Professional Documents
Culture Documents
Clinical Practice Recommendations For Improving Life Participation For People With Aphasia in Long-Term Care
Uploaded by
aOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Practice Recommendations For Improving Life Participation For People With Aphasia in Long-Term Care
Uploaded by
aCopyright:
Available Formats
PERSPECTIVES SIG 2
Clinical Focus
Clinical Practice Recommendations for
Improving Life Participation for People
With Aphasia in Long-Term Care
Jamie H. Aziosa and Jack S. Damicob
Purpose: The purpose of this clinical focus article is to Recommendations: Clinicians in LTC facilities have the
present an overview of the Life Participation Approach to responsibility of delivering services that have a positive
Aphasia as it relates to issues in long-term care (LTC) and impact on communication, social relationships, emotional
provide practical recommendations for implementing the health, and quality of life. Clinical tools and approaches
approach in this setting. The Framework for Living With most appropriate for LTC settings are identified that help
Aphasia is used as a guide to (a) highlight specific challenges to address these goals. Approaches are discussed across
to life participation for residents with aphasia in LTC and several stages representing the therapeutic process, which
(b) propose clinical tools that might help clinicians move is ultimately aimed at moving a resident toward recovery
through the therapeutic process when implementing the Life and increased independence. Case demonstrations are
Participation Approach to Aphasia. provided to illustrate approaches.
M
uch of the early research in aphasia was driven Within the past few decades, many researchers and clinicians
by the idea that all therapeutic activities should have challenged this notion. This has resulted in a movement
be guided by impairment. Therefore, in tradi- away from a focus on language deficits intrinsic to a per-
tional approaches, aphasia was primarily seen from a dis- son with aphasia and toward a discovery of communica-
ability standpoint with the foremost goal of treatment being tion competence and avenues for support (e.g., Ferguson,
physiological recovery of function. Most of the work pub- 1996; Simmons-Mackie & Damico, 1996a). This trend,
lished during this time was devoted to improving language coupled with external influences by disability rights activ-
at a segmented level by maximizing correct responses by ists and a curtailment of funding for services, prompted the
a person with aphasia (e.g., Porch, 1967; Schuell, Jenkins, creation of a philosophy of service delivery that better met
& Jimenez-Pabon, 1964). This idea is still germane to the the needs of people impacted by aphasia, dubbed the Life
medical model of disability and widely used today. As such, Participation Approach to Aphasia (LPAA; LPAA Project
it is not unusual for aphasia therapy to have a primary fo- Group, 2001).
cus on improving deficits in the neurological system The purpose of this clinical focus article is to high-
with a goal of maximum restoration of linguistic function. light the importance of LPAA in long-term care (LTC)
Although this approach is well intentioned and attrac- facilities and equip clinicians with practical recommenda-
tive, it can be misleading, as it operates from an assumption tions for implementing LPAA in this setting. We use the
that recovery requires a focus on “fixing” the impairment. Framework for Living With Aphasia (A-FROM) as a
guide to (a) highlight specific challenges to life participa-
tion for residents with aphasia in LTC and (b) propose
a clinical tools that might help clinicians move through the
Department of Speech and Hearing Sciences, Lamar University,
Beaumont, TX
therapeutic process when implementing LPAA. At the
b
Department of Speech, Language, and Hearing Sciences, University conclusion of the clinical focus article, we provide two
of Colorado Boulder case study demonstrations of LPAA based on the first
Correspondence to Jamie H. Azios: jamie.azios@lamar.edu author’s clinical and research experiences to illustrate this
Editor: Peter Meulenbroek process in LTC.
Received October 4, 2019
Accepted October 12, 2019
Disclosures
https://doi.org/10.1044/2019_PERSP-19-00136 Financial: Jamie H. Azios has no relevant financial interests to disclose. Jack S.
Publisher Note: This article is part of the Forum: Directions and Damico has no relevant financial interests to disclose.
Approaches to Aphasia Inspired by Life Participation Approach to Nonfinancial: Jamie H. Azios has no relevant nonfinancial interests to disclose.
Aphasia Values. Jack S. Damico has no relevant nonfinancial interests to disclose.
384 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020 • Copyright © 2020 American Speech-Language-Hearing Association
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
LPAA as LPAA and social models of disability (Kagan et al.,
2008).
The LPAA is a philosophy rather than a specific treat- The A-FROM was primarily based on the World
ment approach and is based on many of the same values Health Organization’s International Classification of Func-
and beliefs of social or pragmatic approaches to aphasia tioning, Disability and Health (World Health Organization,
(Simmons-Mackie, 2008). In LPAA, there is an unmitigated 2001), a biopsychosocial model of disability that defines
emphasis on goals related to life participation and social health in terms of physical, psychological, and social well-
relationships regardless of a change in language function. being. While the International Classification of Function-
While a clinician implementing LPAA may work on improv- ing, Disability and Health is a broad measure applicable to
ing or compensating for impairment within a relevant life functioning and disability in various health conditions, the
activity, equally important is targeting any barrier to life A-FROM is specific to “living with aphasia” (Kagan et al.,
participation. This is true even if the activity is not directly 2008, p. 265) and the various internal and external factors
related to communication (LPAA Project Group, 2001). that might contribute to the degree of disability experienced
For example, a clinician may help a person with aphasia as the result of a condition. In the A-FROM, life with
work toward a goal of participating in a weekly poker night aphasia is defined as the interaction of four major domains:
with friends, joining a bible study, or hosting a family aphasia severity, communication and language environment,
gathering by training communication partners or making participation in life situations, and personal factors includ-
the environment more “aphasia friendly” (Howe, Worrall, ing identity and affective responses (see Figure 1). Aphasia
& Hickson, 2004). severity refers to the degree of impairment across linguistic
LPAA aligns with the desires of people with aphasia processing, including comprehension, expression, reading,
and their family members. People with aphasia and their and writing. Communication and language environment
family members have discussed the importance of outcomes refers to the physical or social environment in which a per-
related to life participation, prioritizing goals related to son lives and includes the actions and attitudes of others.
maintaining social networks and increasing independence Participation in life situations encompasses the day-to-day
in various life roles and activities (Wallace et al., 2017). activities of people with aphasia and the roles, responsibili-
Living a successful life after aphasia has been directly linked ties, and relationships manifested in these activities. Com-
to resuming activities from prestroke life, adapting activities munication and conversation are critical components of
to increase participation, and developing new hobbies and this domain. Finally, the personal factors domain includes
interests (Brown, Worrall, Davidson, & Howe, 2012). how a person with aphasia may view themselves (i.e., iden-
While there is value in implementing LPAA across tity) and any attitudes and feelings associated with aphasia.
the entire life span of a person with aphasia, including Aphasia assessment and intervention in LTC may occur
acute stages, it may be even more beneficial in later stages across the entire A-FROM schematic. However, the envi-
of recovery when aphasia is deemed chronic. The goals of ronment, participation in life situations, and personal iden-
people with aphasia tend to change over time, with social tity may be the most critical domains for clinicians working
and relationship goals (e.g., conversing with friends, attend- in LTC facilities as institutionalization often comes with
ing social outings) surfacing once the rehabilitation period significant, distinct challenges associated with these categories.
has ended (Worrall et al., 2010). Many individuals with
stroke-related aphasia may return home at this point, but
due to shortened hospital stays and changes to reimburse- Aphasia in LTC
ment, an increasing number of stroke survivors do not. Most LTC facilities are considered what Goffman
In fact, approximately one in five people discharged from (1961) terms “total institutions.” Total institutions are unique
a hospital after stroke is now entering LTC facilities for establishments because they function as both a place of res-
further care (Nguyen et al., 2015). This estimate may be idence and a place of work where two sets of people (i.e.,
higher for those with stroke-related aphasia since language workers and residents) often have divergent sets of values
impairment has been recognized as a predictive factor for for existing in the same space. Inhabitants of total institu-
institutionalization (González-Fernández, Christian, Davis, tions are separated from the outside social world and live a
& Hillis, 2013). relatively enclosed life. All of life participation occurs within
the confines of the facility, and there are minimal oppor-
tunities for engaging in activities in the outside world.
