Professional Documents
Culture Documents
Trans-ViVa-Anes-Lec 10-Complications and Hazards of Anesthesia
Uploaded by
Jeno Luis J. ACUBCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trans-ViVa-Anes-Lec 10-Complications and Hazards of Anesthesia
Uploaded by
Jeno Luis J. ACUBCopyright:
Available Formats
06/12/2021
Asynchronous Complications and Hazards of Anesthesia
Anesthesiology
Victoria Uy-Hofileña, M.D., DPBA
AnatB1
OUTLINE
I. Introduction
II. Upper Airway Obstruction
III. Hypoxemia at the Post-Anesthesia Care Unit (PACU)
IV. Hemodynamic Instability
V. Body Temperature and Shivering
VI. Post-Operative Nausea and Vomiting (PONV)
VII. Spinal Headache
VIII. Others
IX. Hazards in Anesthesia
X. References
INTRODUCTION
Adopted from Lagasse RS: Anesthesia safety: Model or Myth? A review of the
Emergence is associated with physiologic disturbances published literature and analysis of current original data. Anesthesiology
Most common: 97:1609, 2002
o Postoperative nausea and vomiting (PONV)
Studies on anesthesia related mortality shows a 1:185,000
o Hypoxemia
incidence in the united states and is usually related to ASA
o Hypothermia and shivering Physical status.
o Cardiovascular instability
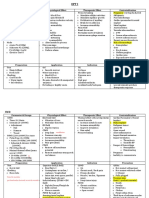
There are so many risks to your anesthesia. There are some we Complications vs. Anesthetic Technique
can control, and there are some we cannot. Complications Anesthetic Technique p-
Up to 7% of anesthesia related malpractice in the US were
GA RA NB Combined value
related to recovery room incidents and the most common is your
Headaches 38 16 - - <0.001*
post op nausea and vomiting. But the most serious outcomes are
Sore throat 211 7 2 2 <0.001*
related to your respiratory and vascular compromise
Myalgia 56 10 1 - 0.825
Nausea 128 22 1 - 0.490
Vomiting 98 23 1 - 0.573
Oral trauma 93 4 - - <0.001*
Teeth trauma 4 - - - -
Thrombophlebiti 85 12 2 - 0.065
s
Memory loss 6 1 - - 0.405
Micturition 36 10 - - 0.952
problems
Nightmares 9 - - - -
Back pain 68 17 - - 0.925
Motor deficit 12 2 1 - 0.163
Paresthesia 31 12 1 1 0.029*
GA: General Anesthesia; RA: Regional Anesthesia; NB: Nerve Block
Upto 7% of anesthesia related malpractice claims in the US were
attributed to recovery room incidents. most common is PONV.
But more serious outcomes are related to airway or respiratory
and cardiovascular compromise
Death Totally Attributable to Each Component of Risk in the
Confidential Enquiry into Perioperative Deaths UPPER AIRWAY OBSTRUCTION
Component Mortality Rate Contribution
Most frequent cause: Loss of pharyngeal muscle tone
Patient 1:870
o Attributed to inhaled and IV anesthetics, NMBD, and opioid
Operation 1:2860
used during anesthesia
Anesthetic 1:185,056
Adopted from Buck N, Devlin HB, Lunn JL,: Report of a Confidential Enquiry into
o Presents with “Paradoxical breathing pattern”
Perioperative Deaths, Nuffield Provincial Hospitals Trust. London, The King’s Normally the abdomen moves outward during
Fund Publishing House, 1987 inspiration, so when you breath against an obstructed
airway, what happens is that what you call your “see-
saw” breathing type of pattern.
o Released by:
Jaw thrust maneuver
CPAP by mask ventilation
CPU College of Medicine | Revised By: Victores Valetudinis | 2022
Resident Neuromuscular Blockade
Considered in patients recovering from anesthesia
Recovery from NMBD
o Diaphragm recovers before pharyngeal muscles
Supportive measures
o Thermoregulation
o Airway support
o Correct electrolyte imbalance
Laryngospasm
In awake patients, opening of the airway is facilitated by the
Most often occurs at time of extubation
contraction of your pharyngeal muscles that goes hand in hand
with the negative inspiratory pressure during breathing. This Jaw thrust + Continuous Positive Airway Pressure (CPAP) is
tone is however depressed in patients who are sleeping or often sufficient to break the spasm.
sedated and the airway will collapse causing a paradoxical Immediate muscle relaxation can be achieved with
breathing pattern. succinylcholine.
