Professional Documents
Culture Documents
Kishimoto 2009
Uploaded by
anitaabreu123Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kishimoto 2009
Uploaded by
anitaabreu123Copyright:
Available Formats
Annals of Otology, Rhinology & Laryngology 118(9):613-620.
© 2009 Annals Publishing Company. All rights reserved.
Implantation of an Atelocollagen Sheet for the Treatment of
Vocal Fold Scarring and Sulcus Vocalis
Yo Kishimoto, MD; Shigeru Hirano, MD, PhD; Tsuyoshi Kojima, MD;
Shin-ichi Kanemaru, MD, PhD; Juichi Ito, MD, PhD
Objectives: The management of vocal fold scarring and sulcus vocalis is challenging. These disorders are thought to be
fibroplastic anomalies in the cover portion of the vocal fold that cause deterioration of the vibratory properties of the vo-
cal fold mucosa. Histologic studies have revealed disorganization of extracellular matrix that needs to be addressed in the
treatment of scarred vocal folds. Replacement of scar tissues with an appropriate implant may lead to regeneration of the
vocal fold mucosa and its tissue properties. This retrospective case study examined the feasibility of using an atelocol-
lagen sheet as a regenerative implant.
Methods: Six patients with a post-cordectomy scar or sulcus vocalis underwent implantation of an atelocollagen sheet
into the lamina propria of the vocal folds. The procedure consisted of elevation of a microflap, dissection and removal
of scar tissue, implantation of the material, and wound closure. Vocal function was evaluated before and after surgery by
stroboscopic examination and by aerodynamic and acoustic analyses.
Results: The postoperative changes of aerodynamic and acoustic parameters varied among patients; however, gradual
improvement was seen in most cases over a year. Stroboscopic findings also revealed gradual improvement of vibratory
properties in most cases.
Conclusions: Implantation of an atelocollagen sheet may have restorative effects on vocal fold scarring and sulcus vo-
calis in terms of tissue properties and function of the mucosa.
Key Words: atelocollagen sheet, human, sulcus vocalis, vocal fold scarring.
INTRODUCTION sulcus vocalis,1,2 and development of new regenera-
tive strategies is being pursued.
The management of vocal fold scarring and sul-
cus vocalis remains a therapeutic challenge.1 Vocal In tissue engineering, regeneration of tissues or
fold scarring occurs after injury and inflammation. organs can be achieved by a combination of scaf-
It disrupts the layer structure of the lamina propria, fold, cell, and regulatory factors under appropri-
changing the biomechanical properties of the vo- ate conditions. According to this concept, we have
cal fold. Sulcus vocalis is a migration of the vocal tried to regenerate injured vocal folds using autolo-
fold epithelium into the normally convex superficial gous mesenchymal stem cells and growth factors.5,6
lamina propria or deeper layers.2 Both of these con- Although we have shown the effectiveness of cell
ditions result in intractable dysphonia and glottal in- therapy5 and growth factor therapy6 in the treatment
sufficiency. Because previous histologic studies3,4 of vocal fold scarring using animal models, there
revealed similar disorganization of extracellular ma- are still some problems for clinical use. Moreover,
trix components in both conditions, it is thought that an appropriate scaffold is usually needed to obtain
strategies for treatment of vocal fold scarring and ideal regenerative effects of cells and growth factors
sulcus vocalis could be the same. inside the vocal fold.
For vocal fold scarring and sulcus vocalis, various Atelocollagen sheeting (Terudermis, Olympus Ter-
kinds of therapeutic strategies, such as voice therapy umo Biomaterials Corp, Tokyo, Japan) is a cross-
or pharmacologic and surgical treatment, have been linked collagen material with abundant micropores
attempted to soften the scarred tissues or to restore that can recruit cells from surrounding tissues. It is
its normal properties. However, to date there is no biocompatible and biodegradable, and has been used
optimal strategy to restore the scarred vocal fold or for coverage and dressing of postsurgical dermal or
From the Department of Otolaryngology–Head and Neck Surgery, Kyoto University Graduate School of Medicine, Kyoto, Japan.
Presented at the meeting of the American Broncho-Esophagological Association, Phoenix, Arizona, May 28-29, 2009.
Correspondence: Shigeru Hirano, MD, PhD, Dept of Otolaryngology–Head and Neck Surgery, Kyoto University Graduate School of
Medicine, Sakyo-ku, Kyoto 606-8507, Japan.
613
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
614 Kishimoto et al, Implantation of Atelocollagen Sheet 614
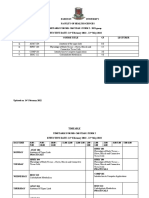
PATIENT DATA
Side
Age Initial Additional Closing Follow-Up
Case Sex (y) Diagnosis Implant Implant Method (mo)
1 M 68 Post-cordectomy scar R Polydioxanone suture 32
R Polydioxanone suture 18.5
2 F 40 Rheumatoid arthritis and post–superficial L Polydioxanone suture 24
cordotomy scar
R Polydioxanone suture 7
3 M 56 Sulcus vocalis Bilateral Fibrin glue 8
4 F 40 Sulcus vocalis L Fibrin glue 17
5 M 60 Post-cordectomy scar L Polydioxanone suture 6
6 F 50 Sulcus vocalis Bilateral Fibrin glue 17
epidermal defects in several parts of the body to stim- pital. Inclusion criteria were sulcus vocalis or vocal
ulate wound healing.7,8 Since 2005, we have treated fold scarring accompanied by hoarseness. The pro-
patients with vocal fold scarring or sulcus vocalis cedure was carried out with the patient’s agreement.
