Professional Documents
Culture Documents
Harms C1-C2 Instrumentation Technique
Uploaded by
Michael ZhengOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Harms C1-C2 Instrumentation Technique
Uploaded by
Michael ZhengCopyright:
Available Formats
SPINE Volume 36, Number 12, pp 945–950
©2011, Lippincott Williams & Wilkins
BIOMECHANICS
Harms C1–C2 Instrumentation Technique
Anatomo-Surgical Guide
Ronald Schulz, MD,* Nicolás Macchiavello, MD,* Elias Fernández,† Xabier Carredano, MD,‡
Osvaldo Garrido, MD,‡ Jorge Diaz, MD,§ and Robert P. Melcher, MD,¶
3.5 mm screw in the lateral masses of C1 and through the pars of C2.
Study Design. Anatomic study.
Dissecting the superior face of the posterior arch of C1 laterally more
Objective. To measure C1 and C2 critical areas related to the
than 10 mm from the posterior tubercule could injure the vertebral
screws trajectory, according to Harms technique, in Latin specimens.
artery.
To investigate vertebral’s artery course in cadavers.
Key words: atlantoaxial fixation, vertebral artery, lateral mass screws.
Summary of Background Data. To our knowledge there are
Spine 2011;36:945–950
no studies addressing vertebral surface measurements for screw
placement, according to Harms C1–C2 instrumentation technique,
A
nor cadaveric measurements of the trajectory of the vertebral artery unique anatomy and biomechanical properties make
in Latin specimens. the atlantoaxial region a surgically challenging one,1–3
Methods. C1 and C2 specimens were measured. C1 measurements: Posterior stabilization techniques with wires are still
height, width, anteroposterior diameter (intraosseus screw length) widely used, but they have many drawbacks. Neurologic risk
and convergence in the axial plane of the lateral mass; length during sublaminar wire passage, weak biomechanical prop-
from the posterior border of the posterior C1 arch to the anterior erties which add the need of post operative immobilization,
cortex of the articular mass (total screw length). C2 measurements: nonunion rates as high as 50%4 and a tendency to displace—
width, height, convergence and sagittal inclination of the pars rather than reduce—the atlantoaxial joint4 have been report-
interarticularis. Direction of the trajectory of the vertebral artery in ed. The addition of Magerl’s technique improved stability of
the suboccipital region in fresh cadavers. the construct and fusion rates.5–7 However, it’s far from being
Results. C1: left mass width 14.20 mm, right: 14.32 mm; left perfect, due to reported high risks of injury to the vertebral
intraosseus screw length: 17.17 mm, right 16.9 mm; left total length artery, which can go up to 18% depending on the series re-
of the screw: 27.14 mm, right: 26.72 mm; left mass height: 10.22 viewed.2,8,9 Other disadvantages of this technique include the
mm, right: 10.29 mm. Right mass convergence: 24.68⬚, left: 22.44⬚. need of extending the approach (which carries propriocep-
C2: width: left 8.75 mm, right: 8.53 mm; height: left 10 mm, right tive impairment and pain) or making additional incisions for
9.81 mm; convergence: left 42.15⬚, right: 38.98⬚; sagittal inclination: screw placement; indirect reduction of C1–C2, which must
left 35.50⬚, right 33.07⬚. Vertebral artery’s medial border is between be kept during the whole procedure, can be difficult and not
13 and 22 mm from the middle line of C1 posterior arch. without risk. Finally, pronounced cervicothoracic kyphosis
Conclusion. Convergence and inclination of the pars are slightly or some abnormalities of the vertebral artery make this tech-
greater than the suggested by Harms. Individual and/or racial variations nique useless.1–3,10
must be considered. There is enough space for safe placement of a The technique published by Harms,11,12 has addressed
many of the problems described above.
From the *Spine Unit, Department of Orthopaedics and Traumatology, Some studies show the feasibility of screw placement based
Hospital Clínico Universidad de Chile, Chile; †Morphology Unit, Depart- on measurements on vertebrae specimens,13–16 and CT images.17
ment of Normal Anatomy, Facultad de Medicina, Universidad de Chile, Chile; There is one study which evaluates the vertebral artery groove
‡Department of Orthopaedics and Traumatology, Hospital Clinico Universidad
de Chile, Chile; §Radiology Department, Hospital Clínico Universidad de of C1 in dry vertebrae and addresses it’s relationship with the
Chile, Chile; ¶Department of Orthopaedics and Traumatology, Center for midline.18 To our knowledge, there are no studies measuring
Spinal Surgery, Klinikum Karlsbad-Langensteinbach, Germany. Latin-American specimens, nor cadavers, to study the course of
Acknowledgement date: December 7, 2009. Revise date: April 20, 2010. the vertebral artery in relation to Harms technique.