LPAA in a Conceptual Framework For persons with aphasia in LTC facilities, the facility “is”
It is often helpful to organize approaches and tech- home. Therefore, LTC facilities are likely one of the most
niques congruent with a particular philosophy within a important health care contexts for implementing LPAA
conceptual framework. Doing so can help guide clinicians and examining outcomes related to life participation.
in creating client-centered goals and selecting useful, appro- Due to the complex nature of an environment with
priate assessments and interventions that target the wants two separate (and potentially conflicting) agendas, there
and needs of the people receiving services. We have chosen are many barriers to successful life participation in LTC.
to use the A-FROM for our purposes here since it was In terms of the communication and language environment,
built upon value-based approaches within our field, such the physical makeup of a facility (e.g., physical layout,
Azios & Damico: Optimizing Life Participation in Long-Term Care 385
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
Figure 1. The Framework for Living With Aphasia. Reprinted with permission from Aphasia Intitute.
acoustics, shared spaces) has been noted to negatively in- dementia-producing conditions (e.g., Moyle et al., 2011).
fluence opportunities for social interaction (van Dijck- For persons with aphasia in LTC facilities, opportunities
Heinen, Wouters, Janssen, & van Hoof, 2014). Many staff to engage in residential activities are even more difficult
members lack the skills required to effectively support due to the inappropriate and inaccessible nature of activi-
residents with specific communicative needs, leading to com- ties. In their observations of natural interactions in LTC
munication breakdowns (Bryan, Axelrod, Maxim, Bell, & facilities, Azios et al. (2018) found that recreational activi-
Jordan, 2002). Additionally, there is considerable staff turn- ties chosen by facilities were not representative of age, cog-
over, impacting the ability for nurse assistants to become nitive and communicative abilities, desires, or individual
familiar with individual interests and practice communica- strengths.
tion strategies (Long, Azios, & Richings, 2019; Page & Increasing life participation in LTC can also be diffi-
Rowles, 2016). Two studies have explicitly focused on real- cult due to personal factors such as identity and attitudes
time interactions between nursing staff in LTC and persons related to aphasia. While there is an increased interest in
with aphasia. Azios, Damico, and Roussel (2018) found providing person-centered care in various facets of health
that staff members in some facilities tend to prioritize phys- care, the act of entering an LTC facility can be viewed as a
ical needs over interactional needs, unintentionally deem- terminal stage of life and promote the belief that an indi-
phasizing communication for social purposes and meaningful vidual’s personhood and life story are ending (Villar &
relationships. Similarly, Saldert, Bartonek-Åhman, and Serrat, 2017). Unfortunately for people with aphasia in LTC
Bloch (2018) discuss that, while nurses do engage in some institutions, depersonalization can happen quickly. Personal
personal, psychosocial aspects of talk during routine care histories of persons with aphasia in LTC facilities are often
activities, the main proportion of interaction (78%–90% of lost due to the individual’s language impairment, and staff
time spent) includes talk central or related to the task at members know little about residents with aphasia except for
hand. the most basic information (Parr, 2007). Additionally,
Participation in daily life activities appears especially people with aphasia in LTC settings have described feelings
limited for residents in LTC facilities. Several researchers of worry, frustration, and sadness as a result of aphasia
have discussed a lack of activity and stimulation in facili- and hopelessness for improving communication abilities
ties, leading to boredom and agitation for persons with (Hartwell, 2015).
386 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
Organizational Culture and the Role of the philosophies prioritize psychosocial outcomes and engage-
Speech-Language Pathologist ment in personally relevant life activities. Also, both models
encourage autonomy and operate under the assumption
Organizational culture in LTC plays an important that consumers can and should make their own decisions
role in mitigating barriers related to life participation. Orga- about their needs and goals. See Figure 2 for additional
nizational culture refers to the shared belief systems, values, features of resident-centered care analogous to the LPAA.
and expectations that drive how people behave and com- By implementing LPAA in LTC, SLPs can be at the fore-
municate within an institution (Hemmelgarn, Glisson, & front of culture change and serve as a model for promoting
James, 2006). There are several types of organizational resident-centered care within the setting.
cultures in health care, but in LTC facilities, most types
are classified under two broad models of care: traditional
and resident centered. Traditional models of care employ Practice Recommendations for Promoting
more authoritative and hierarchical practices where proce- LPAA in LTC
dures for care are rigid, predictable, and organized by those
In most LTC facilities, residents are identified for
who own or manage the facility (Brownie & Nancarrow,
therapy services upon admission. In these cases, the SLP
2013). Contrastingly, resident-centered models of care pro-
has little prior knowledge of the resident’s medical or social
mote a collaborative environment and shared decision
history and will begin a data-gathering process that will
making to increase the independence of residents. Facilities
help to establish a communication diagnosis and severity,
that implement resident-centered care are most interested
describe communicative function across tasks and environ-
in putting a resident’s well-being above all other priorities,
ments, and formulate an appropriate rehabilitation plan.
fostering close and intimate relationships, and encouraging
Other times, residents may be living in a facility for several
engagement in personally meaningful activities (Thomas &
months to years before they are identified for services. The
Johnson, 2003). Several studies have pointed to improved
process of identifying residents who may need services is
resident outcomes in terms of quality of life, safety, health-
unique to each facility, but most facilities employ routine
related measures (e.g., presence of infection), and engage-
screening to assess for any functional changes that may
ment in activities when LTC facilities implement resident-
have occurred over a set period of time. Here, the clinician
centered care (for a review, see Shier, Khodyakov, Cohen,
may have more or less familiarity with the resident at the
Zimmerman, & Saliba, 2014).
start of the assessment process, but residents typically have
Organizational culture impacts the behaviors and ac-
a medical diagnosis (e.g., stroke) and communication
tions of professionals working within the setting. Speech-
diagnosis (e.g., aphasia) prior to assessment. Regardless of
language pathologists (SLPs) have an important role in
the source of referral, assessment and intervention in LTC
providing best practices in LTC facilities but often face
should follow a set of processes or stages aimed at moving a
challenges related to organizational culture. SLPs have re-
resident toward recovery and increased independence.
ported that facilities have unrealistic expectations for pro-
Worrall, Sherratt, and Papathanasiou (2017) suggest the
ductivity standards and that they face ongoing ethical
following five steps: (a) information gathering and sharing,
dilemmas regarding various aspects of clinical decision mak-
(b) collaborative goal setting, (c) pretherapy assessment,
ing (Cutter & Polovoy, 2014). A recent survey of SLPs
(d) therapy, and (e) reassessment. Steps are cyclical, and it
working in LTC facilities found that SLPs’ perceptions of
is customary for SLPs to revisit steps throughout the course
organizational culture impacted decisions to evaluate a
of therapy. Each step is outlined below with a description
resident for language disorders (Douglas, 2016). Results
of procedures most appropriate for promoting LPAA in
from the same study indicated that leadership within the
LTC. Examples of tools used during assessment stages (i.e.,
facility prohibited the majority of responding SLPs to im-
first three steps) are listed in Table 1. Please note this is
plement group therapy, a finding that is incongruous with
not an exhaustive list but are suggested tools deemed most
the large evidence base for this approach (e.g., Elman &
appropriate for clinicians electing to implement LPAA in
Bernstein-Ellis, 1999).
LTC facilities.
Despite these problems, SLPs have the responsibility
of delivering services that will have a positive impact on
communication, social relationships, emotional health, and Step 1: Information Gathering and Sharing
quality of life. While complete culture change in LTC is In the first stage, clinicians are interested in gathering
complex and likely a lofty goal, clinicians can begin to ad- information about a resident’s health condition and medi-
vocate for change by practicing intellectual and behavioral cal history as well as obtaining initial information across
flexibility, developing personal relationships with staff all domains of the A-FROM. For the purposes of LPAA,
members and emphasizing their achievements, understanding the communication environment, participation in day-to-day
how to manage conflicts, and identifying facilitators and activities, and personal identity domains are particularly
barriers across policies and systems (Douglas & Hickey, revealing and can begin to inform the clinician about the
2015). When working directly with people with aphasia, degree to which aphasia impacts life participation. Broad,
many of the foci and objectives of resident-centered care are self-report tools that capture information across multiple
directly in line with those of the LPAA. For example, both domains may be most beneficial at this stage so the SLP
Azios & Damico: Optimizing Life Participation in Long-Term Care 387
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
Figure 2. Corresponding features of Life Participation Approach to Aphasia and Resident-Centered Care.
can begin to understand strengths and barriers across activi- stepping to the other side. People with aphasia are encour-
ties and contexts. Two examples are described below and aged to use the picture to help describe what “living with
include semistructured interviewing and the Assessment for aphasia” means to them.
