Professional Documents
Culture Documents
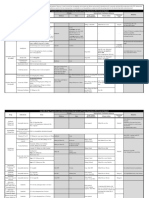
Drug Main ACLS Use Dose/Route Notes
Uploaded by
shadyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Main ACLS Use Dose/Route Notes
Uploaded by
shadyCopyright:
Available Formats
Drug Main ACLS Use Dose/Route Notes
Rapid IV push
close to the hub,
followed by a
Narrow PSVT/SVT
6 mg IV bolus, saline bolus
Wide QRS
may repeat with Continuous cardiac
tachycardia, avoid
Adenosine 12 mg in 1 to 2 monitoring during
adenosine in
min. administration
irregular wide QRS
Causes flushing
and chest
heaviness
VF/pulseless Anticipate
VT: 300mg hypotension,
dilute in 20 to bradycardia, and
30ml., may gastrointestinal
repeat 150mg toxicity
every 3 to 5 Continuous cardiac
VF/pulseless VT
minutes monitoring
VT with pulse
Stable VT with Very long half-life
Amiodarone Tachycardia rate
a pulse: 150mg (up to 40 days)
control
bolus followed Do not use in 2nd
by amiodarone or 3rd-degree heart
drip (300 mg block
should only be Do not administer
used in a code via the ET tube
situation) route
0.5 mg IV/IO
every 3 to 5
Symptomatic Cardiac and BP
minutes
Bradycardia monitoring
Max Dose: 3
Do not use in
mg
glaucoma or
Atropine
tachyarrhythmias
Specific
Minimum dose 0.5
Toxins/overdose 2 to 4 mg IV/IO
mg
(e.g. may be needed
organophosphates)
2 to 20
Fluid resuscitation
mcg/kg/min
first
Shock/CHF Titrate to
Dopamine Cardiac and BP
desired blood
monitoring
pressure
Epinephrine Cardiac Arrest Initial: 1.0 mg Continuous cardiac
(1:10000) IV or monitoring
2 to 2.5 mg NOTE: Distinguish
(1:1000) between 1:1000
Drug Main ACLS Use Dose/Route Notes
Maintain: 0.1 to
0.5 mcg/kg/min
Titrate to desire
blood pressure
0.3-0.5 mg IM and 1:10000
Anaphylaxis Repeat every 5 concentrations
mins as needed Give via central
line when possible
2 to 10
mcg/min
Symptomatic
infusion
bradycardia/Shock
Titrate to
response
Initial: 1 to 1.5
mg/kg IV
loading
Cardiac Arrest Second: Half of
(VF/VT) first dose in 5
Cardiac and BP
to 10 min
Lidocaine monitoring
Maintain: 1 to 4
(Lidocaine is Rapid bolus can
mg/min
recommended cause hypotension
when and bradycardia
Initial: 0.5 to
Amiodarone is Use with caution in
1.5 mg/kg IV
not available) renal failure
Wide Complex Second: Half of
Tachycardia with first dose in 5
Pulse to 10 min
Maintain: 1 to 4
mg/min
Cardiac Arrest:
Cardiac Cardiac and BP
1 to 2 gm
Arrest/pulseless monitoring
diluted in 10
Torsades Rapid bolus can
mL D5W IVP
cause hypotension
and bradycardia
Magnesium If not Cardiac
Use with caution in
Sulfate Arrest: 1 to 2
renal failure
Torsades de Pointes gm IV over 5 to
Calcium chloride
with pulse 60 min
can reverse
Maintain: 0.5 to
hypermagnesemia
1 gm/hr IV
Procainamide Wide QRS 20 to 50 Cardiac and BP
Tachycardia mg/min IV monitoring
Preferred for VT until rhythm Caution with acute
with pulse (stable) improves, MI
hypotension May reduce dose
Drug Main ACLS Use Dose/Route Notes
occurs, QRS
widens by 50%
or MAX dose is with renal failure
given Do not give with
MAX dose: 17 amiodarone
mg/kg Do not use in
Drip = 1 to 2 prolonged QT or
gm in 250 to CHF
500 mL at 1 to
4 mg/min
Tachyarrhythmia
100 mg (1.5
Monomorphic VT Do not use in
mg/kg) IV over
Sotalol 3rd line anti- prolonged QT
5 min
arrhythmic
THERAPEUTIC HYPOTHERMIA
Recommended for comatose individuals with the return of spontaneous circulation
after a cardiac arrest event.
Individuals should be cooled to 89.6 to 93.2 degrees F (32 to 36 degrees C) for at least
24 hours.
OPTIMIZATION OF HEMODYNAMICS AND VENTILATION
100% oxygen is acceptable for early intervention but not for extended periods of time.
