Professional Documents
Culture Documents
L2 Hemiplegia and Cerebrovascular Insufficiency (Word)
Uploaded by
Ashraf Nabil0 ratings0% found this document useful (0 votes)
9 views7 pagesOriginal Title
L2 Hemiplegia and cerebrovascular insufficiency (word)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views7 pagesL2 Hemiplegia and Cerebrovascular Insufficiency (Word)
Uploaded by
Ashraf NabilCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
4th Year 2nd Semester 2nd Module Medicine III
L2: Cerebrovascular insufficiency & Hemiplegia
Cerebrovascular insufficiency
State that results in obstruction in one or more arteries that supply the brain,
May be localized(stroke) or generalized (coma)
May be transient (TIA)or permanent (infarction)
Stroke
A generalized reduction in cerebral blood flow due to systemic hypotension usually
produces syncope
Global hypoxia-ischemia: widespread brain injury due to infarction in the border zones
between the major cerebral artery distributions if low cerebral blood flow persists for a
longer duration
Hypoxic-ischemic encephalopathy: the constellation of cognitive sequelae that ensues
Focal ischemia: usually caused by thrombosis of the cerebral vessels or by an emboli from a
proximal arterial source or the heart
Intracranial hemorrhaqe: bleeding directly into or around the brain; produces symptoms
by:
a) mass effect of neural structures
b) toxic effect of blood itself
c) increasing intracranial pressure
Stroke Mimics (usually global rather than focal neurological symptoms)
• drug intoxication/withdrawal
• infections—herpes simplex encephalitis
• metabolic—hypoglycemia, renal failure, hepatic failure, hypoxia/hypercarbia, endocrine
disorders (thyrotoxicosis, myxedema, adrenal insufficiency)
• migraines • syncope
• seizures—Todd paralysis
• structural—trauma, tumors, subdural hemorrhage
Transient Ischemic Attack
An ischemic episode causing transient focal neurologic symptoms without evidence of
infarct (on MRI) nor persistent symptoms following event.
Symptoms: onset within 24 hours unilateral weakness or sensory symptoms, speech
disturbance, vision, ataxia, dysphagia, dysarthria, binocular diplopia
Management
• Immediate assessment urgent CT/CTA or MRI/MRA,
• ECG, and laboratory investigations
• Control Bl P
1 Neurology BFOM 38 Team
4th Year 2nd Semester 2nd Module Medicine III
Hemiplegia
Is total paralysis of the arm, leg, and trunk on the same side of the body. Severe or complete
loss of motor function on one side of the body.
Hemiplegia is more severe than hemiparesis, where in one half of the body has less marked
weakness.
Causes:
• Cerebrovascular Accident (CVA) • Todd's Paralysis
• Thrombosis, Embolism or • Brain Tumor
hemorrhage Transient Ischemic • Infection (encephalitis, meningitis,
Attack (TIA) brain abscess)
• Migraine syndrome • Subdural empyema
• Head Trauma • Meningitis
• Brain Contusion • Nonketotic hyperosmolar coma
• Subdural Hematoma & Epidural • Vasculitis
Hematoma • Acute necrotizing myelitis
Thrombosis:
o Most common o Slowest Hours
o Wakes up in the morning with weakness
o History of TIA o Old age
Embolism:
o Fastest onset - Seconds o History of heart disease
o No progression {Max. deficit at o Younger age group
onset} o Major deficit ( heart to vessel )
Hemorrhage:
o H/o Prolonged hypertension o Vomiting
o Awake — stress o Altered consciousness
o Head ache o Convulsion
Pathogenesis:
• The exact cause of hemiplegia is not known in all cases.
• Brain is deprived of oxygen and this results in the death of neurons.
• When the corticospinal tract is damaged, the injury is usually manifested on the opposite
side of the body. This happens because the motor fibres of corticospinal tract, which take
origin from the motor cortex in brain, cross to the opposite side in the lower part of medulla
oblongata and then descend down in spinal cord to supply their respective muscles.
2 Neurology BFOM 38 Team
4th Year 2nd Semester 2nd Module Medicine III
Localization: Depending on the site of lesion in brain, the severity of hemiplegia varies.
