Professional Documents
Culture Documents
Appropriate Use Criteria Headache
Appropriate Use Criteria Headache
Uploaded by
GP RS EMCOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Appropriate Use Criteria Headache
Appropriate Use Criteria Headache
Uploaded by
GP RS EMCCopyright:
Available Formats
Johns Hopkins University School of Medicine
Appropriate Use Criteria
Priority Clinical Area: Headache
Setting: Ambulatory and Emergency Department
INTRODUCTION
The Centers for Medicare and Medicaid Services (CMS) Appropriate Use Criteria (AUC) program takes effect January 2020 and requires ambulatory
and emergency medicine providers to consult AUC using a CMS approved clinical decision support mechanism when ordering advanced imaging
(CT, MRI or nuclear medicine) in eight priority clinical areas (PCAs). Headache is included in the PCAs. The purpose of this project was to evaluate
the highest-grade evidence in the literature pertaining to the utility of computed tomography (CT), magnetic resonance imaging (MRI) and nuclear
medicine scanning for outpatients and emergency department patients with headache, focusing on patient outcomes and costs and in keeping
with high value practice.
LITERATURE REVIEW
Jan. 26, 2019
(“Headache”[mh] OR “headache”[tiab]) AND (“tomography, x-ray computed”[mh] OR “computed tomography”[mh]) OR “computed tomography”
[tiab] OR “magnetic resonance imaging”[mh] OR “magnetic resonance”[tiab] OR “MRI”[tiab] OR “nuclear medicine”[mh]) AND (“clinical study”[Pt]
OR “clinical trial”[Pt] OR “comparative study”[Pt] OR “controlled clinical trial”[Pt] OR “evaluation studies”[Pt] OR “meta analysis”[Pt] OR
“multicenter study”[Pt] OR “observational study”[Pt] OR “practice guideline”[Pt] OR “randomized controlled trial”[Pt] OR “systematic review”[Pt]
OR “validation studies”[Pt]) AND 1990:3000[dp] AND eng[la]
PRISMA
• 747 references imported for screening
o Zero duplicates removed
• 747 studies screened against title and abstract
o 627 studies excluded
• 120 studies assessed for full-text eligibility
o 27 studies excluded
• 93 studies included
o 25 studies identified clinical indicators of pathology (“red flags”)
Published December 2019
Johns Hopkins University School of Medicine
Appropriate Use Criteria
Priority Clinical Area: Headache
Setting: Ambulatory and Emergency Department
Publication type
• Two meta-analyses
• Four systematic reviews
• Three prospective studies
• 13 retrospective studies
• Three clinical practice guidelines
Oxford grade
• Three studies Oxford grade 1
• Six studies Oxford grade 2
• Seven studies Oxford grade 3
• Six studies Oxford grade 4
• Three studies Oxford grade 5
Summary statement: Evidence supports avoidance of immediate advanced imaging at presentation in the absence of neurologic findings or clinical
indicators of serious underlying conditions, which include:
• Subarachnoid or parenchymal hemorrhage
• Infection
• Tumor
• Sinus thrombosis
• Arterial dissection
Published December 2019
Johns Hopkins University School of Medicine
Appropriate Use Criteria
Priority Clinical Area: Headache
Setting: Ambulatory and Emergency Department
APPROPRIATE USE CRITERIA
Clinical scenario 1: Clinical scenario 2: Clinical scenario Clinical scenario Clinical scenario Clinical scenario
Concern for subarachnoid Concern for brain 3: Concern for 4: Concern for 5: Concern for 6: Migraine
hemorrhage/aneurysm or abscess or encephalitis sinus cerebral artery tumor patient
Title
bleed thrombosis dissection
One or more of the One or more of the One or more of One or more of One or more of All of the
following: worst headache following: fever, the following: the following: the following: following:
of life, severe headache, papilledema, altered headaches that acute onset, new headache Migraine patient
sudden onset, emesis, mental status, are acute to severe intensity, especially if >50, with recurrent
altered mental status, meningismus, focal subacute, focal, ipsilateral and papilledema or headaches, no
altered cognition, brought neurologic deficit, new continuous, modified by head other evidence if recent change in
on by cough, sexual headache in moderate to and/or neck elevated pattern, no
Definition activity or exertion immunocompromised severe intensity; positioning intracranial history of
patient accompanied by pressure, focal seizures, no
focal neurologic neurologic focal neurologic
deficits or deficit, altered signs or
seizures; in mental status, symptoms
setting of history of cancer
positive D-dimer including lung
cancer
AUC Rules
Published December 2019
Johns Hopkins University School of Medicine
Appropriate Use Criteria
Priority Clinical Area: Headache
Setting: Ambulatory and Emergency Department
Consistent Brain CT without contrast Brain CT without Brain CT without Brain CT Brain CT without No advanced
with AUC contrast, brain MRI contrast, brain angiogram, brain contrast, brain imaging is
CT venogram, MRI with head MRI consistent with
brain MRI with and neck MR AUC for this
MR venogram angiogram clinical
presentation.
