(p ⬍ .05). The other conditions evaluated
as factors that may impede weaning did
not differ between patients with or with-
out CIP (Table 1). The method of weaning
was a 2-hr trial of spontaneous (T-piece)
breathing in 56 patients and the gradual
reduction of pressure support in eight
patients (four with CIP and four without
CIP).
Length of mechanical ventilation was
significantly higher in patients who de-
veloped CIP: median 34 (range 12–99)
days vs. 14 (7– 44) days (p ⬍ .001). The
duration of the weaning period was also
significantly greater in patients with CIP:
median 15 (1–74) days vs. 2 (0 –29) days
(p ⬍ 0.001). Figure 1 shows that the
comparison of the length of weaning pe-
riod by Kaplan-Meier method was statis- Figure 1. Kaplan-Meier curves of probability of remaining under mechanical ventilation after the
tically significant (log-rank test, p ⬍ initiation of weaning for patients with critical illness polyneuropathy (solid lines) and without critical
.0001). illness polyneuropathy (dashed lines). The probability of weaning failure was significantly higher for
Of the 34 patients who developed CIP, patients with critical illness polyneuropathy. Log -rank test, p ⬍ .0001. Time denotes the period from
14 (41.2%) required reintubation (me- the onset of weaning process to final withdrawal of mechanical ventilation.
Crit Care Med 2005 Vol. 33, No. 2 351
Table 2. Reasons for reintubation in 18 patientsa
O
CIP (n ⫽ 14) No CIP (n ⫽ 4) ur study con-
Hypoxemia 8 3 firms that criti-
Increased respiratory work 7 1
Impaired clearance of secretions 6 1 cal illness poly-
Decreased consciousness 3 1
Atelectasis 2 0 neuropathy significantly
Respiratory acidosis 2 1
Upper airway obstruction 0 1 prolongs the duration of me-
Cardiac failure 1 0
CIP, critical illness polyneuropathy.
chanical ventilation and is
a
More than one cause could be diagnosed in a single patient. an independent risk factor
for weaning failure in criti-
Table 3. Comparisons of the lengths of stays of patients with and without critical illness polyneurop-
athy (CIP) cally ill septic patients.
CIP (n ⫽ 34) No CIP (n ⫽ 30) p
DOH before admission to ICU 1.5 (0–73) 1 (0–60) .09 from the acute illness and were not ready
DOH before the onset of weaning 15.5 (7–42) 12 (7–29) ⬍.01 to be weaned off the ventilatory support.
DOH after the onset of weaning 56 (6–342) 18.5 (8–60) ⬍.0001 A recent study attempted to solve this
Length of ICU stay 46.5 (8–134) 22.5 (10–60) ⬍.0001
Length of hospital stay 85 (20–370) 33 (14–106) ⬍.0001
question by evaluating exclusively pa-
tients with a satisfactory level of con-
DOH, duration of hospitalization; ICU, intensive care unit. sciousness. The authors concluded that
mechanical ventilation was more pro-
ter the onset of weaning was also signif- chanical ventilation and, after controlling longed in those patients who developed
icantly higher in patients with CIP than for other confounding variables, is an in- sensorimotor axonal neuropathy com-
in those without CIP. Figure 2 shows that dependent cause of weaning failure. Our pared with those who did not present this
the length of hospital stay was statisti- results also provide compelling data complication (23).
cally different in patients with and with- about the increase in the duration of hos- None of these studies was able to ad-
out CIP using the Kaplan-Meier analysis pital stay caused by this neurologic com- just for risk factors of weaning failure or
(log-rank test, p ⬍ .0001). plication. severity of illness. It is well recognized
Comparison of Failed vs. Successful Discontinuation from mechanical that the characteristics of patients and
Weaning Groups. The failed weaning the severity of illness at admission to the
ventilation begins when the precipitating
group consisted of 33 patients: 18 patients ICU are determinants of the duration of
cause is at least partially reversed. Never-
who required reintubation (eight of them mechanical ventilation (24).
