Professional Documents
Culture Documents
Head-Neck 1 2021 062520
Head-Neck 1 2021 062520
Uploaded by
ShebaTarigan0 ratings0% found this document useful (0 votes)
6 views4 pagesOriginal Title
Head-Neck_1_2021_062520
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views4 pagesHead-Neck 1 2021 062520
Head-Neck 1 2021 062520
Uploaded by
ShebaTariganCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
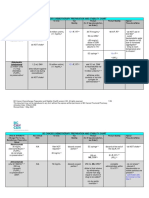
NCCN Guidelines for Head and Neck Cancers V.1.
2021 – Annual 06/25/2020
Guideline Page Institution Vote
Panel Discussion/References
and Request YES NO ABSTAIN ABSENT
SYST-A (2 of 4) Based on the review of the data in the noted 24 0 0 6
External request: reference, the panel consensus was to include
pembrolizumab as an option for advanced MSI-H
Submission from Merck & Co., Inc., on 03/20/20 to head and neck squamous cell carcinoma (non-
consider the inclusion of pembrolizumab in the treatment of nasopharygneal). This is a category 2A, useful in
advanced MSI-H head and neck squamous cell carcinoma certain circumstances recommendation.
be added as a category 2A based on the efficacy data from
the publication by Marabelle et al. Reference:
Marabelle et al. Efficacy of pembrolizumab in
patients with non-colorectal high microsatellite
instability/mismatch repair-deficient cancer:
results from the phase 2 KEYNOTE-158 study. J
Clin Oncol
38:1-10.
STST-A (2 of 4) Based on a review of the data and discussion, 0 24 0 6
External request: the panel consensus did not support the addition
of these specific recommendations in the
Submission from Merck & Co., Inc., on 04/29/20 to Guideline.
consider the inclusion of the updated dosing
recommendations for pembrolizumab, either 200 mg every
3 weeks or 400 mg every 6 weeks administered as a 30- See Submission for references.
minute intravenous (IV) infusion until disease progression,
unacceptable toxicity, or up to 24 months for the treatment
of adult patients with head and neck squamous cell
carcinoma (HNSCC).
SALI-B & NASO-B Based on a review of the data and discussion,
External request: the panel consensus supported the inclusion of
pembrolizumab as a treatment option for:
Submission from Merck & Co., Inc., on 06/17/20 to • Patients with advanced tumor 24 0 0 6
consider the inclusion of pembrolizumab as a treatment mutational burden-high (TMB-H)
option for patients with advanced tumor mutational burden- salivary gland tumors. This is a category
high (TMB-H) salivary gland tumors who have progressed 2A, useful in certain circumstances
following prior treatment and have no satisfactory recommendation.
alternative treatment. • Patients with TMB-H recurrent,
unresectable, or metastatic
Submissions from Foundation Medicine on 06/22/20 and nasopharyngeal cancers. This is a 24 0 0 6
09/15/20 to consider: category 2A, useful in certain
• Amend the algorithm for distant metastases on circumstances, subsequent-line therapy
page SALI-4 to recommend tumor mutational recommendation.
NCCN Guidelines for Head and Neck Cancers V.1.2021 – Annual 06/25/2020
burden (TMB) as determined by a validated and/or
FDA-approved assay to inform the use of The panel consensus did not support the addition
pembrolizumab and add a footnote referencing of a footnote recommending TMB as determined 0 24 0 6
Merino DM, et al. J Immunother Cancer by a validated and/or FDA-approved assay to
2020;8:e000147. inform the use of pembrolizumab.
• Add pembrolizumab as a treatment option for
patients with unresectable or metastatic salivary or Reference:
nasopharyngeal tumors with tissue tumor Marabelle A, Fakih M, Lopez J, et al. Association
mutational burden-high (TMB-H) ≥10 of tumour mutational burden with outcomes in
mutations/megabase, as determined by an FDA- patients with advanced solid tumours treated with
approved test, who have progressed following prior pembrolizumab: prospective biomarker analysis
treatment and who have no satisfactory alternative of the multicohort, open-label, phase 2
treatment options. KEYNOTE-158 study. Lancet Oncol.