with implants of the atelocollagen sheet because of Their ages ranged from 40 to 68 years (average,
its regenerative characteristics. In this study, we ex- 52.3 years), and the postoperative follow-up period
amined the feasibility of the atelocollagen sheet as a varied from 6 to 32 months. The implants were per-
regenerative scaffold in the treatment of vocal fold formed on one side of the vocal fold or both, accord-
scarring and sulcus vocalis. ing to the site and/or severity of the lesion. Four pa-
tients were treated with a unilateral implant in their
MATERIALS AND METHODS initial surgeries, and 2 of these later received an ad-
Patients. The clinical information about patients ditional implant because the effect of the unilateral
and surgical procedures is summarized in the Table. implant was limited. Another 2 patients (cases 3 and
Six adult patients (3 men and 3 women), 3 with post- 6) received simultaneous bilateral implants.
cordectomy scarring and 3 with sulcus vocalis, were Preparation of Terudermis. Terudermis is made
treated with an implant of Terudermis into the vocal by cross-linking atelocollagens derived from bovine
fold during 2006 and 2007 at Kyoto University Hos- skin tissues. The possibility of mad cow disease
A B
Fig 1. (Case 5) Implantation of
atelocollagen sheet into left vo-
cal fold. A) Incision on superior
surface of vocal fold. B) Subepi-
thelial pocket. C) Atelocollagen
C D sheet implanted into pocket. D)
Polydioxanone suture was used
to close pocket.
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
615 Kishimoto et al, Implantation of Atelocollagen Sheet 615
forceps and retracted medially. A vertical incision
along the longitudinal axis of the vocal fold was
made lateral to the scarred site or sulcus on the su-
perior surface of the vocal fold (Fig 1A). Underly-
ing scar tissue was dissected with a microdissector,
and removed when necessary (Fig 1B). Finally, a
subepithelial pocket was made between the epithe-
lium and the vocal ligament in which Terudermis
was to be implanted. Terudermis was cut to a suit-
able size and then inserted into the pocket (Fig 1C).
After implantation of the sheet, the microflap was
put back into its original position. A polydioxanone
suture or fibrin glue was used to close the pocket to
prevent loss or dislocation of the implanted material
Fig 2. Concept of Terudermis implant. (Fig 1D).
caused by this material was excluded. The thick- Figure 2 illustrates the concept of this procedure.
ness of this material is 3 mm, and it contains abun- It was expected that cells, and possibly growth fac-
dant micropores, 50 to 500 μm in diameter, that are tors, might migrate into the implanted sheet of Teru-
thought to be suitable for the influx of cells into the dermis.
sheet. Indeed, it was confirmed that implanted Teru- Assessment. Two trained laryngologists made
dermis recruited cells from the surrounding tissues blind measurements. The assessment consisted of
in animal experiments.9 In addition, the material stroboscopic, acoustic, and aerodynamic examina-
is tolerant to collagenase, and it was confirmed in tions. The voice and stroboscopic samples were re-
rat models that the material remained undamaged 4 corded at normal pitch and normal loudness for 3
weeks after implantation.9 Terudermis is allowed for times at each evaluation. Stroboscopic examinations
use in human patients with any dermal or epidermal were performed with a Digital Video Stroboscopy
defects of the skin or mucosal tissues by the Minis- System model 9295 (KayPENTAX, Lincoln Park,
try of Health, Labor, and Welfare in Japan. New Jersey) to assess temporal changes of the mu-
cosal wave and glottic closure. The amplitude of the
Surgical Procedure. The procedure consisted of mucosal wave and the glottal gap were examined
elevation of a microflap, dissection and removal of with image analysis software (Scion Image beta3b,
underlying scar tissues, implantation of Terudermis, Frederick, Massachusetts). The distance (d1) from
and wound closure. The glottis was exposed with the midline of the glottis to the free edge of the vo-
either a Zeitels Universal Modular Glottiscope (En- cal fold was measured at the anteroposterior middle
docraft LLC, Winter Park, Florida) or a Kleinsasser portion of the vocal fold during the closed phase,
Laryngoscope (Karl Storz GmbH & Co, Tuttlingen, and then the same distance (d2) was measured at the
Germany) under general anesthesia. maximum open phase.
After hydrodissection was performed by subepi The mucosal wave amplitude was normalized by
thelial injection of 1:80,000 epinephrine, the free the distance (L) from the anterior commissure to the
edge of the vocal fold was grasped with micro- vocal process. The normalized mucosal wave am-
A B
Fig 3. In most cases, gradual improvement is shown by A) normalized mucosal wave amplitude and B) normalized glottal gap.
