Professional Documents
Culture Documents
Erythematosus - 2017
Uploaded by
Matheus AugustoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Erythematosus - 2017
Uploaded by
Matheus AugustoCopyright:
Available Formats
F O C U S O N I M M U N O M E TA B O L I S M
REVIEWS
Immunometabolism in systemic lupus
erythematosus
Laurence Morel
Abstract | Systemic lupus erythematosus (SLE) is an autoimmune disease mediated by pathogenic
autoantibodies directed against nucleoprotein complexes. Beyond the activation of autoreactive
B cells, this process involves dysregulation in many other types of immune cells, including CD4+
T cells, dendritic cells, macrophages and neutrophils. Metabolic substrate utilization and
integration of cues from energy sensors are critical checkpoints of effector functions in the
immune system, with common as well as cell-specific programmes. Patients with SLE and
lupus-prone mice present with activated metabolism of CD4+ T cells, and the use of metabolic
inhibitors to normalize these features is associated with therapeutic effects. Far less is known
about the metabolic requirements of B cells and myeloid cells in SLE. This article reviews current
knowledge of the alterations in metabolism of immune cells in patients with SLE and mouse
models of lupus in the context of what is known about the metabolic regulation of these cells
during normal immune responses. How these alterations might contribute to lupus pathogenesis
and how they can be targeted therapeutically are also discussed.
Systemic lupus erythematosus (SLE) is an autoimmune Review discusses these findings, as well as subsequent
disease with a heterogeneous clinical presentation that studies in patients with SLE and in mouse models of
results from a wide array of immunological abnormal lupus, in the context of recent discoveries that have
ities. Tissue damage is mediated by pathogenic auto placed metabolism as a central checkpoint for effector
antibodies, but abnormalities in cell development and programmes first in T cells, and increasingly in other
function are not limited to B cells; indeed, most types of immune cell types.
immune cell have been implicated in SLE pathogenesis1.
A number of spontaneous and induced mouse models T cell metabolism in SLE
of lupus have been developed2, each corresponding to A functional link between metabolism and immune cell
overlapping subsets of the clinical and immunological function was first discovered in T cells6. CD4+ T cells
phenotypes presented by patients with SLE (BOX 1). in patients with SLE and lupus-prone mice have altered
Immune cells respond to stimuli with a rapid prolif signalling and function7, and numerous abnormalities
eration and differentiation into highly specialized effec in the metabolism of these cells have been reviewed
tor cells. These processes are metabolically demanding, elsewhere8–10. Only salient points are summarized and
requiring not only an increased uptake of nutrients integrated here (FIG. 1).
(mostly glucose, fatty acids and glutamine), but also a
switch to specialized metabolic pathways corresponding Mitochondrial abnormalities and oxidative stress.
to specific effector functions. The changes in the amount A dysfunction in cellular metabolism in SLE was first
and type of nutrients taken up, as well as the metabolic reported in T cell mitochondria, which are character
processes by which they are utilized, have been referred ized by membrane hyperpolarization (elevation of the
to as metabolic reprogramming. Immunometabolism mitochondrial transmembrane potential), increased
refers to the metabolic reprogramming that occurs production of reactive oxygen intermediates and ATP
Department of Pathology, during immune responses. Metabolic abnormalities in depletion11. This pioneering study also documented
Immunology, and Laboratory T cells from patients with SLE were first reported 15 years depletion of the intracellular antioxidant glutathione
Medicine, University of
Florida, Gainesville,
ago3, and these observations provided the rationale for (in its reduced state) in SLE11. The increased mitochon
Florida 32610, USA. small clinical trials to explore whether reducing mecha drial mass (‘megamitochondria’) and hyperpolarization
morel@ufl.edu nistic target of rapamycin (mTOR) activation by use of of mitochondria in CD4+ T cells from patients with SLE
doi:10.1038/nrrheum.2017.43 rapamycin or the glutathione precursor N‑acetylcysteine contribute to the activation, impaired activation-induced
Published online 31 Mar 2017 could be a promising therapeutic approach4,5. This cell death and increased necrosis of these cells, with
NATURE REVIEWS | RHEUMATOLOGY ADVANCE ONLINE PUBLICATION | 1
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Key points one of the factors contributing to the decreased ATP levels
found in T cells in SLE. A polymorphism in UCP2 is also
• In systemic lupus erythematous (SLE), CD4+ T cells have a hypermetabolic state associated with SLE susceptibility 22. UCP2 encodes a pro
dominated by oxidation, mitochondrial abnormalities, activation of mTORC1 and tein that uncouples protons from ATP synthesis, thereby
increased glucose flux negatively regulating mitochondrial reactive oxygen spe
• Targeting T cell metabolism has therapeutic effects in mouse models of lupus and in cies (ROS) production, and potentially contributing to
the T cells of patients with SLE the oxidative state observed in T cells in SLE. However,
• Cell-specific metabolic imbalances probably also affect other immune cells in SLE, the same polymorphism is also associated with suscep
including neutrophils, plasma cells and macrophages, and specific metabolic tibility to rheumatoid arthritis (RA), and T cells in RA
targeting of these cells could have therapeutic benefit
are characterized by a hyper-reduced state23, making the
• A better understanding of the complexities of immunometabolism in SLE could lead consequences of this association unclear.
to personalized therapeutic options
• The metabolome, potentially intersecting with the microbiota, might provide mTOR. Mechanistic target of rapamycin (mTOR) is a sen
biomarkers for SLE
sor system composed of two complexes, mTOR complex 1
(mTORC1) and mTORC2, which integrate metabolic
cues to direct genetic programmes regulating cellular
necrosis adding to the pool of cellular debris that stim growth and energy utilization. Polarization of T cells
ulates autoreactive lymphocytes12. Increased mitochon to the inflammatory type 1 T helper (TH1) and TH17
drial biogenesis in response to elevated nitric oxide (NO) subsets is mTORC1‑dependent in both normal24,25 and
levels, combined with defective mitophagy, are the major autoimmune26 T cells. Conversely, inhibition of mTORC1
factors responsible for the increased mitochondrial expands Treg cells26, although mTORC1 is required for the
mass and size of CD4+ T cells in SLE13. Mitochondrial suppressive function of these cells27. The requirement for
remodelling directly controls metabolic reprogramming mTOR in CD4+ follicular helper T (TFH) cells, a critical
of T cells. Mitochondrial fusion promotes assembly of subset in patients with SLE and in lupus-prone mice28,29,
the electron transport chain and thus sustains oxidative is unclear. Virally induced TFH cells do not require
phosphorylation, which is associated with T cell memory mTORC1 activation to the same extent as their TH1 cell
and longevity. Conversely, mitochondrial fission dis counterparts30. However, inhibition of AMP-activated
Electron transport chain
A series of proteins in the inner rupts the electron transport chain and forces a switch to protein kinase (AMPK) and subsequent activation of
mitochondrial membrane that aerobic glycolysis, which is associated with acute T cell mTORC1 by Roquin‑1 promotes TFH cell differentiation31
transfer electrons from one to activation14. These findings are in agreement with the and a lupus-like phenotype32. Finally, emerging results
the other in a series of redox large mitochondrial size and increased oxidative phos suggest a context-dependent regulation of TFH cells by
reactions, resulting in the
movement of protons out of
phorylation in CD4+ T cells in SLE15. Despite hyper mTORC1 or mTORC2 in the normal immune response
the mitochondrial matrix and activity of electron transport chain complex I, ATP in mice33. The role of mTOR in TFH cell polarization and
in the synthesis of ATP. production is decreased in these T cells, leading to the function remains to be addressed in SLE in patients as well
release of reactive oxygen intermediates16. This oxida as in mouse models of spontaneous lupus.
Oxidative phosphorylation
tive stress can promote autoimmunity by modulating mTORC1 activation in CD4+ T cells from patients
A metabolic pathway that
produces ATP from the signal transduction and cytokine production in a T cell- with SLE34 and lupus-prone mice35–37 has multiple conse
oxidation of acetyl-CoA and intrinsic manner 17. A well-documented consequence of quences; most importantly, it enhances glycolysis and pre
the transfer of electrons to the oxidative stress in T cells in SLE is the lysosomal degra vents autophagy, including mitophagy, which is likely to
electron transport chain via dation of the T cell surface glycoprotein CD3ζ chain and contribute to mitochondrial dysfunction. This dysfunc
NADH and FADH2.
its replacement by the highly homologous FcεRIγ chain, tion leads to the development of pathogenic CD4+ T cell
Aeorbic glycolysis which recruits tyrosine-protein kinase SYK and enhances phenotypes in patients with SLE38,39, which is reverted by
(Also known as the ‘Warburg signalling upon T cell receptor (TCR) activation18. treatment with rapamycin or N‑acetylcysteine (which
effect’) The abrupt metabolic Treatment with N‑acetylcysteine replenished the levels inhibits mTORC1)4,5, including the reduction of CD3ζ
switch from oxidative
of glutathione and, indirectly, NADPH, which represent degradation and normalization of TCR signalling 40.
phosphorylation to glycolysis,
regardless of the availability of two major components of the defence system against oxi Several overlapping mechanisms lead to mTORC1 acti
oxygen, to provide energy for dative stress in the mitochondria. This treatment showed vation in T cells in SLE, including mitochondrial dys
cell proliferation and effector a therapeutic effect in patients with SLE5, demonstrating function, over-reactivity of the pentose phosphate pathway
functions. a pathogenic consequence of mitochondrial dysfunction (PPP) and transaldolase activity 40, as well as accumulation
Glycolysis
and oxidative stress in T cells in SLE. of kynurenine, a tryptophan metabolite with immune
An oxygen-independent Genetic factors might contribute to mitochondrial modulatory functions41. Genetic activation of mTORC1
metabolic pathway that dysfunction in T cells in SLE. In mice, the Sle1c2 lupus is also associated with SLE. The development of severe
generates two molecules of susceptibility locus is associated with increased CD4+ lupus-like pathology has been reported in four patients
pyruvate, ATP and NADH from
T cell activation, age-dependent expansion of IFNγ- suffering from tuberous sclerosis42–45, a rare disease
every one molecule of glucose,
supporting the tricarboxylic producing T cells and decreased regulatory T (Treg) cell resulting from mutations in the genes encoding hamartin
acid cycle and providing frequency19. T cells expressing Sle1c2 have increased mito (TSC1) or tuberin (TSC2), which together form the TSC
intermediates for the pentose chondrial mass and express a reduced level of ESRRG, a complex that inhibits mTORC1 activation. Given that the
phosphate pathway, gene that regulates mitochondrial metabolism20. A poly coincidence of tuberous sclerosis and SLE is statistically
glycosylation reactions and for
the synthesis of biomolecules
morphism in MT‑ATP6, which encodes a component of unlikely, these case reports illustrate the link between
(including serine, glycine, mitochondrial membrane ATP synthase (complex V or unrestrained mTORC1 activation and the development
alanine and acetyl-CoA). F0F1 ATP synthase), is associated with SLE21 and might be of SLE.
