Professional Documents
Culture Documents
Active Management of 3RD Stage of Labor
Uploaded by
Farheen khan0 ratings0% found this document useful (0 votes)
283 views7 pagesActive management of the third stage of labor involves 4 components: 1) administration of oxytocin after birth, 2) delayed cord clamping for 1-3 minutes, 3) controlled cord traction to deliver the placenta, and 4) intermittent uterine tone assessment. Oxytocin is the recommended uterotonic drug to prevent postpartum hemorrhage. Delayed cord clamping provides the newborn with extra blood and iron. A study in Tanzania found that competency-based training and quality improvement interventions significantly improved adherence to active management guidelines and reduced postpartum hemorrhage, especially at lower-level facilities. Ensuring health workers receive regular training is important for improving maternal outcomes.
Original Description:
Original Title
ACTIVE MANAGEMENT OF 3RD STAGE OF LABOR
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentActive management of the third stage of labor involves 4 components: 1) administration of oxytocin after birth, 2) delayed cord clamping for 1-3 minutes, 3) controlled cord traction to deliver the placenta, and 4) intermittent uterine tone assessment. Oxytocin is the recommended uterotonic drug to prevent postpartum hemorrhage. Delayed cord clamping provides the newborn with extra blood and iron. A study in Tanzania found that competency-based training and quality improvement interventions significantly improved adherence to active management guidelines and reduced postpartum hemorrhage, especially at lower-level facilities. Ensuring health workers receive regular training is important for improving maternal outcomes.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
283 views7 pagesActive Management of 3RD Stage of Labor
Uploaded by
Farheen khanActive management of the third stage of labor involves 4 components: 1) administration of oxytocin after birth, 2) delayed cord clamping for 1-3 minutes, 3) controlled cord traction to deliver the placenta, and 4) intermittent uterine tone assessment. Oxytocin is the recommended uterotonic drug to prevent postpartum hemorrhage. Delayed cord clamping provides the newborn with extra blood and iron. A study in Tanzania found that competency-based training and quality improvement interventions significantly improved adherence to active management guidelines and reduced postpartum hemorrhage, especially at lower-level facilities. Ensuring health workers receive regular training is important for improving maternal outcomes.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
ACTIVE MANAGEMENT OF 3RD STAGE OF LABOR
COMPONENTS OF ACTIVE MANAGEMENT OF THIRD STAGE
OF LABOR
1. Use of oxytocic after the birth of baby
2. Delayed cord clamping (≥1-3 minutes)
3. Delivery of placenta by controlled cord traction
4. Intermittent uterine tone assessment ( note: uterine massage is no
longer a part of AMTSL as per the latest guidelines of WHO)
DETAILS OF EACH COMPONENT OF AMTSL
Step 1: Use of Oxytocics
OXYTOCIN: it is the preferred drug and the drug recommended by
WHO for preventing PPH
Dose=10 units IM or IV infusion
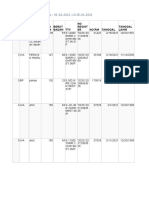
Route Onset of action Duration of action
IM bolus Within 3 mins 3 hours
IV infusion immediate 1 hour
Note: Oxytocin should not be given as IV bolus due to risk of marked
transient fall in BP , abrupt increase in cardiac output, myocardial
ischemia and chest pain.
-oxytocin is synthesized in the paraventucular nucleus of hypothalamus
-it is nonapeptide
-synthetic oxytocin is octapeptide
-half life= 3-4 minutes
-oxytocin loses its effectiveness unless it is stored at 2*-8*C
-at room temperature its shelf life is 3 months
-it is the hormone responsible for milk ejection
-it increases uterine contraction physiologically and law of polarity is
maintained hence it is used for inducing labor and augmenting labor also
If Oxytocin is not available then WHO recommends use of oxytocics
like:
1. Ergometrine (0.25 mg) or Methylergometrine (0.2 mg): They bring
about titanic contraction, hence should not be used for inducing or
augumenting labor. It should not be used during pregnancy.
