Professional Documents
Culture Documents
Applications of CRISPRCas9 Technology in The Treatment of Lung Cancer
Uploaded by
Tharun VasuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Applications of CRISPRCas9 Technology in The Treatment of Lung Cancer
Uploaded by
Tharun VasuCopyright:
Available Formats
TRMOME 1479 No.
of Pages 11
Trends in Molecular Medicine
Review
Applications of CRISPR/Cas9 Technology in
the Treatment of Lung Cancer
Chunyang Jiang ,1,4,* Xiaohui Lin,2,4 and Zhigang Zhao3,*
Since its emergence, the application of CRISPR-associated nuclease 9 (Cas9) Highlights
technology in cancer research has accelerated studies to investigate many as- CRISPR/Cas9-mediated gene editing of
pects of treatment approaches for lung cancer, including the identification of tar- proto-oncogenes or tumor-suppressor
genes offers great potential as a treat-
get genes, construction of animal tumor models, and identification of drug
ment for lung cancer.
resistance-related genes. Moreover, CRISPR/Cas9 can be used in gene therapy
for lung cancer, specifically involving molecular targeted drugs and inhibitors. Drug resistance to chemotherapy is the
This article reviews the current landscape of CRISPR/Cas9 applications for main reason for the poor efficacy of cur-
rent treatments for patients with lung
lung cancer treatment as a basis for further studies. Given its promising perfor- cancer. CRISPR/Cas9 gene editing
mance, in-depth and systematic research on the application of CRISPR/Cas9 technology can be used to evaluate
in lung cancer treatment will be necessary in future studies for its successful im- genes targeted by chemotherapeutic
plementation in clinical practice. drugs and to identify new pathways to
reduce or eliminate resistance to chemo-
therapy in lung cancer.
Lung Cancer Treatment Strategies Using Gene Editing Technologies
Lung cancer is the most common malignancy worldwide. Morbidity and mortality due to lung can- Targeted drug therapy, which involves
several genes such as EGFR, ALK, and
cer rank first among malignant tumors in developed and developing countries including China, the
KRAS, has become an important ap-
USA, and Europe [1,2]. The development of lung cancer involves multiple genes and signaling path- proach in lung cancer treatment. How-
ways [3], and treatment of lung cancer has been the focus of intense clinical research. Cancer gene ever, drug resistance is a growing
therapy (see Glossary) refers to treatment involving active gene changes [4]. Genome repair of lung concern. CRISPR/Cas9 can lower the
resistance of tumors to these molecular
cancer cells and silencing the expression of specific proteins have become popular approaches to targeted drugs or inhibitors by editing re-
study and treat lung cancer. In recent years, the application of gene editing technologies such as lated genes, which will benefit patients
the Cas9 system has attracted increasing attention, and these have been investigated for research with lung cancer.
and treatment of cancer, including lung cancer [5,6]. CRISPR/Cas9 is a robust tool for effectively
editing the genome of a cell. Single-guide RNA (sgRNA)-directed Cas9 activity causes DNA cleav-
age at specific sites, allowing DNA editing at these sites by subsequent DNA repair in mammalian
1
Department of Thoracic Surgery, Tianjin
cells [7]. Compared with the more traditional gene editing techniques such as zinc-finger endonu-
Union Medical Center, 190 Jieyuan
cleases (ZFNs) [8] and transcription activator-like effector nucleases (TALENs) [9], CRISPR/Cas9 Road, Hongqiao District, Tianjin 300121,
gene editing technology is simple and accurate, and can be targeted to edit any gene. The main People’s Republic of China
2
Department of Physics and Chemistry,
differences between CRISPR/Cas9, ZFN, and TALEN are summarized in Table 1 [10–15].
Tianjin Centres for Disease Control and
Prevention, Tianjin 300011, People’s
A personalized system of cell- and animal-based experiments can be established to comprehen- Republic of China
3
Department of Hematology and
sively analyze lung cancer in individual patients using the CRISPR/Cas9 technique, and
Oncology, Tianjin Medical University
genotype-specific defects can be quickly identified on this platform. This approach can also sim- Cancer Institute and Hospital, National
ulate the treatments administered to the patient to expeditiously reveal the resistance mecha- Clinical Research Center for Cancer, Key
Laboratory of Cancer Prevention and
nisms of specific anticancer drugs and aid in the identification of effective treatment
Therapy, Tianjin 300060, People’s
approaches to permanently correct cancer-related gene mutations. CRISPR/Cas9 can also be Republic of China
4
utilized to genetically engineer immune cells for the development of better immunotherapy op- These authors contributed equally to
this work
tions in cancer [15]. Therefore, CRISPR/Cas9 has fueled progress in cancer research in many di-
rections and has become a favorable gene editing tool for precise cancer treatments.
*Correspondence:
Sequence homology between the DNA target site and the guide sequence within the sgRNA chunyangjiang@126.com (C. Jiang) and
ensures the fidelity of Cas9 target selection [16]. Specifically, substantial effort in studies zzhao01@tmu.edu.cn (Z. Zhao).
Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx https://doi.org/10.1016/j.molmed.2019.07.007 1
© 2019 Elsevier Ltd. All rights reserved.
Trends in Molecular Medicine
using cancer cells expressing Cas9 or sgRNA has led to progress, such as the use of cancer- Glossary
specific promoters and drug-induced sgRNA vector systems, allowing more accurate evalua- δ-Catenin: a neuronal protein that
tion and manipulation of specific target cancer cells versus those with wild-type proto- contains 10 armadillo motifs and binds
oncogenes and healthy cells [17,18]. CRISPR/Cas9 can also be used to repair mutations in to the juxtamembrane segment of
classical cadherins. It has a variety of
proto-oncogenes or to knock out specific genes, which may create opportunities for potential
biological functions and modulates the
treatments in cancer. Many studies have shown that using CRISPR/Cas9 to target oncogenic occurrence and development of tumors.
mutations offers a powerful surgical strategy to disrupt oncogenic mutations in cancer treat- Chimeric antigen receptor T (CAR-T)
ment [17]. This treatment was regarded as a revolutionary cancer therapy and marked a new cells: these cells express a fusion
protein between an antitumor
era [19]. In this article we review recent progress in the utilization of CRISPR/Cas9 for lung can- monoclonal antibody and a T cell
cer treatment including targeting oncogenes and tumor-suppressor genes, genes related to receptor (TCR) signaling domain that
chemotherapy drug resistance, and genes related to therapies using targeted drugs and inhib- promotes the antitumor properties of the
itors with the aim of promoting further preclinical research and the clinical treatment of lung T cell.
EG7-OVA cells: a mouse T lymphocyte
cancer. cell line established in 1988. It was
derived from lymphocyte line EL4 of
Application of CRISPR/Cas9 in Studies on Lung Cancer Therapies C57BL/6(H-2b) mice by transfection
with plasmid pAc-neo-OVA.
Gene therapy changes the genetic material of patients through specific methods. Therapeutic
EGFR tyrosine kinase inhibitors
genes are introduced into target cells of patients by directly targeting specific abnormal genes (EGFR-TKIs): small-molecule
for the purpose of treating disease [20,21]. Tumor gene therapy comprises several approaches inhibitors, such as gefitinib or erlotinib,
including tumor-suppressor gene therapy, antisense gene therapy, drug-sensitive gene therapy, that are specific for mutant forms of
EGFR.
drug-resistant gene therapy, and immune gene therapy, among others [22].
Epidermal growth factor receptor
(EGFR): a member of the EGFR/HER
Lung cancer-related proto-oncogenes include MYC, RAS, ERBB1, ERBB2, ROS1, FOS, JUN, family, the expression product of proto-
RAF1, and SRC, among others [23,24]. Approximately 30% of non-small cell lung cancer oncogene ERBB1/EGFR. Non-small-cell
lung cancer cells with EGFR mutations
(NSCLC) cell lines have RAS gene mutations, and c-ERBB-1 protein is overexpressed in
of are highly responsive to EGFR-TKI.
95% of lung squamous cell carcinomas and 75% of lung adenocarcinomas [25,26]. Tumor- Gene therapy: exogenous normal
suppressor genes associated with lung cancer include TP53, RB, CDKN2A, APH, MCC, APC, genes are introduced into target cells to
and NM23 [27,28]. A study of patients with lung cancer revealed that both tumor-suppressor correct or compensate for diseases
caused by defective and abnormal
gene mutations and oncogene overexpression may be involved in the development of lung genes so as to achieve the purpose of
cancer [29]. In recent years the use of gene editing technologies has been evaluated for the treatment; also includes the application
in vitro treatment of cancers [30]. The application of gene editing technology for the treatment of transgenic technologies and other
of lung cancer has also led to some progress. The concept of applying CRISPR/Cas9 in lung nucleic acid-based techniques.