Obstructive Sleep Apnea (OSA)
Particularly prone to airway obstruction
Plans should be made post-operatively.
o “Like for example, allowing the patient to bring CPAP at
home so he can use it post-op.”
Should not be extubated until fully awake
Management of Upper Airway Obstruction
Immediate attention to open airways
o Non-invasive
Jaw thrust
CPAP
Oral/nasal airways
Laryngeal mask airway
o Reintubation of the trachea
If non-invasive measures fail.
Normally, abdomen moves outward during inspiration. When
you breath against an obstructed airway what happens is what HYPOXEMIA AT THE POST-ANESTHESIA CARE UNIT (PACU)
we call a see-saw type of breathing.
Most common causes
o Atelectasis
o Alveolar hypoventilation
Alveolar hypoventilation
Normal ventilator drive:
o Increase PaCo2= Hyperventilation
Post op= depressed ventilatory drive
o Hypercarbia= Increase PaCo2
o Most common cause of hypercarbia is hypoventilation.
o “In healthy person’s breathing room air, what happens if your
PaCO2 increases? Increase in RR. So, there should be
increase in respiratory rate or hyperventilation, however, in
the post-op period, because of the effects of your
anesthetics, residual neuromuscular blockers, etc., this
response to hypercarbia is depressed, increasing the risk
of your patient to develop hypoxemia. There may also be
Obstruction is relieved by simply doing the Jaw thrust and pulmonary edema, gastric aspiration, and pneumonia which
CPAP via facemask ventilation. During the perioperative causes your V/Q mismatch.”
period, support of the airways is needed until the patient is Arterial hypoxemia can be reversed by:
adequately recovered from the effects of drugs used during o Supplemental oxygen
anesthesia. o Reversal of sedatives
o External stimulation to awaken the patient
CPU College of Medicine | Revised by: Victores Valetudinis | 2022 Page 2 of 6
o Dysrhythmias
V/Q Mismatch
Atelectasis: most common cause of post-op pulmonary shunting BODY TEMPERATURE AND SHIVERING
o Management:
Mobilization and sitting position Incidence of post-op shivering
Incentive spirometry o Up to 65% after General Anesthesia (GA)
Positive pressure ventilation by face mask o Up to 33% after epidural
Risk factors:
HEMODYNAMIC INSTABILITY o Male gender
o Induction agents ~ propofol
Manifestations:
o Hypertension Shivering Mechanism
o Hypotension
o Tachycardia Associated (but not always) with hypothermia
o Bradycardia Thermoregulatory in hypothermic patients
o “Hypertension and tachycardia: higher mortality rate” Brain and spinal cord do not recover simultaneously from general
anesthesia
Hypertension o Spinal cord recovers faster
o Uninhibited spinal reflexes ~ clonic activity
Risk Factors:
o Essential hypertension Clinical Effects
o Pain
o Post-operative Nausea and Vomiting (PONV) Patient discomfort
o Hypoventilation with hypercarbia Increase Oxygen consumption
o Urinary retention Increase CO2 production
o Advanced age Increased cardiac output, heart rate and blood pressure
“Hypertension must be controlled at the PACU.” Long term effects:
o MI, delayed wound healing, increased mortality
Hypotension
Treatment
Classified as:
o Hypovolemic Identification and treatment of hypothermia
o Distributive Accurate temperature monitoring
o Cardiogenic Pharmacologic
1. Hypovolemic (Decreased Preload) o Prophylaxis: pre-op Ketamine
Decreased intravascular volume o Opioids: Meperidine
o Blood loss or inadequate replacement
o Third space losses POST-OP NAUSEA AND VOMITING
o “Will respond to IV fluids, and sometimes transfusion
may be necessary.” Incidence: 10-80% develop PONV after general anesthesia
2. Distributive (Decreased Afterload) o “Patients consider it as the most undesirable complication
Causes: of anesthesia.”
o Iatrogenic sympathectomy Consequences:
Sympathectomy: the loss of sympathetic tone o Delayed discharge from PACU
It is an important cause of hypotension peri- o Unanticipated hospital admission
operatively. o Pulmonary aspiration
“Peri-operatively, what can cause this loss in
sympathetic tone? An example is a patient who will
undergo surgery under neuroaxial anesthesia or
spinal or epidural anesthesia and he/she would
be at risk for hypotension.”