theless, this process can fail in patients
were finally extubated and in ten patients Our results confirm that CIP signifi-
meeting weaning criteria, prolonging the
the tracheostomy was necessary because cantly prolongs the duration of mechan-
time of intubation and ventilatory sup-
successful extubation was not achieved) ical ventilation and weaning time. In our
port. Diverse underlying conditions or
and 15 patients in whom the extubation series, the duration of ventilatory support
complications occurring during the pe- before the onset of weaning was signifi-
was not possible and tracheostomy was in- riod of mechanical ventilation can lead to
dicated because of prolonged mechanical cantly longer in patients with the diagno-
this weaning failure. sis of CIP than in those subjects who did
ventilation and impossibility of liberation CIP is a well-recognized cause of
from the ventilator. Twelve of these pa- not present this complication, which is in
weaning failure. Most investigators have agreement with other studies (3, 23).
tients (eight with CIP and four without concluded that the length of mechanical
CIP) were discharged from the ICU with the However, given that the weaning period
ventilation was significantly higher in pa- was also significantly prolonged in pa-
tracheostomy tube in place. This failed
tients with CIP than in patients who did tients with CIP, the longer duration of
weaning group was compared with the rest
not develop this complication although ventilatory support observed in CIP pa-
of the patients (n ⫽ 31) who were suc-
the duration of weaning time was not tients can be attributed to this neurologic
cessfully weaned from the ventilator. Uni-
assessed (4, 6, 7). Two studies specifically abnormality and not to the period elapsed
variate analysis is presented in Table 4.
evaluated the length of weaning period in between the onset of mechanical ventila-
Using multiple logistic regression analy-
patients with CIP obtaining conflicting tion and the beginning of weaning.
sis, CIP was the only risk factor indepen-
dently associated with weaning failure results (5, 8). Likewise, the severity of The occurrence of reintubation in the
(odds ratio, 15.4; 95% confidence inter- conduction abnormalities did not corre- group of patients who did not present CIP
val, 4.55–52.3; p ⬍ .001). late with the length of mechanical venti- (13.5%) is similar to the rate reported
lation or the duration of stay in the ICU previously (14). This rate was signifi-
in 62 patients with the diagnosis of CIP cantly greater in patients with CIP, which
DISCUSSION
(22). may influence the poor outcome of these
In this prospective study, we establish Moreover, many of the patients in- patients. Reintubation has been indepen-
that CIP increases the duration of me- cluded in these studies had not recovered dently associated with mortality during
352 Crit Care Med 2005 Vol. 33, No. 2
discharged alive from the ICU. This find-
ing is of extraordinary importance in view
of the economic burden that it may rep-
resent. Moreover, we cannot overlook
that symptoms due to CIP can persist for
a considerable period of time, and there-
fore these patients may require medical
care for years (4, 27, 28).
Our study has several limitations.
First, only patients with severe sepsis and
septic shock were included in this study.
Consequently, it is unknown whether our
findings can be generalized to other crit-
ically ill patients. Second, we did not
measure lung function variables, which
may have influenced the weaning pro-
cess. Third, we did not assess the associ-
ation between the prolongation of me-
chanical ventilation and the severity of
CIP. Despite all these limitations, our re-
sults shed light on the precise contribu-
Figure 2. Kaplan-Meier curves comparing the length of hospital stay in patients with critical illness tion of CIP to delayed weaning from me-
polyneuropathy (solid lines) and without critical illness polyneuropathy (dashed lines). The length of chanical ventilation in critically ill septic
hospital stay in the whole group was significantly longer in patients with critical illness polyneurop- patients.
athy than in patients who did not develop this neurologic complication. Log-rank test, p ⬍ .0001.