Oxygen should be titrated, so that individual’s pulse oximetry is greater than 94% to
avoid oxygen toxicity.
Do not over ventilate to avoid potential adverse hemodynamic effects.
Ventilation rates of 10 to 12 breaths per minute to achieve ETCO2 at 35 to 40 mmHg.
IV fluids and vasoactive medications should be titrated for hemodynamic stability.
PERCUTANEOUS CORONARY INTERVENTION
Percutaneous coronary intervention (PCI) is preferred over thrombolytics.
Individual should be taken by EMS directly to a hospital that performs PCI.
If the individual is delivered to a center that only delivers thrombolytics, they should
be transferred to a center that offers PCI if time permits.
NEUROLOGICAL CARE
Neurologic assessment is key, especially when withdrawing care (i.e., brain death) to
decrease false-positive rates. Specialty consultation should be obtained to monitor
neurologic signs and symptoms throughout the post-resuscitation period.
You might also like
- IM On Call (LANGE On Call) PDFDocument738 pagesIM On Call (LANGE On Call) PDFindia2puppy100% (8)
- Common ICU DripsDocument1 pageCommon ICU DripsSunshine Willis100% (2)
- Commonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFDocument12 pagesCommonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFYannis Zoldenberg100% (1)
- ACLS Pocket GuideDocument5 pagesACLS Pocket Guidedragnu100% (1)
- Critical Care Intravenous Medications ChartDocument2 pagesCritical Care Intravenous Medications ChartMichelle Danielle MolinaNo ratings yet
- Adenosine: Rapid IV PushDocument4 pagesAdenosine: Rapid IV PushsabboNo ratings yet
- Fármacos CardiacosDocument2 pagesFármacos CardiacosMARILUZ ROSA NOVOA GUTIERREZNo ratings yet
- Pharmacological Tools: Doses, Routes, and Uses of Common DrugDocument1 pagePharmacological Tools: Doses, Routes, and Uses of Common DrugApuntesdemedicinaa blogNo ratings yet
- ACLS Algorithm Pulse No Yes: Stable Patient Unstable Patient Stable PatientDocument1 pageACLS Algorithm Pulse No Yes: Stable Patient Unstable Patient Stable PatientAhmed AlkhaqaniNo ratings yet
- Critical Care Drug Reference SheetDocument12 pagesCritical Care Drug Reference SheetYanina CoxNo ratings yet
- Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 8e, 2016 Cardiac Rhythm Disturbance SDocument2 pagesTintinalli's Emergency Medicine: A Comprehensive Study Guide, 8e, 2016 Cardiac Rhythm Disturbance SDanielGiraldoNo ratings yet
- Paramedic Drugs: Drug Class Indications Dosage NameDocument14 pagesParamedic Drugs: Drug Class Indications Dosage NameIbrahem Al100% (6)
- Dilution Protocol For AdultsDocument23 pagesDilution Protocol For AdultsSharumathi ChandraNo ratings yet
- GambarDocument27 pagesGambarAnonymous feLB4alTNo ratings yet
- Vaso PressorsDocument1 pageVaso PressorsJames BrownNo ratings yet
- Farmacos Reanimacion PediatricaDocument1 pageFarmacos Reanimacion PediatricaMiriam C. F. TapiaNo ratings yet
- ICE DrugsDocument2 pagesICE DrugsRichelle FrondaNo ratings yet
- Pharmacology Part 2Document5 pagesPharmacology Part 2cherrymaemidoriNo ratings yet
- Drug Classification Action Indication Adverse Effect Age and Administration Adrenaline (Epinephrine)Document7 pagesDrug Classification Action Indication Adverse Effect Age and Administration Adrenaline (Epinephrine)Danica LachicaNo ratings yet
- Obat-Obatan Dalam Bantuan Hidup LanjutDocument16 pagesObat-Obatan Dalam Bantuan Hidup LanjutTheresia SihotangNo ratings yet
- ACLS Drug TherapyDocument8 pagesACLS Drug TherapySahrensNo ratings yet
- Acls Medications and Their Use: Garrett Thompson, Pharm.D. Wake Forest University Baptist Medical CenterDocument37 pagesAcls Medications and Their Use: Garrett Thompson, Pharm.D. Wake Forest University Baptist Medical CenterroshamaharaniNo ratings yet
- Medication Administration PolicyDocument76 pagesMedication Administration PolicyJully GaciasNo ratings yet