2020;21(10):1353-1365.
NASO-B Based on the discussion, the panel consensus 24 0 0 6
Internal request: was to include carboplatin + RT followed by
carboplatin/5-FU as an option for patients with
Comment to consider the inclusion of recommendations for nasopharyngeal cancer if cisplatin ineligible or
cisplatin-ineligible patients. intolerant.
Multiple Pages Based on a review of the data and discussion, 24 0 0 6
External request: the panel consensus was to include the following
edits in the NCCN Head and Neck Guidelines
Submissions from ASTRO on 08/13/2019 and 05/28/20 to V.1.2021:
consider multiple recommendations for consideration. • ORPH-A (1 of 2):
• Throughout the guideline, IMRT should be o Added, “IMRT planning can consist
emphasized over 3D-CRT as the standard-of-care of sequential IMRT (S-IMRT) or
in mucosal H&N cancers treated with curative simultaneous integrated boost (SIB)
intent. techniques. Equivalent doses in 2Gy
• OR-2: There is a recommendation for resection of (EQD2) can be used to determine
primary (without neck dissection). Add detail in the appropriate fractionation schemes
decision tree on which patients this is appropriate when using SIB techniques.”
for. A depth of invasion cut off should be o Low to intermediate risk, modified:
considered. Page SURG-A, 6 of 9, indicates 44–50 Gy (2.0 Gy/fraction) used for
dissection should be strongly considered for >4 S-IMRT or the use of an anterior
mm, only used in selective situations for < 2 mm, neck field and to 54–63 Gy (1.6–1.8
and be subject to clinical judgement for 2-4 mm, Gy/fraction) when using SIB
which should be reflected on page OR-2 as well. techniques.
• ORPH-A: In the Principles of Radiation Therapy o Add “See discussion” in footnote 6.
(page ORPH-A 1 of 2), the guideline suggests 44- Information about cetuximab will be
50 Gy (2.0 Gy/fraction) for low to intermediate risk included in the Discussion section.
disease. This should be broken down further to
indicate that for IMRT a biologically equivalent
dose of approximately 50 Gy in 2 Gy fractions or
NCCN Guidelines for Head and Neck Cancers V.1.2021 – Annual 06/25/2020
slightly higher should be prescribed (e.g., 50 Gy [2 • ETHM-2: Revised adverse features in
Gy/fraction] or 54-56 Gy [1.54 Gy-1.63 Gy/fraction] footnote “o” for consideration of adjuvant
in a dose-painting fashion where all target volumes systemic therapy/RT: Adverse features
receive 33-35 fractions), or 44 Gy in 22 fractions if include positive margins, close margins
using a low neck matched AP field. (tumors adjacent to the cribriform plate and/or
• ORPH-A: In footnote 6 on page ORPH-A 1 of 2, medial wall of the orbit), unfavorable histology
the guideline discusses altered fractionation with (high grade, adenoid cystic), high-grade
chemotherapy. It should be expanded to lesions, and intracranial and/or intraorbital
specifically include cetuximab, now level 2B for use extension, cribriform plate location, medial
concurrently with RT. Alternate fractionation should wall of orbit location, perineural invasion, and
be suggested with concurrent cetuximab. lymphovascular space invasion.