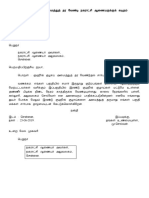
Lewis lung cells: a cell type derived
cancer treatment-related research is briefly summarized in Figure 1. from lung cancer in mice.
miRNAs: a class of noncoding single-
Studies on Oncogenes stranded RNA molecules with a length of
Oncogenes override normal regulatory controls and contribute to the malignant transformation of ~22 nt encoded by endogenous genes;
miRNAs are involved in regulating post-
a cell. Oncogene products can cause eukaryotic cells to grow in an uncontrolled manner, as ob-
transcriptional gene expression.
served in cancer cells. Oncogene addiction of cancer cells, namely inhibition of growth following Off-target effects: treatment effects
the inactivation of a single oncogene in tumor cells, is the theoretical basis of applying CRISPR/ that deviate from a preset target and
Cas9 technology in cancer treatment [31,32]. CRISPR/Cas9 gene editing technology can pre- affect nontarget sites. It is the most
controversial side effect of the CRISPR
cisely recognize DNA sequences and has quickly been implemented to specifically recognize gene-editing technique.
overexpressing or overactivated genes [33]. This approach provides new ideas for the treatment Programmed cell death 1 (PD-1):
of tumors. also known as PDCD1, this protein can
prevent immune cells from producing a
protective immune response. Its ligand
Knockout of target oncogenes which are mutated, overexpressed, or overactivated can be poten- PD-L1 mediates immune escape in
tially therapeutic in cancer. In recent years oncogenes that have been studied in the context of cancer progression.
CRISPR/Cas9 gene editing for the treatment of lung cancer include epidermal growth factor re- PC9 cells: a cell line derived from
human lung cancer. The normal cell
ceptor (EGFR), FAK, NESTIN, RSF1, CTNND2, and IGF1R (summarized in Table 2) [17,34–41].
morphology is epithelioid, and cells
These genes, which have been studied by mutation or overexpression approaches, function as on- display adherent growth.
cogenes to promote the development of lung cancer and enhance the ability of lung cancer cells to Wnt: a key regulatory component of the
invade or metastasize. Wnt signaling pathway. The human
2 Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx
Trends in Molecular Medicine
Using CRISPR/Cas9 knockout of the oncogenic mutant EGFR allele can inhibit the growth and WNT1 gene is located at 12q13; several
other Wnt homologs are also encoded in
proliferation of lung cancer cell lines H1975, A549, and H1650 [17,35], and reduce tumor vol- the genome.
umes in xenograft mice implanted with H1975 or A549 cells [EGFR mutation-specific Cas9 Xenograft mice: mouse models of
reduced tumor size by 81.5% and 78.3% compared with phosphate buffered saline (PBS)- cancer are the most common models in
and Ad/Cas9-treated controls, respectively] [17]. Persistent DNA injury and sensitization to ra- which xenografts of human tumors and
cell lines are grown in mice such as
diotherapy can be detected after knockout of the FAK gene by employing CRISPR/Cas9 in athymic (nude) mice that exhibit very
NSCLC cells with mutant KRAS [36]. Knocking out NESTIN in A549 and H1299 cells can pro- high take rates for xenografts and are
mote apoptosis, inhibit proliferation and colony formation, and suppress cell invasion by ideal hosts for in vivo propagation.
inhibiting epithelial-to-mesenchymal transition [37]. Furthermore, knockout of RSF1 in H460
and H1299 cells leads to cell-cycle arrest in G1 as well as increased apoptosis and decreased
cell migration and proliferation [38]. δ-Catenin acts as an oncogene, promoting malignancy in
lung adenocarcinoma. CRISPR/Cas9 knockout of the CTNND2 gene in Lewis lung cells
and in an established xenograft lung cancer model in C57/B6 mice depleted δ-catenin protein
in cancer cells, and the cells lost their tumorigenic and metastatic ability in vivo via inhibition
of Wnt signaling [39]. IGF1R depletion by CRISPR/Cas9 in HCC827 NSCLC cells reduced
markers of mesenchymal cells and enhanced MET amplification, leading to acquired
resistance to erlotinib, an EGFR tyrosine kinase inhibitor (EGFR-TKI) with higher biological
activity than gefitinib [41]. Overall, current research indicates that CRISPR/Cas9 gene
editing technology for proto-oncogene editing has the potential to develop into a treatment
for lung cancer.
Studies on Tumor-Suppressor Genes
Inactivation of tumor-suppressor genes also plays an important role during tumorigenesis [43,44].
The expression products of tumor-suppressor genes can inhibit cell proliferation, promote cell dif-
ferentiation, inhibit cell migration, and negatively regulate tumor progression [45,46]. Knockout,
mutation, or loss of function of tumor-suppressor genes results in the activation of oncogenes,
leading to tumorigenesis. Some tumor-suppressor genes were identified to be mutated and
expressed at low levels in many cancer types [47]. These tumor-suppressor genes are important
targets for treatment using CRISPR/Cas9 gene editing technology [47]. Through the CRISPR/
Cas9 technology, tumor-suppressor genes can be targeted for repair, and the function and ac-
tivity of tumor-suppressor genes can be restored to inhibit tumorigenesis. CRISPR/Cas9
Table 1. The Main Differences between CRISPR/Cas9, TALEN, and ZFN
Method Principle Characteristics Advantages Limitations Refs
CRISPR/Cas9 Bacterial acquired immune Composed of a Cas9 protein and Low cost; simple Relatively high off-target [10–15]
system; consists of clustered an sgRNA molecule; DNA manufacture and rate
regularly interspaced short endonuclease; lentivirus and operation; quick and
palindromic repeats and Cas adenovirus transmission; targets highly efficient;
proteins endogenous DNA multiple targeted
genomic loci
TALEN Based on transcription Comprises a DNA-binding Highly adaptable; Module assembly and [10,11,14,15]
activator-like effectors (TALEs), domain (TAL repeats) together low cytotoxicity and screening are complex;
pairs of dimeric TALE-based with a cleaving domain (FokI); low off-target effects high cost of use; single
nucleases (TALENs) that introduces double-strand breaks nucleic acid targeting
recognize two adjacent DNA through a FokI dimer; lentivirus site; low import
sequences and adenovirus transmission; efficiency
targets endogenous DNA
ZFN Zinc-finger nucleases, based on Composed of a DNA-binding Highly adaptable; Difficult screening and [10,11,14,15]
a DNA-binding domain from domain and a DNA-cleaving high affinity design; single nucleic
zinc-finger proteins; each unit domain (FokI); zinc-finger acid targeting site;
recognizes nucleotide triplets nucleases; TALENs; adenovirus relatively high off-target
with high specificity transmission; targets rate; most expensive
endogenous DNA
Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx 3
Trends in Molecular Medicine
CRISPR/ Cas9
gene editing
Oncogenes Tumor-suppressor Drug resistance T cells
EGFR, FAK genes genes PD1,
NESTIN, RSF1 GOT1, M FN2 RSF1, ERCC1, NRF2, PDL1
CTNND2, TBX2 KEAP1 Aurora B
M CM 4, SLC2A1 m iR-1304
IGF1R, EP300, CREBBP
CDC20, BIRC5
M ED1, LHX6, SLFN11
IGF1R
KEAP1, M AP2K1, M ET
Em l4Alk fusion gene
Knockout/ Repair/ Enhance drug Restore
inactivation activation sensitivity Immunity
Anti-lung cancer
effect
Trends in Molecular Medicine
Figure 1. Applications of CRISPR/Cas9 in Studies on Lung Cancer Treatment. Studies include targeted
oncogenes, tumor-suppressor genes, drug-resistance genes, and genes related to the tumor immune system.
technology for targeted repair of inactivated tumor-suppressor genes could also play an
important and beneficial role in the treatment of lung cancer. Tumor-suppressor genes currently
being studied using CRISPR/Cas9 approaches are summarized in Table 2 [47–49]. Among
these, one study using CRISPR/Cas9 knockout of Keap1 in a Kras-driven mouse model
of lung adenocarcinoma showed overactivation of Nrf2 and promotion of tumor survival and
growth in mice [48]. Another study confirmed that genetic knockout of the tumor-suppressor
gene mitofusion 2 (MFN2) in the lung cancer cell line A549 promoted survival, increased cell
viability, and promoted cell growth, colony formation, invasion, and metastasis by upregulating
the mTORC2/Akt signaling pathway [47]. Genetic knockout of the tumor-suppressor miR-1304
can increase heme oxygenase-1 (HO-1) expression and promote cell survival and growth [49].
Thus far, few studies have examined tumor-suppressor genes in lung cancer using
the CRISPR/Cas9 gene editing technology, and this should be considered as an important direc-
tion for future research. Repair and activation of silenced tumor-suppressors by employing
CRISPR/Cas9 gene editing has the potential to deliver much-needed hope for lung cancer
treatment.
