Professional Documents
Culture Documents
CT Și RMN
Uploaded by
Aurelia AlexandraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CT Și RMN
Uploaded by
Aurelia AlexandraCopyright:
Available Formats
CT AND MRI
81. CT and MRI
A transfer to the CT or MRI scanner with an anaesthetised patient is not a task to be undertaken lightly. There is
good reason why the CT scanner is sometimes referred to as the ‘doughnut of death’. When answering a question
on scan transfers, it is important to show the examiners that you are well prepared to cope with the potential pitfalls
that may occur on your journey.
What are the principles behind The name comes from the Greek ‘tomo’, meaning slice and ‘graphein’, to
computed tomography (CT) write. CTs take a series of X-ray images around a central axis, either in a
scanning? discontinuous ‘shoot and step’ process, or in a continuous ‘spiral’ manner.
The latter are much quicker and so may reduce motion artefact, and enable
better 3D reconstruction of images.
What are the principles behind > MRI is an alternative way of producing images of the body.
magnetic resonance imaging > MRI visualises soft tissues much better than does CT, and therefore is
(MRI)? more useful in the study of the brain, spinal cord and musculoskeletal
system.
> Atoms with unpaired electrons or protons are in a state of spin that can be
affected by the application of an external magnetic field.
> Hydrogen ions found in water and fat molecules (which make up 60–70%
of the body) are affected in this way and so, when the patient enters the
powerful magnetic field of the scanner (1–2 tesla), their protons align in the
direction of the field.
> The protons then begin to resonate at their ‘precision frequency’.
> The powerful magnet is called the ‘primary magnet’ and its magnetic field
is generated by an electrical current passing through coils of wire, which
are cooled with liquid helium.
> Once the atoms have lined up, a radiofrequency coil is turned on,
generating a second current at right angles to the first.
> The energy generated by this coil is absorbed by the hydrogen ions and
disrupts their alignment.
> When the radiofrequency coil is turned off, the protons release energy (in
the form of low-frequency radiation) and return to their original position.
> It is this low-frequency radiation that is detected by the scanner, and
reconstructed into images.
> Different tissues will give out different amounts of energy and return to
their equilibrium position at different rates, allowing for differentiation
between them. This exchange of energy between spin states is called
‘resonance’.
> Another component of the MRI scanner is the ‘gradient magnet’. These
are smaller magnets that are applied to allow fine-tuning and focusing of
the image on the area being studied. The banging noise in the MRI is the
sound of these magnets being turned on and off.
257
9781785230981_text.indb 257 24/02/16 9:36 pm
02 PHYSICS
> MRIs are either T1 or T2 weighted and this refers to the amount of time
elapsed between the radiofrequency magnet being switched off and the
image being taken, i.e. the ‘relaxation time’. T1 images are taken earlier
than T2. In T1 images fat is bright and water is black, in T2 images fat is
black and water is bright.
> The entire scanner is housed in a room lined with copper or aluminium,
and this room is referred to as the Faraday cage.
> What are the indications for general anaesthesia in the scanner?
> Unstable patient (e.g. for airway protection or from ITU)
> Young child if they cannot cooperate and lie still
> Patient with learning difficulties, as above
> Very anxious or claustrophobic patient
> Patients with movement disorders or who are unable to lie still for
sufficiently long.
What are the problems associated > Generic problems:
with anaesthesia in the scanning • Patients are removed to an often remote and isolated area:
department? This area may be unfamiliar to the responsible doctor. It is important,
therefore, to consider who will be available to help should there be an
emergency during the trip and if possible, to familiarise oneself with the
department and the equipment available there before the transfer.
• Cold and noisy environment: Ambient temperature in an MRI
scanner is cool in order to prevent the magnet from overheating. The
magnets produce a lot of noise and earplugs must therefore be used
and patients covered in order to minimise risk of hypothermia.
• Claustrophobic environment: Space within scanners is extremely
limited, more so in the MRI scanner, and some patients can find this
very distressing.