“How does hypotension happen during sympathetic
blocking? Because of vasodilatation that will
cause venous pooling which will lead to
decrease in venous return, thus the decrease in
preload, afterload and decrease in cardiac output.”
o Critical illness
o Allergic reaction
o Sepsis
3. Cardiogenic (Pump Failure)
Causes:
o Myocardial ischemia and infarction
o Cardiomyopathy
o Cardiac tamponade
CPU College of Medicine | Revised by: Victores Valetudinis | 2022 Page 3 of 6
o Vestibular apparatus
o Cerebral cortex
The Vomit center itself has intrinsic chemoreceptors that can
stimulate or repress vomiting and each of these 4 areas also
respond to different stimuli to affect the vomiting center and how
all these areas interact to modulate nausea and vomiting may
lead us to its specific treatment.
Consequences of PONV
Hospital Physical Psychological
Delayed Dehydration Aversion surgery
discharge from Electrolyte Increased patient
PACU by an imbalance discomfort
additional 15 to Anorexia Dissatisfaction
35 minutes Wound
(average 25 dehiscence
minutes) Bleeding
Additional staff Aspiration
time of 35 Loss of vision
minutes per Esophageal tears
patient on the
average impose
an incremental
cost per patient
over the initial 3
hours
PONV has a lot of consequences. For the hospital, For the
medical practitioner, and most importantly for the patient.
It is a major cause of delayed discharge from the PACU and can
can cost an additional of upto P3000 worth for overtime stay.
Physically for the patient. It can cause dehydration, electrolyte
imbalance, wound dehiscence and other complications. And
PONV maybe the only experience that the patient remembers
and this is a very important cause of patient dissatisfaction.
PONV Process Risk Factors for PONV
The risk for PONV is best predicted by a simplified risk score.
Risk factors include female gender, nonsmoking status, history of
PONV and/or motion sickness, and use of opioids, in addition, the
type of anesthesia and the surgery also impacts PONV
What triggers nausea and vomiting?
The vomiting center located in the medulla oblongata receives Simplified Risk Score to Predict PONV in Adults
input from 4 major areas:
o GIT Risk of PONV increases with number of risk factors present
o Chemoreceptor trigger zone
CPU College of Medicine | Revised by: Victores Valetudinis | 2022 Page 4 of 6
Prevention of PONV should be induced if ≥ 2 risk factors are
present.
Risk Factors Points
Female 1
Non-smoker 1
History of PONV/Motion Sickness 1
Post-operative opioids 1
Sum = 0, 1, 2, 3, 4
The risk score is calculated by giving 1 point for the presence of
each risk factor. It follows that the risk of PONV increases with
the number of risk factors present.
Gender is the strongest patient-specific predictor
3-4x more likely to have PONV
Etiology is unknown but it is associated with higher levels of
progesterone, estrogen
Higher incidence in reproductive period and declines at age 70.
Risk Factors for PONV
After assessing patient risk and reducing baseline risk factors, ANTIEMETIC DRUGS
guidelines recommend prophylaxis for moderate risk patients
using 1 to 2 interventions with the following drugs. And for high-
First-line Antiemetics
risk patients – a multimodal approach is suggested.
ASA 2002
o Prophylaxis with: Three classes with similar efficacy and a relative reduction risk of
~25%
5 HT3 RA, Droperidol, Dexamethasone,
o 5HT3 RAs
Metoclopramide, 5 HT3 RA + Dexa
o If required, rescue with 5 HT3 RA o Corticosteroids
o Dopamine antagonists
ASPAN 2006
o Prophylaxis with 1 or more: Act independently
Have additive effects when used in combination
5 HT3 RA, Droperidol, Dexamethasone, H1 receptor
blocker, Transdermal scopolamine
Second-line Antiemetics
o If required, rescue with Promethazine, Prochlorperazine or
Metoclopramide
SAMBA 2007 Drugs with less favorable side effect profiles or limited efficacy
o Assess patient risk o Metoclopramide
o Reduce baseline risk factors o Haloperidol
o Moderate risk: Prophylaxis with 1-2 interventions: o Dimenhydrinate
5 HT3 RA, Droperidol, Haloperidol, Dexamethasone, H1 o Transdermal Scopolamine
receptor blocker, Transdermal scopolamine,
Promethazine, Ephedrine SPINAL HEADACHE
o High risk- multimodal approach
o If required administer another category of agent Occurs after a neuroaxial anesthesia, more commonly spinal than
Samba 2014 - What’s New? dural. Worsens when standing up, relieved by lying down and
o Risk scoring system for PDNV intake of NSAIDs.
