Professional Documents
Culture Documents
Isolated Diffuse Ground-Glass Opacity in Thoracic CT
Uploaded by
Ayşe BanuCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Isolated Diffuse Ground-Glass Opacity in Thoracic CT
Uploaded by
Ayşe BanuCopyright:
Available Formats
Chest Imaging
Miller and Shah
Ground-Glass Opacity in Thoracic CT
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
Review
Isolated Diffuse Ground-Glass Opacity in Thoracic CT:
Causes and Clinical Presentations
Wallace T. Miller, Jr.1 and Rosita M. Shah
Miller WT, Shah R
round-glass opacity (GGO) is de- with simple clinical information. By isolated, developing dyspnea, and inpatients who are
G fined as increased attenuation of
the lung parenchyma without ob-
scuration of the pulmonary vascu-
we mean patients who show only GGOs with-
out other interstitial or alveolar findings. By
diffuse, we mean patients with GGO that in-
acutely ill. We will review these clinical scenar-
ios and the etiologies most commonly encoun-
tered with each scenario.
lar markings on CT images. This was volves the majority of both lungs.
originally described with reference to thin-
section (high-resolution) CT with collima- Immunocompromised Patients
tions of approximately 1 mm. However, GGO Objective In scenario one, an immunocompromised
also may be evident on thicker-section images We have chosen to emphasize clinical in- patient presents with dyspnea and often fever.
and will have a similar meaning. GGO may be formation as the best means of narrowing the Patients included in this category are HIV-
the result of a wide variety of interstitial and differential diagnosis of patients with isolated positive individuals, patients who have under-
alveolar diseases and frequently represents a diffuse GGO (ID-GGO) because there is sub- gone organ transplantation, and patients who
nonspecific finding [1, 2]. GGOs often will be stantial overlap in the appearance of ID-GGO have received high-dose corticosteroids. In
present in the company of other interstitial or among the various etiologies. Thus, in our ex- this scenario, the opportunistic infections
alveolar findings on CT. As an alveolar find- perience, the various subtypes of GGO—for that cause ID-GGO form the primary differ-
ing, GGO represents partially filled alveoli example, centrilobular nodules and mosaic ential diagnosis.
and often is found at the margins of the con- attenuation—are not able to be discriminated
solidated lung. With interstitial diseases, it among the causes of ID-GGO [9]. Infections Appearing as ID-GGO
has been associated with active inflammation Four large categories of diseases may produce Diffuse infections, particularly Pneu-
in some cases [3–8]. In other situations, GGO ID-GGO: diffuse pneumonias, primarily oppor- mocystis carinii pneumonia (PCP), are
adjacent to interstitial abnormalities repre- tunistic infections; some chronic interstitial dis- among the most common causes of ID-
sents fine fibrosis, below the resolution of CT eases; acute alveolar diseases; and a group of GGOs. In a series of pathologically proven
images. Therefore, if all causes of GGOs are unusual miscellaneous disorders [9]. Table 1 lists causes of ID-GGO, the most common
grouped together, there is an impossibly the most common causes of ID-GGO. causes were a variety of diffuse pneumo-
broad differential generated, which includes a There are five clinical scenarios in which ID- nias, which accounted for 38% (12 of 32) of
large number of interstitial diseases and a GGO is most often encountered: patients who cases [9]. Most of these infections are op-
large array of alveolar diseases. However, the are immunocompromised, patients who are re- portunistic and should be among the first en-
number of diseases that cause diffuse GGOs ceiving bone marrow–suppressing medications, tities to consider when ID-GGO is the
in isolation or as the predominant finding, is outpatients who have slowly progressive dysp- dominant finding on a CT scan of an immu-
relatively small and easily can be prioritized nea, inpatients and outpatients who have acutely nocompromised host.
Received April 19, 2004; accepted after revision July 1, 2004.
1Both authors: Department of Radiology, University of Pennsylvania School of Medicine, 3400 Spruce St., Silverstein 1, Philadelphia, PA 19104. Address correspondence to W. T. Miller
(wallacejr.miller@uphs.upenn.edu).
AJR 2005;184:613–622 0361–803X/05/1842–613 © American Roentgen Ray Society
AJR:184, February 2005 613
Miller and Shah
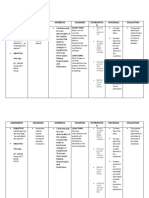
TABLE 1 Causes of Isolated Diffuse Ground-Glass Opacity CMV disease in patients with AIDS is associ-
ated with greater levels of immunosuppres-
Categories Types of Diseases and Infections sion and greater mortality rates than in the
Opportunistic infections Pneumocystis pneumonia (PCP) general HIV-positive population [25].
Cytomegalovirus pneumonia (CMV) Many patients in whom CMV can be de-
Herpes simplex virus pneumonia (HSV) tected in blood, urine, and respiratory secre-
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
Respiratory syncytial virus bronchiolitis
Other tions clinically will be asymptomatic. In
patients with clinical symptoms, fever, cough,
Chronic interstitial diseases Hypersensitivity pneumonitis (HP)
Desquamative interstitial pneumonia (DIP) dyspnea, tachypnea, and an increased alveo-
Respiratory bronchiolitis interstitial lung disease (RBILD) lar-arterial gradient (Aa gradient) most often
Nonspecific interstitial pneumonia (NSIP) will be the presenting symptoms [26].
Acute interstitial pneumonia (AIP) Many patients with CMV viremia will
Lymphocytic interstitial pneumonia (LIP)
have normal imaging studies. However, in
Sarcoidosis
those with imaging findings, CMV pneumo-
Acute alveolar diseases Pulmonary edema
nia usually will appear as ID-GGO on CT
Heart disease
Adult respiratory distress syndrome (ARDS) scans [23, 26, 27] (Fig. 2). In some cases,
Other small (< 5 mm) nodules may be detected and
Diffuse alveolar hemorrhage in more severe cases, diffuse consolidation
Other causes Drug toxicity may be present.
Pulmonary alveolar proteinosis (PAP) P. carinii and CMV pneumonias affect sim-
Bronchiolitis obliterans with organizing pneumonia (BOOP, COP) ilar populations, often have similar imaging
Bronchoalveolar carcinoma
characteristics, and often cannot be distin-
guished on the basis of imaging. In general,
Pneumocystis carinii pneumonia.—PCP is ID-GGOs, either uniformly distributed or PCP is more common; however, in certain se-
a globally distributed saprophytic fungus in a mosaic pattern, are the most common lect settings or situations, such as during the
[10]. Patients with AIDS and other causes of manifestations of PCP on CT scans [18] (Fig. first months after organ transplantation, CMV
immunosuppression, such as organ trans- 1). In HIV-positive patients, this appearance is a frequent cause of ID-GGO [23, 26, 27].
plant recipients, patients with lymphoprolif- is so characteristic of PCP that some physi- Herpes simplex virus.—Herpes viruses are
erative disorders, and patients on high-dose cians argue that it is pathognomonic of PCP a type of DNA virus, which may remain dor-
corticosteroids are predisposed to this op- and no further testing is necessary. With more mant within host cells and reactivate at times of
portunistic infection [11, 12]. Despite dra- severe disease, GGO may progress to consol- reduced host immunity. A large percentage of
matic declines in the incidence of PCP in idation. The CT appearance of PCP rarely the adult population is infected with herpes sim-
HIV-infected patients as a result of highly may take a variety of more unusual patterns plex virus (HSV), which in most cases produces
active antiretroviral therapy (HAART) and including upper-lobe-predominant disease, no clinical symptoms [28]. HSV pneumonia is a
PCP prophylaxis, PCP remains the most focal areas of consolidation, nodules, and rare event and most commonly is seen in immu-
common opportunistic infection in this pop- thin-walled cavities [18–22]. nocompromised patients such as organ trans-
ulation [11, 13, 14]. PCP most commonly Cytomegalovirus pneumonia.—Cytomega- plant recipients, patients with AIDS, patients
occurs in the 4th to 6th month following lovirus (CMV) is a DNA virus of the herpes with severe burns, and patients with malignan-
transplantation and may have up to a 47% group and like other herpes viruses, it can re- cies [29–32].
mortality rate [15, 16]. A history of high- main dormant within a host cell for years and Because it represents a reactivation infection,
dose corticosteroid administration, cancer be reactivated when host immune defenses herpes simplex pneumonia characteristically
chemotherapy, or a hematologic malignancy are depressed. CMV may be an important will occur in the first few months following or-
also may predispose a patient to PCP infec- pathogen in immunocompromised patients gan transplantation [33, 34]. Patients usually
tion [11, 14]. such as HIV-positive patients and in patients will have oral or genital ulcers before the onset
Patients characteristically will present who have undergone organ transplantation of pulmonary symptoms. Dyspnea, cough, and
with fever, nonproductive cough, and dysp- [12]. The majority of adults have been ex- fever herald the onset of pneumonia.
