Professional Documents
Culture Documents
Aerosol Delivery of Recombinant Human DNase I
Uploaded by
herryaptCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aerosol Delivery of Recombinant Human DNase I
Uploaded by
herryaptCopyright:
Available Formats
Aerosol Delivery of Recombinant Human DNase I: In Vitro
Comparison of a Vibrating-Mesh Nebulizer With a Jet Nebulizer
Jeremy C Johnson DO, J Clifford Waldrep PhD, Jennifer Guo MD, and Rajiv Dhand MD FAARC
BACKGROUND: Inhaled recombinant human DNase I (rhDNase) improves clearance of visco-
elastic secretions in patients with cystic fibrosis. Because of their portability, newer-generation
vibrating-mesh nebulizers offer greater convenience for the patient, but their efficiency in deliver-
ing rhDNase has not been determined. METHODS: We compared a newer-generation vibrating-
mesh nebulizer (Omron MicroAir) to a Pari LCⴙ with the Pari ProNeb Ultra compressor (a
commonly employed rhDNase administration system). With the Next Generation Pharmaceutical
Impactor, we determined aerosol particle distribution. We also measured mass output efficiency,
nebulization time, and mass of rhDNase that deposited on a filter during simulated breathing.
RESULTS: The mass median aerodynamic diameter (MMAD) and geometric standard deviation
(GSD) of aerosol from the MicroAir (MMAD 4.3 m, GSD 2.8 m) was equivalent to that from the
Pari LCⴙ (MMAD 4.2 m, GSD 2.7 m). During simulated breathing the MicroAir had a higher
total mass output efficiency (88%) than the Pari LCⴙ (68%) (P < .001), and total nebulization time
was shorter with the MicroAir (6.1 min vs 7.2 min, P ⴝ .03). When nebulized to dryness, the mass
of rhDNase delivered to the filter was comparable with the MicroAir (1.30 ⴞ 0.4 mg) and Pari LCⴙ
(1.21 ⴞ 0.05 mg). CONCLUSION: The MicroAir could be employed as a portable nebulizer for
rhDNase therapy in patients with cystic fibrosis. Key words: nebulizer, vibrating mesh, aerosol,
inhalation, cystic fibrosis, recombinant human DNase I. [Respir Care 2008;53(12):1703–1708. © 2008
Daedalus Enterprises]
Introduction are a major cause of morbidity and mortality in patients with
cystic fibrosis (CF). Deoxyribonucleic acid (DNA) released
Respiratory complications, including persistent bacterial locally by degenerating neutrophils, which accumulate in re-
infections, recurrent exacerbations, and lung destruction,1,2 sponse to infection in the airways, is highly viscous and con-
tributes to development of chronic airway obstruction.3,4 In-
haled recombinant human DNase I (also known as rhDNase,
Jeremy C Johnson DO, J Clifford Waldrep PhD, Jennifer Guo MD, and
Rajiv Dhand MD FAARC are affiliated with the Division of Pulmonary,
dornase alfa, and Pulmozyme) hydrolyzes extra-cellular DNA
Critical Care, and Environmental Medicine, University of Missouri-Co- in purulent secretions of patients with CF, reduces the secre-
lumbia, and Harry S Truman Memorial Veterans Affairs Hospital, Co- tions’ visco-elasticity, and improves secretion clearance.5 A
lumbia, Missouri. few investigators have found that rhDNase nebulized via a
This research was partly supported by Omron Healthcare (which pro- conventional jet nebulizer is safe and improves symptoms
vided the MicroAir nebulizers), the United States Veterans Affairs Re- and pulmonary function in patients with CF.6-11
search Service, the Department of Internal Medicine, University of Mis- With advances in device technology, a plethora of aero-
souri, Columbia, and the Missouri Research Foundation. The device and sol devices and drug formulations are available for clinical
drug manufacturers were not involved in designing the study, collecting,
analyzing, or interpreting the data, or preparing the manuscript. The
use.12-17 For example, recent advances in nebulizer design
authors report no other conflicts of interest related to the content of this have introduced small portable devices based on either a
paper. vibrating mesh or a plate with multiple apertures.12,16,17
The vibrating-mesh nebulizers are being tested for various
Correspondence: Rajiv Dhand MD FAARC, Division of Pulmonary, Crit-
ical Care, and Environmental Medicine, University of Missouri-Colum-
clinical indications.18,19 To the best of our knowledge, these
bia, MA-421 Health Sciences Center, DC043.00, 1 Hospital Drive, Co- newer nebulizers have not been evaluated for aerosol de-
lumbia MO 65212. E mail: dhandr@health.missouri.edu. livery of rhDNase.