Side Effect: Transient increase in BP
Contraindication: Conditions in which
ergomatrine/methylergometrine is absolutely contraindicated
(however,active management with oxytocin can be done in all
cases)
TOPER
T: Twin pregnancy
O: Organic heart disease
P: Preeclampsia
E: Eclampsia
R: Rh negative female
2. Inj PGF-2a (Carboprost):Dose 250 mcg IM. It is contraindicated in
bronchial asthma patients. It acts mainly on myometrium of uterus
hence used in AMTSL and in PPH but not in inducing labor.
3. PGE1- misoprostol: available as tablet. WHO recommends use of
600 mcg orally for preventing PPH, i.e, during active management
of third stage of labor. PGE1 can act on both cervix and uterus and
hence is used for:
a) Ripening of cervix (25-50 mcg every 3-6 hours orally or
vaginally)
b) Inducing labor
c) AMTSL
d) For treating PPH
Side effects: Nausea, vomiting , abdominal pain , shivering or
hyperpyrexia , hypotension. It is contraindicated in previous
cesarean patients.
4. Syntometrine: it is 5 units of oxytocin and 0.5 mg methergine. It is
expensive.
5. Carbetocin: dose 100mcg IV over 1 minute for AMTSL, i.e, for
preventing PPH. It is and analogue of oxytocin and has action
similar to oxytocin. Its advantage is, it has longer half life=85-100
minutes.
6. Tranexamic acid: it is an antifibrinolytic drug which has been
approved by WHO for treating and preventing PPH.
STEP 2: Delayed cord clamping
-delayed cord clamping means clamping the cord between 1-3
minutes of birth
-early cord clamping means clamping the cord before 1 minute
Advantage of delayed cord clamping
80ml of blood (i.e, 50 mg of elemental iron) present in the cord goes
to the newborn and helps in preventing neonatal anemia.
Thus in all cases except the ones listed below- delayed cord clamping
is advised.
Conditions in which early cord clamping is done:
-baby is hypoxic and needs resuscitation or mother is
hemodynamically unstable.
-known heart disease in baby.
-if cord is avulsed or IUDR with abnormal cord Doppler evaluation
Note: earlier in preterm babies, HIV-positive mothers, and Rh
negative females early cord clamping is done in them also.
STEP 3: Delivery of placenta by controlled cord traction (Modified
Brandt-Andrews Technique)
Here with one hand uterus is pushed upwards and backwards and with
other hand traction is given to cord in downward and forward direction
in a steady and slow manner, until complete expulsion of the placenta
occurs.
Note:
-if the placenta is undelivered after 30 minutes, it is called ‘Retained
Placenta’.
-controlled cord traction is only recommended by WHO if skilled birth
attendant is available, otherwise not.
STEP 4: Intermittent uterine tone assessment
-after delivery for early identification of uterine atony, tone assessment
is recommended for all births (uterine massage is now not a component
of AMTSL)
REMEMBER: most important component of AMTSL is the use of
oxytocic.
WHO Recommendations for Active Management of the Third Stage
of Labour (AMTSL), 2012
The use of uterotonics for the prevention of postpartum haemorrhage
(PPH) during the third stage of labour is recommended for all births.
Oxytocin (10 IU, IV/IM) is the recommended uterotonic drug for the
prevention of PPH.
In settings where skilled birth attendants are available, controlled cord
traction (CCT) is recommended for vaginal births if the care provider
and the parturient woman regard a small reduction in blood loss and a
small reduction in the duration of the third stage of labour as important.
In settings where skilled birth attendants are unavailable, CCT is not
recommended.
Sustained uterine massage is not recommended as an intervention to
prevent PPH in women who have received prophylactic oxytocin.
Postpartum abdominal uterine tonus assessment for early identification
of uterine atony is recommended for all women.
CCT is the recommended method for removal of the placenta in
caesarean section.
Improvement in the active management of the third stage of
labor for the prevention of postpartum hemorrhage in
Tanzania: a cross-sectional study.