4 Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx
Trends in Molecular Medicine
Table 2. Gene Editing Studies Using CRISPR/Cas9 for Potential Target Genes in Lung Cancer Treatmenta
Target gene Treated cells or tissues Knockout/other Experimental data after gene editing Function Refs
Mutated H1975 cells and A549 cells; Knockout The killing ability of cancer cells was significantly enhanced and OG [17]
EGFR xenograft mouse model of the tumor volume was reduced in a xenograft mouse model
human lung cancer
CD38 A549 cells; Knockout Inhibition of cell growth, cell invasion, and xenograft tumor growth OG [34]
xenograft in nude mice
Mutated EGFR H1650 cells Genome Reduced cell proliferation OG [35]
(L858R) cleavage
FAK Mutant KRAS NSCLC cells Knockout Persistent DNA injury and sensitization to radiotherapy OG [36]
NESTIN A549 and H1299 cells Knockout Increased apoptosis; reduced proliferation, colony formation and OG [37]
invasion; inhibition of EMT
RSF1 H460 cells and H1299 cells Knockout G1 cell-cycle arrest; increased cell apoptosis; decreased cell OG [38]
migration and proliferation
CTNND2 Lewis lung cells; Knockout Depleted δ-catenin protein; loss of tumorigenic and metastatic OG [39]
xenograft in B6/C57 mice ability of tumor cells in vivo; inhibition of Wnt signaling
TBX2, MCM4, H2009 cells and HCC44 Knockout Knockout of these potential lung cancer-driver genes decreased OG [40]
SLC2A1, CDC20, cells the proliferation of lung cancer cells
BIRC5
IGF1R HCC827 cells Knockout Decreased levels of markers of mesenchymal cells; enhanced OG [41]
intrinsic epithelial signaling
GOT1 A549 cells Knockout Glucose deficiency reduced the viability of GOT1 null cells TS [42]
MFN2 A549 cells Knockout Increased cell activity, colony formation, invasion, and TS [47]
metastasis; upregulation of the mTORC2/Akt signaling pathway
KEAP1 Kras-driven mouse model Knockout Overactivation of Nrf2; promoted Kras-driven LUAD in mice TS [48]
of LUAD
miR-1304 A549 cells Knockout Increased HO-1 expression, cell survival, and growth TS [49]
a
Abbreviations: BIRC5, baculoviral inhibitor of apoptosis repeat-containing 5; EGFR, epidermal growth factor receptor; EMT, epithelial–mesenchymal transition; FAK, focal
adhesion kinase; GOT1, glutamate oxaloacetate transaminase 1; HO-1, hemeoxygenase 1; IGF-1R, insulin-like growth factor 1 receptor; LUAD, lung adenocarcinoma;
MFN2, mitofusin 2; NRF2, nuclear factor-erythroid 2 p45-related factor 2; NSCLC, non-small cell lung cancer; OG, oncogene; RSF-1 (HBXAP), remodeling and spacing
factor 1; TS, tumor-suppressor.
Studies on Chemotherapy Resistance-Related Genes
Chemotherapy aims to prevent cancer cell proliferation, invasion, and metastasis, and eventually
induce cancer cell death as a systemic treatment used alone or in combination with surgery and
radiotherapy. Currently, drug resistance to chemotherapy has become a major underlying cause
for the poor efficacy of chemotherapeutic approaches in malignant tumors and for uncontrolled
progression of disease during treatment. Editing drug-resistance genes can improve the sensitiv-
ity of malignant tumor cells to chemotherapeutics, thereby improving chemotherapeutic efficacy
and curative effects [50].
At present, CRISPR/Cas9 has been used to study genes related to sensitization and drug resis-
tance to lung cancer chemotherapeutics such as cisplatin, carboplatin, and paclitaxel (summa-
rized in Table 3) [38,51–53], providing a theoretical basis for improving the therapeutic efficacy
of chemotherapy in lung cancer. In H460 and H1299 cells, knockout of the RSF1 gene in combi-
nation with paclitaxel resulted in cell-cycle arrest in G1, increased apoptosis, and reduced cell mi-
gration and proliferation [38]. In the xenograft mouse model of lung cancer using H460 cells,
compared with wild-type controls, knockout of RSF1 significantly increased sensitivity to pacli-
taxel and reduced the weight (P b0.01) and volume (P b0.05 ) of the transplanted tumor [38].
One study demonstrated that knockout of ERCC1 by CRISPR/Cas9 could induce hypersensitiv-
ity of lung cancer cell lines to cisplatin [51]. In another study using a xenograft mouse model of
Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx 5
Trends in Molecular Medicine
Table 3. Studies Using CRISPR/Cas9 for Genes Related to Chemotherapeutic Drug Resistance in Lung Cancer Treatmenta
Target Expression in Knockout/other Experimental data Chemotherapeutic Refs
gene cells or tissues drug
RSF1 H460 and Knockout plus G1 cell-cycle arrest, increased cell apoptosis, decreased cell migration Paclitaxel [38]
H1299 cells; paclitaxel and proliferation; decreased tumor volume and weight
H460 cell xenograft treatment
in mice
ERCC1 Panel of lung Knockout Hypersensitivity to chemotherapeutic drugs; Cisplatin [51]
cancer cell lines plus TP53 only modest sensitivity
mutation/
deletion
NRF2 A549 cell lines Knockout Reduced cell proliferation; increased sensitivity to cisplatin, carboplatin, Cisplatin, [52]
and other chemotherapeutic agents. carboplatin
Significant decrease in tumor volume with gene editing in combination
with chemotherapy
Xenograft mouse
model Knockout
Aurora B NSCLC cells Knockout Recovery of TP53 expression; restoration of sensitivity to Cisplatin, paclitaxel [53]
chemotherapeutic drugs
a
Abbreviations: ERCC1, excision repair cross-complementation group 1; HCC827/ER, erlotinib-resistant HCC827; NRF2, nuclear factor-erythroid 2 p45-related factor 2;
RSF1 (HBXAP), remodeling and spacing factor 1.
lung cancer in which the NRF2 gene was knocked out in A549 cells by CRISPR/Cas9 found that
the tumor cells were sensitized to cisplatin and carboplatin, and the volume of the transplanted
tumor was significantly lower relative to that in wild-type animals (130 mm3 vs 660 mm3, and
200 mm3 vs 660 mm3, respectively) [52]. In NSCLC cell lines, knockout of aurora B (AURKB)
by CRISPR/Cas9 led to recovery of the expression of the tumor-suppressor gene TP53 and re-
stored sensitivity to cisplatin and paclitaxel [53]. Studies on lung cancer resistance to chemother-
apeutic drugs provide a scientific basis for improving the sensitivity and reducing or eliminating the
resistance of lung cancer to chemotherapeutics in clinical settings, and raise the possibility of im-
provements in chemotherapy.
Studies on Targeted Drugs and Inhibitor-Related Genes
CRISPR/Cas9 can also play an important role in screening drug targets. By combining
sgRNA and screening markers in the CRISPR library, potential target genes in the whole
genome can be screened rapidly. With the development of new molecular biology tech-
niques, the treatment of advanced NSCLC has changed from traditional chemotherapy
to molecular targeted therapies guided by genotyping. EGFR-TKIs are a widely used exam-
ple [54–56]. However, resistance to EGFR-TKIs has attracted increasing attention in recent
years. The main mechanisms of resistance include secondary mutation in the EGFR gene,
amplification of the target gene, change in tissue phenotype, activation of the bypass path-
way, and deletion or low expression of anti-oncogenes [57]. In recent years, numerous
studies have elucidated the mechanisms of resistance to targeted drugs in lung cancer
[58–60]. Genome-wide CRISPR/Cas9 enhancement/inhibition screening was performed
using erlotinib hydrochloride plus THZ1, a cyclin-dependent kinase 7/12 inhibitor, which
was previously shown to inhibit drug resistance in EGFR-dependent PC9 cells [61]. Inhi-
bition of multiple genes related to the EP300, CREBBP, and MED1 transcription factor
complex can enhance the synergistic effect of erlotinib plus THZ1 [61]. These results iden-
tified genes that specifically enhance or suppress the effect of transcriptional inhibition in
drug-tolerant cells.
6 Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx
Trends in Molecular Medicine
Several studies have examined genes related to resistance to the targeted drugs erlotinib
[41,61,62] and temozolomide [63] in lung cancer using the CRISPR/Cas9 technique
(summarized in Table 4) [41,61–63]. Knockout of the IGF1R gene could significantly reduce
drug resistance to erlotinib in the human NSCLC cell line HCC827 [41]. By contrast, knock-
out of the LHX6 gene in erlotinib-resistant HCC827 cells further increased the invasion ability
of the cells and increased their resistance to erlotinib [62].