2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrrheum
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
F O C U S O N I M M U N O M E TA
RB OILEIW
EV SMS
Box 1 | Major manifestations in SLE and mouse models Several glucose transporters are expressed on T cells,
with GLUT1 and GLUT6 being highly upregulated
Clinical manifestations and immune abnormalities in SLE upon TCR and CD28 stimulation. Increased expres
According to the Systemic Lupus International Collaborating Clinics (SLICC) scheme sion of glucose transporters leads to increased glucose
for the classification of SLE, a patient must present with at least four criteria from uptake and glycolysis50. Glut1 overexpression in mice
among 11 clinical criteria and six immunologic criteria, including at least one clinical
led to the accumulation of activated T cells and the pro
and at least one immunologic criterion, or with biopsy-proven nephritis and
anti-nuclear antibodies (ANA) or anti-double-stranded DNA (anti-dsDNA) antibodies140. duction of autoantibodies51. GLUT1 overexpression has
not been reported in human SLE, but CD4+ T cells from
Corresponding phenotypes in mouse models lupus-prone B6 Sle1.Sle2.Sle3 triple-congenic mice over
The incidence of SLE is heavily gender-biased with a 9:1 female:male ratio. This female
expressed two key genes in glycolysis35,36: Slc16a3, which
preponderance is also found in all mouse models of lupus to varying degrees, except in
the BXSB.Yaa mouse, in which disease is driven by a translocation of X‑chromosome
encodes a lactate transporter, and Hif1a, encoding a tran
encoded Tlr7 to the Y chromosome. All spontaneous mouse models are characterized scription factor induced by mTORC1 activation25. It is
by the production of ANA and anti-dsDNA antibodies, as well as the development of therefore likely that HIF1A is upregulated in T cells from
immune complex glomerulonephritis. Antibodies with RNA specificities (including patients with SLE. Hypoxia-inducible factor 1α (HIF‑1α)
anti‑Sm antibodies) as well as antiphospholipid antibodies are found in a subset of regulates T cell effector functions52; the role of HIF1a in
strains; the former are found in MRL/lpr and BXSB.Yaa mice, and the latter in MRL/lpr SLE is discussed further in the hypoxia section of this
and (NZW×BXSB)F1 mice. Although type I interferon has a role in spontaneous mouse Review. A link between the complement receptor CD46
models of lupus, the interferon signature is not as dominant in these models as in (also known as membrane cofactor protein), which is acti
patients with SLE or in the pristane-induced mouse model. Besides renal pathology, vated in T cells in SLE53, Glut1 expression and mTORC1
MRL/lpr mice present with skin lesions that have most features of cutaneous lupus,
activation has been found in mice54. Dysregulation
some cognitive impairment that represents a subset of neuropsychiatric lupus
manifestations, as well as low incidence of joint inflammation.
of complement signalling in T cells might therefore
contribute to the metabolic abnormalities of T cells in SLE.
SLE, systemic lupus erythematosus.
Cholesterol and glycosphingolipid metabolism.
Glycosphingolipids and cholesterol are inserted in lipid
Glucose metabolism. Three main pathways of glucose rafts in the T cell plasma membrane and are important
utilization — PPP, oxidative phosphorylation and aerobic in regulating TCR signalling. In normal T cells, levels
glycolysis — have been implicated in T cell activation in of glycosphingolipids and cholesterol increase in these
SLE. PPP hyperactivation corresponds to the metabolic rafts following TCR activation, then return to baseline
needs of proliferating T cells during the development of once TCR signalling ceases55. Lipid rafts are aggregated
effector responses, and produces a strong metabolic signa in CD4+ T cells from patients with SLE56. Reduction of
ture in the peripheral blood lymphocytes of patients with lipid raft synthesis restored normal signalling in T cells
SLE41. Whether T cell activation in SLE is the primary from patients with SLE57,58 and decreased lupus pathology
cause of PPP hyperactivation or, alternatively, accelerated in MRL/lpr mice59.
PPP enables T cell activation is unclear. Interestingly, PPP Studies published in 2016 unveiled a critical role for
is also hyperactivated in the T cells of patients with RA, cholesterol in regulating TCR signalling and effector
Pentose phosphate pathway in which the resultant generation of excess NADPH is functions in CD8+ T cells60. Displacing cholesterol with
(PPP) responsible for the inflammatory T cell phenotype23. The cholesterol sulfate (a naturally occurring cholesterol ana
An anabolic metabolic pathway reasons for these opposite outcomes of PPP activation in logue) prevented TCR clustering and decreased signal
parallel to glycolysis that T cells in SLE and RA are presently unclear. ling 61. On the other hand, biochemical studies showed
branches out from glycolysis
with the conversion of glu-
Chronically activated healthy human CD4+ T cells46, as that cholesterol binds TCRβ and prevents its phosphoryl
cose‑6‑phosphate to ribose well as CD4+ T cells from patients with SLE15,35 and lupus- ation62. As yet, these observations have not been extended
5‑phosphate and generates prone mice35,36, showed high levels of oxygen consump to autoreactive T cells. However, in vitro polarized mouse
the reducing equivalents tion, in contrast to acutely activated T cells, which had a TH17 cells are characterized by increased cholesterol
NADPH, ribose 5‑phosphate
more glycolytic phenotype46. These findings suggest that uptake and biosynthesis coupled with decreased meta
(used in the synthesis of
nucleotides and nucleic acids) chronic activation by autoantigens (as occurs in SLE) is bolism and efflux, leading to the production of specific
and erythrose‑4‑phosphos- supported by oxidative phosphorylation, whereas aero sterol–sulfate conjugates that activate nuclear receptor
phate (used in the synthesis of bic glycolysis supports acute activation induced by foreign RORγ63. In addition, statins have been used to treat SLE
amino acids). antigens or in vitro supraphysiological TCR stimulation. in clinical trials and preclinical animal models, with the
Lipid rafts
CD4+ T cells from patients with SLE and lupus-prone results showing the expected reduction in cardiovascular
Microdomains of the plasma mice also display elevated glycolysis35,36, which could morbidity, but mixed results with respect to the non-
membrane that are enriched correspond to a compensatory mechanism to remedi cardiovascular pathology associated with the disease64.
in cholesterol and ate ATP production by defective mitochondria. A dual Statins prevented TH17 polarization in patients with mul
glycosphingolipids and serve
requirement for glycolysis and oxidative phosphorylation tiple sclerosis and promoted Treg cell expansion in patients
as self-organizing centres for
the assembly of signalling has been found in healthy effector memory CD4+ T cells47, with RA (reviewed by Ulivieri and Baldari64); this obser
molecules. a subset that is expanded in SLE48,49. The enhanced glyco vation suggests that statins could be beneficial for patients
lysis and oxidative phosphorylation found in naive CD4+ with SLE, given the role of these T cell subsets in the dis
Statins T cells from lupus-prone mice35 suggests that T cells in ease7. However, the fact that statins not only inhibit cho
A class of lipid-lowering drugs
that inhibit a key enzyme in the
SLE might be fuelled by an intrinsically high metabolism, lesterol synthesis, but also have immunoregulatory effects
synthesis of cholesterol, and that the age-dependent accumulation of effector by preventing protein isoprenylation, makes it difficult
HMG-CoA reductase. memory CD4+ T cells further increases T cell metabolism. to interpret these results from a mechanistic perspective.
NATURE REVIEWS | RHEUMATOLOGY ADVANCE ONLINE PUBLICATION | 3
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Glucose
Glucose T cell
transporter
TCR
Glucose
PPP
R5P ↓ NADPH Kynurenine
↓ Glutathione
PI3K–AKT
NO
mTORC1
Mitochondria
Autophagy
ETC I II III IV V
HIF-1α
Myc
↑ ROS
Lactate Pyruvate TCA cycle ↓ ATP
Solute Glycolysis
carrier
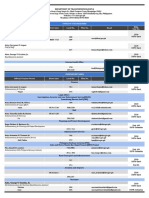
Figure 1 | Metabolic activation of CD4+ T cells in SLE. Glucose is mostly oxidized in the tricarboxylic acid (TCA) cycle
but can also be diverted to the pentose phosphate pathway (PPP). T cell receptor (TCR) stimulation activates
Nature Reviews mechanistic
| Rheumatology
target of rapamycin complex 1 (mTORC1) through the phosphatidylinositol 3‑kinase (PI3K)–AKT pathway. Low levels of
NADPH and glutathione contribute to elevated production of mitochondrial reactive oxygen species (ROS) but decreased
levels of ATP. Low NADPH and glutathione also contribute to mTORC1 activation, directly and/or through elevated levels
of kynurenine. mTORC1 activation activates glucose metabolism through hypoxia-inducible factor 1α (HIF‑1α) and Myc
proto-oncogene protein, and inhibits autophagy, which itself contributes to mitochondrial dysfunction. ETC, electron
transport chain; NO, nitric oxide; R5P. ribose 5‑phosphate.
T cells from patients with SLE support increased promotes IL17 transcription by aryl hydrocarbon recep
glycosphingolipid synthesis, which is associated with tor, indicating that LXRs have immunoregulatory func
increased TCR signalling 58. Pharmacological inhibition tions unrelated to cholesterol homeostasis67. Another
of glycosphingolipid synthesis reduced the activation of potential contributor to glycosphingolipid synthesis in
these T cells in vitro58, demonstrating a causal relationship. T cells in SLE is FLI1, a transcription factor expressed
Several mechanisms could be responsible for increased in T cells with expression levels linked to SLE pathogen
glycosphingolipid levels in T cells in SLE. Increased esis68. One target of FLI1 is NEU1, which controls glycos
expression of oxysterols receptor LXRβ (also known as phingolipid synthesis. Accordingly, Fli1‑haplodeficiency
liver X receptor β), a nuclear receptor that controls cel reduced disease severity in MRL/lpr mice in parallel with
lular lipid metabolism and trafficking, was associated decreased T cell activation68. The latter effect included
with altered trafficking and recycling of glycosphin reduced expression of CXC chemokine receptor 3
golipids, leading to their accumulation in T cells from (CXCR3) by T cells and a correspondingly reduced level
patients with SLE58. The role of LXRs in immune cells is of renal infiltrates69. A variant in the FLI1 promoter region
complex, however, involving both proinflammatory and that leads to increased FLI1 expression is associated with
anti-inflammatory functions65. A genetic polymorphism susceptibility to SLE70. Glycosphingolipid metabolism is
leading to decreased LXRα levels in B cells and increased also defective in the kidneys of MRL/lpr mice and patients
B cell proliferation has been associated with SLE suscep with SLE owing to increased expression of two enzymes,
tibility 66. Deficiency in both the LXRα and LXRβ genes β-1,4‑galactosyltransferase 5 (also known as β4GalT‑5)
4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrrheum
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
F O C U S O N I M M U N O M E TA
RB OILEIW
EV SMS
and neuraminidase 1 (encoded by NEU1), involved in studies have shown a beneficial effect of PPARγ agonists
glycosphingolipid biosynthesis71. Elevated glycosphin in mouse models of lupus81–84, potentially linking FAAH
golipid levels have been associated with inflammation, and PPARγ to SLE pathogenesis.