Allowable Brain CT angiogram, brain Brain CT with contrast Brain CT without Brain CT with
by AUC CT venogram, brain MRI, contrast contrast
brain MRI with MR
venogram, Brain MRI with
head and neck MR
angiogram
Published December 2019
Johns Hopkins University School of Medicine
Appropriate Use Criteria
Priority Clinical Area: Headache
Setting: Ambulatory and Emergency Department
Does not Brain CT with contrast, Brain CT angiogram, Brain CT with Brain CT with Brain CT Brain CT without
meet AUC nuclear medicine brain brain CT venogram, contrast, brain contrast, brain angiogram, contrast, brain
positron emission brain MRI with MR CT angiogram, MRI, brain CT brain CT CT with contrast,
tomography (PET)/CT venogram, Brain MRI brain MRI, brain venogram, brain venogram, brain brain CT
with head and neck MR MRI with head MRI with MR MRI with MR angiogram,
angiogram, nuclear and neck MR venogram, venogram, brain brain CT
medicine brain PET/CT angiogram, nuclear medicine MRI with head venogram, brain
nuclear brain PET/CT and neck MR MRI, brain MRI
medicine brain angiogram, with MR
PET/CT nuclear venogram, brain
medicine brain MRI with head
PET/CT and neck MR
angiogram,
nuclear
medicine brain
PET/CT
No AUC
available
Evidentiary Evidentiary for imaging Evidentiary for imaging Evidentiary for Evidentiary for Evidentiary for Evidentiary
vs appropriateness, appropriateness, imaging imaging imaging
Consensus consensus for exam consensus for exam appropriateness, appropriateness, appropriateness,
protocol protocol consensus for consensus for consensus for
exam protocol exam protocol exam protocol
Published December 2019
Johns Hopkins University School of Medicine
Appropriate Use Criteria
Priority Clinical Area: Headache
Setting: Ambulatory and Emergency Department
MULTIDISCIPLINARY TEAM
The Johns Hopkins University School of Medicine requires that all practicing physicians participating in the development of AUC disclose any
conflicts of interest using the International Community of Medical Journal Editors (ICJME) form. This information is publically available in a timely
fashion upon request, for a period of not less than five years after the most recent published update of the relevant appropriate use criteria.