PLACE: Tanzania
AUTHOR: Dunstan R. Bishanga, John Charles, Gaudiosa Tibaijuka,
Rita Mutayoba, Mary Drake, Young-Mi Kim, Marya Plotkin, Neema
Rusibamayila & Barbara Rawlins
YEAR: 2018
PUBLICATION: BMC Pregnancy and Childbirth volume 18, Article
number: 223 (2018)
Conclusion
The quality of PPH prevention increased substantially in
facilities that implemented competency-based training and
quality improvement interventions, with the most dramatic
improvement seen at lower-level facilities. As Tanzania
continues with efforts to increase facility births, it is imperative
that the quality of care also be improved by promoting use of
up-to-date guidelines and ensuring regular training and
mentoring for health care providers so that they adhere to the
guidelines for care of women during labor. These measures can
reduce maternal and newborn mortality.
You might also like
- Uterine Malformations PDFDocument6 pagesUterine Malformations PDFsaritha OrugantiNo ratings yet
- Forceps DeliveryDocument7 pagesForceps DeliveryJemin KimNo ratings yet
- (11-13) Assess The Knowledge On Minor Ailments of Pregnancy-FormatDocument3 pages(11-13) Assess The Knowledge On Minor Ailments of Pregnancy-FormatMudasir Ahmad BhatNo ratings yet
- 2 Reproductive Tract InfectionsDocument14 pages2 Reproductive Tract InfectionsawalsherNo ratings yet
- Gestational Trophoblastic DiseaseDocument5 pagesGestational Trophoblastic DiseaseWarshak NathNo ratings yet
- Phototherapy On The Postnatal WardDocument5 pagesPhototherapy On The Postnatal WardYwagar Ywagar100% (1)
- MANAGEMENT OF HYDRAMNIOS AND OLIGOHYDRAMNIOSDocument12 pagesMANAGEMENT OF HYDRAMNIOS AND OLIGOHYDRAMNIOSEaster Soma HageNo ratings yet
- Managing Placenta Previa: A Case StudyDocument38 pagesManaging Placenta Previa: A Case StudyJasmin SabnaNo ratings yet
- Abnormal Uterine ActionDocument36 pagesAbnormal Uterine ActionMed PoxNo ratings yet
- Vaginal ExaminationDocument2 pagesVaginal ExaminationRhobin Petate67% (3)
- Procedures ObgDocument12 pagesProcedures Obgraghuram reddyNo ratings yet
- MATERNAL MORBIDITY, MORTALITY AND FERTILITY RATESDocument18 pagesMATERNAL MORBIDITY, MORTALITY AND FERTILITY RATESmadhu.BNo ratings yet
- Abruption PacentaDocument6 pagesAbruption PacentaKondapavuluru JyothiNo ratings yet
- Govt College of Nursig Mbs Hospital, Kota: A Case Study On EclampsiaDocument21 pagesGovt College of Nursig Mbs Hospital, Kota: A Case Study On EclampsiaShalabh JoharyNo ratings yet
- Uterovaginal ProlapseDocument16 pagesUterovaginal Prolapseapi-3705046100% (1)
- Rating Scale For The Gynecologic ExamDocument3 pagesRating Scale For The Gynecologic ExamAnonymous qJM3kLDtNo ratings yet
- RH IncompatibilityDocument35 pagesRH Incompatibilityaparna100% (1)
- Ectopic Pregnancy: DR .Urmila KarkiDocument27 pagesEctopic Pregnancy: DR .Urmila KarkiBasudev chNo ratings yet
- Managing Pelvic Inflammatory DiseaseDocument9 pagesManaging Pelvic Inflammatory DiseaseanweshaNo ratings yet
- Abdominal Palpation & Examination in Pregnancy 5.0 PDFDocument11 pagesAbdominal Palpation & Examination in Pregnancy 5.0 PDFPalaniswami Palaniswami100% (1)
- The Third StageDocument7 pagesThe Third Stagebalaramani6890No ratings yet