including lupus nephritis71, indicating that altered gly
cosphingolipid metabolism can affect SLE pathogenesis Macrophages and dendritic cells. Our understanding of
not only through the immune system, but also at the site the metabolic programmes that govern macrophage and
of tissue injury. dendritic cell (DC) functions has expanded rapidly in the
past 5 years85. However, whether changes in the metabo
Abnormal metabolism in other immune cells lism of these cells has a role in the pathogenesis of SLE is
B cells. Similar to CD4+ T cells, activated B cells are pre largely unknown. The tolerogenic clearance of apoptotic
dominantly glycolytic72, but the existence of metabolic cells by splenic marginal zone macrophages requires the
checkpoints in B cell development is poorly character expression of indoleamine 2,3‑dioxygenase (IDO)86. A
ized. A few studies are, however, relevant to B cells in SLE. primary downstream effector of IDO is the metabolic-
Transgenic mice overexpressing B cell activating factor stress sensing kinase eIF‑2α‑kinase GCN2, the activity of
(BAFF, also known as BLyS or TNF ligand superfamily which is required to prevent autoimmunity induced by
member 13B) produce lupus-like autoantibodies and exposure to apoptotic cells87. In response to amino acid
B cells from these mice are more glycolytic than B cells variations such as tryptophan catabolism by IDO, GCN2
from nontransgenic littermates73. According to this activates a stress-response programme that regulates
result, B cells from patients with SLE and lupus-prone innate immunity 88. The protective effect of GCN2 against
mice, which are exposed to high levels of BAFF, should autoimmune pathology has also been reported in kidneys
also be highly glycolytic (FIG. 2), but this hypothesis has of mice with immune complex-induced nephritis87. IDO
not been formally tested. Massive protein synthesis cor and GCN2 expression protected podocytes from apopto
responding to immunoglobulin secretion coupled with sis and reduced glomerular infiltrates by a process involv
longevity places unique metabolic demands on long- ing autophagy, following immune complex-induced
lived plasma cells74. Enforced mTORC1 activation drives inflammation. Although the molecular mechanisms are
B cells to differentiate into plasma cells75, an effect that still unclear, this metabolic stress response is probably
can be explained by the role of mTORC1 in promoting important in protection from autoimmune pathology.
protein synthesis. mTORC1 is activated in T cells from Indeed, preliminary studies suggest that a GCN2 agonist
patients with SLE34 and in the B cells of lupus-prone mice (halofuginone hydrobromide) has potent therapeutic
in several models of disease76. In vitro studies have also effects in animal models of lupus89. Interestingly, GCN2
shown that rapamycin inhibits BAFF-mediated prolif also mediates the effect of IDO in T cells and inhibits
eration and survival signals77. It is therefore likely that mTORC1 activation88. However, a preliminary study in
mTORC1 activation contributes to plasma cell differen alloreactive human CD4+ T cells has found differences
tiation and production of pathogenic autoantibodies in in the immunosupressive activities of rapamycin and
SLE. The metabolic requirements of long-lived plasma a GCN2 agonist, with the latter being more effective at
cells corresponding to their longevity was addressed in a suppressing TH2 responses90. These results suggest that
2016 study 78. As shown previously for memory T cells47, GCN2 activity should be examined in T cells in SLE.
survival of long-lived plasma cells requires mitochon In DCs, mTOR has a central role in integrating
drial pyruvate import via the mitochondrial pyruvate activation from TLR signals and growth factors with
carrier (MCP) complex 78. Inhibition of glucose utiliza intracellular nutrient levels91. Constitutive mTORC1 acti
tion could therefore target plasma cells in SLE, especially vation impaired DC survival and proliferation but accel
long-lived plasma cells, not only by preventing immuno erated their maturation through Myc proto-oncogene
globulin glycosylation, but also by impairing their sur protein (Myc)-dependent metabolic reprogramming
vival through lack of pyruvate. The latter effect should that included high levels of ROS production92. Given that
also be achieved by the use of MCP inhibitors, which T cells in SLE have activated mTORC1 and produce
Fatty acid oxidation
A metabolic process that could also impair the function of effector memory CD4+ high levels of ROS, as well as having chronic endosomal
produces ATP from the T cells in SLE36. TLR signalling, DCs in SLE probably also have impaired
oxidation of acetyl-CoA The metabolic gene Faah, encoding fatty acid amide metabolism that enhances their maturation, which in
derived from the mobilization hydrolase (FAAH), has been proposed as a susceptibility turn contributes to T cell hyperactivation. A study pub
of fatty acids.
gene in the murine NZM2410‑derived Sle2 locus79. FAAH lished in 2016 showed that type I interferon production
Tricarboxylic acid (TCA) degrades ligands for cannabinoid receptors and members by Toll-like receptor 9 (TLR9)-activated plasmacytoid
cycle of the peroxisome proliferator-activated receptor (PPAR) DCs (pDCs) increased oxidative phosphorylation in
(Also known as the Krebs family. The lupus-associated allele corresponds to an autocrine fashion as well as in neighbouring non-
cycle) A set of connected
increased Faah expression and enhanced B cell receptor haematopoeitic cells, with a specific contribution of fatty
pathways in the mitochondrial
matrix, which metabolize revision in mature B cells, which leads to autoantibody acid oxidation93, which was necessary for full pDC activa
acetyl-CoA derived from production79. Interestingly, increased FAAH levels were tion. Interestingly, fatty acids were the major substrate for
glycolysis or fatty acid found in plasma cells from patients with SLE80. The oxidative phosphorylation in pDCs, and glucose flux and
oxidation, producing NADH mechanism linking increased levels of fatty acid amides mitochondrial pyruvate uptake to the tricarboxylic acid
and FADH2 for the electron
and esters to the B cell receptor repertoire or plasma cell (TCA) cycle were required to generate citrate for de novo
transport chain and precursors
for amino acid and fatty function is unclear. Increased FAAH expression predicts fatty acid synthesis. It is now well established that type I
acid synthesis. decreased PPAR activation and, interestingly, multiple interferons are central to SLE pathogenesis. This new
NATURE REVIEWS | RHEUMATOLOGY ADVANCE ONLINE PUBLICATION | 5
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
BAFF BAFFR
Glucose
Glucose B cell BCR
transporter
Glucose
Repertoire
PI3K–AKT editing
↑ Glycolysis
Fatty acid amides
and esters
Mitochondria FAAH
Lactate Pyruvate MCP ↑ Pyruvate
Endoplasmic
Solute Glycolysis reticulum
carrier
↑ Autophagy
↑ Long-lived
plasma cell survival
Figure 2 | Potential metabolic pathways involved in B cells in SLE. The high level of B cell activating factor (BAFF, also
known as BLyS or TNF ligand superfamily member 13B) found in systemic lupus erythematosus Nature(SLE)
Reviews | Rheumatology
as well as strong B cell
receptor (BCR) signals increase glucose metabolism and glycolysis. This increase might contribute to high levels of
pyruvate import into the mitochondria, which are necessary for the survival of long-lived plasma cells. Finally, increased
expression of fatty acid amide hydrolase (FAAH) might skew the BCR repertoire towards autoreactive specificities and
support plasma cell function or survival. BAFFR, B‑cell activating factor receptor; MCP, mitochondrial pyruvate carrier;
PI3K, phosphatidylinositol 3‑kinase.
metabolic study suggests that inhibition of fatty acid syn TFAM (transcription factor A, mitochondrial) phospho
thesis would decrease type I interferon production by rylation, which is a necessary step in the degradation of
pDCs and therefore have therapeutic benefits. Fatty acid oxidized mtDNA packed into nucleoids97. Consequently,
synthesis is also required for TH17 polarization94, which oxidized nucleoids accumulate in the mitochondria of
suggests that inhibition of fatty acid synthesis could have neutrophils in SLE, and are highly interferogenic when
multiple therapeutic benefits in SLE. extruded in NETs. High levels of mitochondrial ROS also
lead to spontaneous NETosis in the low-density neutro
Neutrophils. Neutrophils contribute to SLE pathogene phils (LDNs) that are characteristic of SLE. Accordingly,
sis through multiple mechanisms, including the produc treatment with a mitochondrial-ROS scavenger
tion of neutrophil extracellular traps (NETs), which are decreased spontaneous NETosis in MRL/lpr mice and
NETosis potent stimulators of type I interferon production95. In reduced disease activity 96. Consequently, mitochondrial
A specialized form of cell patients with SLE, ribonucleoprotein immune complexes oxidation is pathogenic in SLE not only through CD4+
death characterized by the are potent inducers of NETosis. These immune complexes T cells, but also through neutrophils. On the other hand,
release of neutrophil induce mitochondrial membrane hyperpolarization and Nox2‑deficient MRL/lpr mice, which cannot produce
extracellular traps (NETs),
which are chromatin structures
the generation of ROS, leading to oxidation of mitochon NADPH, and consequently have neutrophils that can
loaded with granular and drial DNA (mtDNA), which is the major immunogenic not undergo NETosis, develop accelerated disease98. This
nucleic proteins. factor in NETs96. Exposure to ribonucleoproteins blocks finding is consistent with an increased predisposition to
6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrrheum
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
F O C U S O N I M M U N O M E TA
RB OILEIW
EV SMS
autoimmunity, including SLE, in patients with chronic of SLE at the epigenetic level107, but connections to the
granulomatous disease (CGD), which involves defects multiple impaired metabolic checkpoints have not yet
in NADPH oxidase. These observations suggest that been clearly delineated.
NETosis could have a protective role in clearing apoptotic
debris. However, a 2016 study found that mtDNA oxida Role of hypoxia in lupus
tion occurs through NETosis of LDNs in both patients Hypoxia and immunometabolism are linked in mul
with SLE and those with CGD96. These conflicting results tiple ways in which the transcription factor HIF‑1α
suggest that mitochondrial oxidation of neutrophils dominates108. The cellular level of HIF‑1α is regulated
might promote or amplify disease, whereas apoptotic post-transcriptionally by oxygen-dependent prolyl
debris clearance by NETosis might prevent disease devel hydroxylases that tag HIF‑1α for ubiquitylation and
opment. A 2015 study has also shown that asymmetrical proteosomal degradation. Under hypoxic conditions,
ATP production and mTOR signalling are required for prolyl hydroxylases are inactivated, enabling HIF‑1α
neutrophil chemotaxis99. Whether the defective ATP pro accumulation. Stabilization of HIF‑1α also occurs in
duction coupled with mTORC1 activation seen in T cells pseudohypoxic conditions, such as mTORC1 activation
in SLE extends to neutrophils and contributes to their or high levels of mitochondrial ROS108. HIF‑1α upreg
defective functions in SLE is unknown. ulates a large number of key glycolytic genes, such as
GLUT1, and, accordingly, has a critical role in metabolic
Metabolic control of epigenetic regulation reprogramming of immune cells52. HIF‑1α expression
Epigenetic modifications to DNA and histones are is required for TH17 and, to a lesser extent, TH1 cell dif
impaired at multiple levels in SLE as a consequence, at ferentiation109. The role of HIF‑1α in Treg cell differenti
least in part, of impaired cellular metabolism100. DNA ation and function is more complex, and both positive
hypomethylation in patients with SLE ‘de‑represses’ and negative regulatory effects have been reported52. In
the transcription of key genes in T cells and increases DCs, HIF‑1α promotes proinflammatory responses110.