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
616 Kishimoto et al, Implantation of Atelocollagen Sheet 616
A B
C D
Fig 4. Aerodynamic and acoustic parameters showed gradual
improvements in most cases. A) Maximum phonation time. B)
Mean flow rate. C) Pitch perturbation quotient. D) Amplitude
perturbation quotient. E) Noise-to-harmonics ratio.
plitude (NMWA) was calculated from the formula poral changes of the NMWA and NGG. The NMWA
NMWA = (d2 – d1)/L. This measurement was done showed gradual improvement in all cases except
on the treated side of the vocal fold. The glottal case 3, and the NGG became smaller with time in
gap was examined on the images during the closed 4 of 6 cases.
phase. The glottal area (a) was measured, and the Aerodynamic and Acoustic Examinations. Aero-
normalized glottal gap (NGG) was calculated as dynamic and acoustic parameters had individual
NGG = a/L2. variations, but generally the maximum phonation
The aerodynamic and acoustic examinations were time, mean flow rate, pitch perturbation quotient,
completed at the same time points. Aerodynamic amplitude perturbation quotient, and noise-to-har-
examinations included maximum phonation time monics ratio showed gradual improvement in most
and mean flow rate. The Computerized Speech Lab cases over 1 year (Fig 4).
(KayPENTAX) was used to evaluate the pitch per- Representative Cases. In case 1, a 68-year-old
turbation quotient, amplitude perturbation quotient, man had scarring after undergoing laser cordectomy
and noise-to-harmonics ratio. for glottic carcinoma. The vibration of the right vo-
cal fold was limited, and incomplete glottal closure
RESULTS was observed (Fig 5A). Terudermis was initially im-
Vibratory Examination. Figure 3 shows the tem- planted into the right vocal fold. However, because
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
617 Kishimoto et al, Implantation of Atelocollagen Sheet 617
Fig 5. (Case 1) Stroboscopic findings. A) Before treatment. B) After treatment, vibration of right vocal fold is improved, and
almost complete glottal closure is observed.
the vibration of the vocal fold was still limited, with In case 4, a 40-year-old woman with left sulcus
incomplete glottal closure at the posterior portion vocalis was referred to us. Stroboscopic examina-
of the glottis, a second implant was placed in the tion found no vibration of the vocal fold and a large
posterior portion of the right vocal fold. The glot- glottal gap (Fig 7A). Undermining of the sulcus was
tal closure and vibration of the vocal fold gradually initially done, and fibrous tissues were removed.
improved over 7 months after the second operation However, 3 months after the surgery, her voice had
(Fig 5B). not improved. In subsequent revision surgery, we
resected scarred tissues beneath the epithelium and
In case 2, a 40-year-old woman had an idiopathic implanted Terudermis into the left vocal fold. After
scar that was possibly due to rheumatoid arthritis in the implantation, acoustic and stroboscopic exam-
the vocal fold. She had undergone superficial cordo- ination revealed gradual improvement. Seventeen
tomy by another surgeon to remove the scar tissue. months after the implantation, stroboscopic exami-
Her postoperative voice had not improved 3 months nation revealed improved mucosal wave vibration
after the cordotomy, and she was referred to us. On (Fig 7B).
the first visit, she was nearly aphonic and there was DISCUSSION
no mucosal vibration on stroboscopic examination Various surgical approaches for the treatment of
(Fig 6A). We resected as much scar tissue as pos- vocal fold scarring and sulcus vocalis — medial-
sible beneath the epithelium and implanted Teruder- ization thyroplasty, collagen or fat injection, exci-
mis into the left vocal fold. Figure 6B shows strobo- sion of scar, and lysis of adhesions — have been
scopic findings made 24 months after the implanta- attempted to restore normal vocal fold properties.1,2
tion that indicate the appearance of mucosal vibra- Medialization thyroplasty and collagen or fat injec-
tion. tion result in augmentation effects, which improve
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
618 Kishimoto et al, Implantation of Atelocollagen Sheet 618
Fig 6. (Case 2) Stroboscopic findings. A) Before treatment. B) Mucosal vibration appears in bilateral vocal folds after treat-
ment.
the glottal insufficiency and facilitate entrainment of dehydrothermally cross-linked fibrillar atelocol-
of vocal fold oscillation. However, their effects are lagen and heat-denatured atelocollagen.9,10 Because
limited, because restoration of the normal properties of this structure, the material remains in the implant-
of the vocal fold cannot be achieved by these meth- ed site for a long time, is infiltrated easily by cells
ods. In addition, the effects of excision of scar or ly- from surrounding tissues, and is thought to be an
sis of adhesions depend on the individual’s healing ideal regenerative scaffold because it achieves ac-
ability, and stable outcomes cannot be achieved with ceptance in the early period after implantation that
this approach. Thus, in order to consistently restore results in long-term survival and little contracture.
the normal properties of the vocal fold, a new regen- In the vocal fold, it is expected that the implanted
erative strategy is needed. material provides an appropriate space and environ-
In tissue engineering to regenerate tissues or or- ment for vocal fold fibroblasts to produce extracel-
gans, it is necessary to combine a scaffold, cells, and lular matrix components and thus to restore scarred
regulatory factors under appropriate conditions. In tissues.