CONCLUSIONS
Table 4. Comparisons of patients who failed weaning with patients successfully extubated
Our study confirms that CIP signifi-
Failed Weaning Successful Weaning cantly prolongs the duration of mechan-
(n ⫽ 33) (n ⫽ 31) p ical ventilation and is an independent risk
factor for weaning failure in critically ill
Age, yrsa 62.1 (13.8) 60.4 (14.3) .6
APACHE II at admissiona 19.5 (6.9) 17.7 (6) .3 septic patients. These findings suggest
SOFA at admissiona 7.2 (3.9) 7.1 (4.1) .9 that CIP should be taken into account in
APACHE II (onset of weaning)a 12.5 (4.2) 12.7 (4.7) .9 clinical trials comparing different wean-
SOFA (onset of weaning)a 3.7 (2.3) 4.3 (2.5) .4 ing modes or in studies evaluating com-
Total dose of midazolama,b 3106 (6267) 2128 (3081) .4
Total dose of morphinea,b 610 (1136) 203 (148) .09
plications of mechanical ventilation in
Muscle relaxantsa,b 8 (24.2)c 5 (16.1)d .42 septic patients. CIP also accounts for ex-
CIPe 27 (81.8) 7 (22.6) ⬍.0001 tended ICU and hospital stays. Further
COPDe 5 (15.2) 4 (12.9) .8 studies should focus on specific interven-
Active smokere 11 (33.3) 9 (29) 7 tions (e.g., weaning protocols or rehabil-
Cardiac insufficiencye 1 (3) 2 (6.5) 5
Morbid obesitye 4 (12.1) 3 (9.7) 7 itation programs) that could help to im-
Underweighte 2 (6.1) 1 (3.2) 1 prove the poor prognosis of these
VAPe 18 (54.5) 7 (22.6) .009 patients.
APACHE, Acute Physiology and Chronic Health Evaluation; SOFA, Sequential Organ Failure
Assessment; CIP, critical illness polyneuropathy; COPD, chronic obstructive pulmonary disease; VAP, REFERENCES
ventilator-associated pneumonia. 1. Garnacho-Montero J, Madrazo-Osuna J,
a
Results are expressed as mean (SD); bdoses in milligrams; cfive patients received vecuronium, two García Garmendia JL, et al: Neuromuscular
patients received vecuronium and atracurium, and one patient received exclusively atracurium; dthese disorders of the critically ill patient. Clin
five patients received vecuronium; eresults are expressed as n (%). Pulm Med 2001; 8:354 –359
2. Bolton CF, Gilbert JJ, Hahn AF, et al: Poly-
neuropathy in critically ill patient. J Neurol
hospitalization (25). However, we consid- Moreover, after adjustment for con- Neurosurg Psych 1984; 47:1223–1231
ered reintubation in the ICU, whereas the founding variables, CIP was the only inde- 3. Witt NJ, Zochodne DW, Bolton CF, et al:
majority of the previous studies only con- pendent risk factor for weaning failure. In Peripheral nerve function in sepsis and mul-
sidered reintubation in the following 48 this cohort of critically ill septic patients, tiple organ failure. Chest 1991; 99:176 –184
4. Leijten FSS, Harinck-De Weerd JE, Poort-
or 72 hrs. Our rationalization was that CIP increases ⬎15 times the risk of wean-
vliet DCJ, et al: The role of polyneuropathy in
CIP persists for a large period of time, ing failure. This finding may also explain
motor convalescence after prolonged me-
and CIP has even been described as the the poor outcome of patients with CIP, be- chanical ventilation. JAMA 1995; 274:
cause of ICU readmission because of cause weaning failure has been previously as- 1221–1225
acute neuromuscular respiratory failure sociated with an increased risk of death (14). 5. Druschky A, Herkert M, Radespiel-Tröger M,
after ICU discharge in patients success- CIP significantly lengthens the dura- et al: Critical illness polyneuropathy: clinical
fully weaned from ventilation (26). tion of hospital stay in those patients findings and cell culture assay of neurotox-
Crit Care Med 2005 Vol. 33, No. 2 353
icity assessed by a prospective study. Inten- predictions and outcomes for patients re- 21. Hosmer DW, Lemeshow SA. 1989. Applied
sive Care Med 2001; 27:686 – 693 quiring tracheostomy. Crit Care Med 1999; logistic regression. New York: John Wiley.