Accepted date: April 26, 2010.
The purpose of this study is to correlate the original
The manuscript submitted does not contain information about medical
device(s)/drug(s). suggestions for screw placement, in C1 and C2, accord-
No funds were received in support of this work. No benefits in any form have ing to Harms instrumentation technique, with surface
been or will be received from a commercial party related directly or indirectly measurements taken on vertebrae of Chilean specimens.
to the subject of this manuscript. Significant anatomosurgical differences may exist between
Address correspondence and reprint requests to Ronald Schulz Ibaceta, Ser- patients of different races that might prove relevant in a
vicio de Ortopedia y Traumatologia, Hospital Clínico Universidad de Chile,
Avenida Santos Dumont 999, Independencia, 8380456 Santiago, Chile, technique, which demands high precision in screw place-
E-mail: schulzibaceta@gmail.com. ment. Finally, cadaveric dissections of the C1–C2 region
DOI: 10.1097/BRS.0b013e3181e887df were performed to describe the course of the vertebral
Spine www.spinejournal.com 945
Copyright © 2011 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
BRS203943.indd 945 27/04/11 11:24 PM
BIOMECHANICS Harms C1–C2 Instrumentation Technique • Schulz et al
artery and determine anatomically its risk of injury during
this technique.
MATERIALS AND METHODS
Twenty dry C1 and 20 C2 vertebrae were measured. The
vertebrae were obtained from the Anatomy Department,
Medical School, University of Chile. Demographic data of
these specimens was not available. In addition, anatomic dis-
sections of the suboccipital region were performed in 20 fresh
male cadavers, ages 35 to 75, to measure the distance between
the posterior tubercule of the posterior arch of C1 and the
medial border of the vertebral artery, where it comes out of
C1 in direction of the foramen magnus.
Measurements were made by the same investigator, using a
digital caliper with a 0,02 mm accuracy (Uyustools, Iquique,
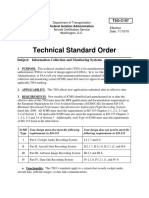
Chile). The measurements taken were the following (Figure 1):
(A) Width of the articular mass of C1, at the level of the
center of the transverse foramen.
(B) Height of C1 articular mass, measured at the point
where screw trajectory is narrower.
(B) AP diameter of the inferior mass of C1, following
the axis of the screw trajectory, according to Harms
technique (intraosseous screw length).
(B) Length from the posterior border of the posterior
arch to the anterior cortex of C1 articular mass, fol-
lowing the screw’s direction (total screw length).
(B) Width of C2 pars, at the level of the center of the
transverse foramen.
(B) Height of C2 pars, at the level of the center of the
transverse foramen.
Digital pictures of the six faces (superior, inferior, anterior,
posterior, and lateral) of each vertebrae were taken. The pic-
tures were then analyzed with OsirixR version 2.5.1 software,
to measure the following angles (Figure 2):
(A) Convergence of the lateral masses of C1 in the axial plane.
(B) Convergence of C2 pars.
(C) Sagittal inclination of C2 pars.
Surgical Dissection and Screw Placement Technique
The surgical dissection was performed after midline incision
down to the suboccipital plane, the rectus capitis major and
obliquus capitis inferior are dissected subperiostically from the
spinous process of C2, to expose the laminae and C1–C2 joint.
After preparing the laminae of C2, the occipital bone is
exposed partially, at the medial part, below the nuchal line. Figure 1. (A) Width of the articular mass of C1, at the level of the center
Once the posterior tubercule of C1 is identified, the rectus of the transverse foramen. (B) Height of C1 articular mass, measured
capitis minor muscle is released from it. at the point where screw trajectory is more narrow. (C) AP diameter
The next step is to remove the muscular tissue from the of the inferior mass of C1, following the axis of the screw trajectory,
atlantooccipital membrane, using blunt dissection, and expose according to Harms technique (intraosseous screw length). (D) Length
from the posterior border of the posterior arch to the anterior cor-
the C2 nerve. Careful dissection of the tissue that surrounds the tex of C1 articular mass, following the screw´s direction (total screw
C2 dorsal root ganglion, below the arch of C1, is carried out. length). (E) Width of C2 pars, at the level of the center of the transverse
At the end, exposure of the pars of C2 is carried on with foramen. (F) Height of C2 pars, at the level of the center of the transverse
help of a Penfield no. 4 dissector. foramen.