DNA immunogenicity 101. The impaired activity of DNA Consequently, it is likely that HIF‑1α drives some of
methyltransferases (DNMTs) in SLE can be attributed, at the metabolic abnormalities that have been observed in
least in part and both directly and indirectly, to oxida SLE. Increased Hif1a expression has been reported
tive stress100. Reduced levels of metabolites derived from in the CD4+ T cells of lupus-prone mice35 but, to date,
methyl group donors have been detected in the sera of no other study directly linking HIF‑1α to lupus has been
patients with SLE102, which suggests that additional defects published. Germinal centre B cells, which are expanded
in the S‑adenosyl-l‑methionine (SAM) cycle might con in SLE, are regulated by hypoxia and mTORC1 activ
tribute to DNA hypomethylation. Epigenetic proinflam ity 111. These effects are complex, however, with variable
matory changes in naive CD4+ T cells from patients with developmental and regional requirements for HIF‑1α
SLE correlated with an enrichment of binding sites for the and mTORC1 activation in germinal centre B cells. No
transcription factor histone-lysine N‑methyltransferase evidence of an association between SLE and genetic var
EZH2 at methylation sites103. EZH2 expression is con iations in HIF1A has been found112, suggesting that if
trolled by the microRNAs miR‑26a and miR‑101, both of HIF‑1α activity is elevated in SLE, it is a secondary effect,
which negatively correlated with SLE disease activity 103. most likely attributable to mTORC1 activation or high
Interestingly, the expression of these two microRNAs is levels of mitochondrial ROS.
glucose-sensitive, with increased glycolysis correlating Reduced angiogenesis is one of the many factors
with high expression of EZH2 in a cancer model104. This that contributes to hypoxia in kidneys affected by lupus
finding suggests that high glucose utilization by T cells nephritis113. A gene expression signature reflecting mito
in SLE could contribute to their DNA hypomethylation chondrial stress and hypoxia has been reported in the
through EZH2 activity, a hypothesis that has yet to be for kidneys of BWF1 and NZM2410 mice with chronic
mally verified. These results also suggest that the thera disease as well as early in post-treatment relapse; this
peutic effects of treatment with 2‑deoxy‑d‑glucose, which signature correlated with the level of hypoxia in the
normalizes some of the phenotypes of T cells in SLE36, kidneys114. Hif1α expression in podocytes has been
might occur through the epigenome. linked to NO‑induced damage in an immune complex-
Acetyl-CoA is essential for histone acetylation. independent form of lupus nephritis in mice115. In
Overexpression of histone acetyl transferase p300 is addition, the glomeruli and tubules from patients with
protective in lupus-prone mice, but whether acetylation lupus nephritis as well MRL/lpr mice express high levels
substrate availability (that is, low acetyl-CoA) is involved of HIF‑1α in correlation with mesangial cell expansion116.
in SLE is unclear 100. Histone deacetylases (HDACs) are Besides gene expression profiling, metabolic correlates
overexpressed in immune cells, particularly in T cells, of Hif1α expression in renal cells have not been yet
from MRL/lpr mice105, which could be secondary to pro established in lupus nephritis.
tein nitration and oxidative stress as histone deacetyla
tion is NAD+-dependent. Similarly, sirtuins (which are Systemic contributions to immunometabolism
also involved in histone deacetylation) are inhibited by The metabolic dysfunctions that have been reported in
NADPH, which also suggests that HDAC activity would immune cells in SLE most likely have cell-intrinsic ori
be increased in T cells in SLE. Accordingly, HDAC gins. However, systemic alterations of metabolism that
inhibitors decreased disease severity in lupus-prone produce a metabolic imbalance could have a second
mice106. Collectively, ample evidence suggests control ary effect on immune cell function. The origin of these
NATURE REVIEWS | RHEUMATOLOGY ADVANCE ONLINE PUBLICATION | 7
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
alterations can be genetic or environmental, with vari presented with a lower level of amino acids in comparison
ations in gut microbiota probably representing a major with healthy subjects, and the most discriminatory metab
source of metabolite imbalance. olite was either decreased tryptophan117 or increased
kynurenine41, a metabolite generated from tryptophan by
Metabolite imbalance. The distribution and abundance IDO. Kynurenine was sufficient to activate mTORC1 in
of metabolites in serum reflect, at least in part, cellular CD4+ T cells from healthy individuals41, suggesting that
metabolic programmes. Profoundly dampened serum this abnormal tryptophan metabolism could enhance
levels of metabolites derived from glycolysis, fatty acid CD4+ T cell activation. The increased level of kynurenine
oxidation and amino acid metabolism were found in in patients with SLE could be the indirect consequence
patients with SLE102, possibly reflecting an increased of oxidation, owing to impaired degradation of kynure
cellular demand for these three metabolic pathways nine by NADPH-dependent kynurenine hydrolase. In
in the immune cells of patients with SLE, as shown in support of this mechanism, N‑acetylcysteine treatment,
lupus-prone mice35. The same study also found a strong which restores NADPH levels, significantly decreased
presence of markers of oxidative damage, which reflects kynurenine levels in peripheral blood lymphocytes41. It
results obtained in studies of CD4+ T cells from patients has also been shown that type I interferons increase the
with SLE17. In addition, imbalances in the lipid profiles expression of IDO in vitro, skewing tryptophan metabo
of patients with SLE were skewed toward a proinfamma lism towards kynurenine production at the expense of ser
tory, prothrombotic state, corresponding to the cardio otonin118. Accordingly, patients with SLE and high type I
vascular morbidity often associated with SLE102. Two interferon activity had high levels of kynurenine and low
studies have reported a metabolome in peripheral blood serotonin levels118, the latter offering a potential link to the
lymphocytes of American patients with SLE41 and in sera neurological pathology associated with SLE.
of Scandinavian patients with SLE117 that was different
from that of healthy controls. Markers of oxidative stress Microbiota. Metabolites produced by the gut microbiota
were common to both studies, with marked decreases in contribute to the serum metabolome119. Patients with SLE
cysteine, NADPH and glutathione levels. In one of these have a distinctive gut microbiota as compared with healthy
studies, these markers of oxidative stress were reversed controls120,121. An analysis of foecal metabolites also showed
by treatment with N‑acetylcysteine41. This result further a distinctive ‘signature’ in patients with SLE as compared
supports the notion that oxidation is a major contribu with healthy controls, individuals with high BMI or
tor to SLE pathogenesis. Interestingly, these patients also patients with AIDS122,123. Which metabolic pathways are
responsible for these differences is not well understood.
Patients However, a block in the metabolism of ribose 5‑phosphate,
with SLE Microbiota
a product of the PPP (which is a hyperactive pathway in
patients with SLE41), was uncovered122. This block in ribose
5‑phosphate processing led to substantially reduced lev
↑ PPP
els of several amino acids, as found in the serum of
patients with SLE117, as well as pyrimidines and purines.
Ribose 5-phosphate
Succinylaminoimidazolecarboxamide ribose‑5ʹ‑phosphate
(SAICAR), a purine synthesis intermediate, was absent in
faeces from patients with SLE122. SAICAR activates the
M2 isoform of pyruvate kinase (PKM2), an enzyme that
supports glycolysis and HIF‑1α transactivation of target
genes in tumour cells124 as well as in immune cells108. The
PRPP Ribose 1,5-bisphosphate status of PKM2 activity, which relies on a balance of cyto
solic inactive monomers and metabolically active dimers,
↓ Amino acid synthesis as well as nuclear HIF‑1α‑binding tetramers, has not been
explored in SLE or other autoimmune diseases. It is pos
↓ Pyrimidine synthesis
sible, however, that low SAICAR production contributes
↓ Purine synthesis ↓ SAICAR to the oxidative stress that has been reported in SLE by
favouring pyruvate oxidation (FIG. 3).
↓ PKM2 Overall, serum and faecal metabolites can represent
the consequence of dysregulated cellular programmes in
↑ Respiration and mtROS Oxidative state immune cells, and might, in turn, have their own direct
effects on the functions of these cells, as reviewed above.
Figure 3 | Gut microbial metabolites and immune dysregulation in SLE. In addition, it is increasingly clear that many metabo
Ribose‑5‑phosphate, produced from an over-reactive pentose phosphate pathway (PPP) lites, such as succinate125, short chain fatty acids126 and
in patients with systemic lupus erythematosus (SLE) or from their gut microbiota, is
kynurenine (as shown above), have immunoregulatory
preferentially metabolized into ribose 1,5‑bisphosphate instead of phosphoribosyl
pyrophosphate (PRPP), which leads to a reduced biosynthesis of amino acids, pyrimidines properties. Therefore, the metabolite imbalance observed
and purines. Low levels of the purine synthesis intermediate succinylaminoimidazolecar- in patients with SLE possibly acts to feed forward the cel
Nature Reviews | Rheumatology
boxamide ribose‑5ʹ‑phosphate (SAICAR) could result in low glycolytic activity of pyruvate lular metabolism that sustains immune activation. This
kinase PKM2, which might in turn promote increased production of mitochondrial process should be further explored with special attention
reactive oxygen species (mtROS), thus contributing to oxidative stress. to the contribution of intestinal dysbiosis.
8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrrheum
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
F O C U S O N I M M U N O M E TA
RB OILEIW
EV SMS
Table 1 | Metabolic effects of standard-of‑care drugs used in patients with SLE Glucocorticoids are known to increase gluconeogen
esis, which leads to fat accumulation, and glucocorticoid
Drug Known mechanism Potential metabolic effect Refs treatment has been directly linked to increased leptin
Mycophenolic acid Inhibits guanosine Reduces AKT–mTOR activation, 35, levels in patients with SLE134,135. As leptin can activate
(mycophenolate (DNA) synthesis glycolysis and oxygen 130 mTORC1 (REF. 136), it is possible that glucocorticoid treat
mofetil) consumption in CD4+ T cells
ments have secondary metabolic effects on immune cells.