nea [17]. Marked hypoxemia also is charac- posed to CMV and, as a result, CMV infec- Herpes pneumonias may appear as ID-
teristic of PCP. In those patients who have tion usually is a reactivation of dormant foci. GGO, widespread consolidation, or a combi-
received corticosteroids, a characteristic In patients receiving organ transplants, the nation of both on chest radiographs and CT
presentation of PCP is the occurrence of fe- timing of immunosuppression is well defined, scans [35, 36]. Rarely, only GGO will be
ver, dyspnea, and ID-GGO toward the end of corresponding to the date of transplantation. present [35]. Associated small pleural effu-
the steroid taper. Survival with modern ther- Thus, the timing of CMV reactivation also is sions commonly are found both by CT and
apy has improved dramatically in patients well defined and most often occurs 1 to 6 chest radiographs [35].
with HIV and now approaches 90%. How- months following transplantation [23]. CMV Respiratory syncytial virus.—Respiratory
ever, PCP continues to have an ominous infection in HIV-positive individuals has de- syncytial virus (RSV) is a common cause of
prognosis in other patients, with a 30–60% clined dramatically with the institution of bronchiolitis and pneumonia in children and
mortality rate [11]. HAART [24]. However, the occurrence of adults. Infection is most likely to occur in the
614 AJR:184, February 2005
Ground-Glass Opacity in Thoracic CT
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
Fig. 1.—29-year-old HIV-positive man with Pneumocystis carinii pneumonia. High- Fig. 2.—36-year-old man with cytomegalovirus pneumonia following renal transplan-
resolution CT image through carina shows widespread ground-glass opacity uni- tation. High-resolution CT image through inferior hilum shows isolated diffuse
formly distributed across lungs. ground-glass opacity widely spread across both lungs.
late winter and early spring and commonly fections as a result of neutropenia but who many more. In a study of drug toxicity in pa-
causes fever, cough, dyspnea, and otalgia also are at risk for other causes of ID-GGO. tients with autologous bone marrow transplan-
with clinical signs of rales, rhonchi, or These patients frequently are thrombocy- tation, 65% of cases of drug toxicity manifested
wheezes. In immunocompetent adults, the topenic and are therefore at increased risk for as GGO [42].
course usually is self-limited and is treated diffuse aveolar hemorrhage, DAH. They also
on an outpatient basis. However, in immuno- may develop drug toxicity as a result of the Outpatients with Slowly
compromised adults, RSV infection may re- systemic chemotherapies they have received. Progressive Dyspnea
sult in a clinically significant pneumonia This leads to the differential of and drug tox- In this third scenario, an otherwise healthy
[37, 38]. icity. In our experience, drug toxicity is the outpatient will complain of mild chronic dysp-
The majority of patients with RSV pulmo- most difficult entity to diagnose and the most nea. Findings of the chest radiograph most of-
nary infection will have normal radiographic common cause of ID-GGO in this population. ten will appear normal or may show a faint
findings [39]. CT scans in 10 patients with In our study of the causes of ID-GGO, drug haze, which may be interpreted as diffuse
RSV infection following lung transplantation toxicity accounted for 4% of all pathology- GGO. In this situation, ID-GGO most often
revealed diffuse GGOs in seven patients, pul- proven cases and therefore represents an impor- will indicate one of the following chronic inter-
monary consolidation in five patients, and tree- tant cause of ID-GGO [9]. Because of the wide stitial diseases: HP, desquamative interstitial
in-bud opacities in four patients [40] (Fig. 3). variety of pharmacologic agents that can result pneumonia (DIP), respiratory bronchiolitis in-
Other viruses.—Many other viruses com- in ID-GGO, there are several histopathologic terstitial lung disease (RBILD), NSIP, acute in-
monly produce upper–respiratory tract illnesses patterns of drug-related damage to the pulmo- terstitial pneumonia (AIP), BOOP, and
and occasionally may produce a limited pneu- nary parenchyma. These include noncardio- sarcoidosis. Rarely, these patients will have
monia. It is likely that many of these will appear genic pulmonary edema, diffuse alveolar some of the unusual unclassified causes of ID-
as widespread or small focal regions of GGO, damage (DAD), nonspecific interstitial pneu- GGO such as pulmonary alveolar proteinosis
which are self-limited and radiographically re- monia (NSIP), DAH, bronchiolitis obliterans (PAP) or bronchoalveolar carcinoma (BAC). A
solve spontaneously. Because few of these pa- with organizing pneumonia (BOOP), hyper- history of smoking may be an important addi-
tients are definitively diagnosed, it is unknown sensitivity pneumonitis (HP), eosinophilic tional factor in this population. DIP and
how often ID-GGO is a manifestation of com- pneumonia, bronchiolitis obliterans, and ve- RBILD are seen almost exclusively among
munity-acquired viral pneumonias. noocclusive disease [41]. Note that the first six smokers and therefore would be unlikely diag-
patterns of damage listed here often will appear noses in patients who do not smoke.
Patients Who Have Received Bone as ID-GGO on CT scans. Drugs, which can
Marrow–Suppressing Chemotherapy cause permeability edema, include cytosine ar- Chronic Interstitial Diseases Appearing as ID-GGO
In scenario two, a patient receiving bone abinoside (ara-C), gemcitabine, interleukin-2, An outpatient with chronic respiratory
marrow–suppressing chemotherapy, usually tumor necrosis factor, and all-transretinoic acid symptoms but without other clinically relevant
for metastatic carcinoma, presents with respi- (ATRA). Other chemotherapy medications that medical conditions who presents with ID-
ratory symptoms in the setting of thrombocy- have been shown to cause ID-GGO include GGO often will have a chronic interstitial lung
topenia and neutropenia. These patients are a daunorubicin, bleomycin, vincristine, carmus- disease. In our study of causes of ID-GGO,
special subset of immunocompromised indi- tine, methotrexate, topotecan, carboplatin, and chronic diffuse interstitial lung diseases ac-
viduals who are at risk for opportunistic in- vinorelbine [41] (Figs. 4 and 5). There likely are counted for 31% (10/32) of pathology-proven
AJR:184, February 2005 615
Miller and Shah
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
Fig. 3.—65-year-old woman with respiratory syncytial virus pneumonia receiving Fig. 4.—75-year-old woman being treated for treated for promyelocytic leukemia and
chemotherapy for ovarian cancer. High-resolution CT image through carina shows presenting with all-transretinoic acid syndrome of noncardiogenic edema. Thick-
extensive ground-glass opacity across both lungs. There also is nonspecific intersti- section CT image through carina shows widespread ground-glass opacities and
tial thickening in more dependent lungs bilaterally; however, ground-glass opacity small bilateral pleural effusions.
remains dominant finding.
cases [9]. Those interstitial diseases that most are a variety of microorganisms that may re- monary edema secondary to an overwhelming
likely will present as ID-GGO include HP, DIP, side in decaying vegetable matter such as ther- allergic response. With lower-dose, chronic ex-
RBILD, and NSIP. Other interstitial diseases mophilic actinomycetes, the Penicillium posures, a granulomatous fibrosis develops in
that rarely may present as ID-GGO include species, the Aspergillus species, and the Myco- the interstitial spaces of the lungs [44].
sarcoidosis and BOOP. bacterium avium-intracellulare complex [43]. There are many of causes of HP, including
Hypersensitivity pneumonitis.—Inhalation A notable exception to this general rule is bird farmer’s lung, cotton worker’s lung (byssino-
of organic or inorganic particles by sensitized fancier’s disease in which the allergens are pro- sis), sugar cane worker’s lung (bagassosis),
individuals may result in the allergic phenom- teins contained in bird feathers, serum, or and mushroom worker’s diseases [43]. Urban
enon known as HP. In most cases, the allergens guano. Acute HP causes a capillary leak pul- populations can be exposed via contaminated
Fig. 5.—37-year-old woman with methotrexate lung toxicity being treated for rheu- Fig. 6.—29-year-old woman with hypersensitivity pneumonitis, slowly progressive
matoid arthritis. High-resolution CT image through carina shows widespread iso- dyspnea, and frequent exposure to birds. High-resolution CT scan of right upper lobe
lated ground-glass opacities with lobular distribution forming mosaic pattern. shows poorly defined centrilobular nodules of ground-glass opacity.