RESPIRATORY CARE • DECEMBER 2008 VOL 53 NO 12 1703
AEROSOL DELIVERY OF RECOMBINANT HUMAN DNASE I
We compared the delivery of rhDNase from the Mi- ity. The nebulizer was connected to the induction port of
croAir nebulizer (Omron Healthcare, Bannockburn, Illi- the NGI with a mouthpiece adapter. The positions of the
nois) to that from the Pari LC⫹ disposable jet nebulizer devices simulated those used in clinical practice, and the
(Pari Respiratory Equipment, Midlothian, Virginia) with aerosols from both devices were entrained into the NGI in
the Pari ProNeb Ultra compressor (Pari Respiratory Equip- line with the horizontal axis of the induction port. Aerosols
ment, Midlothian, Virginia). We choose this jet nebulizer/ were sampled for 2 min, and the experiments were re-
compressor system because it is one of the systems rec- peated in triplicate or quadruplicate with each device. The
ommended by the manufacturer of rhDNase for delivery impacted rhDNA was eluted from the NGI plates after
of rhDNase20 and is commonly employed in clinical prac- agitation for 5 min with 10 mL of ultrapure water.
tice for this application. After determination (via Kunitz assay) of the enzyme
concentrations deposited in the induction port, on each
Methods NGI stage, and on the final filter, the mass median aero-
dynamic diameter (MMAD) and geometric standard devi-
Devices and Drug ation (GSD) of the aerosol were calculated on a log prob-
ability scale on which the effective cutoff diameter is on
The MicroAir nebulizers (lots 32A and 44A) were gifts the ordinate and the cumulative percent less than the size
from Omron Healthcare. We purchased the Pari LC⫹ neb- range (by concentration) is on the abscissa (KaleidaGraph
ulizer and Pari ProNeb Ultra Compressor. In all the tests 3.51, Synergy Software, Reading, Pennsylvania). The
we used a commercial preparation of rhDNase (Pulmozyme, MMAD and GSD were determined by the rhDNase con-
Genentech, South San Francisco, California) that comes in centration distributed within the array of aerosol droplets.
2.5-mL ampules (1.0 mg/mL, 2,500 U) of a solution for The respirable fraction was calculated as the percentage of
inhalation formulated in 8.77 mg/mL sodium chloride, or aerosol particles ⬍ 5.0 m, and the fine-particle fraction
0.15 mg/mL calcium chloride dehydrate and sterile water was calculated as the percentage of aerosol drug particles
for injection. ⬍ 3.3 m.24,25
Deoxyribonuclease Activity of rhDNase Measurement of Mass Delivered to the Filter
Enzymatic activity in nebulized rhDNase samples was
To determine the amount of nebulized rhDNase deliv-
determined by the Kunitz method.21,22 The reaction rate
ered to the filter, samples were collected in a simulated
(maximum enzyme velocity) was measured by the rate of
human lung system.26 We used a respirator pump (Harvard
hydrolysis of DNA, measured spectrophotometrically at
Apparatus, Dover, Massachusetts) and employed an exha-
260 nm and 25°C. The stock DNA substrate solution con-
lation valve, such that aerosol samples were collected onto
tained 4 mg of salmon testes DNA in 0.5 M acetate buffer,
a bacteria/virus filter (Respirgard, Marquest Medical Prod-
pH 5.0, and 0.05 M magnesium chloride solution. Aliquots
ucts, Englewood, Colorado) (Fig. 1). The exhaled air was
of the test samples collected from the cascade impactor
vented into a hood.
(Next Generation Pharmaceutical Impactor [NGI], MSP
Total rhDNase delivered from the MicroAir and
Corporation, Shoreview, Minnesota) plates or inhalation
Pari LC⫹ with 2.5 mL rhDNase was collected on the
filters were added to 1 mL DNA test solution, and the
filters (5 of each), at 12 breaths/min with tidal volume of
reaction rate was measured over 6 min. The calculated
500 mL, and inspiratory-expiratory ratio of 1:1. The Mi-
maximum enzyme velocity reaction rate was used to de-
croAir was held in a horizontal position (see Fig. 1). Both
termine DNase activity. The sensitivity of the assay was
devices were connected to the proximal port of the filter.