Living With Aphasia (ALA; Kagan et al., 2011). The SLP
should make every attempt to gain information from the
perspective of the person with aphasia but may also need Step 2: Collaborative Goal Setting
to rely on family members or care providers in this setting, The next step in the assessment process includes de-
depending on severity of aphasia, presence of comorbidities ciding what is most important to target for therapy. Most
(e.g., hearing loss), and degree of isolation. people with stroke-induced aphasia are able to express
Ethnographic or semistructured interviewing of people their own goals for rehabilitation but are often excluded
with aphasia and family members can help clinicians better from the goal-setting process (Berg, Askim, Balandin,
understand personal viewpoints about aphasia and its im- Armstrong, & Rise, 2017). Since LPAA is “consumer
pact on life participation (Simmons-Mackie & Damico, driven” (LPAA Project Group, 2001, p. 236), it shares
1996b). Questions are usually broad and open-ended, such many values with person-centered care, including the philos-
as “Tell me a little about your aphasia” or “Tell me what ophy that the person with aphasia is the expert in their
a typical day looks like for you,” prompting people with own condition and that decision making about the thera-
aphasia to share their story (Worrall et al., 2017). The clini- peutic process should be collaborative (Hughes, Bamford,
cian can then use follow-up questions to probe deeper into & May, 2008). Thus, to implement LPAA in LTC, SLPs
challenges associated with specific life experiences or activi- must involve the resident with aphasia when creating goals.
ties (e.g., getting dressed, conversing with staff and other Based on the previous step, clinicians should have
residents). See Westby (1990) for a detailed explanation of a few ideas about the major concerns of the resident with
the process of ethnographic interviewing. aphasia. The important part of this stage is to convert
A more formal assessment procedure that may be concerns into written objectives (Worrall et al., 2017). For
beneficial for persons with more severe aphasia or those people with limited expression, the SLP may use instru-
reluctant to share experiences includes the ALA. The ments with picture symbols such as the Life Interests and
ALA is a pictographic, self-report measure based on the Values Cards (Haley, Womack, Helm-Estabrooks, Caignon,
A-FROM. It was created with the input of important stake- & McCulloch, 2010) or Talking Mats to help support the
holders (i.e., people with aphasia, family members) and selection of goals most important to the resident. Both tools
has strong psychometric properties (Simmons-Mackie et al., have been used successfully for collaborative goal setting
2014). The ALA uses a conversational context but helps to in people with varying degrees of aphasia (e.g., Haley,
support expression and comprehension through picto- Womack, Harmon, & Williams, 2015; Murphy & Boa, 2012).
graphic metaphors. For example, one of the most revealing Isaksen (2018) also discusses clinicians attempting collabo-
questions in the ALA includes “The Wall” question, which rative goal setting through supported conversation tech-
can be used in conjunction with semistructured interviews niques (Kagan, 1998) or self-made aphasia-friendly initiatives
to gain perspectives about a specific life activity (Baier, to help support the interaction (e.g., smiley scales).
Hoepner, & Sather, 2018). The question uses a picture of a There are a few frameworks that can help guide clini-
wall with the word “aphasia” and a man at various stages cians in collaborative goal setting. Hersh, Worrall, Howe,
of the wall. There is a scale at the bottom of the picture Sherratt, and Davidson (2012) suggest a process where clini-
ranging from “big problem” to “no problem,” with the man cians establish SMARTER goals, ones that are Shared,
standing away from the wall, beginning to climb over it, or Monitored, Accessible, Relevant, Transparent, Evolving,
388 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
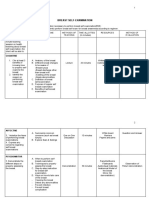
Table 1. Tools for assessment of life participation in long-term care facilities.
Tool Information source A-FROM domain(s)
Ethnographic interviewing Self-report Environment
Participation
Personal identity
Assessment for Living With Aphasia Self-report Environment
Participation
Personal identity
Communicative Profiling System Self-report and clinician rating Environment
Participation
Personal identity
Life Interests and Values Cards Self-report Environment
Participation
Personal identity
FOURC model Self-report Environment
Participation
Personal identity
ASHA-FACS Clinician rating Participation
Communication Effectiveness Index Caregiver rating Participation
Measure of Skill in Supported Conversation Clinician rating Environment
Measure of Participation in Conversation Clinician rating Participation
MECQ-LTC Clinician rating Environment
Participation
CADL-3 Clinician rating Participation
Comprehensive Aphasia Test–Disability and Impact Questionnaire Self-report Environment
Participation
Personal identity
SAQOL-39 Self-report Participation
Personal identity
Burden of Stroke Scale Self-report Participation
Personal identity
Communication Confidence Rating Scale for Aphasia Self-report Participation
Personal identity
Note. Ethnographic interviewing from Westby (1990), Assessment for Living With Aphasia from Kagan et al. (2011), Communicative Profiling
System from Simmons-Mackie and Damico (1996b), Life Interests and Values Cards from Haley et al. (2010), FOURC model from Haley et al.
(2019), American Speech-Language-Hearing Association Functional Assessment of Communication Skills (ASHA-FACS) from Frattali et al.
(2017), Communicative Effectiveness Index from Lomas et al. (1989), Measure of Skill in Supported Conversation and Measure of Participation
in Conversation from Kagan et al. (2004), Montreal Evaluation of Communication Questionnaire for Use in Long-Term Care (MECQ-LTC) from
Le Dorze et al. (2000), Communication Activities of Daily Living–Third Edition (CADL-3) from Holland et al. (2018), Comprehensive Aphasia
Test–Disability and Impact Questionnaire from Swinburn et al. (2004), Stroke and Aphasia Quality of Life Scale (SAQOL) from Hilari et al. (2009),
Burden of Stroke Scale from Doyle et al. (2004), and Communication Confidence Rating Scale for Aphasia from Babbitt et al. (2011). A-FROM =
Framework for Living With Aphasia.
and Relationship centered. Haley, Cunningham, Barry, and improve the ability to converse with other residents during
de Riesthal (2019) describe the FOURC model, a tool to a meal, then the assessment tool or procedure should
help clinicians work with clients to identify meaningful goals reveal a measure of conversation participation at meals.
across four intervention prongs: skills and abilities, inten- Assessments at this stage can be self-report or rated by
tional strategies, environmental supports, and motivation the clinician, but a combination of both measures is
and confidence. The FOURC model was developed as an preferred.
extension of the A-FROM, and each prong correlates with SLPs in LTC have a great responsibility in ensuring
the A-FROM domains associated with living with aphasia. that the communication and language environment of the
facility is accessible. If a resident wants to improve inde-
pendence in communicating health care decisions to staff
Step 3: Pretherapy Assessment members (e.g., taking medication, doctor visits), the SLP
Now that the clinician has a better understanding of must use an assessment tool that reveals barriers in the com-
the goals of the person with aphasia, some measure of per- munication environment when these exchanges occur. The
formance should be gathered as a precursor or baseline to most accessible way to collect this type of data in LTC is
therapy. Tasks during pretherapy assessment should be in- through direct observation. While this method can help a
dividualized, and tools should capture abilities and barriers clinician obtain detailed, resident-specific information, the
related to life participation in a particular domain. For quality of the data often relies on the expertise of the ob-
example, if information gathering and collaborative goal server. Inexperienced observers in LTC may want to use
setting reveal that a resident with aphasia would like to published tools to help guide observations such as the
Azios & Damico: Optimizing Life Participation in Long-Term Care 389
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
Measure of Skill in Providing Supported Conversation for an appendix that includes a checklist of criterion-referenced
Adults With Aphasia (MSC; Kagan et al., 2004) or the Prag- measures and behavioral observations.
matic Protocol (Prutting & Kirchner, 1987). Le Dorze et al.
(2000) developed the Montreal Evaluation of Communica-
tion Questionnaire for Use in Long-Term Care, which is Step 4: Therapy
designed to assess the frequency of communication acts of Intervention in line with the LPAA may address any
residents in LTC and staff members’ degree of effort required domain of the A-FROM, including impairment-focused
for efficient communication. approaches. However, due to distinct barriers and chal-
Securing independence in daily life activities is a com- lenges for people with aphasia in LTC that are associated
mon goal for residents with aphasia in LTC. For this rea- with the communication environment, participation in daily
son, it is often helpful to select a measure of participation life activities, and personal identity, therapies addressing
in conversation (MPC) or other language activity (e.g., these domains may be most valuable. As with LPAA in
reading the newspaper) prior to initiating treatment. For any setting, the focus of intervention can be on both personal
residents with greater levels of independence, the Communi- (internal) and environmental (external) factors through
cation Activities of Daily Living–Third Edition (Holland, any stage of recovery (LPAA Project Group, 2001).