616 AJR:184, February 2005
Ground-Glass Opacity in Thoracic CT
ventilation systems, especially humidifiers of subpleural reticulation may be seen in a mi- Acute interstitial pneumonia.—AIP is a
and air conditioners. Hobbies such as raising nority of patients. rapidly progressive interstitial fibrosis that re-
pigeons or parakeets can result in a form of Respiratory bronchiolitis interstitial lung sembles the organizing stage of DAD. It usually
HP called bird fancier’s disease. disease.—The histology of RBILD reveals ex- will present with progressive dyspnea leading to
CT examinations of HP result in a wide tensive infiltration of alveoli by macrophages as- respiratory failure over several weeks or
spectrum of findings including diffuse alveo- sociated with mild interstitial fibrosis in a months, and occasionally with an antecedent vi-
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
lar consolidation in acute HP, diffuse nodular peribronchiolar distribution [55]. Thus, it is histo- ral-like prodrome [55]. Chest CT may show al-
interstitial lung disease in subacute and logically identical to DIP with the additional cri- veolar consolidation, GGOs, or both, often with
chronic HP, and irregular bands of fibrosis terion that it be most severe in the centrilobular associated traction bronchiectasis [55, 62].
with distortion of the hila in chronic HP [45– regions of the secondary pulmonary lobule. This Lymphocytic interstitial pneumonia.—
49]. However, ID-GGO is among the more similarity has led some authors to suggest that Lymphocytic interstitial pneumonia (LIP) is
common manifestations of subacute HP and, DIP and RBILD are two manifestations of the an idiopathic interstitial abnormality charac-
other than pulmonary edema, HP is probably same disease [55, 56]. On CT, RBILD often will terized by diffuse lymphocytic infiltration of
the most common cause of ID-GGOs in nor- appear as ID-GGO. Very fine, often centrilobular, the interstitium of the lung [63]. It usually is
mal hosts [45, 47, 49] (Fig. 6). These ID- nodules also may be apparent on chest CT [56]. associated with Sjögren’s syndrome in adults
GGOs often will appear as a mosaic pattern. Nonspecific interstitial pneumonia.—NSIP and HIV infection in children. Some reports
Desquamative interstitial pneumonia.— represents an interstitial pneumonia that does have suggested that LIP may represent a pre-
DIP is characterized pathologically by infil- not meet criteria for UIP, DIP, AIP, or BOOP cursor to lymphoma or a low-grade lym-
tration of alveoli by macrophages associated and thus has a variable histologic and radiologic phoma; however, others suggest that LIP
with mild interstitial fibrosis. In the past, appearance [57, 58]. It has been associated with represents a variant of lymphoid hyperplasia
many individuals believed that DIP was an collagen vascular disorders, chronic passive and is not a premalignant condition [64–66].
early phase of usual interstitial pneumonia congestion, and drug toxicity but is most often Diffuse GGO appears to be the most common
(UIP). Currently, DIP is believed to be a direct an idiopathic disorder. When idiopathic, NSIP CT finding in LIP and is present in nearly all
result of smoking-related lung toxicity. Pa- most often affects patients in their 40s, 50s, and patients [66–71]. Bronchovascular and septal
tients with DIP typically are between ages of 60s and presents with an insidious onset of thickening also have been reported [70, 71].
30 to 50 years and present with chronic pro- cough and dyspnea [55]. Thin-walled cysts also may be present in
gressive dyspnea, with or without fevers [50]. ID-GGOs are the most common radio- some cases. Serial CT examinations show re-
Most patients will improve clinically and ra- graphic findings in NSIP and are found in nearly versibility of all findings except cysts [70].
diographically with corticosteroid therapy or 100% of cases. GGO often is found in a sub- Cryptogenic organizing pneumonia and
smoking cessation [6, 51]. pleural distribution but may also show a random bronchiolitis obliterans with organizing
CT scans show ID-GGO in many patients or diffuse distribution [56, 57, 59, 60] (Fig. 8). pneumonia.—BOOP is a histologic pattern of
with DIP. Some studies have found that the Reticulation, either randomly or in a subpleural lung injury. This often is due to a variety of
GGOs predominantly are distributed in the distribution, also is a common finding in one pulmonary insults such as infectious pneumo-
periphery of the lung [52–54]. However, in half to four fifths of cases [56, 57, 60, 61]. Irreg- nia, connective tissue disorders, and bone
many other cases, GGOs also may show a dif- ular linear opacities and traction bronchiectasis marrow transplantation. However, in some
fuse or random distribution (Fig. 7). A pattern also may be seen [56, 59, 60]. cases it may have no recognizable cause. The
Fig. 7.—72-year-old woman with desquamative interstitial pneumonia, slowly pro- Fig. 8.—26-year-old woman with nonspecific interstitial pneumonia, progressive
gressive dyspnea, and 40-pack-year history of smoking. High-resolution CT reveals dyspnea, and positive antinuclear antibodies. High-resolution CT of upper lobes
uniform ground-glass opacity. reveals subpleural areas of ground-glass opacity.
AJR:184, February 2005 617
Miller and Shah
American Thoracic Society/European Respi- ally along the bronchovascular bundles but oc- sandblasters [79]. When found in association
ratory Society International Multidisciplinary casionally as randomly distributed interstitial with silica or other exposures, PAP typically
Consensus Classification Conference has nodules [73–75]. Irregular linear bands of fibro- will present with an acute onset of symptoms.
identified cryptogenic organizing pneumonia sis, traction bronchiectasis, and coarse cystic Leukemia and lymphoma also may predis-
(COP) as the preferred term for idiopathic spaces may develop in stage IV sarcoidosis. pose patients to PAP [80, 81]. PAP was fatal
BOOP [66]. COP is a rare inflammatory con- GGOs are among the least common presenta- in approximately one third of patients before
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
dition presenting with progressive dyspnea tions of sarcoidosis (Fig. 9). When GGOs do oc- the availability of therapy involving high-vol-
and often with fever and constitutional symp- cur in patients with sarcoidosis, careful ume bronchoalveolar lavage; since the intro-
toms that are unresponsive to standard pneu- inspection of the CT image often will reveal a duction of this therapy, many patients can be
monia therapies. It is persistent and can lead fine stippled appearance to the GGO, as if it cured of the disorder and others may be
to serious illness if not treated with corticos- were composed of innumerable, tiny, 1- to 2- treated successfully with repeated episodes of
teroids, a therapy that in most cases will result mm, ill-defined nodules. Sarcoidosis, HP, and bronchoalveolar lavage [82].
in a complete cure of the disease. BOOP, re- RBILD are the causes of GGO most likely to Thin-section CT characteristically will
gardless of cause, most often will appear as give this fine stippled appearance. Rarely, sar- show GGOs in association with thickening of
multifocal alveolar opacities scattered coidosis may appear as multiple large ground- the interlobular septa of the secondary pulmo-
throughout the lungs [72]. Rarely, BOOP may glass masses. This pattern is known as alveolar nary lobules [83–85] (Fig. 10). This combina-
appear as ID-GGO. sarcoid. This appearance is virtually pathogno- tion of findings has been termed the “crazy
Sarcoidosis.—Sarcoidosis is an idiopathic monic of sarcoidosis. paving appearance” and, when present, is
granulomatous disorder with multisystemic quite suggestive of PAP. However, occasion-
ramifications including changes in the Other Diseases Appearing as ID-GGO ally PAP will present as ID-GGO.
meninges, bone, eyes, heart, and skin. Racial PAP.—Other disorders that present as ID- Bronchoalveolar carcinoma.—A form of
predilections include African American and GGO include PAP and BAC. PAP is a rare, id- well-differentiated pulmonary adenocarci-
Puerto Rican residents of the United States iopathic disorder of middle-aged adults. Ac- noma, BAC, has a wide variety of radio-
and West Indians in the United Kingdom. It cumulation of protein and lipid-rich material graphic appearances including solitary
characteristically presents in patients be- within the lung alveoli results in the subacute pulmonary nodules, focal alveolar opacities
tween the ages of 20 and 40 years but may be onset of slowly progressive and often inca- resembling pneumonia, ground-glass nod-
encountered at nearly any age. pacitating dyspnea [76–78]. This accumula- ules, diffuse alveolar consolidation, and ID-
There are a wide variety of CT manifesta- tion appears to be a result of an abnormality of GGOs. Most diffuse BACs will have a domi-
tions of sarcoidosis. Hilar and mediastinal ade- surfactant production, metabolism, or clear- nant mass, nodule, or area of consolidation
nopathy is present in the early and middle stages ance. Occasionally PAP may be associated with associated ID-GGO. Rarely, there will
of the disease. The interstitial lung disease most with exposure to a variety of inorganic dusts, be no such sentinel patch and only ID-GGOs
commonly appears as many small nodules, usu- most commonly silica, such as is seen in will be present [86].
Fig. 9.—46-year-old woman with sarcoidosis who presented with dyspnea and had Fig. 10.—53-year-old man with pulmonary alveolar proteinosis. Slowly progressive
restrictive pulmonary function tests. High-resolution CT image through carina high-resolution CT image through carina shows presence of ground-glass opacities
reveals ground-glass opacities composed of many faint centrilobular nodules widely with slight fine intralobular interstitial thickening. This combination of ground-glass
distributed throughout lungs. opacities and interstitial thickening has been termed “crazy paving.”
618 AJR:184, February 2005
Ground-Glass Opacity in Thoracic CT
Patients with Acute Development of Pulmonary Edema most often is a result of ARDS but has a number
Dyspnea Pulmonary edema is a result of imbalances in of other causes.
