Professional Documents
Culture Documents
Post Cardiac Arrest
Uploaded by
Althea AlcalaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Post Cardiac Arrest
Uploaded by
Althea AlcalaCopyright:
Available Formats
POST CARDIAC ARREST CARE
Alcala Althea D. - BSN 4A
A major component of advanced life support is post cardiac arrest care. The majority of fatalities occur
during the first 24 hours of cardiac arrest. (AHA 2010)
Post cardiac arrest care has the potential to significantly reduce early mortality due to hemodynamic
instability as well as later morbidity and death due to multiorgan failure and brain damage.
Post Cardiac Arrest Care Algorithm is as follows:
➔ First is to verify Return of Spontaneous Circulation (ROSC). When circulation persists and cardiac
resuscitation has stopped for at least 20 minutes, someone is said to have maintained
restoration of spontaneous circulation. Cardiopulmonary resuscitation and defibrillation can be
used to restore spontaneous circulation.
➔ Second is to maintain a patent airway. Consider or include endotracheal tubing and provide 10
breaths per minute. An ETT can help in keeping the airway open in order to give oxygen,
medicine, or anesthesia, it also supports breathing.
➔ Next is to titrate the oxygen to maintain a PETCO2 of 35-40 mm Hg using a quantitative
waveform capnography. Waveform capnography is the continuous quantitative measurement of
exhaled carbon dioxide. (CO2 ). CO2 concentration is displayed graphically as a capnogram
(waveform) representing CO2. If there is no access to a waveform capnography machine, titrate
the oxygen to keep the oxygen saturation 92% to 98%
➔ Proceed to securing an IV line for administration of medications. Maintain systolic blood
pressure above 90 mm Hg and/or mean arterial pressure above 65 mm Hg. I f the patient has a
low blood pressure you can consider either or all of the following:
- Giving 1 to 2 liters of saline or Ringer’s lactate IV fluid
- Starting an epinephrine IV or a dopamine IV infusion
- For extremely low systolic blood pressure, consider giving norepinephrine
- Consider norepinephrine for extremely low systolic blood pressure.
(Depend on what the physician has ordered)
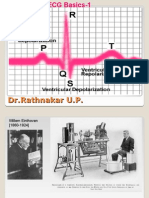
➔ Rule out myocardial infarction through obtaining a 12-lead ECG. If MI is suspected, a
percutaneous coronary intervention (PCI) is considered which uses a catheter (a thin flexible
tube) to place a small structure called a stent to open up blood vessels in the heart that have
been narrowed.
➔ Next is to determine if the patient is comatose.
◆ If the patient is in comatose:
● Keep the body temp 32-36°C for 24 hours initially (Target temperature).
● Obtain an EEG monitoring to rule out nonconvulsive seizures and to give
anticonvulsants if seizure is present
● Obtain head CT to assess cerebral edema which is common in comatose patient,
post cardiac arrest
● Maintain oxygen, glucose, carbon dioxide, etc.to maintain adequate oxygenation
and minimize fraction of inspired oxygenation
● Avoid barotrauma which is an injury to the body because of changes in
barometric (air) or water pressure.
◆ If the patient is awake:
● Maintain oxygen, glucose, carbon dioxide, etc.
● Avoid barotrauma
It is also possible to perform the following:
Therapeutic Hypothermia
● Recommended for comatose individuals with the return of spontaneous circulation after a
cardiac arrest event.
● Individuals should be cooled to 89.6 to 93.2 degrees F (32 to 36 degrees C) for at least 24 hours.
Neurologic Care
● Neurologic assessment is key, especially when withdrawing care (i.e., brain death) to decrease
false-positive rates. Specialty consultation should be obtained to monitor neurologic signs and
symptoms throughout the post-resuscitation period.