6. Thiele RI, Jakob H, Hund E, et al: Sepsis and 27:1714 –1720 22. Zifko UA, Zipko HT, Bolton CF: Clinical and
catecholamine support are the major risk 13. Esteban A, Alia I, Tobin MJ, et al: Effect of electrophysiological findings in critical ill-
factors for critical illness polyneuropathy af- spontaneous breathing trial duration on out- ness polyneuropathy. J Neurol Sci 1998; 159:
ter open heart surgery. Thorac Cardiovasc come of attempts to discontinue mechanical 186 –193
Surg 2000; 48:145–150 ventilation. Am J Respir Crit Care Med 1999; 23. De Jonghe B, Sharshar T, Lefaucheur JP, et
7. Garnacho-Montero J, Madrazo-Osuna J, 159:512–518 al: Paresis acquired in the intensive care
García Garmendia JL, et al: Critical illness 14. Epstein SK, Ciubotaru RL, Wong JB: Effect unit. A prospective multicenter study. JAMA
polyneuropathy: Risk factors and clinical of failed extubation on the outcome of me- 2002; 288:2859 –2867
consequences. A cohort study in septic pa- chanical ventilation. Chest 1997; 112: 24. Seneff MG, Zimmerman JE, Knaus WA, et al:
tients. Intensive Care Med 2001; 27: 186 –192 Predicting the duration of mechanical venti-
1288 –1296 15. Knaus WA, Draper EA, Wagner DP, et al: lation. The importance of disease and pa-
8. Leijten FSS, De Weerd AW, Poortvliet DCJ, et APACHE II, a severity of disease classification
tients characteristics. Chest 1996; 110:
al: Critical illness polyneuropathy in multi- system. Crit Care Med 1985; 13:818 – 829
469 – 479
ple organ dysfunction syndrome and wean- 16. Vincent JL, Moreno R, Takala J, et al: The
25. Epstein SK, Vuong V: Lack of influence of
ing from the ventilator. Intensive Care Med SOFA (Sepsis-related Organ Failure Assess-
gender on outcomes of mechanically venti-
1996; 22:856 – 861 ment) score to describe organ dysfunction/
lated medical ICI patients. Chest 1999; 116:
9. Sander HW, Saadeh PB, Chandswang N, et al: failure. Intensive Care Med 1996; 22:707–710
732–739
Diaphragmatic denervation in intensive care 17. Pittet D, Thiévent B, Wenzel RP, et al: Im-
unit patients. Electromyogr Clin Neuro- portance of pre-existing co-morbidities for 26. Latronico N, Guarneri B, Alongi S, et al:
physiol 1999; 39:3–5 prognosis of septicemia in critically ill pa- Acute neuromuscular respiratory failure af-
10. American College of Chest Physicians/ tients. Intensive Care Med 1993; 19:265–272 ter ICU discharge. Intensive Care Med 1999;
Society of Critical Care Medicine Consensus 18. Willet WC, Dietz WH, Colditz GA: Guidelines 25:1302–1306
Committee: Definition for sepsis and organ for healthy weight. N Engl J Med 1999; 341: 27. De Seze M, Petit H, Wiart L, et al: Critical
failures and guidelines for the use of innova- 427– 434 illness polyneuropathy. A 2-year follow-up
tive therapies in sepsis. Chest 1992; 101: 19. Meduri GU: Diagnosis and differential diag- study in 19 severe cases. Eur Neurol 2000;
1658 –1662 nosis of ventilator-associated pneumonia. 43:61– 69
11. Esteban A, Frutos F, Tobin MJ, et al: A com- Clin Chest Med 1995; 16:61–93 28. Fletcher SN, Kennedy DD, Ghosh IR, et al:
parison of four methods of weaning patients 20. Bolton CF: Sepsis and the systemic inflam- Persistent neuromuscular and neurophysio-
from mechanical ventilation. N Engl J Med matory response syndrome: Neuromuscular logic abnormalities in long-term survivors of
1995; 332:345–350 manifestations. Crit Care Med 1996; 24: prolonged critical illness. Crit Care Med
12. Kollef MH, Aherns TA, Shanon W: Clinical 1408 –1416 2003; 31:1012–1106