In scenario four, the interstitial causes of the Starling forces, which govern the transport Cardiogenic pulmonary edema.—Left-
ID-GGO usually will have a prolonged clini- of fluids between the vascular and interstitial sided heart failure is by far the most common
cal presentation, and chest radiographs most spaces of the lung. During homeostasis, there is cause of hydrostatic edema and thus com-
often will be normal in appearance or show a near balance between these forces, and the monly is known as cardiogenic pulmonary
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
nonspecific interstitial abnormalities. The al- small net transfer of fluid into the interstitium is edema. On thin-section CT, the most common
veolar causes of ID-GGO usually will present removed via the pulmonary lymphatics. How- manifestation of cardiogenic pulmonary
acutely and chest radiographs often will show ever, a disturbance of this equilibrium will lead edema is ID-GGO (Fig. 11). CT also may
diffuse alveolar consolidation. ID-GGO in to excessive transport of water and solutes into show thickening of the interlobular septa. The
this setting most often will be secondary to the interstitial space. If the process continues, GGOs associated with hydrostatic edema of-
one of the acute alveolar causes of ID-GGO: the interstitial lymphatics become overwhelmed ten will have a central, perihilar distribution
cardiogenic pulmonary edema, acute respira- and fluid overflows into the alveoli, leading to and be associated with enlarged pulmonary
tory distress syndrome (ARDS), other causes alveolar edema [87]. vessels and an enlarged heart.
of permeability edema, or DAH. Typically, pulmonary edema is subdivided Adult respiratory distress syndrome.—
into two major etiologic subcategories: hydro- ARDS is the most common cause of noncardio-
Acute Alveolar Diseases Appearing as ID-GGO static pulmonary edema and increased perme- genic pulmonary edema and is a common phys-
In our study of the causes of ID-GGO, acute ability pulmonary edema. In hydrostatic edema, iologic response to a wide variety of insults
alveolar diseases such as DAH, cardiogenic there is increased intravascular hydrostatic pres- including sepsis, aspiration of gastric contents,
edema, and noncardiogenic pulmonary edema sure, which results in a net force driving water overwhelming pneumonia, severe trauma, mul-
accounted for 19% (6/32) of pathology-proven and solutes into the interstitial and, subsequently, tiple fractures, major burns, pancreatitis, pro-
causes of ID-GGO [9]. Because of the need for alveolar spaces of the lung. Hydrostatic edema longed hypotension, disseminated intravascular
pathologic proof, pulmonary edema as a cause most often is a manifestation of left-sided heart coagulation, drug overdose, and thoracic sur-
of ID-GGO is probably underrepresented in this failure. Increased permeability edema usually is gery [88, 89].
series and pulmonary edema likely represents a result of disruption of the capillary epithelial CT scans of ARDS most often will show
the single most common cause of ID-GGO. membrane, which allows plasma proteins to pass bilateral GGO, pulmonary consolidation, or
Thus, an acute clinical presentation of respira- into the interstitial space. These proteins exert an a combination of both [90, 91]. ID-GGO is
tory symptoms in a patient with ID-GGO osmotic force drawing water into the interstitial most often a manifestation of the earlier ex-
should raise the possibility of hydrostatic and space, and if of sufficient volume, they spill into udative phase of disease [90, 91]. Pulmonary
capillary leak pulmonary edema and DAH. the alveolar spaces [87]. Permeability edema opacities often will be most severe in the
Fig. 11.—44-year-old man with cardiogenic edema and with acute onset of dyspnea Fig. 12.—60-year-old man with diffuse alveolar hemorrhage and with acute onset of
and history of mitral stenosis. High-resolution CT image through great vessels shows dyspnea and history of Wegener’s granulomatosis. High-resolution CT image through
geographic ground-glass opacity. right upper lobe bronchus reveals randomly distributed ground-glass opacities.
AJR:184, February 2005 619
Miller and Shah
Clinical Scenarios and Differential Diagnoses of Patients with scenarios: patients who are immunocompro-
TABLE 2 mised, patients who are receiving bone marrow–
Isolated Diffuse Ground-Glass Opacity
suppressing medications, outpatients who have
Scenario Disease Category Differential Diagnoses
slowly progressive dyspnea, inpatients and out-
Immunosuppressed Opportunistic infections PCP, CMV, HSV, RSV, other viruses patients who have acutely developing dyspnea,
(HIV, transplant) and inpatients who are acutely ill. These clinical
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
Bone marrow suppression Opportunistic infections PCP, CMV, HSV, RSV, other viruses scenarios engender limited differential diagnoses
Acute alveolar disease DAH in most cases, as outlined in Table 2.
Miscellaneous Drug toxicity
Slowly progressive dyspnea Chronic interstitial HP, DIP, AIP, NSIP, RBILD, sarcoidosis
disease References
Miscellaneous BOOP, PAP, BAC 1. Leung AN, Miller RR, Muller NL. Parenchymal
opacification in chronic infiltrative lung diseases: CT-
IP/OP acute dyspnea Acute alveolar disease CHF, ARDS, noncardiogenic edema, DAH
pathologic correlation. Radiology 1993;188: 209–214
Debilitated hospital patient Acute alveolar disease CHF, ARDS, volume overload 2. Engeler CE, Tashijian JH, Trenkner SW, Walsh
Note.—PCP = pneumocystis pneumonia, CMV = cytomegalovirus pneumonia, HSV = herpes simplex virus JW. Ground-glass opacity of the lung paren-
pneumonia, RSV = respiratory syncytical virus, DIP = desquamative interstitial pneumonia, RBILD = respiratory chyma: guide to analysis with high resolution CT.
bronchiolitis interstitial pneumonia, HP = hypersensitivity pneumonitis, NSIP = nonspecific interstitial pneumonia, AJR 1993;160:249–251
AIP = acute interstitial pneumonia, BOOP = bronchiolitis obliterans with organizing pneumonia, PAP = pulmonary 3. Muller NL, Staples CA, Miller RR, Vedal S,
alveolar proteinosis, BAC = bronchoalveolar carcinoma, DAH = diffuse alveolar hemorrhage, CHF = cardiogenic Thurlbeck WM, Ostrow DN. Disease activity in
pulmonary edema, ARDS = adult respiratory distress syndrome, IP/OP = inpatient/outpatient. idiopathic pulmonary fibrosis: CT and pathologic
correlation. Radiology 1987;165:731–734
4. Lee JS, Im J, Ahn JM, Kim YM, Han MC. Fibros-
more gravity-dependent regions of the lung. CT scans of DAHs may reveal frank consolida- ing alveolitis: prognostic implication of ground-
glass attenuation at high-resolution CT. Radiology
Unlike chest radiographs, which characteris- tion with obliteration of the pulmonary vascular
1992;184:451–454
tically show uniform consolidation across markings, but often they will appear as ID-GGOs 5. Terriff BA, Kwan SY, Chan-Yeung MM, Muller
the lung parenchyma, 75% of the time CT (Fig. 12). On thin-section CT images, ID-GGO NL. Fibrosing alveolitis: chest radiography and
scan opacification will appear inhomoge- may be spread uniformly throughout the lung, be CT as predictors of clinical and functional impair-
neous or patchy. randomly distributed, appear as centrilobular ment at follow-up in 26 patients. Radiology
opacities, or have a mosaic pattern. 1992;184:445–449
Other noncardiogenic pulmonary edema.—
6. Wells AU, Rubens MB, du Bois RM, Hansell DM.
It is likely that all causes of pulmonary edema Serial CT in fibrosing alveolitis: prognostic sig-
can occasionally result in ID-GGO (Fig. 4). ID- Acutely Ill Hospitalized Patients nificance of the initial pattern. AJR 1993;
GGO has been reported in cases of near drown- In scenario five, it is quite common for gener- 161:1159–1165
ing [92] and fat emboli syndrome [93]. ally debilitated hospitalized patients to undergo 7. Remy-Jardin M, Remy J, Wallaert B, Bataille D,
CT scanning for a wide variety of clinical indica- Hatron PY. Pulmonary involvement in progres-
Diffuse Alveolar Hemorrhage tions unrelated to dyspnea or hypoxia. For exam- sive systemic sclerosis: sequential evaluation with
CT, pulmonary function tests and bronchoalveolar
Alveolar hemorrhage may result from a large ple, chest CT scans often will be obtained on ICU
lavage. Radiology 1993;188:499–506
number of disorders; however, when the process patients to search for causes of a persistent fever. 8. Remy-Jardin M, Giraud F, Remy J, Copin MC,
is diffuse, the differential diagnosis is moder- These patients represent a subset of scenario four: Gosselin B, Duhamel A. Importance of ground-
ately limited. The most common causes of DAH patients with the acute development of dyspnea. glass attenuation in chronic diffuse infiltrative
in outpatients are the group of entities often re- ID-GGO in these patients most often will signify lung disease: pathologic-CT correlation. Radiol-
ferred to as the pulmonary–renal syndromes mild interstitial pulmonary edema due to conges- ogy 1993;189:693–698
9. Shah R, Miller WTJ. Widespread ground-glass
[19]. Goodpasture’s syndrome, Wegener’s gran- tive heart failure, volume overload, or ARDS. It is
opacity in consecutive cases: does lobular distri-
ulomatosis, and systemic lupus erythematosus rare for these patients to have predisposing con- bution assist diagnosis? AJR 2003;180:965–968
are prime examples. Although these disorders ditions for DAH or the more unusual causes of 10. Capitanio MA, Kirkpatrick JAJ. Pneumocystis
may have other pulmonary manifestations, pulmonary edema, and therefore, the differential carinii pneumonia. AJR 1966;97:l74–179
DAH is among the most common radiographi- diagnosis is further limited in this patient popula- 11. Sepkowitz KA. Pneumocystis carinii pneumonia
cally identifiable abnormality. Vasculitises other tion in comparison with those of the more general in patients without AIDS. Clin Infect Dis
1993;7[suppl 2]:S416–S422
than Wegener’s granulomatosis, such as Churg- scenario four.