Members of the headache AUC development team are:
Jonathan Hansen Emergency Medicine, Johns Hopkins Bayview Medical Center
Susan Peterson Emergency Medicine, The Johns Hopkins Hospital
Mustapha Saheed Emergency Medicine, The Johns Hopkins Hospital
Steven Blash Family Medicine, Johns Hopkins Community Physicians
Danny Lee Internal Medicine, Johns Hopkins Community Physicians
Howard Levy Internal Medicine, Johns Hopkins Medicine - Green Spring Station
Sachin Gujar Neuroradiology, The Johns Hopkins Hospital
Rohini Nadgir Neuroradiology, The Johns Hopkins Hospital
Elisabeth Marsh Neurology, The Johns Hopkins Hospital
John Probasco Neurology, The Johns Hopkins Hospital
Nauman Tariq Neurology, Johns Hopkins Bayview Medical Center
Pamela Johnson Radiology, The Johns Hopkins Hospital
Disclosure: AUC developers may receive future royalties from licensure of AUCs to CMS-approved clinical decision support mechanisms.
Published December 2019
You might also like
- Life-Span Human DevelopmentDocument659 pagesLife-Span Human DevelopmentMimaansa gargNo ratings yet
- MKSAP 16 - NeurologyDocument333 pagesMKSAP 16 - NeurologyBacanator100% (4)
- Anatomy StudyDocument124 pagesAnatomy StudyPragya ShrivastavaNo ratings yet
- Lecture 2 HvacDocument38 pagesLecture 2 HvacJohn BennettNo ratings yet
- EFE Gyratory CrusherDocument152 pagesEFE Gyratory CrusherVladimir Sepulveda100% (2)
- Jetting Assist Pile DrivingDocument12 pagesJetting Assist Pile DrivingKenginNo ratings yet
- Introduction To NeuroimagingDocument11 pagesIntroduction To NeuroimagingJojo LastNo ratings yet
- What You Must Know About Neurological Disorders: By: Chulou H. Penales, R.N., M.A.NDocument81 pagesWhat You Must Know About Neurological Disorders: By: Chulou H. Penales, R.N., M.A.Nlisette_sakura100% (1)
- Lecture HeadacheDocument54 pagesLecture HeadachesaharuiNo ratings yet
- Part 3 - Manufacture Flow PDFDocument60 pagesPart 3 - Manufacture Flow PDFmohsengsmNo ratings yet
- Homemade Liposomal CDocument8 pagesHomemade Liposomal CDennis LipterNo ratings yet
- Headache Case Seminar - RCPTDocument25 pagesHeadache Case Seminar - RCPTSurat TanprawateNo ratings yet
- Well Completion and Stimulation - Chapter 3 Well Performance Analysis-NewDocument56 pagesWell Completion and Stimulation - Chapter 3 Well Performance Analysis-NewsouthliNo ratings yet
- L4 Introduction To Travel Tourism and Hospitality Dec11Document7 pagesL4 Introduction To Travel Tourism and Hospitality Dec11As HerlambangNo ratings yet
- Edema ParuDocument42 pagesEdema ParuGP RS EMCNo ratings yet
- (Anglais) Breuss-Cancer-Cure PDFDocument7 pages(Anglais) Breuss-Cancer-Cure PDFPythagore De SamosNo ratings yet
- Approach To HeadacheDocument61 pagesApproach To Headachesabahat.husainNo ratings yet
- Nye 2015Document8 pagesNye 2015Mayra SantanderNo ratings yet
- Indications and Imaging Modality of Choice in Pediatric Headache 2019Document19 pagesIndications and Imaging Modality of Choice in Pediatric Headache 2019Luis GomezNo ratings yet
- Headache and Facial Pain: Key PointsDocument5 pagesHeadache and Facial Pain: Key PointsCaesar Muhammad WijayaNo ratings yet
- Journal ReadingDocument53 pagesJournal ReadingRhadezahara PatrisaNo ratings yet