In addition, some progress has been achieved in the application of CRISPR/Cas9 technology for
the study of lung cancer inhibitor-related genes, including EGFR, ALK, BRAF, MEK, and MET
(summarized in Table 4) [63–67]. In one study, the KEAP1 gene was knocked out in four lung can-
cer cell lines: NCI-H1299, HCC364, NCI-H1975, and HCC827. This study revealed that KEAP1
knockout reduced the sensitivity of BRAF, NRAS, KRAS, EGFR, and ALK mutant lung cancer
cells to inhibitors and promoted cell survival [64]. In studies on MEK1 and MET inhibitors in lung
cancer cells, knockout of MAP2K1 or gene editing of MET could reduce cell activity, inhibit cell
growth and colony formation, and render the cells sensitive to inhibitors [65,66]. In a mouse
model of EML4–ALK-driven lung cancer, editing the Eml4–Alk fusion gene could significantly en-
hance the sensitivity of the mouse tumors to anaplastic lymphoma kinase (ALK) inhibitors [66]. In
patient-derived xenograft mice models of small cell lung carcinoma (SCLC), after editing the
SLFN11 gene, poly(ADP-ribose) polymerase inhibitor therapy (talazoparib, 0.2 mg/kg daily) com-
bined with temozolomide (TMZ, 6 mg/kg every 4 days) significantly reduced tumor volume and
there was no tumor regrowth up to 180 days after the last TMZ treatment [63]. CRISPR/Cas9
gene editing can not only verify the therapeutic effect of targeted drugs and inhibitors in lung
cancer but also promote the development of targeted drug therapies in lung cancer by identifying
new candidate therapeutic targets.
Applications in Other Research Aspects of Lung Cancer Treatment
Modification of the Tumor Immune System Using CRISPR/Cas9
Chimeric antigen receptor T (CAR-T) cell immunotherapy is a T cell immunotherapy ap-
proach that involves genetic modification. T cells of patients are modified to 'attack' the tumor.
Specifically, T cells are modified by CRISPR/Cas9, and the immune system of the patients is mo-
bilized for the treatment of cancer [68] whereby the antitumor properties of the tumor microenvi-
ronment are enhanced to kill the tumor cells. In June 2016, the National Institutes of Health
approved the first clinical trial of CRISPR/Cas9 for CAR-T cell-based therapy in the USA. In that
trial, the CRISPR/Cas9 technology was used in patients with cancer to genetically modify their
T cells, which were then transferred back into the patients to achieve targeted destruction of
tumor cells [69].
In October 2016, Chinese scientists performed the world's first clinical trial of CRISPR/Cas9 in
humans, and the first patient received T cells modified by CRISPR/Cas9 technology, which in-
volved knockout of the programmed cell death 1 (PD1, also known as PDCD1) gene, indicat-
ing that the treatment was progressing smoothly [70]. PD-1 protein can prevent immune cells
from producing a protective immune response, and cancer cells make full use of this functional
feature of PD-1 to constantly propagate and spread throughout the body. Gene-edited T cells
were multiplied in the laboratory and reintroduced into the bloodstream of the patient to restore
the balance in immune response, leading to an anticancer effect. PD-1/PD-1 ligand (PD-L1)-
mediated immune escape in cancer progression has highlighted the crucial importance of this
process. Disruption of the PD-L1 3′-untranslated region (3′-UTR) in mice by CRISPR/Cas9 editing
enables immune evasion by EG7-OVA cancer cells with elevated PD-L1 expression,
suggesting that PD-L1 3′-UTR disruption can serve as a genetic marker to identify cancers that
actively evade antitumor immunity by overexpressing PD-L1 [71]. The application of CRISPR/Cas9
Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx 7
Trends in Molecular Medicine
Table 4. Studies Using CRISPR/Cas9 for Genes Related to Targeted Drugs or Inhibitors in Lung Cancer Treatmenta
Target Expression in cells or Knockout or Experimental data Chemotherapeutic Refs
gene tissues overexpression or targeted drugs
IGF1R HCC827 cells Knockout Decreased resistance to erlotinib Erlotinib [41]
hydrochloride
EP300, PC9 cells Genome-wide Inhibition of multiple genes associated with transcriptional Erlotinib [61]
CREBBP, CRISPR/Cas9 complexes (EP300, CREBBP, and MED1) enhanced the hydrochloride
and MED1 enhanced/inhibited synergism of erlotinib/THZ1
screening
LHX6 HCC827/ER cells Knockout Increased the invasion of HCC827/ER cells and resistance Erlotinib [62]
to erlotinib hydrochloride
SLFN11 SCLC patient- Genomic editing PARP inhibitor in combination with temozolomide Temozolomide; [63]
derived xenograft decreased tumor volume and weight PARP inhibitor
models
KEAP1 NCI-H1299, HCC364, Knockout Reduced sensitivity of BRAF, NRAS, KRAS-, EGFR, and BRAF, MEK, EGFR, [64]
NCI-H1975, and ALK mutant lung cancer cells to inhibitors, and increased and ALK inhibitors
HCC827 cells cell survival
MAP2K1 NCI-H1437 cells Knockout Decreased cell viability, sensitive to MEK1 inhibitors MEK1 inhibitors [65]
MET HEK293 cells Gene editing (MET Decreased cell growth, colony formation, and sensitivity MET inhibitors [66]
gene exon 14 deletion) to MET inhibitors
Eml4–Alk Mouse model of Gene editing Increased response to treatment with ALK inhibitors ALK inhibitors [67]
fusion gene EML4–ALK-driven
lung cancer
a
Abbreviations: CREBBP, CREB binding protein; EGFR, epidermal growth factor receptor; EMT, epithelial–mesenchymal transition; EP300, E1A binding protein p300;
HCC827/ER, erlotinib-resistant HCC827; IGF1R, insulin-like growth factor 1 receptor; PARP, poly(ADP-ribose) polymerase; SCLC, small cell lung carcinoma.
for immunomodulation has made some progress in research for treatment approaches in cancer
including lung cancer; although several clinical trials have been performed, studies on lung cancer
immunotherapy options using CRISPR/Cas9 gene editing technology have been limited.
Using CRISPR/Cas9 for miRNA Detection in Lung Cancer Diagnostics
MiRNAs are associated with a variety of diseases and have potential applications in the diagnosis
and treatment of cancer. However, given the complexity, high cost, and low sensitivity of miRNAs,
methods for the detection of miRNAs need to be improved. One study showed that a novel plat-
form involving isothermal amplification, which is based on rolling circle amplification, CRISPR/
Cas9, and split horseradish peroxidase techniques, can be used for the efficient detection
of miRNAs [72]. Trace amounts of miRNAs can be detected with single-base specificity
using this system, which can effectively detect target miRNAs such as let-7a in clinical serum
samples and distinguish patients with NSCLC from healthy volunteers. This study demonstrated
a remarkable downregulation of let-7a levels in patients with NSCLC compared with healthy
patients (P = 0.0004) [72]. This method, which is the first use of the CRISPR/Cas9 method for
miRNA detection, has potential in lung cancer screening, diagnostics, and prognosis, as well
as for providing information on favorable conditions for early treatment of lung cancer.
CRISPR Barcoding
The intrinsic genetic heterogeneity of tumor cells is the basis for tumor evolution and adaptation to
different environmental conditions. Using CRISPR/Cas9 technology and specific DNA barcodes –
a species identification system based on sequences from a short and standardized DNA region
[73] – it is possible to recapitulate and track the presence of a subset of cancer cells containing
mutations of interest. This method can be used to simulate different mechanisms of resistance
to EGFR inhibitors in lung cancer cells and to evaluate the efficacy of combination drug therapies
8 Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx
Trends in Molecular Medicine
[74]. CRISPR barcoding allows easy comparison of the effects of different mutations within Outstanding Questions
the same heterogeneous cell population. This technique is a fast and highly flexible means to CRISPR/Cas9 gene editing provides
investigate the effects of different genomic modifications in a broad range of functional assays, a new technology to improve the
treatment of lung cancer patients.
and can reproduce the potential crosstalk between genetically distinct cancer cells with or
However, current research is not
without the presence of therapy, thereby providing a model that more closely represents the systematic and in-depth, focusing pri-
complexity of response to treatment. CRISPR barcoding can be used to repair mutations in marily on in vitro cell experiments and
oncogenic driver genes and simultaneously track the fate of cancer cells with thousands of animal lung cancer model studies.
gene markers [74]. CRISPR barcoding promotes functional approaches for understanding
The most important technical
specific mutations, and this will certainly play a positive role in promoting research on the shortcomings of the CRISPR/Cas9 lie
treatment of lung cancer. in its off-target effects. The efficient de-
livery of the CRISPR/Cas9 system is
Deactivated Cas9 to Detect Allele Frequency and Mutation Rates another obstacle to its clinical applica-
tion. Only when these technical prob-
Using the powerful single-basepair specificity and generalizability of the CRISPR/Cas9 system, a lems are effectively solved can it be
small-allele enrichment method based on deactivated Cas9 (dCas9) was developed for efficient applied safely in clinical practice.
single-target and multiplexed enrichment. For the three most common EGFR mutations found
CRISPR/Cas9 must pass strict clinical
in NSCLC (exon 19 deletion, T790M, and L858R) [75], dCas9 has a significant advantage over
tests including specificity assessment
qPCR because of its ability to detect allele frequency and mutation rate. In a study of cell-free to better ensure that it distinguishes
DNA samples from NSCLC patients, N60% of the mutations detected using dCas9 were not de- cancer cells from healthy cells and
tected by qPCR [75]. The dCas9 method is an important application of the CRISPR/Cas9 system evaluation of treatment efficacy. The
application of CRISPR/Cas9 technology
in the field of genomic editing, and one that significantly improves the detection ability of cell-free for gene therapy of malignant tumors
DNA-based diagnosis, thus providing improved detection efficiency for the targeted treatment of continues to faces ethical issues.
lung cancer. Resolution of these difficulties will
ensure that it can be applied to the
clinical practice of lung cancer treatment.