354 Crit Care Med 2005 Vol. 33, No. 2
You might also like
- 2022 Stroke Lecture (Updated Guidelines)Document54 pages2022 Stroke Lecture (Updated Guidelines)Meccar Moniem H. ElinoNo ratings yet
- Management of OSCC CaseDocument40 pagesManagement of OSCC CaseMagdalene Choo Yenli100% (1)
- 110schweickert2009 PDFDocument9 pages110schweickert2009 PDFJulieta EvangelistaNo ratings yet
- Family Health Nursing - Problem Identification Scale For Ranking Health ProblemsDocument20 pagesFamily Health Nursing - Problem Identification Scale For Ranking Health ProblemsKimberly OlarteNo ratings yet
- 11-Vital Signs Unit 12 To 17Document74 pages11-Vital Signs Unit 12 To 17Rashid HussainNo ratings yet
- Extubacion en NeurocriticoDocument3 pagesExtubacion en NeurocriticoJuan Soto FarfanNo ratings yet
- 5 Outcome of Mechanically Ventilated Patients Who Require A TracheostomyDocument9 pages5 Outcome of Mechanically Ventilated Patients Who Require A TracheostomyIsabelNo ratings yet
- Peñuelas Et Al 2011Document8 pagesPeñuelas Et Al 2011GustavoGarcíaNo ratings yet
- Syok Septik - ICU-AWDocument12 pagesSyok Septik - ICU-AWArmi ZakaNo ratings yet
- Outcome of Patients Undergoing Prolonged Mechanical Ventilation (Crit Care Med 2007)Document7 pagesOutcome of Patients Undergoing Prolonged Mechanical Ventilation (Crit Care Med 2007)alexgonzalezherNo ratings yet
- Extubation in Neurocritical Care Patients: Lesson Learned: Understanding The DiseaseDocument3 pagesExtubation in Neurocritical Care Patients: Lesson Learned: Understanding The DiseaseIsabel VillalobosNo ratings yet
- Physiotherapy and Weaning From Prolonged Mechanical VentilationDocument9 pagesPhysiotherapy and Weaning From Prolonged Mechanical VentilationdanielNo ratings yet
- The Long-Term Outcome of Adult Epilepsy Surgery, Patterns of Seizure Remission, and Relapse - A Cohort StudyDocument8 pagesThe Long-Term Outcome of Adult Epilepsy Surgery, Patterns of Seizure Remission, and Relapse - A Cohort StudyNeurologia homicNo ratings yet
- Extending The Preoxygenation Period From 4 To 8 Mins in Critically Ill Patients Undergoing Emergency IntubationDocument4 pagesExtending The Preoxygenation Period From 4 To 8 Mins in Critically Ill Patients Undergoing Emergency IntubationLuis ArdilaNo ratings yet
- Research Article: Prone Position After Liberation From Prolonged Mechanical Ventilation in COVID-19 Respiratory FailureDocument7 pagesResearch Article: Prone Position After Liberation From Prolonged Mechanical Ventilation in COVID-19 Respiratory FailurewiwiNo ratings yet
- Plotnikow, Epidemiologia de Ventilacion Mecanica en Argentina, 2021Document11 pagesPlotnikow, Epidemiologia de Ventilacion Mecanica en Argentina, 2021diego bustosNo ratings yet
- Ferrer 2006Document7 pagesFerrer 2006Fermin LombardiaNo ratings yet
- 12Hiệu quả mở kq sớm pt gộp 2015Document10 pages12Hiệu quả mở kq sớm pt gộp 2015Cường Nguyễn HùngNo ratings yet
- Mechanical Ventilator Discontinuation Process: Lingye Chen,, Daniel Gilstrap,, Christopher E. CoxDocument7 pagesMechanical Ventilator Discontinuation Process: Lingye Chen,, Daniel Gilstrap,, Christopher E. CoxGhost11mNo ratings yet
- Debilidad Gral y DiafragmaticaDocument9 pagesDebilidad Gral y DiafragmaticaterapiafisicapilaresNo ratings yet
- Journal of Critical Care: ArticleinfoDocument7 pagesJournal of Critical Care: ArticleinfoNindy CantikNo ratings yet
- Study of Mechanical Ventilation in ChildrenDocument5 pagesStudy of Mechanical Ventilation in ChildrenDwi Putri SekariniNo ratings yet
