Professional Documents
Culture Documents
Beyond Evidence The Moral Case For International M
Uploaded by
Chinaza AjuonumaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Beyond Evidence The Moral Case For International M
Uploaded by
Chinaza AjuonumaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/6908268
Beyond Evidence: The Moral Case for International Mental Health
Article in American Journal of Psychiatry · September 2006
DOI: 10.1176/appi.ajp.163.8.1312 · Source: PubMed
CITATIONS READS
96 199
3 authors:
Vipin Patel Benedetto Saraceno
Indian Institute of Science Universidade NOVA de Lisboa
105 PUBLICATIONS 16,933 CITATIONS 167 PUBLICATIONS 7,446 CITATIONS
SEE PROFILE SEE PROFILE
Arthur Kleinman
Harvard University
103 PUBLICATIONS 14,428 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Patient-Physician Trust in China View project
Biostatistics View project
All content following this page was uploaded by Benedetto Saraceno on 18 April 2016.
The user has requested enhancement of the downloaded file.
Editorial
Beyond Evidence: The Moral Case
for International Mental Health
T he global burden of disease attributable to mental, neurological, and substance use
disorders is expected to rise from 12.3% in 2000 to 14.7% in 2020 (1). This rise will be
particularly sharp in developing countries. Research has documented the socioeco-
nomic determinants of many disorders, the profound impact on the lives of those af-
fected and their families, and the lack of appropriate care in developing countries. The
enormous gap between mental health needs and the services in developing countries
has been documented in international reports, culminating in the World Health Report
2001 (2). This evidence has increased the profile of international mental health, but ac-
tion still remains limited. With every new public health challenge, mental health is once
more relegated to the background. We argue that moral arguments are just as important
as evidence to make the case for mental health in-
tervention. At the center of these moral arguments
“The overwhelming is the need to reclaim the place of mental health at
majority of the 400 the heart of international public health. We consider
million persons with some moral arguments for international mental
health and an example from another area of public
mental disorders health in which the moral case was an important
globally are not being enough argument for making policy changes and
implementing interventions.
provided with…basic
No health without mental health. Mental health
mental health care.” is closely linked with virtually all global public health
priorities. Alcohol abuse is a major risk factor for un-
safe sexual behavior, and persons with human im-
munodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) have high
rates of cognitive impairment and depression (3). Stress and anxiety predispose to myo-
cardial infarction, and the latter leads to higher rates of depression (4). Maternal depres-
sion is associated with childhood failure to thrive in developing countries; failure to thrive
can lead to developmental delays and psychiatric problems in later life (5). Alcohol abuse
and personality disorder frequently precede violence and depression, and suicide fre-
quently follows (6). The moral case is that there is no health without mental health. Men-
tal health interventions must be tied to any program dealing with physical health.
Mental disorders are treatable in developing countries. Clinical trials have dem-
onstrated the efficacy and cost-effectiveness of locally feasible treatments for depres-
sion, schizophrenia, and substance abuse in developing countries (7–9). All these studies
share one finding: mental illnesses can be treated with cheap and technically simple
treatments. The work of committed grassroots organizations demonstrates how this sec-
tor has been implementing mental health interventions at low cost (10). The moral case
is that it is unethical to deny effective, acceptable, and affordable treatment to millions
of persons suffering from treatable disorders. Community and primary care treatment
programs must be generously supported by donor agencies.
Paying for new psychiatric drugs. Many developing countries were able to produce
generic versions of drugs because of a less rigid enforcement of international patent
regulation. Since a substantial proportion of drug costs are met out of pocket, this al-
lowed newer medications to be accessible to low-income groups. This situation was
changed with the enforcement of the Trade Related Intellectual Property Rights inter-
national agreement in 2005. The agreement dictates that any drug patented after 2005
1312 ajp.psychiatryonline.org Am J Psychiatry 163:8, August 2006
EDITORIAL
will not be available except at the price set by the company that holds the patent (11).
Governments can exempt diseases that are life-threatening or national emergencies
from the Trade Related Intellectual Property Rights charter. Mental illness does not fig-
ure as an exemption category. The moral case is that the mentally ill have a right to ac-
cess affordable, evidence-based treatments. Mental illnesses must be excluded from the
Trade Related Intellectual Property Rights charter.