10 units, based on a 3-point standard curve prepared with
The MicroAir was connected to the filter with a mouth-
1,000 units/mL rhDNase, as reported for each manufac-
piece adapter and mouthpiece. The Pari LC⫹ was con-
tured test lot, with an assay variability of ⬍ 10%.
nected to the filter with a mouthpiece adapter. The nebu-
lization began immediately before the inspiratory stroke of
Aerosol Particle Size Distribution
the pump piston. The nebulizers were run to dryness. Be-
cause the solution remaining in the jet nebulizer gave in-
Aerodynamic particle sizing of the rhDNase aerosols
consistent results with the enzyme assay, we determined
was via cascade impaction with the NGI, as previously
mass output of rhDNase based on nebulizer weights before
described.18,23 rhDNase I aerosols were generated from the
and after nebulization. The nebulizer efficiency was cal-
MicroAir nebulizer and the Pari LC⫹ nebulizer with one
culated by the following formula:
ampule of rhDNase and drawn through the cascade im-
pactor with a vacuum pump at 15 L/min, at a controlled [(pre-nebulization weight – post-nebulization weight)/
temperature of 23–24°C, and at 50 ⫾ 5% relative humid- pre-nebulization weight] ⫻ 100
1704 RESPIRATORY CARE • DECEMBER 2008 VOL 53 NO 12
AEROSOL DELIVERY OF RECOMBINANT HUMAN DNASE I
Fig. 1. Test setup.
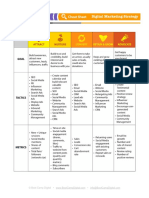
Table 1. Aerosol Characteristics of the Nebulizers
Geometric Standard Respirable Fraction‡ Fine Particle Fraction§
MMAD (m)*
Deviation† % %
MicroAir (mean ⫾ SD) 4.3 ⫾ 0.5 2.8 ⫾ 0.3 56.7 ⫾ 3.0 40.7 ⫾ 6.1
Pari LC⫹ (mean ⫾ SD) 4.2 ⫾ 0.5 2.7 ⫾ 0.4 56.3 ⫾ 4.1 44.0 ⫾ 6.2
* P ⫽ .77
† P ⫽ .69
‡ P ⫽ .92
§ P ⫽ .66
MMAD ⫽ mass median aerodynamic diameter
The rhDNase deposited on the filter was extracted via the respirable range were not statistically different. The
agitation for 5 min with 10 mL ultrapure water, and the respirable fraction from the MicroAir was 56.7 ⫾ 3.0%,
DNase activity was determined via Kunitz assay.21,22 compared to 56.3 ⫾ 4.1% from the Pari LC⫹. The fine-
particle fraction from the MicroAir was 40.7 ⫾ 6.1%,
Data Analysis compared to 44.0 ⫾ 6.2% from the Pari LC⫹ (see Ta-
ble 1).
We used statistics software (Instat 3, GraphPad Soft-
ware, La Jolla, California) to tabulate the data and calcu- Nebulization Time, Output Efficiency, and Mass
late the mean ⫾ SD values. We analyzed the MMAD, Delivered to the Filter
GSD, mass delivered to the filter, respirable fraction, and
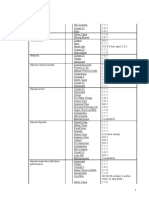
Table 2 shows the devices’ nebulization characteristics
fine-particle fraction data with 2-tailed paired t tests. P val-
with a simulated breathing system. With a charge dose of
ues ⬍ .05 were considered significant.
2.5 mL of rhDNase, the MicroAir nebulized to dryness in
6.1 min, versus 7.2 min with the Pari LC⫹ (P ⫽ .03). As
Results
determined via nebulizer weight before and after nebuli-
zation, the total drug output from the MicroAir
The experiments were designed to measure aerosol de-
(2.2 ⫾ 0.03 mg) was higher than that from the Pari LC⫹
livery of rhDNase from the MicroAir and the Pari LC⫹
(1.7 ⫾ 0.1 mg, P ⬍ .001) (see Table 2). This resulted in
with Pari ProNeb Ultra compressor.
higher nebulizer efficiency with the MicroAir (88%) than
with the Pari LC⫹ (68%, P ⬍ .001), mainly due to the
Aerosol Particle Size and Distribution
MicroAir’s lower residual volume. There was, however,
no significant difference in the amount of rhDNase depos-
Table 1 compares the aerosol characteristics of rhDNase
ited on the filter (MicroAir 1.30 mg, Pari LC⫹ 1.21 mg)
nebulized with the MicroAir versus with the Pari LC⫹, via
(see Table 2).