Internal capsule Brainstem: Midbrain, Pons, Medulla
Cortex Spinal cord
Subcortex - Corona radiata
Internal capsule
• Dense & uniform hemiplegia (UMN Facial )
• Hemisensory blunting
• Homonymous Hemianopia
Cortex
• Non dense nonuniform weakness • Apraxia
• Monoplegias • Cortical sensory loss
• Cortical signs • Convulsions
• Dysphasia
Subcortex
• Pattern of weakness similar to cortical
• Non dense non-uniform weakness
• No cortical signs
Brainstem
• Crossed hemiplegia
• Ipsilateral LMN CN palsy & contralateral hemiplegia
• Cerebellar signs
Spinal cord
• Rare
• No facial
• Brown sequard syndrome [hemiplegia on the side of involvement without face] lesion
above C5
• Effects below the level — UMN type motor loss and sensory loss
• At the level — LMN type
• Above the level — Hyperaesthesia
Midbrain
• Crossed cerebellar ataxia with ipsilateral third nerve palsy (Claude's syndrome):
• Weber's syndrome: third nerve palsy and contralateral hemiplegia:
• Bendict syndrome: Contralateral rhythmic, ataxic action tremor; rhythmic postural or
intention tremor with ipsilateral third nerve palsy
3 Neurology BFOM 38 Team
4th Year 2nd Semester 2nd Module Medicine III
Pons
• LMN Facial + contralateral hemiplegia
• +VI th Nerve + cotralateral hemiplegia
• + Lateral Gaze palsy + cotralateral hemiplegia
Medulla lateral Medullary syndrome
• Same side
• Homer's syndrome
• Loss of pain & touch on the face
• Cerebellar signs
• Palate weakness
• Opposite side
• Loss of pain and temperature sensation on the body and limbs
C/P: Onset and course:
• Acute onset and regressive course (vascular, infective, traumatic lesions).
• Gradual onset & progressive course (neoplastic lesions).
• Intermittent & relapsing course (multiple sclerosis)
Diagnosis: Hemiplegia is identified by clinical manifestations &examination
Signs & Symptoms: Vary from person to person.
• Difficulty with gait, Difficulty with balance while standing or arm and leg walking
• Having difficulty with motor activities, like holding, grasping or pinching
• Increasing stiffness of muscles
• Muscle spasms
• Difficulty with speech
• Difficulty swallowing food
• Significant delay during standing, smiling, crawling or speaking
• Behavior problems like anxiety, anger, irritability, lack of concentration or
• Emotions - depression
Clinical examination:
• General
° Pulse, BP, LN, Clubbing. neurocutaneous markers
° Other systems – DVS Valvular heart disease, CAD, Hypertensive heart disease
• Neurological examination
° Higher functions ° Reflexes
° Cranial nerves ° Sensory — +Cortical
° Tone ° Cerabellar
° Power Grade, symmetry ° Meningeal irritaion
4 Neurology BFOM 38 Team
4th Year 2nd Semester 2nd Module Medicine III
Features of UMN Lesions Features of LMN Lesions
• Weakness • Weakness
• Hypertonia • Hypotonia
• Deep reflex exaggerated • Loss of tendon reflex
• Loss of abdominal reflex • Fasciculation of muscle
• No muscle wasting • Contracture of muscle
• Distal muscle groups affected • Trophic changes
• Axial movements, extraocular, upper facial,
pharyngeal and jaw muscles are spared
• Extensor plantar
Hemiplegia patients usually show a
characteristic gait. The leg on the
affected side is extended and internally
rotated and
The upper limb on the same side is also
adducted at the shoulder, flexed at the
elbow, and pronated at the wrist with the
thumb tucked into the palm and the
fingers curled around it.
