0% found this document useful (0 votes)
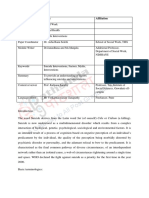
616 views9 pagesPSYC 6253 CBT Intake Form (Template) : Patient Name
Jacqueline is a 24-year-old female seeking counseling for depressive symptoms that have worsened over the past 3 months following a conflict with her friend Derek. She reports symptoms of depressed mood, lack of motivation, guilt, and difficulty concentrating. Jacqueline has a history of alcohol abuse but has maintained sobriety for two years. She was emotionally and physically abused by her mother as a child. The intake assessment indicates Jacqueline has moderately severe depression but no suicidal ideation. Her goals are to manage her depressive symptoms through CBT therapy before considering antidepressant medication again.
Uploaded by
Magishaa ThiyagarajahCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
616 views9 pagesPSYC 6253 CBT Intake Form (Template) : Patient Name
Jacqueline is a 24-year-old female seeking counseling for depressive symptoms that have worsened over the past 3 months following a conflict with her friend Derek. She reports symptoms of depressed mood, lack of motivation, guilt, and difficulty concentrating. Jacqueline has a history of alcohol abuse but has maintained sobriety for two years. She was emotionally and physically abused by her mother as a child. The intake assessment indicates Jacqueline has moderately severe depression but no suicidal ideation. Her goals are to manage her depressive symptoms through CBT therapy before considering antidepressant medication again.
Uploaded by
Magishaa ThiyagarajahCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
- Chief Complaint/Current Functioning: Describes the primary complaints and functional status of the patient, focusing on depressive symptoms and social withdrawal.
- Symptom Assessment: Summarizes symptoms including anxiety, anhedonia, and suicidal thoughts, detailing their impact on daily life.
- Medical History: Outlines medical background, including IBS and treatments tried, with medications and their effects.
- Family History: Explores family dynamics, history of mental health issues, and parental relationships affecting the patient.
- Stressors and Strengths: Analyzes emotional, relational, and personal strengths and stressors, with a table showcasing positive and negative influences.
- DSM Diagnoses: Confirms a diagnosis of Major Depressive Disorder, explaining diagnostic criteria and implications for treatment.
- Goals and Treatment Plan: Details therapeutic goals and strategies, structured around cognitive and behavioral interventions, and tracks progress through specific activities.