NGI analysis. Both devices produced a heterodisperse aero-
sol with comparable distribution of particle sizes (MMAD Discussion
4.3 ⫾ 0.5 m and GSD 2.8 ⫾ 0.3 m with MicroAir vs
MMAD 4.2 ⫾ 0.5 m and GSD 2.7 ⫾ 0.4 m with The present study compared the MicroAir to a currently
Pari LC⫹). The 2 devices’ aerosol particle distributions in utilized breath-enhanced nebulizer (Pari LC⫹) for deliv-
RESPIRATORY CARE • DECEMBER 2008 VOL 53 NO 12 1705
AEROSOL DELIVERY OF RECOMBINANT HUMAN DNASE I
Table 2. Nebulizer Characteristics With a Simulated Breathing System
Time to Output Total Nebulizer Filter
Dryness (min)* Efficiency (%)†‡ Output (mg)†‡ Mass (mg)§储
MicroAir (mean ⫾ SD) 6.1 ⫾ 0.5 88.0 ⫾ 1.7 2.2 ⫾ 0.03 1.30 ⫾ 0.4
Pari LC⫹ (mean ⫾ SD) 7.2 ⫾ 0.5 67.8 ⫾ 4.6 1.7 ⫾ 0.1 1.21 ⫾ 0.05
* P ⫽ .03
† Output is determined via nebulizer weight difference before and after nebulization.
‡ P ⬍ .001
§ Filter mass ⫽ amount of rhDNase deposited on filter, assayed via enzyme activity.
㛳 P ⫽ .24
ery of rhDNase. We found that the MicroAir is a conve- such as the ionic strength, density, surface tension, and
nient and efficient hand-held aerosol generator that pro- viscosity of the solution, also influence drug output and
vides comparable rhDNase output to Pari LC⫹. particle size from a nebulizer that employs a vibrating
The MicroAir has several distinctive features. It is a aperture plate to generate aerosol.33 Despite the differ-
battery-operated, portable device that employs a vibrating ences in test methods, our results (MMAD approximately
mesh for aerosol generation, and it produces a fine aerosol 4.2 m) are comparable to values obtained by previous
with a low velocity.18,27 The MicroAir rapidly aerosolizes investigators. Cipolla and colleagues reported an MMAD
drug solutions, so 2.5 mL of rhDNase is nebulized in a range of 2.6 –5.6 m for aerosols of rhDNase generated by
shorter time than with Pari LC⫹ with the ProNeb Ultra various Pari nebulizers.30 With other jet nebulizers the
compressor. The aerosol particle distribution analysis with particle size distribution of rhDNase aerosols have also
the NGI revealed that both devices produced heterodis- been comparable to our results.29,31
perse aerosols with similar particle sizes. Both MicroAir In our study the Pari LC⫹ aerosolized only 68% of the
and Pari LC⫹ generate aerosol particles within the range rhDNase, whereas 88% of the drug placed in the MicroAir
required for relatively uniform delivery to the airways was aerosolized. However, despite the difference in mass
within the lung.24-26,28 output, the mass of rhDNase delivered to the filter in the
In the present study we employed an enzymatic method simulated breathing experiment was comparable with the
to assay the rhDNase and determine the MMADs and MicroAir and Pari LC⫹, which suggests a higher rhDNase
GSDs. Previous studies29-31 with jet nebulizers employed deposition in the inspiratory tubing en route to the filter
different cascade impaction techniques30 or laser diffrac- with the MicroAir. The similarity in the mass of rhDNase
tion,29,31 and no previous studies have been performed on the filter and the particle size of the aerosols generated
with rhDNase delivered by a vibrating-mesh nebulizer. by the 2 devices suggests that a comparable amount of
Recently, the European Standard (EN 13544-1) was de- rhDNase would be available to the patient with either de-
veloped to standardize laboratory methods for determina- vice, and the difference in pulmonary deposition of rhD-
tion of particle size in nebulized aerosols.32 In our study, Nase between the 2 devices is probably not clinically im-
which was conducted according to the guidelines of the portant. Ideally, these observations would be confirmed
European Nebulizer standard,32 the distribution of rhD- with scintigraphic studies with radiolabeled rhDNase in
Nase particles in the aerosol generated by both devices patients with CF. A study with healthy adults and the
was equivalent. Pari LC⫹ found very close agreement between the respi-
In related studies, previous investigators employed jet rable fraction of tobramycin measured via laser diffraction
nebulizers and various techniques to size rhDNase aero- and the in vivo respirable fraction measured via scintigra-
sols.29-31 Cipolla and colleagues30 used dry weights to de- phy.34 However, in general, in vitro assessments tend to
termine rhDNase deposition on the impactor plates. Other overestimate lung deposition.24,28 In previous investiga-
investigators employed laser diffraction to size aerosol par- tions, clinical response to inhaled rhDNase was similar
ticles.29,31 Those studies assumed that rhDNase and ex- with jet nebulizers with comparable performance and aero-
cipients distribute equally among all aerosol particles, but sol characteristics.31,35 The similarity in aerosol character-
the amount of rhDNase in various fractions cannot be istics and mass delivered to the filter with MicroAir and
directly determined by the techniques employed in previ- Pari LC⫹ suggests that clinical response would be com-
ous studies.29-31 In contrast, we determined rhDNase dep- parable with these 2 devices.