Concluding Remarks
In the past few years CRISPR/Cas9 has emerged and advanced rapidly as a stable, efficient, and
widely used gene editing technology. Compared with other gene editing technologies, CRISPR/
Cas9 has many advantages for the treatment of tumors and has excellent application potential.
Scientists need to make full use of the advantages of CRISPR/Cas9 gene editing technology
and explore its potential for establishing tumor models and for studying the pathogenesis of ma-
lignant tumors and mechanisms of drug resistance. CRISPR/Cas9 gene editing technology is
certain to advance the rapid development of cancer research and bring new hope to cancer
patients.
Although CRISPR technology has developed rapidly in recent years, there are still several issues
related to its technical efficiency. The most important shortcoming of CRISPR/Cas9 gene editing
technology lies in its off-target effects [76,77], which stem from the tolerance of incomplete
matches between sgRNA and genomic DNA by Cas9. Furthermore, many studies have focused
on the efficient delivery of the CRISPR/Cas9 system and associated clinical issues [78–81]. Many
problems at the molecular level that are due to the use of CRISPR/Cas9 gene editing technology
for the treatment of tumors remain to be resolved, and CRISPR/Cas9 must pass strict clinical
tests, including specificity assessment to ensure that cancer cells are distinguished from healthy
cells, and evaluation of treatment efficacy, before it can enter clinical application (see Outstanding
Questions). In addition, the application of gene editing technologies for gene therapy of malignant
tumors continues to face ethical problems, which hinders progress in clinical research. In the fu-
ture, while continuing to improve the CRISPR/Cas9 system, more evidence should be gathered
from animal studies to ensure the safety and feasibility of this technology in clinical practice.
The CRISPR/Cas9 gene editing technology has been applied in many aspects of lung cancer
treatment-related research. This technology is a very promising method for improving the efficacy
of lung cancer treatment. We have reviewed and summarized progress in CRISPR/Cas9
Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx 9
Trends in Molecular Medicine
applications for lung cancer treatment, and have provided references for further studies on the
treatment of lung cancer based on CRISPR/Cas9 gene editing technology. We believe that fur-
ther systematization and in-depth studies are necessary and should be the focus of future re-
search on the application of the CRISPR/Cas9 gene editing technology in lung cancer
treatment before the findings can be extended to clinical practice.
Acknowledgments
This work was supported by the Tianjin City Health Industry Key Project Foundation (grant 16KG153).
References
1. Islami, F. et al. (2018) Proportion and number of cancer cases 25. Neri, M. et al. (2006) Prognostic role of K-Ras mutations in non-
and deaths attributable to potentially modifiable risk factors in small cell lung cancer: Still an issue for open debate. Lung
the United States. CA Cancer J. Clin. 68, 31–54 Cancer 53, 393–395
2. Chen, W. et al. (2016) Cancer statistics in China, 2015. CA 26. Koutsopoulos, A.V. et al. (2007) Simultaneous expression of c-
Cancer J. Clin. 66, 115–132 erbB-1, c-erbB-2, c-erbB-3 and c-erbB-4 receptors in non-
3. Vigneswaran, N. et al. (2005) Microarray gene expression profil- small-cell lung carcinomas: correlation with clinical outcome.
ing of cell lines from primary and metastatic tongue squamous Lung Cancer 57, 193–200
cell carcinoma: possible insights from emerging technology. 27. Virmani, A.K. and Gazdar, A.F. (2003) Tumor suppressor genes
J. Oral Pathol. Med. 34, 77–86 in lung cancer. Methods Mol. Biol. 222, 97–115
4. Alexandrov, L.B. et al. (2013) Signatures of mutational pro- 28. Sasaki, M. et al. (2003) Alterations of tumor suppressor genes
cesses in human cancer. Nature 500, 415–421 (Rb, p16, p27 and p53) and an increased FDG uptake in lung
5. Yi, L. and Li, J. (2016) CRISPR-Cas9 therapeutics in cancer: cancer. Ann. Nucl. Med. 17, 189
promising strategies and present challenges. Biochim. Biophys. 29. Liu, Y. et al. (2004) Tumor suppressor gene 14-3-3sigma is
Acta 1866, 197–207 down-regulated whereas the proto-oncogene translation elon-
6. Moses, C. and Kaur, P. (2019) Applications of CRISPR systems gation factor 1delta is up-regulated in non-small cell lung can-
in respiratory health: entering a new 'red pen' era in genome cers as identified by proteomic profiling. J. Proteome Res. 3,
editing. Respirology 24, 628–637 728–735
7. Doench, J.G. et al. (2014) Rational design of highly active 30. Jubair, L. and McMillan, N.A.J. (2017) The therapeutic potential
sgRNAs for CRISPR-Cas9-mediated gene inactivation. Nat. of CRISPR/Cas9 systems in oncogene-addicted cancer types:
Biotechnol. 32, 1262–1267 virally driven cancers as a model system. Mol. Ther. Nucleic
8. Bhakta, M.S. et al. (2013) Highly active zinc-finger nucleases by Acids 8, 56–63
extended modular assembly. Genome Res. 23, 530–538 31. White, M.K. and Khalili, K. (2016) CRISPR/Cas9 and cancer tar-
9. Moscou, M.J. and Bogdanove, A.J. (2009) A simple cipher gov- gets: future possibilities and present challenges. Oncotarget 7,
erns DNA recognition by TAL effectors. Science 326, 1501 12305–12317
10. Sethi, S. et al. (2018) Study of photochemical cytosine to uracil 32. Russell, S.J. and Peng, K.W. (2007) Viruses as anticancer drugs.
transition via ultrafast photo-cross-linking using vinylcarbazole Trends Pharmacol. Sci. 28, 326–333
derivatives in duplex DNA. Molecules 23, E828 33. Gilbert, L.A. et al. (2013) CRISPR-mediated modular RNA-
11. Bai, Y. et al. (2018) Gene editing as a promising approach for re- guided regulation of transcription in eukaryotes. Cell 154,
spiratory diseases. J. Med. Genet. 55, 143–149 442–451
12. Xiang, G. et al. (2017) Temperature effect on CRISPR-Cas9 me- 34. Bu, X. et al. (2018) CD38 knockout suppresses tumorigenesis
diated genome editing. J. Genet. Genomics 44, 199–205 in mice and clonogenic growth of human lung cancer cells.
13. Shah, S.Z. et al. (2019) Advances in research on genome editing Carcinogenesis 39, 242–251
Crispr-Cas9 technology. J. Ayub Med. Coll. Abbottabad 31, 35. Cheung, A.H. et al. (2018) Specific targeting of point mutations in
108–122 EGFR L858R-positive lung cancer by CRISPR/Cas9. Lab.
14. Guha, T.K. and Edgell, D.R. (2017) Applications of alternative nu- Investig. 98, 968–97621
cleases in the age of CRISPR/Cas9. Int. J. Mol. Sci. 18, E2565 36. Tang, K.J. et al. (2016) Focal adhesion kinase regulates the DNA
15. Sanchez-Rivera, F.J. and Jacks, T. (2015) Applications of the CRISPR- damage response and its inhibition radiosensitizes mutant KRAS
Cas9 system in cancer biology. Nat. Rev. Cancer 15, 387–395 lung cancer. Clin. Cancer Res. 22, 5851–5863
16. Gori, J.L. et al. (2015) Delivery and specificity of CRISPR-Cas9 37. Liu, F. et al. (2017) Nestin servers as a promising prognostic bio-
genome editing technologies for human gene therapy. Hum. marker in non-small cell lung cancer. Am. J. Transl. Res. 9,
Gene Ther. 26, 443 1392–1401
17. Koo, T. et al. (2017) Selective disruption of an oncogenic mutant 38. Chen, X. et al. (2017) Rsf-1 influences the sensitivity of non-small
allele by CRISPR/Cas9 induces efficient tumor regression. cell lung cancer to paclitaxel by regulating NF-kappaB pathway
Nucleic Acids Res. 45, 7897–7908 and Its downstream proteins. Cell. Physiol. Biochem. 44,
18. Kim, W. et al. (2018) Targeting mutant KRAS with CRISPR-Cas9 2322–2336
controls tumor growth. Genome Res. 28, 374–382 39. Huang, F. et al. (2018) delta-Catenin promotes tumorigenesis
19. Jiang, D.J. et al. (2018) Revolution in gene medicine therapy and and metastasis of lung adenocarcinoma. Oncol. Rep. 39,
genome surgery. Genes 9, E575 809–817
20. Check, E. (2005) Gene-therapy trials to restart following cancer 40. Yi, J. et al. (2018) A genome-wide comprehensive analysis of
risk review. Nature 434, 127 alterations in driver genes in non-small-cell lung cancer.