Methotrexate Inhibits purine and Activates AMPK, which inhibits 133 In conclusion, experimental evidence suggests that
pyrimidine (DNA) mTOR activation and glycolysis drugs used in the clinic to treat patients with SLE mod
synthesis
ulate AMPK and mTOR and might therefore have pro
Glucocorticoids Immunosupressant Increase production of leptin, 135 found effects on immune cell metabolism as part of their
which might activate mTOR
therapeutic benefits. Rapamycin, as an mTOR inhibitor,
AMPK, AMP-activated kinase; mTOR, mechanistic target of rapamycin; SLE, systemic lupus has been used effectively in a proof‑of principle study
erythematosus.
in patients with SLE and is currently being tested in a
clinical trial4,133. PPARγ agonists also indirectly inhibit
Metabolic effects of SLE treatments mTOR, among many other functions, and the selective
Many immunosuppressive drugs, including drugs PPARγ agonist pioglitazone, which has shown promising
used to treat patients with SLE, have direct or indirect effects in preclinical models84 and in T cells from patients
effects on immunometabolism (TABLE 1). Mycophenolate with SLE137, is currently in clinical trials for SLE with
mofetil (MMF), the pro-drug of mycophenolic acid, encouraging results133,138,139.
inhibits inosine monophosphate dehydrogenase type II,
a rate-limiting enzyme in the synthesis of guanosine Conclusions
and therefore DNA synthesis. This inhibition leads to Studies in patients with SLE and mouse models of the dis
immunosuppression by limiting T cell proliferation and ease have clearly established, using different approaches,
promoting apoptosis127. Treatment with mycophenolic that CD4+ T cells have a hypermetabolic state dominated
acid affects a number of key metabolic pathways in vitro by oxidation, mitochondrial abnormalities and high glu
with the downregulation of Myc and Hif1α expression in cose flux. Furthermore, targeting this T cell metabolism
endothelial cells128 and downregulation of signalling via showed therapeutic effects. Reducing mTOR activation
phosphatidylinositol‑3‑OH kinase, the serine-threonine with rapamycin4 or oxidation with N-acetylcysteine5
kinase AKT and mTOR in gastric tumour cells129. More reduced disease severity in patients with SLE, and dual
relevant to SLE, mycophenolic acid reduced human CD4+ inhibition of glucose utilization and complex I activity
T cell activation in vitro in correlation with a reduction reversed disease in lupus-prone mice35,36. Although most
of AKT–mTOR activity 130. In addition, mycophenolic research has focused on CD4+ T cells, other immune cells
acid reduced the glycolytic activity of, and oxygen con in SLE are probably affected by metabolic imbalances that
sumption by, human CD4+ T cells activated in vitro 35. might be normalized by these treatments. Deciphering
mTORC1 activation was found in the glomeruli of BWF1 the metabolism of macrophages clearing apoptotic debris
mice, and rapamycin treatment reduced renal pathology and that of germinal centre B cells and long-lived plasma
in this lupus model131. Therefore, it is possible that treat cells might be of particular interest in SLE. There is now
ment with MMF has a beneficial effect on renal pathol evidence that many aspects of metabolic regulation are
ogy through the mTOR pathway. MMF is widely used to cell-specific. A better understanding of the many ways
treat patients with SLE, but the extent to which its ther in which immune effector functions are regulated by
apeutic effect is linked to immunometabolism, includ cell-specific metabolic checkpoints could provide more
ing that of T cells, is currently unknown. Methotrexate, precise and personalized therapeutic options in SLE. In
which is discussed in detail in a Perspectives article in addition to therapeutic potential, the metabolome, poten
this journal132, increases the intracellular levels of AMP, tially intersecting with the microbiota, offers promising
activates AMPK and inhibits mTOR133. venues for disease biomarkers.
1. Liu, Z. & Davidson, A. Taming lupus — a new 6. Frauwirth, K. A. et al. The CD28 signaling pathway 13. Caza, T. N., Talaber, G. & Perl, A. Metabolic regulation
understanding of pathogenesis is leading to clinical regulates glucose metabolism. Immunity 16, of organelle homeostasis in lupus T cells. Clin.
advances. Nat. Med. 18, 871–882 (2012). 769–777 (2002). Immunol. 144, 200–213 (2012).
2. Sang, A., Yin, Y., Zheng, Y.‑Y. & Morel, L. in Progress in 7. Moulton, V. R. & Tsokos, G. C. T cell signaling 14. Buck, M. D. et al. Mitochondrial dynamics controls
Molecular Biology and Translational Science Vol. 105 abnormalities contribute to aberrant immune cell T cell fate through metabolic programming. Cell 166,
(ed. Conn, P. M.) 321–370 (Academic Press, 2012). function and autoimmunity. J. Clin. Invest. 125, 63–76 (2016).
3. Gergely, P. et al. Persistent mitochondrial 2220–2227 (2015). 15. Doherty, E., Oaks, Z. & Perl, A. Increased
hyperpolarization, increased reactive oxygen 8. Fernandez, D. & Perl, A. Metabolic control of T cell mitochondrial electron transport chain activity at
intermediate production, and cytoplasmic activation and death in SLE. Autoimmun. Rev. 8, complex I is regulated by N‑acetylcysteine in
alkalinization characterize altered IL‑10 signaling in 184–189 (2009). lymphocytes of patients with systemic lupus
patients with systemic lupus erythematosus. 9. Choi, S. C., Titov, A. A., Sivakumar, R., Li, W. & erythematosus. Antioxid. Redox Signal. 21, 56–65
J. Immunol. 169, 1092–1101 (2002). Morel, L. Immune metabolism in systemic lupus (2014).
4. Fernandez, D., Bonilla, E., Mirza, N., Niland, B. & erythematosus. Curr. Rheumatol. Rep. 18, 66 (2016). 16. Perl, A., Hanczko, R., Telarico, T., Oaks, Z. &
Perl, A. Rapamycin reduces disease activity and 10. Li, W., Sivakumar, R., Titov, A. A., Choi, S. C. & Landas, S. Oxidative stress, inflammation and
normalizes T cell activation-induced calcium fluxing in Morel, L. Metabolic factors that contribute to lupus carcinogenesis are controlled through the pentose
patients with systemic lupus erythematosus. Arthritis pathogenesis. Crit. Rev. Immunol. 36, 75–98 (2016). phosphate pathway by transaldolase. Trends Mol.
Rheum. 54, 2983–2988 (2006). 11. Gergely, P. et al. Mitochondrial hyperpolarization and Med. 17, 395–403 (2011).
5. Lai, Z. W. et al. N‑Acetylcysteine reduces disease ATP depletion in patients with systemic lupus 17. Perl, A. Oxidative stress in the pathology and
activity by blocking mammalian target of rapamycin in erythematosus. Arthritis Rheum. 46, 175–190 (2002). treatment of systemic lupus erythematosus.
T cells from systemic lupus erythematosus patients: 12. Perl, A., Gergely, P. Jr & Banki, K. Mitochondrial Nat. Rev. Rheumatol. 9, 674–686 (2013).
a randomized, double-blind, placebo-controlled trial. dysfunction in T cells of patients with systemic lupus 18. Tsokos, G. C. Systemic lupus erythematosus. N. Engl.
Arthritis Rheum. 64, 2937–2946 (2012). erythematosus. Int. Rev. Immunol. 23, 293–313 (2004). J. Med. 365, 2110–2121 (2011).
NATURE REVIEWS | RHEUMATOLOGY ADVANCE ONLINE PUBLICATION | 9
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
19. Perry, D. J. et al. Murine lupus susceptibility locus 44. Carrasco Cubero, C., Bejarano Moguel, V., Fernandez 68. Richard, E. M. et al. Reducing FLI1 levels in the MRL/
Sle1c2 mediates CD4+ T cell activation and maps to Gil, M. A. & Alvarez Vega, J. L. Coincidence of lpr lupus mouse model impacts T cell function by
estrogen-related receptor gamma. J. Immunol. 189, tuberous sclerosis and systemic lupus modulating glycosphingolipid metabolism. PLoS ONE
793–803 (2012). erythematosus‑a case report. Reumatol. Clin. 12, 8, e75175 (2013).
20. Huss, J. M., Garbacz, W. G. & Xie, W. Constitutive 219–222 (2016). 69. Sundararaj, K. P. et al. FLI1 levels impact CXCR3
activities of estrogen-related receptors: transcriptional 45. Singh, N., Birkenbach, M., Caza, T., Perl, A. & expression and renal infiltration of T cells and renal
regulation of metabolism by the ERR pathways in Cohen, P. L. Tuberous sclerosis and fulminant lupus in glycosphingolipid metabolism in the MRL/lpr lupus
health and disease. Biochim. Biophys. Acta 1852, a young woman. J. Clin. Rheumatol. 19, 134–137 mouse strain. J. Immunol. 195, 5551–5560 (2015).
1912–1927 (2015). (2013). 70. Morris, E. E. et al. A GA microsatellite in the Fli1
21. Vyshkina, T. et al. Association of common 46. Wahl, D. R. et al. Characterization of the metabolic promoter modulates gene expression and is
mitochondrial DNA variants with multiple sclerosis phenotype of chronically activated lymphocytes. Lupus associated with systemic lupus erythematosus
and systemic lupus erythematosus. Clin. Immunol. 19, 1492–1501 (2010). patients without nephritis. Arthritis Res. Ther. 12,
129, 31–35 (2008). 47. Dimeloe, S. et al. The immune-metabolic basis of R212 (2010).
22. Yu, X. et al. Association of UCP2 -866 G/A effector memory CD4+ T cell function under hypoxic 71. Nowling, T. K. et al. Renal glycosphingolipid
polymorphism with chronic inflammatory diseases. conditions. J. Immunol. 196, 106–114 (2016). metabolism is dysfunctional in lupus nephritis. J. Am.
Genes Immun. 10, 601–605 (2009). 48. Sobel, E. S. et al. Defective response of CD4+ T cells Soc. Nephrol. 26, 1402–1413 (2015).
23. Yang, Z. et al. Restoring oxidant signaling suppresses to retinoic acid and TGFβ in systemic lupus 72. Murray, P. J., Rathmell, J. & Pearce, E. SnapShot:
proarthritogenic T cell effector functions in rheumatoid erythematosus. Arthritis Res. Ther. 13, R106 immunometabolism. Cell Metab. 22, 190–190.e1
arthritis. Sci. Transl Med. 8, 331ra38 (2016). (2011). (2015).
24. Powell, J. D., Pollizzi, K. N., Heikamp, E. B. & 49. Morel, L. et al. Genetic reconstitution of systemic 73. Caro-Maldonado, A. et al. Metabolic reprogramming
Horton, M. R. Regulation of immune responses by lupus erythematosus immunopathology with is required for antibody production that is suppressed
mTOR. Annu. Rev. Immunol. 30, 39–68 (2012). polycongenic murine strains. Proc. Natl Acad. Sci. USA in anergic but exaggerated in chronically BAFF-
25. Chi, H. Regulation and function of mTOR signalling in 97, 6670–6675 (2000). exposed B cells. J. Immunol. 192, 3626–3636
T cell fate decisions. Nat. Rev. Immunol. 12, 325–338 50. Macintyre, A. N. et al. The glucose transporter (2014).
(2012). Glut1 is selectively essential for CD4 T cell 74. Aronov, M. & Tirosh, B. Metabolic control of plasma
26. Perl, A. Activation of mTOR (mechanistic target of activation and effector function. Cell Metab. 20, cell differentiation — what we know and what we don’t
rapamycin) in rheumatic diseases. Nat. Rev. 61–72 (2014). know. J. Clin. Immunol. 36 (Suppl. 1), 12–17 (2016).
Rheumatol. 12, 169–182 (2016). 51. Jacobs, S. R. et al. Glucose uptake is limiting in T cell 75. Benhamron, S., Pattanayak, S. P., Berger, M. &
27. Zeng, H. et al. mTORC1 couples immune signals and activation and requires CD28‑mediated Akt- Tirosh, B. mTOR activation promotes plasma cell
metabolic programming to establish Treg-cell function. dependent and independent pathways. J. Immunol. differentiation and bypasses XBP‑1 for
Nature 499, 485–490 (2013). 180, 4476–4486 (2008). immunoglobulin secretion. Mol. Cell. Biol. 35,
28. Craft, J. E. Follicular helper T cells in immunity and 52. Yang, Z. C. & Liu, Y. Hypoxia-inducible factor‑1α and 153–166 (2015).
systemic autoimmunity. Nat. Rev. Rheumatol. 8, autoimmune lupus, arthritis. Inflammation 39, 76. Wu, T. et al. Shared signaling networks active in B cells
337–347 (2012). 1268–1273 (2016). isolated from genetically distinct mouse models of
29. Blanco, P., Ueno, H. & Schmitt, N. T follicular helper 53. Le Buanec, H. et al. IFN-α and CD46 stimulation are lupus. J. Clin. Invest. 117, 2186–2196 (2007).