osition by direct measurement of its activity in various The Kunitz assay gave unreliable results when assaying
particle fractions. In our previous study with the MicroAir for rhDNase in the solution remaining in the jet nebulizer
we found that various laboratory techniques yielded dif- after nebulization, so we had to resort to weighing the
ferent results for particle size distribution.18 Other factors, nebulizers to determine total drug output. Because of their
1706 RESPIRATORY CARE • DECEMBER 2008 VOL 53 NO 12
AEROSOL DELIVERY OF RECOMBINANT HUMAN DNASE I
ampipathic nature, protein molecules tend to occupy the REFERENCES
surface in protein solutions, and they may undergo surface
denaturation during jet nebulization.36 In contrast to our 1. FitzSimmons SC. The changing epidemiology of cystic fibrosis. J Pe-
findings, earlier investigators29 found that enzymatic ac- diatr 1993;122(1):1-9.
2. Konstan MW, Berge M. Current understanding of the inflammatory
tivity of rhDNase was preserved in the solution remaining process in cystic fibrosis: onset and etiology. Pediatr Pulmonol 1997;
in the nebulizer cup after jet or ultrasonic nebulization. 24(2):137-142.
However, the assay employed by Cipolla and co-workers29 3. Ratjen F, Döring G. Cystic fibrosis. Lancet 2003;361(9358):681-
did not directly assess the action of rhDNase on DNA. 689.
CF is a chronic illness that requires routine and frequent 4. Gibson RL, Burns JL, Ramsey BW. Pathophysiology and manage-
treatments. Similar to other jet nebulizers,29,36 rhDNase ment of pulmonary infections in cystic fibrosis. Am J Respir Crit
Care Med 2003;168(8):918-951.
delivered to the filter retains its activity after nebulization 5. Shak S, Capon DJ, Hellmiss R, Marsters SA, Baker CL. Recombi-
with MicroAir. In patients with CF, MicroAir would be nant human DNase 1 reduces the viscosity of cystic fibrosis sputum.
expected to produce clinical improvement comparable to Proc Natl Acad Sci USA 1990;87(23):9188-9192.
that with other jet nebulizers.6-11 Because of its higher 6. Ramsey BW, Astley SJ, Aitken MA, Burke W, Colin AA, Dorkin
drug-output rate, the MicroAir takes less time to nebulize HL, et al. Efficacy and safety of short-term administration of aero-
solized recombinant human deoxyribonuclease in patients with cys-
rhDNase than does the Pari LC⫹ (see Table 2). MicroAir’s
tic fibrosis. Am J Respir Crit Care Med 1993;148(1):145-151.
faster nebulization rate, compactness, and portability might 7. Fuchs HJ, Borowitz DS, Christiansen DH, Morris EM, Nash ML,
improve patient adherence to treatment. MicroAir is also Ramsey BW. Effect of aerosolized recombinant human DNase on
quieter than a conventional jet nebulizer. exacerbations of respiratory symptoms and on pulmonary function in
patients with cystic fibrosis. N Engl J Med 1994;331(10):637-642.
8. Shah PL, Scott SF, Geddes DM, Hodson ME. Two years experience
Limitations with recombinant human DNase I in the treatment of pulmonary
disease in cystic fibrosis. Respir Med 1995;89(7):499-502.
Our testing was under controlled laboratory conditions 9. McCoy K, Hamilton S, Johnson C; Pulmozyme Study Group. Effects
and therefore did not consider potential problems with of 12-week administration of dornase alfa in patients with advanced
cystic fibrosis lung disease. Chest 1996;110(4):889-895.
patient coordination and irregular breathing patterns that 10. Quan JM, Tiddens HA, Sy JP, McKenzie SG, Montgomery MD,
may be encountered in clinical use. Robinson PJ, et al; Pulmozyme Ealy Intervention Trial Study Group.
We did not test the MicroAir over an extended period, A two-year randomized placebo-controlled trial of dornase alpha in
as would be required in clinical practice. young patients with cystic fibrosis with mild lung function abnor-
The cost of the MicroAir (approximately $200) is higher malities. J Pediatr 2001;139(6):813-820.