946 www.spinejournal.com May 2011
Copyright © 2011 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
BRS203943.indd 946 27/04/11 11:24 PM
BIOMECHANICS Harms C1–C2 Instrumentation Technique • Schulz et al
Figure 2. (A) Convergence angle of the major axis of
C1 lateral mass. (B) Convergence angle of C2 pars. (C)
Sagittal inclination angle of C2 pars
C1 Screws where it comes out of C1 in direction of the foramen magnus,
The entry point of C1 lateral mass is in the middle of the junc- measured between 13 and 22 mm (Figures 3 and 4, Table 1).
tion of the C1 posterior arch and the midpoint of the poste- We observed that the vertebral artery cannot be mobilized in
rior inferior part of the C1 lateral mass. the sulcus of C1 without risking its rupture. Differences were
According to the technique described by Harms and Melcher, not significant between the right and the left side.
the screws follow a posterior to anterior direction, with 5⬚–10⬚
of convergence. On the sagittal plane the trajectory must be Anatomo-Surgical Correlation for C1 Screws
completely parallel to the caudal aspect of the posterior arch of Table 2 shows the results for the measurements of C1.
C1, pointing toward the middle of the anterior tubercule of C1.
C2 Screws
The entry point for C2 screws should be on the superior-
medial aspect of a quadrant formed by the intersection of two
lines, one which bisects C2 pars vertically and the other which
bisects the lamina horizontally. The direction described is 20⬚
to 30⬚ medial, and 20⬚ to 30⬚ cephalad.
RESULTS
Dissection
The distance between the posterior tubercule of the poste-
rior arch of C1 and the medial border of the vertebral artery,
Figure 4. Posterior view, from the occipital bone to approximately C4.
C0 indicates occiput; AV, vertebral artery; C1, posterior arch of C1; C2,
posterior arch of C2; nOM, Mayor occipital nerve.
TABLE 1. The Distance Between the Posterior
Tubercule of the Posterior Arch of
C1 and the Medial Border of the
Vertebral Artery (n ⴝ 20)
Distance Std.
Figure 3. Posterior oblique view of the left side, from the occipital bone (mm) Minimum Maximum Mean Deviation
to C2. C0 indicates occipital; D, distance from the middle line to the
turn of the vertebral artery; C1, posterior arch of C1 (left side); AV, left Left 13 17 14.55 1.43178
vertebral artery; A-C1C2, left C1C2 joint; P, left pars; C2, posterior arch Right 13 22 14.8 2.21478
of C2 (left side).
Spine www.spinejournal.com 947
Copyright © 2011 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
BRS203943.indd 947 27/04/11 11:24 PM
BIOMECHANICS Harms C1–C2 Instrumentation Technique • Schulz et al
TABLE 2. C1 Measurements (n ⴝ 20)
C1 measurements (mm) Minimum Maximum Mean Std. Deviation
Left lateral mass width (mm) 12.00 16.55 14.20 1.39
Right lateral mass width (mm) 12.00 17.80 14.320 1.51
Left screw intraosseous length (mm) 13.90 21.00 17.17 1.85
Right screw intraosseous length (mm) 13.90 20.70 16.90 1.84
Left screw total length (mm) 24.30 30.70 27.14 1.54
Right screw total length (mm) 23.15 30.70 26.72 1.82
AltLeft lateral mass height (mm) 8.00 12.80 10.22 1.39
Reight lateral mass height (mm) 8.40 12.60 10.29 1.28
Right lateral mass convergence (degrees) 17.82 38.81 24.68 4.39
Left lateral mass convergence (degrees) 10.56 41.76 22.44 6.96
TABLE 3. C2 Measurements (n ⫽ 20)
C2 measurements Minimum Maximum Mean Std. Deviation
Right pars convergence (grades) 30.10 45.50 38.98 4.39
Left pars convergence (grades) 31.50 54.90 42.15 6.05
Right pars inclination (grades) 17.97 52.60 33.07 8.62
Left pars inclination (grades) 18.70 51.20 35.50 9.51
Left pars width (mm) 7.10 11.50 8.75 1.26
Right pars width (mm) 7.00 10.45 8.53 1.12
Left pars height (mm) 8.20 12.90 10.00 1.18
Right pars height (mm) 8.20 12.00 9.81 0.99
Convergence used in Harms technique (5⬚–10⬚) is lower The width and thickness of C1 articular masses are big
than the mayor axis of C1 mass. The average convergence enough to allow safe insertion of 3.5 mm screws, with mini-
angle of the left mass (Figure 2A) was 22.4⬚ (min 10.56⬚, max mal risk of injury to the vertebral artery (laterally and cra-
41.76⬚). At the right side, the average was 24.68⬚ (min 17.82⬚, neally), the spinal cord (medially), C1–C2 joint (caudally)
max 38.81⬚). and less frequently to the C0–C1 joint. Nevertheless, notice
When both sides were compared, significant differences should be taken in that the anatomic convergence of the lat-
were found in the length, measured between the posterior eral masses of C1 seems to be higher than suggested in Harms
border of the posterior arch and the anterior cortical of work. This anatomic variation might be explained, among
C1 mass, following the direction of the screw (P ⫽ 0015;
T test), and in the convergence of the lateral masses (P ⫽
0.025; T test).
