Professional Documents
Culture Documents
Anesthesia Consideration For Cranipharyngioma Resection in Pediatric Patient
Uploaded by
pitriaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anesthesia Consideration For Cranipharyngioma Resection in Pediatric Patient
Uploaded by
pitriaCopyright:
Available Formats
esia & Cli
sth n
Journal of Anesthesia & Clinical
ne
ica
al of A
l Research
Nezar et al., J Anesth Clin Res 2017, 8:4
Research
urn
DOI: 10.4172/2155-6148.1000716
Jo
ISSN: 2155-6148
Case Report Open Access
Anesthetic Considerations for Craniopharyngioma Resection in Pediatric Patient
with Fontan Physiology: A Case Report
Al Zughaibi Nezar1, Mahmoud A Haroun1*, Metwally A Mounir1, Mahran A Hamada1 and Mahmoud M Okasha2
1King Abdullah Specialized Children Hospital KASCH, Riyadh, Saudi Arabia
2Faculty of Medicine, Ain Shams University, Egypt
*Corresponding author: Mahmoud A Haroun, Department of Anesthesia, King Abdullah Specialized Children Hospital KASCH, Riyadh, Saudi Arabia, E-mail:
haroun1ahm@hotmail.com
Received date: March 13, 2017; Accepted date: April 10, 2017; Published date: April 17, 2017
Copyright: © 2017 Nezar AZ, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Fontan procedure is a palliative surgery done for patients born with single ventricle physiology. An understanding
of the hemodynamic alterations in such a patient is important for successful perioperative management. Added to
this challenge is the Craniopharyngioma which constitute about 2-6% of all the intracranial tumors in pediatric age
group. Management of craniopharyngiomas in children is very challenging for anesthesiologist, owing to the
developing neurological and physiological status, handling of a growing brain, perioperative endocrinological
complications, and the management of hydration. We discuss the anesthetic considerations for a 6 years old female
with Fontan circulation going for craniopharyngioma resection under general anesthesia.
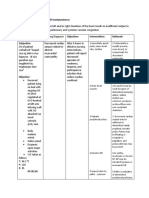
Keywords: Congenital heart disease; Fontan; Craniopharyngioma; hydrocephalus which showed level indicating hemorrhagic
General anesthesia component, pituitary gland was compressed inferiorly by the lesion,
brain parenchyma showed normal signal intensity, posterior fossa
Introduction structures were normal and diagnosed provisionally as
Craniopharyngioma (Figure 1).
In 1971, Fontan and Baudet described a procedure for
management of patients with a single ventricle pathology that diverted
all systemic venous blood into the pulmonary arteries, without
interposition of a ventricle, as a surgical palliation for patients with
tricuspid atresia [1]. With advancement of surgical techniques and
medical management, many patients with Fontan physiology present
for non-cardiac surgeries. Craniopharyngiomas are benign neoplasms
commonly located in the sellar or the suprasellar region and most
commonly presenting as visual defects [2-4]. management of
these intracranial tumors poses a challenge for anesthesiologists
especially if occurred in a patient with Fontan physiology. Also
understanding the Fontan physiology and circulation is essential for
safe and successful anesthetic management of these patients.
Perioperative diagnosis and management of endocrinological
complications of craniopharyngioma is essential for reducing the
mortality and morbidity associated with the surgery.
Case Report
We report here the anesthetic management of 6 years old female
weighing 15 kg, electively scheduled for Craniopharyngioma resection.
Neurologically, the patient presented with headache, vomiting and
seizures. CT brain showed a lesion in the suprasellar cistern extending
to the of the 3rd ventricle, mild active hydrocephalus at both
lateral Ventricles, otherwise cerebellum, basal ganglia and brainstem
were normal. Brain MRI showed a bilobed mainly cystic lesion in the
suprasellar cistern extending into the sella. lesion measured 2.3 ×
1.7 × 3 cm in anteroposterior, transverse, and craniocervical Figure 1: MRI brain.