Fromm, & Wozniak, 2018) can be used to assess functional Approaches targeting the communication and lan-
communication abilities across a wide array of activities. guage environment may be more heavily oriented toward
If a resident with aphasia is interested in developing more external factors. Clinicians may work toward making sign-
social relationships, clinicians may complete a social net- age, notices, and other written information in the LTC
work map (see Simmons-Mackie & Damico, 2001) that de- facility aphasia friendly by adding pictographs, simplifying
tails the quantity, type, and closeness of social contacts. syntax, adding bullets, or bolding and increasing the font
Regardless of severity or level of dependence, a measure of (Rose, Worrall, Hickson, & Hoffmann 2011). For exam-
communicative ability in conversation should preface inter- ple, an SLP may work with a resident to make menus
ventions working toward increasing compensatory strate- more aphasia friendly to increase independence in selecting
gies across communication contexts. While most clinicians foods for meals. Perhaps the most important type of inter-
lack the time and skills required to complete detailed con- vention in LTC involves training communication partners.
versation analysis, the presence and frequency of facilita- Specific techniques in LTC includes the use of individual-
tive behaviors (e.g., writing, gesturing, circumlocution) can ized communication plans (e.g., Généreux et al., 2004).
be tallied during a sample of conversation and used to in- Page and Rowles (2016) describe a communication plan as
form treatment. A few scales have been developed to cap- a one-page document specific to each resident that details
ture interactional and transactional aspects of conversation (a) strategies that staff can use to increase communication
such as the MPC (Kagan et al., 2004). Self-report measures accessibility, (b) specific behaviors that the resident uses
of participation in life situations have also been developed to communicate, and (c) a resident’s likes and dislikes.
and validated including the Communicative Effectiveness Simmons-Mackie et al. (2007) describe a training given to
Index (Lomas et al., 1989). However, SLPs must recognize multiple staff members of an LTC facility that included
many of these scales were not specifically developed for information about aphasia and hands-on experience using
persons with aphasia in LTC, and some items refer to activi- supported conversation techniques. Hickey, Bourgeois, and
ties not representative of this setting. Olswang (2004) trained volunteers on how to converse with
If the shared goal is to increase personal identity and residents with aphasia through a multimodality communi-
positive emotions postaphasia, clinicians may need to cation program. Results from these studies and others
gather measures that assess affective responses to aphasia. indicate that a variety of partners can be trained to commu-
This may be done through self-report measures of particu- nicate with residents with aphasia and partner training is
lar feelings such as confidence (Communication Confidence an important avenue for addressing the communication
Rating Scale for Aphasia; Babbitt, Heinemann, Semik, & and language environment (Simmons-Mackie, Raymer, &
Cherney, 2011). Alternatively, clinicians may select self-report Cherney, 2016).
measures that assess multiple dimensions of health care– Improving participation in daily life activities may
related quality of life but include sections on positive and involve therapy approaches that target both internal and
negative feelings after aphasia (e.g., Burden of Stroke Scale external factors. One common way to improve communi-
[Doyle et al., 2004] and Stroke and Aphasia Quality of cation abilities across multiple daily life activities is to
Life Scale [Hilari et al., 2009]). Since personal narratives improve a resident’s facilitative strategy use in conversation.
serve as an important part of identity formation (Bruner, In LTC, this typically involves bolstering multimodal
1987), baseline data on the ability to recount life experi- communication strategies (e.g., writing, pointing, gesturing)
ences before and after institutionalization and aphasia and other self-cueing strategies (e.g., circumlocution, spell-
may be beneficial. Olness, Gyger, and Thomas (2012) ing). Conversation therapy can be used to increase aware-
outline measures of referential and evaluative function that ness of strategies that are most facilitative and reduce
clinicians may want to assess in personal narratives, includ- behaviors that act as a barrier to getting a message across
ing references to activities, order of events, key background (Damico et al., 2015). Many residents with and without
information, and evaluative devices. The authors provide aphasia discuss reading as an enjoyed activity. In an LPAA
390 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
approach, clinicians may focus on providing the resident decisions, and a lack of “objective” improvement (Hersh,
access to an audio book version of a text or practice com- 2009). In LTC, the SLP will be visible in the facility after
prehension strategies during authentic reading tasks (Lynch, the resident has been discharged from speech services, caus-
Damico, Abendroth, & Nelson, 2013). Finally, group ing even more ambiguity about the discharge process. For
therapy has a long-standing history and evidence base for these reasons, SLPs in LTC must take great care in develop-
improving communication and linguistic abilities (e.g., ing strategies for discharge that underscore best practice
Elman & Berstein-Ellis, 1999), but it may also be imple- and LPAA values. As Simmons-Mackie et al. (2017) sug-
mented in LTC facilities to encourage the development of gest in the 10 best practices of effective aphasia therapists,
relationships among residents and establish a sense of SLPs should not discharge clients from services without
community. Under the new patient-driven payment model, some means of communicative needs and desires (e.g., using
SLPs can continue to utilize group therapy for residents; multimodal communication, visual supports, trained part-
however, minutes for group therapy cannot exceed more ners). Hersh (2003) discusses how clinicians “wean” clients
than 25% of the total treatment time over the course of the from services as part of the discharge process. She suggests
rehabilitation period. that clinicians use beneficial strategies for negotiation
To address personal factors, clinicians may consider purposes, including talking about discharge in advance and
creating stroke support groups within the facility. It may discussing goals with a focus on discharge from the begin-
be difficult in small facilities to begin support groups re- ning. Also, clinicians use encouraging talk when discharge
stricted to persons with aphasia. In the first author’s expe- is near, which helps to boost client’s confidence and pre-
rience of beginning a support group in LTC, it is helpful to pares them for the path toward discharge. SLPs in LTC
include all stroke survivors and discuss differences and should consider implementing these strategies when dis-
similarities between communicative and physical conse- charge is imminent. There may also be future opportunities
quences of stroke. Defining terms such as “aphasia” and sup- to re-evaluate the need for speech therapy services for a
porting stroke survivors’ ability to share their personal resident if there is a need or change in status.
journey among like-minded people can lead to positive and
empowering perspectives (Tregea & Brown, 2013). Counsel-
ing techniques such as those suggested in positive psychol- Case Study Illustrations
ogy can also be used to help build resilience and hope To better illustrate the process of implementing LPAA
(Holland & Nelson, 2020). Recently, there has been a move- in LTC, we present two case studies of long-term residents
ment toward the use of personal narratives as a medium with chronic aphasia. Each study is based on the first
for addressing identity challenges. Strong, Lagerwey, and author’s clinical experiences when she was employed as a
Shadden (2018) discuss a protocol for intervention designed staff member in LTC. Information on demographics, char-
to help a person with aphasia construct a personal narra- acteristics of aphasia, and outcomes presented in the cases
tive about life with aphasia. During the intervention, the was also obtained from facility records as a part of the
SLP works with a person with aphasia to co-construct their study of Hartwell (2015). We have assigned pseudonyms for
life story before and after aphasia through whatever com- each case and have altered some of the details for confiden-
munication means possible. Artifacts such as photographs tiality and explanatory purposes. While we no longer have
are used to help clients formulate stories, and multimodal access to standard scores on assessment batteries for the
communication strategies are explored and practiced for cases, we will provide descriptive data on characteristics and
storytelling. Results of the study indicate that the process severity of aphasia, social and medical histories, and overall
of co-constructing the story helps to support a positive view communicative functioning so readers can employ case-to-
of identity and increase hope and confidence in communi- case transfer for generalization purposes (Firestone, 1993).
cation skills.
Case 1: “Norman”
Step 5: Reassessment Norman was a 72-year-old man who was admitted
After goals have been targeted through an interven- to the LTC facility after experiencing a left hemisphere
tion approach, clinicians should reassess the resident’s abil- stroke. His medical history was remarkable for a small, re-
ities. This can be done through the same techniques used mote right hemisphere stroke, arthritis, hypertension, and
in pretherapy assessment or can represent an overall mea- atrial fibrillation. Prior to admission, Norman lived alone.
surement of the resident’s progress toward goals. In LTC, He was previously married but did not have any children.
most Medicare intermediaries require recertification every Norman graduated high school and worked odd jobs until
30 days, which may be an opportune time for reassessment. he joined the military during World War II. When Norman
SLPs working in LTC should discuss findings from the returned home from war, he moved back to his small
reassessment with the resident, family members, and routine hometown. Norman’s hobbies included playing cards, so-
care providers and work collaboratively toward goal refor- cializing with his friends, and working on cars. He fre-
mation or discharge. The decision to discharge a resident quented bars and enjoyed nightlife. Norman got into an
with chronic aphasia is often difficult due to set time limits altercation one night with a friend, and both parties sus-
to rehabilitation programs, inability to review discharge tained injuries. The police were called, and Norman was
Azios & Damico: Optimizing Life Participation in Long-Term Care 391
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
incarcerated for several years. He experienced his second was not sure of his reading ability, but he stated that he
stroke approximately ten years after his release from prison could read his menu during meals and he was able to recog-
and was admitted to the LTC facility due to inability to nize and understand signage in the facility. The goal
physically care for himself at home. Norman’s name ap- would be to increase reading efficiency and comprehension
peared on a routine screening form given to the SLP. The strategies to participate in reading activities for pleasure.