general, a regenerative scaffold should have bio- Similar approaches have been reported in an at-
compatibility and biodegradability, provide appro- tempt to treat sulcus vocalis. Tsunoda et al11-14 re-
priate space for regeneration, and have an appropri- ported that implantation of temporal fascia into the
ate environment for cells to grow and work. Also, vocal fold resulted in gradual improvements of max-
the viability and function of cells that infiltrate into imum phonation time. Unpublished data also sug-
the scaffolds should be maintained. gested that Alloderm implanted into the Reinke’s
As a candidate for a regenerative scaffold, we space of the sulcus might improve acoustic and stro-
have focused on atelocollagen sheeting (Teruder- boscopic parameters.2 However, how those materi-
mis). The sheeting used in this study is composed als work in the vocal fold is still unclear. One of the
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
619 Kishimoto et al, Implantation of Atelocollagen Sheet 619
Fig 7. (Case 4) Stroboscopic findings. A) Before treatment. B) After treatment, mucosal vibration shows improvement.
biggest advantages of Terudermis was thought to be kind of study. Also, it is difficult to confirm the re-
the porous structure of the sheet that can admit cells, cruitment of cells into the material, because histo-
as already shown in previous animal studies. logic evaluation cannot be achieved in this kind of
study. We do not insist that our scaffold has a defi
In most cases in this study, aerodynamic and
nite regenerative effect. The augmentative effects
acoustic analyses showed gradual improvement in
may overlap; however, we believe that some of the
all parameters over 1 year, with individual variation,
effects of the material are regenerative. The current
and restoration of periodic vibration was also ob-
study has only shown the possibility of Terudermis
served by videostroboscopy. These results suggest
as a regenerative scaffold. Further study is neces-
that the atelocollagen sheet implant has not only an
sary to better understand the material and also to de-
augmentative effect, but also a possible restorative
velop better surgical procedures.
effect. Thus, implantation of the atelocollagen sheet
into the vocal fold may have therapeutic potential in
CONCLUSIONS
cases of vocal fold scarring and sulcus vocalis.
The current study examined the feasibility of an
In case 3 only, most parameters worsened with atelocollagen sheet (Terudermis) implant for treat-
the implantation of Terudermis. It is conceivable ment of scarred vocal folds or sulcus vocalis. Six
that the implanted material was lost or dislocated. patients underwent implantation into the stiffened
In this case, fibrin glue was used to close the pocket. vocal folds. In most cases, videostroboscopic ex-
However, the actual reason for failure of improve- amination and aerodynamic and acoustic analyses
ment is uncertain. Furthermore, it is likely that the showed gradual improvement over 1 year after sur-
effect of an implant may be influenced by individual gery. The results suggest that implantation of Teru
healing ability. dermis may have restorative effects in cases of vocal
It is impossible to use randomized controls in this fold scarring and sulcus vocalis.
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
620 Kishimoto et al, Implantation of Atelocollagen Sheet 620
REFERENCES
1. Hirano S. Current treatment of vocal fold scarring. Curr 2002;26:360-4.
Opin Otolaryngol Head Neck Surg 2005;13:143-7. 9. Koide M, Osaki K, Konishi J, et al. A new type of bio-
2. Dailey SH, Ford CN. Surgical management of sulcus vo- material for artificial skin: dehydrothermally cross-linked com-
calis and vocal fold scarring. Otolaryngol Clin North Am 2006; posites of fibrillar and denatured collagens. J Biomed Mater Res
39:23-42. 1993;27:79-87.
3. Sato K, Hirano M. Electron microscopic investigation of 10. Hatoko M, Kuwahara M, Tanaka A, Yurugi S, Iioka H,
sulcus vocalis. Ann Otol Rhinol Laryngol 1998;107:56-60. Niitsuma K. Correction of bone deformity after resection of der-
4. Tateya T, Tateya I, Sohn JH, Bless DM. Histologic char- moid cyst using artificial dermis implantation. Aesthetic Plast
acterization of rat vocal fold scarring. Ann Otol Rhinol Laryn- Surg 2002;26:35-9.
gol 2005;114:183-91. 11. Tsunoda K, Kondou K, Kaga K, et al. Autologous trans-
5. Kanemaru S, Nakamura T, Omori K, et al. Regeneration plantation of fascia into the vocal fold: long-term result of type-
of the vocal fold using autologous mesenchymal stem cells. 1 transplantation and the future. Laryngoscope 2005;115(suppl
Ann Otol Rhinol Laryngol 2003;112:915-20. 108):1-10.
6. Hirano S, Bless DM, Nagai H, et al. Growth factor ther- 12. Tsunoda K, Baer T, Niimi S. Autologous transplantation
apy for vocal fold scarring in a canine model. Ann Otol Rhinol of fascia into the vocal fold: long-term results of a new pho-
Laryngol 2004;113:777-85. nosurgical technique for glottal incompetence. Laryngoscope
2001;111:453-7.
7. Lee JW, Jang YC, Oh SJ. Use of the artificial dermis for
free radial forearm flap donor site. Ann Plast Surg 2005;55: 13. Tsunoda K, Niimi S. Autologous transplantation of fascia
500-2. into the vocal fold. Laryngoscope 2000;110:680-2.
8. Yurugi S, Hatoko M, Kuwahara M, Tanaka A, Iioka H, 14. Tsunoda K, Takanosawa M, Niimi S. Autologous trans-
Niitsuma K. Usefulness and limitations of artificial dermis im- plantation of fascia into the vocal fold: a new phonosurgical tech
plantation for posttraumatic deformity. Aesthetic Plast Surg nique for glottal incompetence. Laryngoscope 1999;109:504-8.