(Tfh) cells in lupus: activation and involvement in SLE associated with active lupus and skew natural T 77. Zeng, Q. et al. Rapamycin inhibits BAFF-stimulated
pathogenesis. Eur. J. Immunol. 46, 281–290 (2016). regulatory cell differentiation to type 1 regulatory T cell proliferation and survival by suppressing mTOR-
30. Ray, J. P. et al. The interleukin‑2‑mTORc1 kinase axis (Tr1) cells. Proc. Natl Acad. Sci. USA 108, mediated PP2A‑Erk1/2 signaling pathway in normal
defines the signaling, differentiation, and metabolism 18995–19000 (2011). and neoplastic B‑lymphoid cells. Cell. Mol. Life Sci.
of T helper 1 and follicular B helper T cells. Immunity 54. Kolev, M. et al. Complement regulates nutrient influx 72, 4867–4884 (2015).
43, 690–702 (2015). and metabolic reprogramming during Th1 cell 78. Lam, W. Y. et al. Mitochondrial pyruvate import
31. Ramiscal, R. R. et al. Attenuation of AMPK signaling responses. Immunity 42, 1033–1047 (2015). promotes long-term survival of antibody-secreting
by ROQUIN promotes T follicular helper cell 55. Kidani, Y. & Bensinger, S. J. Lipids rule: resetting plasma cells. Immunity 45, 60–73 (2016).
formation. eLife 4, e08698 (2015). lipid metabolism restores T cell function in systemic 79. Pathak, S. et al. Fatty acid amide hydrolase regulates
32. Pratama, A. et al. MicroRNA‑146a regulates ICOS- lupus erythematosus. J. Clin. Invest. 124, 482–485 peripheral B cell receptor revision, polyreactivity, and
ICOSL signalling to limit accumulation of T follicular (2014). B1 cells in lupus. J. Immunol. 196, 1507–1516
helper cells and germinal centres. Nat. Commun. 6, 56. Krishnan, S. et al. Alterations in lipid raft composition (2016).
6436 (2015). and dynamics contribute to abnormal T cell responses 80. Lugar, P. L., Love, C., Grammer, A. C., Dave, S. S. &
33. Zeng, H. et al. mTORC1 and mTORC2 kinase signaling in systemic lupus erythematosus. J. Immunol. 172, Lipsky, P. E. Molecular characterization of circulating
and glucose metabolism drive follicular helper t cell 7821–7831 (2004). plasma cells in patients with active systemic lupus
differentiation. Immunity 45, 540–554 (2016). 57. Jury, E. C., Isenberg, D. A., Mauri, C. & erythematosus. PLoS ONE 7, e44362 (2012).
34. Fernandez, D. & Perl, A. mTOR signaling: a central Ehrenstein, M. R. Atorvastatin restores Lck 81. Aprahamian, T. et al. The peroxisome proliferator-
pathway to pathogenesis in systemic lupus expression and lipid raft-associated signaling in T activated receptor γ agonist rosiglitazone ameliorates
erythematosus? Discov. Med. 9, 173–178 (2010). cells from patients with systemic lupus murine lupus by induction of adiponectin. J. Immunol.
35. Yin, Y. et al. Normalization of CD4+ T cell metabolism erythematosus. J. Immunol. 177, 7416–7422 182, 340–346 (2009).
reverses lupus. Sci. Transl Med. 7, 274ra18 (2015). (2006). 82. Aprahamian, T. R., Bonegio, R. G., Weitzner, Z.,
36. Yin, Y. et al. Glucose oxidation is critical for CD4+ 58. McDonald, G. et al. Normalizing glycosphingolipids Gharakhanian, R. & Rifkin, I. R. Peroxisome
T cell activation in a mouse model of systemic lupus restores function in CD4+ T cells from lupus patients. proliferator-activated receptor gamma agonists in
erythematosus. J. Immunol. 196, 80–90 (2016). J. Clin. Invest. 124, 712–724 (2014). the prevention and treatment of murine systemic
37. Lui, S. L. et al. Rapamycin attenuates the severity of 59. Deng, G. M. & Tsokos, G. C. Cholera toxin B lupus erythematosus. Immunology 142, 363–373
established nephritis in lupus-prone NZB/W F1 mice. accelerates disease progression in lupus-prone mice (2014).
Nephrol. Dial. Transplant. 23, 2768–2776 (2008). by promoting lipid raft aggregation. J. Immunol. 181, 83. Venegas-Pont, M. et al. Rosiglitazone decreases blood
38. Lai, Z. W. et al. Mechanistic target of rapamycin 4019–4026 (2008). pressure and renal injury in a female mouse model of
activation triggers IL‑4 production and necrotic death 60. Yang, W. et al. Potentiating the antitumour response systemic lupus erythematosus. Am. J. Physiol. Regul.
of double-negative T cells in patients with systemic of CD8+ T cells by modulating cholesterol metabolism. Integr. Comp. Physiol. 296, R1282–R1289 (2009).
lupus erythematosus. J. Immunol. 191, 2236–2246 Nature 531, 651–655 (2016). 84. Zhao, W. et al. The peroxisome proliferator-activated
(2013). 61. Wang, F., Beck-Garcia, K., Zorzin, C., receptor gamma agonist pioglitazone improves
39. Kato, H. & Perl, A. Mechanistic target of rapamycin Schamel, W. W. A. & Davis, M. M. Inhibition of cardiometabolic risk and renal inflammation in murine
complex 1 expands Th17 and IL‑4+ CD4‑CD8- double- T cell receptor signaling by cholesterol sulfate, a lupus. J. Immunol. 183, 2729–2740 (2009).
negative T cells and contracts regulatory T cells in naturally occurring derivative of membrane 85. O’Neill, L. A. & Pearce, E. J. Immunometabolism
systemic lupus erythematosus. J. Immunol. 192, cholesterol. Nat. Immunol. 17, 844–850 (2016). governs dendritic cell and macrophage function.
4134–4144 (2014). 62. Swamy, M. et al. A cholesterol-based allostery model J. Exp. Med. 213, 15–23 (2016).
40. Fernandez, D. R. et al. Activation of mammalian of T cell receptor phosphorylation. Immunity 44, 86. Ravishankar, B. et al. Tolerance to apoptotic cells is
target of rapamycin controls the loss of TCRζ in 1091–1101 (2016). regulated by indoleamine 2,3‑dioxygenase. Proc. Natl
lupus T cells through HRES‑1/Rab4‑regulated 63. Hu, X. et al. Sterol metabolism controls TH17 Acad. Sci. USA 109, 3909–3914 (2012).
lysosomal degradation. J. Immunol. 182, differentiation by generating endogenous RORγ 87. Ravishankar, B. et al. The amino acid sensor GCN2
2063–2073 (2009). agonists. Nat. Chem. Biol. 11, 141–147 (2015). inhibits inflammatory responses to apoptotic cells
41. Perl, A. et al. Comprehensive metabolome analyses 64. Ulivieri, C. & Baldari, C. T. Statins: from cholesterol- promoting tolerance and suppressing systemic
reveal N‑acetylcysteine-responsive accumulation of lowering drugs to novel immunomodulators for the autoimmunity. Proc. Natl Acad. Sci. USA 112,
kynurenine in systemic lupus erythematosus: treatment of Th17‑mediated autoimmune diseases. 10774–10779 (2015).
implications for activation of the mechanistic target of Pharmacol. Res. 88, 41–52 (2014). 88. Tsalikis, J., Croitoru, D. O., Philpott, D. J. &
rapamycin. Metabolomics 11, 1157–1174 (2015). 65. Waddington, K. E., Jury, E. C. & Pineda-Torra, I. Liver Girardin, S. E. Nutrient sensing and metabolic stress
42. Psarelis, S. & Nikiphorou, E. Coexistence of SLE, X receptors in immune cell function in humans. pathways in innate immunity. Cell. Microbiol. 15,
tuberous sclerosis and aggressive natural killer-cell Biochem. Soc. Trans. 43, 752–757 (2015). 1632–1641 (2013).
leukaemia: coincidence or correlated? Lupus 26, 66. Jeon, J. Y. et al. Liver X receptors alpha gene 89. McGaha, T. L. IDO‑GCN2 and autophagy in
107–108 (2017). (NR1H3) promoter polymorphisms are associated inflammation. Oncotarget 6, 21771–21772 (2015).
43. Olde Bekkink, M., Ahmed-Ousenkova, Y. M., with systemic lupus erythematosus in Koreans. 90. Eleftheriadis, T. et al. Differential effects of the two
Netea, M. G., van der Velden, W. J. & Berden, J. H. Arthritis Res. Ther. 16, R112 (2014). amino acid sensing systems, the GCN2 kinase and the
Coexistence of systemic lupus erythematosus, tuberous 67. Cui, G. et al. Liver X receptor (LXR) mediates negative mTOR complex 1, on primary human alloreactive
sclerosis and aggressive natural killer-cell leukaemia: regulation of mouse and human Th17 differentiation. CD4+ T‑cells. Int. J. Mol. Med. 37, 1412–1420
coincidence or correlated? Lupus 25, 766–771 (2016). J. Clin. Invest. 121, 658–670 (2011). (2016).
10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrrheum
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
F O C U S O N I M M U N O M E TA
RB OILEIW
EV SMS
91. Sukhbaatar, N., Hengstschlager, M. & Weichhart, T. 109. Shi, L. Z. et al. HIF1α–dependent glycolytic pathway 127. Pasquier, B. Autophagy inhibitors. Cell. Mol. Life Sci.
mTOR-mediated regulation of dendritic cell orchestrates a metabolic checkpoint for the 73, 985–1001 (2016).
differentiation and function. Trends Immunol. 37, differentiation of TH17 and Treg cells. J. Exp. Med. 128. Domhan, S. et al. Molecular mechanisms of the
778–789 (2016). 208, 1367–1376 (2011). antiangiogenic and antitumor effects of mycophenolic
92. Wang, Y. et al. Tuberous sclerosis 1 (Tsc1)-dependent 110. Kohler, T., Reizis, B., Johnson, R. S., Weighardt, H. & acid. Mol. Cancer Ther. 7, 1656–1668 (2008).
metabolic checkpoint controls development of Forster, I. Influence of hypoxia-inducible factor 1α on 129. Dun, B. Y. et al. Transcriptomic changes induced by
dendritic cells. Proc. Natl Acad. Sci. USA 110, dendritic cell differentiation and migration. Eur. mycophenolic acid in gastric cancer cells. Am. J. Transl
E4894–E4903 (2013). J. Immunol. 42, 1226–1236 (2012). Res. 6, 28–42 (2014).