Reversing the brain drain. The most startling finding of the World Health Organi-
zation Atlas report is the impossibly enormous inequity in the distribution of mental
health manpower in the world (12). A tiny fraction of this manpower resides in regions
of the world where over 90% of the global population lives. Despite this glaring ineq-
uity, the demand for specialists in richer countries only grows, worsening the brain-
drain of mental health resources from developing countries. The vast majority of these
professionals have been trained in publically funded medical schools. The moral case
is that the people of poor countries should not be paying for the mental health care of
those living in the richer world. There needs to be an acknowledgment that institutions
in developed countries have an ethical obligation to facilitate the return of profession-
als and to foster long-term partnerships with developing countries to build mental
health capacity.
Violating human rights. There is a history of human rights violations of persons with
mental disorders across the world, but today the most disturbing examples are found in
developing countries. The Asia edition of the newsmagazine Time from Nov. 24, 2003,
detailed contemporary accounts of the lives of people living in mental hospitals in
Southeast Asia. Patients, typically long-term residents, lose contact with their families,
rarely see a mental health professional, are treated with old drugs with severe side ef-
fects, are offered few rehabilitative therapies, are kept in crowded wards with no hint of
dignity, and are given unmodified electroconvulsive therapy. The Erwadi tragedy in In-
dia in 2001, where over 20 persons with mental illness were burned to death when a fire
swept the healing temple where they were chained to their beds, reminds us of human
rights abuses that take place under the guise of traditional medicine. The stigma of
mental illness is so great that the mentally ill are unable to gain employment, finish
schooling, marry, live independently, or have their care paid for by insurance compa-
nies. The moral case is that the rights of the mentally ill continue to be denied by many
sectors in society. We need to provide technical and financial support for hospitals to re-
form, to enable the development of community care programs, to raise mental health
literacy in the community and among health workers, and to ensure that basic rights are
monitored and enforced.
Social change and mental health. Most developing countries are witnessing social
and economic changes at a pace that is unparalleled in history. Not everyone has bene-
fited from these changes. Economic change is coupled with migration from rural to ur-
ban areas, disrupting social networks and household economies. The decrease of trade
barriers reducing costs of consumer items is coupled with cheap imports, leading to un-
employment of small-scale entrepreneurs and farmers. The reduction in state budgets
is being most acutely felt in social spending, where they are most needed. The rising
tide of suicides and premature mortality in some countries, as vividly seen in the alco-
hol-related deaths of men in Eastern Europe and the suicides of farmers in India, indig-
enous peoples in South America, and young women in rural areas in China, can be at
least in part linked to rapid economic and social change (13, 14). The moral case is that
mental health problems are not a luxury item on the health agenda of the poor and mar-
ginalized. Mental disorders must be included in programs directed to promoting the
health of the poor and mental health indicators used to evaluate the larger social im-
pact of globalization.
The overwhelming majority of the 400 million persons with mental disorders globally
are not being provided with even the basic mental health care that we know they should
Am J Psychiatry 163:8, August 2006 ajp.psychiatryonline.org 1313
EDITORIAL
and can receive. Research evidence will not reduce this inequity. To make a change, the
moral case must be heard.
Consider the moral argument that persons with HIV/AIDS in developing countries
had the right to access antiretroviral drugs, that the state had to provide them for free,
that drug companies had to reduce their prices, that apparently complex treatment reg-
imens could be provided by primary health care providers with appropriate training
and support, that discrimination against people with HIV/AIDS had to be combated
vigorously, and that knowledge about HIV/AIDS was the most powerful tool to combat
stigma. These arguments were moral and human rights based. The arguments were
made by a coalition of academics, community leaders, people living with HIV/AIDS,
rock stars, and public heroes. The case they made was so compelling that governments
from India to South Africa changed their policy on antiretroviral drugs. Drug companies
agreed to reduce prices of medicines. The World Health Organization decided on 3×5 as
their lead initiative, aiming to get antiretroviral drugs to 3 million people by 2005.
We believe that the time is ripe for such a global mental health advocacy initiative that
makes the moral case for the mentally ill. It is unacceptable to continue business as
usual. Borrowing from the lessons of our colleagues in other areas of public health, such
an initiative could take the form of a Global Alliance for Mental Health, under the um-
brella of the World Health Organization, in which mental health professionals work
alongside patients, families, and public health groups. The practical design of policies,
programs, and interventions is most likely to be effective when articulated with a moral
orientation toward sufferers of mental illnesses. The Alliance’s primary goal would be to
spearhead a movement to increase access to evidence-based care, perhaps a 5×10 pro-
gram to get 5 million untreated patients into treatment and rehabilitation programs by
2010. Equally important goals would be to combat stigma through concerted cam-
paigns directed at various sectors of society and to strengthen the capacity of health
systems to care for the mentally ill. A key task would be to mobilize the massive re-
sources needed to support mental health program development in poor countries.