• HYPO-A: The recommended fractionation scheme • ETHM-2: The panel consensus was to
with concurrent chemotherapy in hypopharyngeal consider the inclusion of
cancer is 70 Gy in 35 fractions, as no prospective induction/neoadjuvant chemotherapy as an
data has validated other regimens with concurrent option for T3-T4 ethmoid sinus tumors where
chemotherapy in the setting of hypopharyngeal upfront surgery or RT would compromise
cancer. organ function. (See Transparency dated
• GLOT-2/SUPRA-2: Select T3N0 patients should be 09/03/2020 for vote).
removed from the decision tree, as there is no • The panel consensus was not to include
obvious reason why a subset of T3N0 disease induction/neoadjuvant chemotherapy as an
should be treated with radiation alone over option for T3-T4 maxillary sinus tumors.
chemoradiation, given these patients were eligible • ADV-2/ADV-4: Add “+/- palliative RT or
for the VA Larynx and RTOG 91-11 trials, the latter palliative surgery” as an option for PS-2/3,
of which showed improved locoregional control and metastatic head and neck cancer.
laryngeal preservation outcomes with concurrent
chemotherapy. The panel consensus did not support the addition
• GLOT-2: Since the guideline groups T1 and T2 of any other specific recommendations.
tumors with T3 ones, systemic therapy and RT
should be recommended as another option for
post-operative patients with T1-T2, N0 or select
T3, N0 tumors and positive surgical margins.
• GLOT-3, GLOT-4, GLOT-6, SUPRA-3, SUPRA-8:
For T3 tumors requiring (amenable to) total
laryngectomy (N0-N3) and selected T4a patients
who decline surgery, the algorithm should reflect
that chemoradiation is preferred over induction
chemotherapy.
• Hypofractionation should be marked as preferred
for T2N0 (as it is for T1N0).
• ETHM-2: For ethmoid sinus cancers, the use of
postop RT for T1-2 cancers is based on features
including negative margins, favorable histology,
NCCN Guidelines for Head and Neck Cancers V.1.2021 – Annual 06/25/2020
central tumors, and low-grade tumors. Anatomic
location should be incorporated as another
consideration.
• ETHM/MAXI: For sinonasal cancers (ethmoid and
maxillary sinus tumor sections),
induction/neoadjuvant chemotherapy should be
added as an option for T3-T4 tumors where upfront
surgery or radiation would compromise organ
function (i.e., the orbit or skull base is involved
such that there would sacrifice of structures
surgically or to exceed dose tolerances with
radiation).
• ADV-2/ADV-4: Consider re-structuring the
algorithm for M1 disease. Patients with newly
diagnosed metastatic head and neck cancer with
limited systemic burden may benefit from
aggressive locoregional therapy based on analogy
from lung cancer data (such as SABR-COMET),
but the data specific to head and neck cancers are
limited.
• ADV-3: The indications for consideration of
postoperative chemoradiation should be specified
for previously irradiated patients and should
include patients with positive margins and
extranodal extension.
• ADV-4: Curative-intent reirradiation as part of initial
therapy should not be initially recommended for
patients with recurrent or persistent disease with
distant metastases.
SYST-A (EB-3) The NCCN Evidence Blocks™ have been
External request: updated to reflect the panel consensus.
Submission from Merck & Co., Inc., on 06/18/20 to
consider an increase in the number of Evidence Blocks for
efficacy of the regimen for pembrolizumab combination
therapy (pembrolizumab/platinum/5-FU).
