Professional Documents
Culture Documents
ICU One Pager Enteral Nutrition
Uploaded by
jalilCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ICU One Pager Enteral Nutrition
Uploaded by
jalilCopyright:
Available Formats
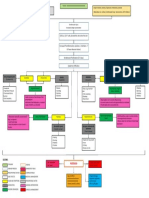
ENTERAL NUTRITION by Nick Mark MD ONE onepagericu.
com Link to the
most current
OBJECTIVES: CALCULATING CALORIC NEEDS:
@nickmmark version →
· Adequate nutrition is essential to maintain normal physiologic functions · Energy expenditure depends on mass, metabolism, & illness.
· Enteric feeding also helps maintain an important immunological barrier · It is not necessary to meet full caloric needs; many benefits of early feeding are realized with any EN. Paradoxically, achieving
· 30-50% of ICU pts are malnourished; malnutrition associated w/ worse outcomes 100% of caloric needs in the 1st week may be harmful. Thus, while early feeding is preferable the goal need not be full calories.
WHEN TO START ENTERAL FEEDS? · Simple formula to estimate basal energy expenditure (BEE) · Indirect calorimetry measures VO2 & VCO2 to calculate EE
· Early enteral nutrition (<48 hrs after onset of critical illness) is associated with 𝑩𝑬𝑬 𝒌𝒄𝒂𝒍/𝒅𝒂𝒚 = 𝟐𝟓 × 𝒘𝒆𝒊𝒈𝒉𝒕 (𝒌𝒈) 𝑬𝑬 𝒌𝒄𝒂𝒍/𝒅𝒂𝒚 = 𝟏𝟒𝟒𝟎× 𝟑. 𝟗𝟒×𝑽𝑶𝟐 + 𝟏. 𝟏𝟏×𝑽𝑪𝑶𝟐
reduced mortality and reduced incidence of infections (particularly pneumonia). For most people use actual weight. If volume overloaded, · Only possible to obtain accurate measurements if FiO2 is < 0.6
· Deliberate underfeeding is not associated with improved outcomes (PERMIT 2015) use dry weight. If obese (BMI > 30 kg/m2) use 110% of IBW. · Respiratory quotient can identify problems or fine-tune feeding:
· No survival advantage with early parenteral nutrition (EPN 2011). · Disease can modify caloric needs: · RQ >1 suggests overfeeding ! decrease carbs or lipids
· Enteral nutrition can be safely given while in the prone position or receiving TTM. · Fever 10% more calories per degree C · RQ <0.8 suggest underfeeding ! increase calories
· EN can also be given while on neuromuscular blockers or while on ECMO. · Peritonitis 20-50% more, Sepsis 40-80% more Indirect calorimetry results in more calories & protein administered.
· Trauma: 20-40% more Burns: +50-100% depends on BSA
WHEN NOT TO START ENTERAL FEEDS?
· Higher protein may be beneficial in select population(TARGET 2018)
· Early EN may be poorly tolerated in patients in shock (NUTRIREA-2); however the Use a calculator to determine the
· Most critically ill patients require 1.2-1.5 g/kg/day of protein
only absolute contraindications to initating enteral nutrition (EN) are bowel rates of a particular enteric feed.
· Patient with burns may require high protein 2 g/kg/day (add supplements if needed)
obstruction, perforation, mesenteric ischemia, or major GI bleeding. · Consider branched chain amino acids (BCAA) in patients with hepatic encephalopathy
ENTERIC FEED FORMULA: RESIDUALS:
· Formulas contain a mixtures of macronutrients (carbohydrates, lipids, & protein) as well as · Residuals are contents that remain in the stomach, after tube feeding is paused.
micronutrients (electrolytes, vitamins, & trace elements). Select based upon clinical context. · At least 500ml of residuals can be safely tolerated without intervention (REGAIN 2010)
Carbohydrate Lipids Protein · If TF are poorly tolerated (residuals >500, vomiting, gastric distension), consider the following:
· Despite theoretical basis, there is little · Maintain head up >30 degrees (good practice to prevent VAP)
clinical evidence for many novel disease 4.0 kcal/g 9 kcal/g 4.0 kcal/g Energy content · Administer pro-kinetic agents (erythromycin is superior to metaclopramide)
specific formula (ARDS, COPD, liver). · Consider advancing FT post-pyloric or into jejunum (especially if vomiting)
0.7 L/g 1.4 L/g 0.8 L/g CO2 produced · Increasingly, there is evidence for NOT checking residuals at all (less RN work, no improvement in outcomes)
· There is also limited evidence for
additives like glutamine, etc 0.9 - 1.0 0.7 0.8 Respiratory quotient FEEDING TUBES (FT):
Nasal can be used in intubated or non-intubated patients but there is a higher risk of
Formula Type Examples sinusitis among people who are intubated.