dimensions respectively encasing the optic chiasma and M1 segment of
right middle cerebral artery. It displaced the inferior wall of the lateral
ventricles superiorly and caused obstructive supratentorial
J Anesth Clin Res, an open access journal Volume 8 • Issue 4 • 1000716
ISSN:2155-6148
Citation: Nezar AZ, Haroun MA, Mounir MA, Hamada MA, Okasha MM (2017) Anesthetic Considerations for Craniopharyngioma Resection in
Pediatric Patient with Fontan Physiology: A Case Report. J Anesth Clin Res 8: 716. doi:10.4172/2155-6148.1000716
Page 2 of 5
The patient gave history of complex congenital heart disease in the muscle relaxation according to the train of four (TOF). By the end of
form of double inlet left ventricle (DILV), pulmonary stenosis (PS). the procedure, total fentanyl used was 110 mcg and rocuronium was 50
She underwent right Blalock-Taussig (BT) shunt (a right subclavian mg. Steroid replacements with 4 mg Dexamethasone was given
artery to right pulmonary artery shunt) shortly after birth, followed by intravenously with induction of anesthesia.
a Glenn procedure (anastomosis between superior vena cava and right
The patient was ventilated using pressure controlled (PC)
pulmonary artery) after few months and finally 2 months before
ventilatory mode with peak inspiratory pres-sure (PIP) of 15 cmH2O,
craniotomy she had BT shunt dissection and modified Fontan
respiratory rate (RR) 18 bpm and Positive End Expiratory Pressure
procedure (this time anastomosing the inferior vena cava to the right
PEEP 4 cmH2O. The end-tidal carbon dioxide was maintained within
pulmonary artery). She was on warfarin 5 mg, furosemide 20 mg and
the range of 30-35 mmHg. Her blood pressure and heart rate were
Captopril 12.5 mg once a day. Functionally, she had no cardiovascular
stable throughout the procedure, and maintained within 20% of the
(CVS) complaints at the time of admission, and was regular in her
baseline values. The patient developed transient mild Diabetes
follow up in pediatric cardiology clinic with fair physical activity. The
insipidus (DI), UOP was more than 6 ml/Kg/h and serum Na in blood
patient was graded 3 as per the American Society of Anesthesiologists
gases was in range of 135-139 mg/dL. It was successfully managed with
(ASA III).
urine output monitoring hourly and replacing IV fluids.
On examination, she was conscious, oriented, well nourished,
Surgery lasted 6 h 24 minutes in supine position with 30 degree
afebrile, her heart rate was 82 beats/minute, regular and equal
head up to provide adequate surgical exposure and venous drainage
bilaterally, arterial blood pressure was 104/73 mmHg and pulse O2
with total blood loss around 100 ml. At the end of the procedure
saturation (SpO2) was 99%. On cardiopulmonary examination there
further analgesia was given in form of 1.5 mg of IV morphine and 250
was equal air entry bilaterally with no adventitious sounds and a grade
mg of IV paracetamol, 0.2 mg of IV Granisetron was given to prevent
2 systolic murmur, on neurological examination there was no
postoperative nausea and vomiting and reversal of muscle relaxant was
neurological deficit or visual disturbance and Glasgow Coma Scale
done using 0.15 mg of IV glycopyrrolate and 0.75 mg of IV
(GCS) was 15/15 while other systemic examination was unremarkable.
neostigmine for the planned extubation. The patient was extubated
Investigations revealed hemoglobin of 11.2 g/dL and normal total successfully in the operating theater and was hemodynamically stable
and differential white blood cell counts. Renal function tests (RFT), having a BP of 110/64 mmHg, HR of 119 bpm and SpO2 of 100%.
liver function tests (LFT), thyroid stimulating hormone (TSH), free T4, Patient was transferred to PICU for further hemodynamic and
blood sugar and serum proteins were within normal limits, serum neurological monitoring. Monitoring UOP, plasma and urinary Na and
sodium (Na) was 132 mg/dl, serum cortisol 34 nmol/L and osmolality for possible diabetes insipidus (DI) was mandatory.
prothrombin time was 22 seconds with an INR of 2.1.