12. Pneumocystis carinii infection. In: Fraser RG,
Strauss vasculitis and microscopic polyangiitis, Pare JAP, Paré PD, Fraser RS, Genereux GP, eds.
also are less common causes of DAH. Patients Conclusion Diagnosis of diseases of the chest, 3rd ed. Phila-
with lymphoma and leukemia also are inclined Unlike GGOs, in the company of other imag- delphia, PA: Saunders, 1991:1035–1081
to DAH as a result of platelet deficiency or ing findings ID-GGOs are caused by a relatively 13. Ives NJ, Gazzard BG, Easterbrook PJ. The changing
platelet malfunction. DAH is a feared complica- limited group of diseases. These can be grouped pattern of AIDS-defining illnesses with the introduc-
tion of bone marrow transplantation because of into four large categories of disease: diffuse pneu- tion of highly active antiretroviral therapy (HAART)
in a London clinic. J Infect 2001;42: 134–139
its high mortality in this population [94]. Bleed- monias, some chronic interstitial diseases, acute
14. Zahar JR, Robin M, Azoulay E, Fieux F, Nitenberg
ing disorders such as antiphospholipid-antibody alveolar diseases, and a group of unusual miscel- G, Schlemmer B. Pneumocystis carinii pneumonia
syndrome and use of anticoagulatory drugs also laneous disorders. Furthermore, the presentation in critically ill patients with malignancy: a descrip-
may predispose patients to DAH. of ID-GGO often falls into one of five clinical tive study. Clin Infect Dis 2002;35:929–934
620 AJR:184, February 2005
Ground-Glass Opacity in Thoracic CT
15. Ettinger NA, Bailey TC, Trulock EP, et al. Cy- with severe respiratory distress. Scand J Infect Dis vidual CT patterns with functional abnormalities.
tomegalovirus infection and pneumonitis: impact 1992;24:283–292 Radiology 1996;199:123–128
after isolated lung transplantation—Washington 32. Schullere D, Spessert C, Fraser VJ, Goodenberger 48. Lynch DA, Cecile SR, Way D, King TE. Hyper-
University Lung Transplant Group. Am Rev DM. Herpes simplex virus from respiratory tract se- sensitivity pneumonitis: sensitivity of high-reso-
Respir Dis 1993;147:1017–1023 cretions: epidemiology, clinical characteristics and lution CT in a population-based study. AJR 1992;
16. Kramer MR, Marshall SE, Starnes VA, Gamberg outcome in immunocompromised and nonimmuno- 159:469–472
P, Amatai Z, Theodore J. Infectious complications compromised hosts. Am J Med 1993;94:29–33 49. Silver SF, Muller NL, Miller RR, Lefcoe MS. Hy-
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
in heart-lung transplantation: analysis of 200 epi- 33. Douglas RGJ, Anderson MS, Weg JG, et al. Her- persensitivity pneumonitis: evaluation with CT.
sodes. Arch Intern Med 1993;153:2010–2016 pes simplex pneumonia: occurrence in an allo- Radiology 1989;173:441–445
17. Kovacs JA, Hiemenz JW, Macher AM, et al. Pneu- transplanted lung. JAMA 1969;210:902–904 50. Muller NL, Colby TV. Idiopathic interstitial pneu-
mocystis carinii pneumonia: a comparison between 34. Mammana RB, Petersen EA, Fuller JK, Siroky K, monias: high-resolution CT and histologic find-
patients with the acquired immunodeficiency syn- Copeland JG. Pulmonary infections in cardiac ings. RadioGraphics 1997;17:1016–1022
drome and patients with other immunodeficiencies. transplant patients: modes of diagnosis, complica- 51. Hartman TE, Primack SL, Swensen SJ, Hansell
Ann Intern Med 1984;100:663–671 tions, and effectiveness of therapy. Ann Thorac D, McGuinness G, Muller NL. Desquamative in-
18. Kuhlman JE, Kavuru M, Fishman EK, Siegelman Surg 1983;36:700–705 terstitial pneumonia: thin-section CT findings in
SS. Pneumocystis carinii pneumonia: spectrum of 35. Aquino SL, Dunagan DP, Chiles C, Haponik EF. 22 patients. Radiology 1993;187:787–790
parenchymal CT findings. Radiology 1990; Herpes simplex virus 1 pneumonia: patterns on 52. McAdams HP, Rosado-de-Christianson ML, We-
175:711–714 CT scans and conventional chest radiographs. J hunt WD, Fishback NF. The alphabet soup revis-
19. Chow C, Templeton PA, White CS. Lung cysts as- Comput Assist Tomogr 1998;22:795–800 ited: the chronic interstitial pneumonias in the
sociated with Pneumocystis carinii pneumonia: 36. Brown MJ, Miller RR, Muller NL. Acute lung dis- 1990’s. RadioGraphics 1996;16:1009–1033
radiographic characteristics, natural history, and ease in the immunocompromised host: CT and 53. Hartman TE, Primack SL, Kang EY, et al. Disease
complications. AJR 1993:527–531 pathologic examination findings. Radiology progression in usual interstitial pneumonia com-
20. Chaffey MH, Klein JS, Gamsu G, Blanc P, Golden 1994;190:247–254 pared with desquamative interstitial pneumonia: as-
JA. Radiographic distribution of Pneumocystis 37. van Dissel JT, Zijlmans JM, Kroes AC, Fibbe WE. sessment with serial CT. Chest 1996;110:378–382
carinii pneumonia in patients with AIDS treated Respiratory syncytial virus, a rare cause of severe 54. Akira M, Yamamoto S, Hara H, Sakatani M, Ueda
with prophylactic inhaled pentamidine. Radiol- pneumonia following bone marrow transplanta- E. Serial computed tomographic evaluation in
ogy 1990;175:715–719 tion. Ann Hematol 1995;71:253–255 desquamative interstitial pneumonia. Thorax
21. Huang L, Stansell J, Osmond D, et al. Perfor- 38. Parham DM, Bozeman P, Killian C, Murti G, 1997;52:333–337
mance of an algorithm to detect Pneumocystis Brenner M, Hanif I. Cytologic diagnosis of respi- 55. Katzenstein AL, Myers JL. Idiopathic pulmonary
carinii pneumonia in symptomatic HIV-infected ratory syncytial virus infection in a bronchoalve- fibrosis: clinical relevance of pathologic classifi-
persons: pulmonary complications of HIV Infec- olar lavage specimen from a bone marrow cation. Am J Respir Crit Care Med 1998;157:
tion Study Group. Chest 1999;115:1025–1032 transplant recipient. Am J Clin Pathol 1993;99: 1301–1315
22. Boiselle PM, Crans CA Jr, Kaplan MA. The 588–592 56. Kim TS, Lee KS, Chung MP, et al. Nonspecific inter-
changing face of Pneumocystis carinii pneumonia 39. Matar LD, McAdams HP, Palmer SM, et al. Res- stitial pneumonia with fibrosis: high-resolution CT
in AIDS patients. AJR 1999;172:1301–1309 piratory viral infections in lung transplant recipi- and pathologic findings. AJR 1998;171:1654–1660
23. Wilczek B, Wilczek HE, Heurlin N, Tyden G, As- ents: radiologic findings with clinical correlation. 57. Hartman TE, Swensen SJ, Hansell DM, et al.