Mental health professionals in rich countries have an important role to play. They can
be advocates to their own health systems to ensure that the moral case is heard and ap-
propriate actions supported. As individuals, they can commit their time to activities
that tackle some of the issues on the international mental health agenda. We believe
that our ultimate professional goal as mental health professionals in a globalized world
is to secure a reasonable opportunity for people with mental disorders to achieve better
health outcomes. We already have the evidence we need to make the case for interna-
tional mental health; it is the moral argument that we now need to make.
References
1. Murray CJL, Lopez AD: Alternative projections of mortality and disability by cause 1990–2020: global burden
of disease study. Lancet 1997; 349:1498–1504
2. World Health Organization: The World Health Report 2001: Mental Health: New Understanding, New Hope.
Geneva, WHO, 2001
3. Catalan J (ed): Mental Health and HIV Infection. Psychological and Psychiatric Aspects. London, Taylor &
Francis, 1999
4. Penninx BWJH, Beekman AT, Honig A, Deeg DJH, Schoevers RA, van Eijk JTM, van Tilburg W: Depression and
cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry 2001; 58:227
5. Patel V, Rahman A, Jacob KS, Hughes M: Effect of maternal mental health on infant growth in low income
countries: new evidence from South Asia. BMJ 2004; 328:820–823
6. World Health Organization: World Report on Violence and Health: Summary. Geneva, WHO, 2002
7. Chatterjee S, Patel V, Chatterjee A, Weiss H: Evaluation of a community based rehabilitation model for
chronic schizophrenia in a rural region of India. Br J Psychiatry 2003; 182:57–62
8. Patel V, Araya R, Bolton P: Treating depression in developing countries. Trop Med Int Health 2004; 9:539–
541
9. Wu Z, Detels R, Zhang J, Li V, Li J: Community-based trial to prevent drug use amongst youth in Yunnan,
China. Am J Public Health 2002; 92:1952–1957
10. Patel V, Thara R: Meeting Mental Health Needs in Developing Countries: NGO Innovations in India. New
Delhi, Sage Publications, 2003
1314 ajp.psychiatryonline.org Am J Psychiatry 163:8, August 2006
EDITORIAL
11. Patel V, Andrade C: Pharmacological treatment of severe psychiatric disorders in the developing world: les-
sons from India. CNS Drugs 2003; 17:1071–1080
12. World Health Organization: Atlas Country Profiles of Mental Health Resources. Geneva, WHO, 2001
13. Sundar M: Suicide in farmers in India. Br J Psychiatry 1999; 175:585–586
14. Phillips MR, Liu H, Zhang Y: Suicide and social change in China. Cult Med Psychiatry 1999; 23:25–50
VIKRAM PATEL, PH.D.
BENEDETTO SARACENO, M.D.
ARTHUR KLEINMAN, M.D.
Address correspondence and reprint requests to Dr. Patel, Sangath Centre, Alto-Porvorim, Goa India 403521;
vikram.patel@lshtm.ac.uk (e-mail).
Drs. Patel, Saraceno, and Kleinman report no conflict of interest.
Clinical Views You Can Use
Have you seen our new feature? This year the Journal debuted “Treat-
ment in Psychiatry,” a regular feature that begins with a hypothetical case
illustrating a problem in current clinical practice. The authors review cur-
rent data on prevalence, diagnosis, pathophysiology, and treatment. The
article concludes with the authors’ treatment recommendations for cases
like the one presented.