11. Hodson ME, Mckenzie S, Harms HK, Koch C, Mastella G, Navarro
than that of Pari LC⫹ and compressor (approximately
J, Strandvik B; Investigators of the Epidemiologic Registry of Cystic
$70). The MicroAir also needs rigorous cleaning; the man- Fibrosis. Dornase alpha in the treatment of cystic fibrosis in Europe:
ufacturer recommends disassembly, immersion in water, a report from the Epidemiologic Registry of Cystic Fibrosis. Pediatr
and disinfection with 10% distilled vinegar after each use Pulmonol 2003;36(5):427-432.
to prevent clogging of the mesh apertures with drug par- 12. Smaldone GC. Advances in aerosols: adult respiratory disease. J
ticles, salts, or microbes. Cleaning and reassembling the Aerosol Med 2006;19(1):36-46.
13. Hess D, Fisher D, Williams P, Pooler S, Kacmarek RM. Medication
MicroAir requires several minutes after each treatment.
nebulizer performance. Effects of diluent volume, nebulizer flow,
Aperture clogging was not a problem in our experiments, and nebulizer brand. Chest 1996;110(2):498-505.
because we adhered to a cleaning regimen. The latest rec- 14. Smaldone GC, LeSouef PN. Nebulization: the device and clinical
ommendation on cleaning the MicroAir (effervescent den- considerations. In: Bisgaard H, O’Callaghan CO, Smaldone GC,
ture cleanser) might further reduce aperture clogging. editors. Drug delivery to the lung. New York: Marcel Dekker; 2002:
269-302.
15. Rau JL. The inhalation of drugs: advantages and problems. Respir
Conclusions Care 2005;50(3):367-382.
16. Smaldone GC. Assessing new technologies: patient-device interac-
tions and deposition. Respir Care 2005;50(9):1151-1160.
The MicroAir produces a fine-particle, heterodisperse
17. Dhand R. Nebulizers that use a vibrating mesh or plate with
rhDNase aerosol that is comparable to that from the multiple apertures to generate aerosol. Respir Care 2002;47(12):
Pari LC⫹. These 2 devices deliver comparable amounts of 1406-1418.
active rhDNase to the airways. The MicroAir has the ad- 18. Waldrep JC, Berlinski A, Dhand R. Comparative analysis of meth-
vantages of higher efficiency, better portability, shorter ods to measure aerosols generated by a vibrating mesh nebulizer. J
drug-delivery time, and greater convenience of use, com- Aerosol Med 2007;20(3):310-319.
19. Dhand R, Sohal H. Pulmonary drug delivery system for inhalation
pared to conventional jet nebulizers. The MicroAir could
therapy in mechanically ventilated patients. Expert Rev Med Devices
be employed as a portable device for rhDNase therapy in 2008;5(1):9-18.
patients with CF. Further studies are needed to determine 20. Package insert. Full prescribing information for Pulmozyme dornase
MicroAir’s clinical efficiency. alfa. San Francisco: Genentech; 1994.
RESPIRATORY CARE • DECEMBER 2008 VOL 53 NO 12 1707
AEROSOL DELIVERY OF RECOMBINANT HUMAN DNASE I
21. Kunitz M. Crystalline deoxyribonuclease; isolation and general prop- 29. Cipolla D, Clark AR, Chan HK, Gonda I, Shire SJ. Assessment of
erties; spectrophotometric method for the measurement of deoxyri- aerosol delivery systems for recombinant human deoxyribonuclease.
bonuclease activity. J Gen Physiol 1950;33(4):349-362. STP Pharma Sciences 1994;4:50-62.
22. Kunitz M. Crystalline deoxyribonuclease; digestion of thymus nu- 30. Cipolla D, Gonda I, Shire SJ. Characterization of aerosols of human
cleic acid; the kinetics of the reaction. J Gen Physiol 1950;33(4): recombinant deoxyribonuclease I (rhDNase) generated by jet nebu-
363-377. lizers. Pharma Res 1994;11(4):491-498.
23. Marple VA, Olson BA, Santhanakrishnan K, Roberts DL, Mitchell 31. Shah PL, Scott SF, Geddes DM, Conway S, Watson A, Nazir T, et
JP, Hudson-Curtis BL. Next generation pharmaceutical impactor: a al. An evaluation of two aerosol delivery systems for rhDNase. Eur
new impactor for pharmaceutical inhaler testing. Part III: extension Respir J 1997;10(6):1261-1266.
of archival calibration to 15 L/min. J Aerosol Med 2004;17(4):335- 32. Boe J, Dennis JH, O’Driscoll BR, Bauer TT, Carone M, Dautzenberg
343. B, et al; European Respiratory Society Task Force on the use of
24. Newman SP. How well do in vitro particle size measurements pre- nebulizers. European Respiratory Society guidelines on the use of
dict drug delivery in vivo? J Aerosol Med 1998;11(Suppl 1):S97- nebulizers. Eur Respir J 2001;18(1):228-242.