- Acute Ischemic StrokeDocument9 pagesAcute Ischemic Strokepuskesmas tarikNo ratings yet
- Management OF Head Injury: DR Echebiri, PDocument26 pagesManagement OF Head Injury: DR Echebiri, PLuther ThengNo ratings yet
- Headaches: Jonathan Rochlin, MD January 9, 2008Document62 pagesHeadaches: Jonathan Rochlin, MD January 9, 2008saheefaNo ratings yet
- Lance Neuro PTHDocument10 pagesLance Neuro PTHRenju KuriakoseNo ratings yet
- When Should Brain Imaging Precede Lumbar Puncture in Cases of Suspected Bacterial MeningitisDocument3 pagesWhen Should Brain Imaging Precede Lumbar Puncture in Cases of Suspected Bacterial Meningitistsiko111No ratings yet
- Practice: A 32-Year-Old Woman With HeadacheDocument2 pagesPractice: A 32-Year-Old Woman With HeadacheFeliNo ratings yet
- From First Symptoms To Diagnosis: Initial Clinical Presentation of Primary Brain TumorsDocument7 pagesFrom First Symptoms To Diagnosis: Initial Clinical Presentation of Primary Brain TumorsMohammad AamirNo ratings yet
- Jamaneurology Topcuoglu 2017 Oi 170047Document8 pagesJamaneurology Topcuoglu 2017 Oi 170047LadycherryNo ratings yet
- Continuous Determination of Optimal Cerebral Perfusion Pressure in Traumatic Brain InjuryDocument8 pagesContinuous Determination of Optimal Cerebral Perfusion Pressure in Traumatic Brain InjurydrdivyapukNo ratings yet
- Invasive Neuromonitoring TechniqueDocument20 pagesInvasive Neuromonitoring TechniqueReza ManefoNo ratings yet
- Ni Hms 707191Document12 pagesNi Hms 707191Denny LukasNo ratings yet
- Neuroimaging of Normal Pressure HydrocephalusDocument29 pagesNeuroimaging of Normal Pressure HydrocephalusApostolos T.No ratings yet
- Diagnose VertigoDocument10 pagesDiagnose VertigoDiayanti TentiNo ratings yet
- Cost and Utility in The Diagnostic Evaluation Of.20Document5 pagesCost and Utility in The Diagnostic Evaluation Of.20mhd.mamdohNo ratings yet
- HSA Controversias 2016Document9 pagesHSA Controversias 2016Ellys Macías PeraltaNo ratings yet
- Infantile Idiopathic Intracranial Hypertension: A Case Study and Review of The LiteratureDocument9 pagesInfantile Idiopathic Intracranial Hypertension: A Case Study and Review of The LiteratureAidee Paola Villca MamaniNo ratings yet
- Bai 2015Document13 pagesBai 2015f7jtbtdqnyNo ratings yet
- Pic CefaleaDocument26 pagesPic CefaleaAdelaida Gaitán KühneNo ratings yet
- CA NasopharyngealDocument6 pagesCA NasopharyngealalmiraerickaiNo ratings yet
- NeuroEmergencies 2020 - Web - EB PDFDocument7 pagesNeuroEmergencies 2020 - Web - EB PDFJimmy AlexanderNo ratings yet
- Community-Acquired Bacterial Meningitis in Adults: Review ArticleDocument10 pagesCommunity-Acquired Bacterial Meningitis in Adults: Review ArticleÁlvaro NBNo ratings yet
- EMRC Headache Slides 2upDocument33 pagesEMRC Headache Slides 2upMohammed AlrashedNo ratings yet
- Nervous System AlterationsDocument45 pagesNervous System AlterationsMajesty ParkerNo ratings yet
- The Natural History of Epilepsy: An Epidemiological View: ReviewDocument6 pagesThe Natural History of Epilepsy: An Epidemiological View: ReviewDiana LeonNo ratings yet
- ENLS Sub-Arachnoid Hemorrhage ProtocolDocument22 pagesENLS Sub-Arachnoid Hemorrhage ProtocolFransiskus MikaelNo ratings yet