Anatomo-Surgical Correlation for C2 Screws
Table 3 shows the measurements of C2.
Comparing both sides, again significant differences were
found in the measurements of the pars convergence (P ⫽
0.002; T test).
DISCUSSION Figure 5. The image on the left shows normal morphology of the pars
Our dissections and measurements in vertebrae show that and the transverse foramen of C2 (A and B). Image on the right shows
Harms C1–C2 instrumentation technique is feasible with a high foramen (B), which will not accommodate a screw. The pars is
reasonable safety. also shorter (A)
948 www.spinejournal.com May 2011
Copyright © 2011 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
BRS203943.indd 948 27/04/11 11:24 PM
BIOMECHANICS Harms C1–C2 Instrumentation Technique • Schulz et al
Figure 6. Left: Posterior view of left C1–
C2 joint. Right: lateral view. C1 indicates
posterior arch of C1; nOM, mayor oc-
cipital nerve; C2, posterior arch of C2;
CA, articular capsule; AV, vertebral artery;
AC1–C2, C1–C2 joint.
other things, by morphologic differences related to race. To Anecdotally, we noticed that there is a nutricious canal at
our knowledge, most of the studies have been performed in the union of the lamina with the pars of C2, which usually
Caucasian and Asiatic population. The reason for using a matches the insertion point of the C2 screw.
smaller convergence for C1 screw placement is that the lateral The learning curve, and the anatomic variations that can
mass losses height from lateral to medial. A screw that follows be found in each patient, must be addressed by surgeons at-
the anatomic convergence is in risk of perforating the C1–C2 tempting this procedure. Probably, racial differences must
or C0–C1 joints. also be considered. Appropriate training and familiarization
In the technique described by Magerl,5 the highest risk for with the technique, and a thorough preoperative examina-
injuring the vertebral artery is at the level of C2 transverse tion, which must include CT and angio-CT scans, would help
foramen. According to Paramore,2 18% of the patients pres- reduce the risks associated with this technique.
ent with a C2 transverse foramen that is to high to allow the
placement of a transarticular screw (Figure 5). In the same
series, 5% of the patients had anatomic conditions that made ➢ Key Points
the C1–C2 transarticular screw too dangerous. Theoretically,
this risk is lower when using Harms technique, because the di- Measurements at critical areas of C1 and C2 for
rection of the screw is convergent, thus moving away from the Harms technique were made in chilean specimens
artery. Still, Harms technique is not free of danger, especially Cadaveric dissections for analysis of the trajectory of
in patients with a high transverse foramen or a narrow pars the vertebral artery were made.
(Figure 5). It is also important to point out the fact that the Vertebral artery is at risk while dissecting C1 posterior
vertebral artery is also at risk during the dissection, at its path arch over 10 mm from the midline.
between C1 and C2, where it is almost impossible to move, Convergence and inclination of C2 pars interarticularis
due to its adherence to the articular capsule and the walls of are greater tha described in original technique.
the transverse foramen (Figure 6). According to our findings,
a laminectomy or the dissection of the superior face of the
posterior arc of C1 should not extend laterally more than Acknowledgments
10 mm from the posterior tubercule, which could be consid- The authors like to thank the Teaching and Research De-
ered arbitrarily as a “safe zone” (the lowest distance measured partment, Chilean Forensic Institute (Servicio Médico Legal
during our dissections, between the posterior tubercule of C1 de Chile) and Department of Anatomy and Developmental
and the medial border of the vertebral artery, was 13 mm). Biology, School of Medicine, University of Chile.
This distance is slightly bigger than the one suggested by
Ebraheim.18 In his work on dry C1 specimens, the distance References
from the midline to the medial-most edge of the vertebral 1. Coric D, Branch CL, Wilson JA, et al. Arteriovenous fistula as a
complication of C1–C2 transarticular screw fixation. J Neurosurg
artery groove averaged 10 mm, with a minimum of 8 mm, 1996;85:340–3.
which led him to suggest that dissection on the superior 2. Paramore CG, Dickman CA, Sonntag VKH. The anatomical suit-
aspect of the posterior ring should remain within 8 mm of ability of the C1–2 complex for transarticular screw fixation. J
the midline. Neurosurg 1996;85:221–4.