Postoperatively she had manifestations of DI that continued for the
Electrocardiogram (ECG) was regular and showed sinus rhythm. Chest
next 2 days and was successfully managed using intranasal
X ray showed mild cardiomegally and clear lung fields.
desmopressin (10 µg per puff) administered one puff two times daily
Echocardiography showed no obstruction to Fontan pathway, patent
together with replacing IV fluids and urine output monitoring hourly.
bilateral bidirectional glenn, mild left and right atrioventricular valve
The child recovered well thereafter and a computed tomography (CT)
(AVV) regurgitation and mildly depressed ventricular systolic
scan after surgery revealed a small amount of residual lesion in
function. No systemic outflow tract obstruction and no pericardial
suprasellar. Anticoagulant was resumed in the postoperative period
effusion were seen. There was a normal single ventricle physiology,
after ensuring adequate homeostasis according to bridging protocol.
patent foramen ovale (PFO) with no thrombi or vegetations.
The histopathological examination confirmed the diagnosis of
A cardiology consultation was done and recommendation was to craniopharyngioma. The patient was discharged on the 10th
bridge warfarin using a low-molecular weight heparin (LMWH) 5 days postoperative day and was prescribed chemotherapy and regular
prior to surgery (40 mg Enoxaparin subcutaneous twice a day to be follow-up.
withheld 12 h prior to surgery), repeat INR one day before the surgery
to be less than 1.5 and give prophylaxis against infective endocarditis. Discussion
Ophthalmic Consultation for fundus examination showed normal
confrontation visual fields but she was not so cooperative to complete Neurosurgery in the pediatric patients is a challenge not only for the
visual fields. neurosurgeon but also for anesthesiologist due to neurophysiological
variations between adult and pediatric population [1]. CBF in infants
On the day of surgery the patient was reassessed and infective and older children (about 90 to 100 mL/100 g/min) is higher than the
endocarditis prophylaxis was given in form of cefazolin 50 mg/kg 1 h adult CBF (50 mL/100 g/min). Also there is tight coupling between
prior to the procedure. She was premedicated using intravenous (IV) CBF and the metabolic requirement for oxygen (CMRO2). CMRO2 in
midazolam 0.1 mg/kg, and then she was taken to the operating room. children is 5.2 mL/100 g/min, which is again higher than the CMRO2
Standard monitors were applied in the form of 5-leads in the adults (3.5 mL/100 g/min). Thus, children are more liable for
Electrocardiogram (ECG), non-invasive arterial blood pressure hypoxia-ischemic insult more than the adult. Cerebral auto-regulation
(NABP) and pulse oximetry. Anesthesia was induced using IV exists in the pediatric brain and any extreme variations in blood
ketamine 2 mg/kg, IV fentanyl 2 µg/kg, IV rocuronium 1 mg/kg and pressure beyond the limits of auto-regulation place the child at a risk of
was intubated uneventfully with cuffed endotracheal tube size 5.5 mm. developing cerebral ischemia or intraventricular hemorrhage. The large
Right radial artery was cannulated for invasive arterial blood pressure head in children represents a large percentage of body surface area and
(IABP) monitoring and left femoral vein was cannulated for central blood volume and so a large volume of their cardiac output is directed
venous pressure (CVP) monitoring. Capnography, urinary catheter to the brain, thus, increasing the risk of hemodynamic instability in the
and temperature monitoring were also established. Anesthesia was perioperative period [2].
maintained with sevoflurane in oxygen: air (40:60) keeping Minimum
alveolar Concentration (MAC) 0.5-1.2, titrating rocuronium for
J Anesth Clin Res, an open access journal Volume 8 • Issue 4 • 1000716
ISSN:2155-6148
Citation: Nezar AZ, Haroun MA, Mounir MA, Hamada MA, Okasha MM (2017) Anesthetic Considerations for Craniopharyngioma Resection in
Pediatric Patient with Fontan Physiology: A Case Report. J Anesth Clin Res 8: 716. doi:10.4172/2155-6148.1000716
Page 3 of 5
Craniopharyngiomas represent about 2-6% of all the intracranial b) adequate preload, c) patent anastomotic connections between the
tumors in the pediatric population [3]. These benign neoplasms are caval veins and pulmonary arteries and d) low intra-thoracic pressure.