SLP conducted a cursory review of his medical chart and Pretherapy assessment included baselining reading
noted the diagnosis of stroke and aphasia and that he had performance and comprehension across a variety of tasks.
not received therapy since his initial 100 days in the facility First, probes were used from a standardized test battery to
(approximately one year prior). The SLP visited Norman identify comprehension at the single word, sentence, and
and conducted a brief interview about his current activities paragraph level. While Norman exhibited some delays, he
in the nursing home and how he felt about his ability to was able to read a sentence-level direction and follow the
communicate with others. Norman expressed that he felt command without any errors. He did make a few errors
his language had deteriorated since his admission and that when answering close-ended questions after reading exposi-
he was no longer confident speaking to others. tory paragraphs. To assess functional reading abilities,
At this point, the SLP decided to conduct a compre- the SLP conducted an analysis of Norman’s oral reading,
hensive assessment to begin to gather information across making note of low-quality changes while reading that
the A-FROM domains. This stage began with a thorough affected the meaning of the text (e.g., omitting important
chart review and a short interview with Norman’s routine words, semantic paraphasias) and any compensatory strat-
nurse aide. The SLP employed ethnographic interviewing egies that appeared to increase reading fluency (e.g., appro-
as a self-report technique to better understand strengths priate word substitution, rereading sections). The SLP
and barriers across the communicative environment, partici- kept a simple tally of low-quality changes to the text and
pation in daily life activities and social relationships, and compensatory strategies during a reading sample as an
feelings associated with aphasia. The SLP also used this objective baseline measure. A simple guide to miscue anal-
time to assess auditory comprehension and verbal expres- ysis with a template for tracking errors can be found on
sion abilities within natural conversation, noting Norman’s the National Center on Intensive Intervention at the Amer-
attempts to self-repair when he had a word-finding prob- ican Institutes for Research website.
lem and any difficulties with understanding and following Norman chose to read a book about a place he was
conversation. Based on the first stage of the assessment, stationed for World War II. The SLP provided a few op-
Norman presented with mild aphasia characterized by tions that were at an appropriate reading level, and Norman
functional auditory comprehension in conversation, intact made the selection. The first step in therapy involved in-
syntax, and word-finding problems for low-frequency words creasing accessibility to external aids that would improve
and proper nouns (especially the names of places). He often reading efficiency and comprehension. This was done
used vague words such as “thing” or “there” as a substitute through “reading ramps” (Elman & Bernstein-Ellis, 2006,
for the word that was inaccessible and had difficulty with p. 33), which included the use of chapter summaries, vocab-
pronoun reference. He paused often during conversation, ulary lists, and an audiobook version of the text (Knollman-
which often led to what he described as “speaking for” Porter, Wallace, Hux, Brown, & Long, 2015). Norman
behaviors by other residents and nurse aides (Croteau & and the SLP worked together to try out these supports while
Le Dorze, 2006). Norman described negative emotions reading to select what supports worked best and at what
associated with his aphasia. He admitted that he isolated stages of reading. Next, the SLP and Norman engaged in
himself from others and could not list a single activity that shared reading tasks that involved taking turns reading
he participated in since he was admitted to the nursing aloud to practice efficiency and comprehension strategies.
home. Even though Norman’s language difficulties were so Some strategies that Norman found most effective were
mild that many nurses did not recognize that he had apha- pacing or rereading of more complex words and sentences,
sia, he felt very poorly about himself and did not have substitution using abbreviations or simpler words, and
confidence to participate in daily life activities. skipping function words (e.g., the) to simplify grammatical
The SLP used the next session for collaborative goal complexity (Lynch et al., 2013). The SLP modeled these
setting. Since Norman’s aphasia was mild, he was able to strategies during reading and also highlighted Norman’s
participate in selecting goals with a few supportive commu- use of the strategies during sessions to increase awareness
nication techniques such as keywording and drawing of the timing and effectiveness of strategies.
(Kagan, 1998). The SLP used these tools to outline potential At reassessment, the SLP completed another analysis
ideas for goals and then facilitated a discussion about pri- of Norman’s reading abilities by tabulating the number
oritizing what was most important to address immediately. of low-quality miscues and compensatory strategies used
It was clear from Norman’s responses that participation during an authentic reading task. She also kept an inventory
in daily life activities, especially activities that would combat of the quantity and types of books that Norman was now
his boredom and loneliness, were of most importance. able to read. After several weeks of intervention, Norman
Through the discussion, Norman revealed that he wanted became interested in reading books about incarceration,
to begin to read again to learn about different topics. He being that he had been incarcerated and had received news
had not read since his aphasia and institutionalization. He that a distant cousin was now in prison. He expressed a
392 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
new desire to work toward writing letters to his distant Based on Celine’s responses on the ALA and inter-
cousin but was concerned with his writing abilities after views with staff members, there were many barriers in the
aphasia. The SLP and Norman revisited the first stages of communication and language environment and challenges
the therapy process and began working toward a new goal associated with participation in life activities (especially
of improving writing abilities to exchange simple letters conversation). The SLP used supported conversation tech-
with his relative. niques, including keywording, drawing, close-ended ques-
tions, and pictographs from the Life Interests and Values
Cards for collaborative goal setting (Haley et al., 2010;
Case 2: “Celine” Kagan, 1998). The SLP provided broad, simple goals and
Celine was a 59-year-old woman who was admitted presented them to Celine with the supports. For example,
to the LTC facility after a left middle cerebral artery stroke the SLP wrote “talking at lunch” and showed a pictograph
resulting in severe aphasia and apraxia. Celine was divorced to Celine, and she responded with “yes” or “no” with
and had three adult children and two grandchildren. Prior varying levels of repetition and emphasis. From this process,
to her stroke, she lived alone and worked as a nanny. Her it was apparent that Celine wanted to increase her ability
friends and family described her as a vivacious woman who to contribute to conversations with the women that sat
enjoyed drinking coffee and talking with friends, going to with her each day for meals.
the beauty parlor, and listening to country music. Celine’s For pretherapy assessment, the SLP needed to better
medical history was remarkable for diabetes and hyperten- understand the range of difficulties and strategies present
sion. She was uninsured at the time of her stroke, so she during Celine’s conversation and also what barriers were
received little rehabilitative services in the weeks after her present in the communication environment. Therefore, the
stroke. She was discharged to the LTC facility at approxi- SLP needed a baseline for the communication and language
mately three weeks postonset. Celine was enrolled in physi- environment and a separate baseline for participation in
cal, occupational, and speech therapy when she entered conversation. This began with two separate observations
the nursing home, but sessions were only approved for across mealtimes, using the MSC to guide observations.
30 min, three times a week. She received impairment-focused The MSC, MPC, and processes for determining scores can
speech therapy that mostly targeted her severe apraxia be accessed for free on the Aphasia Institute website. All
and was discharged approximately two months after admis- three women that Celine ate with were older than her but
sion. Since Celine had not made enough progress to care appeared more physically and cognitively independent than
for herself at home, she remained in the nursing home as a other residents. It was clear that the women had similar
long-term resident. One day, Celine was in her room visi- interests, backgrounds, and mutual acquaintances outside
bly frustrated and emotional. The SLP passed by her room, the facility. Unfortunately, Celine was not included in
noticed her crying, and entered her room to ask if she most of these conversations, and the women used unnatural
needed assistance. Celine was pointing and gesturing but talk when speaking to her (e.g., increased loudness, un-
was unable to communicate why she was upset or what natural pauses, patronizing at times). They also tended to
happened. talk over one another, multiple women speaking at the
The SLP was new to the facility and did not know same time, and would ask strings of questions to Celine
Celine but immediately recognized she had severe aphasia when she was uninvolved in conversation. The SLP used
and was unable to communicate her needs and desires. the rating scale provided in the work of Kagan et al. (2004)
Since Celine had a limited payor source, the facility was as the basis for objective goal formation. To baseline Celine’s
responsible for payment of all therapy services. The SLP conversation abilities, the SLP engaged in a 10-min conver-
requested approval from the facility for assessment and sation with Celine and took an inventory of multimodal
treatment and was granted 30-min sessions, five times a and verbal communication strategies used within the time
week, for a 30-day period. The assessment process started frame. While Celine could write and practiced writing as
with gathering broad information across the A-FROM “homework” given to her by the previous SLP, family,
domains. The SLP conducted a thorough chart review and friends, she did not employ writing during conversation.
and cursory interview with Celine’s nurse and nurse aide, At times, she used pointing and gesturing and changes to
who both worked with Celine over the past few years the frequency and intonation of “yes” and “no” during the
and shared detailed information about her abilities to com- conversation, and she occasionally repeated the SLP’s turn
municate during routine care tasks. Celine’s aphasia and to signal agreement/disagreement or to request more infor-
apraxia were severe, and although her auditory compre- mation on the topic. These strategies, while helpful, were
hension appeared only mildly impaired at the conversational not used consistently or optimally during conversation, and
level, her spontaneous expression was mostly limited to Celine remained mostly passive during the conversation.