pelin P. Prognostic significance of pathological Radiology 1999;213:735–742 Nonspecific interstitial pneumonia: variable ap-
chest radiography in transplant patients affected 40. Ko JP, Shepard JA, Sproule MW, et al. CT mani- pearance at high-resolution CT. Radiology
by cytomegalovirus and/or Pneumocystis carinii. festations of respiratory syncytial virus infection 2000;217:701–705
Acta Radiol 1996;37:727–731 in lung transplant recipients. J Comput Assist To- 58. Katzenstein AL, Fiorelli RF. Nonspecific intersti-
24. Furrer H, Fux C. Opportunistic infections: an up- mogr 2000;24:234–241 tial pneumonia/fibrosis: histologic features and
date. J HIV Ther 2002;7:2–7 41. Rossi SE, Erasmus JJ, McAdams HP, Sporn TA, clinical significance. Am J Surg Pathol 1994;
25. d’Arminio Monforte A, Mainini F, Testa L, et al. Goodman PC. Pulmonary drug toxicity: radio- 18:136–137
Predictors of cytomegalovirus disease: natural logic and pathologic manifestations. Radio- 59. Nishiyama O, Kondoh Y, Taniguchi H, et al. Se-
history and autopsy findings in a cohort of pa- Graphics 2000;20:1245–1259 rial high resolution CT findings in nonspecific in-
tients with AIDS. AIDS 1997;11:517–524 42. Patz EFJ, Peters WP, Goodman PC. Pulmonary terstitial pneumonia/fibrosis. J Comput Assist
26. Waxman AB, Goldie SJ, Brett-Smith H, Matthay drug toxicity following high-dose chemotherapy Tomogr 2000;24:41–46
RA. Cytomegalovirus as a primary pulmonary with autologous bone marrow transplantation: CT 60. Kim EY, Lee KS, Chung MP, Kwon OJ, Kim TS,
pathogen in AIDS. Chest 1997;111:128–134 findings in 20 cases. J Thorac Imaging 1994;9: Hwang JH. Nonspecific interstitial pneumonia with
27. Moon JH, Kim EA, Lee KS, Kim TS, Jung KJ, 129–134 fibrosis: serial high-resolution CT findings with
Song JH. Cytomegalovirus pneumonia: high-res- 43. Inhalation of organic dust. In: Fraser RS, Muller functional correlation. AJR 1999;173:949–953
olution CT findings in ten non-AIDS immuno- N, Colman N, Paré PD, eds. Fraser and Paré’s di- 61. Katoh T, Andoh T, Mikawa K, Tanigawa M, Su-
compromised patients. Korean J Radiol 2000; agnosis of diseases of the chest, 4th ed. Philadel- zuki R, Takagi K. Computed tomographic find-
1:73–78 phia, PA: Saunders, 1999:2361–2385 ings in non-specific interstitial pneumonia/
28. Shanley JD, Jordan MC. Viral pneumonia in the 44. Salvaggio JE, deShazo RD. Pathogenesis of hy- fibrosis. Respirology 1998;3:69–75
immunocompromised patient. Semin Respir In- persensitivity pneumonitis. Chest 1986;89 62. Johoh T, Muller NL, Taniguchi H, et al. Acute in-
fect 1986;1:l93–201 [suppl]:1905–1955 terstitial pneumonia: thin-section CT findings in
29. Whimbey E, Bodey GP. Viral pneumonia in the 45. Remy-Jardin M, Remy J, Wallaert B, Muller NL. 36 patients. Radiology 1999;211:859–863
immunocompromised adult with neoplastic dis- Subacute and chronic bird breeder hypersensitiv- 63. Koss MN, Hochlolzer L, Langloss JM, Wehunt
ease: the role of common community respiratory ity pneumonitis: sequential evaluation with CT WD, Lazarus AA. Lymphoid interstitial pneumo-
viruses. Semin Respir Infect 1992;7:122–131 and correlation with lung function tests and bron- nia: clinicopathological and immunopathological
30. Nash G, Foley FD. Herpetic infection of the mid- choalveolar lavage. Radiology 1993;189:111–118 findings in 18 cases. Pathology 1987;19:178–185
dle and lower respiratory tract. Am J Clin Pathol 46. Buschman DL, Gamsu B, Waldron JA, Klein JS, 64. Nicholson AG, Wotherspoon AC, Diss TC, et al.
1970;54:857–863 King TE. Chronic hypersensitivity pneumonitis: Reactive pulmonary lymphoid disorders. Histo-
31. Prellner T, Flamholc L, Haidl S, Lindholm K, use of CT in diagnosis. AJR 1992;159:957–960 pathology 1995;26:405–412
Widell A. Herpes simplex virus: the most fre- 47. Hansell DM, Wells AU, Padley SP, Muller NL. 65. Kurosu K, Yumoto N, Furukawa M, Kuriyama T,
quently isolated pathogen in the lungs of patients Hypersensitivity pneumonitis: correlation of indi- Mikata A. Third complementarity-determining-re-
AJR:184, February 2005 621
Miller and Shah
gion sequence analysis of lymphocytic interstitial Pulmonary sarcoidosis: correlation of CT and histo- relations. Chest 1997;111:989–895
pneumonia: most cases show a minor monoclonal pathologic findings. Radiology 1993;189:105–109 85. Murch CR, Carr DH. Computed tomography ap-
population hidden among normal lymphocyte clones. 75. Brauner MW, Grenier P, Mompoint D, Lenoir S, de pearances of pulmonary alveolar proteinosis. Clin
Am J Respir Crit Care Med 1997;155:1453–1460 Cremoux H. Pulmonary sarcoidosis: evaluation with Radiol 1989;40:240–243
66. American Thoracic Society; European Respira- high resolution CT. Radiology 1989;172:467–471 86. Trigaux JP, Gevenois PA, Goncette L, Gouat F,
tory Society. The American Thoracic Society/Eu- 76. Rosen SH, Castleman B, Liebow AA. Pulmonary Schumaker A, Weynants P. Bronchioloalveolar car-
ropean Respiratory Society International alveolar proteinosis. N Engl J Med 1958;58: cinoma: computed tomography findings. Eur Respir
Downloaded from www.ajronline.org by 159.146.13.83 on 12/05/20 from IP address 159.146.13.83. Copyright ARRS. For personal use only; all rights reserved
Multidisciplinary Consensus Classification of the 1123–1142 J 1996;9:11–16
Idiopathic Interstitial Pneumonias. Am J Respir 77. Wang BM, Stern EJ, Schmidt RA, Pierson DJ. Diag- 87. Pulmonary edema. In: Fraser RS, Muller N, Colman
Crit Care Med 2002;165:227–304 nosing pulmonary alveolar proteinosis: a review and N, Paré PD, eds. Fraser and Paré’s diagnosis of dis-
67. Ichikawa Y, Kinoshita M, Koga T, Oizumi K, update. Chest 1997;111:460–466 eases of the chest, 4th ed. Philadelphia, PA: Saun-
Fujimoto K, Hayabuchi N. Lung cyst formation in 78. Bedrossian CWM, Luna MA, Conklin RH, Miller ders, 1999:1946–2017
lymphocytic interstitial pneumonia: CT features. WC. Alveolar proteinosis as a consequence of im- 88. Connelly KG, Repine JE. Markers for predicting the
J Comput Assist Tomogr 1994;18:745–748 munosuppression: a hypothesis based on clinical development of acute respiratory distress syndrome.
68. Oldham SA, Castillo M, Jacobson F, Mones JM, and pathologic observation. Hum Pathol 1980; Annu Rev Med 1997;48:429–445
Saldana MJ. HIV-associated lymphocytic interstitial 11:527–535 89. Fowler AA, Hamman RF, Good JT, et al. Adult res-
pneumonia: radiologic manifestations and patho- 79. Buechner HA, Ansari A. Acute silico-proteinosis: a piratory distress syndrome: risk with common pre-
logic correlation. Radiology 1989;170:83–87 new pathologic variant of alveolar proteinosis. Dis disposition. Ann Intern Med 1983;98:593–597
69. McGuinness G, Scholes JV, Jagiradar JS, et al. Un- Chest 1968–1969;55:274 90. Swensen SJ, Tashjian JH, Myers JL, et al. Pulmo-
usual lymphoproliferative disorders in nine adults 80. Green D, Dighe P, Ali NO, Katele GV. Pulmonary nary venoocclusive disease: CT findings in eight pa-
with HIV or AIDS: CT and pathologic findings. Ra- alveolar proteinosis complicating chronic myeloge- tients. AJR 1996;167:937–940
diology 1995;197:59–65 nous leukemia. Cancer 1980;46:1763–1766 91. Tagliabue M, Casella TC, Zincone GE, Fumagalli R,
70. Johkoh T, Ichikado K, Akira M, et al. Lymphocytic 81. Carnovale R, Zornoza J, Goldman AM, Luna M. Salvini E. CT and chest radiography in the evalua-
interstitial pneumonia: follow-up CT findings in 14 Pulmonary alveolar proteinosis: its association with tion of adult respiratory distress syndrome. Acta Ra-
patients. J Thorac Imaging 2000;15:162–167 hematologic malignancy and lymphoma. Radiology diol 1994;35:230–234
71. Johkoh T, Muller NL, Pickford HA, et al. Lympho- 1977;122:303–306 92. Kim KI, Lee KN, Tomiyama N, et al. Near drown-
cytic interstitial pneumonia: thin-section CT find- 82. Metabolic pulmonary disease. In: Fraser RS, Muller ing: thin-section CT findings in six patients. J Com-
ings in 22 patients. Radiology 1999;212:567–572 N, Colman N, Paré PD, eds. Fraser and Paré’s diag- put Assist Tomogr 2000;24:562–566
72. Alasaly K, Muller N, Ostrow DN, Champion P, nosis of diseases of the chest, 4th ed. Philadelphia, 93. Arakawa H, Kurihara Y, Nakajima Y, Yamaki K.
FitzGerald JM. Cryptogenic organizing pneumonia: PA: Saunders, 1999:2699–2735 Pulmonary fat embolism syndrome: CT findings
a report of 25 cases and a review of the literature. (re- 83. Godwin JD, Muller NL, Takasugi JE. Pulmonary al- in six patients. J Comput Assist Tomogr 2000;
view) Medicine (Baltimore) 1995;74:201–211 veolar proteinosis: CT findings. Radiology 1988; 24:24–29
73. Muller NL, Kullnig P, Miller RR. The CT findings of 169:609–613 94. Witte RJ, Gurney JW, Robbins RA, et al. Diffuse
pulmonary sarcoidosis: analysis of 25 patients. AJR 84. Lee KN, Levin DL, Webb WR, Chen D, Storto ML, pulmonary alveolar hemorrhage after bone marrow
1989;152:1179–1182 Golden JA. Pulmonary alveolar proteinosis: high- transplantation: radiographic findings in 39 patients.