Downloaded from aor.sagepub.com at UNIV OF NORTH DAKOTA on May 23, 2015
You might also like
- Anatomy of Respiratory SystemDocument75 pagesAnatomy of Respiratory SystemAnonymous aqeaNUn80% (5)
- Grade 10 Science NotesDocument43 pagesGrade 10 Science NotesIoana Burtea89% (27)
- EmfizemulDocument19 pagesEmfizemulMirela IoanaNo ratings yet
- Abdominal Ultrasound Anatomy.: DR/ Abd Allah Nazeer. MDDocument50 pagesAbdominal Ultrasound Anatomy.: DR/ Abd Allah Nazeer. MDAri Dwi PrasetyoNo ratings yet
- Ian M Symonds Sabaratnam Arulkumaran E M Symonds Essential Obstetrics and Gynaecology PDFDocument449 pagesIan M Symonds Sabaratnam Arulkumaran E M Symonds Essential Obstetrics and Gynaecology PDFVilde Lie100% (8)
- ZL 124 Lecture 7 - Gastrulation in Birds & MammalsDocument36 pagesZL 124 Lecture 7 - Gastrulation in Birds & MammalsNestory MartineNo ratings yet
- The Cardiovascular System: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical CollegeDocument124 pagesThe Cardiovascular System: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical Collegelourd nabNo ratings yet
- Accessory OrgansDocument43 pagesAccessory Organslouradel100% (1)
- Who Classification of Head & Neck Tumors - 2017Document343 pagesWho Classification of Head & Neck Tumors - 2017Pablo Enrique Mejia Paz78% (40)
- Kishimoto 2009Document8 pagesKishimoto 2009anitaabreu123No ratings yet
- Resorbable Collagen Membranes: Histopathologic Features: ResultsDocument5 pagesResorbable Collagen Membranes: Histopathologic Features: Resultsحسن عسيريNo ratings yet
- Bone Regeneration in Sinus Lifts: Comparing Tissue-Engineered Bone and Iliac BoneDocument6 pagesBone Regeneration in Sinus Lifts: Comparing Tissue-Engineered Bone and Iliac BoneArmando Renteria BravoNo ratings yet
- Lou Et Al (2018) - Wound-Healing Effects of 635-nm Low-Level Laser Therapy On Primary Human Vocal Fold Epithelial Cells An in Vitro StudyDocument8 pagesLou Et Al (2018) - Wound-Healing Effects of 635-nm Low-Level Laser Therapy On Primary Human Vocal Fold Epithelial Cells An in Vitro StudyRobson LemosNo ratings yet
- 1990 RozemaDocument5 pages1990 Rozemapiyush joshiNo ratings yet
- The New "Cubism" Graft Technique in Tympanoplasty - A Randomized Controlled TrialDocument9 pagesThe New "Cubism" Graft Technique in Tympanoplasty - A Randomized Controlled Trialian danarkoNo ratings yet
- PRP Treatment Accelerates Healing of Acute Vocal Fold InjuriesDocument5 pagesPRP Treatment Accelerates Healing of Acute Vocal Fold InjuriesConstantin StanNo ratings yet
- Flap Surgical Techniques For Incisional Hernia Recurrences. A Swine Experimental ModelDocument9 pagesFlap Surgical Techniques For Incisional Hernia Recurrences. A Swine Experimental ModelFlorina PopaNo ratings yet
- Yoshimoto 2004Document5 pagesYoshimoto 2004r1comfupchNo ratings yet
- Fat Augmentation Vocal FoldsDocument8 pagesFat Augmentation Vocal FoldsRoy HallakNo ratings yet
- The Z-Meatoplasty For Modified Radical Mastoidectomy in ChildrenDocument4 pagesThe Z-Meatoplasty For Modified Radical Mastoidectomy in ChildrenMita DaudNo ratings yet
- Auricular Prostheses and Osseointegrated Implants: Experience UclaDocument6 pagesAuricular Prostheses and Osseointegrated Implants: Experience UclanoranNo ratings yet
- Mastoid Obliteration 1916-0216-42-49 PDFDocument7 pagesMastoid Obliteration 1916-0216-42-49 PDFFurqan MirzaNo ratings yet
- Bimaxillary Dentoalveolar Protrusion Traits andDocument7 pagesBimaxillary Dentoalveolar Protrusion Traits andSAM PRASANTHNo ratings yet
- Lanigan 1993Document15 pagesLanigan 1993MarkNo ratings yet
- Etiology and Treatment of Congenital Festoons PDFDocument11 pagesEtiology and Treatment of Congenital Festoons PDFprashanth kenchotiNo ratings yet
- The Use of Temporoparietal Fascia Flap For Surgical Treatment of Traumatic Auricle DefectsDocument5 pagesThe Use of Temporoparietal Fascia Flap For Surgical Treatment of Traumatic Auricle Defectslia indria watiNo ratings yet
- Granuloma PCLDocument5 pagesGranuloma PCLEmrys1987No ratings yet
- Bimaxillary Dentoalveolar Protrusion - Traits and Orthodontic CorrectionDocument7 pagesBimaxillary Dentoalveolar Protrusion - Traits and Orthodontic CorrectionAzra NadhiraNo ratings yet
- Fulco Et Al 2014Document10 pagesFulco Et Al 2014Alex PerryNo ratings yet
- IJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.HDocument6 pagesIJGMP - Medicine - Clinical Study of DALK in Heterogeneous Corneal Diseases - Srinivas K.Hiaset123No ratings yet