commonly located in the sellar or the suprasellar region, thus, most
2) Adequate downstream component which requires unobstructed
commonly presenting with mass effect on nerves (commonly present
pulmonary arterial/pulmonary venous flow a) low PAP (<15-20
by visual field defect), vessels or hypothalamic pituitary disorder which
mmHg), and b) low PVR
may present with endocrine abnormalities [2,3,4]. Thus, preoperative
screening and optimization for any hormonal imbalance is essential. Patients with fontan physiology also have baseline venoconstriction
Perioperative steroid replacement therapy is also required. Risk of DI to maximally augment the preload and therefore anesthetics that cause
preoperatively (8-35%), rarely intraoperatively, but most commonly in venodilatation can lead to cardiac instability by detrimental effect to
the postoperative period (70-90%) which causes large volumes of urine CO [11]. So CO is maintained by adequate ventricular filling, normal
loss that need to be replaced on an hourly basis. DI may even require AV valve, adequate diastolic and systolic function and normal sinus
pharmacological treatment with synthetic vasopressin (DDAVP or rhythm. Alterations in ventricular function or the onset of arrhythmias
desmopressin) if the resultant hypovolemia is not corrected with fluids can lead to decreased CO and symptomatic deterioration [7].
[4]. Management of craniopharyngioma poses a challenge for
Late complications of fontan include progressive myocardial
neurosurgeons, endocrinologists, oncologists as well as
dysfunction and failure [12], atrial arrhythmias which are extremely
anesthesiologists on account, includes surgical resection and post-
resistant to pharmacological therapy and causing rapid hemodynamic
surgery radiotherapy/chemotherapy for residual lesion [5,6].
deterioration and heart failure [13], protein losing enteropathy which
Due to modification of surgical techniques and medical care, presents with oedema, immunodeficiency, ascites and fat
patients with congenital heart diseases for noncardiac surgeries malabsorption [14], chronic hepatic venous congestion which progress
expanded and became an important health care issue [7]. One of these to centrilobular necrosis, fibrosis and cirrhosis [15], and renal
patients are patients with fontan physiology which represent a unique dysfunction due to systemic venous hypertension and reduced renal
challenge for the anesthesiologists during the perioperative period, so Perfusion [13]. Patients with fontan physiology are at high risk of
understanding the fontan physiology circulation is essential for safe thromboembolism, due to low flow states, arrhythmias, and
and successful anesthetic management of these patients. It is hypercoagulability. Bridging therapy should be prescribed to patients
recommended for those patients to be managed at centers where the on warfarin until treatment can be continued [16-18]. Risk of infective
relevant cardiologist and intensive care unit expertise are available. endocarditis, so perioperative antibiotic prophylaxis with broad
Anesthesiologists who care for them must be familiar with the fontan spectrum cover is required. The risk of air or fat emboli occurring
physiology and perioperative management to optimize outcomes during major surgery especially head and neck surgery is relatively
because congenital heart disease is a risk factor for increased mortality high in patients with a fenestrated fontan. So some cardiologists
for non-cardiac surgery [7]. recommend closing a fenestration preoperatively for patients
undergoing high risk surgery [7].
In 1971 Fontan and Baudet [8], described a right atrial to
pulmonary artery shunt procedure for tricuspid atresia. It involved During the preoperative evaluation for the patients with fontan
diverting systemic venous blood from the right atrium to the physiology undergoing craniopharyngioma resection, it is important to
pulmonary arteries, thus bypassing the right ventricle. This can be consider the congenital structural pathology, degree of palliation
done in two ways: completed at the time of assessment, the functional status, and
comorbidities found in these patients which varies significantly [7].
Lateral tunnel Fontan where a baffle is placed inside the atrium to
Neurological examination (sensorium, cranial nerves, and any
direct the systemic venous blood from the Inferior Vena Cava (IVC) to
evidences of raised intracranial pressure) [1], so evaluation of these
the lungs.
patients involves a detailed history and physical examination using a
Extra cardiac where the inferior vena cava is split from the heart and multisystem approach with attention to the unique characteristics of
anastomosed to the pulmonary artery using a conduit. A fenestration this patient population (cardiac and neurological). A detailed medical
is created between the right atrium and the conduit which reduces the history should focus on changes in health status, exercise tolerance,
chance for pleural effusion to develop when the pulmonary vascular current medication, hospital admissions, thorough physical
resistance (PVR) becomes significantly raised [7]. examination, and baseline hematological, coagulation and biochemical
investigations (electrolyte , renal and hepatic function) are always
The fontan circulation functions by passive flow of the systemic
necessary even before minor surgery [7], In addition, children with
venous return to the pulmonary vasculature and then to the single
pituitary tumors require complete endocrinological evaluation [1]. A
ventricle. So, pulmonary blood flow and cardiac output are the result
12-lead ECG and echocardiography also required for assessment of
of the pressure difference between the “upstream” component
rhythm, ventricular and valvular function, pulmonary vascular
(consisting of the caval veins and the pulmonary artery) and the
resistance and ventricular end diastolic pressure [7].