“yes,” “no,” “and,” and “thank you.” Celine was unable For baselining and objective goal formulation, the SLP
to participate in an ethnographic interview but was able to used the rating scale provided in the work of Kagan et al.
complete most portions of the ALA. The ALA revealed and a simple frequency count of compensatory strategies in
that Celine was dissatisfied with her life after aphasia. She conversation during the 10-min sample.
had few communication partners within or outside the Therapy was initiated to target the two separate goals
nursing home and engaged in few to no conversations. for decreasing barriers in the communication environment
Azios & Damico: Optimizing Life Participation in Long-Term Care 393
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
and increasing participation in conversation. Since the communication plans helped to decrease worry and other
SLP was able to conduct sessions five times a week, three negative emotions surrounding discharge.
sessions were devoted to individualized conversation inter-
vention with Celine and two sessions were devoted to con-
versation partner training. The SLP approached the three Conclusions and Final Remarks
women at the facility and asked if they would be interested Residents with aphasia in LTC often experience sig-
in learning how to better communicate with Celine. Two nificant barriers associated with the communication and
of the three agreed to learn supported conversation tech- language environment, participation in life situations in-
niques. They expressed that they understood that Celine cluding conversation and the development of relationships,
had a stroke but did not understand the word “aphasia” or and renegotiation of identity after aphasia. Implementing
what it meant. It is important to note that these residents the LPAA in these settings is critical in helping residents
were considered “high functioning” when compared to improve social participation, reengagement in life after
other residents with various cognitive and psychological aphasia, and overall quality of life. Published assessment and
disorder. They were institutionalized because they were intervention tools are appropriate for residents with aphasia
widowed and had various physical ailments that precluded in LTC and can be used during the therapeutic process to
them from driving and living independently at home. The target meaningful, client-centered goals. While many chal-
SLP included both women and Celine in the sessions devoted lenges remain for SLPs in LTC, clinicians must recognize
to partner training. Introductory sessions involved simple that they have a critical role in advocating for residents
explanations of aphasia and the strategies that Celine may with aphasia to receive the best possible care and helping
use to communicate. The residents were taught three basic to change the organizational culture in LTC. The LPAA
strategies: using yes/no questions, slowing rate by pausing in and A-FROM provide a framework for SLPs to begin to
between phrases, and acknowledging when Celine was shape the structure of assessment and intervention in this
frustrated and unable to get her message across. Sessions setting and promote positive and lasting change for residents
involved talking about the strategies, providing models, and with aphasia.
practicing the strategies with feedback. During the individ-
ual sessions with Celine, the SLP implemented a conversa-
tion intervention that worked toward increasing awareness Acknowledgments
of facilitative strategy use (writing, iconic gesturing, verbal We would like to thank the staff members and residents that
repetition) through practice in authentic conversation, self- we have had the pleasure of working with during our time in
evaluation, and feedback. See Damico et al. (2015) for a long-term care facilities. These experiences continue to inspire us
complete description of the approach. in our work and have taught us important clinical lessons that we
At the end of the 30 days, the LTC facility required hope to pass on to the next generation of clinicians in this setting.
a reassessment. The SLP observed mealtimes using the
MSC to track the progress of Celine’s communication part- References
ners and collected a conversation sample with frequency
Azios, J. H., Damico, J. S., & Roussel, N. (2018). Communicative
counts of targeted compensatory strategies. While there
accessibility in aphasia: An investigation of the interactional
were slight improvements in strategy deployment for both context of long-term care facilities. American Journal of Speech-
the partners and Celine, conversation during meals was not Language Pathology, 27(4), 1474–1490.
completely accessible for Celine. Celine expressed that, Babbitt, E. M., Heinemann, A. W., Semik, P., & Cherney, L. R.
although she felt better about her relationship with the women, (2011). Psychometric properties of the Communication Confi-
she remained unhappy with her level of participation in dence Rating Scale for Aphasia (CCRSA): Phase 2. Aphasiology,
conversation. The SLP provided the facility with the objec- 25(6–7), 727–735.
tive data taken during the treatment period, requested ad- Baier, C. K., Hoepner, J. K., & Sather, T. W. (2018). Exploring
ditional time to continue intervention, and was granted snapchat as a dynamic capture tool for social networking in
persons with aphasia. Aphasiology, 32(11), 1336–1359.
another 30 days of treatment. The SLP continued the plan
Berg, K., Askim, T., Balandin, S., Armstrong, E., & Rise, M. B.
of care and was required to discharge Celine after the (2017). Experiences of participation in goal setting for people
final 30 days. Prior to discharge, the SLP created a com- with stroke-induced aphasia in Norway. A qualitative study.
munication plan for the two residents involved in partner Disability and Rehabilitation, 39(11), 1122–1130.
training and also nurse aides working with Celine. The plan Brown, K., Worrall, L. E., Davidson, B., & Howe, T. (2012). Living
detailed effective partner strategies, Celine’s primary com- successfully with aphasia: A qualitative meta-analysis of the
pensatory strategies for getting a message across, and what perspectives of individuals with aphasia, family members, and
context the strategies appeared most beneficial. For exam- speech-language pathologists. International Journal of Speech-
ple, while writing was a strategy that Celine could use effec- Language Pathology, 14(2), 141–155.
Brownie, S., & Nancarrow, S. (2013). Effects of person-centered
tively, she felt uncomfortable using it in more public care on residents and staff in aged-care facilities: A systematic
spaces or in group conversations. The discharge process review. Clinical Interventions in Aging, 8, 1–10.
was difficult for Celine since she did not feel that she had Bruner, J. (1987). Life as narrative. Social Research, 54, 11–32.
reached her desired level of performance in life participa- Bryan, K., Axelrod, L., Maxim, J., Bell, L., & Jordan, L. (2002).
tion. However, advance discussions and the creation of Working with older people with communication difficulties:
394 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
An evaluation of care worker training. Aging & Mental Health, Hemmelgarn, A. L., Glisson, C., & James, L. R. (2006). Organiza-
6(3), 248–254. tional culture and climate: Implications for services and in-
Croteau, C., & Le Dorze, G. (2006). Overprotection, “speaking terventions research. Clinical Psychology: Science and Practice,
for”, and conversational participation: A study of couples with 13(1), 73–89.
aphasia. Aphasiology, 20(2–4), 327–336. Hersh, D. (2003). “Weaning” clients from aphasia therapy: Speech
Cutter, M., & Polovoy, C. (2014). Under pressure. The ASHA pathologists’ strategies for discharge. Aphasiology, 17(11),
Leader, 19, 36–44. 1007–1029.
Damico, J., Tetnowski, J., Lynch, K., Hartwell, J., Weill, C., Hersh, D. (2009). Breaking the connection: Why is it so difficult
Heels, J., & Simmons-Mackie, N. (2015). Facilitating authentic to talk about discharge with our clients with aphasia? Interna-
conversation: An intervention employing principles of construc- tional Journal of Speech-Language Pathology, 11(2), 147–154.
tivism and conversation analysis. Aphasiology, 29(3), 400–421. Hersh, D., Worrall, L., Howe, T., Sherratt, S., & Davidson, B.
Douglas, N. F. (2016). Organizational context associated with (2012). SMARTER goal setting in aphasia rehabilitation. Apha-
time spent evaluating language and cognitive-communicative siology, 26(2), 220–233.
impairments in skilled nursing facilities: Survey results within an Hickey, E., Bourgeois, M., & Olswang, L. (2004). Effects of train-
implementation science framework. Journal of Communication ing volunteers to converse with nursing home residents with
Disorders, 60, 1–13. aphasia. Aphasiology, 18(5–7), 625–637.
Douglas, N. F., & Hickey, E. (2015). Creating positive environ- Hilari, K., Lamping, D., Smith, S. C., Northcott, S., Lamb, A., &
ments in skilled nursing facilities to support best practice imple- Marshall, J. (2009). Psychometric properties of the Stroke and
mentation: An overview and practical suggestions. Seminars in Aphasia Quality of Life Scale (SAQOL-39) in a generic stroke
Speech and Language, 36(3), 167–178. population. Clinical Rehabilitation, 236(6), 544–557.
Doyle, P. J., McNeil, M. R., Mikolic, J. M., Prieto, L., Hula, W. D., Holland, A. L., Fromm, D., & Wozniak, L. (2018). Communication
Lustig, A. P., . . . Elman, R. J. (2004). The Burden of Stroke Activities of Daily Living–Third Edition. Pro Ed.