- Subarachnoid HemorrhageDocument54 pagesSubarachnoid HemorrhagesarahmacielNo ratings yet
- Screening Head Neck ShoulderDocument14 pagesScreening Head Neck ShoulderVinay KumarNo ratings yet
- PDPH MeruDocument6 pagesPDPH MeruTeshome AssefaNo ratings yet
- RCP y PH ArterialDocument2 pagesRCP y PH ArterialPaola LizarzabalNo ratings yet
- Zelin Sun MD, PH.D: Department of Neurosurgery Affiliated Hospital North China University of Science and TechnologyDocument53 pagesZelin Sun MD, PH.D: Department of Neurosurgery Affiliated Hospital North China University of Science and TechnologyMargaret ThatcherNo ratings yet
- .Archivetempmanejo de Cefalea No Traumatica de Inicio Rapido Severo 16 PDFDocument9 pages.Archivetempmanejo de Cefalea No Traumatica de Inicio Rapido Severo 16 PDFM Victoria SalazarNo ratings yet
- A Contemporary Perspective On The Management of Post-Craniotomy Headache and PainDocument7 pagesA Contemporary Perspective On The Management of Post-Craniotomy Headache and PainTika HandayaniNo ratings yet
- Enlsv3.0 Sah FinalDocument8 pagesEnlsv3.0 Sah FinalRatu SetiawanNo ratings yet
- Medical Management of StrokeDocument6 pagesMedical Management of StrokemehakNo ratings yet
- Encefalite Autoimune Soronegativa - June 2023Document12 pagesEncefalite Autoimune Soronegativa - June 2023FernandoNo ratings yet
- Initial Diagnosis and Management of Acutely Elevated Intracranial PressureDocument8 pagesInitial Diagnosis and Management of Acutely Elevated Intracranial PressureGlessin MurilloNo ratings yet
- Lecture. Physiotherapists. TumoursDocument34 pagesLecture. Physiotherapists. TumoursdivinaNo ratings yet
- Journal Reading FithryDocument20 pagesJournal Reading FithryFithry RahmaNo ratings yet
- Brain SPECT Imaging in Complex Psychiatric Cases: An Evidence-Based, Underutilized ToolDocument9 pagesBrain SPECT Imaging in Complex Psychiatric Cases: An Evidence-Based, Underutilized ToolMariaNo ratings yet
- Clinics 5Document19 pagesClinics 5Renju KuriakoseNo ratings yet
- Diagnostic CriteriaDocument12 pagesDiagnostic CriteriaBenjamin NgNo ratings yet
- Pineal Germ Cell Tumors ReviewDocument6 pagesPineal Germ Cell Tumors ReviewWinda HaeriyokoNo ratings yet
- Stroke Simpo Perawat Dan AkupunturDocument54 pagesStroke Simpo Perawat Dan Akupunturaisyah nadhiraNo ratings yet
- Thunderclap Headache: Anne Ducros, Marie-Germaine BousserDocument4 pagesThunderclap Headache: Anne Ducros, Marie-Germaine BousserLeidy Carolina Salazar ChicaNo ratings yet
- Brain Injury After Cardiac Arrest - From Prognostication of Comatose Patients To RehabilitationDocument12 pagesBrain Injury After Cardiac Arrest - From Prognostication of Comatose Patients To RehabilitationHabib G. Moutran BarrosoNo ratings yet
- InvestigationsDocument28 pagesInvestigationsAndrei BulgariuNo ratings yet
- Kwon World Neurosurgery 2016Document4 pagesKwon World Neurosurgery 2016Churl-Su KwonNo ratings yet
- Trauma: HX and PE (Adults) : For The EMS Providers, (Prior To Patient'sDocument3 pagesTrauma: HX and PE (Adults) : For The EMS Providers, (Prior To Patient'sJustine CastilloNo ratings yet