- Acls Patient Algorithms: Greg Cook's Version of A Phoenix Fire DPT ClasicDocument4 pagesAcls Patient Algorithms: Greg Cook's Version of A Phoenix Fire DPT ClasicDouglas Greg CookNo ratings yet
- Nitroglycerin Drug StudyDocument2 pagesNitroglycerin Drug StudyBeatrizz P GellaNo ratings yet
- Acls Algorithms 2012Document12 pagesAcls Algorithms 2012kivuNo ratings yet
- Paediatric Advanced Life Support: Call For Help 2222 Commence/continue CPR (5 Initial Breaths Then CV Ratio 15:2)Document1 pagePaediatric Advanced Life Support: Call For Help 2222 Commence/continue CPR (5 Initial Breaths Then CV Ratio 15:2)Vijay RNo ratings yet
- ACLS Algorithms Adult 2010Document12 pagesACLS Algorithms Adult 2010anon_336736395No ratings yet
- Dem Module 3Document23 pagesDem Module 3Nicolo Martin BelloNo ratings yet
- CRASH CART Presentation PPTX 1 MELODocument33 pagesCRASH CART Presentation PPTX 1 MELOCamille GalasNo ratings yet
- Obat Obat EmergencyDocument34 pagesObat Obat EmergencymatkwokNo ratings yet
- StatusEpilepticus Pocket CardDocument2 pagesStatusEpilepticus Pocket CardDiana MihaiNo ratings yet
- EMD-MNH Clinical Protocal-12 March 2014Document14 pagesEMD-MNH Clinical Protocal-12 March 2014tgrrwccj98No ratings yet
- List of Emergency Drugs and Their Action PDFDocument3 pagesList of Emergency Drugs and Their Action PDFDr. Vishal SengarNo ratings yet
- AlgorithmACLSBradycardiawithapulse PDFDocument1 pageAlgorithmACLSBradycardiawithapulse PDFjohndoe1995No ratings yet
- Resuscitation Drugs (Ali Haedar)Document41 pagesResuscitation Drugs (Ali Haedar)Bayu AkbarNo ratings yet
- Drug List: Medication Adult Dosing Pediatric DosingDocument14 pagesDrug List: Medication Adult Dosing Pediatric DosingAndrew JamesNo ratings yet
- Most Common Medication - in Emergency RoomDocument24 pagesMost Common Medication - in Emergency RoomFerdos AdemNo ratings yet
- Ccu Guideline Nicvd-1Document9 pagesCcu Guideline Nicvd-1Farhan AnikNo ratings yet
- Induction Agents MOA Onset, Duration Special Uses / Notes PropofolDocument3 pagesInduction Agents MOA Onset, Duration Special Uses / Notes PropofolpaveethrahNo ratings yet
- Tachycardia AlgorithmDocument1 pageTachycardia AlgorithmGideon BahuleNo ratings yet
- ED Dilution Guide 2018 - Jan 2019Document42 pagesED Dilution Guide 2018 - Jan 2019asyrafrusydi9901No ratings yet
- ACLS Drug Therapy RevisedDocument4 pagesACLS Drug Therapy RevisedpaveethrahNo ratings yet
- Generic Name Side Effects Before:: Ventricular ArrhythmiasDocument4 pagesGeneric Name Side Effects Before:: Ventricular ArrhythmiasElizabeth Ivory ChuaNo ratings yet
- PCU Medication ListDocument11 pagesPCU Medication ListreneecolemanNo ratings yet
- Name of Drug Dose Action Indication Contraindicatio N Side Effect Nurses ResponsibilityDocument22 pagesName of Drug Dose Action Indication Contraindicatio N Side Effect Nurses ResponsibilityPunam PalNo ratings yet
- Emergency Medicine: KarsimDocument39 pagesEmergency Medicine: KarsimNur HikmahNo ratings yet
- Terbutaline BricanylDocument1 pageTerbutaline BricanylB PNo ratings yet
- Pediatric Cardiac Arrest Algorithm-2015 UpdateDocument2 pagesPediatric Cardiac Arrest Algorithm-2015 UpdateKholida UlfaNo ratings yet
- ACLS Drugs Power Point1Document4 pagesACLS Drugs Power Point1Shu Shan KhoNo ratings yet
- Acls Drug OverviewDocument2 pagesAcls Drug OverviewShannon Davis100% (1)
- CHEST Seizure Status Epilepticus InfographicDocument1 pageCHEST Seizure Status Epilepticus InfographicDRCRISTOBALTENIZANo ratings yet
- Ecart MedicationsDocument39 pagesEcart Medicationsanon_140774008No ratings yet
- Peri-Arrest ArrythmiaDocument14 pagesPeri-Arrest Arrythmiamohamed mowafeyNo ratings yet
- Acls Pharmacology OverviewDocument11 pagesAcls Pharmacology OverviewzoyaligNo ratings yet