93. Wu, D. et al. Type 1 interferons induce changes in 111. Cho, S. H. et al. Germinal centre hypoxia and regulation 130. He, X. et al. Mycophenolic acid-mediated suppression of
core metabolism that are critical for immune of antibody qualities by a hypoxia response system. human CD4+ T cells: more than mere guanine
function. Immunity 44, 1325–1336 (2016). Nature 537, 234–238 (2016). nucleotide deprivation. Am. J. Transplant. 11, 439–449
94. Berod, L. et al. De novo fatty acid synthesis controls 112. Feng, C. C. et al. Lack of association between the (2011).
the fate between regulatory T and T helper 17 cells. polymorphisms of hypoxia-inducible factor 1A (HIF1A) 131. Stylianou, K. et al. The PI3K/Akt/mTOR pathway is
Nat. Med. 20, 1327–1333 (2014). gene and SLE susceptibility in a Chinese population. activated in murine lupus nephritis and downregulated
95. Smith, C. K. & Kaplan, M. J. The role of neutrophils Immunogenetics 66, 9–13 (2014). by rapamycin. Nephrol. Dial. Transplant. 26, 498–508
in the pathogenesis of systemic lupus 113. Davidson, A. What is damaging the kidney in lupus (2011).
erythematosus. Curr. Opin. Rheumatol. 27, nephritis? Nat. Rev. Rheumatol. 12, 143–153 (2016). 132. Rhoads, J. P., Major, A. S. & Rathmell, J. C. Fine tuning
448–453 (2015). 114. Bethunaickan, R. et al. Identification of stage-specific of immune metabolism for the treatment of rheumatic
96. Lood, C. et al. Neutrophil extracellular traps genes associated with lupus nephritis and response to diseases. Nat. Rev. Rheumatol. (in press).
enriched in oxidized mitochondrial DNA are remission induction in (NZB x NZW)F1 and NZM2410 133. Fernández-Ramos, A. A., Poindessous, V., Marchetti-
interferogenic and contribute to lupus-like disease. mice. Arthritis Rheumatol. 66, 2246–2258 (2014). Laurent, C., Pallet, N. & Loriot, M.‑A. The effect of
Nat. Med. 22, 146–153 (2016). 115. Mashmoushi, A. K. & Oates, J. C. Lipopolysaccharide immunosuppressive molecules on T‑cell metabolic
97. Caielli, S. et al. Oxidized mitochondrial nucleoids induces inducible nitric oxide synthase-dependent reprogramming. Biochimie 127, 23–36 (2016).
released by neutrophils drive type I interferon podocyte dysfunction via a hypoxia-inducible factor 1α 134. Tanaka, N., Kusunoki, N., Kusunoki, Y., Hasunuma, T. &
production in human lupus. J. Exp. Med. 213, and cell division control protein 42 and Ras-related C3 Kawai, S. Resistin is associated with the inflammation
697–713 (2016). botulinum toxin substrate 1 pathway. Free Radic. Biol. process in patients with systemic autoimmune diseases
98. Campbell, A. M., Kashgarian, M. & Shlomchik, M. J. Med. 84, 185–195 (2015). undergoing glucocorticoid therapy: comparison with
NADPH oxidase inhibits the pathogenesis of systemic 116. Deng, W. et al. Hypoxia inducible factor‑1 alpha leptin and adiponectin. Mod. Rheumatol. 23, 8–18
lupus erythematosus. Sci. Transl Med. 4, 157ra141 promotes mesangial cell proliferation in lupus nephritis. (2013).
(2012). Am. J. Nephrol. 40, 507–515 (2014). 135. Tanaka, N., Masuoka, S., Kusunoki, N., Nanki, T. &
99. Bao, Y. et al. mTOR and differential activation of 117. Bengtsson, A. A. et al. Metabolic profiling of systemic Kawai, S. Serum resistin level and progression of
mitochondria orchestrate neutrophil chemotaxis. lupus erythematosus and comparison with primary atherosclerosis during glucocorticoid therapy for
J. Cell Biol. 210, 1153–1164 (2015). Sjögren’s syndrome and systemic sclerosis. PLoS ONE systemic autoimmune diseases. Metabolites 6, E28
100. Oaks, Z. & Perl, A. Metabolic control of the 11, e0159384 (2016). (2016).
epigenome in systemic lupus erythematosus. 118. Lood, C. et al. Type I interferon-mediated skewing of the 136. Mejia, P. et al. Dietary restriction protects against
Autoimmunity 47, 256–264 (2014). serotonin synthesis is associated with severe disease in experimental cerebral malaria via leptin modulation
101. Richardson, B. C. & Patel, D. R. Epigenetics in 2013: systemic lupus erythematosus. PLoS ONE 10, and T‑cell mTORC1 suppression. Nat. Commun. 6,
DNA methylation and miRNA — key roles in systemic e0125109 (2015). 6050 (2015).
autoimmunity. Nat. Rev. Rheumatol. 10, 72–74 119. Pedersen, H. K. et al. Human gut microbes impact host 137. Zhao, W. et al. The peroxisome-proliferator activated
(2014). serum metabolome and insulin sensitivity. Nature 535, receptor‑γ agonist pioglitazone modulates aberrant
102. Wu, T. et al. Metabolic disturbances associated with 376–381 (2016). T cell responses in systemic lupus erythematosus. Clin.
systemic lupus erythematosus. PLoS ONE 7, e37210 120. Hevia, A. et al. Intestinal dysbiosis associated with Immunol. 149, 119–132 (2013).
(2012). systemic lupus erythematosus. mBio 5, e01548‑14 138. Bride, K. L. et al. Sirolimus is effective in relapsed/
103. Coit, P. et al. Epigenetic reprogramming in naive (2014). refractory autoimmune cytopenias: results of a
CD4+ T cells favoring T cell activation and non‑Th1 121. Lopez, P. et al. Th17 responses and natural IgM prospective multi-institutional trial. Blood 127, 17–28
effector T cell immune response as an early event in antibodies are related to gut microbiota composition in (2016).
lupus flares. Arthritis Rheumatol. 68, 2200–2209 systemic lupus erythematosus patients. Sci. Rep. 6, 139. Oaks, Z., Winans, T., Huang, N., Banki, K. & Perl, A.
(2016). 24072 (2016). Activation of the mechanistic target of rapamycin in
104. Zhao, E. et al. Cancer mediates effector T cell 122. Rojo, D. et al. Ranking the impact of human health SLE: explosion of evidence in the last five years. Curr.
dysfunction by targeting microRNAs and EZH2 via disorders on gut metabolism: systemic lupus Rheumatol. Rep. 18, 73 (2016).
glycolysis restriction. Nat. Immunol. 17, 95–103 erythematosus and obesity as study cases. Sci. Rep. 5, 140. Petri, M. et al. Derivation and validation of the
(2016). 8310 (2015). Systemic Lupus International Collaborating Clinics
105. Regna, N. L. et al. HDAC expression and activity is 123. Serrano-Villar, S. et al. HIV infection results in metabolic classification criteria for systemic lupus erythematosus.
upregulated in diseased lupus-prone mice. Int. alterations in the gut microbiota different from those Arthritis Rheum. 64, 2677–2686 (2012).
Immunopharmacol. 29, 494–503 (2015). induced by other diseases. Sci. Rep. 6, 26192 (2016).
106. Mishra, N., Reilly, C. M., Brown, D. R., Ruiz, P. & 124. Keller, K. E., Tan, I. S. & Lee, Y. S. SAICAR stimulates Acknowledgements
Gilkeson, G. S. Histone deacetylase inhibitors pyruvate kinase isoform M2 and promotes cancer cell The author’s work is supported by Alliance for Lupus
modulate renal disease in the MRL-lpr/lpr mouse. survival in glucose-limited conditions. Science 338, Research Target Identification in Lupus grants (TIL 85521
J. Clin. Invest. 111, 539–552 (2003). 1069–1072 (2012). and TIL 75018).
107. Long, H., Yin, H., Wang, L., Gershwin, M. E. & Lu, Q. 125. Mills, E. & O’Neill, L. A. Succinate: a metabolic signal
The critical role of epigenetics in systemic lupus in inflammation. Trends Cell Biol. 24, 313–320 Competing interests statement
erythematosus and autoimmunity. J. Autoimmun. 74, (2014). The author declares no competing interests.
118–138 (2016). 126. Correa-Oliveira, R., Fachi, J. L., Vieira, A., Sato, F. T. &
108. Corcoran, S. E. & O’Neill, L. A. HIF1α and metabolic Vinolo, M. A. Regulation of immune cell function by Publisher’s note
reprogramming in inflammation. J. Clin. Invest. 126, short-chain fatty acids. Clin. Transl Immunology 5, e73 Springer Nature remains neutral with regard to jurisdictional
3699–3707 (2016). (2016). claims in published maps and institutional affiliations.