3. Madawi AA, Solanki G, Casey A, et al. Variation of the groove in
Height and width of the pars allow the placement of a the axis vertebra for the vertebral artery: implications for instru-
3.5 mm. The direction suggested in the original technique mentation. J Bone Joint Surg (Br) 1997;79-B:820–3.
(10⬚–30⬚ medial and 20⬚–30⬚ cranial) is slightly different from 4. Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus tran-
our measurements, which are bigger. This difference under- sarticular screw fixation in C1–C2 fusion. Clin Orthop 1999:126–35.
5. Magerl F, Seemann P. Stable Posterior Fusion of the Atlas and Axis
lines the importance of preoperative planning in these pa- by Transarticular Screw Fixation. ed. In: Kehr P, Weidner A (ed).
tients, in which individual anatomic variations must be con- Cervical Spine I. New York, Wien; Springer, 1986:322–7.
sidered. Also, intraoperative documentation with radiographs 6. Dickman C, Sonntag VKH. Posterior C1–C2 transarticular screw
should be always used. fixation for atlantoaxial arthrodesis. Neurosurgery 1998;43:275–80.
Spine www.spinejournal.com 949
Copyright © 2011 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
BRS203943.indd 949 27/04/11 11:24 PM
BIOMECHANICS Harms C1–C2 Instrumentation Technique • Schulz et al
7. Resnick DK, Lapsiwala S, Trost GR. Anatomic suitability of the 13. Hong X, Dong Y, Yunbing C, et al. Posterior screw placement on
C1–C2 complex for pedicle screw fixation. Spine 2002;27:1494–8. the lateral mass of atlas an anatomic study. Spine 2004;29:500–3.
8. Ebraheim N, Rollins JRJ, Xu R, et al. Anatomic consideration of 14. Dong I, Hong X, Jianyi L, et al. Quantitative anatomy of the lateral
C2 pedicle screw placement. Spine 1996;21:691–4. mass of the atlas. Spine 2003;28:860–3.
9. Weidner A, Wähler M, Tsien Chiu S, et al. Modification of C1– 15. Christensen D, Eastlack R, Lynch J, et al. C1 anatomy and di-
C2 transarticular screw fixation by image-guided surgery. Spine mensions relative to lateral mass screw placement. Spine 2007;32:
2000;25:2668–74. 844–8.
10. Mandel IM, Kambach BJ, Petersilge CA, et al. Morphologic consid- 16. Gupta G. Quantitative anatomy of the lateral masses of the atlas
erations of C2 Isthmus dimensions for the placement of transarticu- and axis vertebrae. Neurol India 2000;48:120–5.
lar screws. Spine 2000;25:1542–7. 17. Tan M, Wang H, Wang I, et al. Morphometric evaluation of
11. Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw screw fixation in atlas via posterior arch and lateral mass. Spine
and rod fixation. Spine 2001;26:2467–71. 2003;28:888–95.
12. Stulik J, Vyskocil T, Sebesta P, et al. Harms technique of C1–C2 18. Ebraheim N, Xu R, Ahmad M, et al. The quantitative anatomy
fixation with polyaxial screws and rods. Acta Chir Orthop Trau- of the vertebral artery groove of the atlas and its releation to the
matol Cech 2005;72:22–7. posterior atlantoaxial approach. Spine 1998;23:320–3.