S104. 33. Zhang G, David A, Wiedemann TS. Performance of the vibrating
25. Sangwan S, Condos R, Smaldone GC. Lung deposition and respira- membrane aerosol generating device: Aeroneb micropump nebu-
ble mass during wet nebulization. J Aerosol Med 2003;16(4):379- lizer. J Aerosol Med 2007;20(4):408-416.
386. 34. Coates AL, MacNeish CF, Dinh L, MacNeish CF, Rollin T, Gagnon
26. Smaldone GC, Fuhrer J, Steigbigel RT, McPeck M. Factors deter- S, et al. Accounting for radioactivity before and after nebulization of
mining pulmonary deposition of aerosolized pentamidine in patients tobramycin to insure accuracy of quantification of lung deposition. J
with human immunodeficiency virus infection. Am Rev Respir Dis Aerosol Med 2000;13(3):169-178.
1991;143(4 Pt 1):727-737. 35. Fiel SB, Fuchs HJ, Johnson C, Gonda I, Clark AR. Comparison of
27. Waldrep JC, Dhand R. Advanced nebulizer designs employing vi- three jet nebulizer aerosol delivery systems used to administer re-
brating mesh/aperture plate technologies for aerosol generation. Curr combinant human DNase I to patients with cystic fibrosis. Chest
Drug Deliv 2008;5(2):114-119. 1995;108(1):153-56.
28. Newman SP, Chan HK. In vitro/in vivo comparisons in pulmonary 36. Hung JC, Hambleton G, Super M. Jet nebulizing systems for recom-
drug delivery. J Aerosol Med 2008;21(1):77-84. binant human DNase I. Arch Dis Child 1994;71(6):558-559.
1708 RESPIRATORY CARE • DECEMBER 2008 VOL 53 NO 12
You might also like
- Optimum Way BP 2023Document37 pagesOptimum Way BP 2023herryaptNo ratings yet
- Blogging Tips and TricksDocument1 pageBlogging Tips and TricksherryaptNo ratings yet
- CopywritingForSearch QuickStartDocument4 pagesCopywritingForSearch QuickStartherryaptNo ratings yet
- SEO Advanced QuickStartDocument3 pagesSEO Advanced QuickStartherryaptNo ratings yet
- Conversion Rate Optimization QuickStart GuideDocument3 pagesConversion Rate Optimization QuickStart GuideherryaptNo ratings yet
- Digital Marketing Strategy Cheat SheetDocument1 pageDigital Marketing Strategy Cheat SheetherryaptNo ratings yet
- Digital Marketing Strategy ChecklistDocument1 pageDigital Marketing Strategy ChecklistherryaptNo ratings yet
- Sowell Respiratory Equipment 2022Document11 pagesSowell Respiratory Equipment 2022herryaptNo ratings yet
- Digital Marketing Plan One Page SummaryDocument1 pageDigital Marketing Plan One Page SummaryherryaptNo ratings yet
- Digital Measurement Cheat SheetDocument8 pagesDigital Measurement Cheat SheetherryaptNo ratings yet
- Digital Marketing Measurement Quick Start Guide2Document1 pageDigital Marketing Measurement Quick Start Guide2herryaptNo ratings yet
- OMRON Automatic Blood Pressure Monitor: SpecificationDocument2 pagesOMRON Automatic Blood Pressure Monitor: SpecificationherryaptNo ratings yet
- Brosur RGB Medical Bpm001 + AdaptorDocument2 pagesBrosur RGB Medical Bpm001 + AdaptorherryaptNo ratings yet
- Aerosol Guide RT PDFDocument61 pagesAerosol Guide RT PDFpravikumar1989100% (1)
- OHQ NewsLetter - Vol12 - Afib - 1112 - ENDocument5 pagesOHQ NewsLetter - Vol12 - Afib - 1112 - ENherryaptNo ratings yet
- TB Pulmonary TuberculosisDocument1 pageTB Pulmonary TuberculosisherryaptNo ratings yet
- Pedoman Pelayanan Kegawatdaruratan Psikiatrik PDFDocument125 pagesPedoman Pelayanan Kegawatdaruratan Psikiatrik PDFDita DitotNo ratings yet
- Stability Considerations in Liquid Dosage Forms Extemporaneously ...Document29 pagesStability Considerations in Liquid Dosage Forms Extemporaneously ...herryapt100% (1)
- Leadership DevelopmentDocument312 pagesLeadership Developmentherryapt100% (2)