74. Nishimura K, Itoh H, Kitaichi M, Nagai S, Izumi T. resolution CT, chest radiographic and functional cor- AJR 1991;157:461–464
622 AJR:184, February 2005
You might also like
- Evaluation of The Painful Total Knee Arthroplasty.99377Document9 pagesEvaluation of The Painful Total Knee Arthroplasty.99377Filip starcevic100% (1)
- MycologyDocument129 pagesMycologyPriyanka Rajput100% (4)
- Nursing Care Plan For "AIDS"Document31 pagesNursing Care Plan For "AIDS"jhonroks88% (8)
- Infectious Diseases MCQDocument34 pagesInfectious Diseases MCQfrabziNo ratings yet
- Miller Shah 2012 Isolated Diffuse Ground Glass Opacity in Thoracic CT Causes and Clinical PresentationsDocument10 pagesMiller Shah 2012 Isolated Diffuse Ground Glass Opacity in Thoracic CT Causes and Clinical PresentationsAndrea PescosolidoNo ratings yet
- Cardiac Troponin and Defining Myocardial Infarction: Thomas E. Kaier, Bashir Alaour, and Michael MarberDocument13 pagesCardiac Troponin and Defining Myocardial Infarction: Thomas E. Kaier, Bashir Alaour, and Michael MarberwiwiNo ratings yet
- Oral-Maxillary Sinus Fistula (Oroantral Fistula) :: Clinical Features and Findings On Multiplanar CTDocument4 pagesOral-Maxillary Sinus Fistula (Oroantral Fistula) :: Clinical Features and Findings On Multiplanar CTnataliayobeantoNo ratings yet
- Ajr 161 6 8249719Document7 pagesAjr 161 6 8249719hotmart ventasNo ratings yet
- Chest Radiography in The ICUDocument9 pagesChest Radiography in The ICUNicolás HonoresNo ratings yet
- AJR Chest Radiography in The ICU Parte I 2012Document9 pagesAJR Chest Radiography in The ICU Parte I 2012wfranelicNo ratings yet
- Gastric Tubes and Airway Management in Patients At.15 PDFDocument11 pagesGastric Tubes and Airway Management in Patients At.15 PDFEladio PerezNo ratings yet
- Pictorial Essay: Multidetector CT Urography With Abdominal Compression and Three-Dimensional ReconstructionDocument13 pagesPictorial Essay: Multidetector CT Urography With Abdominal Compression and Three-Dimensional ReconstructionHarley Alejo MNo ratings yet
- Esophagus Normal CT Anatomy 2012Document6 pagesEsophagus Normal CT Anatomy 2012Dr Ankit SharmaNo ratings yet
- Differentiation Between Calcification and Hemorrhage in Brain Tumors Using Susceptibility-Weighted Imaging: A Pilot StudyDocument4 pagesDifferentiation Between Calcification and Hemorrhage in Brain Tumors Using Susceptibility-Weighted Imaging: A Pilot StudyDanaAmaranducaiNo ratings yet
- Cone Beam Computed Tomography Evaluation of The.9Document5 pagesCone Beam Computed Tomography Evaluation of The.9francisco EscorciaNo ratings yet
- Jurnal B 1Document10 pagesJurnal B 1Nasayu Nadia Santika AyuNo ratings yet
- Lumbar Stenosis: Ehud Arbit, MD and Susan Pannullo, MDDocument7 pagesLumbar Stenosis: Ehud Arbit, MD and Susan Pannullo, MDBudhiNo ratings yet
- Acute Subdural Hematoma Because of Boxing.2Document6 pagesAcute Subdural Hematoma Because of Boxing.2Mon ChávezNo ratings yet
- Diagnostic Evaluation of Stroke Etiology.4Document13 pagesDiagnostic Evaluation of Stroke Etiology.4Luis David Beltran OntiverosNo ratings yet
- Subchondroplasty What TheDocument6 pagesSubchondroplasty What TheikhsanNo ratings yet
- AJR Chest Radiography in The ICU Parte II 2012Document10 pagesAJR Chest Radiography in The ICU Parte II 2012wfranelicNo ratings yet
- Assessmen T Diagnosi S Planning Intervention S Rational E Evaluatio NDocument3 pagesAssessmen T Diagnosi S Planning Intervention S Rational E Evaluatio Nmarie judimor gomezNo ratings yet
- Imaging of Cholecystitis: ResidentsDocument8 pagesImaging of Cholecystitis: ResidentsandrefaelNo ratings yet
- Abdominal Aortic AneurysmDocument7 pagesAbdominal Aortic AneurysmShaastieNo ratings yet
- Fibrous Dysplasia Vs Adamantinoma of The TibiaDocument7 pagesFibrous Dysplasia Vs Adamantinoma of The TibiataufikolingNo ratings yet
- Swensen Et Al 2013 High Resolution CT of The Lungs Findings in Various Pulmonary DiseasesDocument9 pagesSwensen Et Al 2013 High Resolution CT of The Lungs Findings in Various Pulmonary Diseasesjeetchoudhary7890No ratings yet
- Pictorial Essay: Abnormal Appendiceal PositionDocument5 pagesPictorial Essay: Abnormal Appendiceal PositionsavinaumarNo ratings yet
- Evidenciasenla Rehabilitacindel Hombro Doloroso 2018Document109 pagesEvidenciasenla Rehabilitacindel Hombro Doloroso 2018Alan Calderón BerrioNo ratings yet
- Handouts 1Document12 pagesHandouts 1banana_rockNo ratings yet
- Highly Commended 2020 - 1Document1 pageHighly Commended 2020 - 1Moeed AliNo ratings yet
- Solid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaDocument11 pagesSolid Renal Masses: What The Numbers Tell Us: Stella K. Kang William C. Huang Pari V. Pandharipande Hersh ChandaranaTạ Minh ZSNo ratings yet
- Assessment Diagnosis Inference Planning Interventio N Rationale EvaluationDocument9 pagesAssessment Diagnosis Inference Planning Interventio N Rationale Evaluationjosh100% (1)
- What The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyDocument8 pagesWhat The Radiologist Needs To Know About Urolithiasis: Part 1 - Pathogenesis, Types, Assessment, and Variant AnatomyQonita Aizati QomaruddinNo ratings yet
- Osteosarkoma PereostealDocument7 pagesOsteosarkoma Pereostealindah21No ratings yet
- Pulmonary Findings in HIV On CTDocument8 pagesPulmonary Findings in HIV On CTNicky ChhajwaniNo ratings yet
- Diagnostic Evaluation of Stroke Etiology: Review ArticleDocument13 pagesDiagnostic Evaluation of Stroke Etiology: Review Articleveerraju tvNo ratings yet
- Handler 1979Document3 pagesHandler 1979KarimNo ratings yet
- Kundra Silverman 2012 Imaging in The Diagnosis Staging and Follow Up of Cancer of The Urinary BladderDocument15 pagesKundra Silverman 2012 Imaging in The Diagnosis Staging and Follow Up of Cancer of The Urinary BladderJelena JovanovicNo ratings yet
- Ipsilateral Displaced Physeal Fractures of The.73Document5 pagesIpsilateral Displaced Physeal Fractures of The.73Camilo Andrés Orduña CepedaNo ratings yet
- Situs Inversus JClinSci - 2018 - 15 - 3 - 168 - 244747Document4 pagesSitus Inversus JClinSci - 2018 - 15 - 3 - 168 - 244747Anonymous 9QxPDpNo ratings yet
- Adult GliomasDocument24 pagesAdult GliomasSofía UrbinaNo ratings yet
- Ajr 15 14445Document8 pagesAjr 15 14445Yuriansyah Dwi Rahma PutraNo ratings yet
- Pathophysiology of Acute Intracerebral and Subarachnoid Hemorrhage: Applications To MR ImagingDocument5 pagesPathophysiology of Acute Intracerebral and Subarachnoid Hemorrhage: Applications To MR ImagingAditya KurniantoNo ratings yet
- Acute Aortic Syndrome RevisitedDocument20 pagesAcute Aortic Syndrome RevisitedVictor ChiabaiNo ratings yet
- Progressive Mobility Therapy in The ICU: Self Directed Study Akiko Kubo, RN, BSN University of Kansas Hospital (KUH)Document20 pagesProgressive Mobility Therapy in The ICU: Self Directed Study Akiko Kubo, RN, BSN University of Kansas Hospital (KUH)DepphaPiieDepphullNo ratings yet
- Hemodynamics 3443434Document12 pagesHemodynamics 3443434lolopoponakerNo ratings yet
- Electrocardiograma Neyssa KimeeDocument15 pagesElectrocardiograma Neyssa KimeeNEYSSA KIMEE SAINT VILNo ratings yet