21. Coskunpinar, E. et al. (2015) Investigation of some DNA repair Anti-Cancer Drugs 29, 10–18
genes association in non small cell lung cancer. Cell. Mol. Biol. 41. Hussmann, D. et al. (2017) IGF1R depletion facilitates MET-
61, 57–62 amplification as mechanism of acquired resistance to erlotinib
22. El-Aneed, A. (2004) Current strategies in cancer gene therapy. in HCC827 NSCLC cells. Oncotarget 8, 33300–33315
Eur. J. Pharmacol. 498, 1–8 42. Zhou, X. et al. (2018) Inhibition of glutamate oxaloacetate trans-
23. Volm, M. et al. (1994) Analysis of c-fos, c-jun, c-erbB1, c-erbB2 aminase 1 in cancer cell lines results in altered metabolism with
and c-myc in primary lung carcinomas and their lymph node me- increased dependency of glucose. BMC Cancer 18, 559
tastases. Clin. Exp. Metastasis 12, 329–334 43. Chen, M.L. et al. (2007) Epigenetic changes in tumor suppressor
24. Oxnard, G.R. et al. (2013) New targetable oncogenes in non- genes, P15, P16, APC-3 and E-cadherin in body fluid.
small-cell lung cancer. J. Clin. Oncol. 31, 1097–1104 Kaohsiung J. Med. Sci. 23, 498–503
10 Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx
Trends in Molecular Medicine
44. Solomon, H. et al. (2010) Inactivation of the p53 tumor suppres- 62. Liao, J. et al. (2017) Down-regulation of miR-214 reverses erloti-
sor gene and activation of the Ras oncogene: cooperative nib resistance in non-small-cell lung cancer through up-
events in tumorigenesis. Discov. Med. 9, 448–454 regulating LHX6 expression. Sci. Rep. 7, 781
45. Yu, X. and Wang, W. (2017) Tumor suppressor microRNA613 63. Lok, B.H. et al. (2017) PARP inhibitor activity correlates with
inhibits glioma cell proliferation, invasion and angiogenesis by SLFN11 expression and demonstrates synergy with temozolo-
targeting vascular endothelial growth factor A. Mol. Med. Rep. mide in small cell lung cancer. Clin. Cancer Res. 23, 523–535
16, 6729–6735 64. Krall, E.B. et al. (2017) KEAP1 loss modulates sensitivity to ki-
46. Sun, H. et al. (2018) SIRT4 acts as a tumor suppressor in gastric nase targeted therapy in lung cancer. eLife 6, e18970
cancer by inhibiting cell proliferation, migration, and invasion. 65. Gannon, H.S. et al. (2016) Identification of an 'exceptional re-
OncoTargets Ther. 11, 3959–3968 sponder' cell line to MEK1 inhibition: clinical implications for
47. Xu, K. et al. (2017) MFN2 suppresses cancer progression MEK-targeted therapy. Mol. Cancer Res. 14, 207–215
through inhibition of mTORC2/Akt signaling. Sci. Rep. 7, 41718 66. Togashi, Y. et al. (2015) MET gene exon 14 deletion created
48. Romero, R. et al. (2017) Keap1 loss promotes Kras-driven lung using the CRISPR/Cas9 system enhances cellular growth and
cancer and results in dependence on glutaminolysis. Nat. Med. sensitivity to a MET inhibitor. Lung Cancer 90, 590–597
23, 1362–1368 67. Maddalo, D. et al. (2014) In vivo engineering of oncogenic chro-
49. Li, C.G. et al. (2017) MicroRNA-1304 suppresses human non- mosomal rearrangements with the CRISPR/Cas9 system.
small cell lung cancer cell growth in vitro by targeting heme Nature 516, 423–427
oxygenase-1. Acta Pharmacol. Sin. 38, 110–119 68. Wu, H. and Cao, C. (2019) The application of CRISPR-Cas9
50. Chen, Y. and Zhang, Y. (2018) Application of the CRISPR/Cas9 genome editing tool in cancer immunotherapy. Brief. Funct.
system to drug resistance in breast cancer. Adv. Sci. 5, Genomics 18, 129–132
1700964 69. Zhan, T. et al. (2019) CRISPR/Cas9 for cancer research and
51. Heyza, J. et al. (2019) Identification and characterization of syn- therapy. Semin. Cancer Biol. 55, 106–119
thetic viability with ERCC1 deficiency in response to interstrand 70. Cyranoski, D. (2016) Chinese scientists to pioneer first human
crosslinks in lung cancer. Clin. Cancer Res. 25, 2523–2536 CRISPR trial. Nature 535, 476–477
52. Bialk, P. et al. (2018) Functional gene knockout of NRF2 In- 71. Kataoka, K. et al. (2016) Aberrant PD-L1 expression through 3'-
creases chemosensitivity of human lung cancer A549 cells UTR disruption in multiple cancers. Nature 534, 402–406
in vitro and in a xenograft mouse model. Mol. Ther. Oncolytics 72. Qiu, X.Y. et al. (2018) Highly effective and low-cost microRNA
11, 75–89 detection with CRISPR-Cas9. ACS Synth. Biol. 7, 807–813
53. Yu, J. et al. (2018) High expression of Aurora-B is correlated with 73. Simeone, M.C. et al. (2013) Application of plastid and nuclear
poor prognosis and drug resistance in non-small cell lung can- markers to DNA barcoding of Euro-Mediterranean oaks
cer. Int. J. Biol. Markers 33, 215–221 (Quercus, Fagaceae): problems, prospects and phylogenetic im-
54. Nishinarita, N. et al. (2018) Smoking history as a predictor of epi- plications. Bot. J. Linn. Soc. 172, 478–499
dermal growth factor receptor tyrosine kinase inhibitors in pa- 74. Guernet, A. et al. (2016) CRISPR-barcoding for intratumor ge-
tients with non-small cell lung cancer harboring EGFR netic heterogeneity modeling and functional analysis of onco-
mutations. Oncology 95, 109–115 genic driver mutations. Mol. Cell 63, 526–538
55. Fu, S. et al. (2018) Estrogen receptor beta1 activation acceler- 75. Aalipour, A. et al. (2018) Deactivated CRISPR associated protein
ates resistance to epidermal growth factor receptor-tyrosine ki- 9 for minor-allele enrichment in cell-free DNA. Clin. Chem. 64,
nase inhibitors in non-small cell lung cancer. Oncol. Rep. 39, 307–316
1313–1321 76. Zhang, X.H. et al. (2015) Off-target effects in CRISPR/Cas9-
56. Girard, N. (2018) Optimizing outcomes in EGFR mutation- mediated genome engineering. Mol. Ther. Nucleic Acids 4, e264
positive NSCLC: which tyrosine kinase inhibitor and when? 77. Shen, B. et al. (2014) Efficient genome modification by CRISPR-
Future Oncol. 14, 1117–1132 Cas9 nickase with minimal off-target effects. Nat. Methods 11,
57. Uramoto, H. et al. (2011) Expression of selected gene for ac- 399–402
quired drug resistance to EGFR-TKI in lung adenocarcinoma. 78. Liu, C. et al. (2017) Delivery strategies of the CRISPR-Cas9
Lung Cancer 73, 361–365 gene-editing system for therapeutic applications. J. Control.