- Business EthicsDocument93 pagesBusiness EthicsherryaptNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Microsoft Word - IRN Fab Transfer PCN NoticeDocument22 pagesMicrosoft Word - IRN Fab Transfer PCN NoticeJadilson PradoNo ratings yet
- What's The Use of Neuroticism?: G. Claridge, C. DavisDocument18 pagesWhat's The Use of Neuroticism?: G. Claridge, C. DavisNimic NimicNo ratings yet
- 1mrk513011-Ben en Auxiliary Current Transformer For Radss 1-Phase and 3-Phase Slce 12 Slce 16 Slxe 4Document4 pages1mrk513011-Ben en Auxiliary Current Transformer For Radss 1-Phase and 3-Phase Slce 12 Slce 16 Slxe 4GustavoForsterNo ratings yet
- Chemistry Mid Term Exam 2014Document8 pagesChemistry Mid Term Exam 2014Adham TamerNo ratings yet
- Afectiuni Si SimptomeDocument22 pagesAfectiuni Si SimptomeIOANA_ROX_DRNo ratings yet
- Data Sheet: W-Series WSI 6/LD 10-36V DC/ACDocument12 pagesData Sheet: W-Series WSI 6/LD 10-36V DC/ACLUIS FELIPE LIZCANO MARINNo ratings yet
- Tim Ingold - From The Transmission of Representations To The Education of Attention PDFDocument26 pagesTim Ingold - From The Transmission of Representations To The Education of Attention PDFtomasfeza5210100% (1)
- Julie RiesenweberDocument14 pagesJulie RiesenweberisidorabilbaoNo ratings yet
- ScilabDocument4 pagesScilabAngeloLorenzoSalvadorTamayoNo ratings yet
- Texas Instruments FootprintsDocument7 pagesTexas Instruments FootprintsSteve SmithNo ratings yet
- M1-Safety StandardsDocument9 pagesM1-Safety StandardscarlNo ratings yet
- Production Technology of Dragon FruitDocument6 pagesProduction Technology of Dragon FruitAbhinash MoirangthemNo ratings yet
- Streamline SWR (S) - Rev - 00-04-2019 PDFDocument2 pagesStreamline SWR (S) - Rev - 00-04-2019 PDFarjun 11No ratings yet
- CopernikDocument2 pagesCopernikSinister JinNo ratings yet
- VlsiDocument79 pagesVlsimdhuq1No ratings yet
- Your Heart: Build Arms Like ThisDocument157 pagesYour Heart: Build Arms Like ThisNightNo ratings yet
- Rubber Lined Piping - A Solution To Corrosion ResistanceDocument5 pagesRubber Lined Piping - A Solution To Corrosion ResistanceMohamed AghilaNo ratings yet
- AC350 Specs UsDocument18 pagesAC350 Specs Uskloic1980100% (1)
- Jib Crane Assembly ManualDocument76 pagesJib Crane Assembly ManualRobert Cumpa100% (1)
- Smart Watch User Manual: Please Read The Manual Before UseDocument9 pagesSmart Watch User Manual: Please Read The Manual Before Useeliaszarmi100% (3)
- Module 12. Big Issues Lesson 12a. Reading. Pages 140-141: No Words TranslationDocument4 pagesModule 12. Big Issues Lesson 12a. Reading. Pages 140-141: No Words TranslationLeonardo Perez AlegriaNo ratings yet
- Polynomial Transformations of Tschirnhaus, Bring and Jerrard4s++Document5 pagesPolynomial Transformations of Tschirnhaus, Bring and Jerrard4s++wlsvieiraNo ratings yet
- Master of Business Administration in Aviation Management MbaamDocument10 pagesMaster of Business Administration in Aviation Management MbaamAdebayo KehindeNo ratings yet
- Refrigeration Engineer Quick ReferenceDocument2 pagesRefrigeration Engineer Quick ReferenceventilationNo ratings yet
- Scientific Exploration and Expeditions PDFDocument406 pagesScientific Exploration and Expeditions PDFana_petrescu100% (2)
- Deva Surya - 19MF02Document30 pagesDeva Surya - 19MF02SaravananNo ratings yet
- FPAL Product Code GuideDocument53 pagesFPAL Product Code GuideSRARNo ratings yet
- CAT25256 EEPROM Serial 256-Kb SPI: DescriptionDocument22 pagesCAT25256 EEPROM Serial 256-Kb SPI: DescriptionPolinho DonacimentoNo ratings yet
- CDM816DSpare Parts Manual (Pilot Control) 2Document55 pagesCDM816DSpare Parts Manual (Pilot Control) 2Mohammadazmy Sobursyakur100% (1)
- 173 EvidenceDocument6 pages173 EvidenceSantiago RubianoNo ratings yet