• Limited space for anaesthetic equipment
• Limited access to the patient: Once the patient is in the scanner it
can be practically impossible to get to them. Before the scan begins it
is important to satisfy yourself that all the leads reach far enough, that
the patient is stable and that you can see the monitor. The scan may
take some time, especially if it is an MRI.
> Specific problems related to the MRI scanner: The magnet in the MRI
adds a whole new layer of problems.
• Ferrous implants: Within the magnetic field, ferrous implants (e.g.
pacemakers, defibrillators, cochlear implants, some aneurysm clips
and foreign bodies) are prone to displacement or torque forces, which
can lead to serious patient injury. Patients with any such implants must
not enter the MRI scanner. Non-ferrous implants are prone to heating
and patients must be warned of this. Both types of implants can cause
image artefacts.
• Ferrous equipment: Ferrous-containing equipment such as
laryngoscopes, stethoscopes, pagers, and gas cylinders are prone to
significant movement within the 50 G line and should therefore not be
taken beyond this point unless securely fastened. Magnetic strips on
identity badges and credit cards will also be wiped if taken within the
magnetic field. Ideally, only ‘MR safe’ and ‘MR conditional’ equipment
should be used within the scanner.
• Monitoring: Special ‘MR safe’ ECG electrodes, BP cuffs and pulse
oximeters are required. ECG leads are short and plaited to minimise
the risk of magnetically induced currents within them, which can burn
the patient (burns are the most common MRI-associated injury). If
a standard anaesthetic machine is used, this is housed outside the
Faraday cage with an extra long Bain circuit connecting it to the
patient. Long gas analysis sampling lines cause a delay in monitoring.
Monitoring equipment can introduce stray radiofrequency currents,
which can degrade the image quality.
258
9781785230981_text.indb 258 24/02/16 9:36 pm
CT AND MRI
• Delivery of anaesthesia: ‘MR conditional’ infusion pumps should
ideally be used. However, standard pumps can also be used outside
the 100 G line (see below). Volatile agents can be administered using
an ‘MR conditional’ anaesthetic machine. If this is not available, a
standard anaesthetic machine can be used outside the cage with an
extra-long Bain circuit.
How are items to be used within The old term ‘MR compatible’ is no longer suitable and the ASTM
an MRI scanner classified? International and FDA have introduced the following classification system:
> MR Safe: Items are completely free of all metallic components. They are
non-metallic, non-conductive and non-radiofrequency reactive. They pose
no hazard in any MR environment.
> MR Conditional: Items are safe under certain tested magnetic
conditions, which should be enumerated on the product (i.e. the magnetic
field strength in which the product can be safely used is stated).
> MR Unsafe: Items pose a hazard in any MR environment.
What is the standard international > SI unit for magnetic flux is the weber (Wb)
unit of magnetic strength? > SI unit for magnetic flux density is the tesla (T), which is used for large
densities. For smaller densities, a smaller unit, the gauss (G) is used. An
average MR scanner produces between 1 and 1.5 T (although newer
machines can now generate up to 3–5 T), while earth’s magnetic field is
about 1 G.