58. Lategahn, J. et al. (2018) Lessons to be learned: the molecular Release 266, 17
basis of kinase-targeted therapies and drug resistance in non- 79. Zhang, L. et al. (2017) Lipid nanoparticle-mediated efficient deliv-
small cell lung cancer. Angew. Chem. 57, 2307–2313 ery of CRISPR/Cas9 for tumor therapy. NPG Asia Mater. 9, e441
59. Hsu, K.H. et al. (2019) High PD-L1 expression correlates with 80. Ellis, K. and Terry, S.F. (2015) Dangerous liaisons: connecting
primary resistance to EGFR-TKIs in treatment naive advanced CRISPR/Cas9 to clinical science. Genet. Test. Mol. Biomarkers
EGFR-mutant lung adenocarcinoma patients. Lung Cancer 19, 409
127, 37–43 81. Kang, X.J. et al. (2017) Addressing challenges in the clinical ap-
60. Lin, J.J. and Shaw, A.T. (2016) Resisting resistance: targeted plications associated with CRISPR/Cas9 technology and ethical
therapies in lung cancer. Trends Cancer 2, 350–364 questions to prevent its misuse. Protein Cell 8, 1–5
61. Terai, H. et al. (2018) ER stress signaling promotes the survival of
cancer 'persister cells' tolerant to EGFR tyrosine kinase inhibi-
tors. Cancer Res. 78, 1044–1057
Trends in Molecular Medicine, Month 2019, Vol. xx, No. xx 11
You might also like
- Targeted Therapies for Lung CancerFrom EverandTargeted Therapies for Lung CancerRavi SalgiaNo ratings yet
- Seminars in Cancer Biology: Tianzuo Zhan, Niklas Rindtor FF, Johannes Betge, Matthias P. Ebert, Michael Boutros TDocument14 pagesSeminars in Cancer Biology: Tianzuo Zhan, Niklas Rindtor FF, Johannes Betge, Matthias P. Ebert, Michael Boutros TKyla BaysaNo ratings yet
- Life Sciences: Review ArticleDocument13 pagesLife Sciences: Review ArticleHelen Gail EmbudoNo ratings yet
- Zhan 2018Document14 pagesZhan 2018Gopal PunithanNo ratings yet
- Advances in Cancer Biology - Metastasis: Ocean Khajuria, Neha SharmaDocument5 pagesAdvances in Cancer Biology - Metastasis: Ocean Khajuria, Neha SharmaMuhamad AliNo ratings yet
- CRISPR-Cas9: A Promising Genetic Engineering Approach in Cancer ResearchDocument2 pagesCRISPR-Cas9: A Promising Genetic Engineering Approach in Cancer ResearchDigdo SudigyoNo ratings yet
- CRISPR/Cas9 and Next Generation Sequencing in The Personalized Treatment of CancerDocument14 pagesCRISPR/Cas9 and Next Generation Sequencing in The Personalized Treatment of Cancerjames oliverNo ratings yet
- CRISPR-cas Gene TherapyDocument23 pagesCRISPR-cas Gene TherapyBenyam ZenebeNo ratings yet
- Journal Cellular Physiology - 2020 - Zhang - CRISPR Cas Gene TherapyDocument24 pagesJournal Cellular Physiology - 2020 - Zhang - CRISPR Cas Gene Therapyandrefc98No ratings yet
- Paper Review On Gene Knock-Out (Advincula, Genova, Nemiz)Document5 pagesPaper Review On Gene Knock-Out (Advincula, Genova, Nemiz)Jean Rose GenovaNo ratings yet
- Impact of Micrornas in Resistance To Chemotherapy and Novel Targeted Agents in Non-Small Cell Lung CancerDocument11 pagesImpact of Micrornas in Resistance To Chemotherapy and Novel Targeted Agents in Non-Small Cell Lung Cancerdai itakoNo ratings yet
- Gene Editing Using CRISPR-Cas9 For The Treatment oDocument3 pagesGene Editing Using CRISPR-Cas9 For The Treatment oLatiefah NWNo ratings yet
- Case Study CRISPRDocument12 pagesCase Study CRISPRjeffersonmanalo787No ratings yet
- Explore Rare Cancer Medicine MutationsDocument6 pagesExplore Rare Cancer Medicine MutationsMikel AngelNo ratings yet
- Cancer Research Papers FreeDocument8 pagesCancer Research Papers Freeafnhdqfvufitoa100% (1)
- Mrna Vaccine cv9103 and cv9104 For The Treatment of Prostate CancerDocument8 pagesMrna Vaccine cv9103 and cv9104 For The Treatment of Prostate Cancerapi-675909478No ratings yet
- Sinclair Frazer Recent Advances in The Delivery andDocument20 pagesSinclair Frazer Recent Advances in The Delivery andhmasoumeh65No ratings yet
- CRISPR/Cas9 Gene Editing: A New Approach For Overcoming Drug Resistance in CancerDocument29 pagesCRISPR/Cas9 Gene Editing: A New Approach For Overcoming Drug Resistance in Cancerjames oliverNo ratings yet
- Tumor Markers in Clinical Practice: General Principles and GuidelinesDocument8 pagesTumor Markers in Clinical Practice: General Principles and GuidelinesNurmalia SariNo ratings yet
- CRISPR-CAS9 Developement and Its Prospect in Hepatocellular Carcinoma Treatement PDFDocument12 pagesCRISPR-CAS9 Developement and Its Prospect in Hepatocellular Carcinoma Treatement PDFNatalia ParraNo ratings yet
- ch210005954p PDFDocument5 pagesch210005954p PDFJanNo ratings yet
- Artigo Cisplatina 1Document12 pagesArtigo Cisplatina 1Daiane RochaNo ratings yet
- CCR Connections Vol. 7, No. 1, 2013Document32 pagesCCR Connections Vol. 7, No. 1, 2013CancerResearchNo ratings yet
- Alternative Splicing in L - 2019 - Biochimica Et Biophysica Acta BBA - Gene ReDocument13 pagesAlternative Splicing in L - 2019 - Biochimica Et Biophysica Acta BBA - Gene RemetrorespoNo ratings yet
- Chitosan-Capped Silver Nanoparticles With Potent and Selective Intrinsic Activity Against The Breast Cancer CellsDocument12 pagesChitosan-Capped Silver Nanoparticles With Potent and Selective Intrinsic Activity Against The Breast Cancer CellsHrishikesh UpadhyayaNo ratings yet
- Lung Cancer Thesis PDFDocument4 pagesLung Cancer Thesis PDFykramhiig100% (2)
- Ne 2019 143972Document35 pagesNe 2019 143972Sara SabinaNo ratings yet
- JurnalDocument2 pagesJurnalElizabeth Puji YantiNo ratings yet
- Bussines EngineringDocument9 pagesBussines EngineringWhulan Rhana TonapaNo ratings yet
- CRISPR/Cas9 Therapeutics: Progress and Prospects: Signal Transduction and Targeted TherapyDocument23 pagesCRISPR/Cas9 Therapeutics: Progress and Prospects: Signal Transduction and Targeted Therapysolmendoza.rodrigo17No ratings yet
- Sciadv Abc9450Document13 pagesSciadv Abc9450Rocio Angie Navarro SeguraNo ratings yet
- Poet Report: KRAS Testing For Colorectal CancerDocument9 pagesPoet Report: KRAS Testing For Colorectal CancerJohn KentNo ratings yet
- Limits To Personalized Cancer MedicineDocument6 pagesLimits To Personalized Cancer MedicineJuan AraújoNo ratings yet
- Tianzuo Zhan, Niklas Rindtorff, Johannes Betge, Matthias P. Ebert, and Michael BoutrosDocument1 pageTianzuo Zhan, Niklas Rindtorff, Johannes Betge, Matthias P. Ebert, and Michael BoutrosMiyuki MeyNo ratings yet
- Tianzuo Zhan, Niklas Rindtorff, Johannes Betge, Matthias P. Ebert, and Michael BoutrosDocument1 pageTianzuo Zhan, Niklas Rindtorff, Johannes Betge, Matthias P. Ebert, and Michael BoutrosMiyuki MeyNo ratings yet
- Assignment Applied Genomics and Proteomics: Mtech (Biotechnology) 3 SEM 2014-2016Document14 pagesAssignment Applied Genomics and Proteomics: Mtech (Biotechnology) 3 SEM 2014-2016rawatpooran05No ratings yet
- First-Line Treatment of Metastatic Renal Cell Carcinoma: A Systematic Review and Network Meta-AnalysisDocument8 pagesFirst-Line Treatment of Metastatic Renal Cell Carcinoma: A Systematic Review and Network Meta-AnalysisDr. Alexandre SatoNo ratings yet
- Cas 112 388Document9 pagesCas 112 388herdianNo ratings yet
- Editorial: Lung Cancer: Prevalent Trends & Emerging ConceptsDocument3 pagesEditorial: Lung Cancer: Prevalent Trends & Emerging Conceptsjeevan georgeNo ratings yet
- Jurnal Tugas Minggu Ke 3-AuNP Prostate Cancer MiceDocument25 pagesJurnal Tugas Minggu Ke 3-AuNP Prostate Cancer Micepath gamingNo ratings yet
- Potential of Chimeric AntigenDocument20 pagesPotential of Chimeric AntigenT SNo ratings yet
- Editorial Transl Medicine ReportsDocument4 pagesEditorial Transl Medicine Reportsapi-334757816No ratings yet
- Pathway Cancer MedicationDocument10 pagesPathway Cancer MedicationWaode RahmahNo ratings yet