950 www.spinejournal.com May 2011
Copyright © 2011 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
BRS203943.indd 950 27/04/11 11:24 PM
You might also like
- Instruction Manual Twin Lobe CompressorDocument10 pagesInstruction Manual Twin Lobe Compressorvsaagar100% (1)
- CT Based Morphometric Analysis of C1 Laminar DimensionsDocument4 pagesCT Based Morphometric Analysis of C1 Laminar DimensionsMichael ZhengNo ratings yet
- Translaminar Screw Fixation in The Subaxial Cervical Spine: EchniqueDocument7 pagesTranslaminar Screw Fixation in The Subaxial Cervical Spine: EchniqueSamet CeyhanNo ratings yet
- State of ArtDocument8 pagesState of ArtJorge RealNo ratings yet
- The Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesDocument4 pagesThe Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesFrontiersNo ratings yet
- 31703195Document13 pages31703195Martina javiera Alarcon AcevedoNo ratings yet
- Atlas c1Document5 pagesAtlas c1davorribicicNo ratings yet
- Bergeron 2007Document7 pagesBergeron 2007МаратNo ratings yet
- Articles by Dr. Nata ParnesDocument19 pagesArticles by Dr. Nata ParnesWatertown Daily TimesNo ratings yet
- Marcati 2017Document9 pagesMarcati 2017J Alan SantosNo ratings yet
- All Arthroscopic Coracoacromial Ligament TransferDocument9 pagesAll Arthroscopic Coracoacromial Ligament TransferMinh ChíNo ratings yet
- Transnasal Prelacrimal Approach To The Inferior Intraconal Space: A Feasibility StudyDocument6 pagesTransnasal Prelacrimal Approach To The Inferior Intraconal Space: A Feasibility Studythanh nguyenNo ratings yet
- Isd 48 121Document5 pagesIsd 48 121kalixinNo ratings yet
- Cerebellopontine Angle TumorsDocument7 pagesCerebellopontine Angle TumorsAslamHentatiNo ratings yet
- Acromioclavicular Joint Dislocation: Repair Through Open Ligament Transfer and Nonabsorbable Suture FixationDocument8 pagesAcromioclavicular Joint Dislocation: Repair Through Open Ligament Transfer and Nonabsorbable Suture FixationParaliov TiberiuNo ratings yet
- Bernardi Et Al. - 2016 - Cone Beam Computed Tomography Investigation of TheDocument6 pagesBernardi Et Al. - 2016 - Cone Beam Computed Tomography Investigation of TheCarlos Torres VillarNo ratings yet
- Jcedv 6 I 3 P 271Document4 pagesJcedv 6 I 3 P 271Suresh K KrishnasamyNo ratings yet
- 4D PlanningDocument6 pages4D Planningpaulwhite1234No ratings yet
- Anatomy of The Terminal Branch of The Posterior Circumflex Humeral ArteryDocument4 pagesAnatomy of The Terminal Branch of The Posterior Circumflex Humeral ArterymotohumeresNo ratings yet
- Singh 2015Document9 pagesSingh 2015Samet CeyhanNo ratings yet
- I Craneofacial CharacteristicDocument7 pagesI Craneofacial CharacteristicJavier Infantes MolinaNo ratings yet
- 05 CastelnuovoDocument7 pages05 Castelnuovogabriele1977No ratings yet
- Endoscopic Anatomy of Sphenoid Sinus For Pituitary Surgery: Original CommunicationDocument6 pagesEndoscopic Anatomy of Sphenoid Sinus For Pituitary Surgery: Original CommunicationKumaran Bagavathi RagavanNo ratings yet
- Ota 2015Document9 pagesOta 2015Luigi D'angeloNo ratings yet
- Podesser 2004Document7 pagesPodesser 2004Tien Li AnNo ratings yet
- Schimming, Eckelt e Kittner (1999) The Value of Coronal Computer Tomograms in Fractures of The Mandibular Condylar ProcessDocument8 pagesSchimming, Eckelt e Kittner (1999) The Value of Coronal Computer Tomograms in Fractures of The Mandibular Condylar ProcessSamádhi FugitaNo ratings yet
- Week 7 NeckDocument29 pagesWeek 7 NeckAbbas OmerNo ratings yet
- Risk To The Vertebral Artery During C-2 Translaminar Screw Placement: A Thin-Cut Computerized Tomography Angiogram-Based Morphometric AnalysisDocument5 pagesRisk To The Vertebral Artery During C-2 Translaminar Screw Placement: A Thin-Cut Computerized Tomography Angiogram-Based Morphometric AnalysisSamet CeyhanNo ratings yet
- Ojsadmin, 302Document7 pagesOjsadmin, 302Abhilash VemulaNo ratings yet
- Nasal Cavity Shape in Unilateral Choanal Atresia and The Role of Fetal Ventilation in Facial GrowthDocument6 pagesNasal Cavity Shape in Unilateral Choanal Atresia and The Role of Fetal Ventilation in Facial GrowthNalendra Tri WidhianartoNo ratings yet