Use of Vasoactive Drugs After Cardiac Arrest
● Vasoactive drugs may be administered after ROSC to support cardiac output, especially blood
flow to the heart and brain. Drugs may be selected to improve heart rate (chronotropic effects),
myocardial contractility (inotropic effects), or arterial pressure (vasoconstrictive effects), or to
reduce afterload (vasodilator effects)
● Common Vasoactive drugs include Epinephrine, Norepinephrine, Phenylephrine Dopamine,
Dobutamine, Milrinone
You might also like
- CardiologyDocument62 pagesCardiologysee yinNo ratings yet
- Lippincott 39 S Anesthesia Review 1001 Questions A PDFDocument429 pagesLippincott 39 S Anesthesia Review 1001 Questions A PDFPeter Kazarin50% (2)
- Chan, Johnson - TreatmentGuidelines PDFDocument0 pagesChan, Johnson - TreatmentGuidelines PDFBogdan CarabasNo ratings yet
- Approach To The Adult Patient With Syncope in The Emergency DepartmentDocument26 pagesApproach To The Adult Patient With Syncope in The Emergency DepartmentVinicius DumontNo ratings yet
- Hepatic Encephalopathy and ComaDocument19 pagesHepatic Encephalopathy and ComaJas Castro JoveroNo ratings yet
- Vitamin E - Dr. Wilfrid E. Shute's Complete Updated Vi - Shute, Wilfrid E., 1907Document236 pagesVitamin E - Dr. Wilfrid E. Shute's Complete Updated Vi - Shute, Wilfrid E., 1907Anonymous gwFqQcnaX100% (2)
- Pacing Week PresentationsDocument54 pagesPacing Week PresentationsjoejenningsNo ratings yet
- Feb 09 Harvey Diamond Fit 4 Life)Document4 pagesFeb 09 Harvey Diamond Fit 4 Life)bethany50% (2)
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- Swan Ganz CathetersDocument27 pagesSwan Ganz CatheterschadchimaNo ratings yet
- Q: Characterize The Different Types of Pacemaker. Explain The Various Steps of PacingDocument4 pagesQ: Characterize The Different Types of Pacemaker. Explain The Various Steps of PacingKRUPALITHAKKAR100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- MVR CabgDocument57 pagesMVR CabgRoshani sharmaNo ratings yet
- Capnography and Its ApplicationsDocument37 pagesCapnography and Its ApplicationsTraceNo ratings yet
- Necrotizing Otitis 2022Document20 pagesNecrotizing Otitis 2022asmashNo ratings yet
- CABGDocument3 pagesCABGprofarmahNo ratings yet
- DR Lila - Patient Preparation For Emergencies Surgeries - New 11012017Document37 pagesDR Lila - Patient Preparation For Emergencies Surgeries - New 11012017bloadyroar100% (1)
- Management of Shock: Role of Inotropic & Vasoactive DrugsDocument50 pagesManagement of Shock: Role of Inotropic & Vasoactive DrugsbajaocNo ratings yet
- Major Haemorrhage ProtocolsDocument3 pagesMajor Haemorrhage ProtocolsleicesterbugNo ratings yet
- Management of The EVDDocument7 pagesManagement of The EVDplethoraldork100% (1)
- Global MigrationDocument31 pagesGlobal MigrationAlthea AlcalaNo ratings yet
- Wide QRS Complex TachyarrhythmiaDocument36 pagesWide QRS Complex TachyarrhythmiaMaruliNo ratings yet
- Seminar On Hemodynamic Monitoring: BY UMA Iind Year MSC NursingDocument52 pagesSeminar On Hemodynamic Monitoring: BY UMA Iind Year MSC NursingAyen AlingNo ratings yet
- 29744226: Cerebral Pathophysiology in Extracorporeal Membrane Oxygenation Pitfalls in Daily Clinical ManagementDocument11 pages29744226: Cerebral Pathophysiology in Extracorporeal Membrane Oxygenation Pitfalls in Daily Clinical ManagementEward Rod SalNo ratings yet
- How-to Manual for Pacemaker and ICD Devices: Procedures and ProgrammingFrom EverandHow-to Manual for Pacemaker and ICD Devices: Procedures and ProgrammingNo ratings yet
- Gap Co2 Cocc 2018Document9 pagesGap Co2 Cocc 2018Cesar Rivas CamposNo ratings yet
- FinaDocument6 pagesFinaPablo Sure20% (5)
- Perioperative Cardiovascular Evaluation For Noncardiac SurgeryDocument46 pagesPerioperative Cardiovascular Evaluation For Noncardiac SurgeryErinne DefrianiNo ratings yet
- This Study Resource Was: Cardiogenic ShockDocument5 pagesThis Study Resource Was: Cardiogenic ShockShyla Manguiat100% (1)
- ARDSnet Protocols PDFDocument2 pagesARDSnet Protocols PDFvbfisioNo ratings yet
- Initial Assessment and ManagementDocument8 pagesInitial Assessment and ManagementAlvin De LunaNo ratings yet
- Cardiac ArrestDocument49 pagesCardiac Arrestpraveenkumar biradarNo ratings yet
- 2 EsiDocument23 pages2 EsizianaNo ratings yet
- Post-Cardiac Arrest Management in Adults - UpToDateDocument34 pagesPost-Cardiac Arrest Management in Adults - UpToDatehatsune100% (1)
- Conducting A: Literature SearchDocument32 pagesConducting A: Literature SearchSolehah OmarNo ratings yet
- FAQs Catheter-Associated Urinary Tract InfectionDocument1 pageFAQs Catheter-Associated Urinary Tract InfectioncateterdoblejotaNo ratings yet
- Ivc FilterDocument15 pagesIvc FilterashishNo ratings yet
- Care of Patient With TPM Slide PresentationDocument16 pagesCare of Patient With TPM Slide PresentationirzehronNo ratings yet
- Selected Nursing Diagnoses and Interventions For Patients With DysrhythmiasDocument19 pagesSelected Nursing Diagnoses and Interventions For Patients With Dysrhythmiaslanie_jecielNo ratings yet
- Cardiopulmonary Bypass: Dr. Ravi Gadani MS, FmasDocument24 pagesCardiopulmonary Bypass: Dr. Ravi Gadani MS, FmasRaviNo ratings yet
- Nursing Management of Mechanically Ventilated PatientsDocument179 pagesNursing Management of Mechanically Ventilated PatientsSourabh AlawaNo ratings yet
- Cardiopulmonary BypassDocument62 pagesCardiopulmonary BypassNidya Putri100% (1)
- Isbi Practice Guidelines For Burn Care Part 2 2018 PDFDocument90 pagesIsbi Practice Guidelines For Burn Care Part 2 2018 PDFAstri SuyataNo ratings yet
- Supraventricular TachycardiaDocument9 pagesSupraventricular TachycardiaclubsanatateNo ratings yet
- CPRDocument4 pagesCPRjeetNo ratings yet
- Baska MaskDocument8 pagesBaska MaskAnish H DaveNo ratings yet
- Emergency Drug (Finale)Document49 pagesEmergency Drug (Finale)SN. CaR67% (3)
- Blood Gas Analysis For Bedside DiagnosisDocument6 pagesBlood Gas Analysis For Bedside DiagnosisMuhamad Wirawan AdityoNo ratings yet
- Cardiac SurgeryDocument27 pagesCardiac SurgeryReeti Singh100% (1)
- Coronary Artery Bypass Graft Report NCM 118Document23 pagesCoronary Artery Bypass Graft Report NCM 118Vhince Norben PiscoNo ratings yet
- Hepatic EncephalopathyDocument21 pagesHepatic EncephalopathyAnonymous n3qy0JdCgNo ratings yet
- Contrast EchocardiographyDocument54 pagesContrast EchocardiographySruthiNo ratings yet
- A Guide To ECG Reporting For Year 3 Medical StudentsDocument2 pagesA Guide To ECG Reporting For Year 3 Medical StudentscsngiuNo ratings yet
- 8.the Atls ProtocolDocument57 pages8.the Atls ProtocolReuben DutiNo ratings yet
- Pleural Fluid AnalysisDocument15 pagesPleural Fluid AnalysisNatalie Sarah MoonNo ratings yet
- Holter MonitoringDocument19 pagesHolter Monitoringomotola Ayobundle-oyewo MA206100% (1)
- Acute Treatment of Hypocalcaemia (Adults)Document2 pagesAcute Treatment of Hypocalcaemia (Adults)Ahed WarwarNo ratings yet
- HBP C315HIS Implant Procedure-eLearnDocument35 pagesHBP C315HIS Implant Procedure-eLearnRichiNo ratings yet
- Arterial LinesDocument9 pagesArterial LinesRei IrincoNo ratings yet
- Nervous System AlterationsDocument45 pagesNervous System AlterationsMajesty ParkerNo ratings yet
- Coronary Artery Bypass SurgeryDocument12 pagesCoronary Artery Bypass SurgeryCarlos Eduardo Quisse SánchezNo ratings yet
- AclsDocument4 pagesAclsAnusha Verghese100% (1)
- ECG Basics 1Document24 pagesECG Basics 1Dr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- Anaphylaxis CEACCP 2004Document3 pagesAnaphylaxis CEACCP 2004kuruppukarlNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
- Practice Essentials: Signs and SymptomsDocument17 pagesPractice Essentials: Signs and Symptomsdwi rizky kurniatiNo ratings yet