o New antiemetics (palonosetron, neurokinin-1 RA) Leakage of CSF from the dura can cause reduced intracranial
pressure aggravated by sitting up
Algorithm for PONV Prophylaxis Headache after spinal anesthesia which is worsened when sitting
up
NSAIDs can be given for pain relief
Increased fluid intake and lying flat
OTHERS
Delirium: in 10% of patients, common in elderly
Emergency excitement: transient confusional state common in
children
Delayed awakening
o Response to stimulation after anesthesia should occur within
60-90 minutes
o Residual sedative: most common cause
Sore throat
Damage to teeth, lips and tongue
Damage to eyes during GA
CPU College of Medicine | Revised by: Victores Valetudinis | 2022 Page 5 of 6
Nerve damage Figure 16. Relationship between Stress Levels and
o Complications may be avoided by performing with due care Performance Happiness and Health
during intubation
HAZARDS IN ANESTHESIA There must be balance between happiness and stress. As future
doctors, you must remember that time management is important
Biological to maintain a balance in your life.
Mechanical
Chemical REFERENCES
Physical
Personal Dr. Hofileña’s PowerPoint Presentattion
MAM Trans
Biological Hazards
Infectious diseases
Precautions should be exercised:
o Prevent infection between patients-anesthesiologist
o Hand hygiene
o Sterilization of all equipment
o Dispose onetime use equipment
Mechanical Hazards
Injury and harm to the anesthesiologist in the workplace
o Slips and falls
o Burns
Chemical Hazards
Noxious pollutants
Anesthetic gases
Fire and explosion
Physical Hazards
Noise pollution
Physical injury: orthopedic, soft tissue injury, eye injury
Electrical hazards
Radiation and nuclear hazards
Personal Hazards
Drug use and addiction: 1-15 doctors with drug or alcohol abuse
Stress and burnout
Exhaustion and fatigue: mental, physical and emotional
Suicide
o More common in anesthesiologists compared to other
specialties because of high levels of stress
CPU College of Medicine | Revised by: Victores Valetudinis | 2022 Page 6 of 6
You might also like
- Anger Management Best Practice HandbookDocument122 pagesAnger Management Best Practice HandbookRomanic Mihaela100% (6)
- USMLE Step 3 Sample Questions For The Test PDFDocument69 pagesUSMLE Step 3 Sample Questions For The Test PDFmarkNo ratings yet
- Basic Concept On NeuroanesthesiaDocument51 pagesBasic Concept On Neuroanesthesiabrojeem100% (1)
- Cardiac Stress Testing - Choosing The Right Test and WhenDocument75 pagesCardiac Stress Testing - Choosing The Right Test and WhenLakshmi PrasannaNo ratings yet
- ATLS - Head Trauma ImodifiedDocument39 pagesATLS - Head Trauma ImodifiedSammon TareenNo ratings yet
- Sterility Testing - Pics PDFDocument15 pagesSterility Testing - Pics PDFdepardieu1973100% (2)
- Presentation of Neurogenic Shock Within The Emergency Department - TaylorDocument6 pagesPresentation of Neurogenic Shock Within The Emergency Department - TaylorAnprtma kaunangNo ratings yet
- Nursing and Midwifery Continuing Professional Development Registration Standard PDFDocument2 pagesNursing and Midwifery Continuing Professional Development Registration Standard PDFwandyhuseinNo ratings yet
- Anaesthesia On The MoveDocument244 pagesAnaesthesia On The MoveLucas ArenasNo ratings yet
- Fall Prevention Presentation1Document26 pagesFall Prevention Presentation1pam937100% (1)