- Movilización y Recuperación Precoces en Pacientes Con Ventilación Mecánica en La UCI Un Estudio de Cohorte Prospectivo Binacional, MulticéntricoDocument10 pagesMovilización y Recuperación Precoces en Pacientes Con Ventilación Mecánica en La UCI Un Estudio de Cohorte Prospectivo Binacional, MulticéntricoByron VarasNo ratings yet
- Weaning Predictors Do Not Predict Extubation Failure in Simple-To-Wean PatientsDocument8 pagesWeaning Predictors Do Not Predict Extubation Failure in Simple-To-Wean PatientsClaudia IsabelNo ratings yet
- Debilidad Gral y DiafragmaticaDocument9 pagesDebilidad Gral y DiafragmaticaGustavoGarcíaNo ratings yet
- Readmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsDocument9 pagesReadmission and Other Adverse Events After Transsphenoidal Surgery: Prevalence, Timing, and Predictive FactorsbobNo ratings yet
- Geriatric Nursing: Canan Karadas, MSC, Leyla Ozdemir, RN, PHDDocument6 pagesGeriatric Nursing: Canan Karadas, MSC, Leyla Ozdemir, RN, PHDCharah IC NuRseNo ratings yet
- 2019 A Phase II Randomized Controlled Trial For Lung and Diaphragm Protective VentilationDocument7 pages2019 A Phase II Randomized Controlled Trial For Lung and Diaphragm Protective VentilationwilsonmauriciolozanoNo ratings yet
- 2015 Article 159Document8 pages2015 Article 159andri anaNo ratings yet
- J of Ultrasound Medicine - 2023 - Marques - Ultrasonography To Access Diaphragm Dysfunction and Predict The Success ofDocument14 pagesJ of Ultrasound Medicine - 2023 - Marques - Ultrasonography To Access Diaphragm Dysfunction and Predict The Success ofÁlvaro Raúl Conto MorenoNo ratings yet
- TMI - Capacidade Funcional Após Artéria Coronária de Cirurgia de Revascularização em Pacientes de Alto RiscoDocument6 pagesTMI - Capacidade Funcional Após Artéria Coronária de Cirurgia de Revascularização em Pacientes de Alto Risco56zw8rqq6jNo ratings yet
- PHYS THER-2013-Clark-186-96Document13 pagesPHYS THER-2013-Clark-186-96Ratih Dwi LestariNo ratings yet
- BackgroundDocument42 pagesBackgroundjineNo ratings yet
- Lansford 2007Document6 pagesLansford 2007Danielle Santos RodriguesNo ratings yet
- 10 1097@CCM 0b013e31818b35f2Document7 pages10 1097@CCM 0b013e31818b35f2omarihuanoNo ratings yet
- Virtual Reality On Pulmonary Function and Functional Independence After Coronary Artery Bypass Grafting - Clinical TrialDocument7 pagesVirtual Reality On Pulmonary Function and Functional Independence After Coronary Artery Bypass Grafting - Clinical TrialDaniel Lago BorgesNo ratings yet
- 30 54 1 SMDocument7 pages30 54 1 SMNYONGKERNo ratings yet
- Jurnal KardioDocument5 pagesJurnal KardiomadeNo ratings yet
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDocument9 pagesResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998No ratings yet
- Nakashima2013 Article CharacterizingTheNeedForTracheDocument7 pagesNakashima2013 Article CharacterizingTheNeedForTracheCristian GiovanniNo ratings yet
- Meroni2017 CompressedDocument8 pagesMeroni2017 Compresseddayllyn iglesiasNo ratings yet
- Rapid Training of Healthcare Staff For Protected Cardiopulmonary Resuscitation in The COVID-19 PandemicDocument3 pagesRapid Training of Healthcare Staff For Protected Cardiopulmonary Resuscitation in The COVID-19 PandemicRicardo BarreraNo ratings yet
- Large Scale Implementation of A Respiratory Therapist WESLEY ELYDocument8 pagesLarge Scale Implementation of A Respiratory Therapist WESLEY ELYKinesio FernandezNo ratings yet
- 143 Full PDFDocument5 pages143 Full PDFVanshika GuptaNo ratings yet