- Updated Lists of Controlled Substances As of October 2019Document14 pagesUpdated Lists of Controlled Substances As of October 2019Marlon RondainNo ratings yet
- The Global MigrationDocument3 pagesThe Global MigrationAlthea AlcalaNo ratings yet
- Organ Donation What Is Organ Donation?Document10 pagesOrgan Donation What Is Organ Donation?Althea AlcalaNo ratings yet
- WEEK 16 Filipino Culture Practices and Beliefs 118 LecDocument6 pagesWEEK 16 Filipino Culture Practices and Beliefs 118 LecAlthea AlcalaNo ratings yet
- Professional Negligence and The Doctrine of Res Ipsa LoquiturDocument7 pagesProfessional Negligence and The Doctrine of Res Ipsa LoquiturAlthea AlcalaNo ratings yet
- IVT ComplicationsDocument4 pagesIVT ComplicationsAlthea AlcalaNo ratings yet
- Sexual HarassmentDocument5 pagesSexual HarassmentAlthea AlcalaNo ratings yet
- Blood TransfusionDocument8 pagesBlood TransfusionAlthea AlcalaNo ratings yet
- MnemonicsDocument20 pagesMnemonicsKhassmeen Delos Santos AradaniNo ratings yet
- MinnaH SaunaReviewDocument9 pagesMinnaH SaunaReviewRobbyNo ratings yet
- Hemodynamically Stable Left Ventricular Pseudoaneurysm: Who Should Manage - Surgeon or Cardiologist?Document4 pagesHemodynamically Stable Left Ventricular Pseudoaneurysm: Who Should Manage - Surgeon or Cardiologist?asclepiuspdfsNo ratings yet
- Amlodipine Side EffectsDocument6 pagesAmlodipine Side Effects1976gt500No ratings yet
- Jeena Jayan - CV Orig-2Document5 pagesJeena Jayan - CV Orig-2Raghavendran RamachandranNo ratings yet
- Coronary Artery Revascularization in Stable Patients With Diabetes Mellitus - UpToDateDocument22 pagesCoronary Artery Revascularization in Stable Patients With Diabetes Mellitus - UpToDateAnca StanNo ratings yet
- Clinical: MCQ TestDocument47 pagesClinical: MCQ TestAhmed AlrkabeNo ratings yet
- Pharmacological Management of Acute Coronary Syndromes (ACS) and Acute Limb Ischemia (ALI)Document44 pagesPharmacological Management of Acute Coronary Syndromes (ACS) and Acute Limb Ischemia (ALI)hendratj90No ratings yet
- Physiological Changes in Older AdultsDocument30 pagesPhysiological Changes in Older AdultsElla Neiza AngelesNo ratings yet
- New England Journal Medicine: The ofDocument13 pagesNew England Journal Medicine: The ofStefania CristinaNo ratings yet
- Tif30Document49 pagesTif30HCX dghhqNo ratings yet
- Aortoiliac Occlusive DiseaseDocument37 pagesAortoiliac Occlusive Diseasewolff_512No ratings yet
- 100 Important Terminologies in Medical Surgical NursingDocument4 pages100 Important Terminologies in Medical Surgical Nursingyuuki konnoNo ratings yet
- Kertas Kerja PinjamanDocument18 pagesKertas Kerja PinjamanWan AzmanNo ratings yet
- Mfine CardiologistsDocument7 pagesMfine Cardiologistsmfine healthNo ratings yet
- Copd and Cardiovascular Disease: Original ArticleDocument9 pagesCopd and Cardiovascular Disease: Original Articlemgoez077No ratings yet
- Course in The Ward Date & Time Doctor's Order Rationale June 29, 2007 9:50pmDocument3 pagesCourse in The Ward Date & Time Doctor's Order Rationale June 29, 2007 9:50pmSean DadulaNo ratings yet
- Vitamin CDocument3 pagesVitamin Cnichitacristina66No ratings yet
- Lecture 3 PDFDocument24 pagesLecture 3 PDFAya MuhannadNo ratings yet
- Science: Jeanelyn Mae B. Pesimo Grade 11 - Abm St. Gregory The GreatDocument14 pagesScience: Jeanelyn Mae B. Pesimo Grade 11 - Abm St. Gregory The GreatJeanelyn Mae PesimoNo ratings yet
- The Heart III - Chapter 19 Case StudyDocument5 pagesThe Heart III - Chapter 19 Case StudyBrad ConnersNo ratings yet
- ECG in Acute MI The - Unknown OcrDocument366 pagesECG in Acute MI The - Unknown OcrER BearNo ratings yet
- Pathophysiology ErDocument3 pagesPathophysiology ErAlexa A. AldayNo ratings yet
- Cardiomems HF System: Product HighlightsDocument2 pagesCardiomems HF System: Product HighlightsanishNo ratings yet