1 T = 1 Wb/m2
1 T = 10 000 gauss
259
9781785230981_text.indb 259 24/02/16 9:36 pm
You might also like
- MRI, Nuclear Medicine 2Document65 pagesMRI, Nuclear Medicine 2Khai QingNo ratings yet
- Magnetic Imaging ResonaceDocument48 pagesMagnetic Imaging ResonaceVĩ ĐặngNo ratings yet
- Magnetic Resonance ImagingDocument5 pagesMagnetic Resonance ImagingLames Ali Sayed Ahmed AttiaNo ratings yet
- Magnetic Resonance Imaging (MRI)Document17 pagesMagnetic Resonance Imaging (MRI)VinothKumarNo ratings yet
- Mri Atro PDFDocument85 pagesMri Atro PDFIno Da ConceicaoNo ratings yet
- 14 Medical Imaging-1Document35 pages14 Medical Imaging-1丁周辰No ratings yet
- Magnetic Resonance Imaging:-: How MRI WorksDocument4 pagesMagnetic Resonance Imaging:-: How MRI WorkscoolmushiNo ratings yet
- Notes On MRI - FinalDocument15 pagesNotes On MRI - FinalAbhi Sachdev100% (1)
- Presented By-Rupinder Kaur B.SC 3 Year Deptt of Radiodiagnosis and Imaging Sector 32 ChandigarhDocument64 pagesPresented By-Rupinder Kaur B.SC 3 Year Deptt of Radiodiagnosis and Imaging Sector 32 ChandigarhPreet SainiNo ratings yet
- Atomic & Nuclear PhysicsDocument9 pagesAtomic & Nuclear PhysicsPyay Lin ThantNo ratings yet
- My MRIDocument58 pagesMy MRIapi-26159412100% (1)
- Magnetic Resonance ImagingDocument6 pagesMagnetic Resonance ImagingmedodiabNo ratings yet
- HelloDocument23 pagesHelloysirola9410No ratings yet
- CH 19A - Remote Sensing (X-Ray)Document21 pagesCH 19A - Remote Sensing (X-Ray)OKAY JAROD PUGNo ratings yet
- Answer Key 5Document9 pagesAnswer Key 5Sajjala Poojith reddyNo ratings yet
- MRIDocument22 pagesMRIRohan GroverNo ratings yet
- Principle and Application of UltrasonographyDocument6 pagesPrinciple and Application of Ultrasonographyabhinav24624No ratings yet
- Mri 1Document42 pagesMri 1Abhishek Sinha100% (1)
- Magnetic Resonance ImagingDocument32 pagesMagnetic Resonance ImagingJolina Anne TempongkoNo ratings yet
- Magnetic Resonance Imaging (MRI)Document13 pagesMagnetic Resonance Imaging (MRI)Kristina RoblesNo ratings yet
- MRI For Dummies Part2 GallezDocument27 pagesMRI For Dummies Part2 GallezIrina Ionete100% (1)
- DR MisbahDocument2 pagesDR MisbahAqee FarooqNo ratings yet
- Anaesthesia in The MRI SuiteDocument8 pagesAnaesthesia in The MRI Suitemohananprasad27No ratings yet
- L1 For MondayDocument37 pagesL1 For MondayHavana, Keren Anne M.No ratings yet
- X Rays A-Level NotesDocument31 pagesX Rays A-Level NotesNoah GruterNo ratings yet
- 2006 Physics NotesDocument7 pages2006 Physics NotesnealNo ratings yet
- Radiography TestingDocument98 pagesRadiography TestingKanda SamyNo ratings yet
- Medical Physics - U6 Physics PresentationDocument52 pagesMedical Physics - U6 Physics Presentationanmolz.ghNo ratings yet
- POI Lab ReviewerDocument2 pagesPOI Lab ReviewerJerick JusayNo ratings yet
- Magnetic Resonance ImagingDocument2 pagesMagnetic Resonance ImagingChirag JainNo ratings yet
- Module 5 PDFDocument98 pagesModule 5 PDFRicky SarkarNo ratings yet
- Magnetic Resonance Imaging: BY.. G.BervinDocument31 pagesMagnetic Resonance Imaging: BY.. G.BervinBERVIN KINGS100% (1)
- Electromagnetic Spectrum GCLDocument64 pagesElectromagnetic Spectrum GCLsucculentcactirootsNo ratings yet
- My Summary in Radiology - A M Abodahab MDDocument387 pagesMy Summary in Radiology - A M Abodahab MDtran quang vinh100% (1)