“downstream” component [9] (the pulmonary veins/atrium/single
ventricle system). The ideal systemic venous pressure of Fontan Intraoperatively, our anesthetic goal is to maintain adequate CO (as
circulation is approximately 10-15 mmHg and the pulmonary venous a slight compromise in CO can be hazardous) and maintaining
atria (functional left atrium) pressure is approximately 5-10 mmHg; so adequate cerebral perfusion and oxygenation. Also we have to ensure
it allows a Trans pulmonary gradient driving pressure of 5-8 mmHg. adequate preload, maintain good ventricular filling and contractility
Any factor that affects this gradient could compromise the single while avoiding an increase in afterload. Since the blood flow from the
ventricle filling and hence the CO [9,10]. So patent fontan circulation systemic veins to the pulmonary circulation is passive, any increase in
depend on: PVR can impair ventricular filling and CO. Consequently, it is
important to avoid any factor increase the PVR that may be
1) Adequate the upstream component flow which depends on a)
precipitated by hypercarbia, hypoxia, acidosis, inadequate analgesia or
unobstructed venous return from IVC and Superior Vena Cava (SVC),
J Anesth Clin Res, an open access journal Volume 8 • Issue 4 • 1000716
ISSN:2155-6148
Citation: Nezar AZ, Haroun MA, Mounir MA, Hamada MA, Okasha MM (2017) Anesthetic Considerations for Craniopharyngioma Resection in
Pediatric Patient with Fontan Physiology: A Case Report. J Anesth Clin Res 8: 716. doi:10.4172/2155-6148.1000716
Page 4 of 5
anesthesia, hypothermia, use of vasoactive drugs, excessive mean aesthetic agents to minimize excessive peak depressant effects, care to
airway pressure, and compression of the lung by pleural effusion or minimize the circulatory effects of positive pressure ventilation,
high PEEP [7]. intensive and invasive monitoring of the circulation throughout the
procedure and rapid access to cardiovascular resuscitation drugs such
So anesthesiologists should choose induction agents with the least
as inotropes and vasopressors are corner-stones of management in
effect on myocardial contractility, cardiac output and pulmonary blood
such a case.
flow [7]. Propofol may cause profound decreases in venous return and
myocardial depression. Etomidate is a suitable induction agent for the
preservation of myocardial contractility, PVR, and vascular tone References
[19,20]. Ketamine may be used but it increases PVR and myocardial 1. Bhatnagar V, Dwivedi D, Tandon U, Bhushan K (2015) The challenges in
oxygen consumption [21]. It is advisable to avoid muscle relaxants that anesthetic management of pediatric craniopharyngioma, Karnataka
cause histamine release, which can result in hypotension and Anaesth J 1: 205-207.
tachycardia which adversely affect the COP and cerebral perfusion. 2. Krass IS (2007) Physiology and metabolism of brain and spinal cord. In:
Succinylcholine and rocuronium are recommended for rapid sequence Handbook of Neuroanaesthesia. Philadelphia: Lippincott Williams &
induction because of their minimal vagolytic and minimal histamine Wilkins 3-22.
release proper-ties. Cisatracurium and vecuronium are also useful for 3. Haupt R, Magnani C, Pavanello M, Caruso S, Dama E, et al. (2006)
their stable hemodynamic properties [22]. High concentrations of Epidemiological aspects of craniopharyngioma. J Pediatr Endocrinol
volatile agents should be avoided due to its dose dependent myocardial Metab 19 Suppl 1: 289-293.
depression. Thus, a low con-centration of an inhalational agent in 4. Karavitaki N, Cudlip S, Adams CB, Wass JA (2006) Craniopharyngiomas.