- On Fetal MeasureDocument40 pagesOn Fetal MeasureHarish Labana100% (2)
- SEMINAR ON Antepartum HaemorrageDocument18 pagesSEMINAR ON Antepartum Haemorragekathyayani arraNo ratings yet
- Genital Tract InjuriesDocument37 pagesGenital Tract InjuriesShady Abdelbari83% (6)
- Genital Tract InjuriesDocument24 pagesGenital Tract InjuriesManisha ThakurNo ratings yet
- Disease Condition:: Hyperemsis Gravidarum: DefinitionDocument4 pagesDisease Condition:: Hyperemsis Gravidarum: DefinitionPriyanka JohnNo ratings yet
- SEMINAR ON TUMOUR COMPLICATING PREGNANCYDocument22 pagesSEMINAR ON TUMOUR COMPLICATING PREGNANCYMonika shankarNo ratings yet
- Abnormal Uterin ActionDocument65 pagesAbnormal Uterin Actionshweta raiNo ratings yet
- Causes and Management of APHDocument42 pagesCauses and Management of APHReena TyagiNo ratings yet
- PuerperiumDocument12 pagesPuerperiumWesam Al-TawilNo ratings yet
- Report of PPHDocument58 pagesReport of PPHNishaThakuriNo ratings yet
- Diagnosis of PregnancyDocument26 pagesDiagnosis of PregnancyRamona GaluNo ratings yet
- Postpartum Hemorrhage (PPH) ManagementDocument38 pagesPostpartum Hemorrhage (PPH) ManagementPrakash ThakullaNo ratings yet
- Menopause Effects and ManagementDocument51 pagesMenopause Effects and ManagementKelvin SuNo ratings yet
- Kangroo Mother Care PDFDocument25 pagesKangroo Mother Care PDFMission Neet-PgNo ratings yet
- Genital ProlapseDocument36 pagesGenital Prolapsemaya100% (1)
- DysmenorrheaDocument28 pagesDysmenorrheaDr Munira MalikNo ratings yet
- Prolonged Labor and Labor InductionDocument28 pagesProlonged Labor and Labor InductionNovia RizqiNo ratings yet
- High Risk Antenatal AssessmentDocument15 pagesHigh Risk Antenatal AssessmentAbishaNo ratings yet
- Seminar MiesDocument16 pagesSeminar Mieshannahashok0% (1)
- DrugDocument11 pagesDrugrihamNo ratings yet
- Postnatal Assessment Tool M.SC NSGDocument12 pagesPostnatal Assessment Tool M.SC NSGM. jehovah Nissie YeshalomeNo ratings yet
- Legislations Clinical Rights and Professional ResponsibilityDocument10 pagesLegislations Clinical Rights and Professional ResponsibilityFarheen khanNo ratings yet
- Drugs Used in Pregnancy, Labour and Puerperium: Presented By:-Ms Lisa Chadha F.Y. MSC Nursing Bvcon, PuneDocument87 pagesDrugs Used in Pregnancy, Labour and Puerperium: Presented By:-Ms Lisa Chadha F.Y. MSC Nursing Bvcon, PuneSanjay Kumar SanjuNo ratings yet
- Augmentation and IOLDocument22 pagesAugmentation and IOLvani reddyNo ratings yet
- Cyctocyle - Care PlanDocument22 pagesCyctocyle - Care Planarchana vermaNo ratings yet
- Seminar On Minor DisorderDocument23 pagesSeminar On Minor Disorderpriti pallabi100% (1)
- Effects of Maternal Drugs On The FetusDocument9 pagesEffects of Maternal Drugs On The FetusJennifer DixonNo ratings yet
- HysterectomyDocument2 pagesHysterectomyJellou MacNo ratings yet
- Normal DeliveryDocument41 pagesNormal DeliveryAliNo ratings yet
- OBG Picture Based Discussion 01Document48 pagesOBG Picture Based Discussion 01Dheeraj Nandal0% (1)
- Assessment of Fetal Well-BeingDocument63 pagesAssessment of Fetal Well-BeingArhum Siddiqi100% (1)
- Obg QuestionsDocument3 pagesObg QuestionsRenuka JamwalNo ratings yet
- Ante Partum HemorrhageDocument30 pagesAnte Partum Hemorrhagetanmai nooluNo ratings yet