- Magnetic Resonance Imaging: The Diffusion and ADC Imaging WayDocument50 pagesMagnetic Resonance Imaging: The Diffusion and ADC Imaging WayEka JuliantaraNo ratings yet
- Role of IN Oral & Maxillofacial Surgery: Mri ImagingDocument34 pagesRole of IN Oral & Maxillofacial Surgery: Mri ImagingAKSHAYA SUBHASHINEE DNo ratings yet
- Remote Sensing - X-Ray NotesDocument21 pagesRemote Sensing - X-Ray NotesJk JeeksNo ratings yet
- Magnetic Resonance Imaging (MRI) - LVRDocument24 pagesMagnetic Resonance Imaging (MRI) - LVRlvrevathi67% (3)
- 1 Magnetic Resonance Imaging - ٠٨٣١٥٤Document61 pages1 Magnetic Resonance Imaging - ٠٨٣١٥٤احمد اليمنيNo ratings yet
- Resolution in Ultrasound ImagingDocument7 pagesResolution in Ultrasound ImagingVyshnavi EaswaranNo ratings yet
- Martin (2015) - Physics of UltrasoundDocument4 pagesMartin (2015) - Physics of Ultrasoundgatorfan786No ratings yet
- Notes: Science & Computer - Term 1, Cycle 2Document23 pagesNotes: Science & Computer - Term 1, Cycle 2chy marizNo ratings yet
- Radiac Cuerpo Negro - SearsDocument5 pagesRadiac Cuerpo Negro - SearsOswaldo BastidaNo ratings yet
- Magnetic Resonance ImagingDocument11 pagesMagnetic Resonance ImagingJohn Paul MarasiganNo ratings yet
- Plain Film. 2. Computed Axial Tomography. 3. Ultrasonography. 4. Magnetic Resonance Imaging. 5. ScintigraphyDocument83 pagesPlain Film. 2. Computed Axial Tomography. 3. Ultrasonography. 4. Magnetic Resonance Imaging. 5. ScintigraphyChris QueiklinNo ratings yet
- 2ND Grading Reviewer in ScienceDocument4 pages2ND Grading Reviewer in ScienceVannie Mondero50% (2)
- 1st Term Science Exam ReviewerDocument6 pages1st Term Science Exam ReviewerAndie MorenoNo ratings yet
- Radiological Equipment: Assignment Presentation On Several TopicsDocument58 pagesRadiological Equipment: Assignment Presentation On Several TopicsAsteway MesfinNo ratings yet
- Mri Srtle .Document40 pagesMri Srtle .falhazmi0069No ratings yet
- MR Image of The KneeDocument7 pagesMR Image of The KneejbsoniNo ratings yet
- Summary of Mri PhysicsDocument16 pagesSummary of Mri Physicsshikha712100% (1)
- MRI 4lDocument3 pagesMRI 4lsarithaNo ratings yet
- Magnetic Resonance Imaging (MRI) : Assignment OnDocument15 pagesMagnetic Resonance Imaging (MRI) : Assignment OnMaina BarmanNo ratings yet
- Lecture MRI 2Document26 pagesLecture MRI 2Heidar ZaarourNo ratings yet
- Lasers: What Do You Understand by The Term Laser'?Document3 pagesLasers: What Do You Understand by The Term Laser'?Aurelia AlexandraNo ratings yet
- Magnetic Resonance Imaging: BasicsDocument39 pagesMagnetic Resonance Imaging: BasicsPriya SalunkeNo ratings yet
- 1587138047MLS 314 Lecture Note (2019-2020)Document29 pages1587138047MLS 314 Lecture Note (2019-2020)rameezchaudhary964No ratings yet
- Mod 4Document14 pagesMod 4ANANDHU PILLAINo ratings yet
- Plasma Astrophysics: International Series of Monographs in Natural PhilosophyFrom EverandPlasma Astrophysics: International Series of Monographs in Natural PhilosophyNo ratings yet
- NMR Case Studies: Data Analysis of Complicated MoleculesFrom EverandNMR Case Studies: Data Analysis of Complicated MoleculesRating: 5 out of 5 stars5/5 (1)
- Ultrasound Și DopplerDocument3 pagesUltrasound Și DopplerAurelia AlexandraNo ratings yet
- Pulse OximetryDocument3 pagesPulse OximetryAurelia AlexandraNo ratings yet
- Anti Fribrinolitic DrugsDocument15 pagesAnti Fribrinolitic DrugsAurelia AlexandraNo ratings yet