Standard (1 kcal/mL) – similar to typical US diet in terms of Ensure, Isosource, Boost, Gastric - used for bolus or continuous feeds TF formula &
carbs/lipid/protein, Used in most ICU patients Osmolite Post-pyloric & jejunal can be used hydration
50-60% 25-40% 10-15% only for continuous feeds.
Concentrated (1.5-2.0 kcal/mL) – same contents, less Ensure plus, Impact 1.5, Twocal Post-pyloric (duodenal) - small
Suction &
volume, useful in patients on fluid restriction HN, Nutren, Renal, Nutren 2.0 Decrease in pneumonia risk; Nasal feeding port
50-60% 25-40% 10-15% used in patients w/ gastric
Oral
outlet obstruction, vomiting.
High protein - useful for patients with high protein needs Isosource HN, Osmolite HN,
(>1.5 g/kg/day) Replete, Boost HP, Peptamen Jejunal - used in specific patients
Pump
45-55% 20-35% ≥20% VHP, Ensure HP, Promote (vomiting, intolerance), OJ/NJ not Vent port
superior OG/NG (ENTERIC 2013) One-way
80 ml/hr
Pre-digested (1-1.5 kcal/ml) - Low lipid content, partially Peptamen, Vivonex PLUS, anti-reflux
Consider permanent gastric
digested/easily absorbed peptides, Used in malabsorption Vivonex TEN, Alitraq valve
tube in people who require
>70% <10% 20%
FT for >4-6 weeks
v1.0 (2022-02-05) CC BY-SA 3.0
High fiber – contains soluble & insoluble fiber, used when Jevity, Ensure with fiber, Promote
Similar outcomes with Larger FTs contain a
there is persistent diarrhea on other feeds with fiber, Nutren 1.0 fiber,
intermittent & continuous small side channel to
50-60% 25-40% 10-15% Compleat, Ultracal enable air venting
tube feeds. Can use either.
Renal – Concentrated (1.5-2.0 kcal/mL), low K+ & PO4, low Nepro, Magnacal Renal, Suplena, Gastric 30-36in Smaller FTs are more
protein, used for people with renal failure Novasource Renal, Renalcal flexible but may collapse
30-40% 30-40% <20% when suction is applied
Post-pyloric 43in
Diabetic – lower carbohydrate content, used in diabetics Choice DM, Glucerna Select, (aka duodenal) The end of the FT has a
Glytrol, Diabetisource AC, radio-opaque line that is
20-40% 40% ≥20%
Jejunal >48in interrupted by side ports
You might also like
- Total Parenteral NutritionDocument12 pagesTotal Parenteral NutritionSheikhNo ratings yet
- Registered Dietitian (RD) Registered Dietitian Nutritionist (RDN)Document14 pagesRegistered Dietitian (RD) Registered Dietitian Nutritionist (RDN)Patrick Larbi AwukuNo ratings yet
- Rotation Checklist - ClinicalDocument3 pagesRotation Checklist - Clinicalapi-240994549100% (1)
- Nutrition Care Process NCP For RenalDocument17 pagesNutrition Care Process NCP For RenalJermeLou BaoNo ratings yet
- Pediatric Nutrition Guidelines For Primary Health Care Providers PDFDocument9 pagesPediatric Nutrition Guidelines For Primary Health Care Providers PDFIsa AguilarNo ratings yet
- Nutr302l NCP NotesDocument14 pagesNutr302l NCP Notesapi-271284613No ratings yet
- MNT for Diabetes Nutrition TherapyDocument27 pagesMNT for Diabetes Nutrition Therapydr.Uci BaharNo ratings yet
- NCP of Patient With GastritisDocument4 pagesNCP of Patient With GastritisBer AnneNo ratings yet
- Malnutriton Case StudyDocument4 pagesMalnutriton Case Studyapi-302848761No ratings yet
- ESPEN 2017 - Abstract BookDocument339 pagesESPEN 2017 - Abstract BookJorianditha Ramadhan100% (1)
- Nutrition Care Process Note-IcuDocument2 pagesNutrition Care Process Note-Icuapi-1032325430% (1)
- 24 HR Food RecallDocument39 pages24 HR Food RecallKon Zhen JieNo ratings yet
- MNT Case Study 1 Spring 2017Document35 pagesMNT Case Study 1 Spring 2017api-332216940No ratings yet