- Okc PDFDocument6 pagesOkc PDFanggiNo ratings yet
- Auricular Prostheses and Osseointegrated Implants: Experience UclaDocument6 pagesAuricular Prostheses and Osseointegrated Implants: Experience UclaPablo Gutiérrez Da VeneziaNo ratings yet
- Endofistula Laser Ablation of Fistula-In-Ano - A New Minimally Invasive Technique For The Treatment of Fistula-In-AnoDocument6 pagesEndofistula Laser Ablation of Fistula-In-Ano - A New Minimally Invasive Technique For The Treatment of Fistula-In-AnoagusNo ratings yet
- Guided Tissue Regeneration in Jaw Reconstruction: Review and ApplicationsDocument2 pagesGuided Tissue Regeneration in Jaw Reconstruction: Review and ApplicationsNurhidayah hasanNo ratings yet
- Modeling of human extraction socketsDocument10 pagesModeling of human extraction socketsMahendra PrihandanaNo ratings yet
- Tube Exposure Repair: 10.5005/jp-Journals-10008-1121Document4 pagesTube Exposure Repair: 10.5005/jp-Journals-10008-1121alineochoaaNo ratings yet
- Mother Touch in Periodontal Therapy: Chorion MembraneDocument7 pagesMother Touch in Periodontal Therapy: Chorion MembraneInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1998-Ricucci-Apical - Limit-II-IEJ PDFDocument17 pages1998-Ricucci-Apical - Limit-II-IEJ PDFGhenciu AndreiNo ratings yet
- RTGD RaspunsuriDocument17 pagesRTGD RaspunsuriDan BrynzaNo ratings yet
- Cranioplasty FinalDocument13 pagesCranioplasty Finalinfobusiness2010No ratings yet
- Easy Graft: "Bioabsorbable Root Analogue For Closure of Oroantral Communications After Tooth Extraction: A Prospective Case-Cohort Study"Document7 pagesEasy Graft: "Bioabsorbable Root Analogue For Closure of Oroantral Communications After Tooth Extraction: A Prospective Case-Cohort Study"Dentapex ThailandNo ratings yet
- Pathological Examination of Experimentally Induced Periodontal Polyp in Mice Technical NoteDocument4 pagesPathological Examination of Experimentally Induced Periodontal Polyp in Mice Technical NotekarinaNo ratings yet
- Ghan em 2005Document5 pagesGhan em 2005asfwegereNo ratings yet
- Cleft Palate CaseDocument5 pagesCleft Palate CaseyomifNo ratings yet
- Free Flaps MaxillaDocument7 pagesFree Flaps MaxillaFahad QiamNo ratings yet
- Study of Jones Procedure For Senile Entropion: Medical ScienceDocument3 pagesStudy of Jones Procedure For Senile Entropion: Medical SciencedhitadwynNo ratings yet
- Management of Broken Instrument by File Bypass Technique: Sultana Parveen, Mozammal Hossain and Md. Farid UddinDocument3 pagesManagement of Broken Instrument by File Bypass Technique: Sultana Parveen, Mozammal Hossain and Md. Farid UddinsetiabektidwikiNo ratings yet
- 00011Document10 pages00011M Joaquin Robles OrtizNo ratings yet
- Tunkel Comparacion Tecnicas2013Document9 pagesTunkel Comparacion Tecnicas2013SergioNo ratings yet
- Surgical Therapy of Peri-ImplantitisDocument17 pagesSurgical Therapy of Peri-Implantitiskaue francoNo ratings yet
- Histological Evaluation of Healing And: Revascularization of The Subepithelial Connective Tissue GraftDocument10 pagesHistological Evaluation of Healing And: Revascularization of The Subepithelial Connective Tissue GraftHector MurilloNo ratings yet
- A Long-Term Study of 370 Autotransplanted Premolars.Document11 pagesA Long-Term Study of 370 Autotransplanted Premolars.jing.zhao222No ratings yet
- Kim2016 Pdo MultifilamenDocument5 pagesKim2016 Pdo Multifilamenyolanda tejaNo ratings yet
- Implant-Supported Nasal Prosthesis. Clinical Case Report: Prótesis Nasal Implantosoportada. Reporte de Un Caso ClínicoDocument6 pagesImplant-Supported Nasal Prosthesis. Clinical Case Report: Prótesis Nasal Implantosoportada. Reporte de Un Caso ClínicoMelina Nataly Robles AcuñaNo ratings yet
- A Hollow Delayed Surgical ObturatorDocument55 pagesA Hollow Delayed Surgical ObturatorvinnycoolbuddyNo ratings yet
- 99 IJPRD EMD TechDocument10 pages99 IJPRD EMD Techinamboy7No ratings yet
- Effect of Hyaluronic Acid On The Osseointegration of Dental ImplantsDocument5 pagesEffect of Hyaluronic Acid On The Osseointegration of Dental Implantsjaviers45No ratings yet
- Frontolateral Partial LaryngectomyDocument7 pagesFrontolateral Partial LaryngectomyJeremy HermantoNo ratings yet
- Congress Auricular Reconstruction AbstractsDocument92 pagesCongress Auricular Reconstruction AbstractsRocio RamirezNo ratings yet