- Cursuri de Revisitare Și ValveDocument4 pagesCursuri de Revisitare Și ValveAurelia AlexandraNo ratings yet
- Sisteme de BreathingDocument5 pagesSisteme de BreathingAurelia AlexandraNo ratings yet
- 22 The Application of Farmacodynamics in The Optimization of Antibiotic Therapy PDFDocument2 pages22 The Application of Farmacodynamics in The Optimization of Antibiotic Therapy PDFAurelia AlexandraNo ratings yet
- The Primary FRCA Structured Oral Examination: Study Guide 1Document13 pagesThe Primary FRCA Structured Oral Examination: Study Guide 1Aurelia Alexandra0% (1)
- Poluare Și ScavengingDocument3 pagesPoluare Și ScavengingAurelia AlexandraNo ratings yet
- ADâncimea de Anestezie MOnITORINGDocument3 pagesADâncimea de Anestezie MOnITORINGAurelia AlexandraNo ratings yet
- Lasers: What Do You Understand by The Term Laser'?Document3 pagesLasers: What Do You Understand by The Term Laser'?Aurelia AlexandraNo ratings yet
- Presiune Arterială WaveformDocument3 pagesPresiune Arterială WaveformAurelia AlexandraNo ratings yet
- Neuromuscular Blockade MonitoringDocument7 pagesNeuromuscular Blockade MonitoringAurelia AlexandraNo ratings yet
- Monitori de DiscnecțieDocument2 pagesMonitori de DiscnecțieAurelia AlexandraNo ratings yet
- venTILATORIDocument3 pagesvenTILATORIAurelia AlexandraNo ratings yet
- Cardiac Utput MonitoringDocument7 pagesCardiac Utput MonitoringAurelia AlexandraNo ratings yet
- Temperature MeasurementDocument4 pagesTemperature MeasurementAurelia AlexandraNo ratings yet
- Carbon Dioxide MeasurementDocument2 pagesCarbon Dioxide MeasurementAurelia AlexandraNo ratings yet
- Featuri de Siguranță A Machinelor AnesteziceDocument3 pagesFeaturi de Siguranță A Machinelor AnesteziceAurelia AlexandraNo ratings yet
- SIGURANȚĂ eLeCTRICĂDocument3 pagesSIGURANȚĂ eLeCTRICĂAurelia AlexandraNo ratings yet
- PH MeasurementDocument2 pagesPH MeasurementAurelia AlexandraNo ratings yet
- Adaptarea Gazelor MediceDocument4 pagesAdaptarea Gazelor MediceAurelia AlexandraNo ratings yet
- Presiune de Sânge MeasurementDocument3 pagesPresiune de Sânge MeasurementAurelia AlexandraNo ratings yet
- Defibrillators: What Is The Difference Between Monophasic and Biphasic Waveform Defibrillators?Document2 pagesDefibrillators: What Is The Difference Between Monophasic and Biphasic Waveform Defibrillators?Aurelia AlexandraNo ratings yet
- COMPONENTE eLeCTRICEDocument3 pagesCOMPONENTE eLeCTRICEAurelia AlexandraNo ratings yet
- ReFLexeSDocument2 pagesReFLexeSAurelia AlexandraNo ratings yet
- Regulatori de PresiuneDocument3 pagesRegulatori de PresiuneAurelia AlexandraNo ratings yet
- Oxygen MeasurementDocument4 pagesOxygen MeasurementAurelia AlexandraNo ratings yet
- States of Matter, Heat Capacity and Latent Heat: PhysicsDocument7 pagesStates of Matter, Heat Capacity and Latent Heat: PhysicsAurelia AlexandraNo ratings yet
- Legile GazelorDocument3 pagesLegile GazelorAurelia AlexandraNo ratings yet
- What Is Flow?: Turbulent Flow Laminar FlowDocument3 pagesWhat Is Flow?: Turbulent Flow Laminar FlowAurelia AlexandraNo ratings yet
- 2011 Frequency AllocationsDocument1 page2011 Frequency Allocationsculeros1No ratings yet
- 8051 Programs Using Kit: Exp No: Date: Arithmetic Operations Using 8051Document16 pages8051 Programs Using Kit: Exp No: Date: Arithmetic Operations Using 8051Gajalakshmi AshokNo ratings yet