- Nutritional Biology Final Exam ReviewDocument9 pagesNutritional Biology Final Exam Reviewjenm1228No ratings yet
- Dietary Assessment Methods in Nutrition EpidemiologyDocument14 pagesDietary Assessment Methods in Nutrition EpidemiologyArMadea De'aMraNo ratings yet
- Nutrition Care ProcessDocument7 pagesNutrition Care ProcessALYSSA NICOLE GINESNo ratings yet
- Nutritional AssessmentDocument7 pagesNutritional AssessmentSaher YasinNo ratings yet
- Case Studies - Type 1 DiabetesDocument4 pagesCase Studies - Type 1 Diabeteszenagit1234560% (2)
- Enteral Nutrition Support Assignment 72618Document8 pagesEnteral Nutrition Support Assignment 72618api-341835458100% (1)
- Nutrition in ICUDocument18 pagesNutrition in ICUSi Thu Swe100% (2)
- PES Statement Cheat SheetDocument17 pagesPES Statement Cheat SheetCarly100% (1)
- Nutrition Intervention - What's AvailableDocument39 pagesNutrition Intervention - What's AvailablesitihawamtNo ratings yet
- Enteral Nutrition Manual Oct 2011Document51 pagesEnteral Nutrition Manual Oct 2011Salilah Mahfudz100% (1)
- Parenteral Nutrition Case StudyDocument5 pagesParenteral Nutrition Case Studyapi-349873323100% (1)
- Nutritional Assessment MethodsDocument2 pagesNutritional Assessment Methodsyaleconsultancy100% (4)
- Obesity and Esophageal DisordersFrom EverandObesity and Esophageal DisordersDhyanesh PatelNo ratings yet
- Clinical Paediatric DieteticsFrom EverandClinical Paediatric DieteticsVanessa ShawNo ratings yet
- Advanced Nutrition and Dietetics in GastroenterologyFrom EverandAdvanced Nutrition and Dietetics in GastroenterologyMiranda LomerNo ratings yet
- Advanced Nutrition and Dietetics in ObesityFrom EverandAdvanced Nutrition and Dietetics in ObesityCatherine HankeyNo ratings yet
- American Diabetes Association Guide to Nutrition Therapy for DiabetesFrom EverandAmerican Diabetes Association Guide to Nutrition Therapy for DiabetesRating: 5 out of 5 stars5/5 (1)
- Monthly Nutrition Companion: 31 Days to a Healthier LifestyleFrom EverandMonthly Nutrition Companion: 31 Days to a Healthier LifestyleNo ratings yet
- Eat Right, Live Well Understanding the Science of NutritionFrom EverandEat Right, Live Well Understanding the Science of NutritionNo ratings yet
- Present Knowledge in Nutrition: Clinical and Applied Topics in NutritionFrom EverandPresent Knowledge in Nutrition: Clinical and Applied Topics in NutritionBernadette P. MarriottNo ratings yet
- Nutrition and Drug InterrelationsFrom EverandNutrition and Drug InterrelationsJohn HathcockNo ratings yet
- Nutrition in the Chemo Chair: From an Oncology Dietitian’s PerspectiveFrom EverandNutrition in the Chemo Chair: From an Oncology Dietitian’s PerspectiveNo ratings yet
- Dietary Fibers: Chemistry and NutritionFrom EverandDietary Fibers: Chemistry and NutritionGeorge InglettRating: 4 out of 5 stars4/5 (1)
- Glucose Intake and Utilization in Pre-Diabetes and Diabetes: Implications for Cardiovascular DiseaseFrom EverandGlucose Intake and Utilization in Pre-Diabetes and Diabetes: Implications for Cardiovascular DiseaseRating: 4 out of 5 stars4/5 (1)
- Dietary Interventions in Gastrointestinal Diseases: Foods, Nutrients, and Dietary SupplementsFrom EverandDietary Interventions in Gastrointestinal Diseases: Foods, Nutrients, and Dietary SupplementsNo ratings yet
- Guidelines for Assessing Nutrition-Related Knowledge, Attitudes and PracticesFrom EverandGuidelines for Assessing Nutrition-Related Knowledge, Attitudes and PracticesNo ratings yet