- Elucidative PAMTarget Sequence For CRISPRCas - 9 Activity in Breast Cancer Using A Computational ApproachDocument5 pagesElucidative PAMTarget Sequence For CRISPRCas - 9 Activity in Breast Cancer Using A Computational ApproachInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Barabadi 2019 - Emerging Theranostic Biogenic Silver Nanoparticles For Breast Cancer PDFDocument21 pagesBarabadi 2019 - Emerging Theranostic Biogenic Silver Nanoparticles For Breast Cancer PDFayiedNo ratings yet
- Personalised Cancer MedicineDocument5 pagesPersonalised Cancer MedicineRomina HeydarinasabNo ratings yet
- 1 s2.0 S0169500221004062 MainDocument9 pages1 s2.0 S0169500221004062 MainandresdemedNo ratings yet
- Systemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewDocument11 pagesSystemic Therapy in The Curative Treatment of Head and Neck Squamous Cell Cancer: A Systematic ReviewLorena Sánchez PérezNo ratings yet
- Journal Cellular Physiology - 2018 - Zarredar - Combination Therapy With KRAS siRNA and EGFR Inhibitor AZD8931 SuppressesDocument8 pagesJournal Cellular Physiology - 2018 - Zarredar - Combination Therapy With KRAS siRNA and EGFR Inhibitor AZD8931 SuppressesSara SabinaNo ratings yet
- Pearls and Pitfalls in The Imaging of Targeted Therapy and Immunotherapy in Lung CancerDocument11 pagesPearls and Pitfalls in The Imaging of Targeted Therapy and Immunotherapy in Lung CancerNelson William UsnayoNo ratings yet
- The Use of Aptamers in Prostate Cancer A Systematic Review ofDocument17 pagesThe Use of Aptamers in Prostate Cancer A Systematic Review ofFernanda LDNo ratings yet
- Rakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerDocument8 pagesRakha Et Al. 2006 Prognostic Markers in Triple Negative Breast CancerdanishNo ratings yet
- Emerging 1Document7 pagesEmerging 1lotiyashubhamNo ratings yet
- An Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesDocument9 pagesAn Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesBobNo ratings yet
- Referensi 1Document9 pagesReferensi 1Indah Syaidatul MNo ratings yet
- Tumor Marker General Principles and Guidelines (S.sharma 2013)Document8 pagesTumor Marker General Principles and Guidelines (S.sharma 2013)Ria DeviNo ratings yet
- Review Article (1) - 1Document9 pagesReview Article (1) - 1sufyanm1005No ratings yet
- Advances in Lung Cancer ResearchDocument5 pagesAdvances in Lung Cancer ResearchJor GarciaNo ratings yet
- Biomarkers For The Lung Cancer Diagnosis and Their Advances in ProteomicsDocument11 pagesBiomarkers For The Lung Cancer Diagnosis and Their Advances in ProteomicsAndi Harmawati NNo ratings yet
- Circulating DNA As Prognostic Biomarker in Patients With Advanced Hepatocellular Carcinoma, A Translational Exploratory Study From The SORAMIC TrialDocument15 pagesCirculating DNA As Prognostic Biomarker in Patients With Advanced Hepatocellular Carcinoma, A Translational Exploratory Study From The SORAMIC Trialmagendi indra muktiNo ratings yet
- The Rattrap LitchartDocument15 pagesThe Rattrap LitchartTharun VasuNo ratings yet
- Qdoc - Tips - Biology Investigatory ProjectDocument20 pagesQdoc - Tips - Biology Investigatory ProjectTharun VasuNo ratings yet
- LETTER WRITING For 6-10Document14 pagesLETTER WRITING For 6-10Tharun VasuNo ratings yet
- Important Questions For Class 12 Chemistry Chapter 1 The Solid State Class 12 Important QuestionsDocument32 pagesImportant Questions For Class 12 Chemistry Chapter 1 The Solid State Class 12 Important QuestionsTharun VasuNo ratings yet
- Emergence of LifeDocument28 pagesEmergence of LifeTharun VasuNo ratings yet
- Pda: A Global Association: Recombinant Factor C - EndolisaDocument29 pagesPda: A Global Association: Recombinant Factor C - EndolisaPiruzi MaghlakelidzeNo ratings yet
- Infernal Gpu SlidesDocument22 pagesInfernal Gpu SlidesRodrigoMansueliNunesNo ratings yet
- Mechanism of Muscle ContractionDocument51 pagesMechanism of Muscle ContractionRizcky Naldy Eka Putra100% (1)
- Human Heredity Principles and Issues 11th Edition Cummings Solutions ManualDocument10 pagesHuman Heredity Principles and Issues 11th Edition Cummings Solutions Manualstacyperezbrstzpmgif100% (32)
- Oxford University Press - Online Resource Centre - Multiple Choice QuestionsDocument5 pagesOxford University Press - Online Resource Centre - Multiple Choice QuestionsHUAWEI HUAWEI50% (2)
- International Rice Research Notes Vol.21 No.2Document100 pagesInternational Rice Research Notes Vol.21 No.2ccquintosNo ratings yet
- A Review of Phytochemistry and Pharmacology of FlavonoidsDocument17 pagesA Review of Phytochemistry and Pharmacology of FlavonoidshycarpenterNo ratings yet
- Glycosyltransferase Engineering For Carbohydrate Synthesis: John B. Mcarthur and Xi ChenDocument14 pagesGlycosyltransferase Engineering For Carbohydrate Synthesis: John B. Mcarthur and Xi ChenJemiNo ratings yet
- CH.7 RESPIRATION IN PLANTS Class 9 Notes IcseDocument7 pagesCH.7 RESPIRATION IN PLANTS Class 9 Notes IcseFebin GeorgeNo ratings yet
- Reagen Dan Instrumen Pendukung Untuk Laboratorium Pengujian COVID-19Document14 pagesReagen Dan Instrumen Pendukung Untuk Laboratorium Pengujian COVID-19Mike SihombingNo ratings yet
- Qualitative Analysis On Salivary Amylase Enzyme ActivityDocument8 pagesQualitative Analysis On Salivary Amylase Enzyme ActivityKorrine Gumabon BalaisNo ratings yet
- PriceList Rafa Topaz - IGM 2022Document9 pagesPriceList Rafa Topaz - IGM 2022yazid al bastomiNo ratings yet
- Chronic Liver Diseases 2017Document373 pagesChronic Liver Diseases 2017Gustavo Moviglia100% (1)
- Chapter 3 - Antibody Topic NotesDocument10 pagesChapter 3 - Antibody Topic NotesAngelica Joy GonzalesNo ratings yet
- Life Sciences P2 Survival KitDocument35 pagesLife Sciences P2 Survival KitMashamba CoutinhoNo ratings yet
- Action of ArtemisininDocument6 pagesAction of ArtemisininPaulo CumbaneNo ratings yet
- Molecular BiologyDocument2 pagesMolecular BiologyAlbert Tesoro Silang Jr.No ratings yet
- Dietary Therapy For A Weakened Middle BurnerDocument28 pagesDietary Therapy For A Weakened Middle Burnernpapadokostas100% (2)
- EtymologyDocument1 pageEtymologyJonee SansomNo ratings yet
- Chapter 2 - Chemistry of Life 2022-09-23 20 - 12 - 32Document25 pagesChapter 2 - Chemistry of Life 2022-09-23 20 - 12 - 32Talia osseilyNo ratings yet
- Final Manuscript RevisionDocument16 pagesFinal Manuscript RevisionArya AdilaksaNo ratings yet
- 2 Methods For Characterizing Microbial Communities in Caves and Karst: A ReviewDocument24 pages2 Methods For Characterizing Microbial Communities in Caves and Karst: A Reviewjames dropNo ratings yet
- Pharmacology I Lecture 2 (Antibiotics) : Protein Synthesis InhibitorsDocument40 pagesPharmacology I Lecture 2 (Antibiotics) : Protein Synthesis Inhibitorsعلي الفواديNo ratings yet
- CarcinogenDocument196 pagesCarcinogenJosé RamírezNo ratings yet
- Biomolecules PDFDocument21 pagesBiomolecules PDFVedant SalgudeNo ratings yet
- CBSE Class 12 Chemistry Biomolecules Questions Answers PDFDocument7 pagesCBSE Class 12 Chemistry Biomolecules Questions Answers PDFLakshmi DesikanNo ratings yet
- Broad-Spectrum Antiviral TherapeuticsDocument15 pagesBroad-Spectrum Antiviral TherapeuticsGian BanaresNo ratings yet
- Joyce 2007Document1 pageJoyce 2007Ben Duncan Málaga EspichánNo ratings yet
- B.SC Botany To Be Applicable From, July 2019 (First Semester Only)Document17 pagesB.SC Botany To Be Applicable From, July 2019 (First Semester Only)pt3790446No ratings yet
- TMP 26 FDDocument64 pagesTMP 26 FDFrontiersNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (39)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (83)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (256)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet