Professional Documents
Culture Documents
Anne Duffy The Nature of The Association Between Childhood ADHD and The Development of Bipolar Disorder A Review of Prospective High-Risk Studies
Uploaded by
Fábio Yutani KosekiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anne Duffy The Nature of The Association Between Childhood ADHD and The Development of Bipolar Disorder A Review of Prospective High-Risk Studies
Uploaded by
Fábio Yutani KosekiCopyright:
Available Formats
Reviews and Overviews
Mechanisms of Psychiatric Illness
The Nature of the Association Between Childhood
ADHD and the Development of Bipolar Disorder:
A Review of Prospective High-Risk Studies
Anne Duffy, M.D., F.R.C.P.C. Objective: The author reviewed pro- of childhood ADHD is not a reliable pre-
spective longitudinal studies of the off- dictor of the development of bipolar disor-
spring of parents with bipolar disorder to der. However, the author found evidence
inform our understanding of the nature that symptoms of inattention may be part
of the association between childhood ADHD of a mixed clinical presentation during the
and the risk of developing bipolar disorder early stages of evolving bipolar disorder
in adolescence and young adulthood. in high-risk offspring, appearing alongside
anxiety and depressive symptoms. The
Method: A literature review of published
author also found preliminary evidence
prospective cohort studies of the offspring
that childhood ADHD may form part of
of bipolar parents since 1985 was un-
a neurodevelopmental phenotype in off-
dertaken using a comprehensive search
spring at risk for developing a subtype of
strategy in several electronic databases.
bipolar disorder unresponsive to lithium
The author provides a qualitative synthe-
stabilization.
sis of results focusing on ADHD and the
association with bipolar disorder in pro-
Conclusions: While childhood ADHD does
spectively assessed high-risk offspring.
not appear to be part of the typical develop-
These results are discussed in light of
mental illness trajectory of bipolar disorder,
findings from other prospective epidemi-
subjective problems with attention can
ological and clinical cohort studies.
form part of the early course, while neuro-
Results: From the reviewed high-risk studies, developmental abnormalities may be ante-
evidence suggests that the clinical diagnosis cedents in a subgroup of high-risk children.
(Am J Psychiatry 2012; 169:1247–1255)
O ne of the most important recent observations in
psychiatry came from the Dunedin longitudinal cohort
the current diagnostic classification systems, which were
primarily designed to describe end-stage rather than evolv-
study—namely, that the majority (almost 75%) of adults ing disorders. Outside of research protocols, there is no
affected with psychiatric disorders had diagnosable psy- systematic language or consensus criteria to describe the
chiatric syndromes before age 18, and almost half before evolution of major psychiatric disorders over the course of
age 15 (1). Furthermore, the nature of antecedent child- development. Rather, antecedents are treated as separate
hood psychopathology was often different from that of the conditions, adding to the variety of meanings of the term
adult disorder (heterotypic development). These findings “comorbid” (2). As discussed by Robins (3), from DSM-III
emphasized that a substantial number of adult psychiatric onward, multiple diagnoses in a single patient have been
disorders manifest clinically much earlier in development, allowed, even when the symptoms fit within a single
although the childhood presentation may not resemble diagnostic category, while temporal relationships between
the full-blown adult disorder. Therefore, the challenge for conditions have been ignored. This approach contradicts
those involved in early detection and intervention is to the principle applied elsewhere in medicine; namely that
map the developmental trajectory of major psychiatric the presentation is subsumed under one diagnosis unless
disorders from the earliest reliable antecedents. The most evidence proves otherwise. What is not clear is the nature
effective research paradigm to accomplish this goal is to of the association between comorbid conditions within
prospectively study high-risk children over the course of individuals, which likely includes 1) different manifesta-
development and into early adulthood. tions (during development and over the course of illness)
The results of longitudinal prospective studies of high- of a common etiological process, 2) complications of
risk youths have already highlighted shortcomings of a primary illness, 3) different illness subtypes (different
This article is the subject of a CME course (p. 1333)
Am J Psychiatry 169:12, December 2012 ajp.psychiatryonline.org 1247
CHILDHOOD ADHD AND THE DEVELOPMENT OF BIPOLAR DISORDER
etiology), and 4) artifact associated with a splitting rather a parent with confirmed bipolar disorder and if they reported on
than a lumping diagnostic convention. The key point for rates of psychopathology among the offspring. A comprehen-
sive search strategy involving combinations of Medical Subject
this article is that the temporal pattern of psychopathology
Headings (ADHD, bipolar disorder, children of bipolar parents,
is important in informing our understanding of differential cohort studies) and title and abstract terms (bipolar, mood
illness trajectories in high-risk youth. disorder, major affective disorder offspring, child, adolescent,
A developmental approach to mapping the natural his- longitudinal prospective, attention deficit) was conducted in
tory of bipolar disorder has been a major research focus MEDLINE, Embase, and PsycINFO. The search was restricted to
publications after January 1985. Reference searching was also
worldwide for over 20 years. Given that bipolar disorder
conducted in all included studies.
has a substantial genetic component with an estimated
heritability of around 85% (4), and that onset occurs in Results
adolescence or young adulthood, children of affected pa-
rents represent a readily identifiable high-risk group that Characteristics of Included Studies
is uniquely well suited to longitudinal research. Assuming The literature search identified nine studies that met
that there is confidence about the bipolar diagnosis in inclusion criteria for review (Table 1). Recruitment and
the parent, longitudinal prospective assessment of the selection criteria as well as the methods employed to
offspring into adulthood allows for the identification of evaluate psychopathology in the parent and offspring
antecedent vulnerabilities and the characterization of the differed among the studies, as detailed elsewhere (18).
early course, while minimizing important confounds, in- However, most studies used semistructured clinical in-
cluding instability of diagnoses in young clinical samples terviews of both the parent and offspring, conducted
(5) and burden-of-illness effects (repeated episodes, psy- by interviewers initially blind to family affiliation, and
chosis, substance use, treatment, and medical illness) (6). consensus diagnostic procedures to arrive at DSM di-
Several published longitudinal prospective studies of agnoses. Some studies included other informants (e.g.,
offspring of bipolar parents have led to the convergent teachers) and used standardized questionnaires to mea-
observation that the index hypomanic or manic episode sure attentional, behavioral, and emotional symptom
is often preceded by childhood anxiety, sleep, and de- levels. Two of the included studies were limited by
pressive disorders in early adolescence. These observa- relatively short follow-up periods and small high-risk
tions are further supported by findings from a number of offspring samples and are not formally discussed here
cross-sectional high-risk studies reporting a wide variety (19, 20). Other studies were more informative given the
of lifetime disorders in offspring of bipolar parents (for comparison groups included (21, 22) and the detailed
reviews, see Delbello and Geller [7], Lapalme et al. [8], and prospective clinical assessments of referred youths (23,
Duffy [9]). What remains a subject of debate is whether or 24). The remaining studies report on larger samples of
not ADHD is a reliable childhood antecedent predicting offspring who had a parent with well-characterized bipolar
the development of bipolar disorder. This question arose disorder and who were followed on average for at least
in part from observations of a high rate of “manic-like” 5 years into adolescence and adulthood (25–27).
symptoms in clinical samples of children with ADHD (10,
11), a high rate of ADHD in clinically referred children Review of Prospective High-Risk Studies
with ultra-rapid cycling bipolar disorder (12), and a high Laroche et al. (23, 28) published findings from a 3- to 7-
rate of comorbidity in some cross-sectional studies of year prospective follow-up study reporting on 37 off-
children of bipolar parents (13). However, the diagnosis spring from 21 families with a bipolar parent selected
of mania in clinically referred pediatric samples is a point from an outpatient clinic; there were no control families
of debate (14), and elevated rates of comorbid ADHD and for comparison. The bipolar parent had to have been
bipolar disorder are not consistently found in pediatric maintained on lithium for at least 1 year and have
clinical (15) or high-risk study cohorts (16, 17). children between 5 and 18 years old. At the time of last
My aim in this article is to clarify the nature of the assessment, the mean age of offspring was 16.2 years
debated association between ADHD and bipolar disorder (range58–25 years). DSM diagnoses were made in 24% of
by reviewing findings from prospective longitudinal the offspring (N59/37) and clustered in the affective/
studies of children and adolescents at familial risk of internalizing domain. While no cases of full-threshold
bipolar disorder and to discuss these findings in light of ADHD were diagnosed, the study reported significantly
those from complementary prospective epidemiological higher scores in hyperactive, anxiety, neurotic, and de-
and clinical cohort studies. I then propose an integrative pression symptoms in the high-risk offspring who had
model of these illness trajectories highlighting areas of a DSM diagnosis (mostly mood and anxiety disorders)
clinical overlap and differentiation. compared with those who did not. These findings suggest
that early in the course of evolving bipolar disorder,
Method anxiety and minor depressive disorders dominate and that
Longitudinal and prospective studies were included in this inattention symptoms may occur in the context of the
review if they were published cohort studies of offspring of evolving mood disorder.
1248 ajp.psychiatryonline.org Am J Psychiatry 169:12, December 2012
ANNE DUFFY
TABLE 1. Prospective Longitudinal Studies of the Offspring of Bipolar Parents Published Between 1985 and 2011
Mean Age at Range of Age Duration of
Authors N % Female Recruitment at Recruitment Follow-Up Lifetime Rate of ADHD
Akiskal et al. (24) 68 43 Juveniles Mean53 years 5.9% high risk
(#24 years old)
Duffy et al. 216 60 16.5 years 8–25 Mean55.5 years 8% high risk; 3% control
(25, 33–36) (up to 15 years)
Hammen et al. (22) 18 56 13.6 years 8–16 Up to 3 years 6% high risk; 5% control
Hillegers et al. 140 49 16.1 years 12–21 5 years 5% high risk
(16, 26, 32)
Laroche et al. 39 36 11.4 years 5–18 3–7 years 0% high risk
(23, 28)
Nurnberger et al. (19) 53 55 19.5 years 15–25 Up to 2 years ADHD in one out of five
affected high risk
Radke-Yarrow et al. 44 50 Stratified into 3 years; 23 yearsa 0% high risk; 0% control
(21), Meyer et al.a 1.5–3.5 and
(29) 5–8 years
Shaw et al. (27, 31) 100 52 Mean 7.5 years 10 years “ADHD relatively absent”
(most ,14)
Zahn-Waxler et al. 7 0 Up to 2 years Up to 4 years 0% high risk; 0% control
(20)
a
Dynamic cohort that included some of the original families.
Radke-Yarrow et al. (21) reported on a community co- with no mood disorder in adulthood. The authors also
hort of children of affectively ill and well mothers after reported that specific deficits in executive functioning
3 years of prospective follow-up. Two siblings from 100 during adolescence (as evidenced by certain parame-
families were included, one in infancy (1.5–3.5 years old) ters on the Wisconsin Card Sorting Test) and premorbid
and the other in early childhood (5–8 years old). An attention problems preceded the formal diagnosis and
association between disruptive behavior disorders and treatment of bipolar disorder. All offspring with both
families under higher stress (x257.05, p,0.01) and from childhood attention problems and executive functioning
lower socioeconomic status (x257.46, p,0.02) was re- deficits in adolescence were diagnosed with bipolar dis-
ported. Children of affectively ill mothers were more likely order. These findings are limited by the small number of
to manifest problems with depression symptoms in middle cases of bipolar disorder and by the degree of assortative
(x2518.69, p,0.0001) and in later childhood (x2510.77, mating in the families. Nonetheless, they are consistent
p,0.0001). Anxiety disorders were identified in infancy with the interpretation that in at least some high-risk
and early childhood in offspring of both healthy and children, cognitive antecedents, but not a clinical diag-
depressed mothers, whereas anxiety did not become nosis of ADHD, are associated with a subsequent risk of
frequent until later childhood in offspring of bipolar developing bipolar disorder.
mothers. In summary, it became evident that children of In a prospective study of school-age children (8–16 years
depressed mothers were the most severely affected with old) of mothers with bipolar disorder, depression, chronic
psychiatric problems across internalizing and externaliz- medical illness, or mothers who were healthy, Hammen
ing domains from preschool through early and later et al. (22, 30) reported on psychopathology and psycho-
childhood. Children of bipolar mothers held an interme- social problems (based on the Child Behavior Checklist
diate position, with psychiatric and behavioral problems completed by the mother and a teacher) at baseline and at
becoming evident in middle and later childhood. A gender 6-month intervals until age 3 years. ADHD was diagnosed
effect, with boys showing more disruptive problems and in 6% of offspring of bipolar mothers compared with 9%
girls more internalizing problems, was also reported. of offspring of depressed mothers and 5% of offspring of
In subsequent years, this cohort was followed up in healthy comparison mothers. A substantial proportion of
adolescence (11–19 years old) and again in young adult- the psychopathology of the offspring of bipolar mothers
hood (18–28 years old), with some families joining the was milder than that of the offspring of depressed
study, some changing category, and others leaving the mothers, with anxiety disorders being prominent. Based
study. Main findings reported by Meyer et al. (29) included on maternal and teacher reports, there was no difference
that 19% (N56/32) of the offspring of bipolar mothers in social competence, school behavior scores, or aca-
and 7% (N53/42) of the offspring from unipolar mothers demic performance ratings between the children of bipolar
developed bipolar disorder at a mean age of 16.6 years. mothers and the children of healthy mothers (30). While
Based on rating scales, the study found a higher rate of limited by the relatively small number of children followed
childhood attention and behavioral symptoms in the off- for up to 3 years, the findings are consistent with the
spring who developed bipolar disorder relative to those interpretation that ADHD is not overly represented among
Am J Psychiatry 169:12, December 2012 ajp.psychiatryonline.org 1249
CHILDHOOD ADHD AND THE DEVELOPMENT OF BIPOLAR DISORDER
the offspring of bipolar mothers and that the early psy- in school, low energy, excited, hyper alert, mood changes/
chosocial and school functioning of these high-risk off- labile, school role impairment, sensitivity, somatic complaints,
spring is generally comparable to that of the healthy and stubborn/determined. There was also evidence of a
population and different from that of children of depressed phasic nature of the symptoms involving mood, energy,
mothers. sleep, and temper problems.
Akiskal et al. (24) charted the prospective course of At the 10-year follow-up, the mean age of the offspring
evolving psychopathology in 68 referred (symptomatic) groups was 17–18 years, and 41% of the offspring of bipolar
juvenile relatives (offspring and siblings) of adult patients parents were tagged as being at risk based on symptom
with confirmed bipolar disorder who were assessed and profiles, compared with 16% of the offspring from com-
treated in a specialty mood disorders outpatient clinic. At parison families (82% from the positive family history
baseline, 44 of the 68 high-risk youths had been previously subgroup). The same core symptoms remained at higher
seen by child mental health professionals, and 16 had been frequency in the high-risk offspring except that low
diagnosed with emotional problems related to family or energy, anger, fearfulness, and sensitivity dropped below
peers, eight with neurotic (anxiety) disorders, seven with significance level, while high energy, sleep difficulties,
conduct disorder, seven with schizophrenia, and four with excessive talking, loud talking, and problems with think-
ADHD. Interestingly, none of the offspring assessed in ing and concentration reached significance. Taken to-
childhood were thought to have a primary mood disorder. gether, these findings suggest that during development,
Within the first year of prospective study, 24 youths were putative prodromal features in high-risk offspring shifted
diagnosed with major depression, 11 with manic or mixed from anxiety-depressive to more manic symptoms. Dis-
episodes, and 22 with subaffective disorders. After an aver- tractibility, stubbornness, and being easily upset were
age of 3 years of prospective study, recurrences occurred first noted early in childhood, alongside the affective
in those with major affective disorders as well as con- symptoms, whereas “problem concentrating” was asso-
version from subaffective to major affective and from ciated with manic-like symptom clusters later in devel-
unipolar to bipolar spectrum. In summary, nonaffective opment. The episodic nature of these symptom clusters
childhood diagnoses preceded the onset of minor and continued throughout development. Furthermore, the
major mood disorders. Depressive and subaffective dis- authors confirmed that ADHD as a syndrome was “rela-
orders predominated early in the course, while full-blown tively absent.”
hypomanic and manic episodes were not seen until after An ongoing prospective study of 140 children of bipo-
age 13. Finally, similar to the findings of Laroche et al. (28), lar parents in the Netherlands, reported by Wals et al.
childhood antecedents of “hyperactivity” and “antisocial” (16, 26, 32), builds on the findings of the previously de-
symptoms were described as “phasic,” occurring along- scribed studies. The majority of families (102 children;
side mood symptoms and not responsive to trials of mean age516.1 years) derived from a community-based
stimulant medication. Dutch Patient Association, while the others were identified
Egeland et al. reported on a prospective study of school- through outpatient clinics. High-risk families had compa-
age children of Amish parents affected with bipolar dis- rable socioeconomic status and higher IQs on average
order (100 children) and healthy parents (110 children) compared with those of the Dutch general population, and
who were systematically assessed at 7 years (31) and 10 76% of families were intact. While symptom rating scales
years (27) after baseline. The study evolved from research were generally comparable between the high-risk group
involving the adult Amish bipolar disorder patients, who and the normative population, daughters of bipolar parents
estimated that their illness manifested 9 to 12 years earlier had higher scores on Child Behavior Checklist subscales
than the age at onset of the full-blown diagnosis. The goal for total problems, internalizing, externalizing, somatic
was to identify which childhood symptoms predicted the complaints, anxious/depressed, social problems, delin-
development of bipolar disorder in the children at genetic quent behavior, and aggressive behavior. Sons of bipolar
risk. All families were from the Amish community and parents scored higher on Child Behavior Checklist sub-
comprised a high-risk group (one bipolar parent and one scales of total problems, externalizing, thought problems,
well parent), a comparison group with positive family and aggressive behavior. On self-report, high-risk older
history (one well sibling of the bipolar disorder proband adolescent girls reported more attention problems, while
and the other well parent), and a comparison group with teachers reported no differences in attention or behavior
negative family history (two well parents and no relatives problems in the high-risk boys or girls compared with the
with bipolar disorder). After 7 years of prospective follow- normative population.
up, 38% of the offspring of bipolar parents were tagged as At last follow-up, covering almost 5 years, the cohort had
being at risk based on symptom profiles, compared with 129 children, with a mean age of 20.8 years (26). The risk of
17% of the offspring from comparison families (83% from ADHD over the prospective waves of assessment remained
the positive family history subgroup). The specific clinical stable, while the risk of mood disorder and bipolar dis-
risk features flagged in the children of bipolar parents order increased. The lifetime risk was 10% for bipolar dis-
included anxious/worried, attention poor/distractible order (I or II), 40% for any diagnosable mood disorder, and
1250 ajp.psychiatryonline.org Am J Psychiatry 169:12, December 2012
ANNE DUFFY
5% for ADHD. In those high-risk offspring with bipolar Conclusions
disorder, the index mood diagnosis was almost always
depressive in polarity, at a mean age of 13.4 years (SD54.2), Major Findings
and the index hypomanic/manic episode manifested a While this qualitative review is limited by the number
mean of 4.9 years (SD53.4) later (at 18.4 years old). Only of prospective longitudinal high-risk studies collectively
one of these 13 bipolar subjects had treatment with sti- assessing a relatively small number of bipolar-affected
mulant medication before the development of the acti- offspring, the findings are consistent across studies. One
vated episode. Collectively, these findings lend further major finding from this review is that childhood ADHD
support to reports of a variety of emotional and behavioral does not appear to be significantly overrepresented
childhood antecedents followed by subaffective and de-
among the offspring of parents with well-characterized
pressive disorders in early adolescence, and hypomanic/
bipolar disorder compared with offspring of healthy
manic episodes later in life. ADHD, as a clinical diagnosis,
parents or with the risk of ADHD in the general pop-
was not higher in the high-risk offspring than in the gen-
ulation. Furthermore, although the data remain limited,
eral population based on either clinical interview assess-
there does not appear to be an association between ADHD
ment or teacher reports.
as a childhood diagnosis and the subsequent risk of bipolar
Finally, our group has published several reports from an
disorder in the high-risk offspring. Therefore, it seems rea-
ongoing longitudinal high-risk study (33–36). The high-risk
sonable to conclude that the clinical diagnosis of ADHD
families (one affected and one well parent) were selected
through specialty clinical research programs and diag- does not appear to be a reliable antecedent in the devel-
nosed based on best estimate procedure. Bipolar parents opmental trajectory toward bipolar disorder.
were divided on the basis of an unequivocal response or However, the risk of ADHD in the studies reviewed may
nonresponse to long-term lithium treatment. Lithium res- have been influenced by the high rate of intactness and
ponse identifies a more homogeneous subtype of classi- relatively high socioeconomic status of the high-risk fami-
cal bipolar disorder (37), while lithium nonresponse is lies. This speculation is indirectly supported by the find-
characterized by a chronic illness course and a higher ings of Birmaher and colleagues (17), who reported in a
familial risk of psychotic disorders (38). cross-sectional study of school-age children that rates of
Early on, we reported an association in the high-risk ADHD were not elevated among the offspring of bipo-
offspring between subjective problems in attention and lar parents relative to comparison subjects after adjust-
symptoms of depression that was not related to any ing for confounding variables (i.e., socioeconomic status
obvious deficit in sustained attention on psychological and non-bipolar disorder psychopathology in biological
testing (39). In subsequent analyses, our group found parents), suggesting that ADHD may be more related to
comparable lifetime rates of clinically significant ADHD the general burden of psychopathology in the families,
(often comorbid with learning disabilities) in high-risk rather than specifically to the risk of bipolar disorder.
(8.3%) and comparison offspring (5.8%) (25). The current Indirect support also comes from Radke-Yarrow et al. (21),
age-adjusted lifetime risk of major affective disorders who reported an association between higher rates of
in 231 high-risk offspring at a mean age of 25.7 years old disruptive behavior disorders in offspring from high-risk
(SD59.23) is estimated at 52.8% (mean age at onset516.8 families of lower socioeconomic status and those with
years) and bipolar disorder at 13.5%. Interestingly, higher more stress.
rates of ADHD and other neurodevelopmental abnor- An additional influence may have been the low rate
malities, including learning disabilities and cluster A traits, of psychopathology in the nonproband parents and low
were observed in the subgroup of offspring of parents comorbidity rates (especially of substance use and con-
who did not respond to lithium (35). Furthermore, a duct disorders) in the bipolar parents in some of the re-
recent analysis (40) found that this neurodevelopmental viewed studies (26, 27, 36). Furthermore, a number of the
phenotype was more frequently observed in high-risk high-risk studies reviewed here included affected parents
offspring who developed a substance use disorder com- with a more classical form of bipolar disorder that was
pared with those who did not (18.0% compared with completely responsive to or at least stabilized by lithium
9.3%, p50.06). While limited by a small sample, across and not typically associated with ADHD (23, 25, 31). For
this high-risk cohort, ADHD does not appear to be a example, among the Amish parent probands, ADHD was
robust predictor of major affective disorder or bipolar relatively absent based on expert clinician retrospective
disorder. Of those high-risk offspring with a childhood review of all available clinical information (31).
diagnosis of ADHD, 28% have so far gone on to develop However, attentional and cognitive symptoms and pro-
a major affective disorder (major depression or bipolar I or blems were reported by high-risk subjects and other in-
II) and 11% a minor affective disorder (dysthymia or de- formants (typically parents) in a number of the studies
pression not otherwise specified), while 93% of the high- reviewed here, consistent with a vulnerability trait in some
risk offspring with a major affective diagnosis did not have or as part of the early course of an evolving major affective
antecedent ADHD. disorder in others. For example, in the findings reported by
Am J Psychiatry 169:12, December 2012 ajp.psychiatryonline.org 1251
CHILDHOOD ADHD AND THE DEVELOPMENT OF BIPOLAR DISORDER
Duffy et al. (25, 35), ADHD was seen at an increased rate in observations add to the substantial evidence from pro-
offspring of parents with a psychotic spectrum bipolar spective studies of psychological and neurological ab-
disorder that failed to stabilize with lithium. A number of normalities in children who go on to develop adult
these children were diagnosed with full-blown ADHD by a schizophrenia, contrasting with the normal or advanced
child and adolescent psychiatrist and went on to develop premorbid intellectual functioning and school perfor-
a diagnosable affective disorder in adolescence. The course mance generally found in children who develop bipolar
of the mood disorder in these offspring (as in the parent) disorder in adulthood (41, 43).
tended to be nonepisodic, with residual symptoms between Another such study, the Oregon Adolescent Depression
acute episodes, and adult relatives had a differentially higher Project, followed a cohort of 1,709 high school students
loading of chronic psychotic disorders. Preliminary findings from representative urban and rural school districts as-
suggest that ADHD may form part of a neurodevelopmen- sessed at four time points from adolescence to early
tal childhood phenotype predicting a particular subtype adulthood. This cohort had a very low rate of full-blown
of bipolar disorder. In other words, bipolar disorder is bipolar disorder, while subthreshold bipolar disorder
known to be a heterogeneous diagnosis, and some subtypes symptoms were more common but transient. In a sub-
appear to overlap clinically and biologically with psychotic sequent analysis investigating the relationship of sub-
spectrum disorders (41). threshold conditions to the subsequent development of
On the other hand, a number of studies reviewed here full-blown disorders, Shankman et al. (44) reported that
reported that problems with attention and distractibility with the exception of ADHD and bipolar disorder, there was
manifest in high-risk offspring as part of a childhood in- an increased probability of escalating to full syndrome dis-
ternalizing condition. Furthermore, an important aspect orders (homotypic continuity). In the case of heterotypic
documented in several studies has been the periodic na- continuity, individual externalizing subthreshold condi-
ture of these early mixed symptom clusters, which again tions predicted the development of other full-syndrome
suggests a bipolar disorder diathesis characterized by a externalizing conditions (i.e., associations between ADHD,
recurrent illness course, rather than by a chronic course, as conduct, and substance use disorders), but not the de-
would be expected in the case of a typical developmental velopment of internalizing disorders or bipolar disorder.
disorder like ADHD. Therefore, in children at confirmed Finally, a recent analyses from the German Early De-
familial risk for the development of bipolar disorder, velopmental Stages of Psychopathology prospective
childhood ADHD may not be a clinical antecedent per se, study confirmed that hypomanic symptoms were common
but rather symptoms of inattention and distractibility and mostly transitory in the general adolescent population
may form part of an early subaffective clinical presentation (45). Almost 40% of 1,565 participants expressed bipolar
on the trajectory toward bipolar disorder. symptoms at one assessment, but only 17% experienced
these symptoms at two assessment times (46). In an
Prospective Studies of Clinically analysis of the association between risk factors, including
and Community-Referred Children ADHD, and the onset and persistence of subthreshold
Given the limitations of the high-risk data reviewed manic and depressive symptoms, cannabis use was asso-
here, findings from complementary prospective studies of ciated with the onset of manic symptoms (odds ratio54.26;
other cohorts of children can inform the interpretation of p50.010), while ADHD was associated with the persistence
the findings from this review. There have been several of depressive symptoms (45). Therefore, findings suggest
large prospective studies of epidemiological samples. One that hypomanic symptoms are often a normative tran-
of these is the Dunedin longitudinal birth cohort study, sient experience in adolescence and that ADHD does not
which followed 1,037 children with assessment points appear to be a risk factor in the general population for
through childhood, adolescence, and early adulthood. In the development of subthreshold or full-blown bipolar
the Dunedin study, adults diagnosed with mania were disorder.
more likely than those without mania to have a history of There have been differing reports on comorbidity rates
juvenile conduct or oppositional disorder and depression, between ADHD and bipolar disorder in pediatric clinical
but not ADHD (1). The authors noted that many adults cohorts, particularly in very young referred children
with bipolar disorder had antecedent childhood anxiety thought to be manic (47). As pointed out by Carlson (14),
disorders, but this association fell short of statistical sig- some of this variation may be due to assessment and
nificance. Interestingly, adults with schizophreniform sampling issues, as well as to differences in the concep-
disorders had a juvenile history of a number of disorders tualization and approach to diagnosis. Specifically, U.S.
including ADHD. In a subsequent report on this cohort research groups typically prefer standardized interviews
(42), schizophreniform disorder was associated with neu- emphasizing individual symptoms, while U.K. research
rodevelopmental and cognitive abnormalities during groups tend to adopt a clinical approach emphasizing
childhood, while adults with bipolar disorder had com- patterns of symptoms.
parable motor, language, and cognitive performance in Recently, Wozniak et al. (48) reported on the persistence
childhood to that of healthy comparison subjects. These of bipolar disorder after 4 years of prospective study in 78
1252 ajp.psychiatryonline.org Am J Psychiatry 169:12, December 2012
ANNE DUFFY
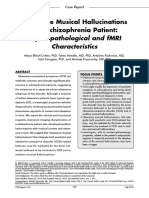
FIGURE 1. Developmental Trajectories of ADHD and Bipolar Disorder
ADHD ADHD ADHD
Oppositional Conduct Sociopathy
School problems disorders Substance use
Energetic
Emotional Cognitive Substance
Distractible
symptoms deficitsa abuse
Impulsiveb
Depressive and
Bipolar disorder
Anxiety disorders Adjustment
Substance use
disorders
Childhood Adolescence Early Adulthood
a
Subthreshold symptoms in a subset at risk for bipolar disorder unresponsive to lithium.
b
Episodic subthreshold symptoms in evolving bipolar disorder.
youths with a mean age of 13.4 years at last assessment nonspecific symptoms early in childhood (Figure 1).
and an estimated age of 4.9 years at onset of bipolar I Trajectories do not suggest that all children with ADHD
disorder. These youths, primarily boys with comorbid will go on to have persistent ADHD or to develop com-
ADHD, were ascertained from a tertiary care psychophar- plications or related disorders such as conduct or sub-
macology clinic that specializes in the treatment of ADHD. stance use disorders or sociopathy as adults, but rather
The course of bipolar disorder was mostly chronic, and these are outcomes of increased risk in this population.
only five children were in remission at last follow-up. Similarly, it is not that all offspring of parents with bipolar
Other reports of persistent manic-like presentations have disorder will manifest early childhood antecedents such as
been published (10, 47), and most of these reports show anxiety disorders or will develop sensitivity to stress or
a high rate of comorbidity with ADHD, externalizing depressive disorders in early adolescence, followed later
disorders, or pervasive developmental disorders. As re- by activated episodes. However, this predictive clinical
viewed recently by Leibenluft (49), some of these presen- sequence reflects a risk probability derived from pro-
tations have been recast as fitting criteria for severe mood spective studies.
dysregulation disorder and on prospective follow-up The other important observation from prospective high-
have not shown continuity with adult bipolar disorder. risk studies is that early in development and in the clinical
On the other hand, prospective studies of children with course, symptoms appear to be nonspecific and often
primary ADHD have been very consistent in supporting overlap between different evolving disorders; in the case
the findings of prospective epidemiological studies, of bipolar disorder and ADHD, impulsivity, labile mood,
namely, that ADHD in children is associated with a and internalizing symptoms (anxiety and depression) are
greater risk of antisocial behavior, criminal activity, con- not uncommon in childhood. Furthermore, in a selected
duct disorder, and substance use disorders in adoles- subset of children from bipolar parents with a high rate
cence and adulthood, but not to an elevated risk of of psychosis in family members and whose illness did
bipolar disorder (50, 51). not respond to lithium prophylaxis, ADHD and learning
disabilities may form part of an early neurodevelop-
Toward an Integrative Developmental Model mental phenotype that overlaps somewhat with the early
of ADHD and Bipolar Disorder presentation in children with primary ADHD. However,
In the end, prospective longitudinal studies provide very the temporal pattern of psychopathology against the
little evidence that ADHD is a reliable antecedent to the backdrop of differential familial risk sheds light on the
development of bipolar disorder that continues into adult- increasingly different illness trajectories, presumably
hood. In fact, substantial evidence has been reported from reflecting shared as well as different underlying patho-
prospective cohort studies of increasingly different illness physiological processes.