- Thoracic CT Findings in Birt-Hogg-Dubé SyndromeDocument4 pagesThoracic CT Findings in Birt-Hogg-Dubé SyndromeicaeeNo ratings yet
- The Adoption of Ultrasound Guided Radiofrequency.31Document3 pagesThe Adoption of Ultrasound Guided Radiofrequency.31drhusseinfaour3126No ratings yet
- Ultrasound Imaging of Congestion in Heart Failure Examinations BeyondDocument10 pagesUltrasound Imaging of Congestion in Heart Failure Examinations BeyondAncylostoma DuodenaleNo ratings yet
- Rotator CuffDocument11 pagesRotator CuffineedsheetzNo ratings yet
- Bcs Article RoleDocument15 pagesBcs Article RoleSowmya ANo ratings yet
- AJR Teaching File: Intraventricular Mass: Clinical HistoryDocument4 pagesAJR Teaching File: Intraventricular Mass: Clinical HistoryDokdem AjaNo ratings yet
- Imaging Pulmonary Infection: Classic Signs and PatternsDocument18 pagesImaging Pulmonary Infection: Classic Signs and Patternssofiana debbyNo ratings yet
- Hepatorenal Syndrome: Pathophysiology, Diagnosis, and ManagementDocument21 pagesHepatorenal Syndrome: Pathophysiology, Diagnosis, and Managementkonas patklinNo ratings yet
- CT Features of Rounded Atelectasis: Findings Were Analyzed and ComparedDocument4 pagesCT Features of Rounded Atelectasis: Findings Were Analyzed and ComparedSandara ParkNo ratings yet
- Jurnal CT ScanDocument12 pagesJurnal CT ScanJefri Rudolf WomsiworNo ratings yet
- Ajr 10 7226Document9 pagesAjr 10 7226cuenta de gmailNo ratings yet
- Preparing A Patient For Cardiac Catheterization.4Document1 pagePreparing A Patient For Cardiac Catheterization.4Quality PmnhNo ratings yet
- European J of Heart Fail - 2017 - Swol - Tracheostomy As A Bridge To Spontaneous Breathing and Awake ECMO in Non TransplantDocument4 pagesEuropean J of Heart Fail - 2017 - Swol - Tracheostomy As A Bridge To Spontaneous Breathing and Awake ECMO in Non Transplantjorge escobar pintoNo ratings yet
- Classification of Subtypes of Ischemic StrokeDocument9 pagesClassification of Subtypes of Ischemic StrokeEddwwin Varillas ReyesNo ratings yet
- Diagnostic - Evaluation - of - Stroke - Etiology.4 2Document13 pagesDiagnostic - Evaluation - of - Stroke - Etiology.4 2YammelyVargasNo ratings yet
- Coronary Vasomotion AbnormalitiesFrom EverandCoronary Vasomotion AbnormalitiesHiroaki ShimokawaNo ratings yet
- MR Imaging of The Spinal Bone MarrowDocument24 pagesMR Imaging of The Spinal Bone MarrowAyşe BanuNo ratings yet
- MRI of Spinal Bone Marro Part 1 Techniques and Normal Age-Related AppearancesDocument11 pagesMRI of Spinal Bone Marro Part 1 Techniques and Normal Age-Related AppearancesAyşe BanuNo ratings yet
- MRI of Spinal Bone Marrow Part 2 T1-Weighted Imaging-Based Differential DiagnosisDocument13 pagesMRI of Spinal Bone Marrow Part 2 T1-Weighted Imaging-Based Differential DiagnosisAyşe BanuNo ratings yet
- Sclerotic Lesions of The Spine MRI AssessmentDocument15 pagesSclerotic Lesions of The Spine MRI AssessmentAyşe BanuNo ratings yet
- Sulfamethoxazole Trimethoprim PDFDocument10 pagesSulfamethoxazole Trimethoprim PDFAsi SyyffaNo ratings yet
- 2.opportunistic Infections in HIV-infected PatientsDocument53 pages2.opportunistic Infections in HIV-infected PatientsAbebe TilahunNo ratings yet
- Chapter 61 Atypical and Parafungal AgentsDocument18 pagesChapter 61 Atypical and Parafungal AgentsbartsnewNo ratings yet
- Acfrogclhto 41rcs7k2x9e9ozhxq6xpyvgxibnamac Wqxg3qiugn 4ovgkuedgemtgeegex2qkvdx2s2tntnpedoovxbx7hfd Okc69rl78zkapufum4ws5t7y1wsieja3x1yqkshoglfvwtjgDocument3 pagesAcfrogclhto 41rcs7k2x9e9ozhxq6xpyvgxibnamac Wqxg3qiugn 4ovgkuedgemtgeegex2qkvdx2s2tntnpedoovxbx7hfd Okc69rl78zkapufum4ws5t7y1wsieja3x1yqkshoglfvwtjgBoy MadNo ratings yet
- Acquired Immune Deficiency SyndromeDocument7 pagesAcquired Immune Deficiency SyndromePankaj YadavanNo ratings yet
- Treatment of Giant Cell Arteritis - UpToDateDocument26 pagesTreatment of Giant Cell Arteritis - UpToDateBeatriz SilvaNo ratings yet
- Pneumonia in Immunocompromised Patients: Respirology (2009) 14 (Suppl. 2) S44 - S50Document7 pagesPneumonia in Immunocompromised Patients: Respirology (2009) 14 (Suppl. 2) S44 - S50intankmlsNo ratings yet
- Paediatric Protocols Kenya PDFDocument35 pagesPaediatric Protocols Kenya PDFMusab Ahmed HirshiNo ratings yet
- Dr. Reviono, DR., SP.P (K) - Update Diagnosis and Management JeroveciDocument20 pagesDr. Reviono, DR., SP.P (K) - Update Diagnosis and Management JeroveciOlivia DwimaswastiNo ratings yet
- A Look Inside Oral Sampling For Detection of Non-OralDocument14 pagesA Look Inside Oral Sampling For Detection of Non-OralrehanaNo ratings yet
- Algoritmo Diagnostico en SdraDocument8 pagesAlgoritmo Diagnostico en SdraPierina VeramatosNo ratings yet
- Seminar, CBD, MGT & Bedside GroupDocument3 pagesSeminar, CBD, MGT & Bedside GroupSarvess MuniandyNo ratings yet
- The Immune Reconstitution Inflammatory SyndromeDocument7 pagesThe Immune Reconstitution Inflammatory SyndromeAlexandra PaunNo ratings yet
- Actue Management of Pneumonia in Adults PatienitDocument8 pagesActue Management of Pneumonia in Adults Patienitxiomara torresNo ratings yet
- Human Immunodeficiency Virus (HIV) Infection and Acquired Immunodeficiency Syndrome (AIDS)Document28 pagesHuman Immunodeficiency Virus (HIV) Infection and Acquired Immunodeficiency Syndrome (AIDS)The Living SonneteerNo ratings yet
- P2 MICRO RATIOaDocument18 pagesP2 MICRO RATIOaJemuel DalanaNo ratings yet
- Ilovepdf Merged 1Document193 pagesIlovepdf Merged 1Angelica RatonNo ratings yet
- 10/2/02 investigation request my wife Karen and I wrote (using the pseudonym "Dr. Bob Smith") and filed with UCLA that triggered the "malariotherapy" investigation of John Fahey MD and other university staffDocument11 pages10/2/02 investigation request my wife Karen and I wrote (using the pseudonym "Dr. Bob Smith") and filed with UCLA that triggered the "malariotherapy" investigation of John Fahey MD and other university staffPeter M. HeimlichNo ratings yet
- Pneumocystis PneumoniaDocument16 pagesPneumocystis PneumoniaMaría Luisa MantillaNo ratings yet
- John Hopkins Specimen Collection Guidelines Updated 06-2019Document28 pagesJohn Hopkins Specimen Collection Guidelines Updated 06-2019Vincent ReyesNo ratings yet
- Patient Education HIV AIDS The Basics 1-30-18Document3 pagesPatient Education HIV AIDS The Basics 1-30-18Henry Leroy Lewis BatresNo ratings yet
- Fungal Lung DiseasesDocument28 pagesFungal Lung Diseasessultan khabeebNo ratings yet
- Pneumocystis Pneumonia: Predisposing Factors Precipitating FactorsDocument2 pagesPneumocystis Pneumonia: Predisposing Factors Precipitating FactorsAlyssa CastroNo ratings yet
- Case Study PPT - PDF HIV With Opportunistic Infection - Madayag March 2023Document71 pagesCase Study PPT - PDF HIV With Opportunistic Infection - Madayag March 2023Rasheda PickettNo ratings yet
- Opportunistic Mycoses: Yeasts: Candida SPP., Cryptococcus Spp. Mycelial or Filamentous FungiDocument10 pagesOpportunistic Mycoses: Yeasts: Candida SPP., Cryptococcus Spp. Mycelial or Filamentous FungiSSJ GAMERNo ratings yet
- Approach To The Immunocompromised Patient With Fever and Pulmonary Infiltrates - UpToDateDocument40 pagesApproach To The Immunocompromised Patient With Fever and Pulmonary Infiltrates - UpToDateJúlio ZoéNo ratings yet