- Danielle Karen Widjaja 22010113130175 Lap - Kti Bab2Document9 pagesDanielle Karen Widjaja 22010113130175 Lap - Kti Bab2Adelia DulanimoNo ratings yet
- Effect of Early Tracheostomy in Mechanically Ventilated PatientsDocument8 pagesEffect of Early Tracheostomy in Mechanically Ventilated PatientsManuel Cuevas EspinozaNo ratings yet
- 262 FullDocument10 pages262 FullDaniel IturriagaNo ratings yet
- Use of Ketorolac Is Associated With Decreased Pneumonia Following Rib FracturesDocument7 pagesUse of Ketorolac Is Associated With Decreased Pneumonia Following Rib Fracturesracut_khansatraNo ratings yet
- BMJ Open 2015 ZhangDocument10 pagesBMJ Open 2015 ZhangLuis CordovaNo ratings yet
- Achieving Sustainability in Reducing Unplanned Extubations in PICUDocument7 pagesAchieving Sustainability in Reducing Unplanned Extubations in PICUKevin Bazán TorrealvaNo ratings yet
- 2022-10# (PEERJ) RR in ECMODocument17 pages2022-10# (PEERJ) RR in ECMOjycntuNo ratings yet
- The Setscore To Predict Tracheostomy Need in Cerebrovascular Neurocritical Care PatientsDocument11 pagesThe Setscore To Predict Tracheostomy Need in Cerebrovascular Neurocritical Care PatientsLuis HernándezNo ratings yet
- 10effect of Early Vs Late Tracheostomy Placement On Survival in Patients Receiving Mechanical Ventilation The TracMan Randomized Trial 2013Document9 pages10effect of Early Vs Late Tracheostomy Placement On Survival in Patients Receiving Mechanical Ventilation The TracMan Randomized Trial 2013Cường Nguyễn HùngNo ratings yet
- Anesthesia Management in Respiratory DepressionDocument7 pagesAnesthesia Management in Respiratory DepressionGandita AnggoroNo ratings yet
- A Comprehensive Protocol For Ventilator Weaning and ExtubationDocument9 pagesA Comprehensive Protocol For Ventilator Weaning and ExtubationPaulaNo ratings yet
- Timing of Tracheostomy As A Determinant of Weaning Success inDocument7 pagesTiming of Tracheostomy As A Determinant of Weaning Success inlucas enderleNo ratings yet
- 10 1056@NEJMoa1812379Document12 pages10 1056@NEJMoa1812379alvaroNo ratings yet
- Extent, Risk Factors, and Outcome of Fluid Overload After Pediatric Heart SurgeryDocument9 pagesExtent, Risk Factors, and Outcome of Fluid Overload After Pediatric Heart SurgeryAngelica Lucero OrtizNo ratings yet
- Pre Hospital PDFDocument4 pagesPre Hospital PDFAndi Tri SutrisnoNo ratings yet
- Garnacho Montero2001Document9 pagesGarnacho Montero2001EviNo ratings yet
- Medical Complications After Stroke: A Multicenter StudyDocument8 pagesMedical Complications After Stroke: A Multicenter StudyVika AriliaNo ratings yet
- Jurding Paru 1Document12 pagesJurding Paru 1Clinton SudjonoNo ratings yet
- Piquet 2021Document8 pagesPiquet 2021Manuel Amade OvalleNo ratings yet
- Case Studies of Postoperative Complications after Digestive SurgeryFrom EverandCase Studies of Postoperative Complications after Digestive SurgeryNo ratings yet
- Ballve 2017Document10 pagesBallve 2017EviNo ratings yet
- Early Mobilization For Patient Use Mechanical VentilatorDocument17 pagesEarly Mobilization For Patient Use Mechanical VentilatorEviNo ratings yet
- Efect of EarlyDocument12 pagesEfect of EarlyEviNo ratings yet
- 10.1371@journal - Pone.0194967 Resiko JatuhDocument14 pages10.1371@journal - Pone.0194967 Resiko JatuhEviNo ratings yet
- Kizilarslanoglu 2016Document7 pagesKizilarslanoglu 2016EviNo ratings yet
- Sepsis 2019Document12 pagesSepsis 2019EviNo ratings yet
- Bed Rest and Myopathies: Arny A. Ferrando, Douglas Paddon-Jones and Robert R. WolfeDocument6 pagesBed Rest and Myopathies: Arny A. Ferrando, Douglas Paddon-Jones and Robert R. WolfeEviNo ratings yet
- Constitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyDocument12 pagesConstitutive Activation of MAPK Cascade in Acute Quadriplegic MyopathyEviNo ratings yet
- Yataco2019.Early Progressive Mobilization of Patients With EVD. Safety An FeasibilityDocument7 pagesYataco2019.Early Progressive Mobilization of Patients With EVD. Safety An FeasibilityEviNo ratings yet
- The Turkish Version of Pain Assessment in Advanced Dementia (PAINAD) ScaleDocument6 pagesThe Turkish Version of Pain Assessment in Advanced Dementia (PAINAD) ScaleEviNo ratings yet
- Garnacho Montero2001Document9 pagesGarnacho Montero2001EviNo ratings yet
- CBC Reference Value TableDocument2 pagesCBC Reference Value Tabletommy areanNo ratings yet
- This Study Resource WasDocument5 pagesThis Study Resource WasPriscilla SNo ratings yet
- Paper 3 Surgery Not Answered Till 2022Document288 pagesPaper 3 Surgery Not Answered Till 2022NEMO2322No ratings yet
- Naegele'S Rule and Age of Gestation: SourceDocument4 pagesNaegele'S Rule and Age of Gestation: SourceAlec AnonNo ratings yet
- Case Study Stroke RehabilitationDocument1 pageCase Study Stroke RehabilitationJanantik PandyaNo ratings yet
- Janie Jacobs Resume March 2019Document2 pagesJanie Jacobs Resume March 2019api-404179099No ratings yet
- Types of Immunity: Presented byDocument12 pagesTypes of Immunity: Presented byGayathri deviNo ratings yet
- COVID-19 Assessment & PPE Pre-Simulation Preparation 1. ReadingsDocument2 pagesCOVID-19 Assessment & PPE Pre-Simulation Preparation 1. ReadingsaliNo ratings yet
- FMGE Mission 200+ OBG Day 5 by DR Raina Chawla - 231113 - 160121Document152 pagesFMGE Mission 200+ OBG Day 5 by DR Raina Chawla - 231113 - 160121CastleKGNo ratings yet
- Rigor MortisDocument20 pagesRigor MortisMurali G RaoNo ratings yet
- Vaccines 09 01233 v2Document12 pagesVaccines 09 01233 v2Milica MilojevicNo ratings yet
- History of Emergency Medical ServicesDocument8 pagesHistory of Emergency Medical Servicesapi-310488610No ratings yet
- Rehab Exercises For Medial EpicondylitisDocument1 pageRehab Exercises For Medial Epicondylitisgaby14No ratings yet
- 1 Patient Assessment Form.Document3 pages1 Patient Assessment Form.Aina HaravataNo ratings yet
- ACLS QuizletDocument7 pagesACLS Quizletek.9006001No ratings yet
- Lung Cancer PathoDocument5 pagesLung Cancer PathoMahlonee LinNo ratings yet
- Asa Physical Status Classification System PDFDocument2 pagesAsa Physical Status Classification System PDFmawarni siahaanNo ratings yet
- Cardiac RehabilitationDocument28 pagesCardiac RehabilitationSajjal JohnsonNo ratings yet
- Basic Hospital Vocabulary: Part 1: Health ProfessionalsDocument6 pagesBasic Hospital Vocabulary: Part 1: Health ProfessionalsMatthias Dos SantosNo ratings yet
- Profile PDFDocument4 pagesProfile PDFsavan anvekarNo ratings yet
- The Use of Subcutaneous Omeprazole in The Treatment of Dyspepsia in Palliative Care PatientsDocument3 pagesThe Use of Subcutaneous Omeprazole in The Treatment of Dyspepsia in Palliative Care PatientscarinasheliapNo ratings yet
- Evergreen Niches For KDPDocument4 pagesEvergreen Niches For KDPSeiNo ratings yet
- Low Back PainDocument8 pagesLow Back PainLev KalikaNo ratings yet
- Lplpo Feb 2023Document3 pagesLplpo Feb 2023santika restiwaniNo ratings yet
- Differential Leukocytes CountDocument2 pagesDifferential Leukocytes CountSalmanNo ratings yet
- Article-Aman Kumar Singh-GNLU-8.12.2020Document12 pagesArticle-Aman Kumar Singh-GNLU-8.12.2020VeronicaNo ratings yet