- The Technique of S2-Alar-Iliac Screw Fixation: A Literature ReviewDocument8 pagesThe Technique of S2-Alar-Iliac Screw Fixation: A Literature Reviewdps_1976No ratings yet
- Indian Journal of Otolaryngology and Head & Neck SurgeryDocument14 pagesIndian Journal of Otolaryngology and Head & Neck SurgeryDrKunal KaradeNo ratings yet
- J ArthrnjknliDocument10 pagesJ ArthrnjknliJahid HasanNo ratings yet
- 1 s2.0 S2212628721002589 MainDocument6 pages1 s2.0 S2212628721002589 MainEvans JohnNo ratings yet
- Chahla 2018Document9 pagesChahla 2018Miguel Angel Lamas RamirezNo ratings yet
- Chimeric Groin Free Flaps Design and Clinical Application - Microsurgery, Vol. 36 Issue 3 (BZ 22588160)Document10 pagesChimeric Groin Free Flaps Design and Clinical Application - Microsurgery, Vol. 36 Issue 3 (BZ 22588160)Manny TrujilloNo ratings yet
- Anderson 2016Document2 pagesAnderson 2016Pallavi SutarNo ratings yet
- Lymphedema Rates in Pedicled ALTP For Coverage in Irradiated Groin Defects 2019Document4 pagesLymphedema Rates in Pedicled ALTP For Coverage in Irradiated Groin Defects 2019yeapdshengNo ratings yet
- Assessment of Location and Course of Inferior Alveolar Canal Using Cone Beam Computed TomographyDocument17 pagesAssessment of Location and Course of Inferior Alveolar Canal Using Cone Beam Computed TomographyIJAR JOURNALNo ratings yet
- Spiral CT Measurement For Atlantoaxial Pedicle Screw Trajectory and Its Clinical ApplicationDocument8 pagesSpiral CT Measurement For Atlantoaxial Pedicle Screw Trajectory and Its Clinical ApplicationMichael ZhengNo ratings yet
- A Sella Turcica Bridge in Subjects With Severe Craniofacial DeviationsDocument6 pagesA Sella Turcica Bridge in Subjects With Severe Craniofacial DeviationskalixinNo ratings yet
- The Importance of Three-Dimensional Imaging From CDocument6 pagesThe Importance of Three-Dimensional Imaging From CRifki KurniawanNo ratings yet
- 8509 30087 1 PBDocument5 pages8509 30087 1 PBWilson Quispe AlanocaNo ratings yet
- Ingles Silla TurcaDocument7 pagesIngles Silla TurcaWily Fernandez0% (1)
- Biomechanics of A Novel Technique For Suprapectoral Intraosseous Biceps TenodesisDocument9 pagesBiomechanics of A Novel Technique For Suprapectoral Intraosseous Biceps TenodesisEllan Giulianno FerreiraNo ratings yet
- Almeida 2015Document5 pagesAlmeida 2015andrea.lopezNo ratings yet
- Artigo Canal RetomolarDocument6 pagesArtigo Canal Retomolarhalaldesvio.0nNo ratings yet
- Andrade 2018Document6 pagesAndrade 2018Fausto Fernandes de CastroNo ratings yet
- MainDocument16 pagesMainel verdaderoNo ratings yet
- Labiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFDocument13 pagesLabiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFAlexandra DumitracheNo ratings yet
- Yamamoto 2007Document8 pagesYamamoto 2007BmNo ratings yet
- Abordaje CombinadoDocument5 pagesAbordaje CombinadoJulia LemboNo ratings yet
- 586 2012 Article 2505Document6 pages586 2012 Article 2505sulthoni ikaNo ratings yet
- CWU and CWDDocument4 pagesCWU and CWDJanfeb DuasatuNo ratings yet
- Virtual Placement of Posterior C1-C2 Transarticular Screw FixationDocument4 pagesVirtual Placement of Posterior C1-C2 Transarticular Screw FixationcaduanselmiNo ratings yet
- All-Epiphyseal, All-Inside Anterior Cruciate Ligament Reconstruction Technique For Skeletally Immature PatientsDocument9 pagesAll-Epiphyseal, All-Inside Anterior Cruciate Ligament Reconstruction Technique For Skeletally Immature Patientshieuminhduong7No ratings yet
- Orthopaedic Surgery - 2020 - Kuang - Figure of Eight Suture Button Technique For Fixation of Displaced Anterior CruciateDocument7 pagesOrthopaedic Surgery - 2020 - Kuang - Figure of Eight Suture Button Technique For Fixation of Displaced Anterior CruciateRisay YrucremNo ratings yet
- Endoscopic Telovelar Approach To The Fourth Ventricle - Anatomic StudyDocument9 pagesEndoscopic Telovelar Approach To The Fourth Ventricle - Anatomic StudyfrancsicovillegaslopezNo ratings yet
- Biomechanical RationaleDocument10 pagesBiomechanical RationalekhudecNo ratings yet
- Quads ReconDocument7 pagesQuads ReconNuno PaisNo ratings yet