Endocr Rev 27: 371-397.
combination with an infusion to titration of a short acting opioid
provides a cardio stable anesthetic [23]. 5. Takahashi H, Yamaguchi F, Teramoto A (2005) Long-term outcome and
reconsideration of intracystic chemotherapy with bleomycin for
In addition to standard monitoring, Central Venous Pressure (CVP) craniopharyngioma in children. Childs Nerv Syst 21: 701-704.
and invasive arterial monitoring are mandatory in Fontan patient as 6. Bajwa SJ, Bajwa SK, Bindra GS (2011) The anesthetic, critical care and
we are expecting significant volume shift. Monitoring the trend of the surgical challenges in the management of craniopharyngioma. Indian J
CVP can help in the assessment of vascular volume status, as it reflects Endocrinol Metab 15: 123-126.
only mean pulmonary artery pressure (mPAP) and not ventricular 7. Kothandan H, Leanne LM, Shah SKS (2015) Fontan Physiology:
Anaesthetic Implications for Non-Cardiac Surgery: A Case Report. Int J
preload. Transesophageal echocardiography (TEE) can be used not
Anesthetic Anesthesiol ogy 2: 020.
only for intraoperative assessment of ventricular preload and function
but also for early detection of air emboli [7] (unfortunately it was 8. Fontan F, Baudet E (1971) Surgical repair of tricuspid atresia. Thorax 26:
240-248.
unavailable in our case). Monitoring of UOP on hourly base is
9. MCGowan F (2005) Perioperative issues in patients with congenital heart
mandatory for early detection of DI [2]. disease. International Anesthesia Research Society, Review course
Inadequate pulmonary blood flow may occur due to hypovolemia lectures 53-61.
or increased pulmonary vascular resistance (PVR) [13]. Although 10. Motoyama KE, Davis PJ (1996) Smith’s Anesthesia for infants and
children (6thedn) 445-539.
positive intrathoracic pressure may limit antegrade flow or even
reverse flow in these systemic venous beds [23], controlled ventilation 11. McClain CD, McGowan FX, Kovatsis PG (2006) Laparoscopic surgery in
a patient with Fontan physiology. Anesth Analg 103: 856-858.
is used for prolonged and major surgery. Controlled ventilation with a
ventilator strategy of low mean airway pressure, moderate alkalosis 12. Piran S, Veldtman G, Siu S, Webb GD, Liu PP (2002) Heart failure and
ventricular dysfunction in patients with single or systemic right
(PH=7.45, pCO2=35 mmHg), tidal volume of 5-6 ml/kg, low ventricles. Circulation 105: 1189-1194.
respiratory rate, short inspiratory times, low PEEP usually allow
13. Nayak S, Booker PD (2008) The Fontan Circulation. Contin Educ
adequate pulmonary blood flow with minimal hemodynamic effects Anaesth Crit Care Pain 8: 26-30.
[7]. 14. Mertens L, Haler DJ, Sauer U, Somerville J, Gewillig M (1998) Protein-
Surgical intervention may be associated with possible neuronal losing enteropathy after the Fontan operation: An international
multicenter study. J Thorac Cardiovasc Surg 115: 1063-1073.
damage to the thalamus and the mammillothalamic tract, that is more
in cases of developing brains of pediatric population and damage to 15. Narkewicz MR, Sondheimer HM, Ziegler JW, Otanni Y, Lorts A, et al.
(2003) Hepatic dysfunction following the Fontan procedure. J Pediatr
nerves in the surgical site vicinity. Our patient had developed DI Gastroenterol Nutr 36: 352-357.
during the postoperative period that was managed with intranasal
16. Coon PD, Rychik J, Novello RT, Ro PS, Gaynor JW, et al. (2001)
desmopressin along with fluid management and UOP monitoring each Thrombus formation after the Fontan operation. Ann Thorac Surg 71:
hour [5,6]. Postoperatively, these patients should be admitted to a 1990-1994.
monitored unit (ICU) to maintaining adequate analgesia, ensuring 17. Weipert J, Noebauer C, Schreiber C, Kostolny M, Zrenner B, et al. (2004)
adequate ventilation, fluid management and providing supplemental Occurrence and management of atrial arrhythmia after long-term Fontan
oxygen are essential [7]. Also monitoring of UOP, fluid management circulation. J Thorac Cardiovasc Surg 127: 457-464.
and controlling of any endocrinal emergency [1]. 18. Walker HA, Gatzoulis MA (2005) Prophylactic anticoagulation following
the Fontan operation. Heart 91: 854-856.