- Manual Removal of Retained Placenta GuideDocument25 pagesManual Removal of Retained Placenta GuideLoorthu Selvi M0% (1)
- Seminar On AphDocument46 pagesSeminar On AphKaruna KumariNo ratings yet
- Examination of Placenta for AbnormalitiesDocument3 pagesExamination of Placenta for AbnormalitiesPriyanka SheoranNo ratings yet
- Role of Dietary Fibers and Nutraceuticals in Preventing DiseasesFrom EverandRole of Dietary Fibers and Nutraceuticals in Preventing DiseasesRating: 5 out of 5 stars5/5 (1)
- 4th Year - Unit 5 - Pharmacotherapeutics in Obstetrics 1Document13 pages4th Year - Unit 5 - Pharmacotherapeutics in Obstetrics 1Rupa Ghosh100% (1)
- Induction and AugmentationDocument23 pagesInduction and AugmentationMerry ZewduNo ratings yet
- All India Institute of Medical Sciences, Jodhpur College of NursingDocument17 pagesAll India Institute of Medical Sciences, Jodhpur College of NursingFarheen khanNo ratings yet
- Oxytocics and TocolyticsDocument6 pagesOxytocics and TocolyticsFarheen khanNo ratings yet
- All India Institute of Medical Sciences Jodhpur College of Nursing Practice Teaching ONDocument12 pagesAll India Institute of Medical Sciences Jodhpur College of Nursing Practice Teaching ONFarheen khanNo ratings yet
- Role and Scope of Independent Nurse Midwifery PractitionerDocument14 pagesRole and Scope of Independent Nurse Midwifery PractitionerFarheen khanNo ratings yet
- Genetic Counselling and Prenatal ScreeningDocument8 pagesGenetic Counselling and Prenatal ScreeningFarheen khanNo ratings yet
- Lesson Plan On ResuscitationDocument17 pagesLesson Plan On ResuscitationFarheen khanNo ratings yet
- First Stage of Labor ManagementDocument6 pagesFirst Stage of Labor ManagementFarheen khanNo ratings yet
- All India Institute of Medical Sciences, Jodhpur College of Nursing Lesson Plan ON TopicDocument12 pagesAll India Institute of Medical Sciences, Jodhpur College of Nursing Lesson Plan ON TopicFarheen khanNo ratings yet
- MIDWIFERYDocument14 pagesMIDWIFERYFarheen khanNo ratings yet
- AIIMS Jodhpur Nursing Student's Paper on Recent Advancements in Infertility ManagementDocument18 pagesAIIMS Jodhpur Nursing Student's Paper on Recent Advancements in Infertility ManagementFarheen khan100% (2)
- Various Childbirth PracticesDocument11 pagesVarious Childbirth PracticesFarheen khan100% (1)
- Legislations Clinical Rights and Professional ResponsibilityDocument10 pagesLegislations Clinical Rights and Professional ResponsibilityFarheen khanNo ratings yet
- Psychological and Social Aspect of MenopauseDocument16 pagesPsychological and Social Aspect of MenopauseFarheen khanNo ratings yet
- Drugs Used in Pregnancy and LaborDocument20 pagesDrugs Used in Pregnancy and LaborFarheen khan100% (1)
- Fenton Preterm Growth Chart - Girls: Lengh TDocument1 pageFenton Preterm Growth Chart - Girls: Lengh Tsripertiwi andryNo ratings yet
- Skilled Birth Attendance HandbookDocument69 pagesSkilled Birth Attendance HandbookKripa Susan100% (2)
- EINCDocument1 pageEINCRaidis PangilinanNo ratings yet
- FINAL-NSD - Case - GROUP-B 2Document53 pagesFINAL-NSD - Case - GROUP-B 2Sharlaine CabanayanNo ratings yet
- OBGYN MCQ GuideDocument37 pagesOBGYN MCQ GuideReving Sagvan50% (2)