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Asesmen GinekologiDocument15 pagesAsesmen GinekologiYumeko AiharaNo ratings yet
- Chemotherapy Sequencing Chart: Review Article Chemotherapy Administration SequenceDocument1 pageChemotherapy Sequencing Chart: Review Article Chemotherapy Administration SequencemubarakdxxNo ratings yet
- งานเคมีบ าบัด กลุ่มงานเภสัชกรรม โรงพยาบาลราชวิถี ตาราง การเตรียมยา และความคงตัวของยาเคมีบ าบัด Reconstitution PreparationDocument11 pagesงานเคมีบ าบัด กลุ่มงานเภสัชกรรม โรงพยาบาลราชวิถี ตาราง การเตรียมยา และความคงตัวของยาเคมีบ าบัด Reconstitution Preparationtotoil22No ratings yet
- Typhon Group Procedures Skills TotalsDocument3 pagesTyphon Group Procedures Skills Totalsapi-642376263No ratings yet
- 1 SMDocument6 pages1 SMolgaNo ratings yet
- SMRT Radiation Therapy IntroDocument18 pagesSMRT Radiation Therapy IntroDar WebNo ratings yet
- 681 FullDocument6 pages681 FullKurnia AnharNo ratings yet
- PosterDocument1 pagePosterNdha Nezz WoanNo ratings yet
- Chemo DrugsDocument4 pagesChemo DrugsFidel SantongNo ratings yet
- Chemo Stability Chart - AtoKDocument59 pagesChemo Stability Chart - AtoKAfifah Nur Diana PutriNo ratings yet
- 2021 Master Competency ListDocument1 page2021 Master Competency Listapi-574059920No ratings yet
- Advanced-Stagehodgkinlymphoma: by Joseph M. Connors, MDDocument5 pagesAdvanced-Stagehodgkinlymphoma: by Joseph M. Connors, MDJOHN LOPERANo ratings yet
- Result Analysis of Treatment Planning System BetweDocument6 pagesResult Analysis of Treatment Planning System BetweAnita FitrianaNo ratings yet
- Kanker ParuDocument10 pagesKanker Parunovi hidayahNo ratings yet
- Contoh EBLDocument4 pagesContoh EBLsalsabila fabianca alsaidNo ratings yet
- Brach y TherapyDocument3 pagesBrach y Therapydincy danielNo ratings yet
- Flattening Filter FreeDocument2 pagesFlattening Filter Freeapi-337168367No ratings yet
- SBRT-VMAT Pulmón: DR Enrique CHAJON Département de Radiothérapie Centre Eugène Marquis Rennes, FranceDocument37 pagesSBRT-VMAT Pulmón: DR Enrique CHAJON Département de Radiothérapie Centre Eugène Marquis Rennes, FranceCristian Max Rau VargasNo ratings yet
- Alkylating Antineoplastic AgentDocument5 pagesAlkylating Antineoplastic AgentMannit ButtarNo ratings yet
- Basic OncologyDocument42 pagesBasic Oncologybudiagungnugraha100% (1)
- Short Report: G. Catimel, F. Chauvin, J. P. Guastalla, P. Rebattu, P. B I R o N M. ClavelDocument3 pagesShort Report: G. Catimel, F. Chauvin, J. P. Guastalla, P. Rebattu, P. B I R o N M. ClavelApril NNo ratings yet
- WCLC2017 Abstract Book WebDocument700 pagesWCLC2017 Abstract Book Webdavid.yb.wangNo ratings yet
- 11. Tiến bộ trong điều trị ung thư trực QN 4 ENGLishDocument45 pages11. Tiến bộ trong điều trị ung thư trực QN 4 ENGLishTrần Đức HưởngNo ratings yet
- Linfoma de Hodgkin: Enfermedad en Relapso/RecaídaDocument31 pagesLinfoma de Hodgkin: Enfermedad en Relapso/RecaídaDANIEL JAIR ENRIQUEZ VERANo ratings yet
- BFM 2000 Treatment SchemaDocument2 pagesBFM 2000 Treatment SchemaAnonymous 9dVZCnTXSNo ratings yet
- Adjuvant and Neoadjuvant ChemotherapyDocument22 pagesAdjuvant and Neoadjuvant Chemotherapyprabushankar7No ratings yet
- LQ SpreadsheetDocument6 pagesLQ SpreadsheetAbraham García HerediaNo ratings yet
- Nitrile Exam Gloves Powder Free, Standard Cuff: Colloidal Oatmeal SystemDocument1 pageNitrile Exam Gloves Powder Free, Standard Cuff: Colloidal Oatmeal SystemFrancisco GarciaNo ratings yet
- Resume MedisDocument6 pagesResume MedisRina ekaNo ratings yet
- Cancer ChemotherapyDocument19 pagesCancer ChemotherapySamatha Mohan100% (1)