- Conjunctival-Limbal Autograft Effective for Primary, Recurrent PterygiumDocument3 pagesConjunctival-Limbal Autograft Effective for Primary, Recurrent PterygiumMichael HumiantoNo ratings yet
- The Internolionol Joumal o (Periodontics & Restorolive DentishyDocument21 pagesThe Internolionol Joumal o (Periodontics & Restorolive DentishyJohanna Andrea CalderónNo ratings yet
- Carnoy's Solution in The Management of Odontogenic KeratocystDocument4 pagesCarnoy's Solution in The Management of Odontogenic KeratocystlydiaNo ratings yet
- Spiegel 2004Document5 pagesSpiegel 2004manuel abantoNo ratings yet
- Perichondrium Graft: Harvesting and Indications in Nasal SurgeryDocument5 pagesPerichondrium Graft: Harvesting and Indications in Nasal SurgerySyahnidel FitaNo ratings yet
- Horizontal Ridge Augmentation Using GBR With A Native Collagen Membrane and 1:1 Ratio of Particulate Xenograft and Autologous Bone: A 3 Year After Final Loading Prospective Clinical StudyDocument9 pagesHorizontal Ridge Augmentation Using GBR With A Native Collagen Membrane and 1:1 Ratio of Particulate Xenograft and Autologous Bone: A 3 Year After Final Loading Prospective Clinical StudyYodel SrnthNo ratings yet
- Intl J Gynecology Obste - 2023 - Clark - Dehydrated Human Amniotic Membrane and Amniotic Fluid Allograft For TheDocument3 pagesIntl J Gynecology Obste - 2023 - Clark - Dehydrated Human Amniotic Membrane and Amniotic Fluid Allograft For TheUrología GinecológicaNo ratings yet
- Dapus 11 Referat 2Document3 pagesDapus 11 Referat 2Akramanto RidwanNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Surgical Management of Childhood Glaucoma: Clinical Considerations and TechniquesFrom EverandSurgical Management of Childhood Glaucoma: Clinical Considerations and TechniquesAlana L. GrajewskiNo ratings yet
- TracheostomyDocument10 pagesTracheostomyanitaabreu123No ratings yet
- Allergic Rhinitis Clinical GuidelineDocument43 pagesAllergic Rhinitis Clinical Guidelineanitaabreu123No ratings yet
- Sulcus Mucosal Slicing TecniqueDocument9 pagesSulcus Mucosal Slicing Tecniqueanitaabreu123No ratings yet
- Clinical Practice Guideline: Tympanostomy Tubes in Children (Update)Document56 pagesClinical Practice Guideline: Tympanostomy Tubes in Children (Update)anitaabreu123No ratings yet
- Brandt Daroff Excercises Quick GuideDocument9 pagesBrandt Daroff Excercises Quick GuideEldar SulejmanovicNo ratings yet
- (Revisi) NANDA CSS - ParotitisDocument40 pages(Revisi) NANDA CSS - Parotitisbunga juliaNo ratings yet
- Preauricular SinusDocument2 pagesPreauricular Sinusanitaabreu123No ratings yet
- Correcting Caudal Septal Deviation With A Modified Horizontal Mattress SutureDocument3 pagesCorrecting Caudal Septal Deviation With A Modified Horizontal Mattress Sutureanitaabreu123No ratings yet
- Vocal Fold Scars - A Common Classifcation Proposal by The AmericanDocument4 pagesVocal Fold Scars - A Common Classifcation Proposal by The Americananitaabreu123No ratings yet
- Vocal Fold Scars Current Concepts and Future Directions. Consensus Report of The Phonosurgery Committee of The European Laryngological SocietyDocument17 pagesVocal Fold Scars Current Concepts and Future Directions. Consensus Report of The Phonosurgery Committee of The European Laryngological Societyanitaabreu123No ratings yet
- Sulcus Mucosal Slicing TecniqueDocument9 pagesSulcus Mucosal Slicing Tecniqueanitaabreu123No ratings yet
- Vocal Fold Scars - A Common Classifcation Proposal by The AmericanDocument4 pagesVocal Fold Scars - A Common Classifcation Proposal by The Americananitaabreu123No ratings yet
- Prevalence of Minor Larynx StructuralDocument7 pagesPrevalence of Minor Larynx Structuralanitaabreu123No ratings yet
- Pre-Auricular Abscess Due To Mycobacterium TuberculosisDocument3 pagesPre-Auricular Abscess Due To Mycobacterium Tuberculosisanitaabreu123No ratings yet
- Recurrent Epistaxis in ChildrenDocument3 pagesRecurrent Epistaxis in Childrenanitaabreu123No ratings yet
- Excision of Preauricular Sinus With Abscess Drainage in ChildrenDocument10 pagesExcision of Preauricular Sinus With Abscess Drainage in Childrenanitaabreu123No ratings yet
- Preauricular SinusDocument2 pagesPreauricular Sinusanitaabreu123No ratings yet
- Analysis of Incidence and Genetic Predisposition of Preauricular SinusDocument3 pagesAnalysis of Incidence and Genetic Predisposition of Preauricular Sinusanitaabreu123No ratings yet