- Drugs Used For Treatment Stable Angina PectorisDocument29 pagesDrugs Used For Treatment Stable Angina PectorisAditya Andra PerdanaNo ratings yet
- Work Comp C4Document5 pagesWork Comp C4ijustwanawriteNo ratings yet
- AONE Nursing CompetenciesDocument11 pagesAONE Nursing CompetenciesAmi NoviantiNo ratings yet
- Optic Neuropathy With Papilledema PDFDocument25 pagesOptic Neuropathy With Papilledema PDFCarolina Jaramillo100% (1)
- Harvard Mens Health Watch January 2021 Harvard HealthDocument8 pagesHarvard Mens Health Watch January 2021 Harvard HealthJefferson Medinaceli MalayaoNo ratings yet
- Complicaciones Del Bloqueo NA 2019Document5 pagesComplicaciones Del Bloqueo NA 2019Alberto ZamoraNo ratings yet
- Neuropathic Pain in Daily Practice: Teddy Wijatmiko, DR - SP.SDocument52 pagesNeuropathic Pain in Daily Practice: Teddy Wijatmiko, DR - SP.Svaen ronaNo ratings yet
- Spinal 2 Chloroprocaine A Comparison With.20Document6 pagesSpinal 2 Chloroprocaine A Comparison With.20Prakarsa Adi Daya NusantaraNo ratings yet
- Neuropathic Pain in Daily Practice: Teddy Wijatmiko, DR - SP.SDocument52 pagesNeuropathic Pain in Daily Practice: Teddy Wijatmiko, DR - SP.SeciNo ratings yet
- Anesthetic ComplicationsDocument2 pagesAnesthetic ComplicationsIsabel CastilloNo ratings yet
- Chapt 3Document5 pagesChapt 3Javier Farias VeraNo ratings yet
- CH 79Document6 pagesCH 79alimonyNo ratings yet
- Anestesia en OftalmologiaDocument39 pagesAnestesia en OftalmologiaTan FloresNo ratings yet
- Anesthesia in Ophthal Mic SurgeryDocument98 pagesAnesthesia in Ophthal Mic SurgeryT Z BenNo ratings yet
- Neurogenic ShockDocument16 pagesNeurogenic ShockAnonymous iEGRcEp2VjNo ratings yet
- FK UWM Spine FractureDocument11 pagesFK UWM Spine FractureEmiliana AnggrainiNo ratings yet
- 15 Complications of Regional AnaesthesiaDocument6 pages15 Complications of Regional AnaesthesiaParvathy R NairNo ratings yet
- Local Anesthetics: Richard D. Minshall, PHD Tobias Piegeler, MDDocument40 pagesLocal Anesthetics: Richard D. Minshall, PHD Tobias Piegeler, MDJohnBedaLatawanMalecdanNo ratings yet
- 290 Residual Neuromuscular Blockade PDFDocument8 pages290 Residual Neuromuscular Blockade PDFade winataNo ratings yet
- SPAPedi Crisis Checklists March 2023Document31 pagesSPAPedi Crisis Checklists March 2023marjana.burmuzoskaNo ratings yet
- Revchilanestv49n01 17-1Document5 pagesRevchilanestv49n01 17-1claudia YamunaquéNo ratings yet
- General Comments: Chair's Report Final Exam 2017.2Document16 pagesGeneral Comments: Chair's Report Final Exam 2017.2Jane KoNo ratings yet
- Case 6Document41 pagesCase 6Christian Dave EndinoNo ratings yet
- OpticIschemia BiousseDocument9 pagesOpticIschemia BiousseyetyningsyNo ratings yet
- Hypertensive Emergency 3Document45 pagesHypertensive Emergency 3saldy meirisandyNo ratings yet
- Regional AnesthesiaDocument50 pagesRegional Anesthesiaapi-28163301No ratings yet
- Advancesinanesthesia Monitoring: Yi Deng,, Jovany Cruz Navarro,, Sandeep MarkanDocument9 pagesAdvancesinanesthesia Monitoring: Yi Deng,, Jovany Cruz Navarro,, Sandeep MarkanUmer HussainNo ratings yet
- Assessment and Concept Map Care Plan: Elizabeth RouxDocument6 pagesAssessment and Concept Map Care Plan: Elizabeth Rouxapi-507304905No ratings yet
- Regional Anesthesia Is Much Better Than General AnesthesiaDocument21 pagesRegional Anesthesia Is Much Better Than General Anesthesiaapi-28163301No ratings yet