Scale (BOSS) provides valid and reliable score estimates of Holland, A. L., & Nelson, R. (2020). Counseling in communication
functioning and well-being in stroke survivors with and with- disorders: A wellness perspective (3rd ed.). Plural.
out communication disorders. Journal of Clinical Epidemiology, Howe, T. J., Worrall, L. E., & Hickson, L. M. H. (2004). What
57, 997–1007. is an aphasia-friendly environment? Aphasiology, 18(11),
Elman, R. J., & Bernstein-Ellis, E. (1999). The efficacy of group 1015–1037.
communication treatment in adults with chronic aphasia. Journal Hughes, J. C., Bamford, C., & May, C. (2008). Types of centred-
of Speech, Language, and Hearing Research, 42(2), 411–419. ness in health care: Themes and concepts. Medicine, Health
Elman, R. J., & Bernstein-Ellis, E. (2006). Aphasia book clubs: Care and Philosophy, 11(4), 455–463.
Making the connection. Stroke Connection, 32–33. Isaksen, J. (2018). “Well, you are the one who decides”: Attempting
Ferguson, A. (1996). Describing competence in aphasic/normal shared decision making at the end of aphasia therapy.
conversation. Clinical Linguistics & Phonetics, 10(1), 55–63. Topics in Language Disorders, 38(2), 126–142.
Firestone, W. A. (1993). Alternative arguments for generalizing from Kagan, A. (1998). Supported conversation for adults with aphasia:
data as applied to qualitative research. Educational Researcher, Methods and resources for training conversation partners.
22(4), 16–23. https://doi.org/10.3102/0013189X022004016 Aphasiology, 12(9), 816–830.
Frattali, C. M., Thompson, C. K., Holland, A. L., Wohl, C. B., Kagan, A., Simmons-Mackie, N., Rowland, A., Huijbregts, M.,
Wenck, C. J., Slater, S. C., & Paul, D. (2017). American Shumway, E., McEwen, S., . . . Sharp, S. (2008). Counting
Speech-Language-Hearing Association Functional Assessment what counts: A framework for capturing real-life outcomes of
of Communication Skills for Adults. American Speech-Language- aphasia intervention. Aphasiology, 22(3), 258–280.
Hearing Association. Kagan, A., Simmons-Mackie, N., Victor, J. C., Carling-Rowland, A.,
Généreux, S., Julien, M., Larfeuil, C., Lavoie, V., Soucy, O., Hoch, J., & Huijbregts, M. (2011). Assessment for Living With
& Le Dorze, G. (2004). Using communication plans to facili- Aphasia (ALA). Aphasia Institute.
tate interactions with communication-impaired persons residing Kagan, A., Winckel, J., Black, S., Duchan, J. F., Simmons-Mackie,
in long-term care institutions. Aphasiology, 18(12), 1161–1175. N., & Square, P. (2004). A set of observational measures for
Goffman, E. (1961). Asylums: Essays on the social situation of rating support and participation in conversation between adults
mental patients and other inmates. Anchor Books. with aphasia and their conversation partners. Topics in Stroke
González-Fernández, M., Christian, A. B., Davis, C., & Hillis, A. E. Rehabilitation, 11(1), 67–83.
(2013). Role of aphasia in discharge location after stroke. Archives Knollman-Porter, K., Wallace, S. E., Hux, K., Brown, J., & Long,
of Physical Medicine and Rehabilitation, 94(5), 851–855. C. (2015). Reading experiences and use of supports by people
Haley, K. L., Cunningham, K. T., Barry, J., & de Riesthal, M. with chronic aphasia. Aphasiology, 29(12), 1448–1472.
(2019). Collaborative goals for communicative life participation Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A., &
in aphasia: The FOURC model. American Journal of Speech- Zoghaib, C. (1989). The Communicative Effectiveness Index:
Language Pathology, 28(1), 1–13. Development and psychometric evaluation of a functional
Haley, K. L., Womack, J. L., Harmon, T. G., & Williams, S. W. communication measure for adult aphasia. Journal of Speech
(2015). Visual analog rating of mood by people with aphasia. and Hearing Disorders, 54(1), 113–124.
Topics in Stroke Rehabilitation, 22(4), 239–245. Le Dorze, G., Julien, M., Genereux, S., Larfeuil, C., Navennec, C.,
Haley, K. L., Womack, J., Helm-Estabrooks, N., Caignon, D., & Laporte, D., & Champagne, C. (2000). The development of a
McCulloch, K. L. (2010). The life interest and values cards. procedure for the evaluation of communication occurring be-
University of North Carolina Department of Allied Health tween residents in long-term care and their caregivers. Aphasiol-
Sciences. ogy, 14(1), 17–51.
Hartwell, J. (2015). Access denied: An investigation of the impact Long, E., Azios, J. H., & Richings, S. (2019). Exploring nurse aide
of aphasia on social inclusion in long-term care facilities (Doctoral perspectives on caring for persons with dementia. Annals of
dissertation). ProQuest (Accession No. 10002394). Long-Term Care, 27(1), 19–24.
Azios & Damico: Optimizing Life Participation in Long-Term Care 395
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
SIG 2 Neurogenic Communication Disorders
LPAA Project Group. (2001). Life Participation Approach to Simmons-Mackie, N. N., & Damico, J. S. (1996b). Accounting for
Aphasia: A statement of values for the future. In R. Chapey (Ed.), handicaps in aphasia: Communicative assessment from an
Language intervention strategies in aphasia and related neurogenic authentic social perspective. Disability and Rehabilitation,
communication disorders (4th ed., pp. 235–245). Lippincott 18(11), 540–549.
Williams & Wilkins. Simmons-Mackie, N. N., & Damico, J. S. (2001). Intervention
Lynch, K. E., Damico, J. S., Abendroth, K. J., & Nelson, R. L. outcomes: A clinical application of qualitative methods. Topics
(2013). Reading performance subsequent to aphasia: Strategies in Language Disorders, 22(1), 21–36.
applied during authentic reading. Aphasiology, 27, 723–739. Simmons-Mackie, N. N., Kagan, A., O’Neill Christie, C., Huijbregts,
Moyle, W., Venturto, L., Griffiths, S., Grimbeek, P., McAllister, M., McEwen, S., & Willems, J. (2007). Communicative access
M., Oxlade, D., & Murfield, J. (2011). Factors influencing and decision making for people with aphasia: Implementing sus-
quality of life for people with dementia: A qualitative perspec- tainable healthcare systems change. Aphasiology, 21(1), 39–66.
tive. Aging & Mental Health, 15(8), 970–977. Simmons-Mackie, N. N., Kagan, A., Victor, J. C., Carling-Rowland,
Murphy, J., & Boa, S. (2012). Using the WHO-ICF with talking A., Mok, A., Hoch, J. S., . . . Streiner, D. L. (2014). The Assess-
mats to enable adults with long-term communication difficulties ment for Living With Aphasia: Reliability and construct
to participate in goal setting. Augmentative and Alternative validity. International Journal of Speech-Language Pathology,
Communication, 28(1), 52–60. 16(1), 82–94.
Nguyen, V. Q., PrvuBettger, J., Guerrier, T., Hirsch, M. A., Simmons-Mackie, N. N., Raymer, A., & Cherney, L. R. (2016). Com-
Thomas, J. G., Pugh, T. M., & Rhoads, C. F. (2015). Factors munication partner training in aphasia: An updated systematic
associated with discharge to home versus discharge to insti- review. Archives of Physical Medicine and Rehabilitation, 97(12),
tutional care after inpatient stroke rehabilitation. Archives of 2202–2221.
Physical Medicine and Rehabilitation, 96(7), 1297–1303. Simmons-Mackie, N. N., Worrall, L., Murray, L. L., Enderby, P.,
Olness, G. S., Gyger, J., & Thomas, K. (2012). Analysis of narra- Rose, M. L., Paek, E. J., & Klippi, A. (2017). The top ten: Best
tive functionality: Toward evidence-based approaches in practice recommendations for aphasia. Aphasiology, 31(2),
managed care settings. Seminars in Speech and Language, 33(1), 131–151.
55–67. Strong, K. A., Lagerwey, M. D., & Shadden, B. B. (2018). More
Page, C. G., & Rowles, G. D. (2016). “It doesn’t require much ef- than a story: My life came back to life. American Journal of
fort once you get to know them”: Certified nursing assistants’ Speech-Language Pathology, 27(Suppl. 1),, 464–476.
views of communication in long-term care. Journal of Geronto- Swinburn, K., Porter, G., & Howard, D. (2004). Comprehensive
logical Nursing, 42(4), 42–51. aphasia test. Psychology Press.