- Sulcus Mucosal Slicing TecniqueDocument9 pagesSulcus Mucosal Slicing Tecniqueanitaabreu123No ratings yet
- Extrapulmonary TuberculosisDocument19 pagesExtrapulmonary Tuberculosisanitaabreu123No ratings yet
- Anosmia and Olfactory Tract Neuropathy in A Case of COVID-19Document4 pagesAnosmia and Olfactory Tract Neuropathy in A Case of COVID-19anitaabreu123No ratings yet
- Educational Value of A Preoperative CT Sinus Checklist A Resident's PerspectiveDocument3 pagesEducational Value of A Preoperative CT Sinus Checklist A Resident's Perspectiveanitaabreu123No ratings yet
- He International Frontal Sinus Anatomy Classification (IFAC) and Classification of The Extent of Endoscopic Frontal Sinus Surgery (EFSSDocument20 pagesHe International Frontal Sinus Anatomy Classification (IFAC) and Classification of The Extent of Endoscopic Frontal Sinus Surgery (EFSSanitaabreu123No ratings yet
- Single-Blinded Prospective Implementation of A Preoperative Imaging Checklist For Endoscopic Sinus Surgery.Document4 pagesSingle-Blinded Prospective Implementation of A Preoperative Imaging Checklist For Endoscopic Sinus Surgery.anitaabreu123No ratings yet
- A Useful Tool-Systematic Checklist For Evaluating Sinus Scans.Document3 pagesA Useful Tool-Systematic Checklist For Evaluating Sinus Scans.anitaabreu123No ratings yet
- Vitamin A BeneficialDocument7 pagesVitamin A Beneficialanitaabreu123No ratings yet
- Single-Blinded Prospective Implementation of A Preoperative Imaging Checklist For Endoscopic Sinus Surgery.Document4 pagesSingle-Blinded Prospective Implementation of A Preoperative Imaging Checklist For Endoscopic Sinus Surgery.anitaabreu123No ratings yet
- Educational Value of A Preoperative CT Sinus Checklist A Resident's PerspectiveDocument3 pagesEducational Value of A Preoperative CT Sinus Checklist A Resident's Perspectiveanitaabreu123No ratings yet
- The Anatomy and Function of the Pleural CavityDocument8 pagesThe Anatomy and Function of the Pleural CavityKina KinaNo ratings yet
- EASL Hepatitis C Treatment Guidelines and Risk Factors for Alcoholic Liver DiseaseDocument13 pagesEASL Hepatitis C Treatment Guidelines and Risk Factors for Alcoholic Liver DiseaseJolaine ValloNo ratings yet
- Cell Organelle Functions and City AnalogsDocument13 pagesCell Organelle Functions and City AnalogsSean GonzalezNo ratings yet
- Nephrolithiasis AnatomyDocument3 pagesNephrolithiasis AnatomyKevin Ker Campaner MerillesNo ratings yet
- Goldfinger Human Anatomy For Artists PDFDocument4 pagesGoldfinger Human Anatomy For Artists PDFSamuelNo ratings yet
- Anatomy of the PelvisDocument10 pagesAnatomy of the PelvisJISHNU TKNo ratings yet
- Small Animal Abdominal Ultrasonography - The SpleenDocument9 pagesSmall Animal Abdominal Ultrasonography - The Spleenludiegues752No ratings yet
- +1 Zoology Focus Area NotesDocument85 pages+1 Zoology Focus Area NotesKhatarnakNo ratings yet
- Staining MethodsDocument8 pagesStaining MethodsMd Arshad100% (1)
- Maternal and Child Nursing - Antepartum Practice Test With AnswersDocument6 pagesMaternal and Child Nursing - Antepartum Practice Test With Answersgelean payodNo ratings yet
- Morphology Internationaljournalplantsciences2011Document14 pagesMorphology Internationaljournalplantsciences2011wenagoNo ratings yet
- Vernix Caseosa Formation and FunctionsDocument5 pagesVernix Caseosa Formation and FunctionsPriscila FloresNo ratings yet
- PhysioPsych Assignment1Document9 pagesPhysioPsych Assignment1Tiffany ZenhoihsangNo ratings yet
- MBCHB YEAR 1 TERM 2. 2022 (2021 Class)Document2 pagesMBCHB YEAR 1 TERM 2. 2022 (2021 Class)BedanNo ratings yet
- Micro McqsDocument1 pageMicro Mcqsmurtaza hashmiNo ratings yet
- Coordination and Control in the Human BodyDocument37 pagesCoordination and Control in the Human Bodywardah nooriNo ratings yet
- Hematology Topics Objectives References: Our Lady of Fatima University Department of Internal MedicineDocument7 pagesHematology Topics Objectives References: Our Lady of Fatima University Department of Internal MedicineAlmar NuñezNo ratings yet
- RBC MORPH UlkaDocument53 pagesRBC MORPH UlkaRushi WalgudeNo ratings yet
- Respiratory System AssignmentDocument3 pagesRespiratory System AssignmentzainaNo ratings yet
- Pelvic Pain - Sundhed - DKDocument11 pagesPelvic Pain - Sundhed - DKPavel BerlinschiNo ratings yet
- Chapter 3 Animal Tissues SolutionDocument6 pagesChapter 3 Animal Tissues SolutionLucky ErrojuNo ratings yet