Conclusion 19. Sprung J, Ogletree-Hughes ML, Moravec CS (2000) The effects of
etomidate on the contractility of failing and nonfailing human heart
The most significant risk in this patient condition combined with muscle. Anesth Analg 91: 68-75.
Fontan physiology is the acute cardio-vascular collapse at induction of 20. Andropoulos DB, Stayer SA, Skjonsby BS, East DL, McKenzie ED, et al.
anesthesia, loss of reserve due to hypovolemia because of the high (2002) Anesthetic and perioperative outcome of teenagers and adults
UOP and possible surgical bleeding. That’s why generous IV fluid with congenital heart disease. J Cardiothorac Vasc Anesth 16: 731-736.
resuscitation to more than normal filling of the heart, slow titration of
J Anesth Clin Res, an open access journal Volume 8 • Issue 4 • 1000716
ISSN:2155-6148
Citation: Nezar AZ, Haroun MA, Mounir MA, Hamada MA, Okasha MM (2017) Anesthetic Considerations for Craniopharyngioma Resection in
Pediatric Patient with Fontan Physiology: A Case Report. J Anesth Clin Res 8: 716. doi:10.4172/2155-6148.1000716
Page 5 of 5
21. Lovell AT (2004) Anaesthetic implications of grown-up congenital heart rocuronium, vecuronium, mivacurium, atracurium and tubocurarine. Br
disease. Br J Anaesth 93: 129-139. J Anaesth 75: 588- 592.
22. Naguib M, Samarkandi AH, Bakhamees HS, Magboul MA, el-Bakry AK 23. Redington AN, Penny D, Shinebourne EA (1991) Pulmonary blood flow
(1995) Histamine-release haemodynamic changes produced by after total cavopulmonary shunt. Br Heart J 65: 213-217.
J Anesth Clin Res, an open access journal Volume 8 • Issue 4 • 1000716
ISSN:2155-6148
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Basic Brain Anatomy and Physiology PDFDocument10 pagesBasic Brain Anatomy and Physiology PDFSenthilkumar Thiyagarajan100% (3)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Short Notes: Melaka Trauma Life SupportDocument104 pagesShort Notes: Melaka Trauma Life SupportSebastian KohNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- VanPutte Seeleys Essentials 11e Chap07 PPT AccessibleDocument109 pagesVanPutte Seeleys Essentials 11e Chap07 PPT AccessibleYhel Trinidad50% (2)
- Algorithm-ACLS Expanded Systematic Approach 200623Document1 pageAlgorithm-ACLS Expanded Systematic Approach 200623Kavya Shree100% (1)
- Craniopharyngioma-The Anesthetic, Critical Care and Syrgical Challenges in The Managemnet of CPNDocument5 pagesCraniopharyngioma-The Anesthetic, Critical Care and Syrgical Challenges in The Managemnet of CPNpitriaNo ratings yet
- Breathing Exercise Effective CoughDocument52 pagesBreathing Exercise Effective CoughDesy Suryani Pais100% (1)
- CHF NCPDocument8 pagesCHF NCPZy Hallasgo100% (1)
- Varicose Veins CaseDocument16 pagesVaricose Veins Casebenak shivalingappaNo ratings yet
- Complete Heart BlockDocument59 pagesComplete Heart BlockJoan Rae Tan71% (7)
- Medicine IM Platinum-1Document357 pagesMedicine IM Platinum-1Bom Tna67% (3)
- Balasubramanian, Mendonca, Pinnock - The Structured Oral Examination in Anaesthesia 2006 PDFDocument277 pagesBalasubramanian, Mendonca, Pinnock - The Structured Oral Examination in Anaesthesia 2006 PDFGold4allNo ratings yet
- Ultrasound-Guided Peripheral Nerve Blocks of The Upper LimbDocument6 pagesUltrasound-Guided Peripheral Nerve Blocks of The Upper LimbpitriaNo ratings yet