- Hemorragia Intracraneal EspontaneaDocument7 pagesHemorragia Intracraneal Espontaneajosue leonardo RuizNo ratings yet
- Cerebral Herniation Syndromes and Intracranial HypertensionFrom EverandCerebral Herniation Syndromes and Intracranial HypertensionMatthew KoenigNo ratings yet
- Ebn AnakDocument22 pagesEbn AnakGP RS EMCNo ratings yet
- Intestinal, Intestinal-Type and Intestine-Localized Metastatic Adenocarcinoma. Immunohistochemical Approach To The Differential DiagnosisDocument16 pagesIntestinal, Intestinal-Type and Intestine-Localized Metastatic Adenocarcinoma. Immunohistochemical Approach To The Differential DiagnosisGP RS EMCNo ratings yet
- PIIS0016508522003900 AGA IBS Constipation2022Document19 pagesPIIS0016508522003900 AGA IBS Constipation2022GP RS EMCNo ratings yet
- Unstable Chest Pain Evidence TableDocument2 pagesUnstable Chest Pain Evidence TableGP RS EMCNo ratings yet
- Family Health Assessment FormDocument7 pagesFamily Health Assessment FormBiway RegalaNo ratings yet
- CFD Analysis of MR FluidDocument7 pagesCFD Analysis of MR FluidVishnuPrasadNo ratings yet
- R1600G Circuit Breaker HarnessDocument5 pagesR1600G Circuit Breaker Harnesstr eoNo ratings yet
- Msds Prestone BeltDocument6 pagesMsds Prestone BeltrizalramNo ratings yet
- Dairy IndustryDocument11 pagesDairy IndustryAbhishek SharmaNo ratings yet
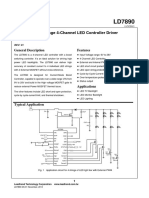
- LD7890 LeadtrendDocument16 pagesLD7890 LeadtrendO6U Pharmacy RecordingsNo ratings yet
- Mount Kilimanjaro (4) : Climbing HistoryDocument3 pagesMount Kilimanjaro (4) : Climbing HistorybrianlaksonoNo ratings yet
- SL020 PDFDocument3 pagesSL020 PDFchidambaram kasiNo ratings yet
- Battle of Tannenberg LineDocument10 pagesBattle of Tannenberg LineblurbNo ratings yet
- Kiribati National Tourism Action PlanDocument35 pagesKiribati National Tourism Action PlanRafeed AlshameryNo ratings yet
- TGADocument71 pagesTGAUma Villashini Gunasekaran100% (1)
- Laplace Transform Part 1Document5 pagesLaplace Transform Part 1Pavirlene Escaño NorteNo ratings yet
- Sufferfest Comparison Chart NEWDocument3 pagesSufferfest Comparison Chart NEWyusuf ravatNo ratings yet
- Standard Buccaneer - USBDocument6 pagesStandard Buccaneer - USBdilnair99No ratings yet
- Evaluation of Loss Coefficient For Stand Alone Radiator: G.Pillutla, R. Mishra, S.M.Barrans J.BarransDocument5 pagesEvaluation of Loss Coefficient For Stand Alone Radiator: G.Pillutla, R. Mishra, S.M.Barrans J.BarransbatazivoNo ratings yet
- Hi-Tech Projects: (An Industrial Monthly Magazine On New Project Opportunities and Industrial Technologies)Document17 pagesHi-Tech Projects: (An Industrial Monthly Magazine On New Project Opportunities and Industrial Technologies)Shridhar L MallapurNo ratings yet
- Australia and India Expert - Coal HandlingDocument13 pagesAustralia and India Expert - Coal HandlingachniajosiNo ratings yet
- Annualreport2010-11 2Document128 pagesAnnualreport2010-11 2Gaurav MunoliNo ratings yet
- IG3 Chapter 2Document39 pagesIG3 Chapter 2Dishita AgrawalNo ratings yet
- Allergy - 2021 - Muraro - EAACI Guidelines Anaphylaxis 2021 UpdateDocument21 pagesAllergy - 2021 - Muraro - EAACI Guidelines Anaphylaxis 2021 UpdateIndah KaDeNo ratings yet