- An Unusual Laryngeal Complication Following Inferior Alveolar Nerve BlockDocument2 pagesAn Unusual Laryngeal Complication Following Inferior Alveolar Nerve BlockJaime Ruiz Jr.No ratings yet
- Bedside Monitor: BSM-3000 SeriesDocument8 pagesBedside Monitor: BSM-3000 Seriesfarouk beNo ratings yet
- Colombian Journal of Anesthesiology: Revista Colombiana de AnestesiologíaDocument4 pagesColombian Journal of Anesthesiology: Revista Colombiana de AnestesiologíaSuci dwi CahyaNo ratings yet
- Nefropatías ÓpticasDocument9 pagesNefropatías Ópticasgabyc164No ratings yet
- (C) (I) Intraoperative in The Care of This PatientDocument1 page(C) (I) Intraoperative in The Care of This PatientkushishaNo ratings yet
- Monitor Bedside BSM-3000 SeriesDocument8 pagesMonitor Bedside BSM-3000 SeriesDouglas Gaitan PotosmeNo ratings yet
- Chair's Report Final Exam 2019.2: General CommentsDocument21 pagesChair's Report Final Exam 2019.2: General CommentsJane KoNo ratings yet
- Current Evaluation and Management of Head Injury - DR EB-East ParkDocument60 pagesCurrent Evaluation and Management of Head Injury - DR EB-East ParkLanlan LesmanaNo ratings yet
- EPTI 神NoteDocument6 pagesEPTI 神NoteChow Man HeiNo ratings yet
- MalamedDocument8 pagesMalamedDr. DhDhNo ratings yet
- Anaesthesia On The Move PDFDocument256 pagesAnaesthesia On The Move PDFSanna Huhtamaki100% (1)
- Can We and Should We Use FFR IFR RFR To Guide The Bifurcation StrategyDocument20 pagesCan We and Should We Use FFR IFR RFR To Guide The Bifurcation Strategyrainmed USNo ratings yet
- Package Insert - JYNNEOSDocument11 pagesPackage Insert - JYNNEOSІрина НовіковаNo ratings yet
- Outcome 2016 (Khoá gây tê vùng dưới hướng dẫn siêu âm ĐHYHN)Document40 pagesOutcome 2016 (Khoá gây tê vùng dưới hướng dẫn siêu âm ĐHYHN)Rùa’s Anesthesia HanoiNo ratings yet
- Neurocritical Care in The General Intensive Care UnitDocument17 pagesNeurocritical Care in The General Intensive Care UnitdanielNo ratings yet
- Perioperative ArrhythmiaDocument66 pagesPerioperative ArrhythmiaVithal DhulkhedNo ratings yet
- ATLS - Head Trauma ImodifiedDocument39 pagesATLS - Head Trauma ImodifiedSammon TareenNo ratings yet
- Facial Neuralgias - ReviewDocument12 pagesFacial Neuralgias - ReviewDr. AtheerNo ratings yet
- Upper Extremity Block Review 1141-1160Document67 pagesUpper Extremity Block Review 1141-1160Cinthia Gonzalez NunezNo ratings yet
- Thunderclap Headache: Anne Ducros, Marie-Germaine BousserDocument4 pagesThunderclap Headache: Anne Ducros, Marie-Germaine BousserLeidy Carolina Salazar ChicaNo ratings yet
- Traumatic Optic NeuropatyDocument10 pagesTraumatic Optic NeuropatyArys SetiawanNo ratings yet
- (Anes) Regional AnesDocument2 pages(Anes) Regional Anesalmira.s.mercadoNo ratings yet
- Final NotesDocument19 pagesFinal NotesJennNo ratings yet
- Vol2 Issue2Document4 pagesVol2 Issue2Aazam AdtechiesNo ratings yet
- Presentation of Neurogenic Shock Within The Emergency Department.Document6 pagesPresentation of Neurogenic Shock Within The Emergency Department.delia wjyNo ratings yet
- Roams Review of All Medical Subjects Pdfdrivecom PDF PDF FreeDocument31 pagesRoams Review of All Medical Subjects Pdfdrivecom PDF PDF FreeBiswajitNo ratings yet
- Promoting Clear Identification of Sepsis, Severe Sepsis & Septic ShockDocument18 pagesPromoting Clear Identification of Sepsis, Severe Sepsis & Septic ShockArif Ardi AntoNo ratings yet
- Complex Care Concept MapDocument6 pagesComplex Care Concept Mapapi-740628337No ratings yet