trajectories of ADHD and bipolar disorder over the course Longitudinal prospective research in large community
of development from a starting place of some overlapping and selected high-risk cohorts has been immensely helpful
Am J Psychiatry 169:12, December 2012 ajp.psychiatryonline.org 1253
CHILDHOOD ADHD AND THE DEVELOPMENT OF BIPOLAR DISORDER
in mapping the early natural history of major psychiatric bipolar disorder in clinically referred children. J Am Acad Child
disorders and in highlighting both homotypic and hetero- Adolesc Psychiatry 1995; 34:867–876
11. Biederman J, Faraone S, Mick E, Wozniak J, Chen L, Ouellette C,
typic developmental continuity of psychopathology over
Marrs A, Moore P, Garcia J, Mennin D, Lelon E: Attention-deficit
the course of illness development. Mapping the early hyperactivity disorder and juvenile mania: an overlooked
clinical course is the first step in advancing studies of the comorbidity? J Am Acad Child Adolesc Psychiatry 1996; 35:
associated neurobiological pathways and identifying novel 997–1008
targets for early intervention. Our diagnostic systems and 12. Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M,
Zimerman B: Two-year prospective follow-up of children with
approaches can catch up to the progress that prospective
a prepubertal and early adolescent bipolar disorder phenotype.
research has made by emphasizing the need, as in other Am J Psychiatry 2002; 159:927–933
areas of medicine, to incorporate the developmental 13. Chang KD, Steiner H, Ketter TA: Psychiatric phenomenology of
trajectory against the backdrop of risk as indicated by child and adolescent bipolar offspring. J Am Acad Child Adolesc
the family history of psychiatric disorders, in order to im- Psychiatry 2000; 39:453–460
14. Carlson GA: Will the child with mania please stand up? Br J
prove the accuracy and validity of psychiatric diagnosis in
Psychiatry 2011; 198:171–172
symptomatic youths. 15. Hassan A, Agha SS, Langley K, Thapar A: Prevalence of bipolar
disorder in children and adolescents with attention-deficit hy-
peractivity disorder. Br J Psychiatry 2011; 198:195–198
Received Nov. 24, 2011; revisions received April 16, May 9, and 16. Wals M, Hillegers MHJ, Reichart CG, Ormel J, Nolen WA, Verhulst
May 22, 2012; accepted May 29, 2012 (doi: 10.1176/appi.ajp.2012. FC: Prevalence of psychopathology in children of a bipolar
11111725). From the Department of Psychiatry, University of Calgary, parent. J Am Acad Child Adolesc Psychiatry 2001; 40:1094–1102
Alberta, Canada. Address correspondence to Dr. Duffy (acduffy@ 17. Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey
ucalgary.ca). MB, Obreja M, Ehmann M, Iyengar S, Shamseddeen W, Kupfer
Dr. Duffy has received personal support awards from the Brain and
D, Brent D: Lifetime psychiatric disorders in school-aged off-
Behaviour Research Foundation (NARSAD Young and Intermediate
spring of parents with bipolar disorder: the Pittsburgh Bipolar
Investigator Awards), from the Canadian Institutes of Health Research
(Young Investigator Award), and from the Canada Research Chairs Offspring study. Arch Gen Psychiatry 2009; 66:287–296
Program. 18. Duffy A, Doucette S, Lewitzka U, Alda M, Hajek T, Grof P: Find-
Supported by an operating grant from the Canadian Institutes of ings from bipolar offspring studies: methodology matters. Early
Health Research (MOP 102761). Interv Psychiatry 2011; 5:181–191
The author thanks Sarah Doucette for assistance with the table and 19. Nurnberger J, Hamovit J, Hibbs ED, Pelligrini D, Guroff JJ, Maxwell
figure and proofreading the manuscript. ME, Smith A, Gershon E: A high-risk study of primary affective
disorder: selection of subjects, initial assessment, and 1-to-2 year
follow-up, in Relatives at Risk for Mental Disorders. Edited by
Dunner D, Gershon E, Barrett J. New York, Raven Press Ltd, 1988,
pp 161–177
References
20. Zahn-Waxler C, Mayfield A, Radke-Yarrow M, McKnew DH,
1. Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton Cytryn L, Davenport YB: A follow-up investigation of offspring
R: Prior juvenile diagnoses in adults with mental disorder: de- of parents with bipolar disorder. Am J Psychiatry 1988; 145:
velopmental follow-back of a prospective-longitudinal cohort. 506–509
Arch Gen Psychiatry 2003; 60:709–717 21. Radke-Yarrow M, Nottelmann E, Martinez P, Fox MB, Belmont
2. Angold A, Costello EJ, Erkanli A: Comorbidity. J Child Psychol B: Young children of affectively ill parents: a longitudinal study
Psychiatry 1999; 40:57–87 of psychosocial development. J Am Acad Child Adolesc Psychi-
3. Robins LN: How recognizing “comorbidities” in psychopathol- atry 1992; 31:68–77
ogy may lead to an improved research nosology. Clin Psychol 22. Hammen C, Burge D, Burney E, Adrian C: Longitudinal study of
Sci Prac 1994; 1:93–94 diagnoses in children of women with unipolar and bipolar af-
4. Bienvenu OJ, Davydow DS, Kendler KS: Psychiatric “diseases” fective disorder. Arch Gen Psychiatry 1990; 47:1112–1117
versus behavioral disorders and degree of genetic influence. 23. LaRoche C, Cheifetz P, Lester EP, Schibuk L, DiTommaso E,
Psychol Med 2011; 41:33–40 Engelsmann F: Psychopathology in the offspring of parents with
5. Bromet EJ, Kotov R, Fochtmann LJ, Carlson GA, Tanenberg- bipolar affective disorders. Can J Psychiatry 1985; 30:337–343
Karant M, Ruggero C, Chang SW: Diagnostic shifts during the 24. Akiskal HS, Downs J, Jordan P, Watson S, Daugherty D, Pruitt DB:
decade following first admission for psychosis. Am J Psychiatry Affective disorders in referred children and younger siblings of
2011; 168:1186–1194 manic-depressives: mode of onset and prospective course. Arch
6. Duffy A, Lewitzka U, Doucette S, Andreazza A, Grof P: Biological Gen Psychiatry 1985; 42:996–1003
indicators of illness risk in offspring of bipolar parents: targeting 25. Duffy A, Alda M, Hajek T, Sherry SB, Grof P: Early stages in the