Since January, the Journal has provided expert opinions on the follow-
ing cases:
January: Borderline Personality Disorder and Suicidality
February: New-Onset Bipolar Disorder in Late Life: A Case of
Mistaken Identity
March: The Schizophrenia Prodrome
April: Posttraumatic Stress Disorder Among Military Returnees
From Afghanistan and Iraq
May: Hallucinations in Children and Adolescents:
Considerations in the Emergency Setting
June: The Importance of Routine for Preventing Recurrence
in Bipolar Disorder
July: Psychotic and Manic-like Symptoms During Stimulant
Treatment of Attention Deficit Hyperactivity Disorder
This month’s Treatment in Psychiatry is on Antidepressants and Bipo-
lar Disorder and can be found on p. 1337
Am J Psychiatry 163:8, August 2006 ajp.psychiatryonline.org 1315
View publication stats
You might also like
- Mental Health Class NotesDocument3 pagesMental Health Class Notessuz100% (4)
- Position PaperDocument14 pagesPosition Paperantonette gammaru100% (1)
- Academic Self-HandicappingDocument1 pageAcademic Self-HandicappingAlexis Autor SuacilloNo ratings yet
- Challenges and Priorities For Global Mental Health Research in LMICDocument24 pagesChallenges and Priorities For Global Mental Health Research in LMICKelvin TungNo ratings yet
- hsc.12749 - Are Mental Health Tribunals Operating in Accordance With International Human Rights StandardsDocument20 pageshsc.12749 - Are Mental Health Tribunals Operating in Accordance With International Human Rights StandardsAdrian WhyattNo ratings yet
- Mental Health Key to Sustainable DevelopmentDocument32 pagesMental Health Key to Sustainable Developmentfionakumaricampbell6631No ratings yet
- Empowering People For Mental Health - A Literature ReviewDocument3 pagesEmpowering People For Mental Health - A Literature ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- WISH Mental Health ReportDocument52 pagesWISH Mental Health ReportMatías ArgüelloNo ratings yet
- AlzheimersDementia 2021Document13 pagesAlzheimersDementia 2021TheawakenedmindsNo ratings yet
- Global Mental HealthDocument4 pagesGlobal Mental HealthFIRDA NURSANTINo ratings yet
- Social Determinants of Mental Health Full ReportDocument55 pagesSocial Determinants of Mental Health Full ReportneetiprakashNo ratings yet
- Mental Health StudyDocument4 pagesMental Health StudyKrishna SapkotaNo ratings yet
- Eugenics as a Factor in the Prevention of Mental DiseaseFrom EverandEugenics as a Factor in the Prevention of Mental DiseaseNo ratings yet
- Disparities in Knowledge, Attitude and Practices On Mental Health Among Healthcare Workers and Community Members in Meru County, KenyaDocument22 pagesDisparities in Knowledge, Attitude and Practices On Mental Health Among Healthcare Workers and Community Members in Meru County, KenyaMuhammad IdrisNo ratings yet
- PIIS0140673607612434Document1 pagePIIS0140673607612434api-26621755No ratings yet
- 3 Editorial BDocument2 pages3 Editorial BmirleinnomineNo ratings yet
- Surgeon General Mental Health Report - 1999 - DCF PDFDocument494 pagesSurgeon General Mental Health Report - 1999 - DCF PDFatjoeross100% (2)
- World Mental Health Day - 2022Document17 pagesWorld Mental Health Day - 2022TesitaNo ratings yet
- 0010 Pre FinalDocument246 pages0010 Pre FinalDanielle Kiara ZarzosoNo ratings yet
- Social Determinants Mental HealthDocument54 pagesSocial Determinants Mental HealthSánchez JenniferNo ratings yet
- Lay CounselorDocument12 pagesLay Counselornurul cahya widyaningrumNo ratings yet
- Mental Health IndustryDocument11 pagesMental Health Industryjordan gallowayNo ratings yet
- CENA C2.editedDocument21 pagesCENA C2.editedEllen Gonzalvo-CabutihanNo ratings yet
- Mental Health Crisis in PakistanDocument2 pagesMental Health Crisis in PakistanUmair Pervaiz GillNo ratings yet
- Scaling-Up Mental Health ServicesDocument12 pagesScaling-Up Mental Health ServicesPierre LaPaditeNo ratings yet
- Read Et Al 2009 PDFDocument16 pagesRead Et Al 2009 PDFJana ChihaiNo ratings yet