- Chordomas and Chondrosarcomas of the Skull Base and SpineFrom EverandChordomas and Chondrosarcomas of the Skull Base and SpineGriffith R. Harsh IVNo ratings yet
- Spiral CT Measurement For Atlantoaxial Pedicle Screw Trajectory and Its Clinical ApplicationDocument8 pagesSpiral CT Measurement For Atlantoaxial Pedicle Screw Trajectory and Its Clinical ApplicationMichael ZhengNo ratings yet
- Radiographic and Clinical Outcomes of C1 - C2 Intra-Articular Screw Fixation in Patients With Atlantoaxial SubluxationDocument9 pagesRadiographic and Clinical Outcomes of C1 - C2 Intra-Articular Screw Fixation in Patients With Atlantoaxial SubluxationMichael ZhengNo ratings yet
- Design A Novel Integrated Screw For Minimally Invasive Atlantoaxial Anterior Transarticular Screw FixationDocument11 pagesDesign A Novel Integrated Screw For Minimally Invasive Atlantoaxial Anterior Transarticular Screw FixationMichael ZhengNo ratings yet
- Kinematic MRI Analysis of Reducible AtlantoaxialDocument7 pagesKinematic MRI Analysis of Reducible AtlantoaxialMichael ZhengNo ratings yet
- Tso C197Document6 pagesTso C197rdpereirNo ratings yet
- O Repensar Da Fonoaudiologia Na Epistemologia CienDocument5 pagesO Repensar Da Fonoaudiologia Na Epistemologia CienClaudilla L.No ratings yet
- Template Remarks For IIDocument18 pagesTemplate Remarks For IIjasleeneceNo ratings yet
- I. Objectives:: Semi-Detailed Lesson Plan in Reading and Writing (Grade 11)Document5 pagesI. Objectives:: Semi-Detailed Lesson Plan in Reading and Writing (Grade 11)Shelton Lyndon CemanesNo ratings yet
- Prospectus (As of November 2, 2015) PDFDocument132 pagesProspectus (As of November 2, 2015) PDFblackcholoNo ratings yet
- RIBA PoWUpdate 131009 ProbynMiersDocument28 pagesRIBA PoWUpdate 131009 ProbynMiersYellowLightNo ratings yet
- Cutler Hammer Dry Type TransformerDocument220 pagesCutler Hammer Dry Type TransformernprajanNo ratings yet
- POLYTHEOREMSDocument32 pagesPOLYTHEOREMSYen LeeNo ratings yet
- Chapter 10 Planetary Atmospheres: Earth and The Other Terrestrial WorldsDocument27 pagesChapter 10 Planetary Atmospheres: Earth and The Other Terrestrial WorldsEdwin ChuenNo ratings yet
- A Short History of Denim: (C) Lynn Downey, Levi Strauss & Co. HistorianDocument11 pagesA Short History of Denim: (C) Lynn Downey, Levi Strauss & Co. HistorianBoier Sesh PataNo ratings yet
- Micronet TMRDocument316 pagesMicronet TMRHaithem BrebishNo ratings yet
- Fish Culture in Ponds: Extension Bulletin No. 103Document32 pagesFish Culture in Ponds: Extension Bulletin No. 103Bagas IndiantoNo ratings yet
- 24 Inch MonitorDocument10 pages24 Inch MonitorMihir SaveNo ratings yet
- Growing Onion Management and Water NeedsDocument25 pagesGrowing Onion Management and Water NeedsKATE NAVAJANo ratings yet
- The Function and Importance of TransitionsDocument4 pagesThe Function and Importance of TransitionsMarc Jalen ReladorNo ratings yet
- Wire Rope TesterDocument4 pagesWire Rope TesterclzagaNo ratings yet
- Ccu 3900alDocument3 pagesCcu 3900alTourchianNo ratings yet
- CAMEL Model With Detailed Explanations and Proper FormulasDocument4 pagesCAMEL Model With Detailed Explanations and Proper FormulasHarsh AgarwalNo ratings yet
- Credit Risk ManagementDocument64 pagesCredit Risk Managementcherry_nu100% (12)
- Your Bentley Bentayga V8: PresentingDocument9 pagesYour Bentley Bentayga V8: PresentingThomas SeiferthNo ratings yet
- PrimerCube Manufacturing GuideDocument57 pagesPrimerCube Manufacturing GuideTinaMaleenaNo ratings yet
- Saes T 883Document13 pagesSaes T 883luke luckyNo ratings yet
- Tylenol CrisisDocument2 pagesTylenol CrisisNida SweetNo ratings yet
- Advanced Statistical Approaches To Quality: INSE 6220 - Week 4Document44 pagesAdvanced Statistical Approaches To Quality: INSE 6220 - Week 4picalaNo ratings yet
- Fh84fr6ht GBR EngDocument6 pagesFh84fr6ht GBR EngEsmir ŠkreboNo ratings yet
- Business OrganizationDocument32 pagesBusiness OrganizationSaugandh GambhirNo ratings yet
- Wind Turbines - I. Al-BahadlyDocument664 pagesWind Turbines - I. Al-Bahadlykevin_leigh_1No ratings yet
- Lit 30Document2 pagesLit 30ReemAlashhab81No ratings yet
- Chemical Classification of HormonesDocument65 pagesChemical Classification of HormonesetNo ratings yet