the hypothalamic-pituitary-adrenal axis and immune system. development of bipolar disorder. J Affect Disord 2010; 121:
Early Interv Psychiatry 2012; 6:128–137 127–135
7. DelBello MP, Geller B: Review of studies of child and adolescent 26. Hillegers MHJ, Reichart CG, Wals M, Verhulst FC, Ormel J, Nolen
offspring of bipolar parents. Bipolar Disord 2001; 3:325–334 WA: Five-year prospective outcome of psychopathology in the
8. Lapalme M, Hodgins S, LaRoche C: Children of parents with adolescent offspring of bipolar parents. Bipolar Disord 2005; 7:
bipolar disorder: a meta-analysis of risk for mental disorders. 344–350
Can J Psychiatry 1997; 42:623–631 27. Shaw JA, Egeland JA, Endicott J, Allen CR, Hostetter AM: A 10-
9. Duffy A: The early natural history of bipolar disorder: what we year prospective study of prodromal patterns for bipolar dis-
have learned from longitudinal high-risk research. Can J Psy- order among Amish youth. J Am Acad Child Adolesc Psychiatry
chiatry 2010; 55:477–485 2005; 44:1104–1111
10. Wozniak J, Biederman J, Kiely K, Ablon JS, Faraone SV, Mundy E, 28. Laroche C, Sheiner R, Lester E, Benierakis C, Marrache M,
Mennin D: Mania-like symptoms suggestive of childhood-onset Engelsmann F, Cheifetz P: Children of parents with manic-
1254 ajp.psychiatryonline.org Am J Psychiatry 169:12, December 2012
ANNE DUFFY
depressive illness: a follow-up study. Can J Psychiatry 1987; 32: 41. Demjaha A, MacCabe JH, Murray RM: How genes and environ-
563–569 mental factors determine the different neurodevelopmental
29. Meyer SE, Carlson GA, Wiggs EA, Martinez PE, Ronsaville DS, trajectories of schizophrenia and bipolar disorder. Schizophr
Klimes-Dougan B, Gold PW, Radke-Yarrow M: A prospective Bull 2012; 38:209–214
study of the association among impaired executive functioning, 42. Cannon M, Caspi A, Moffitt TE, Harrington H, Taylor A, Murray
childhood attentional problems, and the development of bi- RM, Poulton R: Evidence for early-childhood, pan-developmental
polar disorder. Dev Psychopathol 2004; 16:461–476 impairment specific to schizophreniform disorder: results from
30. Anderson CA, Hammen CL: Psychosocial outcomes of children a longitudinal birth cohort. Arch Gen Psychiatry 2002; 59:449–
of unipolar depressed, bipolar, medically ill, and normal 456
women: a longitudinal study. J Consult Clin Psychol 1993; 61: 43. MacCabe JH, Lambe MP, Cnattingius S, Sham PC, David AS,
448–454 Reichenberg A, Murray RM, Hultman CM: Excellent school per-
31. Egeland JA, Shaw JA, Endicott J, Pauls DL, Allen CR, Hostetter AM, formance at age 16 and risk of adult bipolar disorder: national
Sussex JN: Prospective study of prodromal features for bi- cohort study. Br J Psychiatry 2010; 196:109–115
polarity in well Amish children. J Am Acad Child Adolesc Psy- 44. Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR,
chiatry 2003; 42:786–796 Altman SE: Subthreshold conditions as precursors for full
32. Reichart CG, Wals M, Hillegers MH, Ormel J, Nolen WA, Verhulst syndrome disorders: a 15-year longitudinal study of multiple
FC: Psychopathology in the adolescent offspring of bipolar diagnostic classes. J Child Psychol Psychiatry 2009; 50:
parents. J Affect Disord 2004; 78:67–71 1485–1494
33. Duffy A, Alda M, Kutcher S, Fusee C, Grof P: Psychiatric symp- 45. Tijssen MJ, Van Os J, Wittchen HU, Lieb R, Beesdo K, Wichers M:
toms and syndromes among adolescent children of parents Risk factors predicting onset and persistence of subthreshold
with lithium-responsive or lithium-nonresponsive bipolar dis- expression of bipolar psychopathology among youth from the
order. Am J Psychiatry 1998; 155:431–433 community. Acta Psychiatr Scand 2010; 122:255–266
34. Duffy A, Alda M, Kutcher S, Cavazzoni P, Robertson C, Grof E, 46. Tijssen MJ, van Os J, Wittchen HU, Lieb R, Beesdo K, Mengelers
Grof P: A prospective study of the offspring of bipolar parents R, Wichers M: Prediction of transition from common adolescent
responsive and nonresponsive to lithium treatment. J Clin Psy- bipolar experiences to bipolar disorder: 10-year study. Br J
chiatry 2002; 63:1171–1178 Psychiatry 2010; 196:102–108
35. Duffy A, Alda M, Crawford L, Milin R, Grof P: The early mani- 47. Geller B, Tillman R, Bolhofner K, Zimerman B: Child bipolar
festations of bipolar disorder: a longitudinal prospective study I disorder: prospective continuity with adult bipolar I dis-
of the offspring of bipolar parents. Bipolar Disord 2007; 9: order; characteristics of second and third episodes; pre-
828–838 dictors of 8-year outcome. Arch Gen Psychiatry 2008; 65:
36. Duffy A, Alda M, Hajek T, Grof P: Early course of bipolar disorder 1125–1133
in high-risk offspring: prospective study. Br J Psychiatry 2009; 48. Wozniak J, Petty CR, Schreck M, Moses A, Faraone SV, Biederman
195:457–458 J: High level of persistence of pediatric bipolar I disorder from
37. Grof P, Duffy A, Alda M, Hajek T: Lithium response across gen- childhood onto adolescent years: a 4-year prospective longitu-
erations. Acta Psychiatr Scand 2009; 120:378–385 dinal follow-up study. J Psychiatr Res 2011; 45:1273–1282
38. Grof P, Alda M, Grof E, Zvolsky P, Walsh M: Lithium response 49. Leibenluft E: Severe mood dysregulation, irritability, and the
and genetics of affective disorders. J Affect Disord 1994; 32: diagnostic boundaries of bipolar disorder in youths. Am J Psy-
85–95 chiatry 2011; 168:129–142
39. Duffy A, Grof P, Kutcher S, Robertson C, Alda M: Measures of 50. Mannuzza S, Klein RG: Long-term prognosis in attention-deficit/
attention and hyperactivity symptoms in a high-risk sample of hyperactivity disorder. Child Adolesc Psychiatr Clin N Am 2000;
children of bipolar parents. J Affect Disord 2001; 67:159–165 9:711–726
40. Duffy A, Horrocks J, Milin R, Doucette S, Persson G, Grof P: Ad- 51. Langley K, Fowler T, Ford T, Thapar AK, van den Bree M, Harold