- Mental illness overview and plansDocument15 pagesMental illness overview and plansbeibhydNo ratings yet
- 1992 Impotence 091 PDFDocument37 pages1992 Impotence 091 PDFm faisalNo ratings yet
- Future of MHDocument2 pagesFuture of MHAmitranjan BasuNo ratings yet
- Psychedelic Science Contemplative Practices and Indigenous and Other Traditional Knowledge Systems Towards Integrative Community-Based Approaches IDocument17 pagesPsychedelic Science Contemplative Practices and Indigenous and Other Traditional Knowledge Systems Towards Integrative Community-Based Approaches IMariana CNo ratings yet
- Research Paper Mental DisordersDocument8 pagesResearch Paper Mental Disordersfvhdgaqt100% (1)
- Mental Health Report Vol I 10 06 2016 PDFDocument190 pagesMental Health Report Vol I 10 06 2016 PDFVaishnavi JayakumarNo ratings yet
- Mental Health Care in India: Old Aspirations Renewed HopeDocument973 pagesMental Health Care in India: Old Aspirations Renewed HopeVaishnavi JayakumarNo ratings yet
- Saraceno B Freeman M Funk M. PUBLIC MENTAL HEALTHDocument20 pagesSaraceno B Freeman M Funk M. PUBLIC MENTAL HEALTHenviosmentalmedNo ratings yet
- Ywfbask PDFDocument3 pagesYwfbask PDFqwert ytrewqNo ratings yet
- Zamora CHN ResearchDocument9 pagesZamora CHN ResearchHazelGatuslaoZamoraNo ratings yet
- Research Paper On Mental HealthDocument41 pagesResearch Paper On Mental HealthExample100% (1)
- Eating Disorders The Big IssueDocument3 pagesEating Disorders The Big IssueReztariestyadiNo ratings yet
- Globalising Mental Health: A Neoliberal ProjectDocument7 pagesGlobalising Mental Health: A Neoliberal ProjectlizardocdNo ratings yet
- Intelligence and Personality As PredictorsDocument96 pagesIntelligence and Personality As PredictorsTrifan DamianNo ratings yet
- Human rights in mental healthcare A review of current global situationDocument14 pagesHuman rights in mental healthcare A review of current global situationVanshika OberoiNo ratings yet
- Psychiatrization of Society A Conceptual FrameworkDocument11 pagesPsychiatrization of Society A Conceptual Frameworkcoletivo peripatetikosNo ratings yet
- First Year M.Sc. Nursing, Bapuji College of Nursing, Davangere - 4, KarnatakaDocument14 pagesFirst Year M.Sc. Nursing, Bapuji College of Nursing, Davangere - 4, KarnatakaAbirajanNo ratings yet
- Family Mental Health NursingDocument21 pagesFamily Mental Health Nursinghyunra kimNo ratings yet
- Mental Health HealthDocument6 pagesMental Health Healthsarahjehad12345No ratings yet
- Is Borderline Personality Disorder A Serious Mental Illness?Document7 pagesIs Borderline Personality Disorder A Serious Mental Illness?Carolina ValenciaNo ratings yet
- Mental Heath AFRDocument16 pagesMental Heath AFRthursday8893No ratings yet
- Documen 2 TDocument11 pagesDocumen 2 TRhodius NogueraNo ratings yet
- Farmer-Scope For Global HealthDocument2 pagesFarmer-Scope For Global HealthMauricio López-RuizNo ratings yet
- LEXICON International Media Guide For Mental Health - FINAL - LexiconDocument16 pagesLEXICON International Media Guide For Mental Health - FINAL - LexiconVaishnavi JayakumarNo ratings yet
- Mhn-Issues, Trends, Magnitude, Contemporary Practice HealthDocument15 pagesMhn-Issues, Trends, Magnitude, Contemporary Practice HealthAna MikaNo ratings yet
- Challenges of managing mental health in the UAEDocument6 pagesChallenges of managing mental health in the UAEReem AlkaabiNo ratings yet
- Developing Counseling Skills For HealthcareDocument165 pagesDeveloping Counseling Skills For HealthcareHemn HawleryNo ratings yet
- Research Paper On Mental Health in IndiaDocument4 pagesResearch Paper On Mental Health in Indiaqzetcsuhf100% (1)
- Vacarolis Chapter OutlinesDocument181 pagesVacarolis Chapter Outlinesamashriqi100% (1)
- Mental Health and Sensing: October 2020Document17 pagesMental Health and Sensing: October 2020Ahmed AliNo ratings yet
- Pilot StudyDocument6 pagesPilot StudyStanley Yakic BasaweNo ratings yet
- Argumentative Essay Final DraftDocument11 pagesArgumentative Essay Final Draftapi-624112595No ratings yet