- Pre-Invasive Lesions of The Cervix 2020Document58 pagesPre-Invasive Lesions of The Cervix 2020Jeno Luis J. ACUBNo ratings yet
- Trans-Viva-Anes-Lec 11-Pain ManagementDocument4 pagesTrans-Viva-Anes-Lec 11-Pain ManagementJeno Luis J. ACUBNo ratings yet
- Pediatric Growth and Development in A NutshellDocument25 pagesPediatric Growth and Development in A NutshellJeno Luis J. ACUBNo ratings yet
- Fluids and Electrolytes For PediatricsDocument31 pagesFluids and Electrolytes For PediatricsJeno Luis J. ACUBNo ratings yet
- Patient Rights and Responsibilities Legal Medicine Group 2Document1 pagePatient Rights and Responsibilities Legal Medicine Group 2Jeno Luis J. ACUBNo ratings yet
- Quizzes or Shifting ExamsDocument5 pagesQuizzes or Shifting ExamsJeno Luis J. ACUBNo ratings yet
- Labortory Test or ManeuverDocument2 pagesLabortory Test or ManeuverJeno Luis J. ACUBNo ratings yet
- Hemodynamics and Diagnosis Venous Disease-Jvs 1207Document21 pagesHemodynamics and Diagnosis Venous Disease-Jvs 1207Fahrudin ŠabanovićNo ratings yet
- Various Methods of Ligation Ties: Review ArticleDocument6 pagesVarious Methods of Ligation Ties: Review ArticleDivine Macaranas CordovizNo ratings yet
- Arixtra: (Fondaparinux Sodium) InjectionDocument26 pagesArixtra: (Fondaparinux Sodium) InjectionTri Purma SariNo ratings yet
- Infrared Thermal Imaging Identifies Kissing Spines in HorseDocument2 pagesInfrared Thermal Imaging Identifies Kissing Spines in HorseBeckyTengesNo ratings yet
- Practice Test 1Document10 pagesPractice Test 1Riin IrasustaNo ratings yet
- AbtVitalsilRe MushroomDocument2 pagesAbtVitalsilRe Mushroommds9216No ratings yet
- Rational Use of The Drug (Rud) : Rovina Ruslami, DR., SPPD, PHDDocument31 pagesRational Use of The Drug (Rud) : Rovina Ruslami, DR., SPPD, PHDamaliaramadhaniNo ratings yet
- Scenario 2, IzzahpartDocument4 pagesScenario 2, IzzahpartNur Izzah ImranNo ratings yet
- New Report About Holyoke Soldiers' HomeDocument10 pagesNew Report About Holyoke Soldiers' HomeMike PlaisanceNo ratings yet
- Seizure Updated ILAE ClassificationDocument12 pagesSeizure Updated ILAE ClassificationNasheei RadjaNo ratings yet
- V.Bontilao Sr. Integrated School Summative Test in English 7Document6 pagesV.Bontilao Sr. Integrated School Summative Test in English 7Nevaeh CarinaNo ratings yet
- نسخة نسخة الاشعةDocument10 pagesنسخة نسخة الاشعةDina MohamedNo ratings yet
- 11 Farmakokinetika Klinik Antibiotika Aminoglikosida PDFDocument19 pages11 Farmakokinetika Klinik Antibiotika Aminoglikosida PDFIrfanSektionoNo ratings yet
- False Advertisement Gluten Free FoodDocument9 pagesFalse Advertisement Gluten Free FoodElenaNo ratings yet
- Screening Questionnaire: Dha Eligibility LetterDocument2 pagesScreening Questionnaire: Dha Eligibility LetterDr. Emad Elbadawy د عماد البدويNo ratings yet
- DkaDocument32 pagesDkanatheNo ratings yet
- Fibula Wei 2018Document11 pagesFibula Wei 2018Rares CraciunNo ratings yet
- DR - Harish DurejaDocument26 pagesDR - Harish Durejaarpita_949242356No ratings yet
- Sadhana Intensive CourseDocument16 pagesSadhana Intensive Courseapi-241382210No ratings yet
- This Study Resource WasDocument3 pagesThis Study Resource WasCarlito AglipayNo ratings yet
- Hospital Network in IndiaDocument200 pagesHospital Network in IndiaAlex GiDeonNo ratings yet
- Auriculotherapy Manual: Chinese and Western Systems of Ear AcupunctureDocument2 pagesAuriculotherapy Manual: Chinese and Western Systems of Ear AcupunctureYh KooNo ratings yet