olescent substance use disorder during the early stages of bi- G, Owen MJ, O’Donovan MC, Thapar A: Adolescent clinical out-
polar disorder: a prospective high-risk study. J Affect Disord comes for young people with attention-deficit hyperactivity
(Epub ahead of print, Sep 6, 2012) disorder. Br J Psychiatry 2010; 196:235–240
Am J Psychiatry 169:12, December 2012 ajp.psychiatryonline.org 1255
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Adrian Raine - The Neurobiology of PsychopathyDocument13 pagesAdrian Raine - The Neurobiology of PsychopathyFábio Yutani KosekiNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Melatonin Natural Health Products and Supplements Presence of Serotonin and Significant Variability of Melatonin ContentDocument7 pagesMelatonin Natural Health Products and Supplements Presence of Serotonin and Significant Variability of Melatonin ContentFábio Yutani KosekiNo ratings yet
- Adrian Raine - Developmental Aspects of Schizotypy and Suspiciousness A ReviewDocument8 pagesAdrian Raine - Developmental Aspects of Schizotypy and Suspiciousness A ReviewFábio Yutani KosekiNo ratings yet
- Chapter 7. CPTSDDocument10 pagesChapter 7. CPTSDFábio Yutani KosekiNo ratings yet
- Chapter 7. CPTSDDocument10 pagesChapter 7. CPTSDFábio Yutani KosekiNo ratings yet
- Declebck Smits 1999 Zolpidem a Valuable Alternative to Benzodiazepine Hypnotics for Chronic InsomniaDocument1 pageDeclebck Smits 1999 Zolpidem a Valuable Alternative to Benzodiazepine Hypnotics for Chronic InsomniaFábio Yutani KosekiNo ratings yet
- Antisocial Personality Disorder A Current ReviewDocument8 pagesAntisocial Personality Disorder A Current ReviewastrogliaNo ratings yet
- Melatonin Rhythm Abnormalities and Sleep Disorders in The ElderlyDocument9 pagesMelatonin Rhythm Abnormalities and Sleep Disorders in The ElderlyFábio Yutani KosekiNo ratings yet
- Adrian Raine - The Neuromoral Theory of Antisocial, Violent, and Psychopathic BehaviorDocument29 pagesAdrian Raine - The Neuromoral Theory of Antisocial, Violent, and Psychopathic BehaviorFábio Yutani KosekiNo ratings yet
- Adrian Raine A Neurodevelopmental Perspective On Male ViolenceDocument12 pagesAdrian Raine A Neurodevelopmental Perspective On Male ViolenceFábio Yutani KosekiNo ratings yet
- Antisocial Personality As A Neurodevelopmental Disorder: Annual Review of Clinical PsychologyDocument31 pagesAntisocial Personality As A Neurodevelopmental Disorder: Annual Review of Clinical PsychologyRaul Morales VillegasNo ratings yet
- Serotonin Reuptake Inhibitor Treatment of Obsessive-Compulsive Symptoms in Clozapine-Medicated SchizophreniaDocument3 pagesSerotonin Reuptake Inhibitor Treatment of Obsessive-Compulsive Symptoms in Clozapine-Medicated SchizophreniaFábio Yutani KosekiNo ratings yet
- Adrian Raine - NeurocriminologyDocument29 pagesAdrian Raine - NeurocriminologyFábio Yutani KosekiNo ratings yet
- Melatonin Hormone of The NightDocument3 pagesMelatonin Hormone of The NightFábio Yutani KosekiNo ratings yet
- The Use and Misuse of Exogenous Melatonin in The Treatment of Sleep DisordersDocument6 pagesThe Use and Misuse of Exogenous Melatonin in The Treatment of Sleep DisordersFábio Yutani KosekiNo ratings yet
- Serotonin-Based Pharmacotherapy For Acute Neuroleptic-Induced Akathisia A New Approach To An Old Problem - Michael PoyurovskyDocument5 pagesSerotonin-Based Pharmacotherapy For Acute Neuroleptic-Induced Akathisia A New Approach To An Old Problem - Michael PoyurovskyFábio Yutani KosekiNo ratings yet
- Melatonin and Mental IllnessDocument12 pagesMelatonin and Mental IllnessFábio Yutani KosekiNo ratings yet
- A Comparison of Object and Animal HoardingDocument11 pagesA Comparison of Object and Animal HoardingFábio Yutani KosekiNo ratings yet
- Psychiatric Medication-Induced Obesity A Review.Document7 pagesPsychiatric Medication-Induced Obesity A Review.Fábio Yutani KosekiNo ratings yet
- Obsessive Musical Hallucinations in A Schizophrenia Patient Psychopathological and fMRI CharacteristicsDocument4 pagesObsessive Musical Hallucinations in A Schizophrenia Patient Psychopathological and fMRI CharacteristicsFábio Yutani KosekiNo ratings yet
- Melatonin, Aging, and Alzheimer's Disease. Principles and Practice of Geriatric Sleep Medicine, 97-106.Document10 pagesMelatonin, Aging, and Alzheimer's Disease. Principles and Practice of Geriatric Sleep Medicine, 97-106.Fábio Yutani KosekiNo ratings yet
- Clozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewDocument13 pagesClozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewalfredoibcNo ratings yet
- Auld2016 PDFDocument13 pagesAuld2016 PDFJosé Francisco López GilNo ratings yet
- Hoarding Disorder A New Obsessive-Compulsive Related Disorder in DSM-5Document12 pagesHoarding Disorder A New Obsessive-Compulsive Related Disorder in DSM-5Fábio Yutani KosekiNo ratings yet
- Acute Antipsychotic-Induced Akathisia Revisited - Michael PoyurovskyDocument3 pagesAcute Antipsychotic-Induced Akathisia Revisited - Michael PoyurovskyFábio Yutani KosekiNo ratings yet
- Clozapine-Induced Obsessive-Compulsive Symptoms in Schizophrenia A Critical Review Mathias ZinkDocument8 pagesClozapine-Induced Obsessive-Compulsive Symptoms in Schizophrenia A Critical Review Mathias ZinkFábio Yutani KosekiNo ratings yet
- Melatonin: A New Probe in Psychiatric Investigation?: AnnotationDocument6 pagesMelatonin: A New Probe in Psychiatric Investigation?: AnnotationFábio Yutani KosekiNo ratings yet
- Pharmacokinetics of Oral and Intravenous Melatonin in Healthy Volunteers. BMC Pharmacology and ToxicologyDocument5 pagesPharmacokinetics of Oral and Intravenous Melatonin in Healthy Volunteers. BMC Pharmacology and ToxicologyFábio Yutani KosekiNo ratings yet
- Differential Diagnosis of LymphedemaDocument10 pagesDifferential Diagnosis of LymphedemaalfredNo ratings yet