- Hypertensive Urgency EmergencyDocument5 pagesHypertensive Urgency Emergencydamondouglas100% (3)
- DementiaDocument26 pagesDementianadya100% (4)
- Lacunar Infarct - Radiology Reference Article - RadiopaediaDocument8 pagesLacunar Infarct - Radiology Reference Article - RadiopaediaRismanto TorsioNo ratings yet
- Feeding Disorders in ChildrenDocument65 pagesFeeding Disorders in Childrendrhananfathy100% (5)
- Health Locus of Control and Diabetes Adherence 2161 0487.S3 E002Document2 pagesHealth Locus of Control and Diabetes Adherence 2161 0487.S3 E002iulianaNo ratings yet
- Prescription PsychologyDocument7 pagesPrescription PsychologyJose LuisNo ratings yet
- Onco-Critical Care An Evidence-Based ApproachDocument539 pagesOnco-Critical Care An Evidence-Based ApproachZuriNo ratings yet
- Diagnostic Criteria Decision Tree PDFDocument2 pagesDiagnostic Criteria Decision Tree PDFNor Nadia ZakariaNo ratings yet
- Principles of Removable Denture Pros Tho Don Tics 2007-08 - KaddahDocument145 pagesPrinciples of Removable Denture Pros Tho Don Tics 2007-08 - KaddahJudy Abbott100% (1)
- Stevens-Johnson SyndromeDocument4 pagesStevens-Johnson SyndromeBelleNo ratings yet
- Perioperative Hemodynamic MonitoringDocument9 pagesPerioperative Hemodynamic MonitoringjayezmenonNo ratings yet
- Twin Block 3Document2 pagesTwin Block 3GisselaMaldonadoNo ratings yet
- Preeclampsia Pathophysiology andDocument15 pagesPreeclampsia Pathophysiology andYojhaida Zarate CasachahuaNo ratings yet
- SchizophreniaDocument67 pagesSchizophreniaHazirah Mokhtar100% (1)
- Literature ReviewDocument3 pagesLiterature Reviewapi-609233193No ratings yet
- Int Endodontic J - 2022 - Shah - Outcomes Reporting in Systematic Reviews On Surgical Endodontics A Scoping Review For TheDocument22 pagesInt Endodontic J - 2022 - Shah - Outcomes Reporting in Systematic Reviews On Surgical Endodontics A Scoping Review For TheDhiaa AloweadatNo ratings yet
- 5,600 Residents Tested: Case SummaryDocument3 pages5,600 Residents Tested: Case SummaryPeterborough ExaminerNo ratings yet
- MCN 1Document5 pagesMCN 1Aijem RyanNo ratings yet
- Dental Management in Hypertensive PatientsDocument9 pagesDental Management in Hypertensive PatientsIJAERS JOURNALNo ratings yet
- Bell 2015Document5 pagesBell 2015Afien MuktiNo ratings yet
- Nicaragua Reflection PaperDocument3 pagesNicaragua Reflection Paperapi-487254609No ratings yet
- Levels of Care Intensive Care Society 2009Document14 pagesLevels of Care Intensive Care Society 2009bogus987No ratings yet
- Steroids Other Appearance Performance Enhancing Drugs Apeds Research ReportDocument34 pagesSteroids Other Appearance Performance Enhancing Drugs Apeds Research ReportFit and LiftNo ratings yet
- Fees and Charges - Summary From 1 July 2020 Version 1.0, June 2020Document51 pagesFees and Charges - Summary From 1 July 2020 Version 1.0, June 2020QualityMattersNo ratings yet
- Droplet InfectionsDocument11 pagesDroplet InfectionsdevNo ratings yet
- Derek C Angus Caring For Patients With AcuteDocument4 pagesDerek C Angus Caring For Patients With AcuteAnanth BalakrishnanNo ratings yet
- PCNE Classification Scheme For Drug Related Problems-1 (Revised)Document3 pagesPCNE Classification Scheme For Drug Related Problems-1 (Revised)Alan HobbitNo ratings yet
- Test Bank For Health Psychology 7th Edition TaylorDocument21 pagesTest Bank For Health Psychology 7th Edition Taylorwoodwardpunction2vq46zNo ratings yet
- Thesis Statement For Nicotine AddictionDocument8 pagesThesis Statement For Nicotine Addictiongbww46x7100% (2)
- Kudori Therapy - Updated 9th Dec17Document32 pagesKudori Therapy - Updated 9th Dec17Manickavasagam RengarajuNo ratings yet
- Systemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsDocument4 pagesSystemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsRandom PersonNo ratings yet