- Nerve Injury After Peripheral Nerve Blockade-Current Understanding and GuidelinesDocument7 pagesNerve Injury After Peripheral Nerve Blockade-Current Understanding and GuidelinespitriaNo ratings yet
- Fascia Iliaca Compartment BlockDocument7 pagesFascia Iliaca Compartment BlockpitriaNo ratings yet
- Perineural Adjuncts For Peripheral Nerve BlockDocument7 pagesPerineural Adjuncts For Peripheral Nerve BlockpitriaNo ratings yet
- Regional Anesthesia and OutcomesDocument5 pagesRegional Anesthesia and OutcomespitriaNo ratings yet
- Challenges, Solutions, and Advances in Ultrasound-Guided Regional AnesthesiaDocument7 pagesChallenges, Solutions, and Advances in Ultrasound-Guided Regional AnesthesiapitriaNo ratings yet
- Abdominal Wall Blocks For Intra-Abdominal SurgeryDocument6 pagesAbdominal Wall Blocks For Intra-Abdominal SurgerypitriaNo ratings yet
- WFSA Craniopharyngioma Resection PDFDocument5 pagesWFSA Craniopharyngioma Resection PDFpitriaNo ratings yet
- Current State of Noninvasive, Continuous.12 PDFDocument7 pagesCurrent State of Noninvasive, Continuous.12 PDFFIA SlotNo ratings yet
- Basic of Nursing Skill SleepDocument18 pagesBasic of Nursing Skill SleepAnnisa Danni KartikaNo ratings yet
- Selina Concise Biology Class 7 ICSE Solutions For Chapter 4 - Photosynthesis and RespirationDocument8 pagesSelina Concise Biology Class 7 ICSE Solutions For Chapter 4 - Photosynthesis and RespirationArijit SahaNo ratings yet
- Fluid and Electrolytes (Acid Base)Document31 pagesFluid and Electrolytes (Acid Base)Diana TahamidNo ratings yet
- M.SC Questions PaperDocument2 pagesM.SC Questions Paperkhela Ram SorenNo ratings yet
- Sex As A Way To Lose WeightDocument7 pagesSex As A Way To Lose WeightMunther MurjanNo ratings yet
- Electrocardiographic Changes During Acute Mental StressDocument4 pagesElectrocardiographic Changes During Acute Mental StressVeronica JanethNo ratings yet
- Organization of The Human BodyDocument6 pagesOrganization of The Human BodySharmaine DurangoNo ratings yet
- Acute Ischemic Heart DiseaseDocument27 pagesAcute Ischemic Heart DiseaseJaymee CachoNo ratings yet
- Artigo SeminarioDocument7 pagesArtigo SeminarioJairo Sá SousaNo ratings yet
- 10.4 Homeostasis-1Document10 pages10.4 Homeostasis-1صالح ابراهيمNo ratings yet
- Ateneo de Zamboanga University: Case Study (HOSPITAL)Document7 pagesAteneo de Zamboanga University: Case Study (HOSPITAL)Lyka SaysonNo ratings yet
- Anatomy and PhysiologyDocument23 pagesAnatomy and PhysiologyRusca De MedikoNo ratings yet
- Case Study of Atherosclerosis 1. Risk Factors of AtherosclerosisDocument5 pagesCase Study of Atherosclerosis 1. Risk Factors of AtherosclerosisCarly Beth Caparida LangerasNo ratings yet
- Test Thesis 2 10Document36 pagesTest Thesis 2 10adam yassineNo ratings yet
- Aortic and Pulmonary Valve DiseaseDocument2 pagesAortic and Pulmonary Valve DiseaseKaja MatovinovicNo ratings yet
- Respiratory SystemDocument24 pagesRespiratory SystemRhod Jayson RicaldeNo ratings yet
- Regulasi Dan Mekanisme EndokrinDocument121 pagesRegulasi Dan Mekanisme Endokrinluthfiyya syafiqaNo ratings yet
- Dr. Ken Wirastuti, Mkes, SP.S Bagian Ilmu Penyakit Saraf Fakultas Kedokteran-Universitas Islam Sultan AgungDocument20 pagesDr. Ken Wirastuti, Mkes, SP.S Bagian Ilmu Penyakit Saraf Fakultas Kedokteran-Universitas Islam Sultan AgungmarkoyenNo ratings yet
- Synaptic Signalling PDFDocument8 pagesSynaptic Signalling PDFHyunji KimNo ratings yet