- Food Chemistry and Nutrition: A Comprehensive TreatiseFrom EverandFood Chemistry and Nutrition: A Comprehensive TreatiseRating: 5 out of 5 stars5/5 (1)
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionFrom EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionNo ratings yet
- Nutrition in Surgical PatientDocument23 pagesNutrition in Surgical PatientTrịnh ThủyNo ratings yet
- Sarcoma SpecialistDocument5 pagesSarcoma SpecialistaminudinrahmanNo ratings yet
- Pancreatic Pathology For The SurgeonDocument10 pagesPancreatic Pathology For The SurgeonSanjaya SenevirathneNo ratings yet
- Superior Vena Cava SyndromeDocument57 pagesSuperior Vena Cava SyndromeKhadira MohammedNo ratings yet
- Ru 58 42150Document12 pagesRu 58 42150Efen YtNo ratings yet
- What Women SHLD Know VAW PDFDocument2 pagesWhat Women SHLD Know VAW PDFJaymar Donozo100% (1)
- Guideline AAP DMDDocument2 pagesGuideline AAP DMDarifNo ratings yet
- Lacunar InfarctsDocument14 pagesLacunar InfarctsIRENA GENINo ratings yet
- 2018:19 Crime StatsDocument220 pages2018:19 Crime StatsBusinessTech64% (14)
- DR McDaniel PSYC 3023 Abnormal Psych FA 21 Chapter 8 Dissociative POSTDocument27 pagesDR McDaniel PSYC 3023 Abnormal Psych FA 21 Chapter 8 Dissociative POSTHeather JenkinsNo ratings yet
- Expressed EmotionsDocument19 pagesExpressed EmotionsC V KRISHNAPRIYANo ratings yet
- POXVIRUS.pptDocument12 pagesPOXVIRUS.pptdrismailkm20No ratings yet
- Internal Medicine I (Junior)Document6 pagesInternal Medicine I (Junior)Joseph RishmawiNo ratings yet
- English PP2 Final Gauge PredictionDocument58 pagesEnglish PP2 Final Gauge PredictionGreg LanternNo ratings yet
- Chronic multifactorial autoimmune dermatitisDocument1 pageChronic multifactorial autoimmune dermatitisEran Mark RojasNo ratings yet
- KSADS DSM 5 Supp4 DevelopmentalDisruptiveDO FinalDocument28 pagesKSADS DSM 5 Supp4 DevelopmentalDisruptiveDO FinalKsenia Startseva-LoraNo ratings yet
- 9.emotional Disorders in ChildrenDocument31 pages9.emotional Disorders in ChildrenGERSON RYANTONo ratings yet
- CFPC 99 Topics Starter Study DocumentDocument372 pagesCFPC 99 Topics Starter Study DocumentaayceeNo ratings yet
- MCQ Final 2014Document19 pagesMCQ Final 2014JohnSon100% (1)
- Chapter 11 GastrointestinalDocument9 pagesChapter 11 GastrointestinalChyNo ratings yet
- Electroconvulsive TherapyDocument23 pagesElectroconvulsive TherapyRaymund Christopher Dela PeñaNo ratings yet
- Dr. Weny Rinawati - Important and Novel Biomarker For HepatitisDocument24 pagesDr. Weny Rinawati - Important and Novel Biomarker For Hepatitisiq_dianaNo ratings yet
- VAWC Act Protects Women and Children from ViolenceDocument9 pagesVAWC Act Protects Women and Children from ViolenceRames Ely GJNo ratings yet
- NCMB 316 Assignment NCP Part 2Document3 pagesNCMB 316 Assignment NCP Part 2I'm a PepegaNo ratings yet
- Burn ExamDocument3 pagesBurn ExamLovelights ZamoraNo ratings yet
- Internal Medicine - 84 - 110Document7 pagesInternal Medicine - 84 - 110Lorenz L. Llamas IIINo ratings yet
- Lower Back PainDocument9 pagesLower Back PainAishath Samha HussainNo ratings yet
- RetDem ScriptDocument8 pagesRetDem ScriptAlessandra Rafael TayagNo ratings yet
- Can You or Your Child Overdose On VitaminsDocument6 pagesCan You or Your Child Overdose On Vitaminsتوفيق باعبادNo ratings yet
- Harris2021-Management of Otitis Externa - Alo1677913140508Document5 pagesHarris2021-Management of Otitis Externa - Alo1677913140508Jourdy KeintjemNo ratings yet
- Antibiotic Therapy For Deep Neck AbscessDocument7 pagesAntibiotic Therapy For Deep Neck Abscessteu.yamNo ratings yet