- PartographDocument4 pagesPartographElonah Gien DimalaluanNo ratings yet
- Laporan Kunjungan Pustu KlampokDocument61 pagesLaporan Kunjungan Pustu Klampokranggie nindya slamanthaNo ratings yet
- Rajiv Gandhi University of Health Sciences Karnataka, BangaloreDocument22 pagesRajiv Gandhi University of Health Sciences Karnataka, BangaloreSadam HussienNo ratings yet
- 2 Antepartum Haemorrhage: Hannah Yeeles and Swati JhaDocument14 pages2 Antepartum Haemorrhage: Hannah Yeeles and Swati JhadeweNo ratings yet
- Delivery Room - LectureDocument3 pagesDelivery Room - Lectureboxed juiceNo ratings yet
- Dian Anggraini's English Coursework on Medical Tenses and ProceduresDocument8 pagesDian Anggraini's English Coursework on Medical Tenses and ProceduresYohanispendriantoNo ratings yet
- Maternal Anemia As A Risk Factor For Preterm Delivery and Low Birth WeightDocument2 pagesMaternal Anemia As A Risk Factor For Preterm Delivery and Low Birth WeightCarla LagNo ratings yet
- Labor and Delivery Nursing QuestionsDocument8 pagesLabor and Delivery Nursing QuestionsKryzza LeizellNo ratings yet
- Baby shower taboo game cards for expecting parentsDocument5 pagesBaby shower taboo game cards for expecting parentsclealcNo ratings yet
- Koding RS Sansani (Rs Tipe C) OBGYN: No ICD 10 Icd 9 CM KodingDocument4 pagesKoding RS Sansani (Rs Tipe C) OBGYN: No ICD 10 Icd 9 CM Kodingcasemix sansaniNo ratings yet
- Anaesthetic Management of Obstetric: HaemorrhageDocument52 pagesAnaesthetic Management of Obstetric: Haemorrhagerevathidadam55555No ratings yet
- Notes On LaborDocument4 pagesNotes On Laboraijiel talisikNo ratings yet
- Cowden, M. (2016), Children's RightsDocument62 pagesCowden, M. (2016), Children's Rightsivan.ramone1No ratings yet
- Cephalopelvic DisproportionDocument3 pagesCephalopelvic DisproportionAira MiyaNo ratings yet
- EINCDocument14 pagesEINCShiela VillarejoNo ratings yet
- EGOPD 24 Hour Duty Report SummaryDocument8 pagesEGOPD 24 Hour Duty Report SummaryDaniel ShushayNo ratings yet
- Aida Ayu Mailinda SariDocument11 pagesAida Ayu Mailinda SariMay El-MardhatillahNo ratings yet
- Helping a Young Single MotherDocument5 pagesHelping a Young Single MotherKarissa Gentica100% (1)
- Learn About Animals and PlantsDocument30 pagesLearn About Animals and PlantsSyed Azan mehdi shahNo ratings yet
- Duty Report RSUDZA Thursday, April 4 2019: Supervisors: Dr. TGK Puspa Dewi, OBGYN (Oncall) Dr. Cut Rika Maharani, OBGYNDocument5 pagesDuty Report RSUDZA Thursday, April 4 2019: Supervisors: Dr. TGK Puspa Dewi, OBGYN (Oncall) Dr. Cut Rika Maharani, OBGYNIMampu ZaharieNo ratings yet
- Terms in Pregnancy and BirthDocument3 pagesTerms in Pregnancy and BirthTri LestariNo ratings yet
- ANC Guidelines - 18 July 2022 - Final-3 (6942)Document238 pagesANC Guidelines - 18 July 2022 - Final-3 (6942)Sara YehiaNo ratings yet
- Allen RHDocument5 pagesAllen RHVadhilla SafitriNo ratings yet
- Causes of Developmental DisabilitiesDocument87 pagesCauses of Developmental DisabilitiesChristy100% (3)
- Hubungan DKP Dengan Kejadian Ketuban Pecah Dini Di Rsud Dr. M. Yunus BengkuluDocument8 pagesHubungan DKP Dengan Kejadian Ketuban Pecah Dini Di Rsud Dr. M. Yunus BengkuluAjengNo ratings yet