- Guideline MinimunDocument14 pagesGuideline MinimunsofinoyaNo ratings yet
- Bab IDocument20 pagesBab IbadrulNo ratings yet
- Mental Health in IndiaDocument6 pagesMental Health in IndiaStarlin MythriNo ratings yet
- RD TIPS - 10 Choose Ans From A ListDocument2 pagesRD TIPS - 10 Choose Ans From A ListJess NguyenNo ratings yet
- 1 01 Foodborne IllnessDocument28 pages1 01 Foodborne Illnessapi-329321140No ratings yet
- National Guideline On Integrated Vector Management 2020 NewDocument140 pagesNational Guideline On Integrated Vector Management 2020 NewNeha AmatyaNo ratings yet
- SOFA Score: What It Is and How To Use It in TriageDocument4 pagesSOFA Score: What It Is and How To Use It in TriageDr. rohith JaiswalNo ratings yet
- Overview of Public Health NursingDocument6 pagesOverview of Public Health NursingMariah Jane TaladuaNo ratings yet
- Personality Psychology Domains of Knowledge About Human Nature 5th Edition Larsen Solutions ManualDocument17 pagesPersonality Psychology Domains of Knowledge About Human Nature 5th Edition Larsen Solutions Manualcivilianpopulacy37ybzi100% (28)
- Feed Addditives NEW ANN 211Document44 pagesFeed Addditives NEW ANN 211Mohit BhardwajNo ratings yet
- Lit Ing 060523Document6 pagesLit Ing 060523gloriussihombing18No ratings yet
- 10 - Chapter 2Document13 pages10 - Chapter 2Rukhsana HabibNo ratings yet
- Saadat Hasan Manto, Partition, and Mental Illness Through The Lens of Toba Tek SinghDocument6 pagesSaadat Hasan Manto, Partition, and Mental Illness Through The Lens of Toba Tek SinghIrfan BalochNo ratings yet
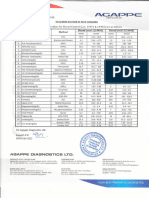
- Agappe Diagnostics Control ValuesDocument1 pageAgappe Diagnostics Control ValuesDinil KannurNo ratings yet
- Nursing Care Plan for Risk of Bleeding During PregnancyDocument4 pagesNursing Care Plan for Risk of Bleeding During PregnancybananakyuNo ratings yet
- Include Invest: InnovateDocument28 pagesInclude Invest: InnovateAstrisa FaadhilahNo ratings yet
- Instant Download Discovering Psychology 7th Edition Ebook PDF PDF ScribdDocument41 pagesInstant Download Discovering Psychology 7th Edition Ebook PDF PDF Scribdjeana.gomez838100% (39)
- Diagnosis and Management of Dyslipidemia in Family PracticeDocument41 pagesDiagnosis and Management of Dyslipidemia in Family PracticeKai ChuaNo ratings yet
- Group 3-Kaposi SarcomaDocument25 pagesGroup 3-Kaposi SarcomaShiangNo ratings yet
- Occupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesMathea Cohen0% (1)
- Krok Review: How To Prepare Krok TestDocument84 pagesKrok Review: How To Prepare Krok Testgaurav100% (2)
- Kent's RepertoryDocument89 pagesKent's RepertoryDrx Rustom AliNo ratings yet
- INFECTION Control and PREVENTION-1Document49 pagesINFECTION Control and PREVENTION-1Jerry AbleNo ratings yet
- Milpersman 1910-402Document1 pageMilpersman 1910-402benpickensNo ratings yet
- FSRH Ukmec Summary September 2019Document11 pagesFSRH Ukmec Summary September 2019Kiran JayaprakashNo ratings yet
- PharmacokineticsDocument95 pagesPharmacokineticsSonalee ShahNo ratings yet
- 111 Predatory UGC's Revised White List Has 111 More Predatory Journals - Science ChronicleDocument31 pages111 Predatory UGC's Revised White List Has 111 More Predatory Journals - Science ChronicleP meruguNo ratings yet
- Pahade Et Al 2021 Indian (Marathi) Version of The Shoulder Pain and Disability Index (Spadi) TranslatioDocument8 pagesPahade Et Al 2021 Indian (Marathi) Version of The Shoulder Pain and Disability Index (Spadi) TranslatioAnnisa Assyifa YustianNo ratings yet
- Vital Signs - Measurements of Basic Body FunctionsDocument27 pagesVital Signs - Measurements of Basic Body FunctionsJames Paulo AbandoNo ratings yet
- Coida Service Book Version 23Document53 pagesCoida Service Book Version 23Lesedi ModibaneNo ratings yet
- Nutrients: Nutrition and Rheumatoid Arthritis in The Omics' EraDocument23 pagesNutrients: Nutrition and Rheumatoid Arthritis in The Omics' EraMikhael FeliksNo ratings yet
- Hepatitis B OverviewDocument11 pagesHepatitis B OverviewJose RonquilloNo ratings yet