NATURE REVIEWS | RHEUMATOLOGY ADVANCE ONLINE PUBLICATION | 11
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
You might also like
- A Simple Guide to the Blood Cells, Related Diseases And Use in Disease DiagnosisFrom EverandA Simple Guide to the Blood Cells, Related Diseases And Use in Disease DiagnosisNo ratings yet
- Littelfuse EVI EV Charging Infrastructure Presentation PDFDocument19 pagesLittelfuse EVI EV Charging Infrastructure Presentation PDFRaka Pratindy100% (1)
- Training Sinal PDFDocument15 pagesTraining Sinal PDFlobitoferoz81No ratings yet
- PAMDocument14 pagesPAMRashed IslamNo ratings yet
- Seoul FoodSeoul Official Dining Guide BookDocument53 pagesSeoul FoodSeoul Official Dining Guide Bookkozaza: book homes in KoreaNo ratings yet
- Polynesian MigrationsDocument2 pagesPolynesian Migrationskinneyjeffrey100% (1)
- Basic Immunology NotesDocument31 pagesBasic Immunology NotesKannan MarikaniNo ratings yet
- Cellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsFrom EverandCellular and Molecular Mechanisms of Inflammation: Receptors of Inflammatory Cells: Structure—Function RelationshipsCharles G. CochraneNo ratings yet
- Reviews: Inflammation in Gout: Mechanisms and Therapeutic TargetsDocument9 pagesReviews: Inflammation in Gout: Mechanisms and Therapeutic TargetsBless MineNo ratings yet
- Primer: Chronic Lymphocytic LeukaemiaDocument22 pagesPrimer: Chronic Lymphocytic Leukaemialengers poworNo ratings yet
- Enfermedades Mitocondriales.Document16 pagesEnfermedades Mitocondriales.cristobalarancibia71No ratings yet
- Tsokos 2016Document15 pagesTsokos 2016karen rinconNo ratings yet
- Metaplasia. Nature ReviewsDocument11 pagesMetaplasia. Nature ReviewsCamila RodríguezNo ratings yet
- The Microbiome and Innate ImmunityDocument10 pagesThe Microbiome and Innate ImmunityGabriel HernándezNo ratings yet
- PRIMER de LES 2016 PDFDocument21 pagesPRIMER de LES 2016 PDFAndres DoblerNo ratings yet
- The Basis For The Immunoregulatory Role of Macrophages and Other Accessory Cells.Document7 pagesThe Basis For The Immunoregulatory Role of Macrophages and Other Accessory Cells.Cristian Gutiérrez VeraNo ratings yet
- Aritículo 001Document15 pagesAritículo 001Mario HonoresNo ratings yet
- Nature - Immune Regulation by Glucocorticoids - 2017Document16 pagesNature - Immune Regulation by Glucocorticoids - 2017Matheus AugustoNo ratings yet
- Reviews: Marked For Death: Targeting Epigenetic Changes in CancerDocument23 pagesReviews: Marked For Death: Targeting Epigenetic Changes in CancerLorena RamosNo ratings yet
- Immunological Reviews - 2020 - Makowski - Immunometabolism From Basic Mechanisms To TranslationDocument10 pagesImmunological Reviews - 2020 - Makowski - Immunometabolism From Basic Mechanisms To TranslationOrfa Esther Barrios PazosNo ratings yet
- Targeting Neoantigens To Augment Antitumour ImmunityDocument14 pagesTargeting Neoantigens To Augment Antitumour Immunitylaura isabellaNo ratings yet
- Metabolomics Beyond Biomarkers and Towards MechanismsDocument9 pagesMetabolomics Beyond Biomarkers and Towards Mechanismsanis k.No ratings yet
- At The Crossroads of Lipid Metabolism and InflammationDocument7 pagesAt The Crossroads of Lipid Metabolism and InflammationChow Sing SingNo ratings yet
- Nrgastro 2017 38Document15 pagesNrgastro 2017 38Fasya DaffaNo ratings yet
- Autophagy in Acute Brain InjuryDocument18 pagesAutophagy in Acute Brain InjuryGaryNo ratings yet
- 10 1038@nrneph 2017 85 PDFDocument13 pages10 1038@nrneph 2017 85 PDFSirGonzNo ratings yet
- All About VcamDocument8 pagesAll About VcamIkhsan AliNo ratings yet
- محاضرةة الانسجةDocument17 pagesمحاضرةة الانسجةAymen MouradNo ratings yet
- Journal Reading 1Document28 pagesJournal Reading 1vesriyogaNo ratings yet
- Innate Lymphoid Cells - 10 Years OnDocument13 pagesInnate Lymphoid Cells - 10 Years OnMario MazónNo ratings yet
- Etiology and Pathogenesis of OLP - Kurago 2015 PDFDocument9 pagesEtiology and Pathogenesis of OLP - Kurago 2015 PDFintanNo ratings yet
- Role of Cytokines in The Pathophysiology of Systemic Lupus ErythematosusDocument12 pagesRole of Cytokines in The Pathophysiology of Systemic Lupus ErythematosusKaren Rincón DNo ratings yet
- The Mucosal Immune System in The Oral Cavity-An Orchestra of T Cell DiversityDocument8 pagesThe Mucosal Immune System in The Oral Cavity-An Orchestra of T Cell DiversityReiska KumalaNo ratings yet
- Otto 2017Document23 pagesOtto 2017yankusumaNo ratings yet
- Genetics and Pathogenesis of Systemic Lupus Erythematosus and Lupus Nephritis PDFDocument13 pagesGenetics and Pathogenesis of Systemic Lupus Erythematosus and Lupus Nephritis PDFhemer hadyn calderon alvitesNo ratings yet
- 2017, Regulation of Genome Organization and Gene Expression by Nuclear MechanotransductionDocument11 pages2017, Regulation of Genome Organization and Gene Expression by Nuclear MechanotransductionErnesto RojoNo ratings yet
- Estefania Gallego PonenciaDocument16 pagesEstefania Gallego PonenciaJilberth Hermann CandeloNo ratings yet
- Chapter Three: The Lymphoid SystemDocument4 pagesChapter Three: The Lymphoid SystemaiaiNo ratings yet
- Single-Cell Metabolic Profiling of Human Cytotoxic T Cells: ArticlesDocument19 pagesSingle-Cell Metabolic Profiling of Human Cytotoxic T Cells: ArticlesShivaprakash Jagalur MuttNo ratings yet
- Primer: Amyotrophic Lateral SclerosisDocument19 pagesPrimer: Amyotrophic Lateral SclerosisBerkay ALpayNo ratings yet
- Cytokines in The Innate Immune ResponseDocument3 pagesCytokines in The Innate Immune ResponseNicole Tan100% (1)
- White Blood CellDocument21 pagesWhite Blood CellAnonymous 0C4OZmRNo ratings yet
- NRDP 20174Document17 pagesNRDP 20174EccoNo ratings yet
- 2a PDFDocument11 pages2a PDFAndrea Il MiodoNo ratings yet
- Lectura Seminario 3 - NF1Document17 pagesLectura Seminario 3 - NF1Diego SoteloNo ratings yet
- Reviews: Microbiota: A Key Orchestrator of Cancer TherapyDocument15 pagesReviews: Microbiota: A Key Orchestrator of Cancer TherapyTiago MachadoNo ratings yet
- Beyond Binding Antibody - Lu Et Al. NatureDocument17 pagesBeyond Binding Antibody - Lu Et Al. NatureSamia NouhNo ratings yet
- Cytokines and Their Role in ImmunityDocument12 pagesCytokines and Their Role in ImmunitySarvesh PatilNo ratings yet
- The Mucosal Immune System in The Oral Cavity - An Orchestra of T Cell DiversityDocument13 pagesThe Mucosal Immune System in The Oral Cavity - An Orchestra of T Cell Diversitywho disNo ratings yet
- Cells and Mediators of Chronic InflammationDocument52 pagesCells and Mediators of Chronic Inflammationtravis efraimNo ratings yet
- Sex Differences in Immune Responses: Sabra L. Klein and Katie L. FlanaganDocument13 pagesSex Differences in Immune Responses: Sabra L. Klein and Katie L. FlanaganannisaNo ratings yet
- Pathomorphology of Immune System. Reactions and Mech Anisms of HypersensitivityDocument72 pagesPathomorphology of Immune System. Reactions and Mech Anisms of HypersensitivityEdi Kerina SembiringNo ratings yet
- Dendritic Cell BiologyDocument12 pagesDendritic Cell BiologyHelena QuintNo ratings yet
- Cells 09 00334 v2Document15 pagesCells 09 00334 v2Vivien WuNo ratings yet
- Autophagy Pathway 1Document16 pagesAutophagy Pathway 1Na-yeon KimNo ratings yet
- Godfrey WH and Kongberg MD 2020 - Metabolic Enzymes and InflammationDocument22 pagesGodfrey WH and Kongberg MD 2020 - Metabolic Enzymes and Inflammationeri.pinedarNo ratings yet
- Immunology of Periodontal DiseasesDocument9 pagesImmunology of Periodontal DiseasesoladunniNo ratings yet
- Coba Browser Baru Dengan Terjemahan Otomatis.: Plaque WhenDocument5 pagesCoba Browser Baru Dengan Terjemahan Otomatis.: Plaque WhenDiana SuhartiNo ratings yet
- Barturen 2018Document20 pagesBarturen 2018jezy2014No ratings yet
- Piezos Thrive Under PressureDocument13 pagesPiezos Thrive Under PressureВладимир ДружининNo ratings yet
- Name: Abby Yong I.D.: 14WAR03484 Group: RBS2 Group 2 Date: 30 September 2015Document10 pagesName: Abby Yong I.D.: 14WAR03484 Group: RBS2 Group 2 Date: 30 September 2015Abby YongNo ratings yet
- About LymphomaDocument17 pagesAbout LymphomaSelviNo ratings yet
- Jurnal LeukimiaDocument13 pagesJurnal LeukimiaNadiya SujatmikoNo ratings yet
- Renal CellDocument10 pagesRenal CellEss liNo ratings yet
- Cellular and Molecular Mechanisms of Inflammation: Vascular Adhesion MoleculesFrom EverandCellular and Molecular Mechanisms of Inflammation: Vascular Adhesion MoleculesCharles G. CochraneNo ratings yet
- Health Group3Document29 pagesHealth Group3Angela OrenseNo ratings yet
- Country Item Name Litre Quart Pint Nip 700 ML IndiaDocument17 pagesCountry Item Name Litre Quart Pint Nip 700 ML Indiajhol421No ratings yet
- Acer Iconia Tab W500 Pegatron EAB00 SchematicsDocument60 pagesAcer Iconia Tab W500 Pegatron EAB00 SchematicsIIIkwarkaNo ratings yet
- WBMDocument90 pagesWBMMiguel RegisNo ratings yet
- O Level Physics ATP ReferencesDocument4 pagesO Level Physics ATP ReferencesHassan Ali BhuttaNo ratings yet
- H250 H250 H250 H250: Variable Area Flowmeter With 3W2 Angular Position TransmitterDocument40 pagesH250 H250 H250 H250: Variable Area Flowmeter With 3W2 Angular Position TransmitterJustine MarashanyeNo ratings yet
- NUMBERS 2 Percentage ChangeDocument2 pagesNUMBERS 2 Percentage ChangeDinangaNo ratings yet
- Lighting Movements-The Fox On The FairwayDocument1 pageLighting Movements-The Fox On The FairwayabneypaigeNo ratings yet
- Spring Diameter of Spring Coil/cm Elastic Limit/n Spring Constant/nm-1 MaterialDocument4 pagesSpring Diameter of Spring Coil/cm Elastic Limit/n Spring Constant/nm-1 MaterialZahari Bin BakriNo ratings yet
- In-Lab Sharp-Edged Orifice Meter ReportDocument9 pagesIn-Lab Sharp-Edged Orifice Meter ReportLiliane AlameddineNo ratings yet
- J-20 Stealth Fighter Design Balances Speed and Agility - Defense Content From Aviation WeekDocument9 pagesJ-20 Stealth Fighter Design Balances Speed and Agility - Defense Content From Aviation WeekMahesNo ratings yet
- Stationery Stock CardDocument100 pagesStationery Stock CardHuny BunyNo ratings yet
- BB204-Toddler Bed Assembly InstructionsDocument10 pagesBB204-Toddler Bed Assembly InstructionsCaloi PastorfideNo ratings yet
- Jammer Final Report Mod PDFDocument41 pagesJammer Final Report Mod PDFNourhanGamalNo ratings yet
- Numerology 666 Meaning: What Angel Number 666 REALLY Means!Document2 pagesNumerology 666 Meaning: What Angel Number 666 REALLY Means!LlNo ratings yet
- January 2005 6677 Mechanics M1: Mark SchemeDocument7 pagesJanuary 2005 6677 Mechanics M1: Mark SchemeWael TareqNo ratings yet
- AE240 Notes Early-Airfoil-Development-Handout-1Document5 pagesAE240 Notes Early-Airfoil-Development-Handout-1mohamedNo ratings yet
- Updated DOTr Directory As of 29 October 2021Document9 pagesUpdated DOTr Directory As of 29 October 2021Twinkle MiguelNo ratings yet
- The National TerritoryDocument39 pagesThe National TerritoryRan RanNo ratings yet
- Apacer SV250 CFast BiCS5 AA2 XX5XXX XXXEX Spec v1 - 3107344Document25 pagesApacer SV250 CFast BiCS5 AA2 XX5XXX XXXEX Spec v1 - 3107344ManunoghiNo ratings yet
- Compliant Offshore StructureDocument50 pagesCompliant Offshore Structureapi-27176519100% (4)
- Lonza ManualsProductInstructions Determination of Protein Concentration 31460Document2 pagesLonza ManualsProductInstructions Determination of Protein Concentration 31460sydneypadillioNo ratings yet
- Managing Housekeeping Inventory: Ihm MumbaiDocument5 pagesManaging Housekeeping Inventory: Ihm MumbaiAbhishek ChowdhuryNo ratings yet
- RymesDocument6 pagesRymesFarida YesminNo ratings yet
- Syllabus: Survey Training Institute, H-8/2 IslamabadDocument7 pagesSyllabus: Survey Training Institute, H-8/2 Islamabadsajid khanNo ratings yet