- I. Objectives Ii. Content Iii. Learning ResourcesDocument13 pagesI. Objectives Ii. Content Iii. Learning ResourcesZenia CapalacNo ratings yet
- Changing Sentences in The Simple Present Tense Into PassiveDocument4 pagesChanging Sentences in The Simple Present Tense Into PassiveBernadette NarteNo ratings yet
- T54125ADocument64 pagesT54125ARaúl FroddenNo ratings yet
- National Pension System (NPS) - Subscriber Registration FormDocument3 pagesNational Pension System (NPS) - Subscriber Registration FormPratikJagtapNo ratings yet
- Visual Metaphor Process BookDocument18 pagesVisual Metaphor Process Bookmatt8859No ratings yet
- Ib Psychology - Perfect Saq Examination Answers PDFDocument2 pagesIb Psychology - Perfect Saq Examination Answers PDFzeelaf siraj0% (2)
- Electronic Parts Catalog - Option Detail Option Group Graphic Film Card DateDocument2 pagesElectronic Parts Catalog - Option Detail Option Group Graphic Film Card DatenurdinzaiNo ratings yet
- Medrano, Rene LynnDocument2 pagesMedrano, Rene LynnRene Lynn Labing-isa Malik-MedranoNo ratings yet
- GATE Chemical Engineering 2015Document18 pagesGATE Chemical Engineering 2015Sabareesh Chandra ShekarNo ratings yet
- Progressive Muscle Relaxation ExerciseDocument2 pagesProgressive Muscle Relaxation Exerciseraghu2362704100% (1)
- Emerson Mentor MP ManualDocument182 pagesEmerson Mentor MP ManualiampedrooNo ratings yet
- Analyst - Finance, John Lewis John Lewis PartnershipDocument2 pagesAnalyst - Finance, John Lewis John Lewis Partnershipsecret_1992No ratings yet
- Energy BodiesDocument1 pageEnergy BodiesannoyingsporeNo ratings yet
- Admission: North South University (NSU) Question Bank Summer 2019Document10 pagesAdmission: North South University (NSU) Question Bank Summer 2019Mahmoud Hasan100% (7)
- Piaggio MP3 300 Ibrido LT MY 2010 (En)Document412 pagesPiaggio MP3 300 Ibrido LT MY 2010 (En)Manualles100% (3)
- Kunst 1600 Case AnalysisDocument3 pagesKunst 1600 Case AnalysisrakeshNo ratings yet
- Lennox IcomfortTouch ManualDocument39 pagesLennox IcomfortTouch ManualMuhammid Zahid AttariNo ratings yet
- Practice Test - Math As A Language - MATHEMATICS IN THE MODERN WORLDDocument8 pagesPractice Test - Math As A Language - MATHEMATICS IN THE MODERN WORLDMarc Stanley YaoNo ratings yet
- Hypothesis Testing Random MotorsDocument8 pagesHypothesis Testing Random MotorsLinn ArshadNo ratings yet
- Powering Laser Diode SystemsDocument134 pagesPowering Laser Diode SystemsNick100% (1)
- Design of Footing R1Document8 pagesDesign of Footing R1URVESHKUMAR PATELNo ratings yet
- Turbine Start-Up SOPDocument17 pagesTurbine Start-Up SOPCo-gen ManagerNo ratings yet
- Ateneo de Naga University: Professional Training For Teacher 4.0Document10 pagesAteneo de Naga University: Professional Training For Teacher 4.0Rosemarie BrionesNo ratings yet
- 02 Lab 1.HCIDocument2 pages02 Lab 1.HCILopao SerojemNo ratings yet
- CKRE Lab (CHC 304) Manual - 16 May 22Document66 pagesCKRE Lab (CHC 304) Manual - 16 May 22Varun pandeyNo ratings yet
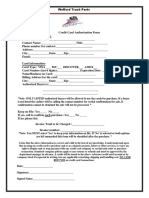
- Credit Card Authorization Form WoffordDocument1 pageCredit Card Authorization Form WoffordRaúl Enmanuel Capellan PeñaNo ratings yet
- Lab 3 Report Fins RedoDocument3 pagesLab 3 Report Fins RedoWestley GomezNo ratings yet
- Mathematics4 q4 Week4 v4Document11 pagesMathematics4 q4 Week4 v4Morales JinxNo ratings yet