Investigations:
• Labs:
° CBC, lytes, urea, Cr, glucose, troponin,
° CK, PTT, INR, AST, ALT, ALP, bilirubin, total cholesterol, TGL, LDL, HDL,
homocysteine, ESR
• Imaging
° CT head without contrast
° MRI head (more sensitive than CT head in detecting acute ischemic stroke)
° angiogram (CT, MR, contrast)
° carotid Dopplers, echocardiogram (TEE > TTE)
• Special
° ECG—ST depression, QT prolongation, inverted T, prominent U waves
° holter monitor—evaluation for occult atrial fibrillation
° EEG—if seizures
° toxicology screen
5 Neurology BFOM 38 Team
4th Year 2nd Semester 2nd Module Medicine III
Ischemic stroke
Categories of treatment:
Designed to reverse or lessen the amount of tissue infarction and improve clinical outcome
1. Medical Support 4. Antithrombotic Treatment
2. IV Thrombolysis 5. Neuroprotection
3. Endovascular Techniques 6. Stroke Centers and Rehabilitation
1. Medical Support
• Immediate Goal: optimize cerebral perfusion in the surrounding ischemic penumbra
• Attention is also directed toward preventing the common complications of bedridden
patients:
° infections
° deep venous thrombosis (DVT)
• Blood pressure is lowered in:
° malignant hypertension
° concomitant myocardial ischemia
° BP >185/110 mmHg and thrombolytic therapy is anticipated
° B1-adrenergic blocker such as Esmolol can be a first step to decrease cardiac work and
maintain BP
2. IV Thrombolysis: rtPA:
Indications Contraindications
Clinical diagnosis of STROKE Sustained BP > 185/110 mmHg despite Rx
Onset of symptoms to time of drug Platelets LESS THAN 100,000;
administration is LESS THAN 3 HOURS Hematocrit LESS THAN 25%;
Glucose LESS THAN 50 or GREATER
THAN 400 mg/dl
CT scan show no hemorrhage or edema of Use of Heparin within 48 HOURS and
GREATER THAN 1/3 of the MCA territory prolonged PTT or elevated INR ; GI bleeding
preceding 21 DAYS
Age ≥ 18 years old Rapidly improving , minor stroke symptoms
Consent by patient or surrogate Prior stroke or head injury within 3
MONTHS; recent myocardial infarction
Major surgery in preceding 14 days
Coma or stupor
6 Neurology BFOM 38 Team
4th Year 2nd Semester 2nd Module Medicine III
3. Endovascular Techniques
• Vessels that involve a large clot volume and often fail to open with IV rtPA alone:
° middle cerebral artery (MCA)
° internal carotid artery
° basilar artery
• Endovascular mechanical thrombectomy:
° Adjunctive treatment of acute stroke in patients who are ineligible for, or have
contraindications to thrombolytics, or those who have failed to have vascular
recanalization with IV thrombolytics
4. Antithrombotic Treatment
Platelet inhibition:
• ASPIRIN: the ONLY antiplatelet agent that has been proven effective for the acute
treatment of ischemic stroke
• The use of aspirin within 48 hours of stroke onset reduced both stroke recurrence risk and
mortality minimally
Prognosis
• It is not a progressive disorder, except like in a growing brain tumor.
• Complications
° Neurologic — cerebral edema, seizures, hemorrhagic transformation of infarction with
or without hematoma, neurological deficits (dysphagia, falls, compressive neuropathies)
° Non-neurologic — myocardial infarction, arrhythmia, aspiration, pneumonia, UTI,
DVT, pulmonary embolism, malnutrition, pressure sores, orthopedic complications,
contractures, sleep disordered breathing, depression
7 Neurology BFOM 38 Team
You might also like
- STROKE: Handbook with activities, exercises and mental challengesFrom EverandSTROKE: Handbook with activities, exercises and mental challengesNo ratings yet
- Neuro - Internal Medicine, Dr. A. MowafyDocument117 pagesNeuro - Internal Medicine, Dr. A. MowafyMohammed RisqNo ratings yet
- HUD Settlement Statement - 221-1993Document4 pagesHUD Settlement Statement - 221-1993Paul GombergNo ratings yet
- Cerebrovascular DiseaseDocument54 pagesCerebrovascular Diseaselisaagustina100% (1)
- Q1.Flaccid Paresis: Diagnostical VariantsDocument47 pagesQ1.Flaccid Paresis: Diagnostical VariantsNelson OduorNo ratings yet
- FULL BODY WORKOUT A PDF Jeremyethier PDFDocument15 pagesFULL BODY WORKOUT A PDF Jeremyethier PDFGaston.R100% (1)
- Neurology Multiple Choice Questions With Explanations: Volume IIFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IIRating: 5 out of 5 stars5/5 (2)
- Neurology Equations Made Simple: Differential Diagnosis and NeuroemergenciesFrom EverandNeurology Equations Made Simple: Differential Diagnosis and NeuroemergenciesNo ratings yet
- Cerebrovascular Accident or Stroke: By: Thalia Nicole SanchezDocument19 pagesCerebrovascular Accident or Stroke: By: Thalia Nicole SanchezMaesy LorenaNo ratings yet
- Cerebrovascular Accident (CVA) "Stroke": Ma. Tosca Cybil A. Torres, RN, MANDocument53 pagesCerebrovascular Accident (CVA) "Stroke": Ma. Tosca Cybil A. Torres, RN, MANMa Tosca Cybil TorresNo ratings yet
- Tues 10-20 Peripheral Nerve Disorders - A Practical OverviewDocument36 pagesTues 10-20 Peripheral Nerve Disorders - A Practical OverviewGery FirmansyahNo ratings yet
- Sample SHARKS Worksheet PDFDocument10 pagesSample SHARKS Worksheet PDFAmruta Chhajed100% (2)
- CVA or StrokeDocument14 pagesCVA or StrokeJoenalyn AliguinNo ratings yet
- Neuropatologi KuliahDocument67 pagesNeuropatologi KuliahNanda PutriarmyNo ratings yet
- Oleh: Dr. Cahyono Kaelan, PH.D, SP - PA (K), SP.S: NeuropathologyDocument67 pagesOleh: Dr. Cahyono Kaelan, PH.D, SP - PA (K), SP.S: NeuropathologyMagfira Al HabsyiNo ratings yet
- STROKEDocument108 pagesSTROKELorelie Asis75% (4)
- NeuropathologyDocument67 pagesNeuropathologyEmanuelNo ratings yet
- 4th Problem Emergency Medicine Group 1Document82 pages4th Problem Emergency Medicine Group 1Jonathan TandajuNo ratings yet
- Neurology Multiple Choice Questions With Explanations: Volume IFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IRating: 4 out of 5 stars4/5 (7)
- Cisco VoipDocument37 pagesCisco VoipLino Vargas0% (1)
- Tunisia - Country Profile: 1 Background 2 2 Population 2Document18 pagesTunisia - Country Profile: 1 Background 2 2 Population 2stand4xNo ratings yet
- StrokeDocument27 pagesStrokeJASON KO CHIA SHENGNo ratings yet
- Compiled Stroke RehabDocument121 pagesCompiled Stroke RehabJeel MohtaNo ratings yet
- Pathology of The CnsDocument38 pagesPathology of The Cnscy lifeNo ratings yet
- To Neurology: Rini AndrianiDocument46 pagesTo Neurology: Rini Andrianiwaraney palitNo ratings yet
- Neurology: - Neuron: Nerve, Logos: Knowledge - Neurology: Deals With The Prevention, Therapy andDocument49 pagesNeurology: - Neuron: Nerve, Logos: Knowledge - Neurology: Deals With The Prevention, Therapy andis kimNo ratings yet
- Unconscious and Comatose Patients DR Moses KazevuDocument17 pagesUnconscious and Comatose Patients DR Moses KazevuMoses Jr KazevuNo ratings yet
- Approach To Comatose Patient: Abyot B5 Female SideDocument16 pagesApproach To Comatose Patient: Abyot B5 Female SideashuNo ratings yet
- Hemiplegia: Jinu Janet Varghese Group: 4 Year: 3 Tbilisi State Medical UniversityDocument21 pagesHemiplegia: Jinu Janet Varghese Group: 4 Year: 3 Tbilisi State Medical UniversitySundarNo ratings yet
- Brain Hemorrhage and Dementia GuideDocument42 pagesBrain Hemorrhage and Dementia Guidevenia endah tamaraNo ratings yet
- Disorders of The Brainstem and Cranial Nerves SY 2022-2023Document141 pagesDisorders of The Brainstem and Cranial Nerves SY 2022-2023Geraldine Teopy100% (1)
- Brain-Attack or Stroke or Cerebrovascular-AccidentDocument29 pagesBrain-Attack or Stroke or Cerebrovascular-AccidentMission JupiterNo ratings yet
- Brain TumorDocument43 pagesBrain TumorjeremiahNo ratings yet
- Head Trauma DR Petra SPBSDocument64 pagesHead Trauma DR Petra SPBSAlessia Wyneini TirzaNo ratings yet
- StrokeDocument58 pagesStrokeMarah AbdulrahimNo ratings yet
- Introduction To Clinical Medicine (ICM) : Case Studies Neurologic DisordersDocument142 pagesIntroduction To Clinical Medicine (ICM) : Case Studies Neurologic DisordersomarNo ratings yet
- Neurology (Cerebrovascular Disease)Document69 pagesNeurology (Cerebrovascular Disease)Mahadhir AkmalNo ratings yet
- Brain InjuryDocument35 pagesBrain InjuryAkhil Adhithyan RamNo ratings yet
- Pathology of the Central Nervous System: Neurodegenerative Diseases and CNS TumorsDocument67 pagesPathology of the Central Nervous System: Neurodegenerative Diseases and CNS TumorsLIEBERKHUNNo ratings yet
- Head Trauma: George Ayoub - Med3Document23 pagesHead Trauma: George Ayoub - Med3Joe KhdeirNo ratings yet
- NeurologyDocument42 pagesNeurologyPierre BenardNo ratings yet
- Stroke: Cerebrovascular Accident Could BeDocument8 pagesStroke: Cerebrovascular Accident Could Berazan asadNo ratings yet
- How To Localize Neurological LesionDocument25 pagesHow To Localize Neurological LesionBeenish IqbalNo ratings yet
- Neurology Review: Omar K. MRCP Ireland 2015Document58 pagesNeurology Review: Omar K. MRCP Ireland 2015Manmeet SNo ratings yet
- Intracranial HemorrhageDocument75 pagesIntracranial HemorrhageDea DNo ratings yet
- Nervous System (S.S)Document112 pagesNervous System (S.S)Suman ShahNo ratings yet
- NeurologyDocument37 pagesNeurologyDevangkumar PatelNo ratings yet
- Cerebrovascular DisordersDocument23 pagesCerebrovascular Disordersbpt2No ratings yet
- CVA SushilaDocument70 pagesCVA SushilaSushila Hamal ThakuriNo ratings yet
- REHABILITASI MEDIK PADA PENDERITA STROKEDocument55 pagesREHABILITASI MEDIK PADA PENDERITA STROKEKrisma susantiNo ratings yet
- 19 - Traumatic Brain InjuryDocument62 pages19 - Traumatic Brain InjurymichelleNo ratings yet
- Examination of Unconscious PersonDocument33 pagesExamination of Unconscious Personsylvia haryantoNo ratings yet
- Cerebral Ischemic StrokeDocument78 pagesCerebral Ischemic Strokemirabel IvanaliNo ratings yet
- Spinal Cord DS C1Document76 pagesSpinal Cord DS C1Dagmawi BahiruNo ratings yet
- Pathology of the Central Nervous System (CNSDocument53 pagesPathology of the Central Nervous System (CNSRikizu HobbiesNo ratings yet
- Headache Neuroimaging FinalDocument85 pagesHeadache Neuroimaging Finaldinesh kumarNo ratings yet
- Neurosurgery Case 1Document111 pagesNeurosurgery Case 1api-3704562No ratings yet
- Pathology of CNS: Eric M. Mirandilla MD, DPSPDocument71 pagesPathology of CNS: Eric M. Mirandilla MD, DPSPDhruva PatelNo ratings yet
- Seminar on Management of StrokeDocument54 pagesSeminar on Management of Stroke7762n9qsntNo ratings yet
- Module 56 - Group 4Document27 pagesModule 56 - Group 4Katherine May F. LloritoNo ratings yet
- Dr. Cahyono K, PH.D, SP - PA, SP.S - Patologi Anatomi Neurofisiologi PDFDocument66 pagesDr. Cahyono K, PH.D, SP - PA, SP.S - Patologi Anatomi Neurofisiologi PDFinnalNo ratings yet
- Medical Disorders of The CNS, CvaDocument46 pagesMedical Disorders of The CNS, CvaMalueth AnguiNo ratings yet
- Stroke: Nivedita MPT (Neuro)Document27 pagesStroke: Nivedita MPT (Neuro)MenakaNo ratings yet
- Tues 10-20 Peripheral Nerve Disorders - A Practical OverviewDocument37 pagesTues 10-20 Peripheral Nerve Disorders - A Practical OverviewfatehmaanNo ratings yet
- Aicardi’s Diseases of the Nervous System in Childhood, 4th EditionFrom EverandAicardi’s Diseases of the Nervous System in Childhood, 4th EditionAlexis ArzimanoglouNo ratings yet
- L1 Cerebrovascular Anatomy and Nerves of Lower LimbDocument48 pagesL1 Cerebrovascular Anatomy and Nerves of Lower LimbAshraf NabilNo ratings yet
- L3 Blood Supply of The Brain From DR - Shawky NeurologyDocument5 pagesL3 Blood Supply of The Brain From DR - Shawky NeurologyAshraf NabilNo ratings yet
- L4 Paraplegia & Neurogenic Bladder EditedDocument4 pagesL4 Paraplegia & Neurogenic Bladder EditedAshraf NabilNo ratings yet
- Lesson 5Document16 pagesLesson 5DANANo ratings yet
- Showcase your talent and skills at Momentum 2021Document48 pagesShowcase your talent and skills at Momentum 2021Tanishq VermaNo ratings yet
- A Case Study On Strategies To Deal With The Impacts of COVID-19 Pandemic in The Food and Beverage IndustryDocument13 pagesA Case Study On Strategies To Deal With The Impacts of COVID-19 Pandemic in The Food and Beverage IndustryPeyman KazemianhaddadiNo ratings yet
- Plates of The Dinosaur Stegosaurus - Forced Convection Heat Loos FinsDocument3 pagesPlates of The Dinosaur Stegosaurus - Forced Convection Heat Loos FinsJuan Fernando Cano LarrotaNo ratings yet
- Emmanuel Oneka - CV-3Document3 pagesEmmanuel Oneka - CV-3Emmanuel OnekaNo ratings yet
- Readings in Philippine History: Tanza, Boac, MarinduqueDocument16 pagesReadings in Philippine History: Tanza, Boac, MarinduqueLucy SyNo ratings yet
- bài tập ôn MA1Document34 pagesbài tập ôn MA1Thái DươngNo ratings yet
- Tds CPD Sika ViscoCrete 2100 Us PDFDocument2 pagesTds CPD Sika ViscoCrete 2100 Us PDFSamirHashimNo ratings yet
- 5 Harms of Excessive Use of Electronic GamesDocument3 pages5 Harms of Excessive Use of Electronic GamesPierre MarucciNo ratings yet
- User's Manual: 2.5" External Hard DriveDocument26 pagesUser's Manual: 2.5" External Hard DriveMathew PhilipNo ratings yet
- Lesson 2.1Document16 pagesLesson 2.1Jeremie Manimbao OrdinarioNo ratings yet
- CH 6 SandwichesDocument10 pagesCH 6 SandwichesKrishna ChaudharyNo ratings yet
- Calculus (Solution To Assignment Iv) : February 12, 2012Document4 pagesCalculus (Solution To Assignment Iv) : February 12, 2012Mawuena MelomeyNo ratings yet
- The Making of BuckshotDocument13 pagesThe Making of BuckshotDominicNo ratings yet
- CRM Assignment FrankfinnDocument4 pagesCRM Assignment FrankfinnJyoti Choudhary60% (5)
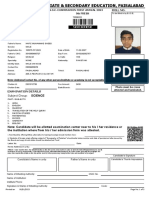
- Roll No. Form No.: Private Admission Form S.S.C. Examination First Annual 2023 9th FRESHDocument3 pagesRoll No. Form No.: Private Admission Form S.S.C. Examination First Annual 2023 9th FRESHBeenish MirzaNo ratings yet
- 37LG5500Document33 pages37LG5500Toni011973No ratings yet
- Reg0000007635187Document2 pagesReg0000007635187Amal JimmyNo ratings yet
- Sonic sdw45Document2 pagesSonic sdw45Alonso InostrozaNo ratings yet
- AssignmentDocument34 pagesAssignmentAnshika SharmaNo ratings yet
- 2nd Quarter Week 7Document5 pages2nd Quarter Week 7Lymieng LimoicoNo ratings yet
- 14 Month Old Milestones and DevelopmentDocument6 pages14 Month Old Milestones and Developmentjovilene.abrinaNo ratings yet
- Legal Disclaimer - Learn About Our Limited Liability and Legal DisclaimerDocument2 pagesLegal Disclaimer - Learn About Our Limited Liability and Legal DisclaimermagamuthaNo ratings yet
- 5 Ear Disorders of DogsDocument14 pages5 Ear Disorders of DogsKoleen Lopez ÜNo ratings yet
- GSAA HET 2005-15, Tranche M2 - JPMorgan Investment Funds / Income Oppt'y FundDocument192 pagesGSAA HET 2005-15, Tranche M2 - JPMorgan Investment Funds / Income Oppt'y FundTim BryantNo ratings yet
- Be Healthy, Happy and Holy - Sleep by 10 PM (By Mahanidhi Swami) PDFDocument4 pagesBe Healthy, Happy and Holy - Sleep by 10 PM (By Mahanidhi Swami) PDFDay FriendsNo ratings yet