Parr, S. (2007). Living with severe aphasia: Tracking social exclu- Thomas, W. H., & Johnson, C. (2003). Elderhood in Eden. Topics
sion. Aphasiology, 21(1), 98–123. in Geriatric Rehabilitation, 19(4), 282–290.
Porch, B. (1967). Porch index of communicative ability. Consulting Tregea, S., & Brown, K. (2013). What makes a successful peer-led
Psychologists Press. aphasia support group? Aphasiology, 27(5), 581–598.
Prutting, C. A., & Kirchner, D. M. (1987). A clinical appraisal of van Dijck-Heinen, C. J. M. L., Wouters, E. J. M., Janssen, B. M.,
the pragmatic aspects of language. Journal of Speech and Hearing & van Hoof, J. (2014). The environmental design of residential
Disorders, 52(2), 105–119. care facilities: A sense of home through the eyes of nursing
Rose, T. A., Worrall, L. E., Hickson, L. M., & Hoffmann, T. C. home residents. International Journal for Innovative Research
(2011). Aphasia friendly written health information: Content in Science and Technology, 1(4), 57–69.
and design characteristics. International Journal of Speech- Villar, F., & Serrat, R. (2017). Changing the culture of long-term
Language Pathology, 13(4), 335–347. care through narrative care: Individual, interpersonal, and
Saldert, C., Bartonek-Åhman, H., & Bloch, S. (2018). Interaction institutional dimensions. Journal of Aging Studies, 40, 44–48.
between nursing staff and residents with aphasia in long-term Wallace, S. J., Worrall, L., Rose, T., Le Dorze, G., Cruice, M.,
care: A mixed method case study. Nursing Research and Prac- Isaksen, J., . . . Gauvreau, C. A. (2017). Which outcomes are
tice, Article ID 9418692, 1–11. most important to people with aphasia and their families? An
Schuell, H., Jenkins, J. J., & Jimenez-Pabon, E. (1964). Aphasia international nominal group technique study framed within
in adults: Diagnosis, prognosis, & treatment. Hoeber Medical the ICF. Disability and Rehabilitation, 39(14), 1364–1379.
Division, Harper. Westby, C. (1990). Ethnographic interviewing: Asking the right
Shier, V., Khodyakov, D., Cohen, L. W., Zimmerman, S., & Saliba, questions to the right people in the right ways. Journal of Child-
D. (2014). What does the evidence really say about culture hood Communication Disorders, 13, 101–112.
change in nursing homes? The Gerontologist, 54(Suppl. 1),, World Health Organization. (2001). International classification for
S6–S16. functioning, disability and health (ICF).
Simmons-Mackie, N. N. (2008). Social approaches to aphasia in- Worrall, L., Brown, K., Cruice, M., Davidson, B., Hersh, D., Howe,
tervention. In R. Chapey (Ed.), Language intervention strategies T., & Sherratt, S. (2010). The evidence for a life-coaching
in aphasia and related neurogenic communication disorders approach to aphasia. Aphasiology, 24(4), 497–514.
(5th ed., pp. 290–318). Lippincott Williams & Wilkins. Worrall, L., Sherratt, S., & Papathanasiou, I. (2017). Therapy ap-
Simmons-Mackie, N. N., & Damico, J. S. (1996a). The contribution proaches in aphasia. In I. Papathanasiou & P. Coppens (Eds.),
of discourse markers to communicative competence in aphasia. Aphasia and related neurogenic communication disorders (2nd ed.,
American Journal of Speech-Language Pathology, 5(1), 37–43. pp. 109–127). Jones & Bartlett Learning.
396 Perspectives of the ASHA Special Interest Groups • Vol. 5 • 384–396 • April 2020
Downloaded from: https://pubs.asha.org 88.15.111.91 on 11/24/2021, Terms of Use: https://pubs.asha.org/pubs/rights_and_permissions
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Guidelines Based On VDI 6022 PDFDocument7 pagesGuidelines Based On VDI 6022 PDFbauer_mendoza3510100% (2)
- YCC Broad Brush Risk AssessmentDocument250 pagesYCC Broad Brush Risk AssessmentMamadou ThioyeNo ratings yet
- PainDocument14 pagesPainAmer Abdulla SachitNo ratings yet
- AerobicsDocument3 pagesAerobicsjohn kevin pascuaNo ratings yet
- Revised Teaching Plan Group 2 BSN Y2 11Document2 pagesRevised Teaching Plan Group 2 BSN Y2 11PagodNo ratings yet
- 50 in 50 PDFDocument110 pages50 in 50 PDFHardyNo ratings yet
- Clinical Exam of The Psychiatric PX HX MSE Signs Symptoms Modified For Senior Clerks 2021Document139 pagesClinical Exam of The Psychiatric PX HX MSE Signs Symptoms Modified For Senior Clerks 2021Rakesh KumarNo ratings yet
- Uts FinalsDocument9 pagesUts Finalsmaxi dmNo ratings yet
- Necropsical DiagnosisDocument372 pagesNecropsical Diagnosistataru lauraNo ratings yet
- I. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationDocument2 pagesI. Nursing Care Plan Assessment Diagnosis Planning Interventions Rationale EvaluationBryan Andrew GonzalesNo ratings yet
- OET Speaking Course - Pocketbook: Question But Limits The Scope)Document5 pagesOET Speaking Course - Pocketbook: Question But Limits The Scope)Norman Argie Nofianto100% (1)
- READYMIX Safety Data SheetDocument9 pagesREADYMIX Safety Data Sheetalbarajeel forwarding001No ratings yet
- Case Study On Preterm LaborDocument81 pagesCase Study On Preterm Laborkarl montanoNo ratings yet
- BAB I SomatoformDocument3 pagesBAB I SomatoformDewiRekmawatiPradaswariNo ratings yet
- Área C Ingeniería: Simulacro Virtual Acem Semestral - Repaso San Marcos 2021-IDocument26 pagesÁrea C Ingeniería: Simulacro Virtual Acem Semestral - Repaso San Marcos 2021-IPERCY VITON DIAZNo ratings yet
- OASIS Item Guidance Patient History & Diagnoses Oasis ItemDocument20 pagesOASIS Item Guidance Patient History & Diagnoses Oasis ItembiskwetNo ratings yet
- Introduction To Pharmacology For Nursing StudentsDocument4 pagesIntroduction To Pharmacology For Nursing StudentsConrad TarihoranNo ratings yet
- Increase Height and Grow Taller Using Brain Wave Binaural Beats - Natural Height GrowthDocument12 pagesIncrease Height and Grow Taller Using Brain Wave Binaural Beats - Natural Height GrowthIsidro P. Buquiron100% (1)
- The Accuracy of Fibroscan in A Real World StudyDocument2 pagesThe Accuracy of Fibroscan in A Real World StudyRaeni Dwi PutriNo ratings yet
- Download pdf Case Studies In Veterinary Immunology 1St Edition Laurel Gershwin Author ebook full chapterDocument53 pagesDownload pdf Case Studies In Veterinary Immunology 1St Edition Laurel Gershwin Author ebook full chapterjaime.currie230100% (2)
- Fetal EchocardiographyDocument3 pagesFetal EchocardiographypolygoneNo ratings yet
- Trainee Train Driver: Information PackDocument21 pagesTrainee Train Driver: Information PackDean ArcherNo ratings yet
- Incidence of Dry Socket After Third Molar ExtractionDocument2 pagesIncidence of Dry Socket After Third Molar ExtractionI Gusti Ayu WulanNo ratings yet
- Shangrila 590 User ManualDocument91 pagesShangrila 590 User ManualTuchilo ViorelNo ratings yet
- Marine Placenta: Anti-Aging Type I Collagen SynthesisDocument1 pageMarine Placenta: Anti-Aging Type I Collagen Synthesisonald lumowaNo ratings yet
- OSCE Tool For Improving B. Sc. Nursing Students' Antenatal, ExaminationDocument12 pagesOSCE Tool For Improving B. Sc. Nursing Students' Antenatal, ExaminationIOSRjournalNo ratings yet
- Pengaruh Brain Gym Dan Resistance Exercise Pada LaDocument5 pagesPengaruh Brain Gym Dan Resistance Exercise Pada LaTiur Theresia SitorusNo ratings yet
- Insulin and Oral Hypoglycemic DrugsDocument45 pagesInsulin and Oral Hypoglycemic DrugsRamadi PrameelaNo ratings yet
- Skin Cancer: Dedicated To: Carlos Garcia MD Dermatology at OuhscDocument44 pagesSkin Cancer: Dedicated To: Carlos Garcia MD Dermatology at OuhscabrarashrafNo ratings yet
- Medical and HealthDocument16 pagesMedical and HealthMUTHUMUNEESH WARANNo ratings yet